
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Audiol. Otol. , 16 February 2024
Sec. Clinical Research in Auditory Implants and Hearing Aids
Volume 2 - 2024 | https://doi.org/10.3389/fauot.2024.1362443
 Sho Kurihara1,2*
Sho Kurihara1,2* Akira Ganaha1,3
Akira Ganaha1,3 Takeshi Nakamura1
Takeshi Nakamura1 Kan Kubuki1
Kan Kubuki1 Emi Saruwatari1
Emi Saruwatari1 Koudai Matsui4
Koudai Matsui4 Kuniyuki Takahashi1
Kuniyuki Takahashi1 Tetsuya Tono1,5
Tetsuya Tono1,5Purpose: Bone-conduction devices can be considered a viable treatment option for patients experiencing asymmetric hearing loss (AHL), especially those with severe to profound hearing loss (HL) present in one ear. However, there are only a few reports on the effects of bone-anchored hearing aids (BAHAs) on patients with AHL. This retrospective study analyzed in detail the effects of BAHA on softer sounds than other hearing aids and identified situations in which BAHA had a negative effect.
Methods: Patients with AHL, characterized by severe to profound hearing loss in one ear with a difference of ≥45 dB from that of the contralateral ear, underwent BAHA implantation in the ear with worse hearing. The BAHA effects were evaluated by assessing the word recognition score (WRS) and speech reception threshold (SRT) using the Japanese Oldenburg Sentence Test for various signal settings and noise directions. For a subjective analysis, the Speech, Spatial and Qualities of Hearing Scale (SSQ12) score was determined.
Results: Thirteen patients who underwent BAHA implantation at the Miyazaki University Hospital between 2007 and 2021 were included. The BAHA demonstrated a significant improvement in the WRS from 40 to 70 dB sound pressure levels. Although the SRT showed significant improvement in noisy environments when speech was presented to the BAHA-wearing side, it worsened significantly when noise was presented to this side. In the survey of subjective hearing ability, both the total and subscale SSQ12 scores improved significantly after wearing the BAHA.
Conclusion: This study identified scenarios in which BAHAs were beneficial and detrimental to individuals with AHL. Generally used audiological tests, such as the WRS with fixed sound pressure, may underestimate the effectiveness of BAHAs for softer sounds. In addition, depending on the direction of the noise, BAHAs may have adverse effects. These results could help patients comprehend the potential benefits and limitations of bone-conduction devices for their hearing.
Bone-conduction devices (BCDs) convert sound energy into skull bone vibrations, thereby directly stimulating the cochlea. They have been under development since the 1970s and are widely used in patients with conductive or mixed hearing loss (HL) (Mudry and Tjellström, 2011). Because patients with chronic otitis media or aural atresia have difficulty achieving adequate results with air conduction (AC) hearing aids, BCDs can be an effective treatment option. Moreover, BCDs are a treatment option for single-sided deafness (SSD) because they provide sound input to the contralateral cochlea via bone conduction (BC; Kitterick et al., 2016; Magele et al., 2019). Patients with SSD often have worse sound localization abilities and speech recognition difficulties in noisy and other challenging listening situations due to the loss of binaural processing (Welsh et al., 2004; Yu, 2020). The use of BCDs by patients with SSD improves speech perception and provides subjective benefits (Pfiffner et al., 2009; Wazen et al., 2010; Wesarg et al., 2013; Hampton et al., 2022; Huber et al., 2022). Their effects on speech discrimination in noise have been controversial and dependent on the signal setting and noise direction; however, a systematic review that assessed the efficacy of bone-anchored hearing aids (BAHAs) concluded they have favorable effects based on speech discrimination in noisy circumstances (Kim et al., 2017).
Asymmetric hearing loss (AHL) is a condition similar to SSD. AHL is defined as an interaural asymmetry of 20 dB hearing loss at two contiguous frequencies or 15 dB HL at any two frequencies from 2 to 8 kHz (Gimsing, 2010; Durakovic et al., 2019). For patients with hearing loss who have a large left–right hearing difference, a conventional AC hearing aid is often used in the better hearing ear. For that strategy, patients give up sound source input from the worse hearing ear. Wearing a BCD in the worse ear for patients with AHL may solve this problem. To date, only a few reports on the effect of BCD on patients with AHL have been published; some reports show more favorable results for patients with AHL when compared to patients with SSD (Monini et al., 2020), while others show a deteriorative effect in noise conditions (Schwartz and Kobylk, 2016).
Although these BCD studies of patients with AHL have yielded further insights, they have not been able to fully evaluate the contribution of BAHAs in daily life. In particular, evaluations of the effects of softer sounds, such as whispering voices, are lacking. Most previous studies fixed the sound pressure level of speech signals to a level similar to that encountered in everyday life (65–75 dB) to assess the effects of BCDs on word recognition. However, BCDs can further promote the effect of softer sound stimuli in AHL. Moreover, in some scenarios, listening comprehension is worsened by BCDs when noise is presented to the BCD-wearing side. It is important to know under what circumstances and to what degree hearing performance can be compromised.
This study investigated patients with asymmetric hearing loss, marked by severe to profound hearing loss in one ear with a difference of ≥45 dB from that in the contralateral ear, who underwent implantation on the side with worse hearing. This target group was established because patients with more significant left–right differences in hearing tend to be the ones who have to give up sound input from the worse-hearing ear. A word-recognition test was performed by sweeping the sound pressure from a low speech level (40 dB). Additionally, discrimination of speech in noise was analyzed by changing the directions of the noise and the signal speaker. The findings of this study can provide insights into the use of BCDs in patients with AHL and can be applicable to patients with SSD.
This retrospective study was conducted through a comprehensive review of patient charts. Among the patients who underwent BAHA implantation (Baha Connect System®, Cochlear Ltd., Sydney, Australia) at Miyazaki University Hospital between 2007 and 2021, 13 met the Japanese criteria (Japan Otological Society, 2019), which requires a BC hearing level of < 45 dB HL for Baha 5 sound processor, and underwent BAHA implantation in the ear with the worse hearing. The mean age at the time of implantation was 65 (range 46–80) years. All patients had been using BAHA for at least 6 months. Of the 13 patients, 12 had acquired hearing loss (vestibular schwannoma in 1, cholesteatoma surgery in 6, and chronic otitis media in 5 patients), and 1 had congenital hearing loss. All patients had AHL (differences in threshold averages at 500, 1, 2, and 4 kHz exceeded 45 dB HL). The patient characteristics and pure-tone thresholds are shown in Table 1.
The study was conducted in accordance with the Declaration of Helsinki and approved by the ethics review board of the University of Miyazaki (protocol code O-0702). Informed consent was obtained from all participants involved in the study.
All 13 participants received a Baha 5 sound processor fitted by experienced audiologists using the Baha Fitting Software. The final gain settings were established by measuring the actual thresholds.
The hearing threshold was measured using the BAHA. The inspection sounds were presented using audiometers (AA-H1; Rion, Tokyo, Japan) that met the Japanese Industrial Standards.
To evaluate the word recognition score (WRS), the 67-S (Japanese nonsense monosyllable CD) was evaluated 1 m from the front speaker unit in a shielded room. The responses were obtained by uttering a sound. All speech-perception test grades were calculated as percentages of correct answers. Experienced audiologists performed all tests.
BAHA-aided and unaided conditions were tested with signals presented from the front (0° azimuth) or at the implanted ear (±90° azimuth). To emulate a real-life clinical situation, the contralateral ear was not masked by using a hearing aid when the signal was presented to the implanted ear.
The contralateral ear was covered with earmuffs and ear plugs or masked with narrowband noise during pure-tone and sound-field audiometry and by broadband noise during speech tests. Experienced audiologists determined the requirement for masking.
The Japanese Oldenburg Sentence Test (OLSA) was used to determine speech discrimination in noise. Twenty test sentences per list were presented in random combinations with a fixed scheme (name, adjective, object, number, and verb) using background noise at a sound pressure level (SPL) of 65 dB. The signal-to-noise ratio (SNR), with a 50% correct word score (critical S/N), was achieved by adjusting the SPL for each sentence depending on the response to each test item and was defined as the speech-reception threshold (SRT). The tests were performed with and without the BAHA. To emulate a real-life clinical situation, when presenting the signal to the ear with an implant, the contralateral ear was not masked with a hearing aid if the patient used one.
Sound presentation was applied in three different conditions as follows: (1) Both speech and noise were presented from the front (original setting of OLSA); (2) speech was presented from the side speaker (±90° azimuth) toward the worse-hearing ear, whereas noise was presented from the side speaker (±90° azimuth) toward the better-hearing ear; (3) speech was presented from the side speaker (±90° azimuth) toward the better-hearing ear, whereas noise was presented from the side speaker (±90° azimuth) toward the worse-hearing ear.
The short form (SSQ12) of the Speech, Spatial and Qualities of Hearing scale (SSQ49) in Japanese was used to self-assess hearing disabilities at baseline and when the BAHA was fitted. The SSQ12 had provided results similar to those of the SSQ49 in a previous large clinical study (Noble et al., 2013).
The results were analyzed using PRISM software (GraphPad, La Jolla, CA, USA). The results are presented as the mean ± standard deviation (SD). The significance level was set at 5%. A two-tailed Wilcoxon signed-rank test was used to compare the scores of assessments conducted with and without the BAHA.
The average preoperative pure-tone audiogram and SD for all patients are presented in Figure 1A. The mean AC and BC thresholds of the better-hearing ear were 41.03 (SD 14.51) dB HL and 25.38 (SD 5.977) dB HL, respectively, and those of the worse-hearing ear were 111.9 (SD 17.69) dB HL and 62.18 (SD 9.680) dB HL, respectively.
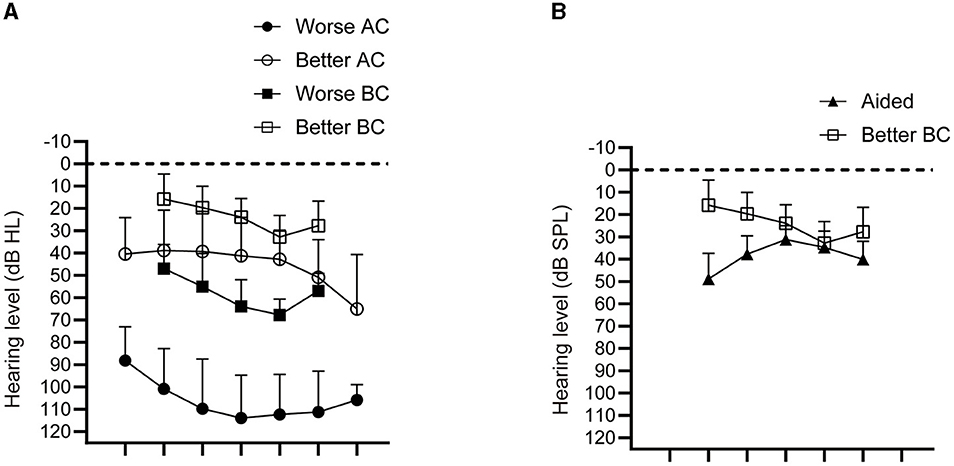
Figure 1. Average hearing and bone-anchored hearing aid (BAHA)–aided thresholds. (A) Average and standard deviation of air conduction (AC) and bone conduction (BC; n = 13). (B) Average and standard deviation of hearing thresholds in the sound field aided by the BAHA by masking the better-hearing ear. The BC threshold of the better-hearing ear is depicted together with the BAHA-aided thresholds (n = 13).
Figure 1B shows the mean hearing thresholds in the sound field aided by the BAHA after masking better-hearing ears. Aided postoperative sound-field thresholds have been reported to correlate with the BC threshold of the better-hearing ear (Pfiffner et al., 2009). Therefore, BC thresholds in the better-hearing ear were compared. Although some deviations were observed in the low-frequency range, the sound-field thresholds in the BAHA group were similar to the BC thresholds of better-hearing ears.
For each patient, the WRS was measured in the aided or unaided condition with varying sound pressure levels. Under each condition, the sound pressure increased until the WRS reached its peak value. WRS plots for each sound pressure are shown in Figure 2A. The maximum WRS (arrow in Figure 2A) did not change with BAHA use. However, the sound pressure at which it reached the maximum WRS (arrowhead in Figure 2A) decreased significantly with BAHA use (Figures 2B, C). Furthermore, we analyzed the effects of the BAHA when the signal was presented from the worse-hearing ear side, which was the aided ear side, in eight patients. The WRS was measured under aided and unaided conditions by varying the sound pressure for stimulus presentation from 40 dB to 80 dB SPL (Figure 3). The results showed that BAHAs significantly improved the WRS at presentation pressures from 40 to 70 dB SPL (40 dB, p = 0.0234; 50 dB, p = 0.0156; 60 dB, p = 0.0156; and 70 dB, p = 0.0156). However, no significant difference was observed for sound presented at 80 dB SPL (80 dB, p = 0.813).
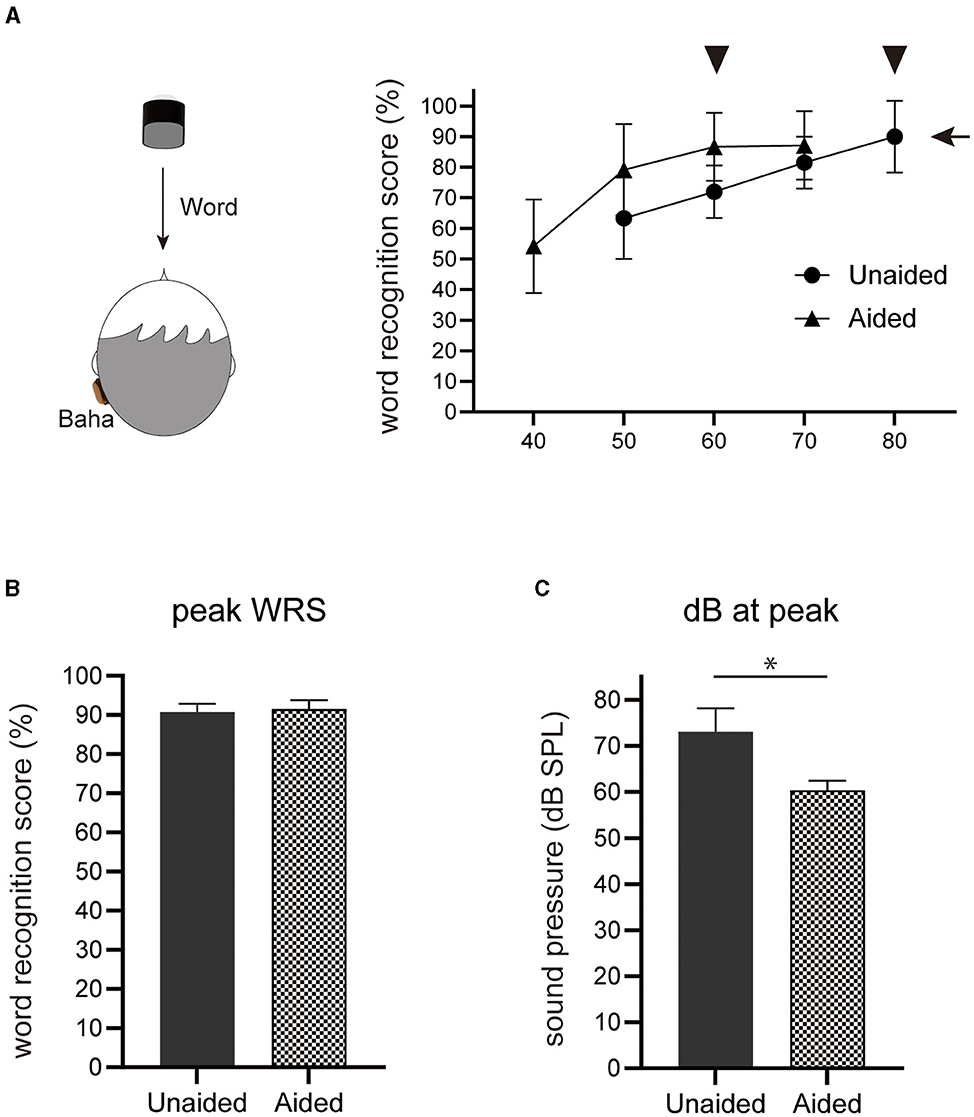
Figure 2. Word recognition score (WRS) under varying presented sound pressures. (A) Schematics of the speaker setting and WRS curve depicted by varying the presented word signal. An arrow indicates the maximum WRS, and the arrowheads indicate the hearing level (n = 13). Note that the measurement of WRS utilized a monosyllable word list. (B) The average and standard deviation of the maximum WRS (n = 13). (C) The average and standard deviation of the threshold in the maximum WRS (n = 13). *p < 0.05.
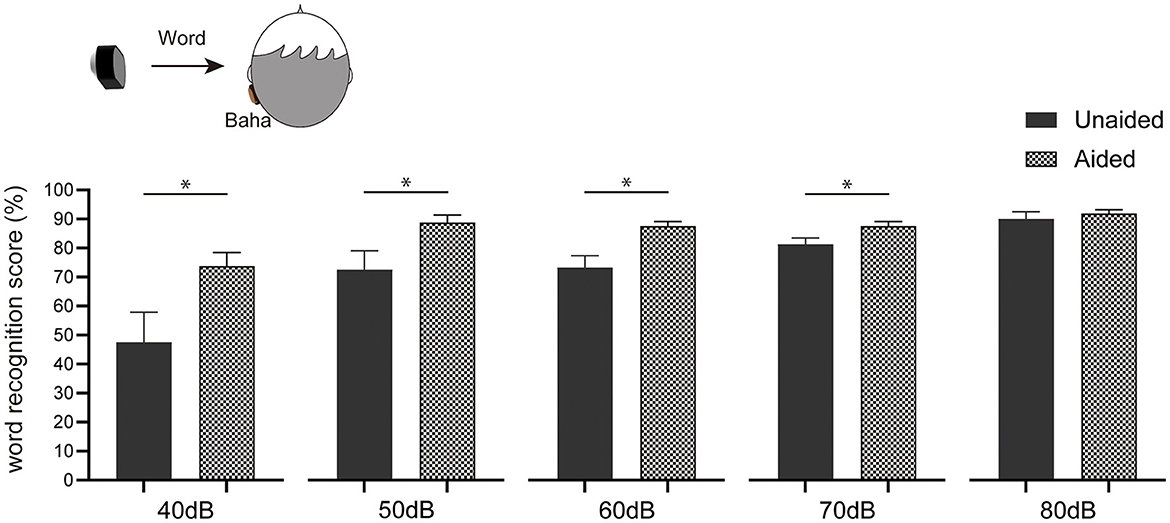
Figure 3. Word recognition score analyzed by setting the signal from the worse-hearing ear. From 40 dB to 80 dB SPL, word signals were presented from the worse-hearing ear (n = 8). *p < 0.05.
This study aimed to explore the impact of BAHAs on auditory function in challenging noisy environments. Specifically, adding to the original OLSA setting by presenting both speech and noise from the front (0°), we analyzed advantageous scenarios, that is, when speech was presented from the side speaker (±90°) toward the worse-hearing ear and noise was presented from the side speaker (±90°) toward the better-hearing ear. We also analyzed the disadvantageous scenario, that is, when speech was presented from the side speaker (±90°) toward the better ear and noise was presented from the side speaker (±90°) toward the worse-hearing ear. To emulate a real-life clinical situation, when presenting a signal in the ear with an implant, the contralateral ear was not masked and had a hearing aid if the patient used one. Of the 13 patients, 6 underwent the test. The results showed that, in the original OLSA setting, no difference was observed in the SRT due to the use of BAHAs (p = 0.750; Figure 4A). In the advantageous scenario, where speech was presented from the BAHA-wearing side, the SRT significantly improved (p = 0.031; Figure 4B) but significantly worsened when noise was presented from the BAHA-wearing side (p = 0.031; Figure 4C).
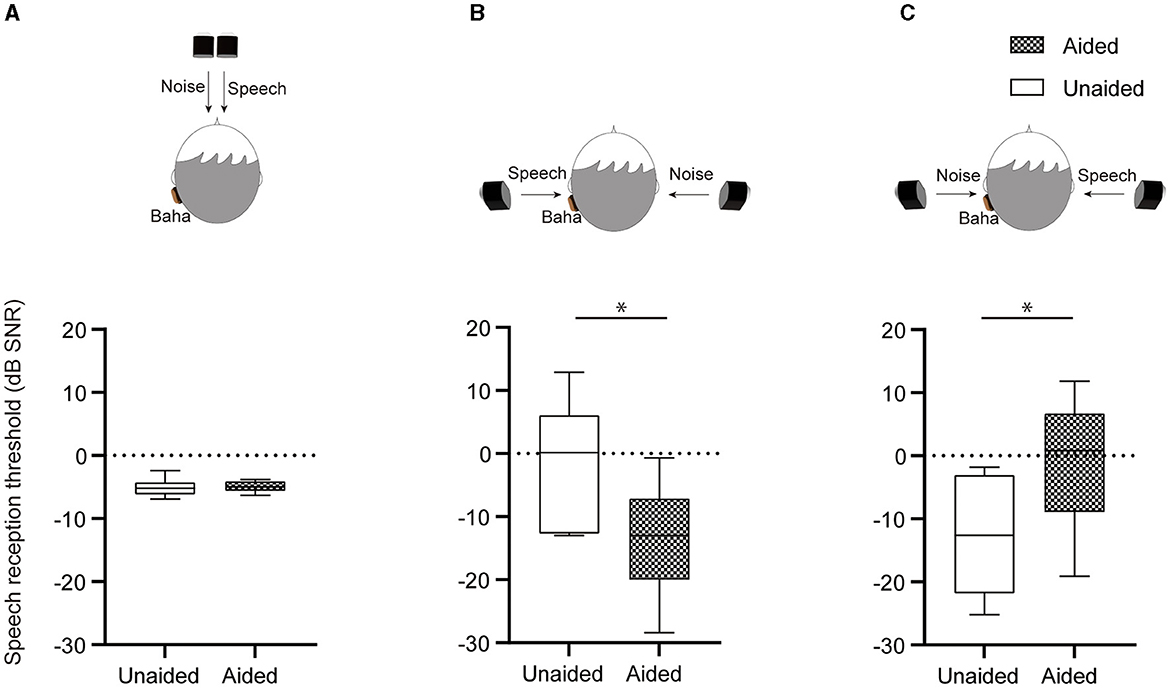
Figure 4. Speech discrimination in noise test. (A) In the original Japanese Oldenburg Sentence Test (OLSA) setting, both speech and noise are presented from the front (0°; n = 6). (B) Possible advantageous scenario: Speech is presented from the side speaker (±90°) toward the worse-hearing ear, and noise is presented from the side speaker (±90°) toward the better-hearing ear (n = 6). *p < 0.05. (C) Possible disadvantageous scenario: Speech is presented from the side speaker (±90°) toward the better-hearing ear, and noise is presented from the side speaker (±90°) toward the worse-hearing ear (n = 6). *p < 0.05.
SSQ12 items can be categorized into the following three subcategories: speech, spatial, and quality. Moreover, significant differences were observed in all categories (Figure 5).
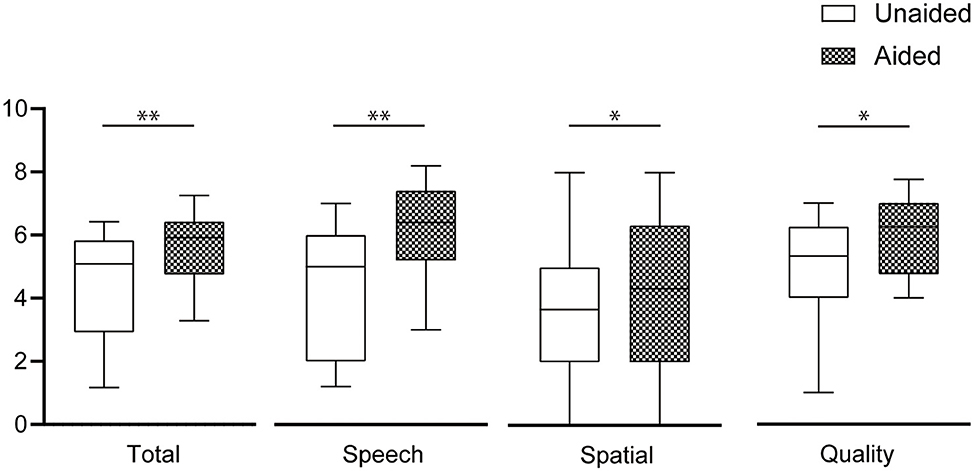
Figure 5. Subjective assessment of the Speech, Spatial and Qualities of Hearing Scale (SSQ12). The averages and standard deviations of the total items and the three subgroups (speech, spatial, and quality) have been calculated separately (n = 11). *p < 0.05, **p < 0.01.
The present investigation assessed the efficacy of BAHAs in individuals with hearing impairment, specifically in those with asymmetric hearing loss. In this study, asymmetric hearing loss was characterized by severe to profound hearing loss in one ear with a difference of >45 dB between the hearing abilities of the left and right ear. In such conditions, patients tend to give up sound input from the worse-hearing ear. Among the 13 subjects included in this study, 4 individuals were already using a hearing aid in their better-hearing ear (as indicated in Table 1). For the monosyllable word recognition test, the tests were carried out without the use of hearing aids. This approach was specifically chosen to examine the pure effect of BAHAs on hearing capabilities in patients with asymmetric hearing loss. By comparison, the speech discrimination in noise test was conducted with the use of hearing aids. This decision was made to simulate more realistic everyday scenarios. These audiological tests ensure a comprehensive evaluation of the BAHA's impact, both in controlled environments without hearing aids and in more practical settings with the hearing aids in use. The WRS curves were depicted by changing the sound pressure of the word signal from 40 to 80 dB SPL, depending on the hearing ability of the patient. Although the maximum WRS did not change, the sound pressure at which the maximum WRS was achieved was significantly reduced with the use of the BAHA. A WRS of 60 dB SPL was observed in approximately 65% and 85% of the patients without BAHAs and with BAHAs, respectively (Figure 2A). While previous investigations typically assessed WRS using a fixed sound pressure for the presented word, Pfiffner et al. (2009) utilized varying sound pressures (50, 65, and 80 dB SPL) to measure WRS. Despite lacking specific details regarding these values, their study demonstrated that the use of BAHAs was associated with improved WRS, at low and high sound pressure levels. These findings are consistent with the results of our investigation.
The WRS was measured by presenting the word from the BAHA-wearing side, that is, the worse-hearing ear, to analyze the effects of the BAHA in a situation where the most preferred effect was expected (Figure 3). The sound pressure of the word presentation was varied from 40 to 80 dB SPL. The results showed that the WRS significantly improved with BAHAs over a wide range of sound pressures for the presented word. This suggested that BAHAs pick up sound sources from the worse-hearing ear side and help patients recognize soft to ordinary speech sound levels. These results also indicated that measuring the effects of BCDs by varying the sound pressure of the presented word signal is useful for ensuring a more objective analysis of how BCDs affect patient hearing in various situations. Few studies have investigated the effect of BAHAs on AHL, and the left–right difference in hearing observed in participants in previous studies has been smaller than that in the participants in this study. Monini et al. (2020) used interaural threshold difference ≧15 dB HL, and Bruschini et al. (2020) used interaural asymmetry of 20 dB hearing loss at two contiguous frequencies or 15-dB HL at any two frequencies from 2 to 8 kHz as a selection criterion for eligible patients. Consequently, this study scrutinizes and compares its findings with those of previous comparable studies on SSD, which is a similar condition.
In the analysis of the SRT in noise, no significant differences were observed in the original OLSA settings (Figure 4A). Although previous studies of patients with SSD have reported that BCDs improve the SRT when speech and noise are presented from the front, a simple comparison is difficult because of the different testing procedures conducted. For example, the hearing-in-noise test (Niparko et al., 2003), monosyllabic word list (Andersen et al., 2006), and simplified Hirsch tests (Saroul et al., 2013) have been used. A recent report assessing the effects of BONEBRIDGE, a transcutaneous BCD, in patients with SSD used the OLSA to test speech discrimination in noise and found results similar to those of this study (no significant difference between patients with and without BONEBRIDGE; Huber et al., 2022). In our study, we used extreme scenarios to assess the efficacy of the BAHA. In the scenario where the BAHA was most effective, speech was presented to the side containing the BAHA implant (the worse-hearing ear), and noise was presented to the better-hearing ear. The SRT improved significantly under these conditions. Conversely, for the scenario in which the BAHA could yield negative effects, noise was presented to the BAHA-wearing side (the worse-hearing ear), and speech was presented to the better-hearing ear. The SRT decreased significantly under these conditions.
A few reports have shown negative results with BAHAs for patients with SSD. Hol et al. (2010) reported that the SNR worsened with the BAHA when the signal was presented from the front and noise was presented from the BAHA-wearing side. The results obtained in this study suggest that the current BAHA system can negatively affect listening performance in certain situations. Whether the OLSA is suitable for measuring the effects of BAHAs under noisy conditions remains an issue that should be considered. Although discontinuous noise is applied in the OLSA, a relatively steady noise is considered to be applicable in real life. In the case of steady and continuous noise, the noise reduction function of a sound processor may be effective.
Both the total and subscale SSQ12 scores improved significantly with the BAHA. The mean differences in speech hearing, spatial hearing, and speech quality were 1.873, 0.7273, and 0.9394, respectively. Greater improvement in the speech-hearing subscale reflected WRS improvement. A meta-analysis of the effects of BCDs on the quality of life of patients with SSD concluded that BCDs improved the Abbreviated Profile of Hearing Aid Benefits and the SSQ but not the Health Utilities Index-3 (Hampton et al., 2022). In the same study, the mean difference was 2.03 for speech and 1.51 for spatial hearing, indicating a greater improvement than that obtained in the present study. Although objective assessments indicated that BCDs do not enhance sound localization in individuals with SSD (Kim et al., 2017), it is plausible that BCDs may affect spatial hearing ability, which cannot be measured using existing audiological evaluations.
This study had several limitations. First, BAHAs are not approved for use by individuals with SSD, which is the most common cause of severe asymmetric hearing loss, in Japan. Therefore, our findings cannot be directly compared with those of other SSD investigations. Second, the sample size was small; therefore, we were unable to perform subgroup analyses based on patients' hearing abilities. Moreover, not all tests could be conducted on every patient, further limiting the comprehensiveness of our study results. Finally, the subjective evaluation was insufficient. Only a simplified version of the questionnaire, the SSQ12, was used, which was inconsistent with an objective evaluation.
However, this study revealed the advantages of BAHA implantation in the worse-hearing ear while also highlighting the possibility of worsened hearing in noisy environments. These findings can assist clinicians in deciding whether surgical intervention is feasible, considering a patient's typical environment. It can also enable patient education regarding the potential negative consequences of BAHAs and permit them to adjust the device according to the situation. Nevertheless, additional research with a larger sample size is required to understand the effects of BAHA implantation in worse-hearing ears fully. This study examined the effects of a BCD in patients with asymmetric hearing loss who wore a BCD in the worse-hearing ear and the situations in which the device seemed beneficial and non-beneficial. We found that the BAHA device significantly improved patients' WRS under a sound pressure level of 40–70 dB SPL. Conversely, it may worsen the hearing performance in situations where noise is present on the BCD-wearing side. The findings of this study yield insights into the use of BCDs in patients with asymmetric hearing loss, including SSD. Moreover, this information could help patients comprehend the potential benefits and limitations of BCDs for their hearing.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by the Ethics Review Board of the University of Miyazaki (protocol code O-0702). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin because Informed consent was obtained in the following structured manner. Upon receiving approval from the Ethics Committee of the Faculty of Medicine at the University of Miyazaki, the research team disseminated detailed information about this clinical study via the university's website. This included: (i) the purpose and significance of the study, the subjects involved, and the methods employed, including the type of information utilized; (ii) the name of the implementing organization, the individual responsible for the study, and contact information for queries or complaints; (iii) the approach for managing personal information, encompassing aspects of information disclosure. This study information remained publicly accessible from the time of the Ethics Committee's approval until the conclusion of the study period. The lack of objections from study participants or their representatives was interpreted as implied consent. Opt-out Procedure: Participation in the study was entirely voluntary. In the event of a participant's decision to withdraw, all information gathered about that participant up to that point would be, as a general rule, destroyed. However, the data could be retained and used if consent was expressly given by the participant. After public dissemination of the data, such as through academic presentations or publications, destruction of the data is not feasible.
SK: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing—original draft, Writing—review & editing. AG: Conceptualization, Formal analysis, Investigation, Writing—original draft, Writing—review & editing. TN: Formal analysis, Investigation, Writing—review & editing. KK: Investigation, Writing—review & editing. ES: Investigation, Writing—review & editing. KM: Investigation, Writing—review & editing. KT: Investigation, Writing—review & editing. TT: Conceptualization, Writing—review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by JSPS KAKENHI Grant 22K16914 awarded to TN.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Andersen, H. T., Schrøder, S. A., and Bonding, P. (2006). Unilateral deafness after acoustic neuroma surgery: subjective hearing handicap and the effect of the bone-anchored hearing aid. Otol. Neurotol. 27, 809–814. doi: 10.1097/01.mao.0000227900.57785.ec
Bruschini, L., Canelli, R., Morandi, A., Cambi, C., Fiacchini, G., Berrettini, S., et al. (2020). Bone anchored hearing aids for the treatment of asymmetric hearing loss. J. Int. Adv. Otol. 16, 313–317. doi: 10.5152/iao.2020.8879
Durakovic, N., Valente, M., Goebel, J. A., and Wick, C. C. (2019). What defines asymmetric sensorineural hearing loss? Laryngoscope. 129, 1023–1024. doi: 10.1002/lary.27504
Gimsing, S. (2010). Vestibular schwannoma: when to look for it? J. Laryngol. Otol. 124, 258–264. doi: 10.1017/S0022215109991423
Hampton, T., Milinis, K., Whitehall, E., and Sharma, S. (2022). Association of bone conduction devices for single-sided sensorineural deafness with quality of life: a systematic review and meta-analysis. JAMA Otolaryngol. Head Neck Surg. 148, 35–42. doi: 10.1001/jamaoto.2021.2769
Hol, M. K., Kunst, S. J., Snik, A. F., Bosman, A. J., Mylanus, E. A., and Cremers, C. W. (2010). Bone-anchored hearing aids in patients with acquired and congenital unilateral inner ear deafness (Baha CROS): clinical evaluation of 56 cases. Ann. Otol. Rhinol. Laryngol. 119, 447–454. doi: 10.1177/000348941011900704
Huber, A. M., Strauchmann, B., Caversaccio, M. D., Wimmer, W., Linder, T., De Min, N., et al. (2022). Multicenter results with an active transcutaneous bone conduction implant in patients with single-sided deafness. Otol. Neurotol. 43, 227–235. doi: 10.1097/MAO.0000000000003418
Japan Otological Society (2019). Indication criteria for bone-anchored hearing aids (Baha® System). Available online at: https://www.otology.gr.jp/ (accessed January 28, 2023).
Kim, G., Ju, H. M., Lee, S. H., Kim, H. S., Kwon, J. A., et al. (2017). Efficacy of bone-anchored hearing aids in single-sided deafness: a systematic review. Otol. Neurotol. 38, 473–483. doi: 10.1097/MAO.0000000000001359
Kitterick, P. T., Smith, S. N., and Lucas, L. (2016). Hearing instruments for unilateral severe-to-profound sensorineural hearing loss in adults: a systematic review and meta-analysis. Ear. Hear. 37, 495–507. doi: 10.1097/AUD.0000000000000313
Magele, A., Schoerg, P., Stanek, B., Gradl, B., and Sprinzl, G. M. (2019). Active transcutaneous bone conduction hearing implants: systematic review and meta-analysis. PLoS ONE. 14:e0221484. doi: 10.1371/journal.pone.0221484
Monini, S., Battilocchi, L., Salerno, G., Filippi, C., and Barbara, M. (2020). Bone conductive implantation in asymmetric hearing loss (AHL). Acta Otolaryngol. 140, 651–658. doi: 10.1080/00016489.2020.1752396
Mudry, A., and Tjellström, A. (2011). Historical background of bone conduction hearing devices and bone conduction hearing aids. Adv. Oto-Rhino-Laryngol. 71, 1–9. doi: 10.1159/000323569
Niparko, J. K., Cox, K. M., and Lustig, L. R. (2003). Comparison of the bone anchored hearing aid implantable hearing device with contralateral routing of offside signal amplification in the rehabilitation of unilateral deafness. Otol. Neurotol. 24, 73–78. doi: 10.1097/00129492-200301000-00015
Noble, W., Jensen, N. S., Naylor, G., Bhullar, N., and Akeroyd, M. A. (2013). A short form of the speech, spatial and qualities of hearing scale suitable for clinical use: the SSQ12. Int. J. Audiol. 52, 409–412. doi: 10.3109/14992027.2013.781278
Pfiffner, F., Kompis, M., and Stieger, C. (2009). Bone-anchored hearing aids: correlation between pure-tone thresholds and outcome in three user groups. Otol. Neurotol. 30, 884–890. doi: 10.1097/MAO.0b013e3181b4e8eb
Saroul, N., Akkari, M., Pavier, Y., Gilain, L., and Mom, T. (2013). Long-term benefit and sound localization in patients with single-sided deafness rehabilitated with an osseointegrated bone-conduction device. Otol. Neurotol. 34, 111–114. doi: 10.1097/MAO.0b013e31827a2020
Schwartz, S. R., and Kobylk, D. (2016). Outcomes of bone anchored hearing aids (Baha) for single sided deafness in nontraditional candidates. Otol. Neurotol. 37, 1608–1613. doi: 10.1097/MAO.0000000000001225
Wazen, J. J., Van Ess, M. J., Alameda, J., Ortega, C., Modisett, M., and Pinsky, K. (2010). The Bahaystem in patients with single-sided deafness and contralateral hearing loss. Otolaryngol. Head Neck Surg. 142, 554–559. doi: 10.1016/j.otohns.2009.12.047
Welsh, L. W., Welsh, J. J., Rosen, L. F, and Dragonette, J.E. (2004). Functional impairments due to unilateral deafness. Ann. Otol. Rhinol. Laryngol. 113, 987–993. doi: 10.1177/000348940411301209
Wesarg, T., Aschendorff, A., Laszig, R., Beck, R., Schild, C., Hassepass, F., et al. (2013). Comparison of speech discrimination in noise and directional hearing with 2 different sound processors of a bone-anchored hearing system in adults with unilateral severe or profound sensorineural hearing loss. Otol. Neurotol. 34, 1064–1070. doi: 10.1097/MAO.0b013e31828bb781
Keywords: asymmetric hearing loss, bone-conduction hearing aid, hearing in noise, Japanese-Oldenburg Sentence Test, speech spatial qualities of hearing scale
Citation: Kurihara S, Ganaha A, Nakamura T, Kubuki K, Saruwatari E, Matsui K, Takahashi K and Tono T (2024) Pros and cons of a bone-conduction device implanted in the worse hearing ear of patients with asymmetric hearing loss. Front. Audiol. Otol. 2:1362443. doi: 10.3389/fauot.2024.1362443
Received: 28 December 2023; Accepted: 29 January 2024;
Published: 16 February 2024.
Edited by:
In Seok Moon, Yonsei University Health System, Republic of KoreaReviewed by:
Sten Olof Martin Hellström, Karolinska Institutet (KI), SwedenCopyright © 2024 Kurihara, Ganaha, Nakamura, Kubuki, Saruwatari, Matsui, Takahashi and Tono. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sho Kurihara, c2t1cmloYXJhQGppa2VpLmFjLmpw
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.