
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Audiol. Otol., 10 May 2024
Sec. Vestibular Disorders
Volume 2 - 2024 | https://doi.org/10.3389/fauot.2024.1378569
 E. C. Martin1
E. C. Martin1 L. E. G. H. de Joode1
L. E. G. H. de Joode1 F. Lucieer1
F. Lucieer1 D. Sitters1
D. Sitters1 P. A. E. G. Delespaul2
P. A. E. G. Delespaul2 C. Leue2
C. Leue2 S. C. F. van de Weijer3
S. C. F. van de Weijer3 A. Meijers-Erdkamp3
A. Meijers-Erdkamp3 E. Grill4
E. Grill4 A. Zwergal5
A. Zwergal5 N. Guinand6
N. Guinand6 A. Perez-Fornos6
A. Perez-Fornos6 V. van Rompaey7,8
V. van Rompaey7,8 J. Widdershoven1
J. Widdershoven1 M. L. Kimman9
M. L. Kimman9 R. van de Berg1*
R. van de Berg1*Introduction: Vestibular disorders have a high prevalence and impact on general health. Currently questionnaires to measure vestibular symptoms and the impact on daily life, do not capture disease-specific symptoms or induce recall bias. The DizzyQuest was introduced, to measure vestibular symptoms in the flow of daily life, using the ecological momentary assessment (EMA) strategy. The development and content validity of the DizzyQuest are described in this article.
Methods: The development process consisted of two stages: First, the development of a concept version of the DizzyQuest based on the conceptual model of positive health, semi-structured interviews with patients diagnosed with bilateral vestibulopathy (BV) and expert input. Second, the assessment of content validity through a 4-week pilot trial, followed by focus group meetings with patients and professionals separately.
Results: Patient interviews, an expert meeting and a conceptual model resulted in the first pilot version of the DizzyQuest, which included a morning-, within-day-, evening- and attack-questionnaire. To report patient characteristics, complimentary patient- and doctor-questionnaires were added. The pilot trial (N = 5) and two patient focus group meetings resulted in multiple suggestions for response options. Two professional focus group meetings provided recommendations for sampling time and sampling schedule. As a result, two versions of the DizzyQuest were developed, consisting of a regular DizzyQuest (DQ) and an extended DizzyQuest-XL (DQ-XL).
Conclusion: The DizzyQuest enables the administration of multiple questionnaires during the flow of daily life, therefore increasing reliability and ecological validity. The DQ and DQ-XL, using a big data approach, has the potential to improve precision medicine.
Vestibular dysfunction is very prevalent and can have a big impact on general health and wellbeing. Prevalence rates of vestibular dysfunction vary between 2% in the population below 49 years old, to 32% in individuals aged above 79 years old (Grill et al., 2018). Depending on the severity of the disorder, up to 57% of patients experience difficulties in their social life and anxiety and depressive symptoms frequently occur. Furthermore, the risk to fall increases, possibly with severe injuries as a result (Agrawal et al., 2013; Ganança, 2015). In order to measure severity of vestibular symptoms and their impact on quality of life, a range of questionnaires is currently used: disease-specific questionnaires like the Dizziness Handicap Inventory (DHI), domain-specific questionnaires like the Hospital Anxiety and Depression Scale (HADS) and generic health-related quality of life questionnaires like the EuroQol-5D-5L (EQ-5D-5L) (Kammerlind et al., 2005; Mutlu and Serbetcioglu, 2013; Pelosi et al., 2013; Grigol et al., 2016; Sugaya et al., 2018). These questionnaires have some disadvantages with respect to precise measurement of severity and impact of vestibular disorders. Vestibular disorders like BPPV, vestibular migraine, Meniere's disease and vestibular paroxysmia are characterized by fluctuating symptoms (Lempert et al., 2012; Lopez-Escamez et al., 2015; von Brevern et al., 2015; Strupp et al., 2016) (e.g., attacks). A disease-specific questionnaire focused on symptoms in the last month such as the DHI, may miss or might not be best suited to capture specific fluctuating symptomatology which can be relevant from a therapeutical point of view (Lucieer et al., 2020). Recall bias especially, might significantly impact quality and quantity of reported symptoms (de Joode et al., 2020). Therefore, the Ecological Momentary Assessment (EMA), a measurement strategy in which the same questionnaires are administered multiple times in the flow of daily life (repeated sampling), seems particularly appropriate for the evaluation of vestibular disorders. After all, it eliminates recall bias and is able to capture daily fluctuations. This might provide reliable and detailed insights in self-reported symptoms of vestibular disorders and impact on daily life, which more precisely reflect a real-world setting.
Recently, a complementary tool, the DizzyQuest, was introduced by the DIZZYNET network (Zwergal et al., 2016, 2020; de Joode et al., 2020; Martin et al., 2020, 2022). The aim of the Dizzyquest, an app-based vestibular diary, is to measure the presence and/or intensity of vestibular symptoms and their relation to the conceptual framework of positive health (Huber et al., 2016; Positive Health ZonMw), in the daily flow of life. Several definitions of positive health were previously proposed, varying from “a state far beyond the mere absence of disease” and “wellbeing,” to “resilience” and “capacities” (Bodryzlova and Moullec, 2023). The DizzyQuest uses the definition of positive health as proposed by Huber et al. In this case, positive health is defined as “health contributes to people's ability to deal with the physical, emotional and social challenges in life. And to be in charge of their own affairs, whenever possible.” It comprises six dimensions: bodily functions, mental functions & perceptions, spiritual dimensions, quality of life, social & societal participation, and daily functioning (Huber et al., 2016; Positive Health ZonMw; IfPH, 2020). The DizzyQuest captures the severity and dynamics of vestibular symptoms and their impact on quality of life by using repetitive measurements during daily life using time sampling (morning, within day and evening questionnaires). This EMA measurement strategy is increasingly used in the context of health care as a tool to measure a wide range of health outcomes in an ecological valid way (Csikszentmihalyi et al., 1977; van Os et al., 2017). Since the DizzyQuest involves daily standardized questionnaires which are used in the flow of daily life, recall bias is very low and its ecological validity is expected to be higher than currently used questionnaires for vestibular disorders (Shiffman et al., 2008; Palmier-Claus et al., 2011; Verhagen et al., 2016; van Os et al., 2017). However, although a first version of the DizzyQuest was previously introduced, the development and validity testing of the DizzyQuest has not yet been clearly described. Therefore, the objective of this paper was to describe the development and content validity of the DizzyQuest.
The DizzyQuest was developed and validated in two stages: (1) Development of a concept version of the DizzyQuest based on the conceptual model of positive health, patient interviews, and expert input, and (2) assessment of content validity through a pilot study and focus groups with patients and professionals.
The DizzyQuest aims to measure self-reported presence and/or intensity of vestibular symptoms and their relation to the conceptual framework of positive health (Positive Health ZonMw), in the daily flow of life. To address positive health, questions about vestibular symptoms are accompanied by questions about cognition, emotions, context and stressful events. This allows the study of positive health dimensions: bodily functions, mental functions & perceptions, quality of life, social & societal participation, and daily functioning.
The DizzyQuest was developed for use in all patients with acute, episodic or chronic (or a combination of these) vestibular disorders (Newman-Toker and Edlow, 2015), in whom it is desired from a personal, clinical or scientific point of view, to monitor and evaluate vestibular symptoms with respect to the above mentioned domains of positive health. Requirements for the target population include the ability to read and understand the questions, and being able to operate the application.
To better understand the impact of vestibular disorders on daily life, and which aspects of positive health play an important role, a qualitative research approach using semi-structured interviews with patients was used. Detailed methods and results of the interviews were previously separately described (Lucieer et al., 2020). For the purpose of structurally describing the development and content validity of the DizzyQuest, a brief summary of the methodology is described here (Lucieer et al., 2020). Convenience sampling was used to include participants who reflected a range of the patient population in terms of age, sex and severity of the vestibular disorder that had resulted in bilateral vestibulopathy, according to the Barany Society Criteria (Strupp et al., 2017). They were recruited from the vestibular department of Maastricht UMC+, a tertiary referral center for patients with vestibular disorders.
Individual interviews were conducted face-to-face by a trained interviewer between June 2016 and August 2018. The semi-structured interviews included several open-ended questions with ample room for patients to describe their experiences. The interviewer was free to follow respondent-driven topics. The questions related to experienced symptoms (physical/vestibular, cognitive, and emotional), context (situations and triggers), consequences and behavior, and relationships. The interviews were audio recorded. Verbatim transcription and data analysis was done until saturation was reached. The latter was determined by comparing codes of new transcripts to codes of previous transcripts. After saturation, the remaining interviews were partially transcribed and screened for additional symptoms. All transcribed interviews were coded independently by two researchers, using an open coding approach. The initial codes were compared and in consensus divided into main categories. Subsequently, subcategories were identified independently by the two researchers. It was checked whether the identified subcategories corresponded. In case of disagreement between the two researchers, consensus was reached after reassessing the original data. After that, a thematic analysis was used to classify and organize the data into key themes, resulting a in a conceptual model based on the positive health framework (Lucieer et al., 2020).
Expert meetings were held to develop the DizzyQuest. Participants were included based on their expertise in different professional backgrounds. During the expert meetings, the type of questionnaires to be included in the DizzyQuest, potential questionnaire items, response options, recall period, and lay-out were discussed. The meetings followed a semi-structured interview approach in which a trained moderator (RvdB) systematically followed a list of all potential domains and items to be included in the DizzyQuest. These domains and items were obtained from the interviews with the target population, and from a database that was constructed during more than 30 years of experience with EMA (Csikszentmihalyi et al., 1977; van Os et al., 2017). Relevance and comprehensiveness of each domain and items within the domain were taken into account. The expert meetings were not recorded and transcribed, since modifications were instantaneously incorporated or initiated in consensus by all participants involved. An iterative process followed. Follow-up expert meetings were scheduled to re-evaluate the modifications again, until no modifications were desired anymore by the participants. This was considered as having reached saturation level. Eventually the input from the target population and professionals resulted in the first version of the DizzyQuest, which consisted of four questionnaires to capture symptoms and their psychosocial context: (1) morning questionnaire to evaluate quality of sleep of the past night; (2) within-day questionnaire to evaluate real-time symptoms during the day; (3) evening questionnaire to reflect on symptoms of the past day, and; (4) attack questionnaire to report on symptoms after an attack of vertigo and/or dizziness (Martin et al., 2020). Furthermore, two questionnaires were included to capture baseline patient characteristics: the “patient questionnaire” (to be filled in by the patient) and the optional “doctor questionnaire” (to be filled in by the health care professional). Results could be found in an online result monitor.
A pilot trial was conducted in five patients with various vestibular disorders, including episodic and chronic subtypes, to investigate feasibility of the DizzyQuest and to obtain preliminary feedback about its format and items. They were recruited by “Stichting Hoormij,” a patient association for patients with inner ear disorders in The Netherlands. After initial connection, and approval to participate, patients were contacted by a study team member (SvdW or AE) and received a patient information brochure about the trial. In case patients indicated that they wanted to participate, they were invited for an instruction meeting. During this meeting, patients were instructed about the use of the DizzyQuest by running through the DizzyQuest questionnaires. Written informed consent was obtained prior to start of the trial.
The pilot trial involved using the concept (Dutch) version of the DizzyQuest for a period of 4 weeks. During the trial, each day of the 1st week, the morning (1 time), within-day (10 times) and evening (1 time) questionnaire were administered at different frequencies. The attack questionnaire was only completed after a vertigo attack. The other 3 weeks, only the evening and attack questionnaires were completed. After the trial, patients were contacted by telephone to get feedback about the DizzyQuest. This involved an individual debriefing using two standard debriefing questionnaires. Topics included practicality (ease of use), clarity of the instructions, items, and response options, and whether the items and recall period were relevant and comprehensive. The notes of the interviews and the additional written comments of the patients were discussed in a consensus meeting (SvdW, AE, RvdB). Together, the consensus committee discussed the comments and notes and the DizzyQuest was revised regarding comprehensibility and comprehensiveness, where necessary. This revised version was used in the final steps of the validation described next (Martin et al., 2020).
Two patient focus groups were organized in two separate cities in The Netherlands (Maastricht and Utrecht. Patients with various vestibular disorders and their partners were recruited from the vestibular department of Maastricht UMC+, “Stichting Hoormij” and “Stichting de Negende Van”. The latter is a patient association for patients with DFNA9 (a hereditary autosomal dominant COCH-gene mutation, resulting in progressive vestibulocochlear impairment). The focus groups were led by an experienced moderator (RvdB) who was assisted by two other researchers (EM, LdJ). Both have a medical background and were trained in interviewing patients and extracting relevant information from patient interviews.
During the focus groups, relevance, comprehensibility and comprehensiveness were discussed of all items in the questionnaires (except the doctor questionnaire) and the items in the results monitor. During the focus group interviews, each item was displayed on a large screen for the whole group. In case different options were possible (e.g., visualizing results in a bar or pie chart), all options were explicitly discussed in the group. Specific attention was paid to the intended meaning of response options and on the language used to describe the items. Furthermore, patients and their partners were free to add missing items of topics. The moderator followed-up on responded-driven topics and summarize responses to each item, and subsequently verifying the correctness of the summary with the group. Each focus group lasted around 1 h. Groups were recorded and transcribed verbatim, and two trained researchers (EM, LdJ) independently analyzed the transcriptions for content. A consensus meeting was organized between the two researchers to identify (in)consistencies in their findings, and possible improvements for the DizzyQuest were discussed. Key findings of the focus groups were then discussed with the experts involved in item generation, to reach consensus on the possible changes to be made to the DizzyQuest.
Two focus groups were held to assess relevance and comprehensiveness of the DizzyQuest, as judged by health care professionals. The focus groups were organized during the annual Dizzynet meetings in Germany in 2018 and 2019 (Zwergal et al., 2018, 2019). Before these focus groups, an introductory presentation of 15 min was given by one of the authors (RvdB), and participants got the opportunity to test the DizzyQuest on their devices (e.g., smartphone). The groups were led by the trained moderator (RvdB) who was assisted by one of the authors (JW). Due to the international nature of the audience, a translated version (English) was used. Since these focus groups mainly involved professionals who could use the DizzyQuest in the future, specific attention was paid to the relevance and comprehensiveness of the DizzyQuest in general (e.g., questionnaire items, response options, recall period) and the doctor questionnaire. In the first focus group, the items of the DizzyQuest were discussed using a face-to-face open group discussion. Topics included, among others, the usefulness of having a morning, within-day, evening and attack questionnaire, and which items to incorporate in the doctor questionnaire including patient co-morbidities, vestibular test results and lay-out. In this focus group, only notes were made (by author JW) to be able to incorporate the preliminary changes in the DizzyQuest, as suggested by the professionals. During the second focus group, proposed changes of the DizzyQuest identified in the first focus group with professionals (e.g., developing a less extensive DizzyQuest, leaving out morning- and within-day questionnaire) were discussed. Each item was again discussed regarding relevance and comprehensibility. Possible modifications were discussed until consensus was reached. This second focus group was also not transcribed, since modifications (decided in consensus) were instantaneously made in the word file displayed on the screen. This word file served as input for the DizzyQuest doctor questionnaire.
This study was in accordance with the legislation and ethical standards on human experimentation in the Netherlands and in accordance with the Declaration of Helsinki (amended version 2013). The medical ethical committee of Maastricht UMC+ approved this study (2018-0809) and written informed consent was obtained from all patients participating in a trial.
Results of the input from the patient interviews were already published separately (Lucieer et al., 2020). In sum, 50 patients with bilateral vestibulopathy resulting from different etiologies participated. These etiologies included acute, episodic and chronic vestibular syndromes (Newman-Toker and Edlow, 2015). Gender was equally distributed (25 female, 25 male), and their age ranged from 21 to 79 years old (mean age 60 years). The socio-economic backgrounds differed between patients: in total 32 patients were unemployed (16 retired, 15 on disability and 1 studying) and 18 patients employed (11 full-time and 7 part-time due to illness) (Lucieer et al. manuscript in preparation). A summary of the responses extracted from the study population can be found in Table 1. Regarding symptoms, three main categories were identified: physical, cognitive and emotions. These symptoms were more bothersome while performing certain activities (e.g., cycling or driving a car), leading to feeling limited in these type of activities. Resulting behavior implied slowing down and/or paying more attention while performing activities or avoiding them.
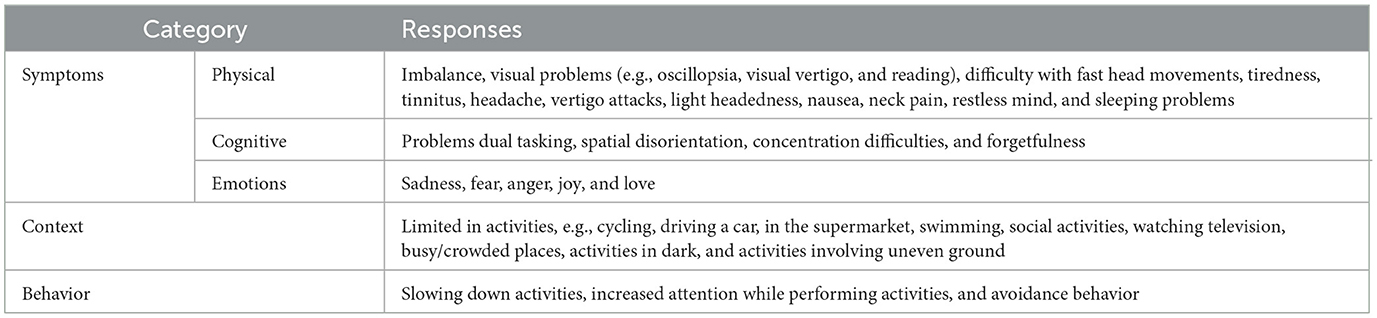
Table 1. Summary of responses extracted from the target population (n = 50) (Lucieer et al., 2020).
The expert meetings involved eight professionals with different specialties (otorhinolaryngology, psychiatry, psychology, EMA, mHealth, and master students of Medicine). Table 2 presents a summary of the main input from the eight participants. In terms of general design, the main topic involved the use of different questionnaires with different sampling types and sampling schedules, in order capture fluctuating neuro-otological symptoms and their psychosocial context as reliable as possible. This included decreasing recall bias using momentary assessment and increasing ecological validity using an app-based platform that can administer questionnaires in the daily flow of life. It was decided to use the app-based platform “UM ESM,” which is an experimental version of the PsyMate™ app (www.psymate.eu) used for research at Maastricht University. It can be downloaded for devices running on Android and iOS. This platform facilitates the administration of multiple questionnaires and sampling schemes (Mujagic et al., 2015; Martin et al., 2020).
Furthermore, it was decided to develop questions that might be able to capture multiple responses at the same time (e.g., asking for “limitation in activities” instead of asking limitation of each activity separately). By this, it was prevented that the questionnaires would become too extensive. After all, questionnaires are administered multiple times and this might be considered a burden (Verhagen et al., 2016) by participants. The number of items were therefore restricted to have an average person fill in the questionnaire in approximately 2 min. This also included avoiding “branching” (i.e., to ask a specific follow-up question, depending on the answer to the previous question, often resulting in additional questions) to a certain extent.
The conceptual model, patient interviews and expert meetings resulted in the first pilot version of the DizzyQuest. This version included a morning questionnaire, within-day questionnaire, evening questionnaire and an attack questionnaire. Sampling schedules as presented in Table 2 were used. Two additional questionnaires were included to capture baseline patient characteristics: the “patient questionnaire” (to be filled in by the patient, 1 time only) and the optional “doctor questionnaire” (to be filled in by the health care professional, 1 time only). Results could be found in an online result monitor.
Five patients with episodic (Meniere's disease, n = 2) and chronic (DFNA9, n = 3) vestibular disorders participated in the pilot trial. Gender was predominantly female (n = 4), mean group age was 52 years old (range 42 to 68 years), and socio-economic backgrounds differed between patients. Table 3 illustrates the summary of responses, extracted from the debriefings of the pilot trial. It can be observed that “becoming more conscious about symptoms” could be considered as a positive as well as a negative factor. Furthermore, additional suggestions were made regarding response options.
In total 11 patients, with various vestibular disorders and different demographic backgrounds participated in the two focus groups. Table 4 illustrates patient characteristics of the two meetings.
During these focus groups, patients mainly addressed the need that the wording of symptoms and triggers mentioned in the DizzyQuest should closely match their complaints and that as many symptoms and triggers as possible should be included.
In general, the items included in the questionnaires were considered relevant. Regarding comprehensibility, suggestions were made to better specify symptoms, e.g., “balance” should also include “feeling drunk,” and “visual problems while moving” should include “recognizing faces, being able to focus, etc.” To improve comprehensiveness, suggestions were made to include additional items, e.g., “vertigo” (in Dutch language, “dizziness” and “vertigo” can be used interchangeably), “fear of falling” and “being bothered by movements and patterns near me.” “Lying down or rolling over in bed” was mentioned as an additional trigger. A summary of the main responses extracted from the two focus groups with patients can be found in Supplementary material 1.
In the two focus groups, more than twenty professionals participated with various backgrounds (otorhinolaryngology, neurology, epidemiology, and physical therapy). Overall, comments were positive regarding relevance, and multiple group members indicated a wish to use the DizzyQuest in the future. Main comments for improvement involved the sampling type and sampling schedule. The sampling schedule with momentary assessment was considered a burden by the professionals and not all of them were convinced about the added value of the morning and within-day questionnaire, especially when using it in clinical context. It was therefore advised to develop two versions of the DizzyQuest: a smaller version (mainly for clinical use) and an extensive version (mainly for research). Furthermore, the Doctor questionnaire was extensively revised to increase comprehensibility and comprehensiveness: e.g., vestibular disorders were categorized into acute/episodic/chronic and additional disorders were included like “motion sickness,” “multicanal BPPV” and “post traumatic injury.” It was also suggested that the DizzyQuest could be combined with other devices that can be used in home setting (e.g., mobile hearing test or video goggles to record nystagmus). A summary of the main responses obtained during these focus groups, can be found in Supplementary material 2.
The step-by-step development process of the DizzyQuest resulted in four questionnaires to capture symptoms and their psychosocial context, which can be used in various combinations: a morning, within-day, evening and attack questionnaire. Two standard packages of the DizzyQuest were developed: the regular DizzyQuest (DQ), which includes the evening and attack questionnaire, and the DizzyQuest-XL (DQ-XL), which administers all four questionnaires. Both the DQ and DQ-XL contain the additional patient and doctor questionnaires to capture baseline patient characteristics, and have the ability to present results in an online monitor. The DizzyQuest can be administered as long as required (e.g., 1 week or 1 year). This depends on the wish of the clinician, patient and/or researcher (Martin et al., 2020; Schenck et al., 2021). The final format of the questionnaires are presented in Supplementary material 3.
This paper provides a detailed description of the development process and content validity of the DizzyQuest, an instrument to evaluate vestibular symptoms with respect to the specific domains of positive health (Positive Health ZonMw). The development of the DizzyQuest was guided by the conceptual framework of positive health, combined with patient interviews, expert meetings, a pilot trial, and focus groups with patients and professionals.
The main feedback from the expert meetings was related to the general design, sampling strategies and sampling schedules: the DizzyQuest should include the administration of multiple questionnaires (morning, within-day, evening and attack questionnaires) during the daily flow of life. Patients mainly addressed the fact that the wording of symptoms and triggers should closely match their complaints and that as many items as possible should be included. Professionals were especially concerned about the burden of the within-day questionnaire (which is administered 10 times a day) and proposed to also develop a shorter DizzyQuest, without all four questionnaires to capture symptoms. This resulted in the development of two versions of the DizzyQuest: the regular DizzyQuest (DQ) including the evening and attack questionnaires, and the more extensive DizzyQuest-XL (DQ-XL), incorporating the additional within-day and morning questionnaires.
The final design of the DizzyQuest (both versions) aims to increase reliability and ecological validity, by using an app-based platform that enables administration of multiple questionnaires during the daily flow of life. This is likely to decrease recall bias and results might more closely reflect daily life experiences (Csikszentmihalyi et al., 1977; van Os et al., 2017). The incorporated questionnaires are administered using a mix of time and event sampling strategies. Additional questionnaires were developed to capture baseline characteristics (patient and doctor questionnaire) and an online result monitor provides insights in reported items. To capture topics relevant to the specific domains of positive health, questionnaire items included: neuro-otologic symptoms, cognition, emotions (including positive and negative affect, agitation), context, and stressful events (mainly activity related). The amount of items was kept relatively low, to prevent unwanted reactivity as much as possible, most likely increasing the adherence to the DizzyQuest (Verhagen et al., 2016). A previous 1 month-trial with a preliminary DizzyQuest demonstrated desired adherence to the DizzyQuest, with response rates of 90%, 62%, and 87%, regarding the morning, within-day- and evening questionnaire respectively (Martin et al., 2020).
Furthermore, lay-out, language and response options are simple, promoting accessibility for patients with low literacy levels (Kimman et al., 2017).
Involvement of professionals in the development of the DizzyQuest resulted in the decision to develop four questionnaires and to use repeated measurements with time and event sampling strategies. This was decided since symptoms of vestibular disorders can occur acutely, episodically and chronically (Newman-Toker and Edlow, 2015). It was therefore preferred that the DizzyQuest would be able to capture fluctuations of symptoms, including attacks of vertigo. Using a time sampling strategy, fluctuations can be measured in time (van Os et al., 2017). It also provides the opportunity to capture non-events: the fact that an event (e.g., vertigo attack) did not happen, is also recorded (Verhagen et al., 2016).
By adding event sampling (attack questionnaire) the DizzyQuest also facilitates capturing very discrete vertigo attacks with little recall bias. After all, the attack questionnaire can be completed directly after an attack, without having to wait until the next questionnaire is administered by the DizzyQuest (e.g., the evening questionnaire). A previous trial with a preliminary DizzyQuest involving more than 60 patients with vestibular disorders, already showed the benefit of having the opportunity to choose between time and event sampling to capture vertigo attacks: depending on the topic, each strategy has its own pros and cons to most reliably investigate the clinical or research question (de Joode et al., 2020). Nevertheless, participants should always be clearly instructed on the definition of the investigated event (e.g., what is considered a vertigo attack).
The aim of this development is to have both the DQ and DQ-XL available for download on devices running on Android and iOS facilitating multiple purposes. Regarding the DQ, clinical care might be complemented and improved by having structured vestibular diaries which capture all important aspects of disease: not only symptoms and triggers, but also their psychosocial context. This could aid the diagnostic process but might also be beneficial for monitoring treatment effect or as part of a personalized intervention itself (Boh et al., 2016), improving precision medicine. Regarding the DQ-XL, the added value would be from a research perspective: using repeated measures during the day, can provide valuable insights in the existence of symptoms and their interaction with environmental and psychosocial factors. This benefit has already been proven in many disorders, including tinnitus and depression (Wenze and Miller, 2010; Hartmann et al., 2015; Broen et al., 2016; Moore et al., 2016; Goldberg et al., 2017). For vestibular disorders, the DQ-XL might for example more reliably capture environmental triggers for symptoms and stress related variability (if any present), than previously attempted (Yeo et al., 2018).
Both versions facilitate generating a large amount of data, which could be valuable when considering a big data approach (2020) to investigate vestibular disorders. Therefore, the DizzyQuest and DizzyQuest-XL will be part of the Dizzynet Network database (Zwergal et al., 2016) in which it is possible to anonymously store relevant data, necessary to improve knowledge and insights in vestibular disorders.
Finally, it was also suggested by the professionals that the DizzyQuest could be combined with wearables, like a mobile hearing test or video goggles to record nystagmus. Based on these suggestions, a preliminary version of the DizzyQuest was already combined with a mobile hearing test. It was illustrated that combining these two is feasible and that differences in self-reported hearing loss severity measured by the DizzyQuest, showed a significant relationship with the individual hearing threshold differences between the two ears of the same patients. This demonstrated the validity of the DizzyQuest in this context (Martin et al., 2022).
Some limitations of this study should be addressed. The main limitation involved the focus groups with patients: most of them were member of a patient association or were planning to join one. This might have induced a selection bias, since members of patients associations are more likely to have chronic complaints (not reflecting the patient population that only suffers from an isolated vertigo episode) and can have lower self-reported quality of life than non-members (Prummer et al., 2019). Nevertheless, this might have also provided a wider range of responses than when interviewing mainly non-members.
It should also be commented that the input from the target population was already previously described. To structurally describing the development and content validity of the DizzyQuest, it was decided to intentionally replicate these findings again in this paper. These findings should therefore not be regarded as “new findings:” they were only included to meticulously show all performed steps during the development of the DizzyQuest.
The DizzyQuest was developed as an instrument to evaluate vestibular symptoms with respect to the specific domains of positive health. Its design has the potential to increase reliability and ecological validity, by using an app-based platform that enables administration of multiple questionnaires during the daily flow of life. Based on input from patients and professionals, two versions of the DizzyQuest were developed: the regular DizzyQuest (DQ: mainly for clinical purposes) and the DizzyQuest-XL (DQ-XL: mainly for research). The DQ and DQ-XL are tools that may to complement and improve precision medicine, using a big data approach.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by the Medical Ethical Committee of Maastricht UMC+ (2018-0809). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
EM: Writing—original draft, Writing—review & editing, Data curation, Investigation, Project administration, Resources. LJ: Data curation, Investigation, Resources, Writing—original draft. FL: Resources, Writing—review & editing, Data curation, Investigation. DS: Data curation, Writing—original draft. PD: Resources, Software, Writing—review & editing. CL: Resources, Software, Writing—review & editing. SW: Resources, Software, Writing—review & editing. AM-E: Writing—review & editing, Resources, Software. EG: Writing—review & editing. AZ: Writing—review & editing. NG: Writing—review & editing. AP-F: Writing—review & editing. VR: Writing—review & editing. JW: Investigation, Writing—review & editing, Supervision. MK: Conceptualization, Validation, Writing—review & editing, Methodology. RB: Conceptualization, Project administration, Resources, Supervision, Writing—original draft, Writing—review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fauot.2024.1378569/full#supplementary-material
IfPH (2020). Available online at: https://www.iph.nl/en/knowledge-base/what-is-positive-health/ (accessd May 03, 2022).
Agrawal, Y., Ward, B. K., and Minor, L. B. (2013). Vestibular dysfunction: prevalence, impact and need for targeted treatment. J. Vestib. Res. 23, 113–117. doi: 10.3233/VES-130498
Bodryzlova, Y., and Moullec, G. (2023). Definitions of positive health: a systematic scoping review. Glob. Health Promot. 30, 6–14. doi: 10.1177/17579759221139802
Boh, B., Lemmens, L. H., Jansen, A., Nederkoorn, C., Kerkhofs, V., Spanakis, G., et al. (2016). An ecological momentary intervention for weight loss and healthy eating via smartphone and Internet: study protocol for a randomised controlled trial. Trials 17:154. doi: 10.1186/s13063-016-1280-x
Broen, M. P., Marsman, V. A., Kuijf, M. L., Van Oostenbrugge, R. J., van Os, J., Leentjens, A. F., et al. (2016). Unraveling the relationship between motor symptoms, affective states and contextual factors in Parkinson's disease: a feasibility study of the experience sampling method. PLoS ONE 11:e0151195. doi: 10.1371/journal.pone.0151195
Csikszentmihalyi, M., Larson, R., and Prescott, S. (1977). The ecology of adolescent activity and experience. J. Youth Adolesc. 6, 281–294. doi: 10.1007/BF02138940
de Joode, L., Martin, E. C., Stultiens, J. J. A., Leue, C., Delespaul, P., Peeters, F., et al. (2020). The DizzyQuest: to have or not to have… a vertigo attack? J. Neurol. 267, 15–23. doi: 10.1007/s00415-020-10043-x
Ganança, M. M. (2015). Vestibular disorders in the elderly. Braz J. Otorhinolaryngol. 81, 4–5. doi: 10.1016/j.bjorl.2014.11.001
Goldberg, R. L., Piccirillo, M. L., Nicklaus, J., Skillington, A., Lenze, E., Rodebaugh, T. L., et al. (2017). Evaluation of ecological momentary assessment for tinnitus severity. JAMA Otolaryngol. Head Neck Surg. 143, 700–706. doi: 10.1001/jamaoto.2017.0020
Grigol, T. A. d. A. E. S., Silva, A. M., Ferreira, M. M., Manso, A., Ganança, M. M., and Caovilla, H. H. (2016). Dizziness handicap inventory and visual vertigo analog scale in vestibular dysfunction. Int. Arch. Otorhinolaryngol. 20, 241–243. doi: 10.1055/s-0035-1567808
Grill, E., Heuberger, M., Strobl, R., Saglam, M., Holle, R., Linkohr, B., et al. (2018). Prevalence, determinants, and consequences of vestibular hypofunction. Results from the KORA-FF4 survey. Front. Neurol. 9:1076. doi: 10.3389/fneur.2018.01076
Hartmann, J. A., Wichers, M., Menne-Lothmann, C., Kramer, I., Viechtbauer, W., Peeters, F., et al. (2015). Experience sampling-based personalized feedback and positive affect: a randomized controlled trial in depressed patients. PLoS ONE 10:e0128095. doi: 10.1371/journal.pone.0128095
Huber, M., van Vliet, M., Giezenberg, M., Winkens, B., Heerkens, Y., Dagnelie, P. C., et al. (2016). Towards a ‘patient-centred' operationalisation of the new dynamic concept of health: a mixed methods study. BMJ Open 6:e010091. doi: 10.1136/bmjopen-2015-010091
Kammerlind, A.-.S. C, Ledin, T. E. A., Skargren, E. I. B., and Odkvist, L. M. (2005). Long-term follow-up after acute unilateral vestibular loss and comparison between subjects with and without remaining symptoms. Acta Otolaryngol. 125, 946–953. doi: 10.1080/00016480510043477
Kimman, M. L., Rotteveel, A. H., Wijsenbeek, M., Mostard, R., Tak, N. C., van Jaarsveld, X., et al. (2017). Development and pretesting of a questionnaire to assess patient experiences and satisfaction with medications (PESaM Questionnaire). Patient. 10, 629–642. doi: 10.1007/s40271-017-0234-z
Lempert, T., Olesen, J., Furman, J., Waterston, J., Seemungal, B., Carey, J., et al. (2012). Vestibular migraine: diagnostic criteria. J. Vestib Res. 22, 167–172. doi: 10.3233/VES-2012-0453
Lopez-Escamez, J. A., Carey, J., Chung, W. H., Goebel, J. A., Magnusson, M., Mandalà, M., et al. (2015). Diagnostic criteria for Menière's disease. J. Vestib. Res. 25, 1–7. doi: 10.3233/VES-150549
Lucieer, F. M. P., Van Hecke, R., van Stiphout, L., Duijn, S., Perez-Fornos, A., Guinand, N., et al. (2020). Bilateral vestibulopathy: beyond imbalance and oscillopsia. J. Neurol. 267, 241–255. doi: 10.1007/s00415-020-10243-5
Martin, E. C., Leue, C., Delespaul, P., Peeters, F., Janssen, A. M. L., Lousberg, R., et al. (2020). Introducing the DizzyQuest: an app-based diary for vestibular disorders. J. Neurol. 267, 3–14. doi: 10.1007/s00415-020-10092-2
Martin, E. C., Verkaik, R., Stultiens, J. J. A., van de Berg, M. R., Janssen, A. M. L., Leue, C., et al. (2022). The DizzyQuest: relation between self-reported hearing loss, tinnitus and objective hearing thresholds in patients with Meniere's disease. J. Neurol. 269, 5239–5248. doi: 10.1007/s00415-021-10909-8
Moore, R. C., Depp, C. A., Wetherell, J. L., and Lenze, E. J. (2016). Ecological momentary assessment versus standard assessment instruments for measuring mindfulness, depressed mood, and anxiety among older adults. J. Psychiatr. Res. 75, 116–123. doi: 10.1016/j.jpsychires.2016.01.011
Mujagic, Z., Leue, C., Vork, L., Lousberg, R., Jonkers, D. M., Keszthelyi, D., et al. (2015). The Experience Sampling Method–a new digital tool for momentary symptom assessment in IBS: an exploratory study. Neurogastroenterol. Motil. 27, 1295–1302. doi: 10.1111/nmo.12624
Mutlu, B., and Serbetcioglu, B. (2013). Discussion of the dizziness handicap inventory. J. Vestib. Res. 23, 271–277. doi: 10.3233/VES-130488
Newman-Toker, D. E., and Edlow, J. A. (2015). TiTrATE: a novel, evidence-based approach to diagnosing acute dizziness and vertigo. Neurol. Clin. 33, 577–599. doi: 10.1016/j.ncl.2015.04.011
Palmier-Claus, J. E., Myin-Germeys, I., Barkus, E., Bentley, L., Udachina, A., Delespaul, P. A., et al. (2011). Experience sampling research in individuals with mental illness: reflections and guidance. Acta Psychiatr. Scand. 123, 12–20. doi: 10.1111/j.1600-0447.2010.01596.x
Pelosi, S., Schuster, D., Jacobson, G. P., Carlson, M. L., Haynes, D. S., Bennett, M. L., et al. (2013). Clinical characteristics associated with isolated unilateral utricular dysfunction. Am. J. Otolaryngol. 34, 490–495. doi: 10.1016/j.amjoto.2013.04.008
Positive Health ZonMw. Available online at: https://www.zonmw.nl/en/research-and-results/positive-health/ (accessd May 03 2022).
Prummer, C. M., Kerezoudis, P., Tombers, N. M., Peris-Celda, M., Link, M. J., Carlson, M. L., et al. (2019). Influence of selection bias in survey studies derived from a patient-focused organization: a comparison of response data from a single tertiary care center and the acoustic neuroma association. Otol. Neurotol. 40, 504–510. doi: 10.1097/MAO.0000000000002151
Schenck, A. A., Kruyt, J. M., van Benthem, P. P., Cannegieter, S. C., van den Hout, W. B., Böhringer, S., et al. (2021). Effectiveness of endolymphatic duct blockage versus endolymphatic sac decompression in patients with intractable Ménière's disease: study protocol for a double-blinded, randomised controlled trial. BMJ Open 11:e054514. doi: 10.1136/bmjopen-2021-054514
Shiffman, S., Stone, A. A., and Hufford, M. R. (2008). Ecological momentary assessment. Annu. Rev. Clin. Psychol. 4, 1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415
Strupp, M., Kim, J. S., Murofushi, T., Straumann, D., Jen, J. C., Rosengren, S. M., et al. (2017). Bilateral vestibulopathy: diagnostic criteria consensus document of the classification committee of the bárány society. J. Vestib. Res. 27, 177–189. doi: 10.3233/VES-170619
Strupp, M., Lopez-Escamez, J. A., Kim, J.-.S, Straumann, D., Jen, J. C., Carey, J., et al. (2016). Vestibular paroxysmia: diagnostic criteria. J. Vestib. Res. 26, 409–415. doi: 10.3233/VES-160589
Sugaya, N., Arai, M., and Goto, F. (2018). Changes in cognitive function in patients with intractable dizziness following vestibular rehabilitation. Sci. Rep. 8:9984. doi: 10.1038/s41598-018-28350-9
van Os, J., Verhagen, S., Marsman, A., Peeters, F., Bak, M., Marcelis, M., et al. (2017). The experience sampling method as an mHealth tool to support self-monitoring, self-insight, and personalized health care in clinical practice. Depr. Anxiety 34, 481–493. doi: 10.1002/da.22647
Verhagen, S. J., Hasmi, L., Drukker, M., van Os, J., and Delespaul, P. A. (2016). Use of the experience sampling method in the context of clinical trials. Evid. Based Ment. Health. 19, 86–89. doi: 10.1136/ebmental-2016-102418
von Brevern, M., Bertholon, P., Brandt, T., Fife, T., Imai, T., Nuti, D., et al. (2015). Benign paroxysmal positional vertigo: diagnostic criteria. J. Vestib. Res. 25, 105–117. doi: 10.3233/VES-150553
Wenze, S. J., and Miller, I. W. (2010). Use of ecological momentary assessment in mood disorders research. Clin. Psychol. Rev. 30, 794–804. doi: 10.1016/j.cpr.2010.06.007
Yeo, N. L., White, M. P., Ronan, N., Whinney, D. J., Curnow, A., Tyrrell, J., et al. (2018). Stress and unusual events exacerbate symptoms in menière's disease: a longitudinal study. Otol. Neurotol. 39, 73–81. doi: 10.1097/MAO.0000000000001592
Zwergal, A., Brandt, T., Magnusson, M., and Kennard, C. (2016). DIZZYNET–a European network initiative for vertigo and balance research: visions and aims. J. Neurol. 263 Suppl 1, S2–9. doi: 10.1007/s00415-015-7912-3
Zwergal, A., Brandt, T., Straka, H., Straumann, D., and Dieterich, M. (2018). DIZZYNET 2018: visions and perspectives of future vestibular research. J. Neurol. 265, 1–2. doi: 10.1007/s00415-018-9041-2
Zwergal, A., Grill, E., Lopez, C., and Dieterich, M. (2019). DIZZYNET 2019: approaching the future of vestibular research. J. Neurol. 266, 1–2. doi: 10.1007/s00415-019-09514-7
Keywords: vestibular disorders, bilateral vestibulopathy (BV), DizzyQuest, ecological momentary assessment (EMA), content validity, positive health
Citation: Martin EC, de Joode LEGH, Lucieer F, Sitters D, Delespaul PAEG, Leue C, van de Weijer SCF, Meijers-Erdkamp A, Grill E, Zwergal A, Guinand N, Perez-Fornos A, van Rompaey V, Widdershoven J, Kimman ML and van de Berg R (2024) Development and content validity of the DizzyQuest. Front. Audiol. Otol. 2:1378569. doi: 10.3389/fauot.2024.1378569
Received: 29 January 2024; Accepted: 24 April 2024;
Published: 10 May 2024.
Edited by:
Eugen Constant Ionescu, Hospices Civils de Lyon, FranceReviewed by:
David Tomé, Polytechnic of Porto (P.Porto), PortugalCopyright © 2024 Martin, de Joode, Lucieer, Sitters, Delespaul, Leue, van de Weijer, Meijers-Erdkamp, Grill, Zwergal, Guinand, Perez-Fornos, van Rompaey, Widdershoven, Kimman and van de Berg. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: R. van de Berg, cmF5bW9uZC52YW5kZS5iZXJnQG11bWMubmw=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.