
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Bioeng. Biotechnol. , 10 February 2022
Sec. Biomechanics
Volume 10 - 2022 | https://doi.org/10.3389/fbioe.2022.814099
 Zugui Wu1†
Zugui Wu1† Xiangling Ye1†
Xiangling Ye1† Zixuan Ye1†
Zixuan Ye1† Kunhao Hong1,2†
Kunhao Hong1,2† Zehua Chen1
Zehua Chen1 Yi Wang1
Yi Wang1 Congcong Li1
Congcong Li1 Junyi Li1
Junyi Li1 Jinyou Huang2
Jinyou Huang2 Yue Zhu3
Yue Zhu3 Yanyan Lu4*
Yanyan Lu4* Wengang Liu1,2*
Wengang Liu1,2* Xuemeng Xu1,2*
Xuemeng Xu1,2*Background: Clinical incidences of chronic low back pain among the elderly are increasing. However, studies have not fully elucidated on changes in biomechanical properties of paravertebral muscles in patients with unilateral chronic low back pain. We evaluated the changes in biomechanical properties of painful and non-painful paravertebral muscles in elderly patients with unilateral chronic low back pain.
Methods: Biomechanical properties of paravertebral muscles, including muscle tone and stiffness, in elderly patients with unilateral chronic low back pain were measured using MyotonPRO. Lumbar Lordosis and Sacral Slope were measured by magnetic resonance imaging. Cross-sectional areas of paravertebral muscles were evaluated using ImageJ software version 1.53. Chronic low back pain severity was assessed by Visual Analogue Scale (VAS) and Oswestry Disability Index (ODI) scores. The correlations between VAS scores, ODI scores, Lumbar Lordosis, Sacral Slope, cross-sectional areas (painful side), disease duration, and biomechanical properties of paravertebral muscles in the painful side were analyzed.
Results: A total of 60 elderly patients with unilateral chronic low back pain were enrolled in this study. The muscle tone and stiffness of paravertebral muscles on the painful side were significantly higher than those on the non-painful side (p < .05). Cross-sectional areas of paravertebral muscles on the painful side at the L3 level were smaller than those of the non-painful side (p < .05). The VAS scores and ODI scores were significantly positively correlated with muscle tone and stiffness of paravertebral muscles on the painful side (p < .05 and p < .01, respectively). There were no significant correlations between disease duration, cross-sectional areas (painful side), Lumbar Lordosis, or Sacral Slope and muscle tone and stiffness of paravertebral muscles on the painful side (p > .05).
Conclusion: In elderly patients with unilateral chronic low back pain, muscle tone and stiffness of paravertebral muscles on the painful side are higher than for those on the non-painful side. The asymmetry of biomechanical properties of paravertebral muscles is associated with severity of chronic low back pain.
Chronic low back pain (CLBP) is one of the leading causes of disability in the elderly (Vos et al., 2012; Morlion, 2013; GBD 2016 Disease and Injury Incidence and Prevalence Collaborators, 2017). It is defined as pain that occurs in the area from the lower back edge of the ribs to the upper edge of gluteal muscles for more than 3 months (Airaksinen et al., 2006). The pain and dysfunction caused by CLBP affect patients’ quality of life and often require medical attention, which significantly increases healthcare costs (Ma et al., 2014). At the same time, chronic low back pain is also a common cause of delayed working hours, and the economic loss caused by delayed working hours is huge (Guo et al., 1999). The increase in medical cost and the loss of working time, these factors impose a significant socio-economic burden on patients (Guo et al., 1999; Freburger et al., 2009; Ma et al., 2014; Foster et al., 2018). Biomechanical characteristics include muscle tone, stiffness, Lumbar Lordosis, Sacral Slope, etc., which are closely related to the occurrence of Lumbar and back diseases (Chaléat-Valayer et al., 2011; Andonian et al., 2015). The Sacral Slope (sagittal) was defined as the angle between the upper edge of the sacral endplate and the horizontal line. There are many evaluation methods for Sacral Slope, and the most commonly used is the four-line Cobb method. Muscle tone is the inherent pressure of a muscle when it does not contract spontaneously. Stiffness indicates the ability of a muscle to resist contraction as a result of external forces (the pressure to deform it). In addition, biomechanical properties of muscles, such as muscle tone and stiffness, form the basis for maintaining muscle functionality and are critical for maintaining body balance as well as postural stability (Masi and Hannon, 2008). Biomechanical properties of lower back muscles affect the stability of the spine (White et al., 2018). Patients with CLBP have been shown to exhibit altered muscle tone and stiffness of paravertebral muscles (Haładaj and Topol, 2016; Nair et al., 2016), which may be associated with symptoms of CLBP and underlying pathological mechanisms (Kawchuk et al., 2001). Pain increases muscle tone, which then aggravates pain, leading to improper postural control (Roland, 1986; Lo et al., 2019). Although there are many methods for treating CLBP (Rubinstein et al., 2011; Haładaj and Topol, 2016), selection of appropriate intervention measures and their effects should be clinically assessed (Kravitz et al., 1981; Shah et al., 2020). Manual palpation is often used for clinical evaluation of musculoskeletal diseases, such as lower back muscles and spine (Abbott et al., 2009; Masaki et al., 2017). However, the reliability and stability of manual palpation has not been ascertained (Seffinger et al., 2004; Jonsson and Rasmussen-Barr, 2018). MyotonPRO is a non-invasive muscle monitoring device that can quickly measure the biomechanical properties of muscles, such as muscle tone and stiffness (Aird et al., 2012; Bailey, 2013). It is highly accurate when applied to healthy people or patients (Hu et al., 2018; Lohr et al., 2018).
Differences in muscle tone and stiffness of paravertebral muscles between young patients with CLBP and healthy people have been reported (Ilahi et al., 2020). However, the study did not compare nor investigate whether there are differences on both sides (left and right) of paravertebral muscles. Although CLBP incidences in young people are gradually increasing, they are more prevalent among the elderly. However, only a limited number of studies have evaluated the biomechanical properties of paravertebral muscles in elderly CLPB patients. Previously, we reported on differences in tone and stiffness of paravertebral muscles between elderly CLBP patients and healthy people (Wu et al., 2020). Our results showed that the tone and stiffness of paravertebral muscles in patients with bilateral CLBP were significantly higher than those in healthy people. However, the elasticity of paravertebral muscles in patients with bilateral CLBP was significantly lower than that in healthy people. In addition, the study also found that the changes in biomechanical properties were related to the degree of pain. But, we only included patients with bilateral CLBP. In patients with unilateral CLBP, the non-painful side can be used as a control for the painful side (Wand et al., 2014). It is, therefore, imperative to evaluate the symmetry of muscles on both sides of the spine as this may provide critical information for clinical treatment. Liu et al. (2019) found that, when compared to the convex side, muscle tone and stiffness were significantly higher on the concave side of paravertebral muscles in adolescent patients with idiopathic scoliosis. Other studies have also reported significant differences in cross-sectional areas of paravertebral muscles between painful and non-painful sides of patients with unilateral CLBP, and that paravertebral muscle asymmetry is significantly related to CLBP (Barker et al., 2004). Therefore, there is a close association between lower back diseases and asymmetric changes in paravertebral muscles. However, studies have not evaluated the differences in biomechanical properties of paravertebral muscles between painful and non-painful sides in elderly patients with unilateral CLBP.
In this study, we used Magnetic resonance imaging (MRI) technology to measure the participants’ Lumbar Lordosis, Sacral Slope and Cross-Sectional Areas of paravertebral muscles, and MyotonPRO to measure the muscle tone and stiffness of the paravertebral muscles. We compared the muscle tone and stiffness of paravertebral muscles in the painful and non-painful sides of elderly patients with unilateral CLBP. In addition, correlations between Visual Analogue Scale (VAS) scores, Oswestry Disability Index (ODI) scores, disease duration, cross-sectional areas (CSAs) (painful side), Lumbar Lordosis, and Sacral Slope as well as biomechanical parameters of the painful paravertebral muscles were investigated. Our findings elucidate on the pathogenesis of CLBP and inform on its prevention and treatment.
Sixty (30 males and 30 females) elderly patients, aged between 60 and 75 years, with unilateral CLBP were recruited in this study. Their data were obtained from the orthopedic clinic of Guangdong Second Traditional Chinese Medicine Hospital. The inclusion criteria were (GBD 2016 Disease and Injury Incidence and Prevalence Collaborators, 2017): Aged 60–75 years (Morlion, 2013); Low back pain symptoms lasting more than 12 weeks (below the 12 thoracic vertebrae to the upper edge of the buttocks) (Vos et al., 2012); Unilateral CLBP (left and right sides are not restricted) (Airaksinen et al., 2006); No history of spinal surgery and (Ma et al., 2014) No intervention at least 4 weeks prior to inclusion in this study. The exclusion criteria were (GBD 2016 Disease and Injury Incidence and Prevalence Collaborators, 2017): Body mass index (BMI) ≥ 30 kg/m2 (Morlion, 2013); Presence of other diseases related to low back pain, including scoliosis, ankylosing spondylitis, and other related diseases (Vos et al., 2012); A history of spinal surgery (Airaksinen et al., 2006); The presence of neurological diseases, such as Parkinson’s disease among others. The research team screened and recruited eligible participants and obtained their relevant clinical information, including name, gender, age, height, weight, and information on the history of CLBP, such as disease duration and painful side among others. The research members involved in collecting basic and CLBP information for the participants were not involved in assessment of biomechanical parameters and cross-sectional areas of paravertebral muscles.
The research team member that performed this assessment had been professionally trained by Myoton and passed the professional assessment test. This researcher had more than 3 years of experience operating MyotonPRO. MyotonPRO (MyotonPRO®, Estonia) was used to measure biomechanical properties of paravertebral muscles in the orthopedic outpatient department of Guangdong Second Traditional Chinese Medicine Hospital. Before tests were performed, study participants were asked to rest on beds for 10 min to relax their muscles (Andonian et al., 2015). At the start of the test, participants were instructed to lie in prone positions with their heads in the center of the examination bed, and with their hands on both sides of the body. Before commencing the test, upper edges of the iliac spine on both sides were first palpated, the level between L3 and L4 spinous processes were determined, and then, the position between L1 to L5 spinous processes were identified and marked. The bulge of paravertebral muscles on both sides of the marked point served as the assessment site (Nair et al., 2016; Hu et al., 2018; Lo et al., 2019). The assessment begun from L1 to L5 on the left side and then on the right side. To reduce the interference of abdominal pressure fluctuations, participants were asked to hold their breath for 5 s at the end of expiration, before performing the tests (Hu et al., 2018). Two members of the research team performed the tests on a single participant, and the average of the two measurements was taken as the final value. The coefficient of variation was observed after each measurement, and if greater than 3%, the patient was reassessed. Measurements taken by MyotonPRO included those for muscle tone and stiffness.
Muscle tone and stiffness of bilateral paravertebral muscles were measured at each level from L1 to L5. The MyotonPRO probe was vertically mounted on the surface of measuring mark point, and then pressed to the appropriate depth, which was indicated by a change in light color from red to green. The device sent a mechanical pulse through the probe that stimulated the muscle, resulting in natural damping oscillations. Based on the natural damped oscillation signals, the MyotonPRO equipment automatically calculated muscle tone and stiffness. Muscle tone (F, measured in Hz) is the inherent pressure of a muscle when it does not contract spontaneously. The higher the Hz value, the higher the muscle tone (Van Deun et al., 2018). Stiffness (S, measured in N/m) indicates the ability of a muscle to resist contraction as a result of external forces (the pressure to deform it). The higher the N/m value, the higher the stiffness (Schneider et al., 2015).
The Lumbar Lordosis, Sacral Slope, and the cross-sectional areas of paravertebral muscles were measured using the Signa HDx 1.5-T MRI system (GE Healthcare, Milwaukee, WI, United States). The Signa HDx 1.5-T MRI system with a spine coil was used to obtain T2 weighted sagittal and transverse MR images: T2 weighted sagittal [repetition time (TR), 4,000 ms; echo time (TE), 100 ms; field of view (FOV), 30 cm; matrix, 320 × 256; slice thickness, 4 mm; interslice gap, 1 mm; number of excitations (NEX), 2]; T2 weighted transverse [repetition time (TR), 5,100 ms; echo time (TE), 85 ms; field of view (FOV), 16 cm; matrix, 256 × 192; slice thickness, 4 mm; interslice gap, 1 mm; number of excitations (NEX), 2)]. Single-voxel point-resolved spectroscopy sequence was set with parameters as follows: repetition time (TR), 2000 ms; echo time (TE), 35 ms; average number of signals, 64; voxel of interest (VOI), 15 × 15 × 15 mm3 (3.4 ml); and acquisition time, 164 s. The Lumbar Lordosis and Sacral Slope of all participants were measured using the MRI technology. Measurements of Lumbar Lordosis and Sacral Slope were performed by a radiologist with 10 years of experience. The Sacral Slope was defined as the angle between the upper edge of the sacral endplate and the horizontal line. Lumbar Lordosis was evaluated by the four-line method cobb angle. Measurements of Lumbar Lordosis and Sacral Slope were performed as shown in Figure 1. Participants’ lumbar and paravertebral muscles were scanned using magnetic resonance imaging to obtain cross-sectional images of intervertebral disc midpoints at levels of L1-L2, L2-L3, L3-L4, L4-L5, and L5-S1. After obtaining cross-sectional images of paravertebral muscles, a researcher traced the contours of paravertebral muscles on the screen (Figure 2). Based on profiles of paravertebral muscles, the Image J 1.53 software program (United States National Institutes of Health, Bethesda, Maryland) was used to calculate their cross-sectional areas. The researcher who performed this assay was blinded to the pain site and to other related information of participants (Tsai et al., 2021).
The visual analog scale was used to evaluate pain intensities of participants. The higher the value, the higher the pain intensity. Disability levels of participants were assessed using the Oswestry Disability Index (ODI) scale. The ODI scale consists of 10 questions, each with a score between 0 and 5. The higher the ODI score, the higher the degree of disability.
Statistical analyses were performed using SPSS version 26.0 (IBM, Armonk, New York, United States). Descriptive statistics were performed using basic information of the participants, including their age, height, weight, and disease-related information, as well as their VAS scores, ODI scores, disease duration, cross-sectional areas, Lumbar Lordosis, and Sacral Slope. The Shapiro-Wilk test was used to assess data distribution. Paired Student’s t-test was used to compare muscle tone, stiffness, and cross-sectional areas of paravertebral muscles on painful and non-painful sides. The Pearson correlation test (normal distribution) or Spearman correlation test (non-normal distribution) were used to analyze correlations between VAS scores, ODI scores, disease duration, cross-sectional areas (painful side), Lumbar Lordosis, Sacral Slope and muscle tone as well as stiffness of paravertebral muscles on the painful side. Statistical significance was set at p ≤ .05.
Sixty (30 male and 30 female) elderly participants with unilateral CLBP were recruited in this study. Every participant completed the entire trial protocol. The basic information and disease-related details of these participants are shown in Table 1.
The cross-sectional areas of paravertebral muscles on the painful side at L3 level were significantly smaller than those on the non-painful side (p < .05). However, there were no significant differences in cross-sectional areas of paravertebral muscles (painful and non-painful side) at other levels (p > .05). Table 2 shows the cross-sectional areas of paravertebral muscles of 60 participants.
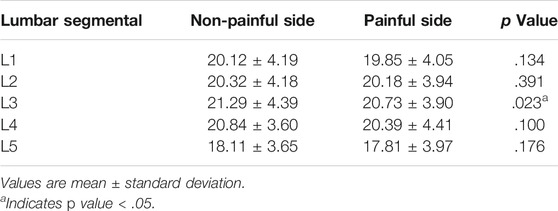
TABLE 2. The cross-sectional areas of paravertebral muscles and statistical analysis results of paired student’s t-test (n = 60).
Muscle tone on the painful side were significantly higher than those on the non-painful side (Table 3; Figures 3, 4). It was revealed that stiffness of paravertebral muscles on the painful side were significantly higher than on the non-painful side (Table 3; Figures 3, 4). There were positive correlations between biomechanical properties of paravertebral muscles on the painful side and VAS as well as ODI scores. However, there were no correlations with regards to disease duration, cross-sectional areas (painful side), Lumbar Lordosis, and Sacral Slope. VAS scores indicated that muscle tone were positively correlated with painful side paravertebral muscles. ODI scores were also positively correlated with muscle tone of paravertebral muscles on the painful side. Moreover, they were positively correlated with stiffness of paravertebral muscles on the painful side. There were no significant correlations (p > .05) between muscle tone and stiffness of paravertebral muscles on the painful side and disease duration, cross-sectional areas (painful side), Lumbar Lordosis, or Sacral Slope (Table 4).

TABLE 3. Biomechanical parameters of paravertebral muscles and statistical analysis results of paired student’s t-test (n = 60).
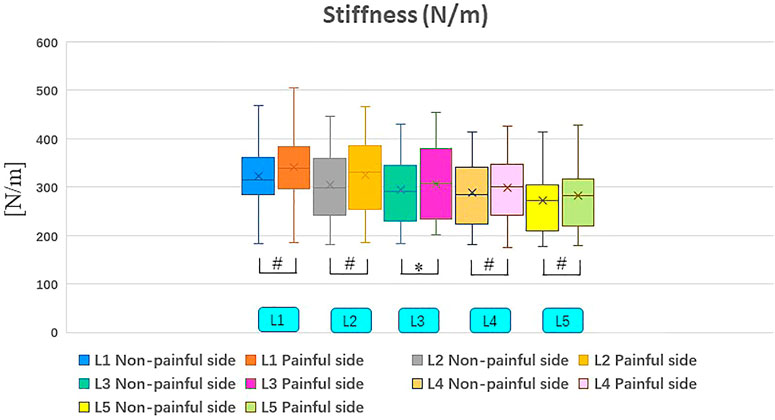
FIGURE 4. Non-painful and painful side differences in stiffness. #Indicates p value < .01; *Indicates p value < .05.
Chronic low back pain (CLBP) is caused by multiple factors. However, its pathogenesis has not been clearly established. Various hypotheses have been proposed to explain its mechanisms, including suggestions that CLBP originates from the nerves, lumbar intervertebral discs, lumbar joints, and muscles among others (Morlion, 2013). Studies also suggest that paravertebral muscles are involved in the occurrence and development of CLBP because they play an essential role in maintaining spinal stability (Hides et al., 1996; Sions et al., 2017). Elucidation of the characteristics of trunk muscles of CLBP patients can provide important information for clinical diagnosis and treatment (Sions et al., 2017). Our hypothesis that biomechanical properties of paravertebral muscles are asymmetric between the painful and non-painful sides, and that this is linked to CLBP severity, was supported in this study. However, it was unclear whether changes in biomechanical properties of paravertebral muscles occurred before or after CLBP. Overall, studies support CLBP-induced changes in paravertebral muscles.
According to some studies, morphologies of paravertebral muscles change after CLBP (Hides et al., 1994; Mannion et al., 2000). Other studies have found significant variations in cross-sectional areas of paravertebral muscles between symptomatic and asymptomatic sides of CLBP patients (Hides et al., 1994; Hides et al., 1996), which could be associated with CLBP onset (Hides et al., 2008). The decrease in cross-sectional areas of unilateral paravertebral muscles could be due to disuse atrophy or compensatory hypertrophy of contralateral paravertebral muscles (Dangaria and Naesh, 1998). Pain and an inactive lifestyle may cause paraspinal muscle atrophy, which is significantly associated with pain (Mattila et al., 1986; Danneels et al., 2000; Barker et al., 2004). Masaki et al. (2017) evaluated the relationship between CLBP and muscle stiffness using multiple regression analysis. They found that stiffness of multifidus muscles was an independent influencing factor of low back pain, therefore, they concluded that CLBP-induced muscle spasms was the possible cause for the increase in multifidus muscle stiffness (Masaki et al., 2017). Sherman (1985) investigated the relationship between CLBP and muscle contraction and found that there was a significant positive correlation between pain intensity and muscle contraction. Furthermore, compared to healthy people, CLBP patients exhibit lower muscle strength, endurance, and anti-fatigue abilities (Nicolaisen and Jørgensen, 1985; Roy et al., 1989). According to histological examinations, proportions of type I muscle fibers in muscles of CLBP patients were lower than in asymptomatic patients, the proportions of type II muscle fibers were higher, and anti-fatigue abilities of type II muscle fibers were weaker than those of type I muscle fibers (Mannion et al., 1997). Moreover, muscle stiffness can be caused by a lack of contractile activities when muscles are in a contracted state for extended periods (Park et al., 2017). Pain, among other factors, may cause the paravertebral muscles on the painful side to remain in a contracted state for a long time. Muscle mobility is normally reduced in a contracted state, resulting in changes in transverse bridges of muscle fibers and elimination of sarcomeres (Brauer and Barker, 2003). This could be one of the causes of the increase in muscle tone and stiffness. Moreover, in scoliosis patients, the side of paravertebral muscles with reduced muscle activities exhibited low proportions of type I muscle fibers and high proportions of type II muscle fibers (Mannion et al., 1998). These studies indicate that decreasing muscular activities are correlated with changes in muscular fibers, which could explain the differences in biomechanical properties of paravertebral muscles.
Previous morphological and histological studies of paravertebral muscles in CLBP patients have revealed, to a certain extent, the mechanism of changes in biomechanical properties of paravertebral muscles in patients with unilateral CLBP. The asymmetry of biomechanical properties of paravertebral muscles on painful and non-painful sides may be attributable to various factors, such as increased pain, decreased muscular activities, decreased muscular anti-fatigue abilities, changes in muscle cross-sectional areas, and higher proportions of type II muscle fibers. Although some researchers have carried out relevant studies, these results have not been confirmed by a large number of clinical trials and molecular biological experiments. We speculate that these factors may be related to the biomechanical properties of the paraspinal muscles. In the future, we hope to conduct more clinical trials and molecular biology experiments to analyze further the causes and specific mechanisms of changes in the biomechanical properties of paravertebral muscles.
We found that there were no significant correlations between disease duration and biomechanical properties of paravertebral muscles, which could be due to significant differences in disease duration among participants. Furthermore, CLBP is a pain syndrome with many causes, and disease durations are not positively correlated with CLBP severity; however, they are affected by various factors, such as pain degree and psychological factors (Chaléat-Valayer et al., 2011). Biomechanical parameters of the spine, such as Lumbar Lordosis, play an essential role in maintaining the stability of the lumbar spine (Ko et al., 2018), indicating that changes in Lumbar Lordosis and Sacral Slope are essential to CLBP occurrence. Accordingly, compared to healthy people, there are significant differences in Lumbar Lordosis and Sacral Slopes of CLBP patients with CLBP (Chaléat-Valayer et al., 2011). In addition, curvatures of the lumbar spine and biomechanical changes in the spine can change the tension and pressure of paravertebral muscles and ligaments, leading to CLBP (Jackson and McManus, 1994). We found that there were no significant correlations between Lumbar Lordosis, Sacral Slope, and biomechanical properties of paravertebral muscles. This may be due to the small sample size and to the fact that lumbar lordosis angles and sacral inclination angles for patients were within a small range. In addition, Lumbar Lordosis and Sacral Slope were affected by many factors, such as degree of pain and muscle strength.
Studies reported that cross-sectional areas of bilateral paravertebral muscles in patients with unilateral chronic low back pain are asymmetric (Chon et al., 2017). The asymmetry of cross-sectional areas of paravertebral muscles may be the cause of changes in biomechanical properties. We measured the cross-sectional areas of paravertebral muscles in patients with unilateral chronic low back pain and found that cross-sectional areas of paravertebral muscles on the painful side at L3 level were smaller than those on the non-painful side. However, this may be due to the small number of samples included in the study, and the duration of the disease in these patients was concentrated in a small range. At other levels of the lumbar spine, there were no significant changes in cross-sectional areas of paravertebral muscles or in asymmetry. However, from the measurement results, the cross-sectional area of the paravertebral muscles on the painful side and the non-painful side tends to change. Presently, influencing factors of paravertebral muscle biomechanical asymmetry in elderly patients with unilateral CLBP are unclear. However, based on previous studies involving patients with unilateral CLBP and the findings of this study, it is notable that there were significant differences between painful and non-painful paravertebral muscles, including abnormally elevated muscle tone and stiffness of the paravertebral muscles, as well as a reduction in the cross-sectional area of the paravertebral muscles, and these differences may be of the underlying pathological mechanisms of CLBP. Furthermore, these differences can be combined with other asymmetry variations in paravertebral muscles to further explore the pathogenesis of CLBP.
Besides providing a foundation for evaluating the clinical characteristics of CLBP, our findings may be provide a potential reference for assessing the effectiveness of clinical interventions. At present, many clinical interventions are used to treat CLBP, such as dry needling, myofascial release, etc. (Arguisuelas et al., 2017; Tüzün et al., 2017). However, the evaluation of clinical efficacy is mainly focused on the results reported by patients actively, and the results of subjective reports may lack objectivity. In addition, the biomechanical properties of paravertebral muscles were also used for diagnosis and evaluation of efficacy, but most of them were evaluated by manual palpation (Abbott et al., 2009; Masaki et al., 2017). The reliability of manual palpation in the clinical application was doubted by researchers (Seffinger et al., 2004; Jonsson and Rasmussen-Barr, 2018). Given that the tone and stiffness of the paravertebral muscles in patients with CLBP are higher than those of healthy people, a future study can evaluate whether clinical interventions can reduce these abnormally increased muscle tone and stiffness. Although determination of the root cause of asymmetry of biomechanical properties between painful and non-painful sides is challenging, this study forms the basis for evaluation of CLBP. Future studies should use large sample sizes to assess the specific mechanisms involved in changes in biomechanical characteristics.
This cross-sectional study has several limitations. First, with a small sample size, this study provides a preliminary analysis of biomechanical properties of paravertebral muscles in elderly patients with unilateral CLBP. Second, the results may be affected by disease characteristics of patients, such as disease duration, pain intensity, and degree of daily activities. Third, we did not control the specific pain areas of patients with unilateral chronic low back pain, such as pain in the upper, middle and lower lumbar spines. The included patients may have some bias. Fourth, MRI images are subjected to an increasing shrinking factor the further the distance from the center of the field of view. Shrinking factors at the key points used in this study could not be determined as CT scan images were not available for grometrical comparison. In future studies, these influencing factors should be strictly controlled to reduce the possibility of bias, while further increasing the sample sizes and exploring other new discoveries.
Biomechanical properties of paravertebral muscles in elderly patients with unilateral CLBP are asymmetrical, and muscle tone as well as stiffness of paravertebral muscles on the painful side are significantly higher than those on the non-painful side. Besides, asymmetric biomechanical properties of paravertebral muscles are associated with CLBP severity.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by The Ethics Committee of Guangdong Second Traditional Chinese Medicine Hospital. The patients/participants provided their written informed consent to participate in this study.
ZG-W, YY-L, WG-L, and XM-X designed the entire research program; ZG-W, XL-Y, ZX-Y, and JY-Hcollected all of the data; ZG-W, KH-H, CC-L, JY-L, Y-Z, and YY-L carried out the analysis; ZG-W, XL-Y, ZX-Y, and YY-L wrote the first draft of the manuscript; ZG-W was the main contributor to the manuscript; ZG-W, KH-H, ZH-C, Y-W, and XM-X reviewed and revised the manuscript; XM-X and WG-L oversaw the implementation of the entire research program. All authors reviewed and approved the final submitted version.
This work was supported by the Guangdong Provincial Science and Technology Innovation Strategy Special Fund (2021B1111610007); Natural Science Foundation of Guangdong Province (2021A1515011545).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We are grateful to all participants included in this study who contributed data to this study. In addition, we would also like to thank the radiologists of Guangdong Second Traditional Chinese Medicine Hospital for their guidance on MRI-related technologies.
Abbott, J. H., Flynn, T. W., Fritz, J. M., Hing, W. A., Reid, D., and Whitman, J. M. (2009). Manual Physical Assessment of Spinal Segmental Motion: Intent and Validity. Man. Ther. 14 (1), 36–44. doi:10.1016/j.math.2007.09.011
Airaksinen, O., Brox, J. I., Cedraschi, C., Hildebrandt, J., Klaber-Moffett, J., Kovacs, F., et al. (2006). Chapter 4 European Guidelines for the Management of Chronic Nonspecific Low Back Pain. Eur. Spine J. 15, S192–S300. doi:10.1007/s00586-006-1072-1
Aird, L., Samuel, D., and Stokes, M. (2012). Quadriceps Muscle Tone, Elasticity and Stiffness in Older Males: Reliability and Symmetry Using the MyotonPRO. Arch. Gerontol. Geriatr. 55 (2), e31–e39. doi:10.1016/j.archger.2012.03.005
Andonian, B. J., Masi, A. T., Aldag, J. C., Barry, A. J., Coates, B. A., Emrich, K., et al. (2015). Greater Resting Lumbar Extensor Myofascial Stiffness in Younger Ankylosing Spondylitis Patients Than Age-Comparable Healthy Volunteers Quantified by Myotonometry. Arch. Phys. Med. Rehabil. 96 (11), 2041–2047. doi:10.1016/j.apmr.2015.07.014
Arguisuelas, M. D., Lisón, J. F., Sánchez-Zuriaga, D., Martínez-Hurtado, I., Doménech-Fernández, J., and Doménech-Fernández, J. (2017). Effects of Myofascial Release in Nonspecific Chronic Low Back Pain. Spine (Phila Pa 1976) 42 (9), 627–634. doi:10.1097/BRS.0000000000001897
Bailey, L. (2013). Parameters Representing Muscle Tone, Elasticity and Stiffness of Biceps Brachii in Healthy Older Males: Symmetry and Within-Session Reliability Using the MyotonPRO. J. Neurol. Disord. 1 (1), 1000116. doi:10.4172/2329-6895.1000116
Barker, K. L., Shamley, D. R., and Jackson, D. (2004). Changes in the Cross-Sectional Area of Multifidus and Psoas in Patients with Unilateral Back Pain. Spine 29 (22), E515–E519. doi:10.1097/01.brs.0000144405.11661.eb
Brauer, S., and Barker, R. (2003). Stroke Rehabilitation: Guidelines for Exercise and Training to Optimise Motor Skill. Aust. J. Physiother. 49 (4), 279. doi:10.1016/S0004-9514(14)60149-5
Chaléat-Valayer, E., Chaléat-Valayer, E., Mac-Thiong, J.-M., Paquet, J., Berthonnaud, E., Siani, F., et al. (2011). Sagittal Spino-Pelvic Alignment in Chronic Low Back Pain. Eur. Spine J. 20, 634–640. doi:10.1007/s00586-011-1931-2
Chon, J., Kim, H.-S., Lee, J. H., Yoo, S. D., Yun, D. H., Kim, D. H., et al. (2017). Asymmetric Atrophy of Paraspinal Muscles in Patients with Chronic Unilateral Lumbar Radiculopathy. Ann. Rehabil. Med. 41 (5), 801–807. doi:10.5535/arm.2017.41.5.801
Dangaria, T. R., and Naesh, O. (1998). Changes in Cross-Sectional Area of Psoas Major Muscle in Unilateral Sciatica Caused by Disc Herniation. Spine 23 (8), 928–931. doi:10.1097/00007632-199804150-00016
Danneels, L. A., Vanderstraeten, G. G., Cambier, D. C., Witvrouw, E. E., De Cuyper, H. J., and Danneels, L. (2000). CT Imaging of Trunk Muscles in Chronic Low Back Pain Patients and Healthy Control Subjects. Eur. Spine J. 9 (4), 266–272. doi:10.1007/s005860000190
Foster, N. E., Anema, J. R., Cherkin, D., Chou, R., Cohen, S. P., Gross, D. P., et al. (2018). Prevention and Treatment of Low Back Pain: Evidence, Challenges, and Promising Directions. The Lancet 391 (10137), 2368–2383. doi:10.1016/S0140-6736(18)30489-6
Freburger, J. K., Holmes, G. M., Agans, R. P., Jackman, A. M., Darter, J. D., Wallace, A. S., et al. (2009). The Rising Prevalence of Chronic Low Back Pain. Arch. Intern. Med. 169 (3), 251–258. doi:10.1001/archinternmed.2008.543
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators (2017). Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 328 Diseases and Injuries for 195 Countries, 1990-2016: a Systematic Analysis for the Global Burden of Disease Study 2016. Lancet 390 (10100), 1211–1259. doi:10.1016/S0140-6736(17)32154-2
Guo, H. R., Tanaka, S., Halperin, W. E., and Cameron, L. L. (1999). Back Pain Prevalence in US Industry and Estimates of Lost Workdays. Am. J. Public Health 89 (7), 1029–1035. doi:10.2105/ajph.89.7.1029
Haładaj, R., and Topol, M. (2016). Multiple Impulse Therapy in the Assessment of Paraspinal Muscle Tone in Patients with Low Back Pain. Ortop Traumatol. Rehabil. 18 (6), 537–547. doi:10.5604/15093492.1230520
Hides, J. A., Richardson, C. A., and Jull, G. A. (1996). Multifidus Muscle Recovery Is Not Automatic after Resolution of Acute, First-Episode Low Back Pain. Spine 21 (23), 2763–2769. doi:10.1097/00007632-199612010-00011
Hides, J. A., Stokes, M. J., Saide, M., Jull, G. A., and Cooper, D. H. (1994). Evidence of Lumbar Multifidus Muscle Wasting Ipsilateral to Symptoms in Patients with Acute/subacute Low Back Pain. Spine 19 (2), 165–172. doi:10.1097/00007632-199401001-00009
Hides, J., Gilmore, C., Stanton, W., and Bohlscheid, E. (2008). Multifidus Size and Symmetry Among Chronic LBP and Healthy Asymptomatic Subjects. Man. Ther. 13 (1), 43–49. doi:10.1016/j.math.2006.07.017
Hu, X., Lei, D., Li, L., Leng, Y., Yu, Q., Wei, X., et al. (2018). Quantifying Paraspinal Muscle Tone and Stiffness in Young Adults with Chronic Low Back Pain: a Reliability Study. Sci. Rep. 8 (1), 14343. doi:10.1038/s41598-018-32418-x
Ilahi, S., T. Masi, A., White, A., Devos, A., Henderson, J., and Nair, K. (2020). Quantified Biomechanical Properties of Lower Lumbar Myofascia in Younger Adults with Chronic Idiopathic Low Back Pain and Matched Healthy Controls. Clin. Biomech. 73, 78–85. doi:10.1016/j.clinbiomech.2019.12.026
Jackson, R. P., and McManus, A. C. (1994). Radiographic Analysis of Sagittal Plane Alignment and Balance in Standing Volunteers and Patients with Low Back Pain Matched for Age, Sex, and Size. Spine 19 (14), 1611–1618. doi:10.1097/00007632-199407001-00010
Jonsson, A., and Rasmussen-Barr, E. (2018). Intra- and Inter-rater Reliability of Movement and Palpation Tests in Patients with Neck Pain: A Systematic Review. Physiother. Theor. Pract. 34 (3), 165–180. doi:10.1080/09593985.2017.1390806
Kawchuk, G. N., Kaigle, A. M., Holm, S. H., Rod Fauvel, O., Ekström, L. L., Hansson, T., et al. (2001). The Diagnostic Performance of Vertebral Displacement Measurements Derived from Ultrasonic Indentation in an In Vivo Model of Degenerative Disc Disease. Spine 26 (12), 1348–1355. doi:10.1097/00007632-200106150-00018
Ko, K.-J., Ha, G.-C., Yook, Y.-S., and Kang, S.-J. (2018). Effects of 12-week Lumbar Stabilization Exercise and Sling Exercise on Lumbosacral Region Angle, Lumbar Muscle Strength, and Pain Scale of Patients with Chronic Low Back Pain. J. Phys. Ther. Sci. 30 (1), 18–22. doi:10.1589/jpts.30.18
Kravitz, E., Moore, M. E., and Glaros, A. (1981). Paralumbar Muscle Activity in Chronic Low Back Pain. Arch. Phys. Med. Rehabil. 62 (4), 172–176.
Liu, Y., Pan, A., Hai, Y., Li, W., Yin, L., and Guo, R. (2019). Asymmetric Biomechanical Characteristics of the Paravertebral Muscle in Adolescent Idiopathic Scoliosis. Clin. Biomech. 65, 81–86. doi:10.1016/j.clinbiomech.2019.03.013
Lo, W. L. A., Yu, Q., Mao, Y., Li, W., Hu, C., and Li, L. (2019). Lumbar Muscles Biomechanical Characteristics in Young People with Chronic Spinal Pain. BMC Musculoskelet. Disord. 20 (1), 559. doi:10.1186/s12891-019-2935-z
Lohr, C., Braumann, K.-M., Reer, R., Schroeder, J., and Schmidt, T. (2018). Reliability of Tensiomyography and Myotonometry in Detecting Mechanical and Contractile Characteristics of the Lumbar Erector Spinae in Healthy Volunteers. Eur. J. Appl. Physiol. 118 (7), 1349–1359. doi:10.1007/s00421-018-3867-2
Ma, V. Y., Chan, L., and Carruthers, K. J. (2014). Incidence, Prevalence, Costs, and Impact on Disability of Common Conditions Requiring Rehabilitation in the United States: Stroke, Spinal Cord Injury, Traumatic Brain Injury, Multiple Sclerosis, Osteoarthritis, Rheumatoid Arthritis, Limb Loss, and Back Pain. Arch. Phys. Med. Rehabil. 95 (5), 986–995.e1. doi:10.1016/j.apmr.2013.10.032
Mannion, A. F., Käser, L., Weber, E., Rhyner, A., Dvorak, J., and Müntener, M. (2000). Influence of Age and Duration of Symptoms on Fibre Type Distribution and Size of the Back Muscles in Chronic Low Back Pain Patients. Eur. Spine J. 9 (4), 273–281. doi:10.1007/s005860000189
Mannion, A. F., Meier, M., Grob, D., and Müntener, M. (1998). Paraspinal Muscle Fibre Type Alterations Associated with Scoliosis: an Old Problem Revisited with New Evidence. Eur. Spine J. 7 (4), 289–293. doi:10.1007/s005860050077
Mannion, A. F., Weber, B. R., Dvorak, J., Grob, D., and Müntener, M. (1997). Fibre Type Characteristics of the Lumbar Paraspinal Muscles in normal Healthy Subjects and in Patients with Low Back Pain. J. Orthop. Res. 15 (6), 881–887. doi:10.1002/jor.1100150614
Masaki, M., Aoyama, T., Murakami, T., Yanase, K., Ji, X., Tateuchi, H., et al. (2017). Association of Low Back Pain with Muscle Stiffness and Muscle Mass of the Lumbar Back Muscles, and Sagittal Spinal Alignment in Young and Middle-Aged Medical Workers. Clin. Biomech. 49, 128–133. doi:10.1016/j.clinbiomech.2017.09.008
Masi, A. T., and Hannon, J. C. (2008). Human Resting Muscle Tone (HRMT): Narrative Introduction and Modern Concepts. J. Bodywork Mov. Therapies 12 (4), 320–332. doi:10.1016/j.jbmt.2008.05.007
Mattila, M., Hurme, M., Alaranta, H., Paljärvi, L., Kalimo, H., Falck, B., et al. (1986). The Multifidus Muscle in Patients with Lumbar Disc Herniation. Spine 11 (7), 732–738. doi:10.1097/00007632-198609000-00013
Morlion, B. (2013). Chronic Low Back Pain: Pharmacological, Interventional and Surgical Strategies. Nat. Rev. Neurol. 9 (8), 462–473. doi:10.1038/nrneurol.2013.130
Nair, K., Masi, A. T., Andonian, B. J., Barry, A. J., Coates, B. A., Dougherty, J., et al. (2016). Stiffness of Resting Lumbar Myofascia in Healthy Young Subjects Quantified Using a Handheld Myotonometer and Concurrently with Surface Electromyography Monitoring. J. Bodywork Mov. Therapies 20 (2), 388–396. doi:10.1016/j.jbmt.2015.12.005
Nicolaisen, T., and Jørgensen, K. (1985). Trunk Strength, Back Muscle Endurance and Low-Back Trouble. Scand. J. Rehabil. Med. 17 (3), 121–127. doi:10.1037//0090-5550.30.3.157
Park, S. K., Yang, D. J., Kim, J. H., Heo, J. W., Uhm, Y. H., and Yoon, J. H. (2017). Analysis of Mechanical Properties of Cervical Muscles in Patients with Cervicogenic Headache. J. Phys. Ther. Sci. 29 (2), 332–335. doi:10.1589/jpts.29.332
Roland, M. O. (1986). A Critical Review of the Evidence for a Pain-Spasm-Pain Cycle in Spinal Disorders. Clin. Biomech. 1 (2), 102–109. doi:10.1016/0268-0033(86)90085-9
Roy, S. H., De Luca, C. J., and Casavant, D. A. (1989). Lumbar Muscle Fatigue and Chronic Lower Back Pain. Spine 14 (9), 992–1001. doi:10.1097/00007632-198909000-00014
Rubinstein, S. M., van Middelkoop, M., Assendelft, W. J. J., de Boer, M. R., and van Tulder, M. W. (2011). Spinal Manipulative Therapy for Chronic Low-Back Pain. Spine 36 (13), E825–E846. doi:10.1097/BRS.0b013e3182197fe1
Schneider, S., Peipsi, A., Stokes, M., Knicker, A., and Abeln, V. (2015). Feasibility of Monitoring Muscle Health in Microgravity Environments Using Myoton Technology. Med. Biol. Eng. Comput. 53 (1), 57–66. doi:10.1007/s11517-014-1211-5
Seffinger, M. A., Najm, W. I., Mishra, S. I., Adams, A., Dickerson, V. M., Murphy, L. S., et al. (2004). Reliability of Spinal Palpation for Diagnosis of Back and Neck Pain. Spine 29 (19), E413–E425. doi:10.1097/01.brs.0000141178.98157.8e
Shah, J., Tanwar, T., Iram, I., Aldabbas, M., and Veqar, Z. (2020). Effect of Increased Lumbar Lordosis on Lumbar Multifidus and Longissimus Thoracis Activation during Quadruped Exercise in Patients with Chronic Low Back Pain: An EMG Study. J. Appl. Biomech. 36, 436–443. doi:10.1123/jab.2020-0040
Sherman, R. A. (1985). Relationships between Strength of Low Back Muscle Contraction and Reported Intensity of Chronic Low Back Pain. Am. J. Phys. Med. Rehabil. 64 (4), 190–200. doi:10.1016/0304-3959(84)90683-3
Sions, J. M., Elliott, J. M., Pohlig, R. T., and Hicks, G. E. (2017). Trunk Muscle Characteristics of the Multifidi, Erector Spinae, Psoas, and Quadratus Lumborum in Older Adults with and without Chronic Low Back Pain. J. Orthop. Sports Phys. Ther. 47 (3), 173–179. doi:10.2519/jospt.2017.7002
Tsai, J.-Y., Hung, I. Y., Guo, Y. L., Jan, Y.-K., Lin, C.-Y., Shih, T. T.-F., et al. (2021). Lumbar Disc Herniation Automatic Detection in Magnetic Resonance Imaging Based on Deep Learning. Front. Bioeng. Biotechnol. 9, 708137. doi:10.3389/fbioe.2021.708137
Tüzün, E. H., Gildir, S., Angın, E., Tecer, B. H., Dana, K. Ö., and Malkoç, M. (2017). Effectiveness of Dry Needling versus a Classical Physiotherapy Program in Patients with Chronic Low-Back Pain: a Single-Blind, Randomized, Controlled Trial. J. Phys. Ther. Sci. 29 (9), 1502–1509. doi:10.1589/jpts.29.1502
Van Deun, B., Hobbelen, J. S. M., Cagnie, B., Van Eetvelde, B., Van Den Noortgate, N., and Cambier, D. (2018). Reproducible Measurements of Muscle Characteristics Using the MyotonPRO Device: Comparison between Individuals with and without Paratonia. J. Geriatr. Phys. Ther. 41 (4), 194–203. doi:10.1519/JPT.0000000000000119
Vos, T., Flaxman, A. D., Naghavi, M., Lozano, R., Michaud, C., Ezzati, M., et al. (2012). Years Lived with Disability (YLDs) for 1160 Sequelae of 289 Diseases and Injuries 1990-2010: a Systematic Analysis for the Global Burden of Disease Study 2010. Lancet 380, 2163–2196. doi:10.1016/S0140-6736(12)61729-2
Wand, B. M., Catley, M. J., Luomajoki, H. A., O'Sullivan, K. J., Di Pietro, F., O'Connell, N. E., et al. (2014). Lumbar Tactile Acuity Is Near Identical between Sides in Healthy Pain-free Participants. Man. Ther. 19 (5), 504–507. doi:10.1016/j.math.2014.01.002
White, A., Abbott, H., Masi, A. T., Henderson, J., and Nair, K. (2018). Biomechanical Properties of Low Back Myofascial Tissue in Younger Adult Ankylosing Spondylitis Patients and Matched Healthy Control Subjects. Clin. Biomech. 57, 67–73. doi:10.1016/j.clinbiomech.2018.06.006
Keywords: biomechanical properties, paravertebral muscle, muscle tone, stiffness, chronic low back pain
Citation: Wu Z, Ye X, Ye Z, Hong K, Chen Z, Wang Y, Li C, Li J, Huang J, Zhu Y, Lu Y, Liu W and Xu X (2022) Asymmetric Biomechanical Properties of the Paravertebral Muscle in Elderly Patients With Unilateral Chronic Low Back Pain: A Preliminary Study. Front. Bioeng. Biotechnol. 10:814099. doi: 10.3389/fbioe.2022.814099
Received: 12 November 2021; Accepted: 17 January 2022;
Published: 10 February 2022.
Edited by:
Yang Liu, Hong Kong Polytechnic University, Hong Kong SAR, ChinaReviewed by:
Chi-Wen Lung, Asia University, TaiwanCopyright © 2022 Wu, Ye, Ye, Hong, Chen, Wang, Li, Li, Huang, Zhu, Lu, Liu and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xuemeng Xu, eHV4dWVtZW5nQDE2My5jb20=; Wengang Liu, OTE0MTk0MDc5QHFxLmNvbQ==; Yanyan Lu, OTU0MjMzNDExQHFxLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.