
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Bioeng. Biotechnol. , 10 January 2023
Sec. Biomaterials
Volume 10 - 2022 | https://doi.org/10.3389/fbioe.2022.1119720
This article is part of the Research Topic Clinic-oriented Multifunctional Biomaterials: From Rational Design to Applications View all 12 articles
 Xingbo Cai1,2
Xingbo Cai1,2 Bin Wang1,2
Bin Wang1,2 Bihuan Zhang1,2
Bihuan Zhang1,2 Yue Zhang1,2
Yue Zhang1,2 Teng Wang2
Teng Wang2 Wei Lin2
Wei Lin2 Youjun Huang3
Youjun Huang3 Bingquan Chen3
Bingquan Chen3 Siyuan Zhou3
Siyuan Zhou3 Sheng Lu4*
Sheng Lu4* Yongqing Xu2*
Yongqing Xu2*Background: Total wrist arthroplasty is an effective treatment for end-stage wrist arthritis from all causes. However, wrist prostheses are still prone to complications such as prosthesis loosening and periprosthetic fractures after total wrist arthroplasty. This may be due to the wrist prosthesis imprecise matching with patient’s bone. In this study, we designed and developed a personalized three-dimensional printed microporous titanium artificial wrist prosthesis (3DMT-Wrist) for the treatment of end-stage wrist joint, and investigated its safety and effectiveness.
Methods: Total wrist arthroplasty was performed using 3DMT-Wrist in 14 cases of arthritis between February 2019 and December 2021. Preoperative and postoperative visual analog scale scores, QuickDASH scores, wrist range of motion, and wrist grip strength were evaluated. Data were statistically analyzed using the paired samples t-test.
Results: After 19.7 ± 10.7 months of follow-up, visual analog scale decreased from 66.3 ± 8.9 to 6.7 ± 4.4, QuickDASH scores decreased from 47.4 ± 7.3 to 28.2 ± 7.6, grip strength increased from 5.6 ± 1.4 to 17.0 ± 3.3 kg. The range of motion improved significantly in palmar flexion (30.1° ± 4.9° to 44.9° ± 6.5°), dorsal extension (15.7° ± 3.9° to 25.8° ± 3.3°), ulnar deviation (12.2° ± 3.9° to 20.2° ± 4.3°) and radial deviation (8.2° ± 2.3° to 16.2 ± 3.1). No dislocation or loosening of the prosthetic wrist joint was observed.
Conclusion: Total wrist arthroplasty using 3DMT-Wrist is a safe and effective new treatment for various types of end-stage wrist arthritis; it offers excellent pain relief and maintains the range of motion.
Total wrist arthroplasty (TWA) has been performed for more than 40 years, and has offered good results in terms of pain relief and improvement of range of motion (ROM) and wrist function; however, the carpal component tends to loosen and subside on long-term follow-up. The first-generation Swanson silastic wrist prosthesis was developed in 1967, and offers the longest available follow-up data for over 15 years; however, silicone is prone to fracture and this procedure has a revision rate of 15%–41% (Damert, 2019). In the 1970s, the second generation of wrist prosthesis was developed by Meuli (Sulzer, acquired by Zimmer) and Volz (Howmedica, acquired by Stryker). These titanium prostheses had a bifurcated design and required bone cement for fixation. Unfortunately, it was demonstrated a high failure rate (Srnec et al., 2018). The third generation of artificial wrist prostheses were developed in 2000; these were mainly biaxial artificial wrist joints, biaxial total wrist implants (DePuy), and universal total wrist implants (KMI). These implants had a prosthetic coating, polyethylene components, and involved screw fixation; however, the main components still required bone cement fixation (Berber et al., 2018; Elbuluk et al., 2018; Reigstad and Røkkum, 2018; Srnec et al., 2018). The fourth generation prosthetic wrist joints emerged in 2003. These included the ReMotion (Stryker) and Maestro (Zimmer Biomet) systems, and involved biologic fixation without the need of cement (Herzberg et al., 2012; Bidwai et al., 2013; Boeckstyns et al., 2013; Sagerfors et al., 2015). This represented a significant improvement over previous generation. In this context, studies have reported better results with the fourth generation of artificial wrist joints (Bidwai et al., 2013; Froschauer et al., 2021). In contrast to wrist fusion, TWA preserves wrist mobility and provides effective pain relief (Fischer et al., 2020; Berber et al., 2020; Matsui et al., 2020; Zhu et al., 2021). However, the carpal component still tends to loosen on long-term follow-up (Reigstad et al., 2017).
Additive manufacturing, often known as three-dimensional (3D) printing or prototyping, can convert 3D digital models into functioning components regardless of their geometry (Raheem et al., 2021). Selective laser melting metal 3D printing technology is able to construct complex free-form surfaces, print parts with proper toughness and elastic modulus, and even surface coating layer (Yang et al., 2021). Owing to these properties, 3D printing technology has been employed in the field of hand surgery research for artificial lunar bone replacement and good results have been obtained in the treatment of advanced Kienböck’s disease (Ma et al., 2020). Trabecular bone grows within the grid of these implants and permeates throughout the porous structure. In addition, the body identifies human bones and microporous titanium as one structure, leading to good osteogenesis (Núñez et al., 2013). In the field of TWA research, customized artificial wrist prostheses have not been made using 3D-printed personalized microporous titanium. This study therefore aimed to investigate the safety and feasibility of developing a personalized 3D-printed microporous titanium artificial wrist prosthesis (3DMT-Wrist) system for the treatment of end-stage wrist arthritis.
Patients fulfilling the following criteria were included in this study: 1) diagnosed with rheumatoid arthritis, osteoarthritis, or deformity of the wrist with significant pain and limitation of movement (or combined with ulnar displacement instability of the radial wrist joint); 2) requiring total wrist fusion (including fusion of the radial wrist and midcarpal joints) with low requirements for life quality; 3) having severe ischemic necrosis of the wrist bones with an advanced stage of joint collapse; and 4) having good general condition, with good function of the heart, liver, kidney, brain, and other organs.
The following patients were excluded: 1) those with poor general condition and serious complications, 2) having tuberculosis or septic infection of the wrist joint, and 3) those demonstrating poor compliance or the inability to perform relevant postoperative functional rehabilitation exercises.
This study included 14 patients who underwent TWA using the individualized 3DMT-Wrist system at our hospital between February 2019 and December 2021 (Table 1). They were seven men and seven women in the study; they had an average age of 45.2 ± 13.5 (23–70) years. Overall, 3, 1, and 10 cases had rheumatoid arthritis, an open segmental defect caused by gunshot injury, and osteoarthritis, respectively. Patients were evaluated both preoperatively and postoperatively, based on findings on wrist radiography and computed tomography, pain levels, and wrist function. The level of wrist pain was evaluated based on the visual analog scale (VAS) scores and wrist function, which was evaluated based on the QuickDASH score, wrist grip strength, and wrist ROM (palmar flexion, dorsal extension, ulnar and radial deviation, pronation, and supination). Grip strength measurements were performed by a resident surgeon using the JAMAR hydraulic hand dynamometer (Sammons Preston, United States); the ROM was recorded using a goniometer. Radiographs were obtained at 1, 3, 6, and 12 months postoperatively. At least 2 mm of movement around the prosthesis-bone interface on serial radiographs were considered to be indicative of implant loosening; two surgeons performed the examination consistently.
The 3DMT-Wrist was developed by our research team in collaboration with MicroPort OrthoRecon Co. As shown in Figure 1A, the microporous titanium artificial wrist joint consisted of three parts: carpal and radial components and a polyethylene joint ball. The 3DMT-Wrist body material is Ti6Al4V and was manufactured by a metal 3D printer (SLMS310, Xi’an Plastica Additive Technology Co., China). The joint ball material is highly cross-linked ultra-high molecular weight polyethylene, which is manufactured by mechanical processing. The carpal component included a carpal platform, a central carpal column, screws on the left and right sides, a cylindrical projection on the carpal platform, and a carpal stem of Ti6Al4V with a diameter of 5 mm (which was fixed by inserting into the waist of the capitate); it had a 1-mm-thick porous surface to facilitate bone growth. Screws with a diameter of 4.0 mm could be placed in the screw holes on both sides of the carpal stem; in order to achieve fixation of the carpal component, radial and ulnar screws were aimed at the second and fourth metacarpal, respectively.
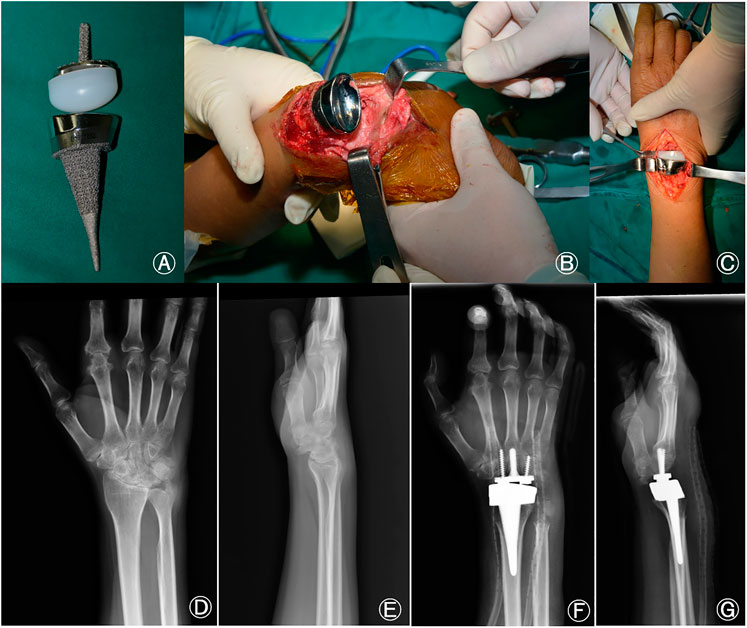
FIGURE 1. (A) Microporous titanium total wrist joint prosthesis, (B) Intraoperative carpal and radial osteotomy have been completed and the radial component is being installed. (C) Polyethylene has been inserted into the carpal component and the artificial wrist joint has been reset, (D) Preoperative posteroanterior radiographs of the wrist, (E) Preoperative lateral radiographs of the wrist, (F) Posteroanterior radiographs of the wrist at 1 month after TWA, (G) Lateral radiographs at 1 month after TWA. TWA, total wrist arthroplasty.
The polyethylene joint ball had a semi-ellipsoidal shape and was 40 mm long and 18 mm wide. It was prepared in three different sizes based on the height; the sizes were as follows: 12.5 mm (size I), 17.5 mm (size II), and 22.5 mm (size III). The polyethylene joint ball formed an elliptical joint with the radial component to maximize restoration of the wrist joint motion pattern.
The radial component consisted of a radial shank and an articular socket composed of Ti6Al4V and a CoCrMo alloys, respectively. The length of the radial shank was 65 mm and the proximal diameter was either 5 mm (size S#) or 7 mm (size L#); the ulnar deviation angle was approximately 15°. The surface of the radial stalk was porous and had a thickness of 1 mm to facilitate bone growth; the articular fossa was polished to reduce friction between the articular surfaces.
For clinical application, bilateral wrist joints, distal forearms, and metacarpals were first scanned by computed tomography; anatomical data relating to the wrist joints were obtained by mirroring the flip image. These data were provided to the company (which qualified based on biomechanical testing results) and the hospitals for use (Figure 2).
The affected limb was exsanguinated using a tourniquet after general or brachial plexus anesthesia; the tourniquet pressure was then maintained during surgery. An 8-cm incision was placed from the root of the third metacarpal to the distal radius via the Lister’s tuberosity; the skin and subcutaneous tissue were incised. The dorsal carpal capsule was lifted from the distal radius to the base of the metacarpal and the ulnar head was removed using biting forceps. The wrist was palmar flexed and the osteotomy line was marked on the distal radius using an electric knife; the median nerve was then protected using a periosteal stripper. The distal radius was osteotomized with a pendulum saw and reamed based on the individual medullary contour; as shown in Figure 1B, this was followed by insertion of the radial component. The thickness of the artificial carpal joint polyethylene and carpal component was measured to determine the thickness of the carpal bone to be osteotomized; after marking, the required segment was removed using a pendulum saw. The medullary cavity of the third metacarpal was then drilled from the center of the capitate section using an electric drill and the position was confirmed via radiographic fluoroscopy. The carpal stem was then driven in after reaming and fixed using screws on both sides. The radial stem was inserted, followed by insertion of polyethylene into the carpal component; as shown in Figure 1C, the artificial wrist joint was reset and moved to observe the ROM and check for the likelihood of dislocation. The procedure was confirmed to be satisfactory after fluoroscopic inspection of the artificial wrist joint. The tourniquet was then released, hemostasis was ensured, and the wound was irrigated. The in-situ suture of the U-shaped tissue flap was handled with care during the procedure to prevent dorsal dislocation of the wrist joint. The operation was completed after suturing of the incision and application of vacuum sealing drainage over the incision site.
The cast was removed after 2 weeks and active and passive exercises were performed; the degree of dorsal extension was increased by 3–5° every 3 days to gradually increase the ROM. Cefazolin (1 g) was administered intravenously after surgery along with Aescuven Forte, which was administered orally. In this context, postoperative edema may occur easily after surgery to the wrist, as the soft tissue layer on the dorsal aspect is thin (with only tendons and no muscle coverage).
Radiographs were obtained at 1, 3, 6, and 12 months after surgery.
The SPSS version 19.0 statistical software package was used for data analysis. Measurement data, including the VAS and QuickDASH scores, grip strength, and wrist mobility, were evaluated based on the ROM. Preoperative and postoperative data were compared using the paired t-test; p < .05 was considered statistically significant. All data have been presented as means with standard deviation.
Our study had a before–after design, in which the patients’ VAS and QuickDASH scores were assessed based on questionnaires administered before and after surgery. Data pertaining to wrist ROM and grip strength were obtained by physical measurement. Allocation concealment was not performed; blinding of treatment allocation was not possible owing to the nature of the interventions. This study was approved by the local ethics committee before patient enrolment.
The mean age of the patients was 45.2 ± 13.5 (23–70) years, and the cohort had a male-to-female ratio of 1:1. Among the 14 patients, 10, 3, and 1 were diagnosed with osteoarthritis, rheumatoid arthritis, and traumatic arthritis, respectively. None experienced prosthesis loosening or dislocation or required revision surgery during the study period. One patient with a history of a gunshot wound in the wrist experienced occasional postoperative wrist and back pain due to severe trauma and surrounding soft tissue injury. All patients were followed up for 19.7 ± 10.7 (7–41) months (Figures 3, 4). At the final follow-up (Table 2), the VAS score decreased from 66.3 ± 8.9 to 6.7 ± 4.4 (t = 19.71, p < 0.05), and the QuickDASH score decreased from 47.4 ± 7.3 to 28.2 ± 7.6 (t = 16.18, p < 0.05). The grip strength increased from 5.6 ± 1.4 kg to 17.0 ± 3.3 kg (t = −22.0, p < 0.05) and the ROM improved significantly for palmar flexion, dorsal extension, and ulnar and radial deviation, with no significant differences for pronation or supination. The palmar flexion angle improved from 30.1° ± 4.9° to 44.9° ± 6.5° (t = −8.4, p < 0.05), the dorsal extension angle improved from 15.7° ± 3.9° to 25.8° ± 3.3° (t = −11.9, p < 0.05), the ulnar deviation angle increased from 12.2° ± 3.9° to 20.2° ± 4.3° (t = −4.9, p < 0.05), and the radial deviation angle increased from 8.2° ± 2.3° to 16.2° ± 3.1° (t = −14.2, p < 0.05). There was no statistical difference for pronation and supination (p > 0.05) (Table 3; Figure 5). Evaluation at the final follow-up showed no loosening or dislocation of the wrist in any patient. The preoperative and postoperative radiographs are shown in Figures 1D–G, 6.

FIGURE 3. Osteoarthritis of the left wrist joint in a female patient aged 46 years. (A,B): preoperative anteroposterior and lateral radiographs, (C,D): postoperative anteroposterior and lateral radiographs at 6 months, (E,F): postoperative anteroposterior and lateral radiographs at 12 months.
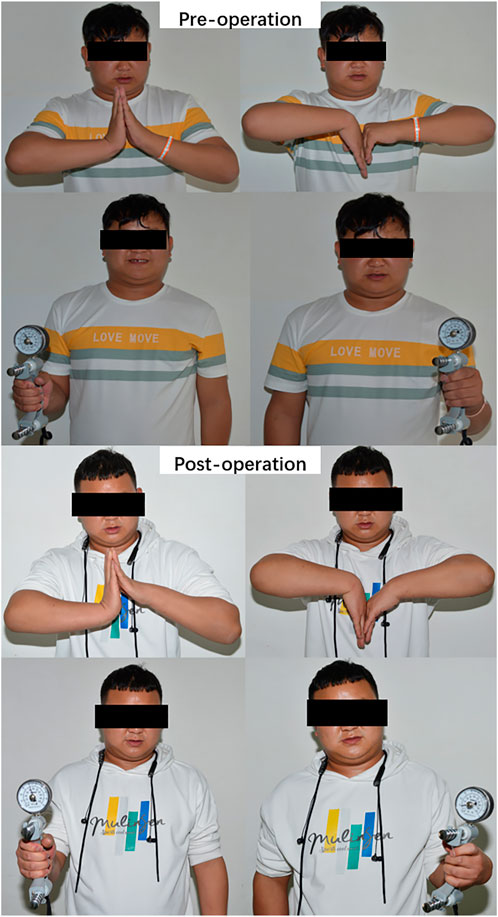
FIGURE 4. A patient with rheumatoid wrist arthritis with 24 months of follow-up after 3DMT-Wrist TWA.
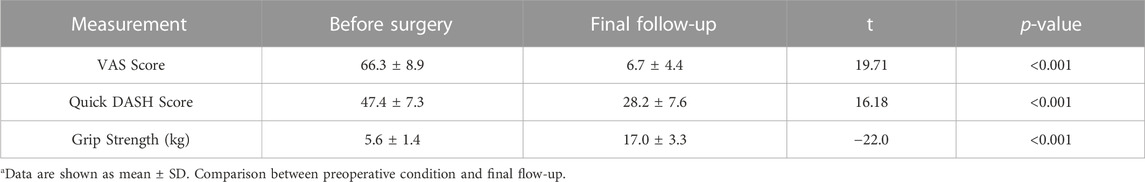
TABLE 2. Comparison of VAS score, quick dash score, grip strength before surgery and final follow-upa.
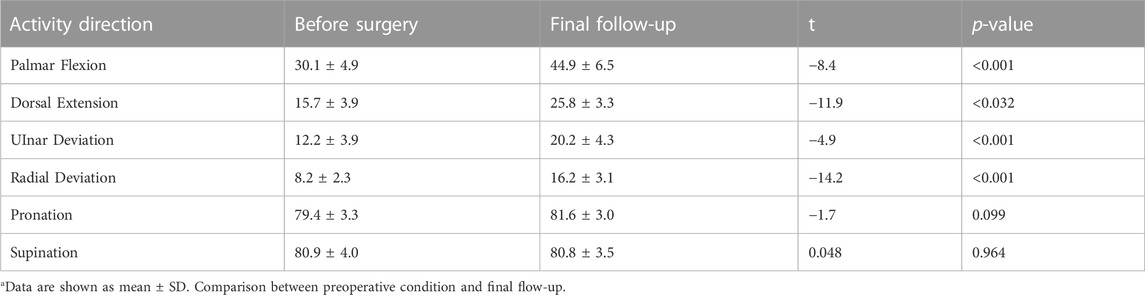
TABLE 3. Comparison of ROM before surgery and final follow-upa.
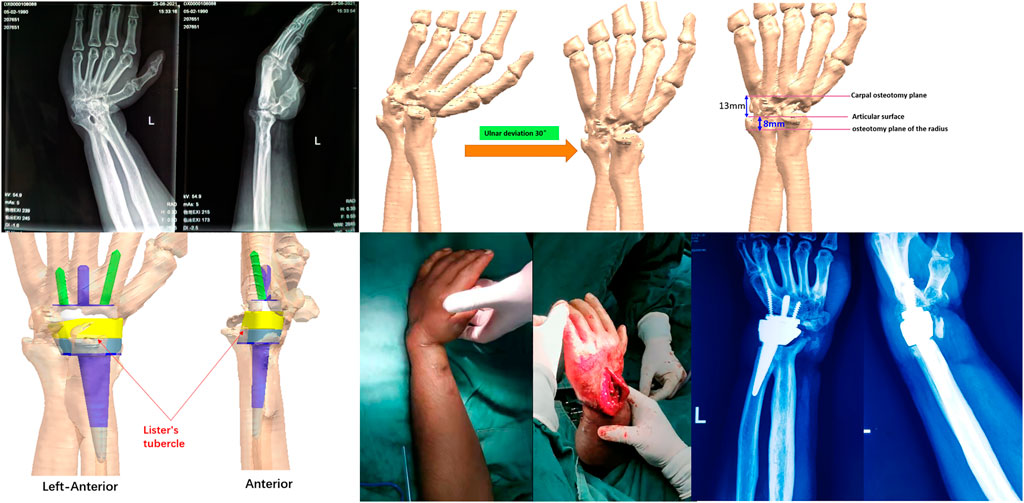
FIGURE 6. A complicated case with non-development of the carpal bones owing to a donkey bite at the age of 3 years. The patient demonstrated loss of wrist and forearm movement, but experienced pain relief and could move the wrist following personalized total wrist arthroplasty.
In this study, the 14 participants who had undergone TWA with the 3DMT-Wrist system showed a decrease in VAS scores from 66.3 ± 8.9 to 6.7 ± 4.4 at 1.6 years after surgery; the QuickDASH scores also decreased from 47.4 ± 7.3 to 28.2 ± 7.6. These findings suggest that TWA using the 3DMT-Wrist system offered significant pain relief and improved function and ROM of the wrist joint. Except for in one patient with a history of a gunshot wound to the wrist (who had occasional dorsal wrist pain after surgery due to severe trauma and surrounding soft tissue damage), wrist pain had disappeared in all cases. The grip strength increased from 5.6 ± 1.4 kg to 17.0 ± 3.3 kg, probably reflecting the reduction in wrist pain; loosening of the prosthesis or joint dislocation were not observed on the radiographs. It is worth noting that all patients who underwent TWA using the 3DMT-Wrist system demonstrated excellent pronation and supination ability; this was mostly because ulnar head excision was performed in all cases to remove inflammatory tissue from the distal radioulnar joint and ease wrist pain. In this context, the most recent follow-up did not reveal ulnar impingement.
Our study showed that the 3DMT-Wrist system can offer the following ROM: palmar flexion by 44.9° ± 6.5°, dorsal extension by 25.8° ± 3.3°, ulnar deviation by 20.2° ± 4.3°, radial deviation by 16.2° ± 3.1°, pronation by 81.6° ± 3.0°, and supination by 80.8° ± 3.5°. Brumfield et al. (Brumfield and Champoux, 1984) found that patients with a wrist joint ROM of 10° palmar flexion and 35° dorsal extension were capable of performing most daily activities. Palmer et al. (Palmer et al., 1985) measured functional wrist motion in 10 normal individuals using triaxial electrical goniometry. They assessed wrist motion by asking the participants to perform 52 standardized tasks; the results showed that normal wrist ROM included 5° flexion, 30° dorsal extension, 10° radial deviation, and 15° ulnar deviation. In this context, a recent study showed that daily hand activities can be accomplished at 60% of the maximum ROM of the wrist (Nadeem et al., 2022). This indicates that the ROM offered by the 3DMT-Wrist system is adequate for all requirements of daily life.
Implant loosening is evaluated by continuous radiographs, and is characterized by permeability around the stem or migration by at least 2 mm from the stem profile to the implanted tantalum bead. Data from a study that performed 10-year follow-up after placement of fourth-generation total wrist prostheses (Table 4) have indicated the overall cumulative implant survival rate (with revision as the primary outcome) to be 92%. On including radiologically loosened implants that had not been fixed, the overall implant survival rate was found to be 75% (Fischer et al., 2020). Five-year survival rates of up to 90%–97% have been observed with Maestro or ReMotion implants. In this context, Biax and Maestro implants have been withdrawn from the market as they are no longer economically viable and the Universal II has been updated to the Freedom version (Harlingen et al., 2011). In a study, the cumulative implant survival for Biax, Remotion, and Maestro implants was found to be 81%, 94%, and 95%, respectively, after 5 years of follow-up; the corresponding rates of radiographic loosening were 26%, 18%, and 2%, respectively (Sagerfors et al., 2015).
The ReMotion system includes a titanium plasma-coated CoCr stem for press-fit fixation in the cranial and radial bones, two CoCr carpal screws, and an ovoid CoCr metal-ultra high molecular weight polyethylene joint (Herzberg et al., 2012). The Motec prosthesis has a sandblasted calcium phosphate-coated titanium stem for cementless screw fixation of the capitate/third metacarpal and radius and a metal-on-metal ball-and-socket joint made of CoCr; a small amount of bone cement is required for TWA (Thillemann et al., 2016). In their study, Holm-Glad et al. (Holm-Glad et al., 2022) observed statistically significant increases in blood Cr and Co levels in participants who had undergone TWA with the metal-on-metal Motec prosthesis. Notably, the 3DMT-Wrist system consists of Ti6Al4V carpal and radial components and a polyethylene joint ball; the radial component consists of a Ti6Al4V shank and a CoCrMo articular socket. The surfaces of the carpal and radial stems have a microporous structure measuring 1 mm in thickness; as they are synthesized in one piece by metal 3D printing, there are no issues related to the loss of coating. In addition, the joint interface of the 3DMT-Wrist system comprises metal-on-polyethylene; metal debris should not therefore be generated during activity.
The 3DMT-Wrist system appeared to offer good clinical results. This may be attributed to the personalization of the implant; the osteotomy position and center of rotation of the native joint were planned individually prior to surgery with the aim of maximal restoration of the biomechanical characteristics of the wrist. In addition, the shape of the osteotomy surface was consistent with that of the radius; this minimized the pressure of the prosthesis on the osteotomy plane. The congruence was maintained with the aim of reducing complications such as prosthesis loosening and sinking. Compared to the fourth generation Motec prosthesis, the 3DMT-Wrist radial component is better shaped to match the inner wall of the cortical bone; this improves stability and strength of the radial component until adequate bone growth occurs. This also prevents early loosening due to differences in elastic modulus between the prosthesis and cancellous bone.
Our study has a number of limitations. First, it had a small sample size. In this context, the 3DMT-Wrist system is newly designed, and is not related to the four generations of total wrist joint prostheses currently in use; the duration of follow-up was therefore limited in addition to the sample size. However, follow-up will be continued and further cases will be included to increase the sample size and validate the results of this study. In this context, Krukhaug et al. found no difference in TWA outcomes between high- and low-volume centers in Norway (Krukhaug et al., 2011). Second, the current study did not to compare outcomes of the novel system with those in current use; this is mainly because TWA has recently gained popularity in China and no available total wrist prostheses have been designed and manufactured in the country. Third, the duration of follow-up was inadequate and no cases required revision; however, the patients will be continuously followed-up in future.
In conclusion, the novel 3D-printed microporous titanium artificial wrist joint prosthesis can significantly relieve wrist pain and improve function with good fixation and ROM. The developed prosthesis demonstrated no dislocation or need for revision after 1.6 years’ follow up; this suggests that the novel design has considerable potential for clinical application.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by the Ethics Committee of 920th Hospital of Joint Logistics Support Force, PLA [ER 2019-018 (other)-02]. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
YX, SL, and XC contributed to the conception of the study; XC, BW, BZ, YZ, TW, and WL performed the experiment; XC, BW, and BZ contributed significantly to analysis and manuscript preparation; XC, BW, BZ, and YZ performed the data analyses and wrote the manuscript; YH, BC, and SZ helped perform the analysis with constructive discussions.
The work was partially supported by: 920th Hospital of Joint Logistics Support Force, PLA (2020YGB04); Yunnan Provincial Clinical Orthopaedic Trauma Medical Center (ZX20191001); Yunnan Orthopedics and Sports Rehabilitation Clinical Medicine Research Center (202102AA310068); Yunnan Key Laboratory of Digital Orthopaedics, Yunnan Provincial Science and Technology Department (202005AG070004); LU,WEIJIA WILLIAM expert workstation of Yunnan Province (202005AF150038); Yunnan Provincial Digital Orthopaedic Innovation Team (202105AE160015); Health Commission of Yunnan Province (L-2019006); Yunnan Province Science and Technology Department (202001AS070028); Yunnan Province Science and Technology Program Major Project (202102AA310042).
We would like to thank YH, BC, and SZ for their assistance in design and manufacture of wrist prostheses in this research. We would also like to thank BW for his assistance in photo collection.
YH, BC, and SZ were employed by Suzhou MicroPort OrthoRecon Co.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Berber, O., Garagnani, L., and Gidwani, S. (2018). Systematic review of total wrist arthroplasty and arthrodesis in wrist arthritis. J. Wrist Surg. 7 (5), 424–440. doi:10.1055/s-0038-1646956
Berber, O., Gidwani, S., Garagnani, L., Spiteri, M., Riley, N., McNab, I., et al. (2020). Salvage of the failed total wrist arthroplasty: A systematic review. J. Wrist Surg. 9 (5), 446–456. doi:10.1055/s-0040-1713728
Bidwai, A. S., Cashin, F., Richards, A., and Brown, D. J. (2013). Short to medium results using the remotion total wrist replacement for rheumatoid arthritis. Hand Surg. 18 (2), 175–178. doi:10.1142/s0218810413500202
Boeckstyns, M. E., Herzberg, G., and Merser, S. (2013). Favorable results after total wrist arthroplasty: 65 wrists in 60 patients followed for 5–9 years. Acta Orthop. 84 (4), 415–419. doi:10.3109/17453674.2013.823588
Brumfield, R. H., and Champoux, J. A. (1984). A biomechanical study of normal functional wrist motion. Clin. Orthop. Relat. Res. 187, 23–25. doi:10.1097/00003086-198407000-00004
Damert, H. G. (2019). Total wrist arthroplasty-a review. Orthopade 48 (5), 402–412. doi:10.1007/s00132-019-03725-6
Elbuluk, A. M., Milone, M. T., Capo, J. T., Bosco, J. A., and Klifto, C. S. (2018). Trends and demographics in the utilization of total wrist arthroplasty. J. Hand Surg. Asian Pac 23 (4), 501–505. doi:10.1142/s2424835518500492
Fischer, P., Sagerfors, M., Jakobsson, H., and Pettersson, K. (2020). Total wrist arthroplasty: A 10-year follow-up. J. Hand Surg. Am. 45 (8), 780.e1–780.e10. doi:10.1016/j.jhsa.2020.02.006
Froschauer, S. M., Holzbauer, M., Hager, D., Kwasny, O., and Duscher, D. (2021). Proximal row carpectomy with total scapoidectomy vs. Conventional carpal resection for ReMotion total wrist arthroplasty. J. Clin. Med. 10 (9), 1865. doi:10.3390/jcm10091865
Harlingen, D. v., Heesterbeek, P. J. C., and J de Vos, M. (2011). High rate of complications and radiographic loosening of the biaxial total wrist arthroplasty in rheumatoid arthritis: 32 wrists followed for 6 (5–8) years. Acta Orthop. 82 (6), 721–726. doi:10.3109/17453674.2011.636669
Herzberg, G., Boeckstyns, M., Sorensen, A. I., Axelsson, P., Kroener, K., Liverneaux, P., et al. (2012). Remotion" total wrist arthroplasty: Preliminary results of a prospective international multicenter study of 215 cases. J. Wrist Surg. 1 (1), 17–22. doi:10.1055/s-0032-1323642
Holm-Glad, T., Rokkum, M., Rohrl, S. M., Roness, S., Godang, K., and Reigstad, O. (2022). A randomized controlled trial comparing two modern total wrist arthroplasties: Improved function with stable implants, but high complication rates in non-rheumatoid wrists at two years. Bone Jt. J. 104-b (10), 1132–1141. doi:10.1302/0301-620x.104b10.bjj-2022-0201.r2
Krukhaug, Y., Lie, S. A., Havelin, L. I., Furnes, O., and Hove, L. M. (2011). Results of 189 wrist replacements. A report from the Norwegian Arthroplasty Register. Acta Orthop. 82 (4), 405–409. doi:10.3109/17453674.2011.588858
Ma, Z. J., Liu, Z., Shi, Q., Li, T., Liu, Z., Yang, Z., et al. (2020). Varisized 3D-printed lunate for kienbock's disease in different stages: Preliminary results. Orthop. Surg. 12 (3), 792–801. doi:10.1111/os.12681
Matsui, Y., Minami, A., Kondo, M., Ishikawa, J., Motomiya, M., and Iwasaki, N. (2020). A minimum 5-year longitudinal study of a new total wrist arthroplasty in patients with rheumatoid arthritis. J. Hand Surg. Am. 45 (3), 255.e1–255.e7. doi:10.1016/j.jhsa.2019.06.011
Nadeem, M., Loss, J. G., Li, Z. M., and Seitz, W. H. (2022). Ulnar extension coupling in functional wrist kinematics during hand activities of daily living. J. Hand Surg. 47 (2), 187.e1–187.e13. e113. doi:10.1016/j.jhsa.2021.03.026
Núñez, F. A., Arguelles, A. A., Lozano, L. L., Popescu, D., MaculeF., , and Suso, V. S. (2013). Use of trabecular metal in total knee arthroplasty in severely and morbidly obese patients (BMI > 35 kg/m2). Acta Ortop. Mex. 27 (2), 97.
Palmer, A. K., Werner, F. W., Murphy, D., and Glisson, R. (1985). Functional wrist motion: A biomechanical study. J. Hand Surg. Am. 10 (1), 39–46. doi:10.1016/s0363-5023(85)80246-x
Raheem, A. A., Hameed, P., Whenish, R., Elsen, R. S., G, A., Jaiswal, A. K., et al. (2021). A review on development of bio-inspired implants using 3D printing. Biomimetics (Basel) 6 (4), 65. doi:10.3390/biomimetics6040065
Reigstad, O., Holm-Glad, T., Bolstad, B., Grimsgaard, C., Thorkildsen, R., and Rokkum, M. (2017). Five-to 10-year prospective follow-up of wrist arthroplasty in 56 nonrheumatoid patients. J. Hand Surg. Am. 42 (10), 788–796. doi:10.1016/j.jhsa.2017.06.097
Reigstad, O., and Røkkum, M. (2018). Wrist arthroplasty using prosthesis as an alternative to arthrodesis: Design, outcomes and future. J. Hand Surg. Eur. 43 (7), 689–699. doi:10.1177/1753193418784707
Sagerfors, M., Gupta, A., Brus, O., and Pettersson, K. (2015). Total wrist arthroplasty: A single-center study of 219 cases with 5-year follow-up. J. Hand Surg. Am. 40 (12), 2380–2387. doi:10.1016/j.jhsa.2015.09.016
Srnec, J. J., Wagner, E. R., and Rizzo, M. (2018). Total wrist arthroplasty. JBJS Rev. 6 (6), e9. doi:10.2106/jbjs.rvw.17.00123
Thillemann, J. K., Thillemann, T. M., Munk, B., and Kroner, K. (2016). High revision rates with the metal-on-metal Motec carpometacarpal joint prosthesis. J. Hand Surg. Eur. 41 (3), 322–327. doi:10.1177/1753193415595527
Yang, X., Ma, W., Gu, W., Zhang, Z., Wang, B., Wang, Y., et al. (2021). Multi-scale microstructure high-strength titanium alloy lattice structure manufactured via selective laser melting. RSC Adv. 11 (37), 22734–22743. doi:10.1039/d1ra02355a
Keywords: 3D-printed microporous titanium artificial wrist joint, artificial wrist joint prosthesis, end-stage carpal arthritis, long-term follow up, total wrist arthroplasty
Citation: Cai X, Wang B, Zhang B, Zhang Y, Wang T, Lin W, Huang Y, Chen B, Zhou S, Lu S and Xu Y (2023) Safety and efficacy of a novel three-dimensional printed microporous titanium prosthesis for total wrist arthroplasty in the treatment of end-stage wrist arthritis. Front. Bioeng. Biotechnol. 10:1119720. doi: 10.3389/fbioe.2022.1119720
Received: 09 December 2022; Accepted: 22 December 2022;
Published: 10 January 2023.
Edited by:
Meng Tian, Sichuan University, ChinaReviewed by:
Jianxun Ding, Changchun Institute of Applied Chemistry (CAS), ChinaCopyright © 2023 Cai, Wang, Zhang, Zhang, Wang, Lin, Huang, Chen, Zhou, Lu and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sheng Lu, ZHJsdXNoZW5nQDE2My5jb20=; Yongqing Xu, eHV5b25ncWluZ2ttQDE2My5uZXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.