- 1Data Science & Machine Learning Division, PERMEDIQ GmbH, Wang, Germany
- 2Faculty of Electrical Engineering and Computer Science, Hochschule Aalen, Aalen, Germany
- 3John von Neumann Faculty of Informatics, Óbuda University, Budapest, Hungary
Background: Medicine is characterized by its inherent uncertainty, i.e., the difficulty of identifying and obtaining exact outcomes from available data. Electronic Health Records aim to improve the exactitude of health management, for instance using automatic data recording techniques or the integration of structured as well as unstructured data. However, this data is far from perfect and is usually noisy, implying that epistemic uncertainty is almost always present in all biomedical research fields. This impairs the correct use and interpretation of the data not only by health professionals but also in modeling techniques and AI models incorporated in professional recommender systems.
Method: In this work, we report a novel modeling methodology combining structural explainable models, defined on Logic Neural Networks which replace conventional deep-learning methods with logical gates embedded in neural networks, and Bayesian Networks to model data uncertainties. This means, we do not account for the variability of the input data, but we train single models according to the data and deliver different Logic-Operator neural network models that could adapt to the input data, for instance, medical procedures (Therapy Keys depending on the inherent uncertainty of the observed data.
Result: Thus, our model does not only aim to assist physicians in their decisions by providing accurate recommendations; it is above all a user-centered solution that informs the physician when a given recommendation, in this case, a therapy, is uncertain and must be carefully evaluated. As a result, the physician must be a professional who does not solely rely on automatic recommendations. This novel methodology was tested on a database for patients with heart insufficiency and can be the basis for future applications of recommender systems in medicine.
1 Introduction
In daily business, physicians are confronted with the constant integration and evaluation of different parameters to assess the patient’s condition and in this way, establish correct diagnoses as well as therapies, which are standardized and encoded as Therapy Keys (TKs). This assessment is particularly difficult for health professionals due to the constant work overload in health centers. In addition, there is a cognitive impairment that represents selecting an item, like a potential therapy, from a portfolio with several options (Hall and Walton, 2004). To this end, support systems represent the most effective option to assist the daily work of health professionals; but these systems require mathematical models.
Traditionally, such support systems have been defined as expert systems (Sandell and Bourne, 1985), (Zhou et al., 2021). But recently, with the development of efficient computing methods, the use of deep learning methods has found more acceptance, for instance for pattern recognition not only of medical images but also of data contained in EHRs for the development of, for instance, recommender systems in medicine (Rajkomar et al., 2018). Any model used in medicine must, however, be explainable, i.e., the customer must be able to understand how the results can be obtained.
Conventional methods of machine learning, like decision trees, are essentially explainable since the derivation of the final result can be tracked throughout the entire computation process. However, these methods are limited by their accuracy and scalability, i.e., their ability to handle an ever-growing amount of information. Deep learning methods are an attractive option over other modeling alternatives. The methods based on this method are unfortunately unexplainable, since the computation of the network’s weights follows internal coupled optimization processes that are difficult to explain and present to customers with little technical background in the field. To this end, significant effort has been made in order to establish and standardize explainability in deep learning (Linardatos et al., 2020a).
Alternatively, deep-learning models can be explainable with a change in the network’s structure, for instance by combining neural networks with continuous logic and multi-criteria decision-making tools (Csiszár et al., 2020) leading to the definition of Logical Neuronal Networks (LONNs). Recently, this methodology has been applied to recommender systems in medicine, providing the option to define the logical combination of a hierarchy of parameters (Ochoa et al., 2021). However, one limitation of this methodology is its inherent inflexibility, which could be responsible for the low performance of this modeling methodology (Wang, 2021). Medical customers desire control over the logical combinations, and the smaller and better-defined as well as more generalizable the network is, the easier it is to make it understandable to them, perhaps at the expense of precision.
An explainable model must also manage uncertainties in the data. The recording of health data is prone to uncertainties and errors, coming from the inherent biological variability (considering that every organism is exposed to an environment, implying the recording of data in non-controlled experimental conditions), to errors in the recording of diagnoses (which is about 63% in EHRs1), leading to a persistent epistemic uncertainty in the recorded data in EHRs, which is present in all biomedical research (Viale, 2021). This implies that models should be essentially non-deterministic and that the model must be stochastic, rather than flexible or “smart” in its architecture. Thus, an explainable model must be able to tell the customer how high its precision is by indicating the corresponding amount of uncertainty2. Explainable models are not only concerned with transparency of the structure and information flow, leading to a final prediction based on simple, generalizable models (Occam’s razor), but also imply the possibility of generating parallel models reflecting this uncertainty.
Now we combined LONNs with Bayesian Neural Networks (BNNs) (Lampinen and Vehtari, 2001) to create a new modeling methodology known as BaLONNs. To represent uncertainty and imprecision in real data, previous efforts have combined fuzzy logic with Bayesian Networks (Pan and Bester, 2018), but no implementation has been made in the context of deep learning.
We tested this novel approach for the prediction of the kind of heart failure (HF) and the expected therapy time (TL) of patients with diabetes, using a Pakistan Data Base from the UCI repository (Chicco and Jurman, 2020). Based on these results, we now aimed to develop not only an improved explainable model but also a human-centered application that informs the customer when the model is “unsure” about a given prediction.
This article is organized as follows. In the next section, we introduce the methodology and modeling strategy. Thereafter, we report testing the methodology and provide qualitative as well as validation results. Finally, we discuss the implications of the introduced methodology and provide an outlook on the next research steps.
2 Methodology
2.1 Data extraction, feature engineering and data balancing methods
This analysis uses data from diabetic patients, some of whom have heart failure (Pakistan Database, from the UCI repository3). The corresponding attributes are listed in Table 1, where V1 to V10 are the inputs, and O1, as well as O2, are the model targets. Observe that the parameter “Time” is a metric of the total time (in months) that the patient has been treated. In the recorded data we are not dealing with the variability of several measurements of a single parameter for one patient (aleatoric uncertainty), or the complete uncertainty about the internal processes of the system (ontological uncertainty), but with the implicit variations between patients contained in the data (epistemic uncertainty), which have different origins: from biological/physiological variability to systematic errors in the recording of the data.
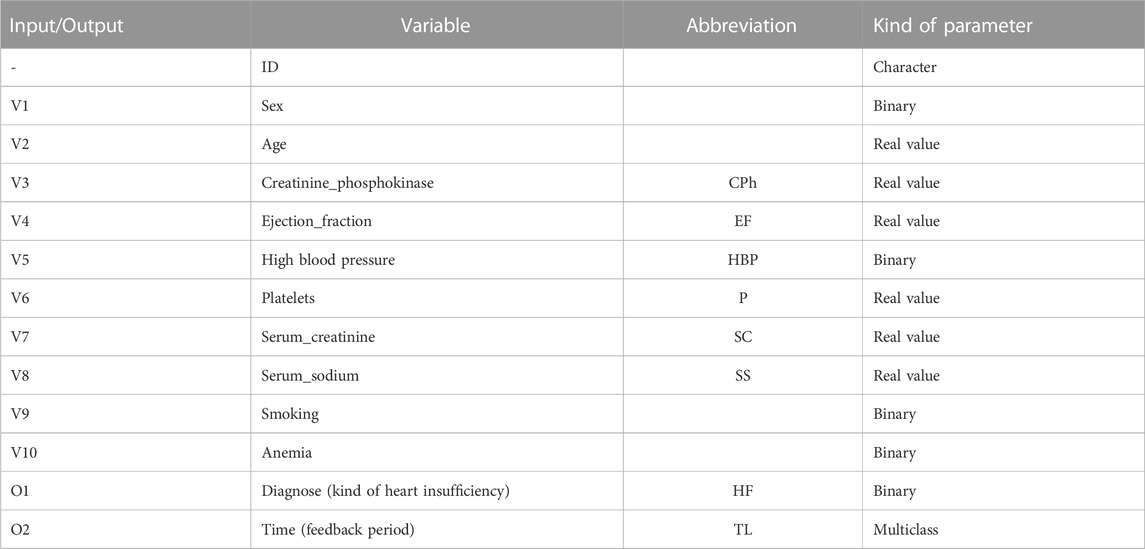
TABLE 1. Principal input and output parameters extracted from the HER of diabetic patients with heart insufficiency.
Since we required a large population, we synthesized additional patients from the original database. Personal information, like identification number (ID), age, and sex, was also correspondingly modeled. For the simulation of the distribution of diagnoses, we used the “synthpop” package4, basically using linear regression models for each parameter (Nowok et al., 2016).
From this data we can extract two main features.
• the kind of heart failure HF as a binary value representing patients with systolic heart failure (SHF, HF = 1) and heart failure with preserved ejection fraction (HFNEF, HF = 0)
• the therapy length TL, representing the time the patients are treated. In this last case, we transform the registered time
While the first parameter HF is related to the kind of therapy a patient becomes, the second one, TL, is related to the quality of this therapy, such that a low-quality therapy corresponds to TL = 0, a medium-quality therapy corresponds to TL = 1 or TL = 2, and a high-quality therapy corresponds to TL = 3. Therefore, this one is a problem with two different tasks (TL, HF) and can be defined as a Multitask Learning (MLP) problem, where multiple tasks are simultaneously learned by a shared model.
To solve this problem, we opted to implement the model as a regression algorithm. This seems a natural strategy because regression algorithms, by definition, have a notion of the relative distance of target values (Crawshaw, 2020).
Since these classes are essentially imbalanced, we require balancing methods to reduce bias in our modeling. To this end, we implemented Synthetic Minority Oversampling TEchnique (SMOTE) to both HF and TL to create an oversampling of less frequent values. Despite its limitations, we selected this method because, according to Blagus et al., it is beneficial for low-dimensional data (Blagus and Lusa, 2013). In Figure 1, we present the original data distribution of TL before and after data balancing with SMOTE.
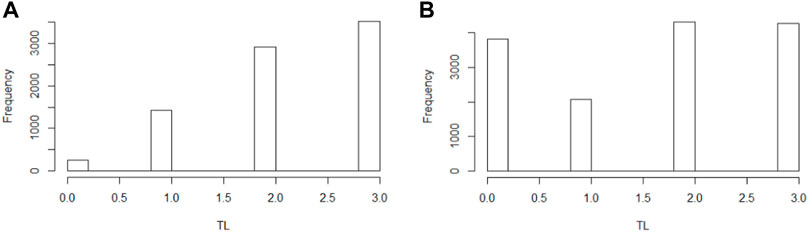
FIGURE 1. Distribution therapy length in the population in the original population (A) and the SMOTE balanced population (B).
80% of the data is used exclusively for model training and validation. The final 20% of the data is test data used to evaluate the quality of the model. For both model training and quality evaluation, we normalized the input data.
2.2 Baseline models
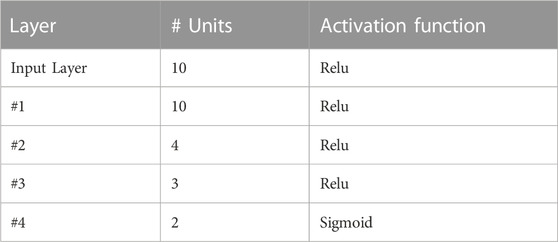
Our baseline model is essentially a deep-learning model with dense fully interconnected neuron layers implemented on TensorFlow.
The basic architecture of the baseline model is resumed in Table 2, which has been selected to compare its performance against the LONN architecture. Observe that in this model we have implemented rectified linear layers, using MSE (Mean Square Error) as a loss function. Recent investigations have demonstrated that rectified linear functions are the most effective in representing data processing in neural networks5, particularly for networks with many layers (Urenda, 2020). Additionally, the ordinal classification problem of the therapy length is, based on Kramer et al., handled as a regression problem with an additional post-processing step (Kramer et al., 2001).
2.3 Bayesian Neural Networks (BNN)
Often, errors occur in the way data is entered into EHRs. This is in part because the information in EHRs is partially manually curated, implying epistemic uncertainty in the stored data6.
To correctly model this uncertainty, we implement models that marginalize the distribution of parameters in order to make prediction7 by implementing the weights in the neuronal network as a distribution defined as a Gaussian process. In this way, a trained model is not the result of the optimization of single parameters, but the optimization of the statistical distribution of these parameters. The same network with finitely many weights is known as a Bayesian neural network8. To this end, we aim to minimize the evidence lower bound of the network weights, which is defined as9,10
where
Thus, the network will be trained such that
The implementation has been performed on TensorFlow in R using R-Studio. The final trained model is an object containing the training functions for the distributions in the statistical layers. These Bayes layers are then used to evaluate the effect of epistemic uncertainty in two models.
• BNN: Bayesian Neural Networks (stochastic baseline model).
• BaLONN: Bayesian LONN.
2.4 LONNs and bayesian layers
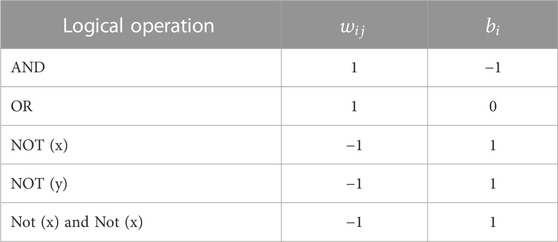
The application of LONNs for the evaluation of medical data has been described by Ochoa et al. (Ochoa et al., 2021), whereby single layers are replaced by frozen weights and bias representing logical operations. Here, a single Perceptron in the NN network is activated by so-called Squashing activation functions, a differentiable and parametric family of functions that satisfy natural invariance requirements and contain rectified linear units as a particular case (Urenda, 2020). These activation functions are in this framework defined as follows:
where
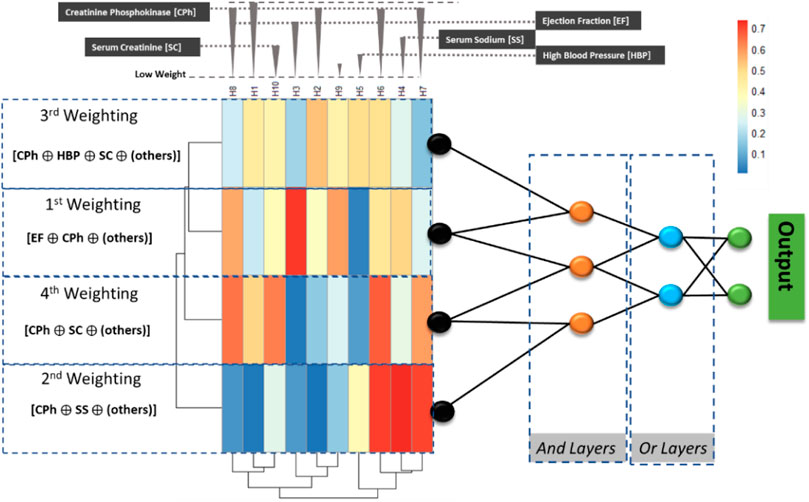
FIGURE 2. The implemented ProbLONNs contain distributed weights in the initial layer representing the weight distribution. The number of neurons in the hidden layers is defined according to the parameters presented in Table 2. In a multiclass problem, the implemented model tries to predict between, for instance, two classes based on the logical decision after combining parameters that have been identified by relevance depending on the weight estimated in the first model layers.
To visualize the model explainability, we exemplarily show the way how the LONN model performs a computation with the parameters listed in Table 1: Observe that the Creatine_Phosphokinase (CPh) has a high statistical weight in the model; thus, this parameter, combined with other parameters having also a high weight in the first layers, are combined in the logical gates to predict the two outcomes, HF and TL.
Thus, the baseline model is modified by freezing the weights and biases in the layers that are modeled as logical switches (see the parameters listed in Table 2). This definition implies that the number of trainable parameters for weight estimation gets reduced, also implying a reduction of the degrees of freedom of the model.
According to this, the following exemplary logical combination is performed using a LONN to predict Heart Failure (HF) and Therapy Length (TL) (abbreviations according to Figure 2; Table 1) [Creatin Phosphokinase, High blood pressure, Serum Creatinine, others] AND [Creatinine Phosphokinase, Ejection Fraction, others] OR [Creatin Phosphokinase, Serum Creatinine, others] AND [Creatinine Phosphokinase AND Ejection Fraction], where “others” refer to other parameters with a lower weight. Using logical notation, the logical combination of parameters can be described in the following way:
Observe that all the above-documented logic operators are fuzzy, i.e., logical operations are not exact but essentially fuzzy due to the implemented continuous-valued operators. In addition, because the logical layers are essentially frozen, there is little chance that the model will be overfitted if multiple layers are coupled into the model.
Our implemented Logic-Operator neural network (LONN) is thus a method simulating the cognitive logical thinking process (Figure 3).
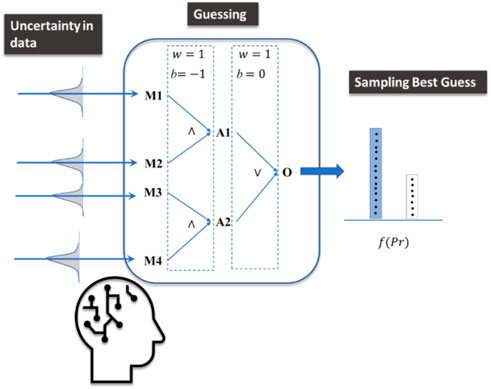
FIGURE 3. The implemented model mimics cognitive processes under uncertainty, where guesses are performed and finally sampled considering different options (outputs) to take a final decision. While a decision is made, other alternative answers are not fully discarded.
We simulate human thinking by introducing probabilistic layers (Sohn and Narain, 2021) which recognize not only Bayesian inference but also their inherent uncertainty, as well as the possibility of representing both uncertainty and inaccuracy (Pan and Bester, 2018). Therefore, the results of the model are not intended to present accurate solutions and results. Rather, these results represent both a plausible prediction of an outcome and its corresponding uncertainty.
By plotting this cognitive process, we are dealing not only with a single model prediction but with the sample of results provided by models with different weights provided by the Bayesian model (see Figure 4). Accordingly, the mathematical implication of combining LONNS with Bayesian networks is that the possible fuzzy logic combinations are not unique but distributed. In terms of the explainability of the model, this means that the fuzzy logic combinations provided (e.g., Figure 1 and Figure 2) are the mean of all averaged possible combinations identified by the model.
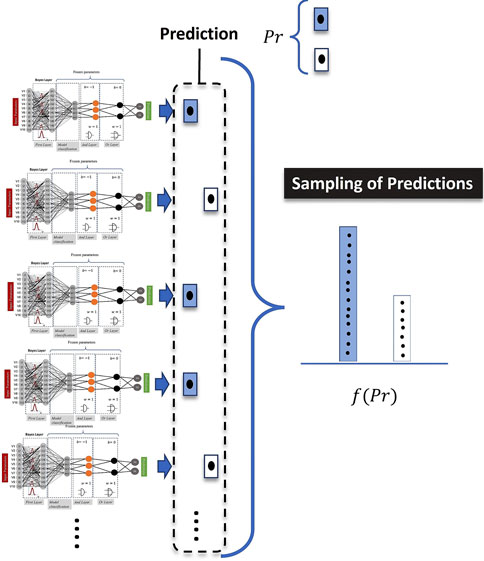
FIGURE 4. Intuitive meaning of the application of Bayes in the model definition. For the computation of a single prediction, the computed results are sampled.
3 Results and model validation with variability
For the model definition we performed a systematic evaluation of the following parameters.
• Normalization, for instance treatment times and other parameters.
• Meta parameter analysis.
o Dependency of the model on activation functions.
⁃ Dependency of model distributions on activations.
⁃ Dependence of model distributions on LONNs.
o Learning Rate—Adam.
o Number of neurons.
o Number of epochs.
• Architecture analysis—especially for LONNs.
• Statistics—distribution functions in the Bayesian strata—possibly new definition of the model.
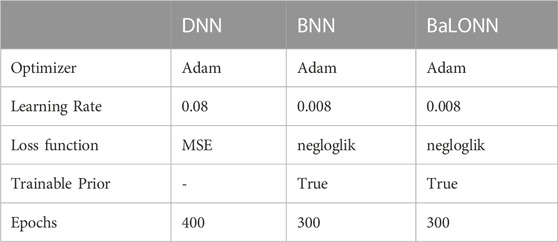
Furthermore, we performed a systematic analysis of the influence of the parameters in the Bayesian layers on the model precision (standard deviation in the prior and posterior standard deviations). Based on the previous definitions, we performed different computations using the meta-parameters for each model listed in Table 4 considering Deep Neural networks (DNN) and Bayes Neural Networks (BNN).
3.1 Evaluation metrics
The fact that we are dealing with uncertainties implies that the result is non-deterministic, i.e., the outputs can consist of a sample of several plausible outputs. For instance, for some patients, the evaluation of the expected therapy time can be a range (for instance, the expectation is that the patient will get a medium to long therapy time TL), and not an exact outcome (either a medium OR a long TL). In a real clinical environment, this ambivalent scenario is much more realistic than a pure deterministic one. For this reason, the validation must be performed using distributed outputs.
To compute the final validation and its corresponding statistics, we define the true prediction for each patient
In our validation, we opt to use micro averages14, i.e., averages biased by class frequency. To this end, we must count the number of true predictions obtained after sampling the outcomes from the statistical model. If the distance between the average and the target lies below a tolerance value, then this state will be considered as a true prediction
Since we are simultaneously dealing with a binary (HF) and a multiclass (TL)15 prediction, we require an adaption of the prediction
• For
• For
In a nutshell,
while the total error was estimated as:
3.2 Model performance
To test the correct functionality of the models, we perform a first inspection of the prediction’s distribution. For the baseline model (NNs), we employ the predicted values, while for the BNN, we compute the mean value from the sampled predictions. This first general result indicates, first, that the model has variability and, second, that it can reproduce the test data dynamics.
Furthermore, we analyze the predicted variability and check if it is generated by both the model structure and the information integration, and not by the stochastics. As a result of a first inspection, we discovered that the mean value distribution of the sampled predictions derived by BNNs is different from the target distribution (Figure 5), which samples the absolute values. As a result, the way in which the uncertainty of the outputs is modeled can affect the overall distribution of the prediction.
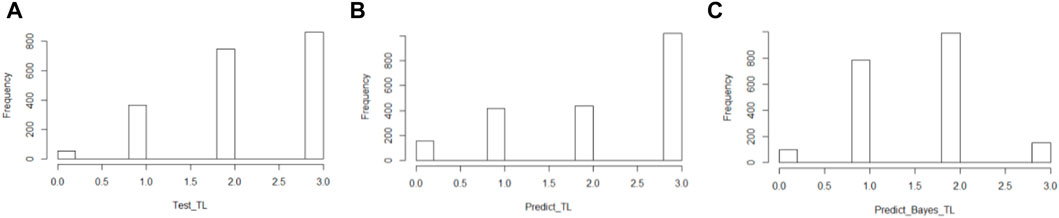
FIGURE 5. Distribution of the therapy length (TL) of the target data (A), the prediction computed with the baseline model (B), and the BNNs (C).
Our next step was to analyze the model performance by sampling different predictions for each patient. Before applying this concept to BaLONNs, we explored the performance of BNNs to better understand their behavior. It is necessary to carry out a detailed validation of the predictions, considering the possibility of ambiguous results, as shown in Figure 3. It is possible to get a short or middle expected TL for a single patient, but the distribution gives more weight to one of the prognoses, as shown in Figure 5. Therefore, the main expectation is a short TL, with a low chance of a middle TL. A boxplot can be used to represent the predicted outcomes of a patient population, as opposed to just a single prediction.
In Figure 6, we deploy this boxplot for a small fraction of the patient population and measure the distance to target values to validate the model. The color keys represent the quality of the validation. Green stands for a perfect validation, blue for a prediction where the target value lies inside the distribution of the predictions, and red for an incorrect prediction, where the target lies outside the distribution of the computed predictions.
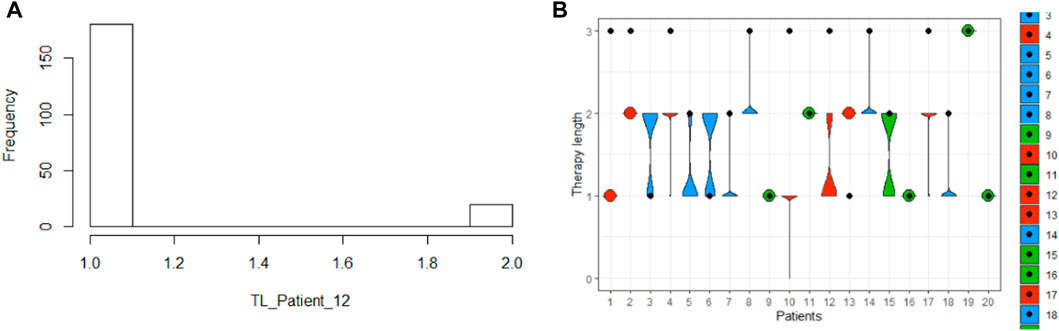
FIGURE 6. Precision of the prognosis of the therapy length for one patient with an ambiguous output (A), and for a patient cohort (20 patients) in the whole population with validation results: green is a perfect prognosis, blue is a by-prognosis that is still fulfilled inside the uncertainty of the prediction, and red is an off-prognosis. The black points are the targets.
The computation of the error considers the fact that both observables, therapy length and class of heart failure, are distributed as well. Finally, the results can be either represented using box plots or violin plots (Figure 7).
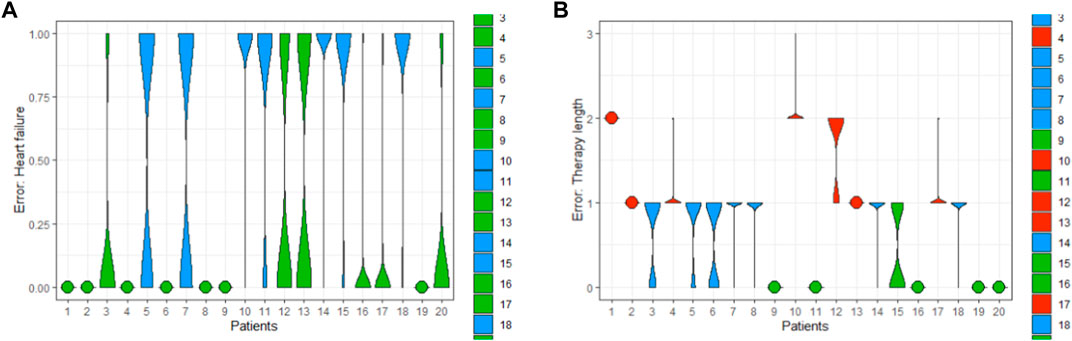
FIGURE 7. Exemplary error of the predictions of HF (A) and TL (B) computed for a patient cohort (20 patients).
These kinds of visualizations are useful ways to qualitatively understand how the implemented models are working.
• Green when a model is relatively confident,
• Blue when the model delivers a prognosis with high uncertainty,
• And red, when the uncertainty is extremely large.
Of course, this has an implication for the final validation: with this implementation, we were able to reduce the error to 24.48% and 21.24%, representing an improvement of about 3% with respect to pure deterministic models (total error of baseline model was 37.7%). But this error reduction has been obtained because we account predictions “in blue”, i.e., we are accepting off-predictions, where the targets lie inside the predicted distribution. Otherwise, the computed predictions of the BNNs only considering the true positives/negatives could deliver a much higher prediction error (see Figure 7).
3.3 Parameter analysis
To get a better insight into the performance of the model, we assessed the model sensitivity to the standard deviation of the prior,
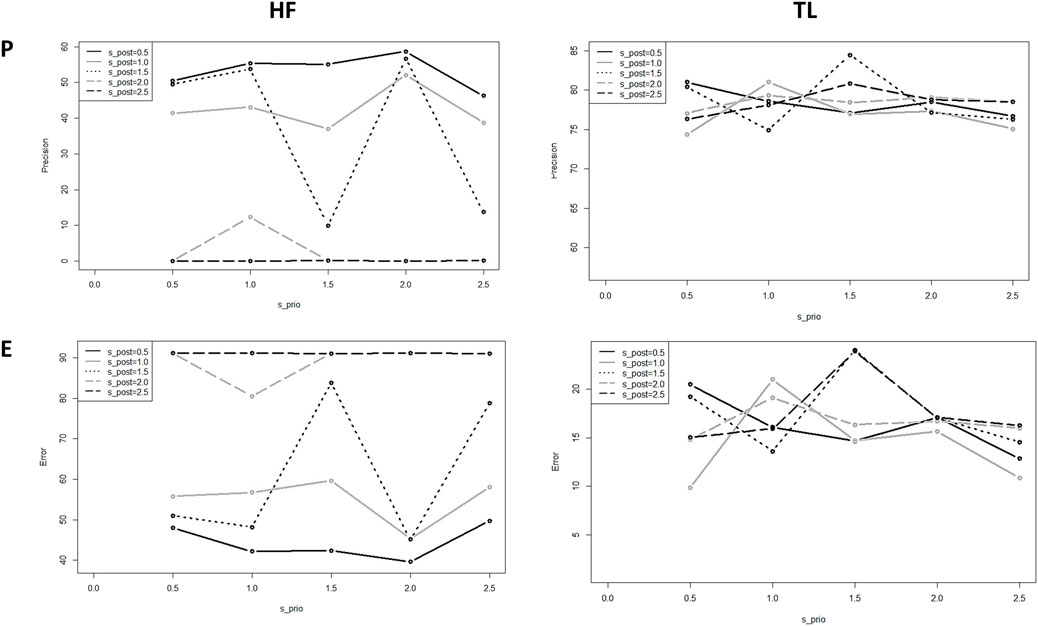
FIGURE 8. Precision and error of the predicted HF and TL using BNNs for different standard deviations;
In this test, we observe for almost all the values a high model sensitivity on the prior and posterior standard variations. Also, the precision obtained for HF is smaller than the precision obtained for TL, due that HF is a binary output and has fewer degrees of freedom than the multilabel output TL; we can understand the behavior of this state as a physical binary state that gets polarized beyond a critical value in the fluctuations of the system, represented by
Since the standard deviation influences the distribution of the weights in the model, it is to assume that this definition must reflect the distribution of the uncertainty in the training dataset. Otherwise, the model follows its own dynamics, deteriorating its ability to fit experimental targets.
From these results, we conclude that one plausible combination is
When we tested the model sensitivity for the BaLONNs, we observed that there is a lower fluctuation of the precision/error values for

FIGURE 9. Computed precision of the BaLONNs for HF (A) and TL (B) and different standard deviations;
We obtain acceptable validations for
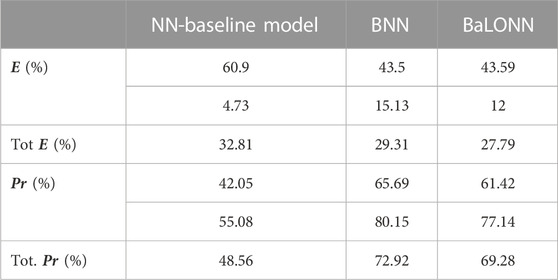
TABLE 5. Validation results for the baseline model, BNNs and BaLONNs. For the stochastic models, we have averaged over 1,000 different models.
The modeling of epistemic uncertainty increases the precision of the modeling, simply because we are accepting ambiguous results as true predictions inside the tolerance range. In contrast, the base model is trying to make an exact and predictive prediction based on the training data. This effect reflects the fact that the inherent stochastics play a relevant role when a prediction is computed.
Furthermore, we observed that the validation of HF using BaLONNs does not get the same quality as a fully trainable model, despite the mean error lying below the mean error of BNNs. Since the logic gates are frozen/non-trainable parameters, the whole model has fewer degrees of freedom, limiting the possibility that the model converges to the target values. In this case, we face again the typical tradeoff problem: either to accept dealing with interpretable models with less accuracy or to have an accurate model with less interpretability.
We have also observed that while the precision of HF gets increased by adjusting the model’s hyperparameters, the TL’s precision decreases. The integration of these parameters in a single model is to some degree problematic, firstly considering that both parameters have a different number of states, and secondly, because their coupling is weak, i.e., TL depends on HF as well as additional parameters that are not integrated into the model. This was in particular evident in the NN-baseline model. Despite this, we could find a reasonable tradeoff in the parameter selection to deliver acceptable accuracy for both parameters.
4 Discussion
The definition of explainability usually focuses on methods to make the outcomes from black-box models, like DNNs, interpretable. Lime and SHAP, for example, use local explainability to build surrogate models for black box machine learning models to provide them with interpretability17. In our approach, we have opted for a different strategy by implementing nodes in the DNN model that can be defined as logical operators, LONN, which are interpretable. By doing this, we set up a hierarchy of parameters in the input layers that can then be logically combined, without requiring additional surrogate models.
In a nutshell, the concept of explainability in AI requires a particular taxonomy.
i. Computational Explainability: AI-explainability on a computational level refers to the correlation between model outputs and inputs, i.e., the evaluation of the plausibility of model predictions in the context of the inputs (Linardatos et al., 2020b).
Similarly, the Shapley index, a concept borrowed from the Game Theory, evaluates how individual input features have a marginal contribution (in game theory, how much individual features “cooperate” to get a final output18) on the final mode output, a concept frequently used in machine learning.
ii. Instances of Explainability: Additionally, Bayesian-NNs19 are applied to analyze instances of explainability, i.e., to account uncertainties in predictions.
iii. Structural Explainability: Finally, explainability can be also understood in terms of what currently the model is computing, i.e., by understating the internal processes in the model’s architecture, and how the model automatically generates a hierarchy of input parameters, a concept that has been already developed for deep neural networks (LoNNs—cite first article)
Clearly, our implementation belongs to the third class of explainability, where we are trying to gain more insight into how the computing process takes place.
However, the problem of structural explainability does not only revolve around how information is integrated and how the corresponding outputs are computed based on the interconnectedness of the inputs. It also concerns the implicit handling of uncertainty in the data. This factor is particularly relevant in the medical field, where biological variability has an influence on the development of a disease. Thus, while for one patient a specific diagnosis or outcome can clearly be established after therapy, for another patient there may be variability that cannot simply be ignored and that affects both the diagnosis and the assessment of the outcome of therapy. Therefore, interpretability must consider not only the information flow and output computation in a model but also the fact that in certain cases it is not possible to estimate an exact value. As a result, models taking epistemic uncertainty and explainability into consideration, such as our BaLONNs, aim to continuously inform the customer when the model cannot behave deterministically and when the prediction it makes is uncertain.
We believe that the inclusion of this kind of variability in assistant systems, like recommender or expert systems in medicine, is an important step, also in the design of human-centered solutions. Several studies have shown that trusting digital systems beyond their capacity and functionality can present high actual costs, as well as more nuanced effects of compromising organizational integrity and personal security (Hardré et al., 2016). This is, in particular, relevant in the medical field, where the pressure in daily business might lead to strongly relying on automatic systems (Goddard et al., 2012), which, despite being well-validated, could lead to wrong decisions when customers assume that the outputs are precise when in reality are not.
Our novel approach is essentially an integration of LONNs with probabilistic layers. Our preliminary results have demonstrated that this approach can fulfill its goal: we are able to get acceptable validation values as well as acceptable precision in the prediction of the two parameters used in this study, namely, the prediction of the kind of heart insufficiency (HF) and the expected therapy time of the patients (TL). However, the precision of the model lies below a conventional deep learning model (which can be much more precise if we increase the number of layers). As we have found in a previous study, explainability implies a tradeoff between model performance and precision: while explainable models are often small and constrained to few elements to keep them explainable, the expected precision is in this case significantly lower than for classical black-box models20. The customer must decide at the end how much precision she wants to sacrifice in exchange for a simple model.
The potential next step in this work is to introduce a level of stochasticity not only in the extreme layers but also in the logical switches, as well as in the number of these switches. In this way, we generate different explainable models, assuming that not only one but a family of explainable models is able to model the data. An additional analysis, not performed in this study, is the relation between stochasticity and minority oversampling using SMOTE, i.e., if by implementing SMOTE the underlying epistemic uncertainty of the training datasets gets distorted. Finally, the handling of stochasticity could be computationally intensive when large datasets are analyzed; perhaps alternative methods, like quantum computing, could be helpful to generate more efficient stochastic BaLONN models from large datasets.
5 Conclusion
In this work, we presented a novel modeling technique that combines a structural explainable model architectures based on logic neural networks (LONNs) and Bayesian methods in a single BaLONN model. In this way, we improve user-centered solutions that inform users when they are uncertain about a prediction, in this case, the prediction of therapy based on physiological parameters. Unlike other solutions, this approach does not nudge customers to accept the model’s predictions. While this solution does not present an answer to well-founded critics against AI as technology, for instance as a surveillance tool (Fulterer, 2022), it is at least a way to compensate for well-known deficits in the implementation of this technology, making it user-centered (in our case for physicians) by deploying results that can be distrusted by the user. By doing so, we can avoid blindly relying on models to deliver high-quality results21.
We demonstrated that our model reaches a precision of 69%, considering that some of the true predictions are ambiguous but lie in the tolerance range of acceptability. This precision lies below the 70% precision of Bayesian neural networks. However, we think that the slight reduction in precision is an acceptable tradeoff considering that the architecture of the NN is composed of a few neurons and that some of these neurons are non-trainable.
This result is thus a relevant basis for the development of assistant and expert methods, for instance, recommender systems, in critical fields like medicine where the customer’s work should not be fully automated, and his expertise is continuously required.
Data availability statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author.
Author contributions
OC and JGDO conceived the initial idea. OC, LM, and JGDO developed the idea and designed the first model prototype. JGDO and LM developed the prototypes, wrote the programs and notebooks, and performed the computations. LM implemented the loop computation for the analysis of the model sensitivity. JGDO wrote the first article draft. OC, LM, and JGDO contributed to the final version of the article. All the authors contributed to the final version of the article. We also acknowledge Felix Weil for his constant support to this work.
Funding
The project no. 2019-2.1.11-TÉT-2020-00217 has been implemented with the support provided by the National Research, Development and Innovation Fund of Hungary, financed under the 2019-2.1.11-TÉT-2020-00217 funding scheme. The article processing charge was funded by the Baden-Württemberg Ministry of Science, Research and Culture and Aalen University of Applied Sciences in the funding program Open Access Publishing.
Acknowledgments
We want to thank Martin Grundman and Thomas Schimper for their ideas and critical feedback in the development of these concepts, as well as Hans Stettmeier for his constant support. JGDO is also grateful to with Anna Nitschke for her feedback regarding the explainability taxonomy.
Conflict of interest
Authors JGDO and LM were employed by the company PERMEDIQ GmbH.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
EHR; Electronic Health Record, NN; Neural Network, DNN; Deep Neural Network, BNN; Bayes Neural Network, LONN; Logic Neural network, BaLONN; Bayesian logical Neural Network, BNN; Bayesian Neural Network, HF; Heart Failure, TL; Therapy Length.
Footnotes
1https://healthinfoservice.com/most-common-icd-10-error-codes/
2https://www.heise.de/hintergrund/Wie-eingebautes-Misstrauen-KI-Systeme-sicherer-machen-kann-6049154.html?wt_mc=rss.red.ho.ho.atom.beitrag.beitrag
3The data has been obtained from the UCI repository: https://archive.ics.uci.edu/ml/datasets/Heart+failure+clinical+records
4https://www.r-bloggers.com/generating-synthetic-data-sets-with-synthpop-in-r/
5https://scholarworks.utep.edu/cgi/viewcontent.cgi?article=2170&context=cs_techrep
6In case of evaluation of time series, for instance in ECGs, we expect to find aleatoric uncertainty
7https://cedar.buffalo.edu/∼srihari/CSE574/Chap5/Chap5.7-BayesianNeuralNetworks.pdf
8https://blogs.rstudio.com/ai/posts/2019-06-05-uncertainty-estimates-tfprobability/
9https://en.wikipedia.org/wiki/Evidence_lower_bound
10https://xyang35.github.io/2017/04/14/variational-lower-bound/
11https://blogs.rstudio.com/ai/posts/2019-11-07-tfp-cran/
12https://blogs.rstudio.com/ai/posts/2019-06-05-uncertainty-estimates-tfprobability/
13https://www.mathworks.com/help/stats/prob.normaldistribution.negloglik.html
14https://stats.stackexchange.com/questions/156923/should-i-make-decisions-based-on-micro-averaged-or-macro-averaged-evaluation-mea
15In this work we are dealing with both a multiclass and a multilabel model: with the single model outputs, we are dealing with a multiclass classification, while after sampling all the outputs we are dealing with a multilabel classification.
16This observation resembles a phase transition, where
17https://towardsdatascience.com/idea-behind-lime-and-shap-b603d35d34eb
18https://towardsdatascience.com/the-shapley-value-for-ml-models-f1100bff78d1
19https://towardsdatascience.com/bayesian-neural-network-7041dd09f2cc
20https://www.interpretable.ai/interpretability/what/
21This corresponds to a kind of experimenter bias, where model expectations supported by validated models can distort the real interpretation of the model’s output.
References
Blagus, R., and Lusa, L. (2013). SMOTE for high-dimensional class-imbalanced data. BMC Bioinforma. 14 (1), 106. doi:10.1186/1471-2105-14-106
Chicco, D., and Jurman, G. (2020). Machine learning can predict survival of patients with heart failure from serum creatinine and ejection fraction alone. BMC Med. Inf. Decis. Mak. 20 (1), 16. doi:10.1186/s12911-020-1023-5
Crawshaw, M. (2020). Multi-task learning with deep neural networks: A survey. ArXiv200909796. Available: http://arxiv.org/abs/2009.09796.
Csiszár, O., Csiszár, G., and Dombi, J. (2020). Interpretable neural networks based on continuous-valued logic and multicriteria decision operators. Knowl. Based Syst. 199, 1059722020. doi:10.1016/j.knosys.2020.105972
Fulterer, R. (2022). Ex-googlerin whittaker: «KI nur durch massenüberwachung möglich. Neue Zürcher Ztg. Available: https://www.nzz.ch/technologie/ki-kommt-direkt-aus-dem-ueberwachungsmonopol-der-tech-firmen-ld.1700728.
Goddard, K., Roudsari, A., and Wyatt, J. C. (2012). Automation bias: A systematic review of frequency, effect mediators, and mitigators. J. Am. Med. Inf. Assoc. JAMIA 19 (1), 121–127. doi:10.1136/amiajnl-2011-000089
Hall, A., and Walton, G. (2004). Information overload within the health care system: A literature review. Health Inf. Libr. J. 21 (2), 102–108. doi:10.1111/j.1471-1842.2004.00506.x
Hardré, P. L. (2016). “Chapter 5 - when, how, and why do we trust technology too much?,” in Emotions, technology, and behaviors. Editors S. Y. Tettegah, and D. L. Espelage (San Diego: Academic Press), 85–106. doi:10.1016/B978-0-12-801873-6.00005-4
Kingma, D. P., and Ba, J. (2017). Adam: A method for stochastic optimization. ArXiv14126980 Cs. Available: http://arxiv.org/abs/1412.6980.
Kramer, S., Widmer, G., Pfahringer, B., and Groeve, M. (2001), Prediction of ordinal classes using regression trees. Fundam. Inf. 47, 45. doi:10.1007/3-540-39963-1_45
Lampinen, J., and Vehtari, A. (2001). Bayesian approach for neural networks--review and case studies. Neural Netw. Off. J. Int. Neural Netw. Soc. 14 (3), 257–274. doi:10.1016/s0893-6080(00)00098-8
Linardatos, P., Papastefanopoulos, V., Kotsiantis, S., and Explainable, A. I. (2020). Explainable AI: A review of machine learning interpretability methods. Entropy Basel Switz. 23 (1), E18. doi:10.3390/e23010018
Linardatos, P., Papastefanopoulos, V., Kotsiantis, S., and Explainable, A. I. (2020). Explainable AI: A review of machine learning interpretability methods. Entropy Basel Switz. 23 (1), E18. doi:10.3390/e23010018
Nowok, B., Raab, G. M., and Dibben, C. (2016). synthpop: Bespoke creation of synthetic data in R. J. Stat. Softw. 74 (1), 11. doi:10.18637/jss.v074.i11
Ochoa, J. G. D., Csiszár, O., and Schimper, T. (2021). Medical recommender systems based on continuous-valued logic and multi-criteria decision operators, using interpretable neural networks. BMC Med. Inf. Decis. Mak. 21 (1), 186. doi:10.1186/s12911-021-01553-3
Rajkomar, A., Oren, E., Chen, K., Dai, A. M., Hajaj, N., Hardt, M., et al. (2018). Scalable and accurate deep learning with electronic health records. Npj Digit. Med. 1 (1), 18–10. doi:10.1038/s41746-018-0029-1
Sandell, H. S., and Bourne, J. R. (1985). Expert systems in medicine: A biomedical engineering perspective. Crit. Rev. Biomed. Eng. 12 (2), 95–129.
Sohn, H., and Narain, D. (2021). Neural implementations of Bayesian inference. Curr. Opin. Neurobiol. 70, 121–129. doi:10.1016/j.conb.2021.09.008
Urenda, J. (2020). Why squashing functions in multi-layer neural networks. Dep. Tech. Rep. Available: https://scholarworks.utep.edu/cs_techrep/1398.
Viale, R. (2021). The epistemic uncertainty of COVID-19: Failures and successes of heuristics in clinical decision-making. Mind Soc. 20 (1), 149–154. doi:10.1007/s11299-020-00262-0
Wang, G. (2021). A logical neural network structure with more direct mapping from logical relations. ArXiv210611463. Available: http://arxiv.org/abs/2106.11463.
Keywords: explainable AI, electronic health records, epistemic uncertainty, logical neural networks, bayes neural networks
Citation: Diaz Ochoa JG, Maier L and Csiszar O (2023) Bayesian logical neural networks for human-centered applications in medicine. Front. Bioinform. 3:1082941. doi: 10.3389/fbinf.2023.1082941
Received: 28 October 2022; Accepted: 01 February 2023;
Published: 15 February 2023.
Edited by:
Ruichu Cai, Guangdong University of Technology, ChinaCopyright © 2023 Diaz Ochoa, Maier and Csiszar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Orsolya Csiszar, b3Jzb2x5YS5jc2lzemFyQGhzLWFhbGVuLmRl
 Juan G. Diaz Ochoa
Juan G. Diaz Ochoa Lukas Maier1
Lukas Maier1 Orsolya Csiszar
Orsolya Csiszar