
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Bioeng. Biotechnol. , 05 April 2022
Sec. Biomechanics
Volume 10 - 2022 | https://doi.org/10.3389/fbioe.2022.799443
Background: This study was aimed at evaluating the changes in cup coverage (CC) and hip center of rotation (HCOR) in acetabular defects of various severities treated with acetabular revision using jumbo cups.
Methods: A total of 86 hips were included. The American Academy of Orthopedic Surgeons (AAOS) classification of these patients was as follows: 16 patients, AAOS I; 16 patients, AAOS II; and 16 patients, AAOS III. A three-dimensional (3D) implant simulation technique was used to visualize the placement of jumbo cups during revision arthroplasty. The acetabular anteversion, inclination, CC, and the HCOR were measured.
Results: The inclination and anteversion of simulated acetabular cups in AAOS I–III groups were consistent with the normal acetabular anatomy. Compared with the controls, in AAOS I–III groups, the HCOR was significantly increased and CC was significantly decreased. The HCOR elevation was significantly higher in AAOS III patients than in AAOS I (p = 0.001) and AAOS II patients (p < 0.001). The use of the jumbo cup technology for acetabular revision would decrease the CC in AAOS I–III patients to 86.47, 84.78, and 74.51%, respectively.
Conclusion: Our study demonstrated that in patients with acetabular defects, acetabular revision arthroplasty using jumbo cups will lead to decreased CC and HCOR upshift. Upon classifying these patients according to the AAOS classification, CC decreased with the severity of acetabular defects, and the elevation of the HCOR in AAOS III patients exceeded 10 mm and was significantly higher than in other patients.
With the widespread application of primary total hip arthroplasty (THA), there is an inevitable increase in the need for revision arthroplasty because of aseptic loosening, infection, recurrent dislocation, and periprosthetic fracture (Bozic et al., 2009; Aggarwal et al., 2019; Hoskins et al., 2020; Hoskins et al., 2021). Revision hip surgery is frequently performed for primary THA failure. Acetabular bone defects, a non-anatomical hip center, and complexities of the surgical technique typically make acetabular revision arthroplasty extremely challenging for the orthopedic surgeon (Solomon et al., 2018; Lochel et al., 2019). Some widely acknowledged acetabular bone defect evaluation systems and treatment principles, including the American Academy of Orthopedic Surgeons (AAOS) classification (D'Antonio et al., 1989) and Paprosky classification (Paprosky et al., 1994), play an important role in clinical practice. According to the anatomical morphology of the acetabular defect, the AAOS classification includes five types: segmental deficiencies, cavitary deficiencies, combined deficiencies, pelvic discontinuity and arthrodesis. The Paprosky classification was divided into three types based on the position of hip center of rotation (HCOR), the degree of tear drop damage, the degree of sciatic osteolysis, and the integrity of the Kohler line. These classification systems can evaluate the location and severity of bone defects. They have great guiding significance in clinical practice and help reconstruct acetabular bone defects and HCOR.
Presently, numerous surgical tools and strategies have been developed to resolve the dilemma caused by the acetabular defect. In this view, some of the approaches are a combination of compact grafting with cups (Green et al., 2018), jumbo cups (von Roth et al., 2015; McLaughlin and Lee, 2018), rings or cages (Innocenti et al., 2021), shells with a high HCOR (Russell et al., 2021), and cup–cage constructs (Wang et al., 2020). The use of jumbo cups is a common and effective technique to treat extensive acetabular defects. It offers the advantages of simplifying revision surgery, avoiding extensive bone grafting, and increasing the surface contact area between the cup and host bone (Lachiewicz and Watters, 2016). von Roth et al. (2015) conducted a 20-year follow-up study and reported that acetabular revision with a jumbo cup has good long-term results with regard to survival, radiographic stability, and clinical outcomes. Although several reports have been published on the results of jumbo cups use for revision arthroplasty (Dearborn and Harris, 2000; Moon et al., 2019), jumbo cups will result in native HCOR elevation as well as an unknown coverage with the host bone.
To our knowledge, few studies have reported on quantitative changes in the cup coverage (CC) and HCOR after revision surgery using jumbo cups, particularly for different grades of acetabular defects. Meanwhile, a previous study (Yang et al., 2017) has recommended the use of implant simulation technology to determine the position and effective bone mass of the acetabulum in a 3D environment. Based on the 3D implant simulation technology, we wondered whether multiple types of bone defects can be treated in the clinic using the jumbo component alone. In this study, we simulated the implantation of a jumbo cup for the treatment of acetabular bone defects to explore the generalizability and consequences of the jumbo technique.
Taken together, the primary goal of the present study was to use 3D implants with jumbo cups [Asians definition (Fan et al., 2008)] to simulate acetabular revision to elucidate 1) the changes of HCOR in AAOS I–III acetabular defects and identify whether there are any significant differences and 2) the extent of initial CC that can be achieved with a jumbo cup.
Between July 2015 and September 2020, 82 patients who visited our hospital for a failed acetabular cup were included. We retrospectively reviewed the preoperative computed tomography (CT) imaging data in our department. Institutional review board approval was obtained. The inclusion criteria for this study were as follows: 1) Primary THA revision involved the acetabular bone defect; 2) The revision involved unilateral hip, and the contralateral hip was normal; 3) CT imaging data were available; and 4) Jumbo cup size conformed to the definition for Asians. Of the 82 subjects, we excluded 11 subjects who had undergone THA re-revision, 10 subjects with inferior quality or no CT imaging data, and 13 subjects with revision of bilateral hips. Ultimately, we retrospectively evaluated 48 subjects (48 acetabular defects) who met the inclusion criteria. Nineteen patients (38 hips) without hip disease or deformities and with CT findings available were chosen as controls. Acetabular defects were identified by a previously described method and were classified according to the AAOS classification system (D'Antonio et al., 1989). Accordingly, 16 acetabular defects were graded as AAOS I, 16 as AAOS II, and 16 as AAOS III. Demographic data for the subjects are shown in Table 1.
Pelvic CT scans including the entire pelvis and proximal femur were obtained using a Toshiba Aquilion CT scanner (120 kVp, 320 mA, 512 × 512 matrix, and 0.5-mm slice thickness). All CT slices were saved in the Digital Imaging and Communications in Medicine format and imported into Mimics 19.0 software (Materialise NV, Leuven, Belgium) for 3D reconstruction. A metal artifact-minimizing protocol was used where possible by adjusting the gray level of the image, manually identifying the metal artifact, and restoring the existing structure. The acetabular prosthesis was removed on the premise of fully retaining the host bone.
Before the simulated implantation, the pelvic position was standardized with reference to the anterior pelvic plane defined by the bilateral anterior superior iliac spines and the pubic tubercles (Fujii et al., 2012; Yang et al., 2017) (Figure 1). The center of the jumbo cup is regarded as the HCOR, and rotation center of the contralateral hip was determined by Mose technique (Mose, 1980).

FIGURE 1. In the three-dimensional simulation, according to the left anterior superior iliac spines (L-ASIS), right anterior superior iliac spines (R-ASIS), and pubic tubercles to determine the anterior pelvic plane (APP).
According to the revision acetabular cups, a set of virtual acetabular cups was created using 3-matic 11.0 software (Materialise). The acetabular cups had a 4-mm shell thickness, and the diameter ranged from 50 to 70 mm in 2-mm intervals; then, these 3D models were imported into Mimics software in the stereolithography (STL) format.
In the 3D simulation, the inferior edge of the virtual cup should be flush with the obturator level to the extent possible to mimic the installation of the cup in a clinic. The simulated acetabular cup was marginally adjusted to reconstruct native anteversion and achieve cup inclination of 40° ± 10° within the allowable range of the real surgery, so as to maximize the preservation of the natural bone of the acetabulum. The jumbo cup size was chosen to best accommodate the anteroposterior diameter of the acetabulum with bone defect. This diameter could be adjusted to achieve maximum bone contact. The central point of the cup was considered as the HCOR.
The contact surface area between the acetabular cup and native bone was determined as the effective bone mass, and sufficient bone mass was essential for the initial stability of the implanted cup. On the basis of the implantation simulation, uncovered area (Su) of the acetabular cup was defined as the area of the surface uncovered by the native bone. The total acetabular cup surface area (St) represented the area available for surface contact. CC was calculated as the ratio of (St—Su) to St (Figure 2).
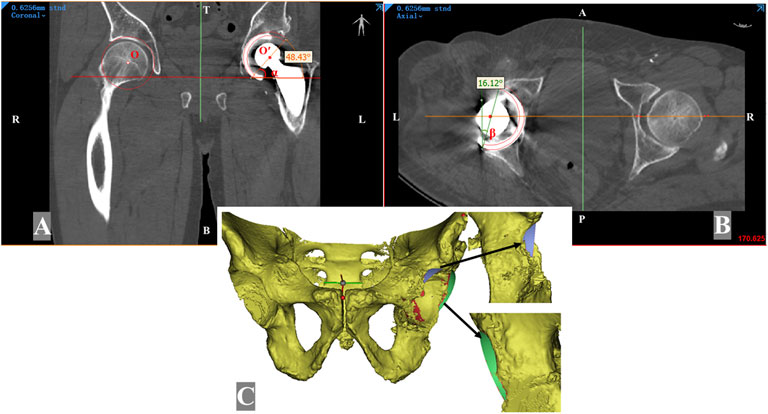
FIGURE 2. Measurement of the simulated implanted acetabular cup on the Mimics software. The reoriented planes (A, B) are resliced from the anterior pelvic plane. The hip center of rotation on the implanted acetabular cup side is marked as point O; the contralateral normal center of rotation is determined by Mose technique and marked as point O′. The vertical distance between point O and point O′ is the hip rotation center elevation. The inclination angle (α) was measured in the coronal plane (A), and the anteversion angle (β) was measured in the axial plane (B). (C) Segmentation was performed according to the border between the covered part (red region) and the uncovered part (blue region and green region) of the acetabular cup.
The distribution map of the uncovered area of the jumbo cup was created to visualize the localization of the missing bone contact. After implantation simulation, the uncovered area was delineated on the acetabular component and exported in the STL format. Then, these files were imported into Magics 22.03 software (Materialise), the uncovered areas of all sizes of cups were unified into the same side by mirror image processing and standardized to 60-mm acetabular component. All uncovered areas were overlapped on the 60-mm acetabular model to create a compilation of the uncovered areas and generate a visual heat map. To easily indicate the specific location of the loss of bone contact, a clock diagram was made according to the opening orientation of the acetabular cup.
The height difference of the HCOR was defined as the height difference between the jumbo cup and the contralateral hip center. The calculation was performed as follows. First, we identified the inferior edge of the teardrops on both sides on the coronal plane to obtain the inter-teardrop line, then the distance between both hip centers and the inter-teardrop line was measured. If unilateral teardrop osteolysis was noted, a mirror image of the contralateral teardrop was used to replace it. Furthermore, bilateral acetabular anteversion and inclination were measured in axial and coronal images, individually (Figure 2).
Statistical analysis was performed using SPSS 22.0 (IBM, Chicago, IL, United States). The significance level was set at p < 0.05, which was tested using the independent-samples Student t test. All measurements were performed by two experienced surgeons simultaneously. We used G*Power software version 3.1.9.7 (Medistat, Kiel, Germany)) to calculate the sample size of the study. Based on a confidence level of 95% (α = 0.05) and a power (1–β) of 80%, effect size = 0.43 which was calculated from our pilot tests, number of groups = 4, a total sample size of 64 samples was required. Therefore, at least 16 samples were required for each subgroup. The measurements were then repeated by one of the two surgeons with a minimum interval of 4 weeks since the previous measurement. This helped evaluate inter- and intraobserver reliability. A one-way random effects model of the intraclass correlation coefficient (ICC) was used to quantify interobserver and intraobserver reliability of the measurements to assess the reproducibility. A reliability coefficient >0.75 was considered to indicate good reliability.
The use of 3D implant simulation technology is promising for the evaluation and preoperative planning of acetabular revision arthroplasty with acetabular defects. The size and position parameters of the acetabular cups are shown in Table 2. The size of the implanted acetabular cups was significantly larger in the AAOS I–III groups than in the control group (p < 0.001). We found the inclination and anteversion of the simulated acetabular cups in the AAOS I–III groups to be mostly consistent with normal acetabular anatomy, except for the inclination in the AAOS–III group, which was significantly greater than that in the control group (44.40° ± 2.53° vs. 47.23° ± 2.55°; p = 0.001). The remaining position parameters did not statistically significantly differ among the subgroups.
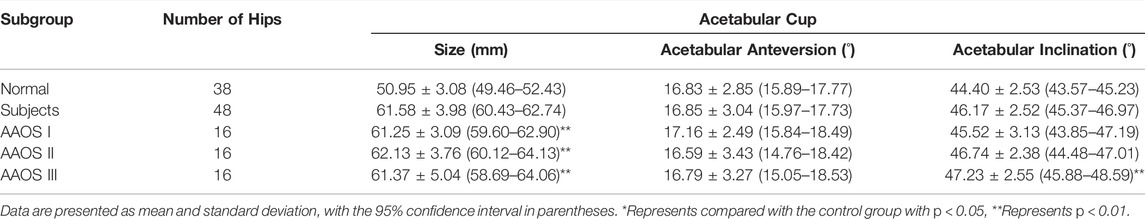
TABLE 2. The size and position parameters of implanted acetabular cups in 3-Dimensional environment.
Our 3D implant simulation results show that the jumbo cup technology can lead to HCOR elevation and provide satisfactory initial acetabular CC (Table 3). Compared with the control group, the HCOR of AAOS I–III groups was significantly increased (1.68 ± 1.07 mm vs. 7.24 ± 3.85 mm; p < 0.001). Our results showed that the heights of the HCOR in AAOS I–III were upshifted by 5.11, 5.37, and 11.25 mm, respectively. The independent-samples Student t test of these data showed that the HCOR elevation was significantly higher in the AAOS III group than in AAOS I (p = 0.001) and AAOS II groups (p < 0.001; Figure 3). Furthermore, our results showed that the use of the jumbo cup technology for acetabular revision gradually reduced the CC in AAOS I–III groups to 86.47, 84.78, and 74.51%, respectively. In addition, we found a statistically significant difference between AAOS I and AAOS III groups in this regard (p = 0.002).
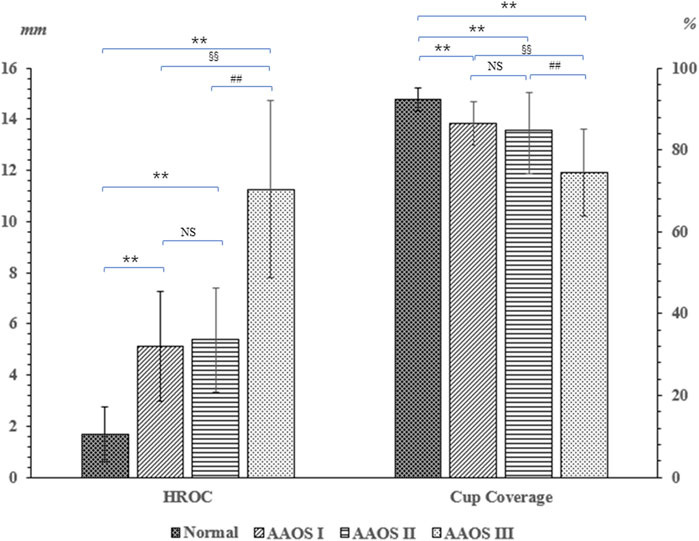
FIGURE 3. Comparison of the implanted acetabular cup hip rotation of center elevation and cup coverage in the control and AAOS I–III groups. Represents compared with the control group with p < 0.05, ** Represents p < 0.01. #p < 0.05 represents the statistical difference between the AAOS II and AAOS III; ## Represents p < 0.01. §p < 0.05 Represents the statistical difference between the AAOS I and AAOS III; §§ Represents p < 0.01.
Based on the heat map results, the localization of the missing bone contact could be clearly visualized. Our results showed that for AAOS I group undergoing acetabular revision with a jumbo cup, the location of missing bone contact was mainly concentrated in the posterior wall (1 o’clock to 3 o’clock) and anterior wall (8 o’clock to 10 o’clock) of the acetabulum (Figure 4). For AAOS II group, the results showed that the location of the bone defect was mainly concentrated in the anterosuperior wall (8 o’clock to 12 o’clock) (Figure 5). Conversely, in AAOS III group, it was mainly concentrated in the posterosuperior wall (12 o’clock to 4 o’clock) and the bottom of the acetabulum (Figure 6).
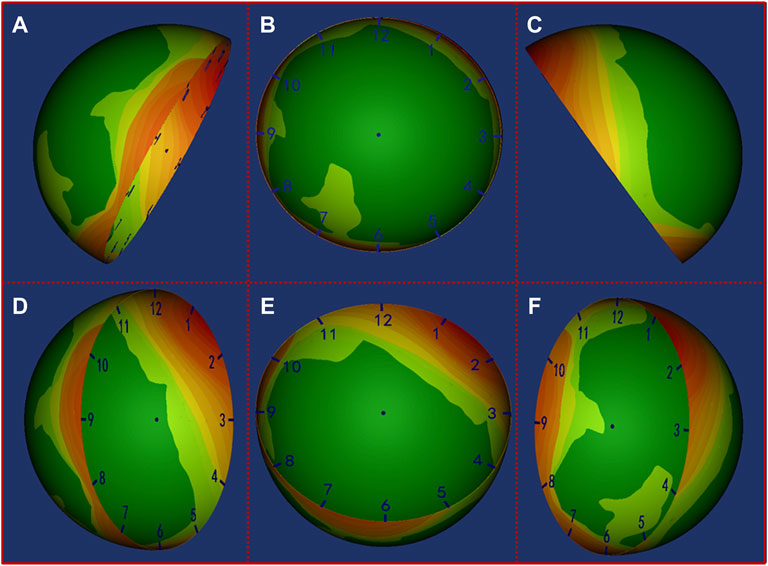
FIGURE 4. Distribution map of the uncovered area in AAOS I group. Green to red indicates that the uncovered frequency ranges from low to high. (A) Front view of the pelvis, (B) opening orientation view of the cup, (C) Back view of the pelvis, (D) Lateral view of the cup from front to back, (E) Lateral view of the cup from bottom to top, (F) Lateral view of the cup from back to front.
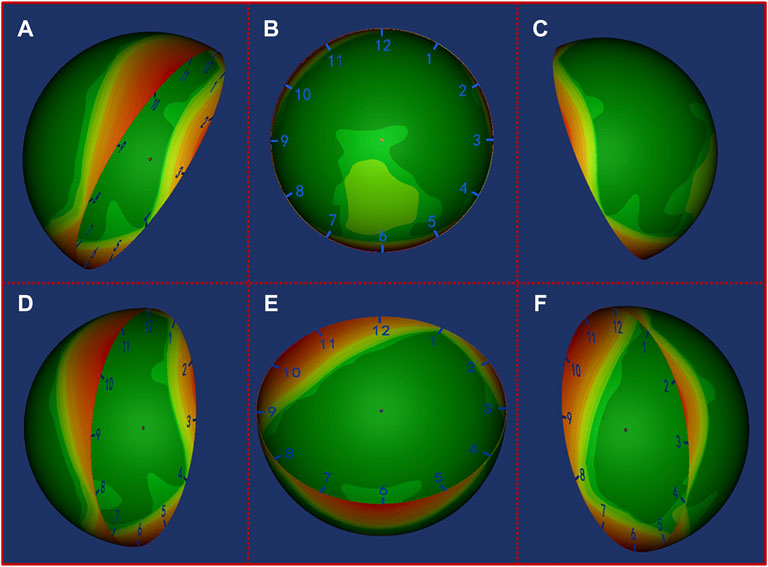
FIGURE 5. Distribution map of the uncovered area in AAOS II group. Green to red indicates that the uncovered frequency ranges from low to high. (A) Front view of the pelvis, (B) opening orientation view of the cup, (C) Back view of the pelvis, (D) Lateral view of the cup from front to back, (E) Lateral view of the cup from bottom to top, (F) Lateral view of the cup from back to front.
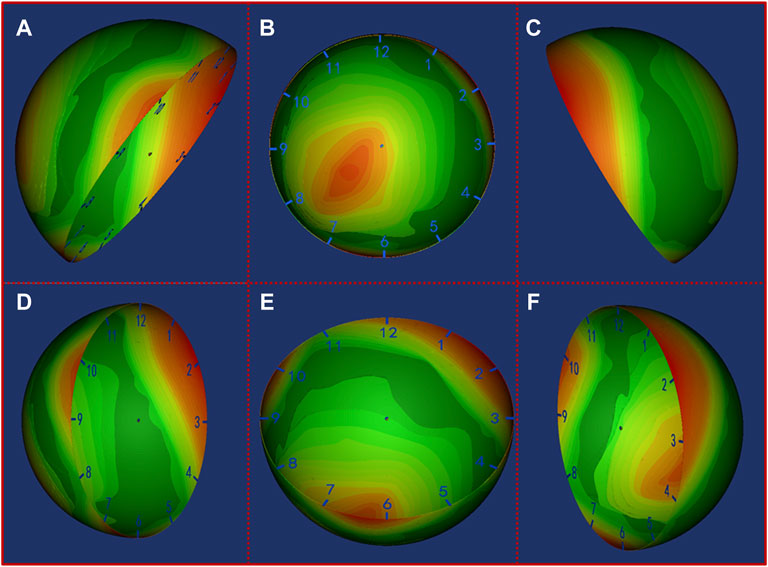
FIGURE 6. Distribution map of the uncovered area in AAOS III group. Green to red indicates that the uncovered frequency ranges from low to high. (A) Front view of the pelvis, (B) opening orientation view of the cup, (C) Back view of the pelvis, (D) Lateral view of the cup from front to back, (E) Lateral view of the cup from bottom to top, (F) Lateral view of the cup from back to front.
As shown in Table 4, ICC results for intra- and interobserver reliabilities were in the excellent range.
Some studies (Sariali et al., 2016; Yang et al., 2017; Liu et al., 2018) have proven that for complex anatomical deformities of the hip, such as developmental dysplasia of the hip (DDH) and acetabular bone defects, CT imaging data-based preoperative 3D planning can help with 1) comprehensively and accurately understanding the extent of the lesion and accordingly determining the implant location of the prosthesis, 2) pre-evaluation of the potential peri- and postoperative risks, and 3) improving the surgical effect. Acetabular revision arthroplasty for patients with moderate-to-extensive bone defects is often difficult for orthopedic surgeons, and using a jumbo acetabular cup is a relatively straightforward procedure for revision (von Roth et al., 2015). The use of jumbo cups in acetabular revisions can provide a larger circumference for ring fixation and a larger contact surface area to enhance bone ingrowth with the host bone. However, it would result in compromised CC and HCOR elevation. The present study revealed two principal findings. First, acetabular revision arthroplasty with jumbo cups for the treatment of AAOS I–III acetabular bone defects can lead to significant HCOR elevation, particularly for AAOS III, wherein the elevation is > 10 mm (11.25 ± 3.46 mm). Second, the contact area between the jumbo cup and the host bone can be accurately quantified by 3D simulation implantation technology. We found that the average CC obtained with the jumbo cup technology in patients with AAOS I–III acetabular bone defects was not less than 70%, which may provide good initial cup stability and prevent early loosening.
Ideally, the acetabular prosthesis should be placed in the living host bone as close as possible to the anatomical HCOR. However, this may be difficult or even impossible in patients with severe acetabular bone defects. In this study, we found that acetabular revision arthroplasty with the jumbo cup technology upshifted the HCOR and provided better initial contact between the jumbo cup and the host bone. This is in line with the application effect of high hip center technology in the treatment of complex anatomical deformities of the hip (Liu et al., 2018; Montalti et al., 2018).
Several previous studies have reported that acetabular revision with the jumbo cup technology can elevate the HCOR (Nwankwo and Ries, 2014; Zhou et al., 2018; Zhang et al., 2019). For instance, Nwankwo and Ries (2014) retrospectively analyzed the X-ray radiographic images of 98 patients having undergone cementless jumbo cup acetabular revisions and found that acetabular revision arthroplasty with jumbo cups upshifted HCOR by approximately 11 mm. Nevertheless, our results reported that the average HCOR elevation in patients with acetabular bone defects who underwent acetabular revision arthroplasty was 7.24 mm, indicating a lesser elevation than that reported by Nwankwo et al. This difference could be attributed to them not having taken into account the severity of the acetabular bone defect. To our surprise, after stratifying the acetabular bone defect using the AAOS classification, we found that only AAOS III patients showed an HCOR upshift of approximately 11.25 mm, which is in agreement with Nwankwo et al.’s findings. In a retrospective study, Zhang et al. (2019) included 61 patients who underwent acetabular revision using jumbo cups and measured the height of HCOR in 42 patients with a normal contralateral hip. The mean HCOR elevation in the revision side was found to be approximately 8.2 mm higher than that on the normal side, which is in line with our findings.
Bringing the HCOR to a more anatomical position during revision surgery may improve the biomechanics of the hip (Patel et al., 2003; Galia et al., 2017). Acetabular revision with the jumbo cup is evidently not conducive to HCOR anatomical reconstruction and is regarded as a surgical procedure that affects hip biomechanics, which has caused surgeons’ concerns. Johnston et al. (1979) were the first to design a mathematical model of the hip to evaluate the mechanical changes, and they showed that the hip load was the greatest when the HCOR was placed laterally, superiorly, and posteriorly. However, they did not focus on the results of simple upshift of HCOR. Based on a 3D computer model, Delp et al. (1996) found that superolateral placement of the HCOR resulted in an average reduction 28% in the abductor muscle moment arm. This could lead to muscle imbalance and prosthetic joint dislocations (Renkawitz et al., 2016; Hu et al., 2021). Further, Bicanic et al. (2009) quantified the relationship between the displacement of HCOR and the joint response force in the experiment and found that upshifting the HCOR by 1 mm will increase the joint response force by 0.1%. This also reminds us that upshifting the HCOR will increase the load pressure, thus increasing the wear of the prosthesis due to increased friction at the interface. In addition, the HCOR elevation will lead to differences in the leg length and postoperative kinematics (Karaismailoglu et al., 2019; Hu et al., 2022). In a retrospective study, Dou et al. (2013) found that acetabular revision increased HCOR elevation, thus resulting in leg length differences. Hu et al. (2022) found that laterally or superiorly placed HCOR would increase abnormal extension and internal rotation, resulting in impaired gait patterns. These aspects need attention, especially for largely HCOR elevation in acetabular revision.
However, the current study confirmed that the use of the jumbo cup still leads to a HCOR upshift, particularly in AAOS III patients, which reminds surgeons that the use of the jumbo cup technology in more severe acetabular bone defects requires in-depth consideration as it may change hip biomechanics, increase the risk of component loosening, and increase the need of re-revision surgery (Delp et al., 1996; Peng et al., 2021). Of course, these negative effects can be averted through technological advancements in the development of prostheses, such as improving the friction interface (Hu et al., 2015) and increasing the length of the femoral head (Woelfle et al., 2014). It is encouraging that some authors have reported good clinical results using jumbo cups with improved manufacturing processes (Fan et al., 2008; Warschawski et al., 2021).
Increasing the contact area between the acetabular cup and the host bone can ensure good initial stability, which is a crucial success factor of hip arthroplasty revision. CC is usually used to evaluate this contact area and in DDH hip replacement (Yang et al., 2017; Liu et al., 2018; Mou et al., 2020; Takasago et al., 2021). Generally, insufficient CC will increase the stress at the bone cup interface, thus increasing the probability of mechanical failure (Apostu et al., 2018; Zuo et al., 2021). Several clinical studies have shown that a CC value of ≥70% is acceptable and can ensure initial stability and prevent earlier loosening (Xu et al., 2012; Li et al., 2013). In the CT analysis study, Liu et al. (2018) found that the high hip center technology can effectively increase CC in DDH Crowe Type III patients. The HCOR is moved up by 25 mm and can provide a CC value of nearly 85%. To our knowledge, no study has quantitatively evaluated acetabular CC in hip revision surgery using a jumbo cup. We found in our 3D simulation study that with bone defect aggravation, the CC of the acetabulum gradually decreased; however, HCOR elevation remained significantly higher in AAOS III patients than in AAOS I and AAOS II patients with acetabular bone defects. It is reassuring that CC reached >70% even in AAOS III patients. This also explains the great prospects brought about by the use of the jumbo cup technology in increasing bone contact of the host bone with bone trabecular metal, thus potentially improving the ingrowth and ongrowth ability of host bone (Shen et al., 2022).
This study has some limitations. First, relatively few patients were included, resulting in a fewer subitems distribution of AAOS I and AAOS II (segmental defect and cavity defect), prevented further detailed subitems analysis in acetabular revision using jumbo cups. But the results still showed significant differences in the overall classification. Second, AAOS IV patients with pelvic discontinuity were not included, mainly due to the short study time span and the rarity of AAOS IV patients. For pelvic discontinuity, however, the clinical treatment principle is to use the acetabular cup to obtain initial stabilization with bone press-fit contact between the anterosuperior and posteroinferior acetabulum to reconstruct the discontinuity of the acetabulum. It is inappropriate to use the CC evaluation, which is different from AAOS I–III acetabular defect. Therefore, this will not affect our conclusion. Third, this study is only a performed 3D simulation study with a singular focus on imaging parameters, which may not fully represent the surgical situation. Nevertheless, these imaging indicators are of great significance, which is conducive to making preoperative plans and avoiding revision failure-related complications in complex situations. In addition, the selected acetabular cup size is determined by the remaining bone stock. In some cases, the anteversion may be compromised to obtain better CC even if the average anteversion angle of the implanted acetabular cup was normal.
In summary, although the use of jumbo cups for acetabular revision arthroplasty in patients with AAOS I–III offers reduced initial CC with increasing severity of the acetabular bone defect, the CC consistently remained >70%. In addition, it is associated with significant elevation of >10 mm of the HCOR in AAOS III patients. This information may remind the surgeons additional procedures are needed to compensate for the elevation of the hip center using jumbo cups.
The raw data supporting the conclusion of this article will be made available by the authors, further inquiries should be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Institutional ethical board review was obtained for the present study (No: 2016-nsfc020). The patients/participants provided their written informed consent to participate in this study.
XS: Conceptualization, Data analysis, Methodology, Writing-original draft and review. HT: Methodology, Data analysis, Investigation. YL: Methodology, Data analysis, Investgation. JZ: Project administration, Supervision, Writing- review and editing. ZG: Project administration, Supervision, Writing- review and editing. JX: Conceptualization, Funding acquisition, Methodology, Supervision, Writing- review and editing.
This work was supported by funding from the National Nature Science Foundation of Youth in China (No.81601907), China Postdoctoral Science Foundation (No. 2020M670863), Natural Science Foundation of Jilin Province (No.20200201345JC), Department of Finance of Jilin Province (No.2020SCZ63).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Aggarwal, V. K., Elbuluk, A., Dundon, J., Herrero, C., Hernandez, C., Vigdorchik, J. M., et al. (2019). Surgical Approach Significantly Affects the Complication Rates Associated with Total Hip Arthroplasty. Bone Jt. J. 101-B (6), 646–651. doi:10.1302/0301-620X.101B6.BJJ-2018-1474.R1
Apostu, D., Lucaciu, O., Berce, C., Lucaciu, D., and Cosma, D. (2018). Current Methods of Preventing Aseptic Loosening and Improving Osseointegration of Titanium Implants in Cementless Total Hip Arthroplasty: A Review. J. Int. Med. Res. 46 (6), 2104–2119. doi:10.1177/0300060517732697
Bicanic, G., Delimar, D., Delimar, M., and Pecina, M. (2009). Influence of the Acetabular Cup Position on Hip Load during Arthroplasty in Hip Dysplasia. Int. Orthopaedics (SICOT) 33 (2), 397–402. doi:10.1007/s00264-008-0683-z
Bozic, K. J., Kurtz, S. M., Lau, E., Ong, K., Vail, T. P., and Berry, D. J. (2009). The Epidemiology of Revision Total Hip Arthroplasty in the United States. J. Bone Joint Surg. Am. 91 (1), 128–133. doi:10.2106/JBJS.H.00155
D'Antonio, J. A., Capello, W. N., Borden, L. S., Bargar, W. L., Bierbaum, B. F., Boettcher, W. G., et al. (1989). Classification and Management of Acetabular Abnormalities in Total Hip Arthroplasty. Clin. Orthopaedics Relat. Res. 243, 126–137. doi:10.1097/00003086-198906000-00019
Dearborn, J. T., and Harris, W. H. (2000). Acetabular Revision Arthroplasty Using So-Called Jumbo Cementless Components: an Average 7-year Follow-Up Study. J. Arthroplasty 15 (1), 8–15. doi:10.1016/s0883-5403(00)90999-9
Delp, S. L., Wixson, R. L., Komattu, A. V., and Kocmond, J. H. (1996). How superior Placement of the Joint center in Hip Arthroplasty Affects the Abductor Muscles. Clin. Orthopaedics Relat. Res. 328, 137–146. doi:10.1097/00003086-199607000-00022
Dou, Y., Zhou, Y., Tang, Q., Yang, D., and Liu, J. (2013). Leg-Length Discrepancy after Revision Hip Arthroplasty: Are Modular Stems Superior? The J. Arthroplasty 28 (4), 676–679. doi:10.1016/j.arth.2012.08.009
Fan, C.-Y., Chen, W.-M., Lee, O. K., Huang, C.-K., Chiang, C.-C., and Chen, T.-H. (2008). Acetabular Revision Arthroplasty Using Jumbo Cups: An Experience in Asia. Arch. Orthop. Trauma Surg. 128 (8), 809–813. doi:10.1007/s00402-007-0492-7
Fujii, M., Nakashima, Y., Sato, T., Akiyama, M., and Iwamoto, Y. (2012). Acetabular Tilt Correlates with Acetabular Version and Coverage in Hip Dysplasia. Clin. Orthop. Relat. Res. 470 (10), 2827–2835. doi:10.1007/s11999-012-2370-z
Galia, C. R., Diesel, C. V., Guimarães, M. R., and Ribeiro, T. A. (2017). Total Hip Arthroplasty: A Still Evolving Technique. Rev. Bras Ortop 52 (5), 521–527. doi:10.1016/j.rboe.2016.09.011
Green, C. M., Buckley, S. C., Hamer, A. J., Kerry, R. M., and Harrison, T. P. (2018). Long-Term Results of Acetabular Reconstruction Using Irradiated Allograft Bone. Bone Jt. J 100-B (11), 1449–1454. doi:10.1302/0301-620X.100B11.BJJ-2018-0478.R2
Hoskins, W., Bingham, R., Dyer, C., Rainbird, S., and Graves, S. E. (2021). A Comparison of Revision Rates for Dislocation and Aseptic Causes between Dual Mobility and Large Femoral Head Bearings in Primary Total Hip Arthroplasty with Subanalysis by Acetabular Component Size: An Analysis of 106,163 Primary Total Hip Arthroplasties. J. Arthroplasty 36 (9), 3233–3240. doi:10.1016/j.arth.2021.05.008
Hoskins, W., Bingham, R., Lorimer, M., Hatton, A., and de Steiger, R. N. (2020). Early Rate of Revision of Total Hip Arthroplasty Related to Surgical Approach: An Analysis of 122,345 Primary Total Hip Arthroplasties. J. Bone Jt. Surg Am 102 (21), 1874–1882. doi:10.2106/JBJS.19.01289
Hu, D., Tie, K., Yang, X., Tan, Y., Alaidaros, M., and Chen, L. (2015). Comparison of Ceramic-On-Ceramic to Metal-On-Polyethylene Bearing Surfaces in Total Hip Arthroplasty: A Meta-Analysis of Randomized Controlled Trials. J. Orthop. Surg. Res. 10, 22. doi:10.1186/s13018-015-0163-2
Hu, X., Zheng, N., Chen, Y., Dai, K., Dimitriou, D., Li, H., et al. (2021). Optimizing the Femoral Offset for Restoring Physiological Hip Muscle Function in Patients with Total Hip Arthroplasty. Front. Bioeng. Biotechnol. 9, 645019. doi:10.3389/fbioe.2021.645019
Hu, Y., Zou, D., Sun, Q., Jiang, M., Li, H., Tsai, T.-Y., et al. (2022). Postoperative Hip Center Position Associated with the Range of Internal Rotation and Extension during Gait in Hip Dysplasia Patients after Total Hip Arthroplasty. Front. Bioeng. Biotechnol. 10, 831647. doi:10.3389/fbioe.2022.831647
Innocenti, M., Muratori, F., Mazzei, G., Guido, D., Frenos, F., Lucenteforte, E., et al. (2021). The Use of a Non-Biological, Bridging, Antiprotrusio Cage in Complex Revision Hip Arthroplasty and Periacetabular Reconstructive Oncologic Surgery. Is Still Today a Valid Option?: A Mid/long-Term Survival and Complications' Analysis. Arch. Orthop. Trauma Surg. 142, 681–690. doi:10.1007/s00402-021-03929-6
Johnston, R. C., Brand, R. A., and Crowninshield, R. D. (1979). Reconstruction of the Hip. A Mathematical Approach to Determine Optimum Geometric Relationships. J. Bone Jt. Surg. 61 (5), 639–652. doi:10.2106/00004623-197961050-00001
Karaismailoglu, B., Erdogan, F., and Kaynak, G. (2019). High Hip Center Reduces the Dynamic Hip Range of Motion and Increases the Hip Load: A Gait Analysis Study in Hip Arthroplasty Patients with Unilateral Developmental Dysplasia. J. Arthroplasty 34 (6), 1267–1272. doi:10.1016/j.arth.2019.02.017
Lachiewicz, P. F., and Watters, T. S. (2016). The Jumbo Acetabular Component for Acetabular Revision: Curtain Calls and Caveats. Bone Jt. J 98-B (1 Suppl. A), 64–67. doi:10.1302/0301-620X.98B1.36139
Li, H., Wang, L., Dai, K., and Zhu, Z. (2013). Autogenous Impaction Grafting in Total Hip Arthroplasty with Developmental Dysplasia of the Hip. J. Arthroplasty 28 (4), 637–643. doi:10.1016/j.arth.2012.07.007
Liu, B., Gao, Y.-H., Ding, L., Li, S.-Q., Liu, J.-G., and Qi, X. (2018). Computed Tomographic Evaluation of Bone Stock in Patients with Crowe Type III Developmental Dysplasia of the Hip: Implications for Guiding Acetabular Component Placement Using the High Hip Center Technique. J. Arthroplasty 33 (3), 915–918. doi:10.1016/j.arth.2017.10.021
Löchel, J., Janz, V., Hipfl, C., Perka, C., and Wassilew, G. I. (2019). Reconstruction of Acetabular Defects with Porous Tantalum Shells and Augments in Revision Total Hip Arthroplasty at Ten-Year Follow-Up. Bone Jt. J. 101-B (3), 311–316. doi:10.1302/0301-620X.101B3.BJJ-2018-0959.R1
McLaughlin, J. R., and Lee, K. R. (2018). Acetabular Revision Arthroplasty Using an Uncemented Deep Profile Jumbo Component: A Ten to Sixteen Year Follow-Up Study. J. Arthroplasty 33 (2), 496–499. doi:10.1016/j.arth.2017.09.002
Montalti, M., Castagnini, F., Giardina, F., Tassinari, E., Biondi, F., and Toni, A. (2018). Cementless Total Hip Arthroplasty in Crowe III and IV Dysplasia: High Hip Center and Modular Necks. J. Arthroplasty 33 (6), 1813–1819. doi:10.1016/j.arth.2018.01.041
Moon, J.-K., Ryu, J., Kim, Y., Yang, J.-H., Hwang, K.-T., and Kim, Y.-H. (2019). Acetabular Revision Arthroplasty Using Press-Fitted Jumbo Cups: An Average 10-Year Follow-Up Study. Arch. Orthop. Trauma Surg. 139 (8), 1149–1160. doi:10.1007/s00402-019-03214-7
Mose, K. (1980). Methods of Measuring in Legg-Calve-Perthes Disease with Special Regard to the Prognosis. Clin. Orthop. Relat. Res. 150, 103–109. doi:10.1097/00003086-198007000-00019
Mou, P., Liao, K., Chen, H.-l., and Yang, J. (2020). Controlled Fracture of the Medial wall versus Structural Autograft with Bulk Femoral Head to Increase Cup Coverage by Host Bone for Total Hip Arthroplasty in Osteoarthritis Secondary to Developmental Dysplasia of the Hip: A Retrospective Cohort Study. J. Orthop. Surg. Res. 15 (1), 561. doi:10.1186/s13018-020-02088-5
Nwankwo, C. D., and Ries, M. D. (2014). Do Jumbo Cups Cause Hip Center Elevation in Revision THA? A Radiographic Evaluation. Clin. Orthop. Relat. Res. 472 (9), 2793–2798. doi:10.1007/s11999-014-3632-8
Paprosky, W. G., Perona, P. G., and Lawrence, J. M. (1994). Acetabular Defect Classification and Surgical Reconstruction in Revision Arthroplasty. A 6-Year Follow-Up Evaluation. J. Arthroplasty 9 (1), 33–44. doi:10.1016/0883-5403(94)90135-x
Patel, J. V., Masonis, J. L., Bourne, R. B., and Rorabeck, C. H. (2003). The Fate of Cementless Jumbo Cups in Revision Hip Arthroplasty. J. Arthroplasty 18 (2), 129–133. doi:10.1054/arth.2003.50038
Peng, Y.-W., Shen, J.-M., Zhang, Y.-C., Sun, J.-Y., Du, Y.-Q., and Zhou, Y.-G. (2021). Jumbo Cup in Hip Joint Renovation May Cause the Center of Rotation to Increase. World J. Clin. Cases 9 (22), 6300–6307. doi:10.12998/wjcc.v9.i22.6300
Renkawitz, T., Weber, T., Dullien, S., Woerner, M., Dendorfer, S., Grifka, J., et al. (2016). Leg Length and Offset Differences above 5mm after Total Hip Arthroplasty are Associated with Altered Gait Kinematics. Gait Posture 49, 196–201. doi:10.1016/j.gaitpost.2016.07.011
Russell, S. P., O'Neill, C. J., Fahey, E. J., Guerin, S., Gul, R., and Harty, J. A. (2021). Trabecular Metal Augments for Severe Acetabular Defects in Revision Hip Arthroplasty: A Long-Term Follow-Up. J. Arthroplasty 36 (5), 1740–1745. doi:10.1016/j.arth.2020.12.033
Sariali, E., Boukhelifa, N., Catonne, Y., and Pascal Moussellard, H. (2016). Comparison of Three-Dimensional Planning-Assisted and Conventional Acetabular Cup Positioning in Total Hip Arthroplasty: A Randomized Controlled Trial. J. Bone Jt. Surg Am 98 (2), 108–116. doi:10.2106/JBJS.N.00753
Shen, X., Qin, Y., Li, Y., Tang, X., and Xiao, J. (2022). Trabecular Metal Versus Non-Trabecular Metal Acetabular Components For Acetabular Revision Surgery: A Systematic Review And Meta-Analysis. Int. J. Surg. 100, 106597. doi:10.1016/j.ijsu.2022.106597
Solomon, L. B., Abrahams, J. M., Callary, S. A., and Howie, D. W. (2018). The Stability of the Porous Tantalum Components Used in Revision THA to Treat Severe Acetabular Defects: A Radiostereometric Analysis Study. J. Bone Jt. Surg Am 100 (22), 1926–1933. doi:10.2106/JBJS.18.00127
Takasago, T., Goto, T., Wada, K., Hamada, D., and Sairyo, K. (2021). Postoperative Radiographic Evaluation and Simulation Study for Optimal Cup Placement in High-Hip centre Total Hip Arthroplasty. HIP Int. 31 (3), 335–341. doi:10.1177/1120700019884547
von Roth, P., Abdel, M. P., Harmsen, W. S., and Berry, D. J. (2015). Uncemented Jumbo Cups for Revision Total Hip Arthroplasty: A Concise Follow-Up, at a Mean of Twenty Years, of a Previous Report. J. Bone Jt. Surg Am 97 (4), 284–287. doi:10.2106/JBJS.N.00798
Wang, C. X., Huang, Z. D., Wu, B. J., Li, W. B., Fang, X. Y., and Zhang, W. M. (2020). Cup-Cage Solution for Massive Acetabular Defects: A Systematic Review and Meta-Analysis. Orthop. Surg. 12 (3), 701–707. doi:10.1111/os.12710
Warschawski, Y., Garceau, S. P., Joly, D. A., Kuzyk, P., Gross, A., and Safir, O. (2021). The Effect of Femoral Head Size, Neck Length, and Offset on Dislocation Rates of Constrained Acetabular Liners. J. Arthroplasty 36 (1), 345–348. doi:10.1016/j.arth.2020.07.067
Woelfle, J. V., Fraitzl, C. R., Reichel, H., and Wernerus, D. (2014). Significantly Reduced Leg Length Discrepancy and Increased Femoral Offset by Application of a Head-Neck Adapter in Revision Total Hip Arthroplasty. J. Arthroplasty 29 (6), 1301–1307. doi:10.1016/j.arth.2013.11.028
Xu, Y. S., Wang, Y., Lu, L., and Wei, B. G. (2012). Application of Uncemented Zweymüller Hip Prosthesis in Adult Patients with Hip Osteoarthritis Secondary to Developmental Dysplasia. Chin. Med. J. (Engl) 125 (10), 1799–1803. doi:10.3760/cma.j.issn.0366-6999.2012.10.021
Yang, Y., Zuo, J., Liu, T., Xiao, J., Liu, S., and Gao, Z. (2017). Morphological Analysis of True Acetabulum in Hip Dysplasia (Crowe Classes I-IV) via 3-D Implantation Simulation. J. Bone Jt. Surg. 99 (17), e92. doi:10.2106/JBJS.16.00729
Zhang, J., Huang, Y., Zhou, B., and Zhou, Y. (2019). Mid‐Term Follow‐Up of Acetabular Revision Arthroplasty Using Jumbo Cups. Orthop. Surg. 11 (5), 811–818. doi:10.1111/os.12522
Zhou, B., Zhou, Y., Yang, D., Tang, H., Shao, H., and Huang, Y. (2018). The Utilization of Metal Augments Allows Better Biomechanical Reconstruction of the Hip in Revision Total Hip Arthroplasty with Severe Acetabular Defects: A Comparative Study. J. Arthroplasty 33 (12), 3724–3733. doi:10.1016/j.arth.2018.08.027
Keywords: three-dimensional, acetabular revision, bone defect, jumbo cup, cup coverage
Citation: Shen X, Tian H, Li Y, Zuo J, Gao Z and Xiao J (2022) Acetabular Revision Arthroplasty Based on 3-Dimensional Reconstruction Technology Using Jumbo Cups. Front. Bioeng. Biotechnol. 10:799443. doi: 10.3389/fbioe.2022.799443
Received: 23 October 2021; Accepted: 21 March 2022;
Published: 05 April 2022.
Edited by:
Alexandros E. Tsouknidas, University of Western Macedonia, GreeceReviewed by:
Björn Rath, Klinikum Wels-Grieskirchen, AustriaCopyright © 2022 Shen, Tian, Li, Zuo, Gao and Xiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianlin Xiao, eGlhb2ppYW5saW4xMEBqbHUuZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.