
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Audiol. Otol. , 07 February 2025
Sec. Tinnitus
Volume 3 - 2025 | https://doi.org/10.3389/fauot.2025.1509444
Purpose: The primary objective of this study was to investigate the prevalence and characteristics of tinnitus related to COVID-19 vaccination. Specifically, we aimed to assess the impact of COVID-19 vaccination on the onset and severity of tinnitus, including changes in loudness, pitch, anxiety, and speech perception. Additionally, we sought to identify potential risk factors associated with new-onset tinnitus and the exacerbation of pre-existing symptoms.
Design: A comprehensive survey was administered to 372 individuals who reported new-onset tinnitus or worsening of pre-existing tinnitus following COVID-19 vaccination. Data on tinnitus characteristics before and after COVID-19 vaccination were collected. The survey documented pre-existing medical conditions, and changes in tinnitus loudness, pitch, and related anxiety. Respondents were divided into two groups: those with pre-existing tinnitus and those with new-onset tinnitus following vaccination. Statistical analyses were conducted to compare changes across these groups and to explore associations with vaccine type (mRNA vs. non-mRNA) and pre-existing medical conditions.
Results: Of the respondents, 53% with pre-existing tinnitus reported worsened symptoms following vaccination, with significant increases in loudness, pitch, and anxiety. Additionally, 47% of respondents developed new-onset tinnitus, with this group reporting higher severity and anxiety levels compared to those with pre-existing tinnitus. There was no significant difference in tinnitus onset latency between mRNA vaccines (Pfizer and Moderna) and non-mRNA vaccines (Johnson & Johnson). Pandemic-related anxiety was identified as a contributing factor to the exacerbation of tinnitus symptoms.
Conclusions: The results indicate that COVID-19 vaccination is associated with an increased risk of both new-onset tinnitus and worsening pre-existing tinnitus. Significant increases in tinnitus loudness, pitch, and anxiety post-vaccination, along with challenges in speech perception, emphasize the need for further research into the auditory effects of COVID-19 vaccination. Identifying risk factors, such as underlying health conditions and psychological stress, will be crucial in developing strategies for the management and treatment of tinnitus in vaccinated individuals.
The COVID-19 pandemic has led to a wide range of health complications, extending beyond respiratory illness to include neurological, cardiovascular, and auditory symptoms. Among these, tinnitus—a condition characterized by the perception of ringing or buzzing in the ears without an external source—has emerged as a significant concern. As cases of COVID-19 soared globally, so did reports of tinnitus, either as a new onset or as a worsening of pre-existing symptoms. Understanding the prevalence and characteristics of tinnitus during the pandemic is critical to addressing its physical and psychological impact (Beukes et al., 2021).
Various studies have reported tinnitus as a prominent side effect within the field of otolaryngology following COVID-19 infection (Colizza et al., 2022; Jafari et al., 2022; Leong et al., 2023; Ong and Cruz, 2022) and vaccination (Finsterer and Edmonds, 2022; Medina and Gómez, 2022; Dorney et al., 2023). In the early stages of the pandemic, tinnitus emerged as one of the initial indicators of COVID-19 (Liang et al., 2020). Subsequent case reports (Daher et al., 2022; Narozny et al., 2021) and comprehensive studies further indicated its frequent occurrence among affected patients (Munro et al., 2020; Narozny et al., 2021). These reports are further supported by studies demonstrating that a significant proportion of COVID-19 patients experienced either the worsening of pre-existing tinnitus or the development of new-onset tinnitus symptoms during the pandemic. For instance, Beukes et al. (2021) found that nearly 40–50% of individuals with COVID-19 experienced worsened tinnitus or developed new-onset symptoms.
Additionally, a global study conducted by Feng et al. (2023) involving over 3,100 patients from 48 countries reported that tinnitus became a widespread issue, potentially linked to COVID-19 and the stress and anxiety associated with the pandemic. Stress and anxiety are well-documented contributors to the onset and severity of tinnitus, further underscoring the need to study tinnitus in the context of COVID-19 (Liang et al., 2020). Potential factors contributing to tinnitus in COVID-19 patients include direct impact on the auditory system, inflammation within the inner ear, immune responses triggered by the virus (Liang et al., 2020), and systemic illness effects (Wang et al., 2024). These findings highlight the multifaceted nature of tinnitus during the pandemic, as patients with long COVID frequently exhibit neurological manifestations such as tinnitus, vertigo, and dizziness (Degen et al., 2022).
Building upon these findings, this study was designed to assess the prevalence and impact of COVID-19 infection and vaccination on tinnitus, focusing on several key areas. One primary goal was to determine whether COVID-19 vaccination exacerbates symptoms in individuals with pre-existing tinnitus (Yellamsetty and Gonzalez, 2023; Wang et al., 2024), and whether the vaccines might trigger the new onset of tinnitus in those previously unaffected. In addition, the study aimed to evaluate perceptual changes in tinnitus, such as variations in pitch, loudness, and annoyance. Furthermore, the study also explored the psychological effects of the pandemic, particularly anxiety, and how these emotional factors influenced tinnitus perception. By examining the rate and distribution of tinnitus cases across different vaccine manufacturers, gender differences across age groups, tinnitus onset latency post-vaccination, and the effects of medication and health conditions, this study offers a comprehensive understanding of the factors influencing tinnitus following COIVD-19 vaccination. These findings are expected to guide healthcare professionals in developing more effective treatment protocols for managing auditory health issues linked to COVID-19 and vaccination.
A detailed questionnaire was developed to gather comprehensive information on participants' demographics, medical history, and tinnitus-related experiences before and after receiving the COVID-19 vaccine. The survey consisted of several sections, including demographic data, vaccine details (type of vaccine, dosage, and booster information), medical history (including pre-existing conditions), audiological evaluations, and tinnitus characteristics that are self-reported. The survey included questions adapted from standardized instruments, such as the Tinnitus Handicap Inventory (THI) and the Tinnitus Reaction Questionnaire (TRQ), to assess tinnitus severity. Respondents were asked to rate their tinnitus symptoms in terms of severity, pitch, loudness, and annoyance and to report changes in tinnitus before and after COVID-19 infection and vaccination.
Data were collected through an online survey conducted at San José State University between December 2022 and July 2023. The Institutional Review Board (IRB) at San José State University approved the study to ensure compliance with ethical guidelines. Informed consent was obtained electronically from all participants, who were assured of their anonymity and confidentiality throughout the study. Participants were pre-screened based on their vaccination status and whether they experienced new or worsening tinnitus following vaccination.
The survey also included questions on the type of vaccine administered (Pfizer, Moderna, Johnson & Johnson), the number of doses/boosters received (here, a booster refers to a dose received after full vaccination), and any changes in tinnitus symptoms after each dose or booster. Additionally, participants provided information about pre-existing medical conditions, noise exposure history, and any attempted treatments for tinnitus. The data collected provided a comprehensive overview of tinnitus symptoms, including the onset or exacerbation of tinnitus post-vaccination and the potential role of pre-existing medical conditions.
Open-ended responses describing participants' tinnitus were analyzed using advanced text mining and topic modeling techniques. Text mining allows for processing large amounts of text to uncover notable patterns in word usage and linguistic structure (Das et al., 2016). Topic modeling, specifically Latent Dirichlet Allocation (LDA), was employed to extract recurring themes or word groupings from the data, functioning as a tool for semantic analysis (Liu et al., 2016). Following the approach outlined by Etu et al. (2023), the topic modeling process involved defining the number of topics, preprocessing the data (such as removing stop words), and iteratively refining the model to improve the coherence of the topics. To ensure the validity of the identified topics, we conducted internal consistency checks and sought feedback from audiology experts to confirm that the extracted themes were clinically relevant and aligned with professional insights. This approach allowed for the identification of recurring themes and patterns in the textual data, with key topics related to tinnitus characteristics emerging from the analysis. The textual responses were categorized into distinct topics, reflecting the diversity of tinnitus experiences, including descriptions of high-pitched ringing, buzzing, cricket-like sounds, and unilateral tinnitus.
Quantitative data were analyzed using pairwise correlation analyses to assess the relationships between age, gender, history of medical conditions, vaccine type, and tinnitus severity. Statistical significance was determined using Spearman correlation coefficients, with p-values indicating the strength of associations between variables. The analysis also examined whether specific vaccine types or doses were linked to changes in tinnitus severity and the impact of noise exposure on post-vaccine tinnitus symptoms.
A total of 426 responses were collected through the survey, of which 46 respondents did not complete the survey, leaving 380 fully completed responses. After data cleaning, which involved removing four duplicate and four inaccurate responses, 372 responses were retained for analysis. The average age of participants was 54.7 years (SD = 14.4). The gender distribution included 187 females, 181 males, and four identifying as “Other.” In terms of ethnicity, 291 respondents identified as European American, 30 as Hispanic/Latino, six as Black/African American, six as American Indian/Alaskan Native, eight as Middle Eastern, 11 as South Asian, seven as East Asian, 11 as “Other,” and two did not respond. Of the 372 respondents, 48 reported having contracted COVID-19, with only one individual requiring hospitalization.
Figure 1 illustrates the geographical distribution of participants in the study, providing an overview of the specific regions and cities from which data were collected. The map highlights key clusters of participants across different areas, including major metropolitan cities such as San Francisco, Los Angeles, and New York, as well as more rural and suburban regions. This visualization offers insight into the diverse geographic locations of the respondents within the United States of America (USA), ensuring a comprehensive representation of the study's urban and rural populations. Additionally, 53 respondents indicated their location as outside the USA; while these locations are not displayed on the map, they were included in the overall data analysis.
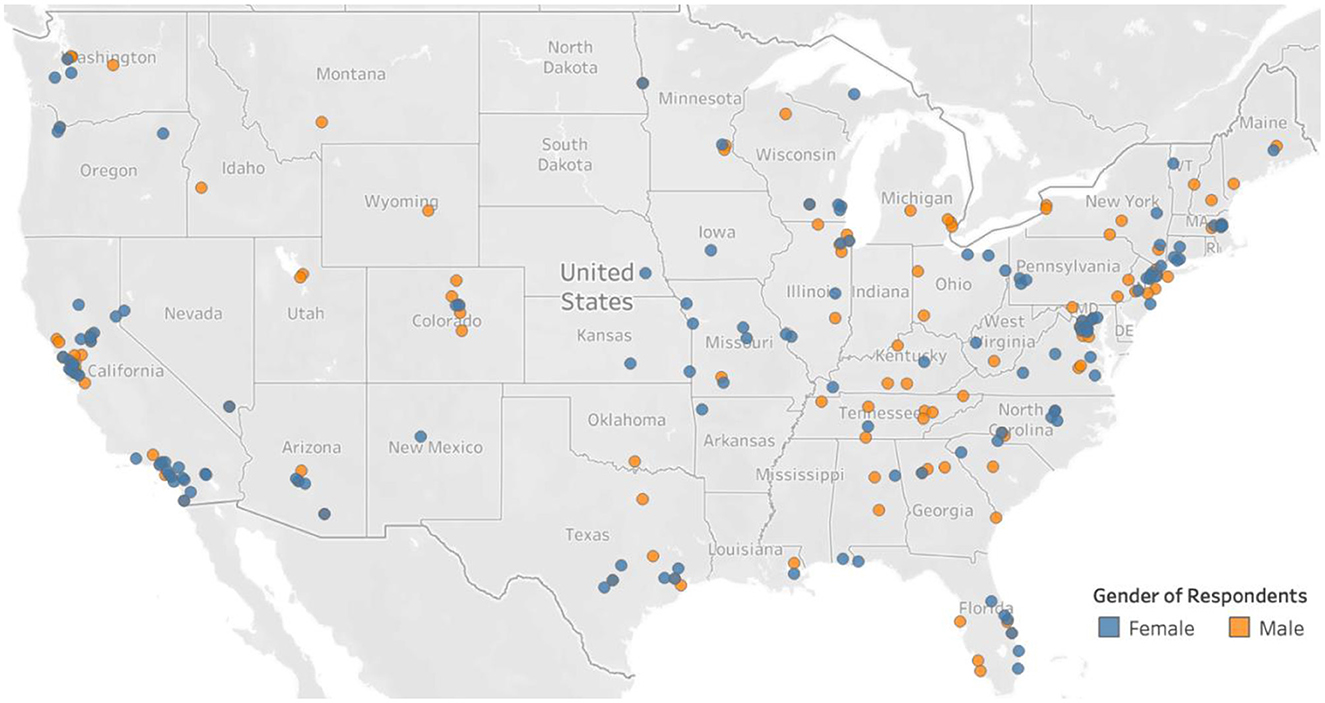
Figure 1. Respondent location across the United States. Fifty-three responses were from other countries and are not shown on the map.
The distribution of tinnitus cases across vaccine manufacturers shows that Pfizer had the highest number of reported cases (203 total, 161 U.S.), followed by Moderna (136 total, 131 U.S.), with Johnson & Johnson accounting for the fewest cases (33 total, 27 U.S.; Table 1). These differences could be because more Pfizer vaccines were distributed to the public than Moderna and Johnson & Johnson vaccines.
Tinnitus cases were most prevalent in the older age groups, particularly among participants aged 51–64 and 65+, with the highest incidence seen in females in the 51–64 group (71 cases) and males in the 65+ group (56 cases; Table 2). Younger age groups (18–34 and 35–50) reported fewer cases overall, with a more balanced distribution between males and females (z = −0.87, p > 0.05).
Table 3 shows the total number of doses of vaccines received by our survey respondents separated by age groups. A majority of the respondents received two doses, and many also took two boosters. These results indicate that the vaccines were generally well received by the survey respondents despite the vaccine-related tinnitus and tinnitus exacerbation.
Figure 2 illustrates the incidence of tinnitus symptoms (either onset or worsening) following COVID-19 vaccination among the 372 survey respondents. Of the 197 (53%) individuals with pre-existing tinnitus, 37 (19%) reported worsened symptoms after the first dose, 37 (19%) after the second dose, 41 (21%) after the first booster, and smaller percentages after subsequent boosters. A proportion test found no significant difference in the rates of worsened tinnitus between the first and second doses (z = 0, p > 0.05). Among the 175 individuals without prior tinnitus, onset was most frequently reported after the second dose (51 cases, 29.1%) and the first dose (47 cases, 26.9%), with no significant difference in onset rates between the two doses (z = −0.43, p > 0.05). A chi-square test confirmed a significant difference in the distribution of tinnitus cases across vaccination stages (χ2 = 74.10, p < 0.001). The difference in our results compared to the earlier report by Wang et al. (2024) may be due to variations in sample characteristics and population. In the previous study, data were collected from Facebook groups formed during the pandemic, where the severity of tinnitus-related issues and the motivation to join these support groups may have been higher. In contrast, the current dataset includes individuals from general platforms and tinnitus-specific groups, resulting in a more diverse representation.
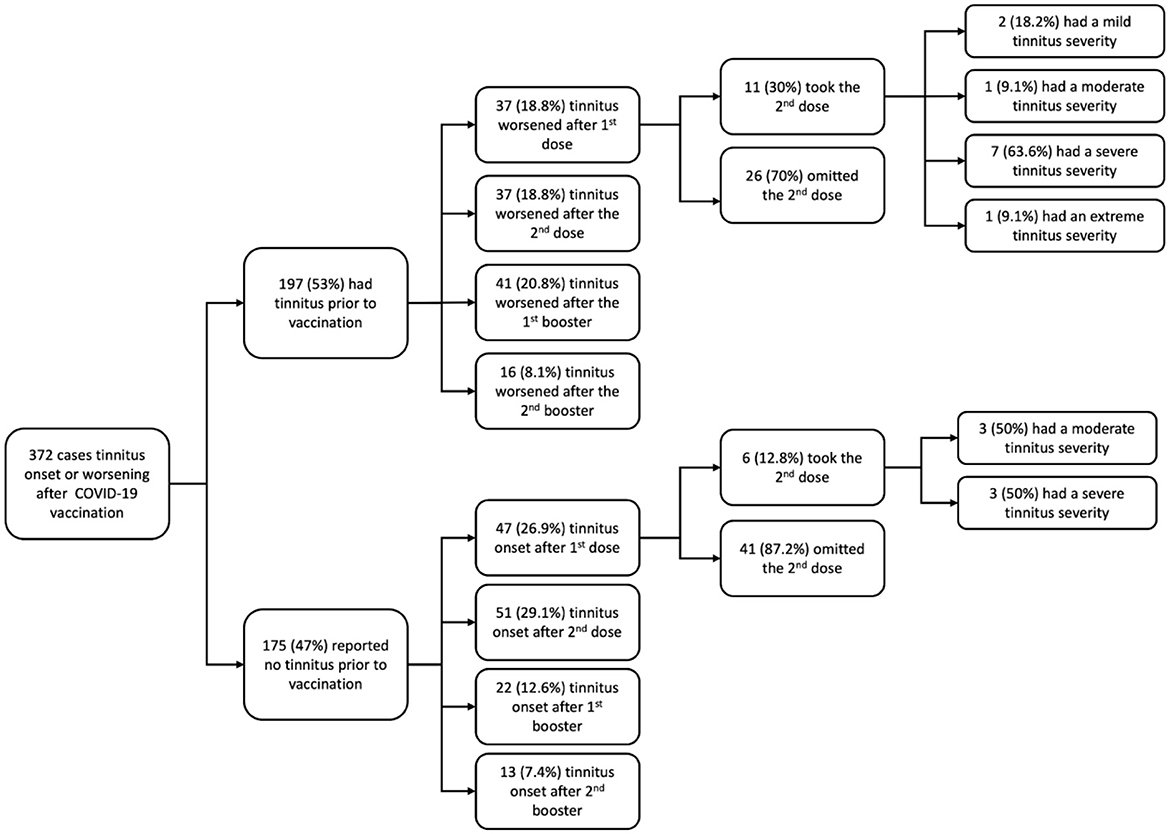
Figure 2. Showing the survey response breakdown, tinnitus onset, and worsening following COVID-19 vaccination: this figure shows the distribution of tinnitus onset and worsening among 372 respondents after receiving COVID-19 vaccines. Of the 197 respondents with pre-existing tinnitus, a significant proportion experienced worsening symptoms after the first and second doses, while 175 respondents without prior tinnitus reported onset after the second dose. A chi-square test revealed a significant variation in tinnitus occurrence across vaccination stages (χ2 = 74.10, p < 0.001). The figure does not show responses for the third booster vaccination and respondents who did not report which dose they noticed a tinnitus change.
Among the 372 respondents, 120 reported tinnitus in both ears, 12 center of the ears, 29 left ear, 27 right, nine other, and the remaining 175 no response.
In the 372 survey cases, 264 reported symptom (tinnitus or worsening of existing tinnitus) onset latency relative to the vaccination date. The majority of cases reported tinnitus onset within hours to a few days post-vaccination, 15.2% experienced tinnitus onset within 4 h of vaccination, 17% within 24 h, 25.8% between 1 and 7 days, 13.6% between 1 and 4 weeks, 4.5% after a month, 11% between 1 and 3 months, 6.1% between 3 and 6 months, and 6.8% more than 6 months after vaccination. When comparing mRNA vaccines (Pfizer and Moderna, n = 239) to non-mRNA vaccines (Johnson & Johnson, n = 25), there was no significant difference in the timing of tinnitus onset Mann Whitney test, U = 2925, p = 0.864), results consistent with the previously reported data (Wang et al., 2024).
A pairwise correlation analysis revealed a significant positive correlation between age and history of disorders (r = 0.44, p < 0.05), indicating that older individuals reported more medical conditions than younger individuals. However, no significant correlations were found between age and gender (r = 0.04, p > 0.05) or between gender and history of disorders (r = 0.04, p > 0.05), suggesting that gender does not play a significant role in the history of medical conditions in this dataset.
Many survey respondents reported several neurological, psychiatric, and other pre-existing medical conditions, including tinnitus. We asked the respondents to rate the change in tinnitus severity following COVID-19 vaccination on a scale of 0–10. A pairwise correlation analysis on some common medical conditions, respondent demographics, and tinnitus severity revealed that the reported tinnitus severity scores were not significantly correlated with any respondent's pre-existing medical condition and demographic (Figure 3). Age was significantly correlated with hearing loss (r = 0.35, p < 0.01), head trauma (r = 0.14, p < 0.001), neurological disorder (r = 0.11, p = 0.03), cancer (r = 0.21, p < 0.001), cardiovascular disease (r = 0.25, p < 0.001), osteoporosis (r = 0.24, p < 0.001), and hypertension (r = 0.26, p < 0.001). These results are consistent with our previous study (Wang et al., 2024). Gender was negatively correlated with osteoporosis (r = −0.20, p < 0.001), indicating that females in the study were more likely to report osteoporosis, reflecting known gender-related risks for this condition.
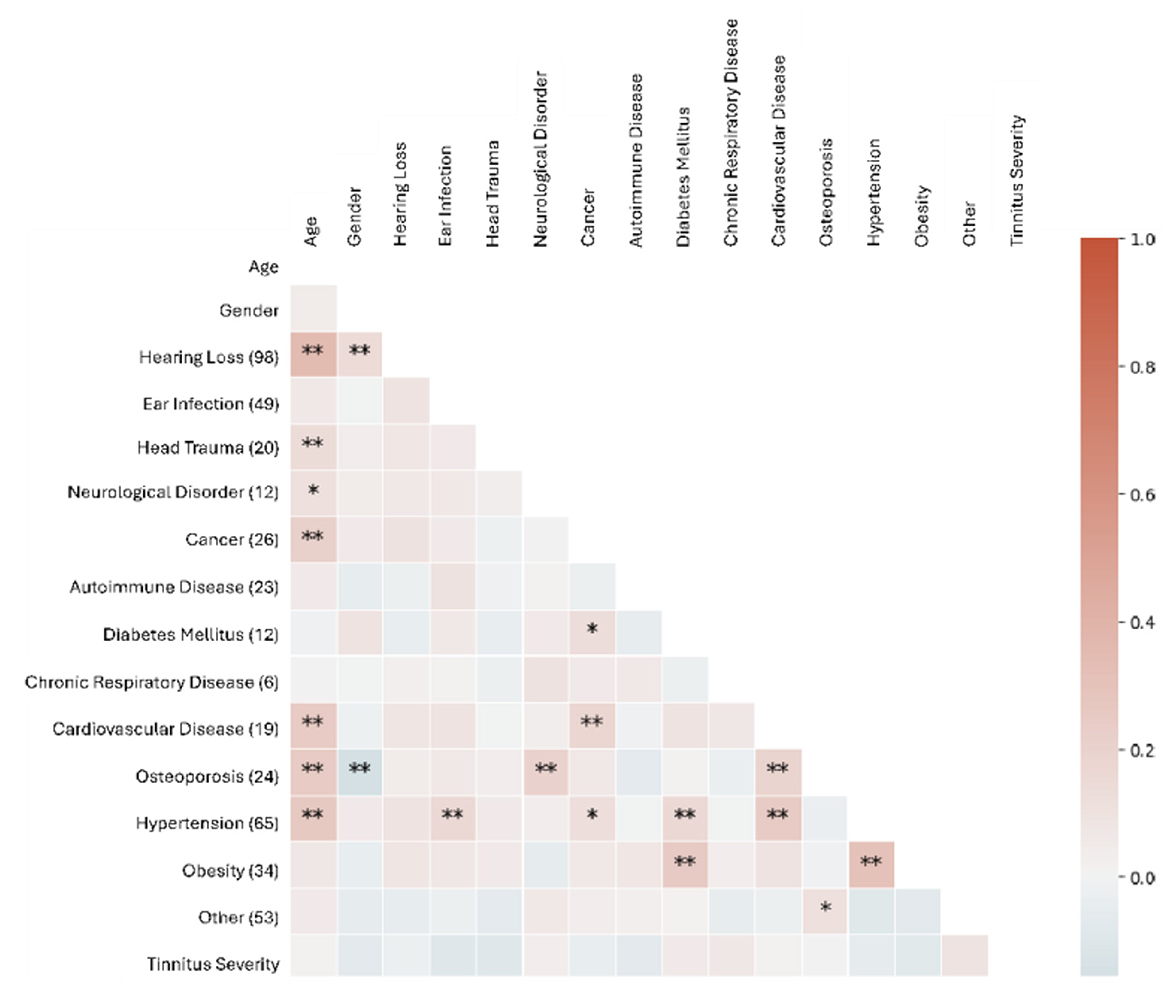
Figure 3. Spearman correlation between age, pre-existing medical conditions, and post-vaccine increase in tinnitus severities. The number of respondents reporting each medical condition is on the left axis. The variable “other” is a group of single reported disorders. Single (*) and double (**) asterisks indicate p < 0.05 and p < 0.01, respectively.
In the survey, 197 respondents reported pre-vaccination tinnitus. In this subpopulation (Figure 4), age was significantly correlated with several health conditions, including hearing loss (r = 0.31, p < 0.01), cancer (r = 0.23, p < 0.001), cardiovascular disease (r = 0.23, p < 0.001), osteoporosis (r = 0.16, p < 0.05), and hypertension (r = 0.23, p < 0.001). These correlations suggest that older respondents were more likely to have these health conditions, consistent with age-related health risks. Gender was negatively correlated with osteoporosis (r = −0.20, p < 0.001), indicating that females in the study were more likely to report osteoporosis, reflecting known gender-related risks for this condition. In this subpopulation, post-vaccination increases in tinnitus severity was not correlated with age or history of the surveyed disorders.
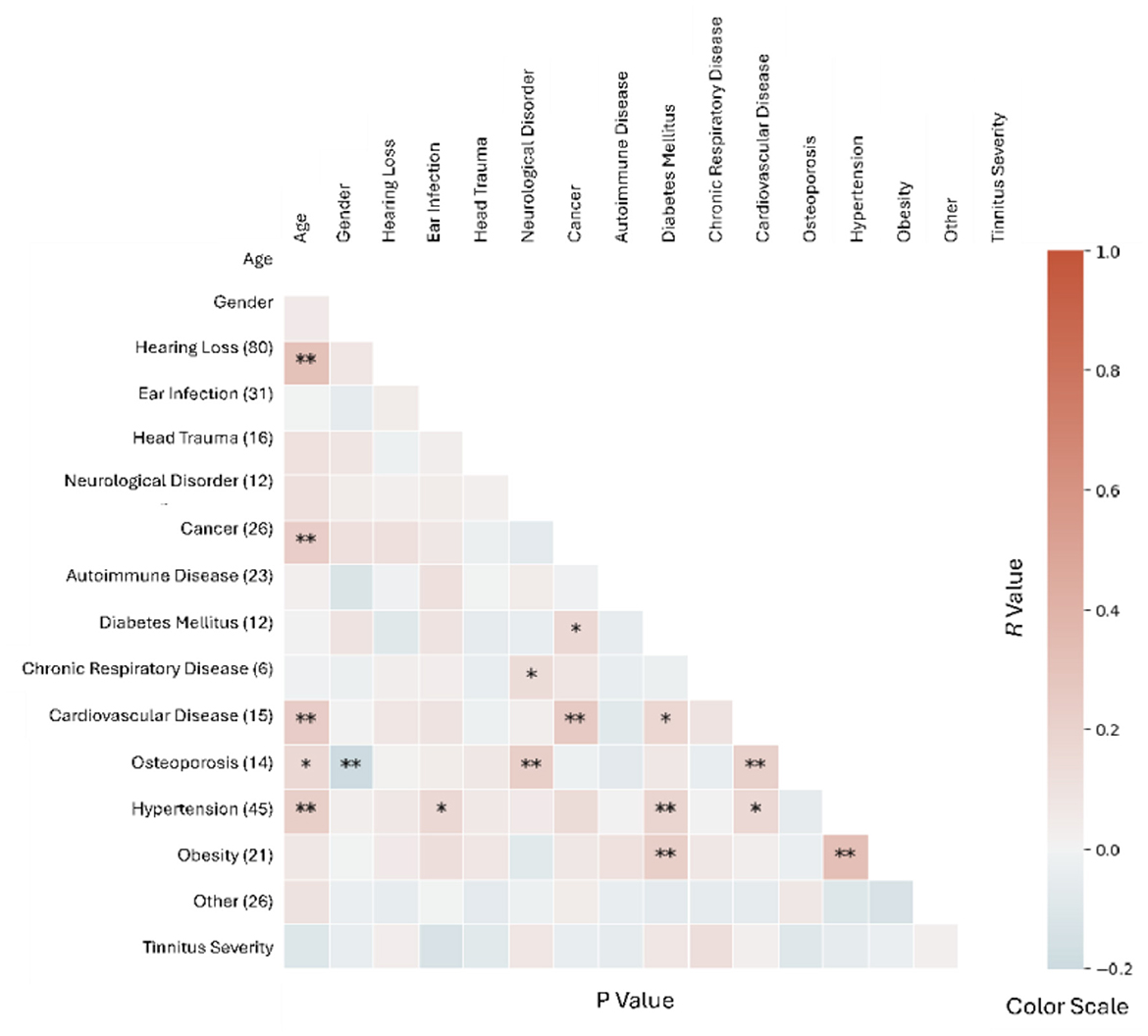
Figure 4. Spearman correlation between age, pre-existing medical conditions, and increases in tinnitus severity in respondents with pre-vaccination tinnitus. The number of respondents reporting each medical condition is on the left axis. The variable “other” is a group of single reported disorders. Single (*) and double (**) asterisks indicate p < 0.05 and p < 0.01, respectively.
Among the respondents, 342 reported post-vaccination tinnitus. In this subpopulation (Figure 5), significant correlations emerged between tinnitus severity and certain pre-existing conditions. Age showed a significant negative correlation with increases in tinnitus severity (r = −0.15, p < 0.01), indicating that older individuals reported less severe tinnitus post-vaccination. This finding suggests that older individuals with tinnitus may be more accustomed to or less affected by symptom severity or that younger individuals might be more sensitive to changes in tinnitus severity post-vaccination. Interestingly, negative correlations were observed between increases in tinnitus severity and specific conditions, including ear infections (r = −0.11, p < 0.05), head trauma (r = −0.12, p < 0.05), autoimmune disease (r = −0.11, p < 0.05), and hypertension (r = −0.11, p < 0.01).
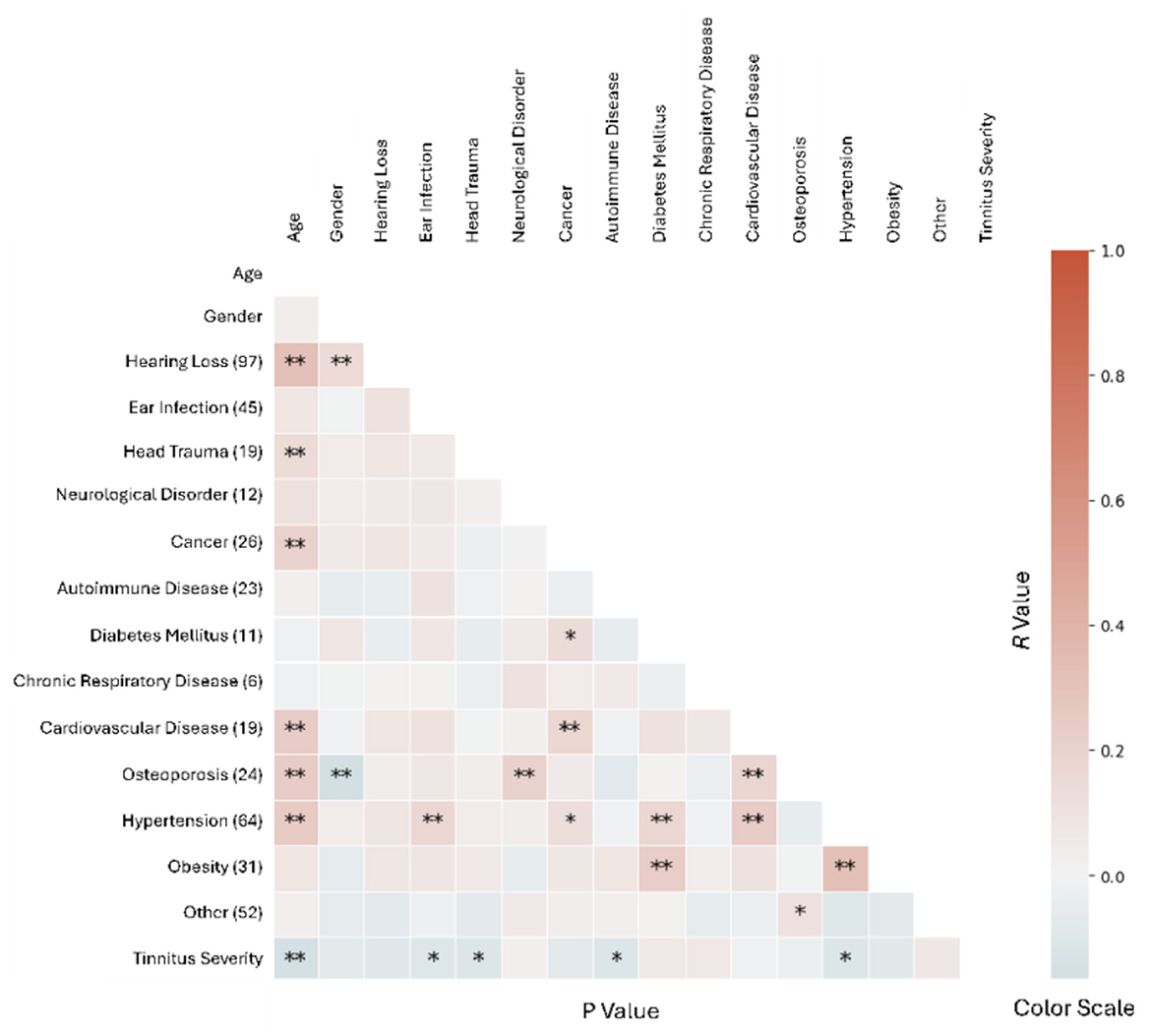
Figure 5. Spearman correlation between age, pre-existing medical conditions, and increases in tinnitus severity in respondents who reported post-vaccination tinnitus. The number of respondents reporting each medical condition is on the left axis. The variable “other” is a group of single reported disorders. Single (*) and double (**) asterisks indicate p < 0.05 and p < 0.01, respectively.
To further understand the influence of pre-existing disorders on tinnitus, we compared tinnitus loudness before and after COVID-19 vaccination between respondents with and without diabetes, hypertension and obesity (Figure 6). The increase in tinnitus severity following COVID-19 vaccination was significantly worse in respondents with diabetes (t = 3.78, p = 0.0034) than in those without the disorder. In addition, compare to respondents without hypertension, those with hypertension had more severity pre-vaccination tinnitus (t = 1.66, p = 0.0022) but not post-vaccination tinnitus. The difference between post- vs. pre-vaccination tinnitus was less in hypertensive respondents than the rest, but the difference was not statistically significant. Similarly, respondents with obesity tended to have more severe pre-existing tinnitus and less increases in tinnitus severity following COVID-19 vaccination (not statistically significant). These results indicate that certain metabolic disorders might lead to worse pre-existing or post-COVID-19 vaccination tinnitus. Furthermore, the negative correlations between post-vaccination increases in tinnitus severity and certain disorders (ear infection, head trauma and autoimmune diseases) seen in Figure 5 were likely due to worse pre-existing tinnitus, rather than protection against vaccination-related tinnitus.
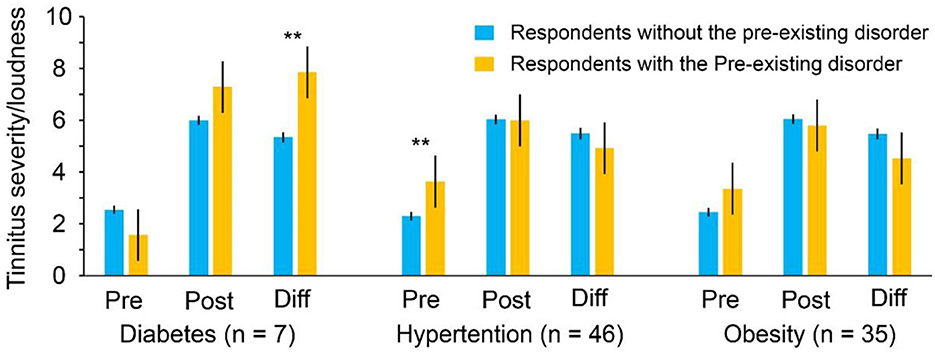
Figure 6. Effects of diabetes, hypertension and obesity on tinnitus severity/loudness before and after COVID-19 vaccination. Pre: reported tinnitus loudness before COVID-19 vaccination; Post: reported tinnitus loudness after COVID-19 vaccination; Diff: reported increase in tinnitus severity following COVID-19 vaccination. Double (**) asterisks indicate p < 0.01.
A majority of the respondents had rarely (20.5% never and 66.4% not very often) been exposed to very loud noise. Only 5.4% of respondents experienced loud noise weekly. The loud noise experience was not significantly correlated with changes in tinnitus severity following COVID vaccination (r = −0.03, p = 0.62). These results suggest that while tinnitus severity varies widely post-vaccination, noise exposure is not a key factor influencing symptom changes following COVID-19 vaccination.
The survey respondents provided detailed descriptions of their tinnitus experiences, which were analyzed using text-mining techniques to identify key themes. Four distinct topics emerged, each offering insight into how tinnitus manifests among individuals.
This topic centers on persistent, high-pitched sounds such as ringing, buzzing, or hissing, which many respondents reported as a dominant characteristic of their tinnitus. The impact of these constant sounds is significant, affecting daily activities and quality of life. The variability in sound type reflects the individualized nature of tinnitus. Some respondents expressed concern that their symptoms may have been influenced by COVID-19 vaccination, highlighting the need for further research into potential vaccine-related triggers. Below are selected excerpts from the textual responses that closely align with the key topics identified in the analysis:
Excerpt 1: “Constant ringing in both ears at a very high pitch. It's so loud I sometimes can't hear over it.”
Excerpt 2: “High pitch whine that changes volume as if turning up a radio.”
Many respondents described their tinnitus as constant and loud, often accompanied by a hissing sound. A notable portion of these individuals associated their symptoms with receiving the Pfizer and Moderna vaccine, suggesting a perceived link between the vaccine and tinnitus onset or worsening. The combination of constant high-pitched sounds and their perceived connection to vaccination indicates a particularly severe form of tinnitus, which warrants further investigation into potential causes and exacerbations. Additionally, many respondents reported changes in auditory speech perception (Yellamsetty et al. in preparation),1 particularly in noisy environments, with a noticeable worsening of sound tolerance. Issues such as difficulties tolerating loud sounds and hearing challenges were commonly noted. Below are selected excerpts from the textual responses that closely align with the key topics identified in the analysis:
Excerpt 3: “The vaccine induced a very high pitch tinnitus in both ears that is much higher in pitch and louder than my previous tinnitus and constant I was dealing with.”
Excerpt 4: “Constant high-pitched buzzing in my left ear. After Covid vax, I now have buzzing in right ear as well, although at a lower volume and slightly lower pitch.”
This topic focuses on loud tinnitus primarily affecting one ear, often accompanied by additional symptoms such as ear pain or pulsations. The unilateral nature, combined with the variability in sound intensity and pitch, suggests a more complex form of tinnitus. The presence of accompanying symptoms indicates a need for further clinical investigation, as this type of tinnitus may be related to underlying conditions. The physical and emotional toll on those affected is significant, profoundly disrupting their wellbeing and daily life. Below are selected excerpts from the textual responses that closely align with the key topics identified in the analysis:
Excerpt 5: “Left ear I hear my heart beating, right ear is a hissing and ringing sound.”
Excerpt 6: “100% of the time LOUD ringing in right ear. Left ear hum/ringing comes and goes. Top of the head ringing fluctuates between unbearably loud and bearable.”
A unique form of tinnitus was described by respondents as resembling the sound of crickets or other insect-like noises, often accompanied by buzzing or hissing. Many reported this type of tinnitus as constant, though some noted fluctuations in intensity or the presence of other auditory symptoms. The distinctive nature of these sounds suggests that this form of tinnitus is particularly disruptive, affecting hearing and the overall perception of sound in daily life. Below are selected excerpts from the textual responses that closely align with the key topics identified in the analysis:
Excerpt 7: “It sounds like crickets or an alarm that is in the distance. It gets louder at night and is constant all day from when I wake up to bedtime.”
Excerpt 8: “Reactive tinnitus that fluctuates regularly, especially to loud sounds. Dominant tone is crickets in mid-range but can move into higher ranges. Also hear other tones off and on, like buzzing and clicking.”
The diverse descriptions of tinnitus reflect the complexity of the condition, with symptoms ranging from high-pitched ringing to more unique sounds like crickets. The perceived link between tinnitus and the Moderna vaccine among some respondents points to the need for further research into vaccine-related auditory symptoms. Additionally, the presence of unilateral tinnitus and other symptoms, such as ear pain, underscores the importance of investigating potential underlying conditions in affected individuals.
Tinnitus characteristics were assessed using self-reported ratings for loudness, pitch, and anxiety on a 0 to 10 scale, where 0 represented “very soft/low” and 10 represented “very loud/high.” Before the COVID-19 vaccination, 56 respondents (29.8%) reported unilateral tinnitus (left or right ear), 120 (63.8%) reported bilateral tinnitus (both ears), and 12 (6.4%) experienced tinnitus in the center of the head.
For those with pre-existing tinnitus (Figure 7), the mean loudness rating increased significantly from 4.83 before vaccination to 6.68 after vaccination (t = −7.96, p < 0.05). Tinnitus pitch also increased from a mean of 6.88 to 7.67 post-vaccination (t = −3.66, p < 0.05). While there was no significant correlation between loudness and pitch (r = 0.06, p > 0.05), participants rated these characteristics differently (t = −9.39, p < 0.05). Anxiety related to tinnitus also rose significantly, from a mean of 3.91 before vaccination to 5.49 afterward (t = −4.94, p < 0.05). For individuals with new-onset tinnitus post-vaccination (Figure 7), the mean severity rating was 6.07. Loudness ratings were higher, with a mean of 7.18, and pitch increased to 7.83. Anxiety levels also rose, with a mean rating of 7.74, and many respondents reported significant interference with hearing and speech comprehension in various settings.
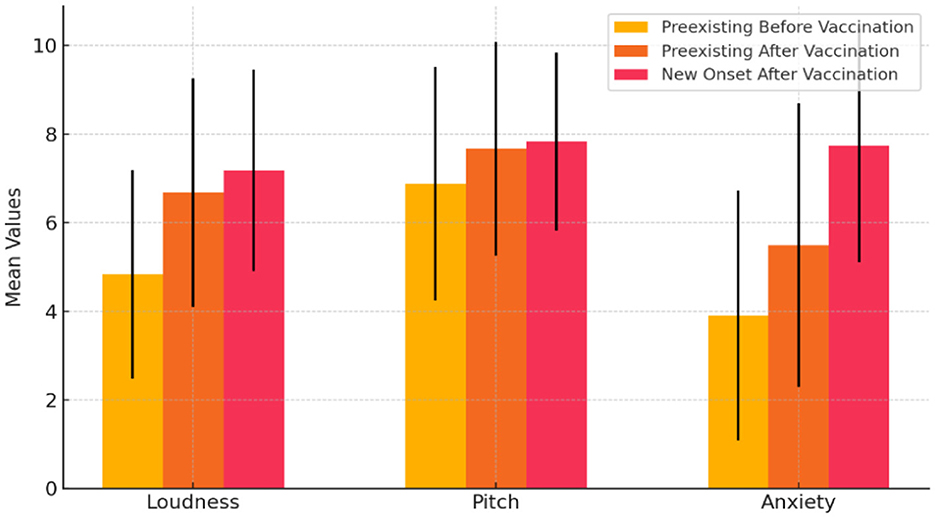
Figure 7. Comparison of tinnitus (loudness, pitch, and anxiety) before and after COVID-19 vaccination for individuals with pre-existing and new-onset tinnitus. Rated on a 0 to 10 Scale, where 0 represents “very soft/low” and 10 represents “very loud/high”.
These findings suggest that tinnitus worsened in terms of loudness, pitch, and anxiety after vaccination, with moderate effects on sound tolerance. This worsening highlights the need for further research on the auditory effects of COVID-19 vaccination, particularly for those with pre-existing tinnitus.
This study sought to explore the prevalence, characteristics, and potential triggers of tinnitus among individuals who received COVID-19 vaccinations, with particular attention to how pre-existing medical conditions and demographics might influence tinnitus severity. The findings from the survey, supported by text mining analysis, reveal key trends and correlations that contribute to a deeper understanding of how tinnitus manifests in the context of COVID-19 vaccination.
The mechanisms by which COVID-19 vaccination increases the risk of tinnitus are unknown. The rapid onset of tinnitus following COVID-19 vaccination suggest that the tinnitus is not caused by vaccine-induced responses, which develops gradually over many days after immunization. Instead, it was mediated by a direct pathway. Spike proteins can disrupt the blood-brain barrier (DeOre et al., 2021; Petrovszki et al., 2022; Rhea et al., 2021; Zhang et al., 2021), induce microglial activation/neuroinflammation (Albornoz et al., 2023; Frank et al., 2022) and neuronal death (Oh et al., 2022). It may also cause aggregation of β-amyloid proteins, prions, α-synuclein and tau, potentially leading to neurodegeneration (Chakrabarti et al., 2022; Idrees and Kumar, 2021; Tavassoly et al., 2020). It is unclear whether COVID-19 vaccines, modified forms of the spike protein, can cause similar neurological damages, leading to tinnitus and other neurological symptoms. COVID-19 vaccines may also cause endothelial dysfunction and vascular inflammation (Cernera et al., 2024; Terentes-Printzios et al., 2022; Yoshimoto et al., 2023; Ariyoshi et al., 2023), which could disrupt blood-brain barrier and other brain function, and possibly lead to tinnitus and other mental health issues (Yang et al., 2013).
One of the main findings of this study is the significant distribution of tinnitus cases among different COVID-19 vaccine manufacturers, with Pfizer being the most frequently associated with tinnitus, followed by Moderna and Johnson & Johnson. Although the exact cause of this difference remains unclear, the higher incidence of tinnitus in Pfizer and Moderna vaccine recipients may warrant further investigation into the specific immune or inflammatory responses triggered by these vaccines. The perceived link between tinnitus onset and the vaccines, particularly the Moderna vaccine, as seen in Topic 2 of the text mining analysis, underscores the need for longitudinal studies to determine causal relationships.
The results also highlight how demographic factors, such as age and gender, correlate with tinnitus severity and the history of medical conditions. The significant positive correlation between age and the history of disorders (r = 0.44, p < 0.05) aligns with existing literature that associates increasing age with the accumulation of chronic conditions, including hearing loss, diabetes mellitus (Samocha-Bonet et al., 2021), and cardiovascular diseases (Tan et al., 2018), which are known risk factors for tinnitus (Baracca et al., 2011; Gaspar et al., 2011; Stegeman et al., 2021). However, the lack of a statistically significant correlation between gender, age, and history of disorders suggests that gender does not play a major role in determining the severity or occurrence of tinnitus in this sample. This outcome could be influenced by several factors, including sample size, the distribution of gender across age groups, or potential variations in reporting patterns between genders.
In the post-vaccination phase, tinnitus severity was not significantly correlated with any specific pre-existing medical condition or demographic factor, except for age and certain conditions like hearing loss and hypertension (Wang et al., 2024). This finding aligns with prior research indicating that older adults and those with cardiovascular diseases or hypertension are more susceptible to tinnitus, as these conditions can affect blood flow and nerve function in the auditory system (Gaspar et al., 2011; Tan et al., 2018). Interestingly, the correlation between age and pre-existing conditions such as cancer, cardiovascular disease, and osteoporosis before vaccination remained consistent post-vaccination, suggesting that age-related health factors might continue to influence tinnitus in vaccinated individuals.
The findings of this study provide critical insights into the relationship between COVID-19 vaccination and tinnitus, particularly in individuals with pre-existing tinnitus and those who developed tinnitus post-vaccination. For individuals with pre-existing tinnitus, there was a notable increase in loudness, pitch, and anxiety after vaccination, suggesting that the vaccine may exacerbate these symptoms (Fioretti et al., 2022). The significant rise in anxiety post-vaccination also points to the emotional toll that worsening tinnitus can have, emphasizing the need for psychological and medical support for affected individuals (Yellamsetty, 2023). In the case of new-onset tinnitus, the severity of symptoms—such as high levels of loudness, pitch, and anxiety—suggests that this group experiences a more intense form of tinnitus (Yellamsetty and Shin, in preparation).2 Furthermore, many respondents self-reported changes in speech understanding, particularly in noisy environments (Yellamsetty et al. in preparation, see text footnote 1), along with a worsening of sound tolerance. Commonly reported issues included difficulty tolerating loud sounds and challenges with hearing. These effects may be related to immune responses or inflammation triggered by the vaccine, underscoring the need for further investigation into the underlying causes of vaccine-related tinnitus.
Additionally, there was no significant difference in symptom onset between mRNA and non-mRNA vaccines, indicating that other factors, such as individual health conditions or stress, may play a more significant role in tinnitus onset. Respondents also reported increased difficulty with speech perception and sound tolerance, showing how the condition affects daily functioning. The rise in anxiety levels further underscores the need for healthcare providers to be aware of the psychological impact of tinnitus and to provide appropriate interventions, such as counseling or therapy.
The analysis of noise exposure, both pre- and post-vaccination, revealed no statistically significant correlation between noise exposure and tinnitus severity. However, it is noteworthy that many respondents, particularly post-vaccination, reported varying degrees of tinnitus severity, ranging from mild to extremely severe. This finding suggests that while loud noise is a recognized risk factor for tinnitus (Bauer et al., 2016; Bhatt et al., 2016), its interaction with post-vaccine tinnitus may not be straightforward or require more detailed exposure metrics to fully understand its role. Additionally, the subjective nature of tinnitus and individual variability in noise exposure may have contributed to the lack of clear correlations in this area.
The text mining analysis revealed four types of tinnitus experiences, highlighting the diversity of symptoms among respondents. Descriptions ranged from high-pitched, constant ringing and hissing (Topic 1) to cricket-like buzzing sounds (Topic 4), reflecting the wide range of auditory experiences reported. Notably, many respondents experiencing loud, constant tinnitus (Topic 2) associated the onset or worsening of symptoms with the Moderna vaccine, emphasizing the need for further research into potential auditory side effects of vaccines.
The variability in tinnitus sounds, including unilateral tinnitus (Topic 3), suggests different underlying causes, such as cochlear damage or central nervous system involvement, which have been supported by previous research (Cederroth et al., 2019; Henry et al., 2014). The cricket-like and fluctuating tinnitus (Topic 4) aligns with existing studies showing that tinnitus can manifest in diverse forms, potentially influenced by physiological and psychological factors (Henry et al., 2014). These findings reinforce the complexity of tinnitus and the importance of individualized approaches to understanding and treating the condition.
These findings have several clinical implications. First, the variability in tinnitus severity and type underscores the importance of personalized approaches to tinnitus management. Audiologists and healthcare providers should consider the wide range of factors influencing tinnitus, from vaccine type to pre-existing medical conditions, when assessing and treating patients. Additionally, the potential link between COVID-19 vaccines and tinnitus, particularly with specific vaccines, warrants further investigation through controlled studies to better understand the mechanisms behind this phenomenon.
Moreover, the significant associations between age and certain pre-existing conditions, both before and after vaccination, highlight the need for ongoing monitoring of older adults and those with chronic health issues, as these populations may be at greater risk for developing or worsening tinnitus following vaccination.
In conclusion, while this study provides important insights into the relationship between COVID-19 vaccines, demographics, pre-existing conditions, and tinnitus severity, further research is needed to establish clearer causal pathways and to explore potential treatment options for those experiencing post-vaccine tinnitus.
One limitation of this study is its reliance on self-reported data, which may introduce recall bias and affect the accuracy of the participants' responses regarding their tinnitus symptoms before and after COVID-19 vaccination. Additionally, the sample size, while sufficient for identifying trends, may not be large or diverse enough to fully represent the general population, particularly regarding specific subgroups such as those with varying underlying health conditions or different vaccination types. The study also lacks long-term follow-up data, limiting the ability to assess the persistence or progression of tinnitus symptoms over time. Finally, without objective audiological assessments, the findings are based solely on subjective experiences, which may vary between individuals and complicate the generalizability of the results.
This study provides valuable insights into the relationship between COVID-19 vaccinations, tinnitus, and various demographic and medical factors. The findings reveal that tinnitus symptoms, both onset and worsening, are commonly reported after receiving the Pfizer and Moderna vaccines, with a small subset of respondents linking their tinnitus to the vaccines themselves. Additionally, correlations between age, pre-existing medical conditions, and tinnitus severity emphasize this condition's complex and multifaceted nature. While no significant correlation was found between noise exposure and tinnitus severity, the variability in tinnitus descriptions, from high-pitched ringing to cricket-like sounds, highlights the individualized experience of those affected. These results underscore the importance of personalized approaches to tinnitus management and the need for further research to explore potential triggers, including vaccines, and to establish clearer mechanisms underlying the condition. Understanding these nuances will be critical in developing more effective treatment strategies for those suffering from tinnitus in pre- and post-vaccine contexts.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by San Jose State University IRB Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
AY: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. E-EE: Formal analysis, Validation, Visualization, Writing – review & editing. SB: Validation, Visualization, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
The author(s) declare that Gen AI was used in the creation of this manuscript. Generative AI was utilized in this manuscript to assist with language refinement, and the improvement of clarity. The content of the manuscript, including the data analysis, research findings, and conclusions, were entirely developed by the author(s). The AI was used as a tool for revising text, and all intellectual contributions are the sole responsibility of the author(s).
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. ^Yellamsetty, A., Etu, E. E., Fortuna, G., Bao, S. (in preparation). Tinnitus and COVID-19: Impacts on Hearing and Speech Perception.
2. ^Yellamsetty, A., and Shin, M. (in preparation). Psychological Effects of COVID-19 and Tinnitus Perception.
Albornoz, E. A., Amarilla, A. A., Modhiran, N., Parker, S., Li, X. X., Wijesundara, D. K., et al. (2023). SARS-CoV-2 drives NLRP3 inflammasome activation in human microglia through spike protein. Mol. Psychiatry 28, 2878–2893. doi: 10.1038/s41380-022-01831-0
Ariyoshi, T., Hoshide, M., Motonaga, T., Korenaga, Y., Azuma, Y., Ichimura, T., et al. (2023). Childhood primary angiitis of the central nervous system following COVID-19 vaccination (BNT162b2/Pfizer-BioNtech): a case report. Hum. Vaccin. Immunother. 19:2261167. doi: 10.1080/21645515.2023.2261167
Baracca, G., Del Bo, L., and Ambrosetti, U. (2011). “Tinnitus and hearing loss,” in Textbook of Tinnitus (New York, NY: Springer), 285–291. doi: 10.1007/978-1-60761-145-5_35
Bauer, C. A., Berry, J., and Brozoski, T. J. (2016). Clinical trials supported by the tinnitus research consortium: lessons learned, the Southern Illinois University experience. Hear. Res. 334, 65–71. doi: 10.1016/j.heares.2015.05.001
Beukes, E. W., Onozuka, J., Brazell, T. P., and Manchaiah, V. (2021). Coping with tinnitus during the COVID-19 pandemic. Am. J. Audiol. 30, 385–393. doi: 10.1044/2021_AJA-20-00188
Bhatt, J. M., Lin, H. W., and Bhattacharyya, N. (2016). Prevalence, severity, exposures, and treatment patterns of tinnitus in the United States. JAMA Otolaryngol. Head Neck Surg. 142, 959–965. doi: 10.1001/jamaoto.2016.1700
Cederroth, C. R., Gallus, S., Hall, D. A., Kleinjung, T., Langguth, B., Maruotti, A., et al. (2019). Towards an understanding of tinnitus heterogeneity. Front. Aging Neurosci. 11:446253. doi: 10.3389/fnagi.2019.00053
Cernera, G., Gelzo, M., De Placido, P., Pietroluongo, E., Raia, M., Scalia, G., et al. (2024). Serum biomarkers of inflammation and vascular damage upon SARS-Cov-2 mRNA vaccine in patients with thymic epithelial tumors. Clin. Chem. Lab. Med. 62, 1198–1205. doi: 10.1515/cclm-2023-1283
Chakrabarti, S. S., Tiwari, A., Jaiswal, S., Kaur, U., Kumar, I., Mittal, A., et al. (2022). Rapidly progressive dementia with asymmetric rigidity following ChAdOx1 nCoV-19 vaccination. Aging Dis. 13:633. doi: 10.14336/AD.2021.1102
Colizza, A., Ralli, M., Turchetta, R., Minni, A., Greco, A., and de Vincentiis, M. (2022). Otolaryngology adverse events following COVID-19 vaccines. Eur. Rev. Med. Pharmacol. Sci. 26, 4113–4116. doi: 10.26355/eurrev_202206_28981
Daher, G. S., Nassiri, A. M., Vanichkachorn, G., Carlson, M. L., Neff, B. A., and Driscoll, C. L. W. (2022). New onset tinnitus in the absence of hearing changes following COVID-19 infection. Am. J. Otolaryngol. 43:103208. doi: 10.1016/j.amjoto.2021.103208
Das, S., Sun, X., and Dutta, A. (2016). Text mining and topic modeling of compendiums of papers from transportation research board annual meetings. Transp. Res. Rec. 2552, 48–56. doi: 10.3141/2552-07
Degen, C. V., Mikuteit, M., Niewolik, J., Schröder, D., Vahldiek, K., Mücke, U., et al. (2022). Self-reported tinnitus and vertigo or dizziness in a cohort of adult long COVID patients. Front. Neurol. 13:884002. doi: 10.3389/fneur.2022.884002
DeOre, B. J., Tran, K. A., Andrews, A. M., Ramirez, S. H., and Galie, P. A. (2021). SARS-CoV-2 spike protein disrupts blood–brain barrier integrity via RhoA activation. J. Neuroimmune Pharmacol. 16, 722–728. doi: 10.1007/s11481-021-10029-0
Dorney, I., Bobak, L., Otteson, T., and Kaelber, D. C. (2023). Prevalence of new-onset tinnitus after COVID-19 vaccination with comparison to other vaccinations. Laryngoscope 133, 1722–1725. doi: 10.1002/lary.30395
Etu, E. E., Sureshbabu, K., Summerville, S., Parmar, A., and Huang, G. (2023). What changes the travel pattern: a national survey on the impacts of the COVID-19 pandemic on older adults' public transportation usage. J. Transp. Health 33:101718. doi: 10.1016/j.jth.2023.101718
Feng, S. J., Voruz, F., Yu, M., and Lalwani, A. K. (2023). COVID-19 and hearing loss—a narrative review. Front. Audiol. Otol. 1:1233793. doi: 10.3389/fauot.2023.1233793
Finsterer, J., and Edmonds, R. (2022). Persisting, unilateral tinnitus 22 days after first dose of an mRNA-based SARS-CoV-2 vaccine. J. Family Med. Prim. Care. 11, 3330–3332. doi: 10.4103/jfmpc.jfmpc_1927_21
Fioretti, A., Natalini, E., Triggianese, G., Eibenstein, R., Angelone, A. M., Lauriello, M., et al. (2022). Impact of the COVID-19 lockdown on patients with chronic tinnitus—preliminary results. Audiol. Res. 12, 327–336. doi: 10.3390/audiolres12030034
Frank, M. G., Nguyen, K. H., Ball, J. B., Hopkins, S., Kelley, T., Baratta, M. V., et al. (2022). SARS-CoV-2 spike S1 subunit induces neuroinflammatory, microglial and behavioral sickness responses: evidence of PAMP-like properties. Brain Behav. Immun. 100, 267–277. doi: 10.1016/j.bbi.2021.12.007
Gaspar, L., Makovnik, M., Bendzala, M., Hlinstakova, S., Ocadlik, I., and Gasparova, E. (2011). “Components of metabolic syndrome and their relation to tinnitus,” in Up to Date on Tinnitus (London: IntechOpen), 117. doi: 10.5772/26980
Henry, J. A., Roberts, L. E., Caspary, D. M., Theodoroff, S. M., and Salvi, R. J. (2014). Underlying mechanisms of tinnitus: review and clinical implications. J. Am. Acad. Audiol. 25, 005–022. doi: 10.3766/jaaa.25.1.2
Idrees, D., and Kumar, V. (2021). SARS-CoV-2 spike protein interactions with amyloidogenic proteins: potential clues to neurodegeneration. Biochem. Biophys. Res. Commun. 554, 94–98. doi: 10.1016/j.bbrc.2021.03.100
Jafari, Z., Kolb, B. E., and Mohajerani, M. H. (2022). Hearing loss, tinnitus, and dizziness in COVID-19: a systematic review and meta-analysis. Can. J. Neurol. Sci. 49, 184–195. doi: 10.1017/cjn.2021.63
Leong, S., Teh, B. M., and Kim, A. H. (2023). Characterization of otologic symptoms appearing after COVID-19 vaccination. Am. J. Otolaryngol. 44:103725. doi: 10.1016/j.amjoto.2022.103725
Liang, Y., Xu, J., Chu, M., Mai, J., Lai, N., Tang, W., et al. (2020). Neurosensory dysfunction: a diagnostic marker of early COVID-19. Int. J. Infect. Dis. 98, 347–352. doi: 10.1016/j.ijid.2020.06.086
Liu, L., Tang, L., Dong, W., Yao, S., and Zhou, W. (2016). An overview of topic modeling and its current applications in bioinformatics. SpringerPlus 5, 1–22. doi: 10.1186/s40064-016-3252-8
Medina, M. C., and Gómez, M. R. (2022). Tinnitus, sudden sensorineural hearing loss, and vestibular neuritis as complications of the astra zeneca COVID-19 vaccine. Cureus, 14:e20906. doi: 10.7759/cureus.20906
Munro, K. J., Uus, K., Almufarrij, I., Chaudhuri, N., and Yioe, V. (2020). Persistent self-reported changes in hearing and tinnitus in post-hospitalisation COVID-19 cases. Int. J. Audiol. 59, 889–890. doi: 10.1080/14992027.2020.1798519
Narozny, W., Tretiakow, D., and Skorek, A. (2021). Tinnitus in COVID-19 Pandemic. Los Angeles, CA: SAGE Publications Sage, 197S–198S. doi: 10.1177/0145561320988364
Oh, J., Cho, W. H., Barcelon, E., Kim, K. H., Hong, J., and Lee, S. J. (2022). SARS-CoV-2 spike protein induces cognitive deficit and anxiety-like behavior in mouse via non-cell autonomous hippocampal neuronal death. Sci. Rep. 12:5496. doi: 10.1038/s41598-022-09410-7
Ong, K. M. C., and Cruz, T. L. G. (2022). Otologic and vestibular symptoms in COVID-19: a scoping review. World J. Otorhinolaryngol. Head Neck Surg. 8, 287–296. doi: 10.1002/wjo2.57
Petrovszki, D., Walter, F. R., Vigh, J. P., Kocsis, A., Valkai, S., Deli, M. A., et al. (2022). Penetration of the SARS-CoV-2 spike protein across the blood–brain barrier, as revealed by a combination of a human cell culture model system and optical biosensing. Biomedicines 10:188. doi: 10.3390/biomedicines10010188
Rhea, E. M., Logsdon, A. F., Hansen, K. M., Williams, L. M., Reed, M. J., Baumann, K. K., et al. (2021). The S1 protein of SARS-CoV-2 crosses the blood–brain barrier in mice. Nat. Neurosci. 24, 368–378. doi: 10.1038/s41593-020-00771-8
Samocha-Bonet, D., Wu, B., and Ryugo, D. K. (2021). Diabetes mellitus and hearing loss: a review. Ageing Res. Rev. 71:101423. doi: 10.1016/j.arr.2021.101423
Stegeman, I., Eikelboom, R. H., Smit, A. L., Baguley, D. M., Bucks, R. S., Stokroos, R. J., et al. (2021). Tinnitus and its associations with general health, mental health and hearing loss. Prog. Brain Res. 262, 431–450. doi: 10.1016/bs.pbr.2021.01.023
Tan, H., Lan, N., Knuiman, M., Divitini, M. L., Swanepoel, D. W., Hunter, M., et al. (2018). Associations between cardiovascular disease and its risk factors with hearing loss—a cross-sectional analysis. Clin. Otolaryngol. 43, 172–181. doi: 10.1111/coa.12936
Tavassoly, O., Safavi, F., and Tavassoly, I. (2020). Seeding brain protein aggregation by SARS-CoV-2 as a possible long-term complication of COVID-19 infection. ACS Chem. Neurosci. 11, 3704–3706. doi: 10.1021/acschemneuro.0c00676
Terentes-Printzios, D., Gardikioti, V., Solomou, E., Emmanouil, E., Gourgouli, I., Xydis, P., et al. (2022). The effect of an mRNA vaccine against COVID-19 on endothelial function and arterial stiffness. Hypertens. Res. 45, 846–855. doi: 10.1038/s41440-022-00876-6
Wang, W., Yellamsetty, A., Edmonds, R. M., Barcavage, S. R., and Bao, S. (2024). COVID-19 vaccination-related tinnitus is associated with pre-vaccination metabolic disorders. Front. Pharmacol. 15:1374320. doi: 10.3389/fphar.2024.1374320
Yang, G., Parkhurst, C. N., Hayes, S., and Gan, W. B. (2013). Peripheral elevation of TNF-α leads to early synaptic abnormalities in the mouse somatosensory cortex in experimental autoimmune encephalomyelitis. Proc. Natl. Acad. Sci. USA 110, 10306–10311. doi: 10.1073/pnas.1222895110
Yellamsetty, A. (2023). COVID-19 vaccination effects on tinnitus and hyperacusis: longitudinal case study. Int. Tinnitus J. 27, 253–258. doi: 10.5935/0946-5448.20230039
Yellamsetty, A., and Gonzalez, V. (2023). A report on emerging evidence and implications of COVID-19 related tinnitus: preliminary survey results. Otolaryngol. Open Access J. 8:000271. doi: 10.23880/ooaj-16000271
Yoshimoto, K., Kaneda, S., Asada, M., Taguchi, H., Kawashima, H., Yoneima, R., et al. (2023). Giant cell arteritis after COVID-19 vaccination with long-term follow-up: a case report and review of the literature. Medicina 59:2127. doi: 10.3390/medicina59122127
Keywords: tinnitus, COVID-19 vaccination, pre-existing tinnitus, new-onset tinnitus, auditory symptoms, loudness, pitch, anxiety
Citation: Yellamsetty A, Etu EE and Bao S (2025) Impact of COVID-19 vaccination on tinnitus onset and severity: a comprehensive survey study. Front. Audiol. Otol. 3:1509444. doi: 10.3389/fauot.2025.1509444
Received: 11 October 2024; Accepted: 24 January 2025;
Published: 07 February 2025.
Edited by:
Divya Bharatkumar Adhia, University of Otago, New ZealandReviewed by:
Prashanth Prabhu, All India Institute of Speech and Hearing (AIISH), IndiaCopyright © 2025 Yellamsetty, Etu and Bao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anusha Yellamsetty, YW51c2hhLnllbGxhbXNldHR5QHNqc3UuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.