- Sports Medicine Department, Beijing Jishuitan Hospital, Beijing, China
Objective: Suture tape (ST) is a common synthetic material in the repairing surgery of soft tissue. Recently, ST augmentation (STA) technique has been described as a novel way to improve the mechanical property of grafts in the anterior cruciate ligament (ACL) reconstruction (ACLR). However, the clinical outcomes of ACLR using ST-augmented grafts have not been clarified. This systematic review aimed to summarize the specific technique of STA and evaluate the clinical outcomes after ACLR with STA.
Methods: A electronic search of PubMed and Embase databases with a manual search of Google Scholar was performed to identify studies that reported the clinical outcomes of ACLR with STA. Each included study was abstracted regarding the study features, patient data, surgical information, and outcome measures.
Results: Nine studies were included, representing 314 knees in 314 patients undergoing ACLR with STA. Technically, ST was fixed independently from grafts in six studies and along with grafts in two studies. Most studies applied an equal or slightly less tension on ST than ACL graft. Clinically, significant improvements were found in the Lysholm, IKDC, and KOOS scores after a mean follow-up of 16.7 months. Physical examinations of 220 patients showed significant restoration of knee stability at the final follow-up. 59 of 80 (73.8%) patients returned to preinjury sports level at a minimum 2 year follow-up. Six of 266 (2.3%) patients had a graft failure during the first 2 years postoperatively. The use of ST was significantly associated with better Tegner scores and a trend toward significantly higher rates of return to sport compared to standard ACLR. No significant difference was found in most subjective scores, knee laxity, and graft failures between ACLR with or without STA.
Conclusion: ACLR with STA achieved overall favorable clinical outcomes. Patients using ST-augmented grafts were seemingly associated with better sports performance compared to standard ACLR. But ACLR with STA was not superior to ACLR alone in most functional scores, knee stability measures, and graft failure rates. A tension equal to or slightly less than the ACL graft should be carefully applied on ST during fixation to avoid stress shielding of the graft.
Introduction
Anterior cruciate ligament (ACL) injury is a common sports-related knee trauma with steadily increasing incidence over recent years, exceeding seven injuries per 100,000 games among adolescent athletes (Bram et al., 2021). Due to the critical role of an intact ACL in maintaining knee kinematics (Markolf et al., 2009), ligament reconstruction has long time been the gold standard treatment for ACL injury in restoring stability, preventing early degeneration, and achieving return to preinjury sports (Lai et al., 2018). Despite the well-accepted clinical outcomes of arthroscopic ACL reconstruction (ACLR) using soft tissue grafts, the long process of ligamentization could make the grafts vulnerable to reinjury (Claes et al., 2011), and a high risk of graft failure would be worrying (Samuelsen et al., 2017). Previous studies demonstrated that outcomes after ACLR was related to graft choices (Mouarbes et al., 2019). Considering the inherent biological characteristics of commonly used grafts, interest in methods to increase the strength of graft construct has gradually risen in past decades.
Although synthetic devices to replace the ACL graft have been available since the 1970s, high failure rates and complications such as effusion and synovitis have been reported and limited their wide use (Batty et al., 2015). Other than total substitution, an addition of a broad, braided, ultrahigh-molecular-weight polyethylene/polyester suture tape (ST) is frequently applied in the repairing surgery for soft tissue, including at least the rotator cuff tendon (Boksh et al., 2022), ulnar collateral ligament (Carr et al., 2020), and lateral ankle ligament (Lewis et al., 2021). For the ACL injury, adding an ST as an internal brace was reported to improve the clinical outcomes of ACL suture repair, with comparable results in subjective scores, knee stability, and graft failure rate to standard ACLR (Murray et al., 2020; Hoogeslag et al., 2022). Such inspiring findings indicate that adding an ST to the ACL graft might promote graft healing and remodeling and probably reduce the residual laxity and graft rupture for patients undergoing ACLR.
Currently, the ST augmentation (STA) technique has been described as a novel way to enhance the graft for ACLR (Figure 1), supporting the graft in a load-sharing manner and acting as a “safety belt” to prevent the graft from excessive tension, especially in the early phase of ligamentization (Bachmaier et al., 2018). This effect was supported by biomechanical studies demonstrating that ACLR with STA improved graft stiffness and failure load compared to ACLR alone, reducing tibial displacement under anterior load (Torres et al., 2022). In the clinical scenario, the STA technique has been used for ACLR in several sports medicine centers worldwide in recent 5 years (Mackenzie et al., 2022). However, the clinical superiority of ST-augmented grafts remained unclear, and a summary of available literature on clinical outcomes of ACLR with STA is lacking.
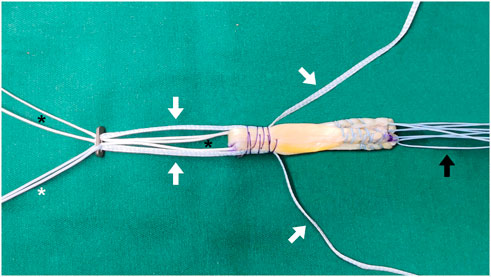
FIGURE 1. The final construct of ST-augmented quadrupled (8-strand) semitendinosus and gracilis tendon autograft, with the ST passing through the femoral button eyelets. White arrow: ST; black arrow: braided nonabsorbable suture; white asterisk: pull suture; black asterisk: adjustable loop suture. ST, suture tape.
Therefore, the purpose of this study was to systematically 1) summarize the specific technique of STA and 2) evaluate the clinical outcomes after ACLR with STA. It was hypothesized that ACLR using ST-augmented grafts would be associated with better functional outcome measures and lower graft failure rates compared to standard ACLR.
Methods
This systematic review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement (Page et al., 2021) and was registered in INPLASY (registration number: INPLASY2022100125).
Search strategy
An electronic search of PubMed and Embase databases was conducted on 12 September 2022 to explore studies reporting clinical outcomes of ACLR using ST-augmented grafts. The following key terms were used for the electronic search: (anterior cruciate ligament OR ACL) AND (tape OR augment OR reinforce OR internal brace). The full search strategies used for each of these electronic databases are available in Supplementary Appendix Tables S1, S2. A manual search of Google Scholar was then performed to identify studies not indexed by the Web of Science.
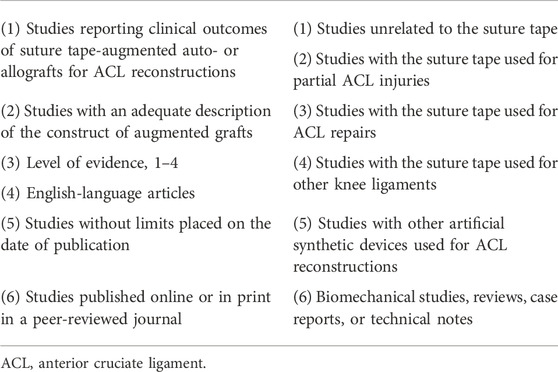
Two authors (Z.Z. and Z.F.) independently assessed all studies and cross-checked the finalized ones according to the inclusion and exclusion criteria (Table 1). The titles and abstracts were initially screened for relevance, then the full texts were critically retrieved for further selection. Reference lists of all included articles were reviewed for potentially eligible studies. Any disagreement about a study’s inclusion was resolved by discussion with a third senior author (H.Z.) involved if consensus could not be achieved.
Data extraction
Each finally included study was abstracted regarding the study features, patient data, surgical information, and outcome measures. Two authors (G.S. and Y.L.) independently extracted the original data, and the final decision on the disagreement was made by a third senior author (H.Z.).
Study features consisted of author name, publication year, journal, study design, level of evidence, and methodological quality. Patient data comprised number of cases, sex, age, length of follow-up, and meniscal status. Surgical information was extracted from the specific descriptions in the original studies, including graft details (choice, construct, diameter, and fixation), tape details (indication, product, and fixation), and concomitant procedures. For outcome measures, all subjective and objective results including pain and function scores, knee laxity measurements, return to sports, graft failures, and other complications were documented. Comparison analysis between pre- and postoperative conditions and between patients with and without STA was recorded. Radiographic and arthroscopic outcomes extracted by follow-up magnetic resonance imaging (MRI) and second-look arthroscopy were not reviewed in this systematic review, as there was no available data in the original studies.
Descriptive statistics were used to report study characteristics, patient data, surgical information, and outcome measures. A quantitative comparison (meta-analysis) of the data was considered inappropriate due to the heterogeneity between studies.
Quality appraisal
The methodologic quality of each included study was assessed with the Methodological Index for Non-Randomized Studies (MINORS). The items in the MINORS criteria for non-randomized studies were scored as 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate) (Slim et al., 2003). For comparative studies, the ideal MINORS score was 24, and a study was considered at low risk of bias when it scored 21–23 and at high risk of bias when it scored ≤20. For non-comparative studies, corresponding thresholds were 16, 13–15, and ≤12 (Slim et al., 2003). The MINORS score of each study was calculated independently by two authors (G.S. and Y.L.). Any disagreement was resolved by discussion until a consensus was reached.
Results
Literature search
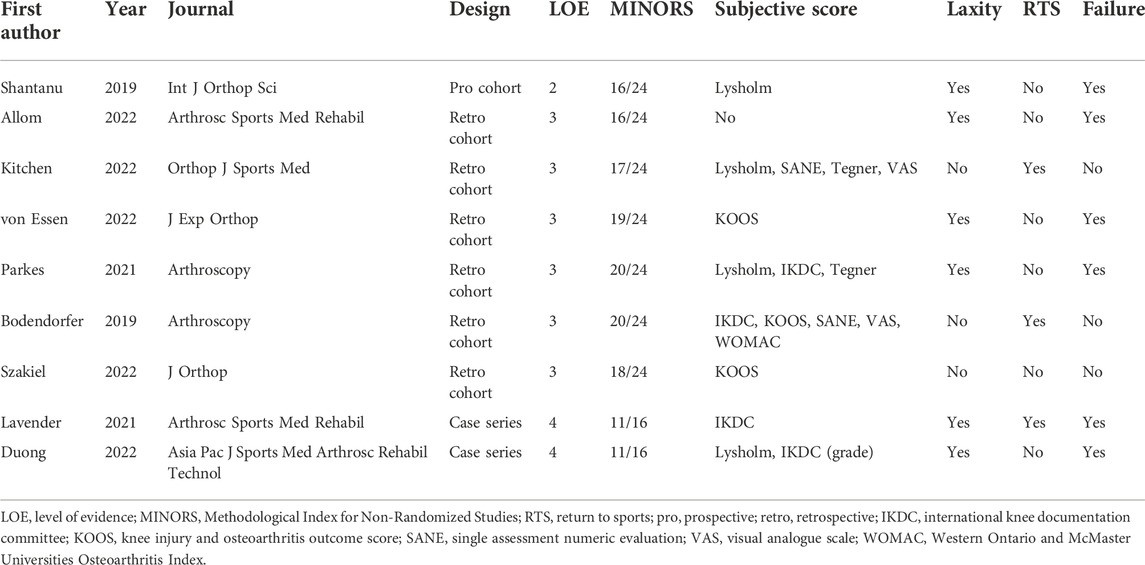
The electronic and manual search identified 1,250 studies for initial screening, and 74 studies proceeded to full-text review. Critical application of the inclusion and exclusion criteria finally yielded nine studies (Figure 2). One was a prospective cohort study (level 2) (Shantanu et al., 2019), six were retrospective cohort studies (level 3) (Bodendorfer et al., 2019; Parkes et al., 2021; Allom et al., 2022; Kitchen et al., 2022; Szakiel et al., 2022; von Essen et al., 2022), and two were case series (level 4) (Lavender et al., 2021; Duong et al., 2022). All seven comparative studies were designed to compare patients who underwent ACLR with and without ST-augmented grafts (Table 2).
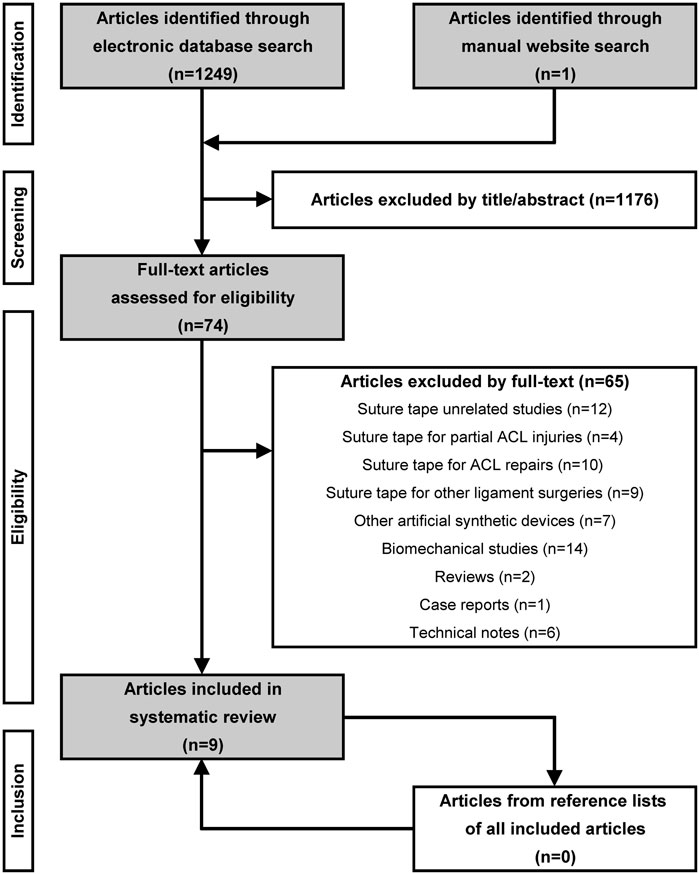
FIGURE 2. Flowchart of search strategy following the PRISMA 2020 statement (Page et al., 2021). ACL, anterior cruciate ligament.
Quality appraisal
A high risk of bias was confirmed in all seven comparative studies with a mean MINORS value of 18.0 ± 1.6 (range, 16–20). The two non-comparative studies were also at high risk of bias with a MINORS value of 11 for each (Table 2). The risk of bias mainly came from an unblinded assessment of the study endpoint, followed by a lack of prospective calculation of the study size and a historical comparison between the study and control group. The full appraisal for each study is available in Supplementary Appendix Table S3.
Patient characteristics
A total of 314 knees of 314 patients undergoing ACLR with STA were enrolled in this systematic review (Table 3). There were 190 (60.5%) males and 124 females (39.5%) with a mean age of 26.6 years (range, 15.7–33.0 years). The mean clinical follow-up was 16.7 months (range, 6.0–29.0 months). The meniscal status at the time of ACLR was documented in six studies, and the incidence of meniscal tears was 49.0% (125/255) overall, 32.0% (72/225) for the medial, and 32.9% (74/225) for the lateral.
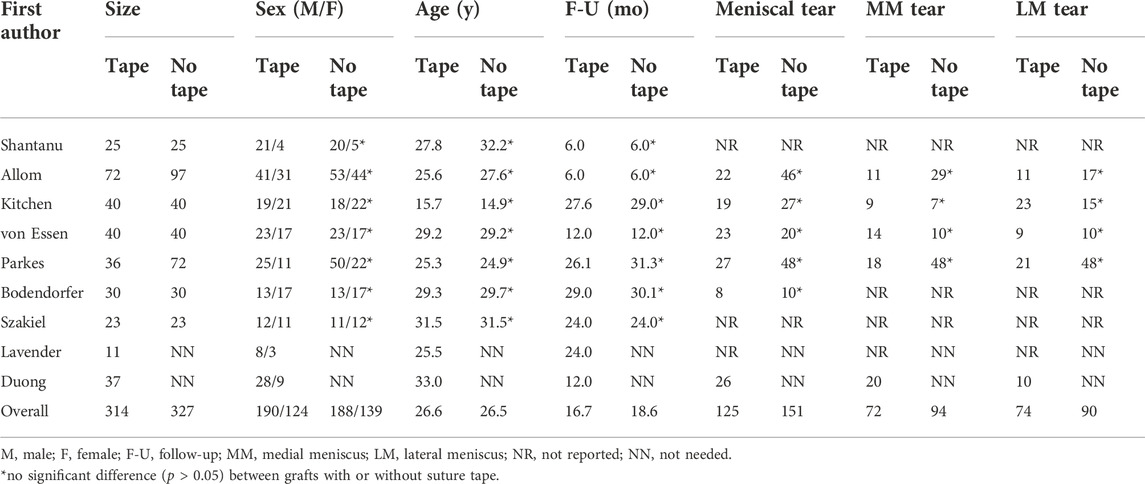
TABLE 3. Patient characteristics between anterior cruciate ligament reconstruction with or without suture tape augmentation.
Surgical information
ACLRs were performed with 283 hamstring tendon auto- or allografts in eight studies, 20 quadriceps tendon autografts in one study, and 11 bone-patellar tendon-bone autografts in one study (Table 4). ACL grafts were augmented with FiberTape (Arthrex, United States) in 231 patients and InternalBrace (Arthrex, United States) in 11 patients, and the product used in the rest 72 patients was not described. Different fixation methods of the graft-ST construct were applied. On the femoral side, the suspensory device was used in eight studies, with the ST passing through the eyelets of the suspensory button in eight studies and the loop of the suspensory button in two studies. On the tibial side, the suspensory device was used in seven studies and the interference screw in two studies, with the ST fixed independently from the graft using an additional anchor before graft fixation in six studies and along with the graft using the same fixation device in two studies. Most studies applied an equal or slightly less tension on the ST than the ACL graft during fixation. For all studies, the use of ST was based on the surgeon’s preference, except for one prospective cohort study with randomized selection. Concomitant lateral extra-articular tenodesis was performed in one study (Allom et al., 2022) for 84/169 patients with risk factors for graft rupture.
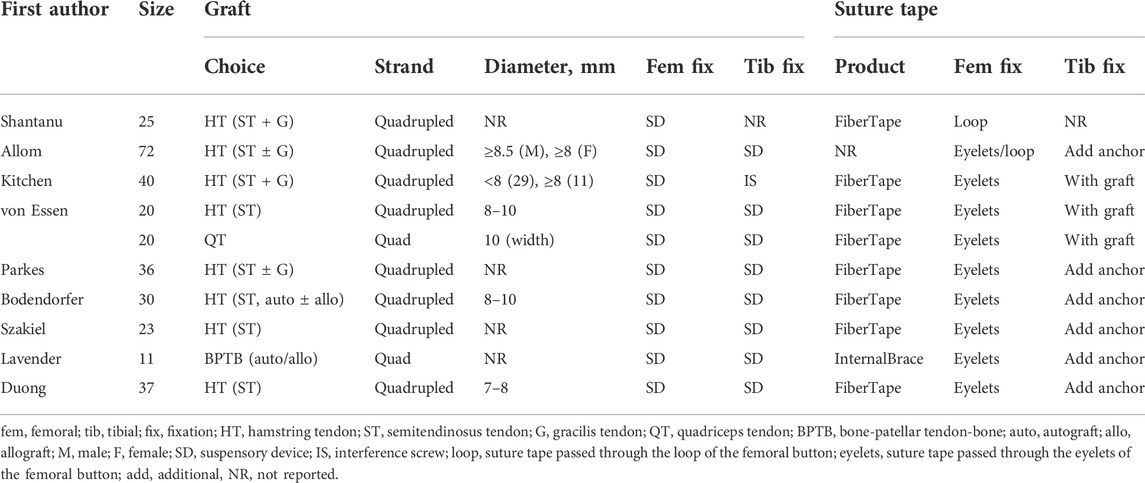
TABLE 4. Surgical technique of anterior cruciate ligament reconstruction with suture tape augmentation.
Subjective scores
Overall, eight subjective scores were reported in eight out of nine studies: the Lysholm score in four studies, International Knee Documentation Committee (IKDC) score in three studies, Knee injury and Osteoarthritis Outcome Score (KOOS) score in three studies, Single Assessment Numeric Evaluation (SANE) score in two studies, Tegner activity score in two studies, visual analogue scale (VAS) score in two studies, Western Ontario and McMaster Universities Osteoarthritis (WOMAC) score in one study, and IKDC grade in one study. The remaining one study (Allom et al., 2022) not reporting any subjective score (Table 2).
Seven studies compared subjective scores between pre- and postoperative status for ACLR with STA, and significant improvement was reported in six studies. Those used at least in two studies included the Lysholm score from 61.2 to 91.2 (Shantanu et al., 2019; Duong et al., 2022), IKDC score from 30.7 to 85.8 (Bodendorfer et al., 2019; Lavender et al., 2021), and KOOS score from 60.9 to 89.1 (Bodendorfer et al., 2019; Szakiel et al., 2022; von Essen et al., 2022). The IKDC grade was reported in one study (Duong et al., 2022) with the grade (A/B/C/D) from 0/0/19/18 to 30/7/0/0. The comparison of the other three scores was only performed in one study (Bodendorfer et al., 2019) with the SANE score from 96.0 to 90.0, VAS score from 7.1 to 1.6, and WOMAC score from 35.5 to 2.2. Only one study (Parkes et al., 2021) demonstrated no significant improvement in the Tegner score (from 7.2 to 7.1).
Six studies compared subjective scores between ACLR with or without STA at the final follow-up. The Tegner score used in two studies (Parkes et al., 2021; Kitchen et al., 2022) both yielded superior results in the augmentation group. Results of other scores were inconsistent across studies. Only one study (Bodendorfer et al., 2019) reported that the VAS (1.6 versus 3.4), IKDC (87.6 versus 73.2), KOOS (92.2 versus 87.1), SANE (90.0 versus 80.0), and WOMAC (2.2 versus 6.2) score were all significantly better in augmentation group. However, no significant superiority of any score other than the Tenger was found in the augmentation group among other studies (Table 5).
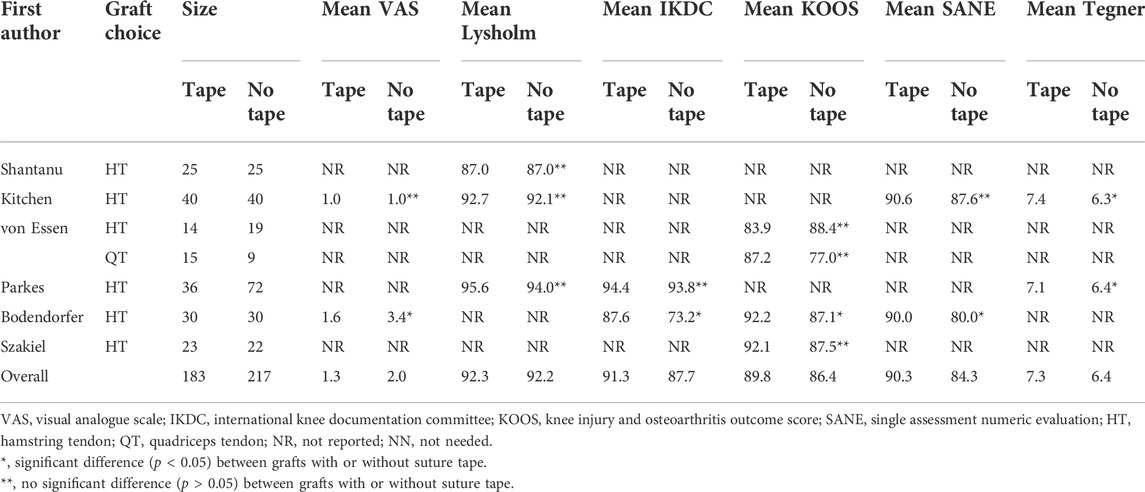
TABLE 5. Postoperative subjective scores between anterior cruciate ligament reconstruction with or without suture tape augmentation.
Objective knee laxity
Knee laxity was evaluated by the Lachman test in five studies, pivot shift test in four studies, and KT-1000/2000 arthrometer test in two studies (Table 6). In all these studies, significant improvement in objective stability was reported in patients with ST-augmented grafts at the final follow-up. The comparative analysis of knee laxity between ACLR using ST-augmented grafts and not was performed in four studies. No studies reported superior objective stability in the augmentation group at the final follow-up, although one of which (Shantanu et al., 2019) reported better improvement in grades of the Lachman test as the preoperative laxity in the augmentation group was severer.
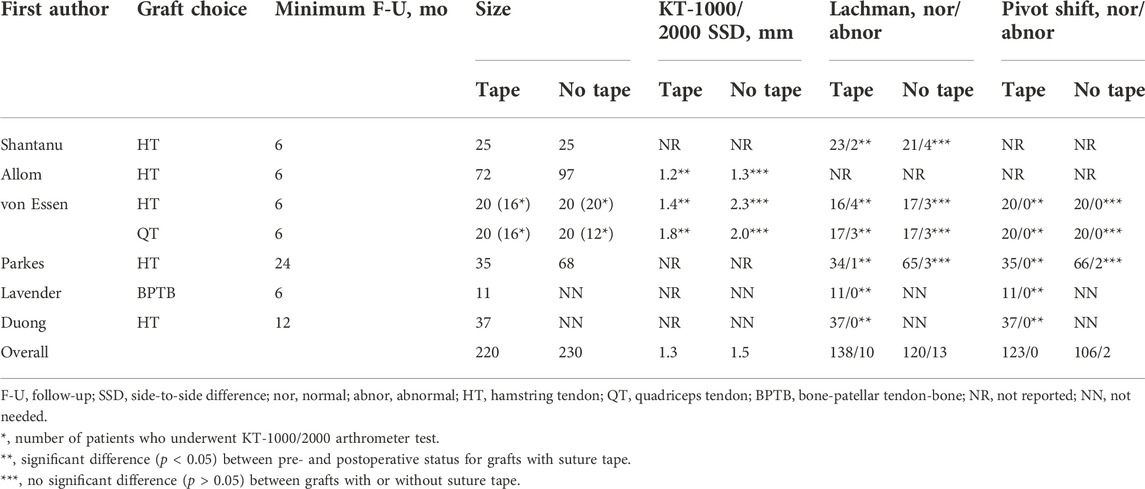
TABLE 6. Postoperative objective knee laxity between anterior cruciate ligament reconstruction with or without suture tape augmentation.
Return to sports
The ability to return to preinjury sports level was evaluated in three studies, with an overall rate of 73.8% (range, 69.2%–81.8%) in patients with ST-augmented ACL grafts (Table 7). The ability to return to sports between patients with or without STA was compared in two studies. Both demonstrated no (but a trend toward) significant difference in the rate of return to sports at a minimum 2-year follow-up, and one of them (Bodendorfer et al., 2019) reported that the use of ST was significantly correlated with earlier time to return (9.2 months versus 12.9 months).

TABLE 7. Return to preinjury sports level between anterior cruciate ligament reconstruction with or without suture tape augmentation.
Graft failures and other complications
The graft failure and other major complications were recorded in seven studies (Table 8). The overall failure rate of ST-augmented grafts was 2.3% (range, 0%–6.7%) among 266 patients. The comparison of failure between grafts with or without ST proceeded in five studies. Almost all studies reported a lower failure rate in ST-augmented grafts, but the difference did not meet statistical significance. Other complications including further meniscal tear, arthrofibrosis, cyclops lesion, and infection were also not significantly different in any of these studies.
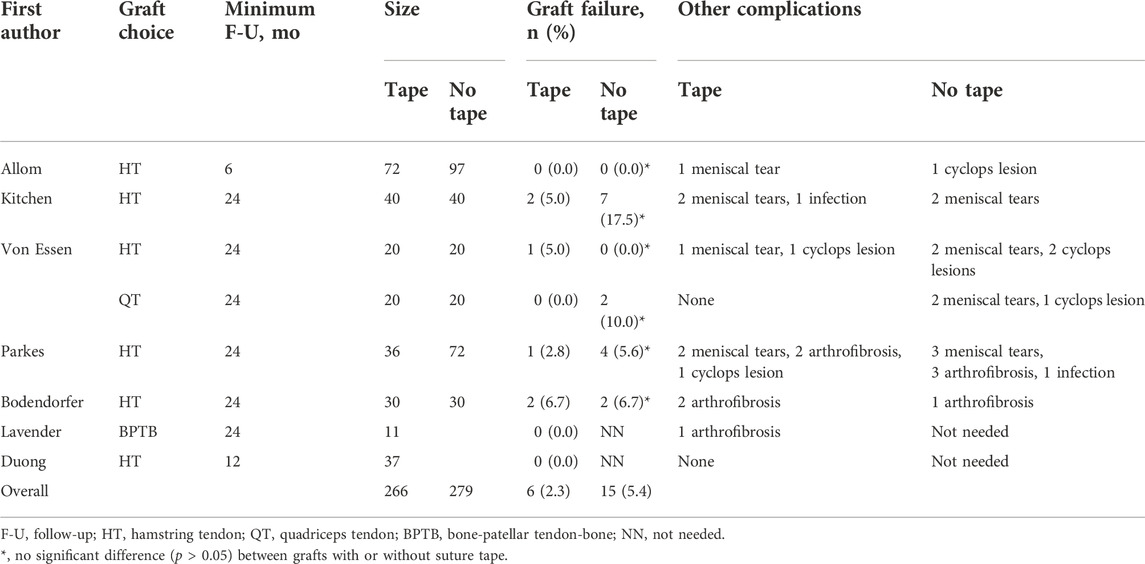
TABLE 8. Graft failure and other complications between anterior cruciate ligament reconstruction with or without suture tape augmentation.
Discussion
The most important findings of this systematic review could be summarized as follows: 1) patients with ST-augmented grafts obtained overall favorable clinical outcomes after ACLR; 2) the use of ST was associated with significantly higher Tegner activity score and a trend toward significantly better ability to return to sports compared with standard ACLR; 3) no significant differences in most subjective scores, knee laxity, and graft failure were found between patients undergoing ACLR with STA and ACLR alone; and 4) most authors preferred an equal or slightly less tension on the ST than the ACL graft during fixation.
In recent 2–5 years, the use of ST to improve the biomechanical performance of ACL graft has been a hot topic in the field of sports medicine, intending to protect the graft from over-loads during the early rehabilitation phase when the graft is weak secondary to necrosis and remodeling process during this time (Claes et al., 2011). As suggested by animal models, adding an ST improved the mechanical properties of the ACL graft by the load-sharing effect, characterized by reduced graft elongation and increased load to failure (Bachmaier et al., 2018), and this function was especially dramatic in smaller -diameter grafts (Noonan et al., 2020), occurring earlier and carrying final loads with a greater extent (Bachmaier et al., 2022). Cadaveric studies further demonstrated that the increased graft-ST construct stiffness was associated with improved knee stability after ACLR, manifested as decreased tibial displacement under anterior load when the ACL graft was augmented with ST (Torres et al., 2022).
Despite increased mechanical strength, an over-tensioned ST possibly led to stress shielding of the ACL graft, compromising the graft ligamentization process (Muellner et al., 2001). Therefore, proper tension of the ST should be carefully applied during fixation in clinical practice to avoid stress shielding of the graft. Among the included studies, the majority preferred to fix the ST independent from the graft on the tibial side, with equal or slightly less manual tension on the ST. If fixed together, the ST was pulled to just remove the slack but without applying tension on the ST. For the same purpose, some suggested fixing the ST in full or hyperextension and the graft in 30° of flexion. As proposed by biomechanical studies, an ideal augmentation effect should be dynamic, permitting lower loads transferred by the graft and only acting as a “safety belt” when strains exceed (Bachmaier et al., 2018). However, whether mechanically improved graft constructs would achieve better surgical outcomes of ACLR in clinical scenarios needs to be further verified.
For the functional outcomes in patients with ACLR and STA, this systematic review showed consistent improvements in nearly all subjective scores at a mean follow-up of 16.7 months, indicating amelioration of clinical symptoms. Meanwhile, significant improvement in objective knee stability was reported in five studies, and no positive pivot shift was observed at the final follow-up. However, as opposed to the study hypothesis, the addition of ST failed to show superiority in either subjective scores or objective stability compared to standard ACLR among nearly all included studies. Based on this evidence, improved mechanical behavior of ST-augmented grafts would not necessarily lead to better subjective function and mechanical stability after ACLR, and the clinical implication of STA requires assessments from specific aspects.
Interestingly, the only subjective score exhibiting superiority in STA was the Tegner activity score, implying better maintenance of sports level in patients using augmented grafts. Such findings were consistent with the results on the ability to return to sports that patients with STA had a significantly earlier time to return to preinjury level and a trend toward a significantly higher proportion to return to preinjury level. Meanwhile, the rate (69.2%–81.8%) of return to preinjury level in patients undergoing ACLR and STA was comparable with the literature. In a recent systematic review of ACLR in the athletic population, the rate of return to preinjury level was 32%–64% in bone-patellar tendon-bone autografts and 9%–65% in hamstring tendon autografts (DeFazio et al., 2020). The causes of better sports performance in patients with STA was unable to be clarified according to the current data since the objective stability was similar and the rehabilitation protocol was identical between patient with or without STA. A potential explanation could be the better confidence in return to sports in patients with STA as they were aware of the use of ST (Keays et al., 2022).
One of the expectations for the use of STA is to protect the ACL graft from a high risk of failure. In this systematic review, the failure rate of ST-augmented ranged from 0% to 6.7%, considered satisfactory and compared similarly to the results of previous studies that 0%–6.1% of athletes experienced graft ruptures at a minimum 2-year follow-up after standard ACLR (DeFazio et al., 2020). Nevertheless, although the use of ST was seemingly associated with a lower failure rate, the difference between grafts with or without ST was not of statistical significance. Considering that half to three-quarters of graft failures would occur in the first 1–2 years following ACLR (Webster and Feller, 2016), the mechanical protection of ST to the ACL graft might not reduce the risk of failures.
The biocompatibility of synthetic material is another concern about the intra-articular use of ST. Even for the more recent designs of synthetic ligament devices, the chronic inflammatory response of the synovium was still reported to be a common finding after ACLR using the Ligament Augmentation and Reconstruction System, which comprises fibers of terephthalic polyethylene polyester (Tulloch et al., 2019). However, histologic assessments in an animal model did not confirm any ST-associated immune responses or cartilage erosions at 6 months following ACLR and STA (Smith et al., 2019). In this systematic review, complications including arthrofibrosis, cyclops lesion, and infection were at a low incidence and similar between ACLR with or without STA, supporting the safety of ST added in ACL grafts.
Clinically, the signal intensity on MRI has been commonly used to monitor the graft ligamentization process after ACLR, with a higher intensity revealing a poor structural strength (Fleming et al., 2011). According to radiological studies, the signal intensity of ACL graft reached its peak at 6 months, followed by a gradual decline until 2–3 years postoperatively (Lansdown et al., 2020; Warth et al., 2020). Unfortunately, no included studies conducted an MRI analysis of ACL grafts. A serial evaluation of the graft signal is necessary to explore if the ligamentization process would be improved with the STA technique in future studies.
Limitations
The limitations of this systematic review were largely from the results of input literature. Firstly, the low level of evidence and high risk of bias within the majority of included studies lowered the validity of this review. Second, the heterogeneity and insufficient data across the original literature restricted the application of a formal meta-analysis. Third, variable reports of outcome measures made this review unable to draw a firm conclusion on the superiority of STA from the clinical perspective. Fourth, the surgical indication of STA lacked a specific description, leading to uncertainty that patients with what features would more benefit from the ST-augmented grafts. Fifth, no radiological or arthroscopic methods were used to evaluate the intra-articular condition after ACLR with STA. Despite the limitations, this is the first study to systematically review the clinical outcomes of ACLR with STA, with a comparison to standard ACLR. This study could be helpful to direct future studies that seek to explore the clinical effectiveness of STA in ACLR.
Conclusion
Clinically, the application of STA achieved overall favorable outcomes in patients with ACLR. ACLR using ST-augmented grafts was seemingly associated with better sports performance compared to standard ACLR. However, despite inconsistent reports across original studies, ACLR with STA did not yield superior results in most functional scores, knee stability measures, and graft failure rates than ACLR alone. Technically, proper tension of the ST should be carefully applied during fixation with an equal or slightly less tension on the ST than the ACL graft to avoid stress shielding of the graft.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: This is a systematic review using data extracted from previously published literature. Requests to access these datasets should be directed to TZ, emhlbmd0b25nMjAyMEBwa3UuZWR1LmNu.
Author contributions
TZ conducted the descriptive statistics and drafted the manuscript. YC participated in the data analysis and helped to draft the manuscript. GS and YL extracted the original data and assessed the methodologic quality. ZZ and ZF retrieved the literature and completed the study inclusion. HZ conceived the study and was involved in the study inclusion and data extraction. All authors reviewed and approved the final version of the manuscript.
Funding
GS has received funding from the National Natural Science Foundation of China (82002288) and Beijing Municipal Health Commission (BJRITO-RDP-2023). YL has received funding from the Beijing Municipal Excellent Talents Foundation (2018000021469G224). HZ has received funding from the National Natural Science Foundation of China (82172514), Beijing Municipal Science and Technology Commission (Z211100002921043), Capital Health Research and Development of Special Fund (CFH 2020-1-2071 and CFH 2020-2-2075), and Beijing Jishuitan Hospital High-Level Talent Program (XKGG202109).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fbioe.2022.1065314/full#supplementary-material
References
Allom, R. J., Wood, J. A., Chen, D. B., and Macdessi, S. J. (2022). The addition of suture tape to the hamstring graft construct does not reduce instrumented knee laxity following ACL reconstruction. Arthrosc. Sports Med. Rehabilitation 4 (2), e545–e551. doi:10.1016/j.asmr.2021.11.015
Bachmaier, S., Smith, P. A., Argintar, E. H., Chahla, J., Higgins, L. D., and Wijdicks, C. A. (2022). Independent suture augmentation with all-inside anterior cruciate ligament reconstruction reduces peak loads on soft-tissue graft. A biomechanical full-construct study. Arthrosc. J. Arthrosc. Relat. Surg. 38 (1), 88–98. doi:10.1016/j.arthro.2021.09.032
Bachmaier, S., Smith, P. A., Bley, J., and Wijdicks, C. A. (2018). Independent suture tape reinforcement of small and standard diameter grafts for anterior cruciate ligament reconstruction: A biomechanical full construct model. Arthrosc. J. Arthrosc. Relat. Surg. 34 (2), 490–499. doi:10.1016/j.arthro.2017.10.037
Batty, L. M., Norsworthy, C. J., Lash, N. J., Wasiak, J., Richmond, A. K., and Feller, J. A. (2015). Synthetic devices for reconstructive surgery of the cruciate ligaments: A systematic review. Arthrosc. J. Arthrosc. Relat. Surg. 31 (5), 957–968. doi:10.1016/j.arthro.2014.11.032
Bodendorfer, B. M., Michaelson, E. M., Shu, H. T., Apseloff, N. A., Spratt, J. D., Nolton, E. C., et al. (2019). Suture augmented versus standard anterior cruciate ligament reconstruction: A matched comparative analysis. Arthrosc. J. Arthrosc. Relat. Surg. 35 (7), 2114–2122. doi:10.1016/j.arthro.2019.01.054
Boksh, K., Haque, A., Sharma, A., Divall, P., and Singh, H. (2022). Use of suture Tapes versus conventional sutures for arthroscopic rotator cuff repairs: A systematic review and meta-analysis. Am. J. Sports Med. 50 (1), 264–272. doi:10.1177/0363546521998318
Bram, J. T., Magee, L. C., Mehta, N. N., Patel, N. M., and Ganley, T. J. (2021). Anterior cruciate ligament injury incidence in adolescent athletes: A systematic review and meta-analysis. Am. J. Sports Med. 49 (7), 1962–1972. doi:10.1177/0363546520959619
Carr, J. B., Camp, C. L., and Dines, J. S. (2020). Elbow ulnar collateral ligament injuries: Indications, management, and outcomes. Arthrosc. J. Arthrosc. Relat. Surg. 36 (5), 1221–1222. doi:10.1016/j.arthro.2020.02.022
Claes, S., Verdonk, P., Forsyth, R., and Bellemans, J. (2011). The "ligamentization" process in anterior cruciate ligament reconstruction: What happens to the human graft? A systematic review of the literature. Am. J. Sports Med. 39 (11), 2476–2483. doi:10.1177/0363546511402662
Defazio, M. W., Curry, E. J., Gustin, M. J., Sing, D. C., Abdul-Rassoul, H., Ma, R., et al. (2020). Return to sport after ACL reconstruction with a btb versus hamstring tendon autograft: A systematic review and meta-analysis. Orthop. J. Sports Med. 8 (12), 232596712096491. doi:10.1177/2325967120964919
Duong, T. D., Tran, D. T., Do, B. N. T., Nguyen, T. T., Le, S. M., and Le, H. H. (2022). All-inside arthroscopic anterior cruciate ligament reconstruction with internal brace ligament augmentation using semitendinosus tendon autograft: A case series. Asia-Pacific J. Sports Med. Arthrosc. Rehabilitation Technol. 29, 15–21. doi:10.1016/j.asmart.2022.05.002
Fleming, B. C., Vajapeyam, S., Connolly, S. A., Magarian, E. M., and Murray, M. M. (2011). The use of magnetic resonance imaging to predict ACL graft structural properties. J. Biomechanics 44 (16), 2843–2846. doi:10.1016/j.jbiomech.2011.09.004
Hoogeslag, R. a. G., T Veld, R., Brouwer, R. W., De Graaff, F., and Verdonschot, N. (2022). Huis inAcute anterior cruciate ligament rupture: Repair or reconstruction? Five-year results of a randomized controlled clinical trial. Am. J. Sports Med. 50 (7), 1779–1787. doi:10.1177/03635465221090527
Keays, S. L., Mellifont, D. B., Keays, A. C., Stuelcken, M. C., Lovell, D. I., and Sayers, M. G. L. (2022). Long-term return to sports after anterior cruciate ligament injury: Reconstruction vs No reconstruction-A comparison of 2 case series. Am. J. Sports Med. 50 (4), 912–921. doi:10.1177/03635465211073152
Kitchen, B. T., Mitchell, B. C., Cognetti, D. J., Siow, M. Y., Howard, R., Carroll, A. N., et al. (2022). Outcomes after hamstring ACL reconstruction with suture tape reinforcement in adolescent athletes. Orthop. J. Sports Med. 10 (4), 232596712210855. doi:10.1177/23259671221085577
Lai, C. C. H., Ardern, C. L., Feller, J. A., and Webster, K. E. (2018). Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: A systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br. J. Sports Med. 52 (2), 128–138. doi:10.1136/bjsports-2016-096836
Lansdown, D. A., Xiao, W., Zhang, A. L., Allen, C. R., Feeley, B. T., Li, X., et al. (2020). Quantitative imaging of anterior cruciate ligament (ACL) graft demonstrates longitudinal compositional changes and relationships with clinical outcomes at 2 years after ACL reconstruction. J. Orthop. Res. 38 (6), 1289–1295. doi:10.1002/jor.24572
Lavender, C., Singh, V., Berdis, G., Fravel, W., Lamba, C., and Patel, T. (2021). Anterior cruciate ligament (ACL) reconstruction augmented with bone marrow concentrate, demineralized bone matrix, autograft bone, and a suture tape (the fertilized ACL). Arthrosc. Sports Med. Rehabilitation 3 (6), e1719–e1722. doi:10.1016/j.asmr.2021.07.030
Lewis, T. L., Joseph, A., Patel, A., Ahluwalia, R., and Ray, R. (2021). Modified brostrom repair with suture tape augmentation for lateral ankle instability: A systematic review. Foot Ankle Surg. 27 (3), 278–284. doi:10.1016/j.fas.2020.12.004
Mackenzie, C. E. A., Huntington, L. S., and Tulloch, S. (2022). Suture tape augmentation of anterior cruciate ligament reconstruction increases biomechanical stability: A scoping review of biomechanical, animal, and clinical studies. Arthrosc. J. Arthrosc. Relat. Surg. 38 (6), 2073–2089. doi:10.1016/j.arthro.2021.12.036
Markolf, K. L., Park, S., Jackson, S. R., and Mcallister, D. R. (2009). Anterior-posterior and rotatory stability of single and double-bundle anterior cruciate ligament reconstructions. J. Bone Jt. Surgery-American Volume 91 (1), 107–118. doi:10.2106/JBJS.G.01215
Mouarbes, D., Menetrey, J., Marot, V., Courtot, L., Berard, E., and Cavaignac, E. (2019). Anterior cruciate ligament reconstruction: A systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone-patellar tendon-bone and hamstring-tendon autografts. Am. J. Sports Med. 47 (14), 3531–3540. doi:10.1177/0363546518825340
Muellner, T., Kwasny, O., Loehnert, V., Mallinger, R., Unfried, G., Schabus, R., et al. (2001). Light and electron microscopic study of stress-shielding effects on rat patellar tendon. Archives Orthop. Trauma Surg. 121 (10), 561–565. doi:10.1007/s004020100281
Murray, M. M., Fleming, B. C., Badger, G. J., Team, B. T., Freiberger, C., Henderson, R., et al. (2020). Bridge-enhanced anterior cruciate ligament repair is not inferior to autograft anterior cruciate ligament reconstruction at 2 Years: Results of a prospective randomized clinical trial. Am. J. Sports Med. 48 (6), 1305–1315. doi:10.1177/0363546520913532
Noonan, B. C., Bachmaier, S., Wijdicks, C. A., and Bedi, A. (2020). Independent suture tape reinforcement of tripled smaller-diameter and quadrupled grafts for anterior cruciate ligament reconstruction with tibial screw fixation: A biomechanical full construct model. Arthrosc. J. Arthrosc. Relat. Surg. 36 (2), 481–489. doi:10.1016/j.arthro.2019.06.036
Page, M. J., Moher, D., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 372, n160. doi:10.1136/bmj.n160
Parkes, C. W., Leland, D. P., Levy, B. A., Stuart, M. J., Camp, C. L., Saris, D. B. F., et al. (2021). Hamstring autograft anterior cruciate ligament reconstruction using an all-inside technique with and without independent suture tape reinforcement. Arthrosc. J. Arthrosc. Relat. Surg. 37 (2), 609–616. doi:10.1016/j.arthro.2020.09.002
Samuelsen, B. T., Webster, K. E., Johnson, N. R., Hewett, T. E., and Krych, A. J. (2017). Hamstring autograft versus patellar tendon autograft for ACL reconstruction: Is there a difference in graft failure rate? A meta-analysis of 47, 613 patients. Clin. Orthop. Relat. Res. 475 (10), 2459–2468. doi:10.1007/s11999-017-5278-9
Shantanu, K., Singh, S., Ratha, S., Kumar, D., and Sharma, V. (2019). Comparative study of functional outcomes of arthroscopic ACL reconstruction by augmented hamstring graft with fiber tape and hamstring graft alone: A prospective study. Int. J. Orthop. Sci. 5 (3), 165–173. doi:10.22271/ortho.2019.v5.i3d.1526
Slim, K., Nini, E., Forestier, D., Kwiatkowski, F., Panis, Y., and Chipponi, J. (2003). Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J. Surg. 73 (9), 712–716. doi:10.1046/j.1445-2197.2003.02748.x
Smith, P. A., Bozynski, C. C., Kuroki, K., Henrich, S. M., Wijdicks, C. A., and Cook, J. L. (2019). Intra-articular biocompatibility of multistranded, long-chain polyethylene suture tape in a canine ACL model. J. Knee Surg. 32 (6), 525–531. doi:10.1055/s-0038-1655765
Szakiel, P. M., Aksu, N. E., Kirloskar, K. M., Gruber, M. D., Zittel, K. W., Grieme, C. V., et al. (2022). Rehabilitation and functional outcomes in internally braced and standard ACL reconstructions. J. Orthop. 33, 95–99. doi:10.1016/j.jor.2022.07.002
Torres, S. J., Nelson, T. J., Pham, N., Uffmann, W., Limpisvasti, O., and Metzger, M. F. (2022). Suture tape augmentation increases the time-zero stiffness and strength of anterior cruciate ligament grafts: A cadaveric study. Arthrosc. Sports Med. Rehabilitation 4 (4), e1253–e1259. doi:10.1016/j.asmr.2022.02.008
Tulloch, S. J., Devitt, B. M., Norsworthy, C. J., and Mow, C. (2019). Synovitis following anterior cruciate ligament reconstruction using the LARS device. Knee Surg. Sports Traumatol. Arthrosc. 27 (8), 2592–2598. doi:10.1007/s00167-018-5280-0
Von Essen, C., Sarakatsianos, V., Cristiani, R., and Stalman, A. (2022). Suture tape reinforcement of hamstring tendon graft reduces postoperative knee laxity after primary ACL reconstruction. J. Exp. Orthop. 9 (1), 20. doi:10.1186/s40634-022-00454-2
Warth, R. J., Zandiyeh, P., Rao, M., Gabr, R. E., Tashman, S., Kumaravel, M., et al. (2020). Quantitative assessment of in vivo human anterior cruciate ligament autograft remodeling: A 3-dimensional UTE-T2* imaging study. Am. J. Sports Med. 48 (12), 2939–2947. doi:10.1177/0363546520949855
Keywords: anterior cruciate ligament, suture tape, synthetic materials, augmentation, outcomes
Citation: Zheng T, Cao Y, Song G, Li Y, Zhang Z, Feng Z and Zhang H (2023) Suture tape augmentation, a novel application of synthetic materials in anterior cruciate ligament reconstruction: A systematic review. Front. Bioeng. Biotechnol. 10:1065314. doi: 10.3389/fbioe.2022.1065314
Received: 09 October 2022; Accepted: 21 November 2022;
Published: 03 January 2023.
Edited by:
Yansong Qi, Inner Mongolia People's Hospital, ChinaReviewed by:
Ning Liang, First Hospital of Tsinghua University, ChinaBo Ren, Xi'an Honghui Hospital, China
Hosam Alzahrani, Taif University, Saudi Arabia
Copyright © 2023 Zheng, Cao, Song, Li, Zhang, Feng and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Zhang, emh1aTc2QDEyNi5jb20=
 Tong Zheng
Tong Zheng Yanwei Cao
Yanwei Cao