
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Audiol. Otol., 05 March 2024
Sec. Tinnitus
Volume 2 - 2024 | https://doi.org/10.3389/fauot.2024.1322596
This article is part of the Research TopicTinnitus Tools and Protocols for Effective Clinical PracticeView all 11 articles
Introduction: Combination devices offering both amplification and sound therapy are commonly used in tinnitus management. However, there is insufficient evidence supporting the relationship between sound therapy and tinnitus outcomes. The aim of this study was to explore longitudinal effects of sound therapy on tinnitus-related distress using a combination device.
Method: Twenty participants with mild to moderate tinnitus related distress were fitted with combination devices that included three sound-therapy programs. The sound-therapy programs were selected by the participants from the available sounds offered in the combination device. The sounds comprised fractal music, nature sounds and combinations of the two. Participants were asked to wear the devices for 12 months and to complete questionnaires related to tinnitus distress at baseline and 1, 2, 4, 6, and 12 months after starting the treatment. Additionally, at 2, 4, 6, and 12 months, the device log data capturing information about amplification and sound-therapy use were collected.
Results: Tinnitus handicap inventory (THI), tinnitus functional index (TFI), tinnitus awareness and annoyance decreased following the device fitting. This improvement plateaued at 4 months. The degrees of improvement in THI, TFI and tinnitus annoyance were correlated with daily hours of sound-therapy use but not with daily hours of amplification-only or total device use.
Conclusions: A combination sound therapy consisting of therapy sounds, amplification as needed, and counseling was associated with a reduction in tinnitus-related distress. A future randomized controlled trial should be conducted to allow for detangling the effect of sound therapy from effects of amplification, counseling, placebo, and time itself, and to investigate the predictors of sound-therapy benefit and use.
Tinnitus refers to perception of noise without any external stimuli (Baguley, 2002). It affects ~10–15% of adults (Gallus et al., 2015; McCormack et al., 2016; Biswas et al., 2022), with about 20% of the affected population experiencing symptoms that negatively affect quality of life (Jastreboff and Hazell, 1993; Davis et al., 2000; Sereda et al., 2018). The most common problems associated with tinnitus are stress, concentration difficulties, insomnia, and decreased speech discrimination (Axelsson and Sandh, 1985). The available evidence indicates that various tinnitus management programs offer distinct advantages. Among these, Cognitive Behavioral Therapy (CBT), which aims at reducing one's negative response to tinnitus, is considered a favorable approach for tinnitus treatment (Tunkel et al., 2014; Makar et al., 2017). Sound therapy, hearing aids and combination devices (amplification and sound therapy within one device) area also constituent of many tinnitus management programs, and together with information and counseling are the primary choice for tinnitus management in audiology departments (Sereda et al., 2018).
Several studies have shown that sound therapy is an effective method to decrease the tinnitus-related distress, emotional reaction to and awareness of tinnitus (Kuk et al., 2010; Sweetow and Sabes, 2010; Krick et al., 2015; Liu et al., 2021). Sound therapies were initially based on broadband noise but now include noise shaped according to the audiogram (Henry et al., 2015), narrowband signals focusing on the frequency of tinnitus (Hoare et al., 2014b), notch noise (Jin et al., 2021), nature sounds (Barozzi et al., 2016; Sereda et al., 2017), music (Krick et al., 2015), or fractal tones (Tyler et al., 2017). Fractal tones are semi-randomly generated tones that sound like wind chimes. These tones utilize harmonic but unpredictable tonal sequences. They are pleasant and relaxing but not associated with music that the listener can remember, thus a greater likelihood of passive (rather than active) listening is induced. The spectrum and level of these tones compensate for the in-situ hearing loss of the wearers (Tyler et al., 2017). The variety of available sound types can accommodate different user needs as the degree to which users like the tones has been shown to relate to improvements in tinnitus distress (Jørgensen, 2022). Although the mechanisms behind sound therapy leading to tinnitus improvement are unknown, it has been hypothesized that sound therapy reduces tinnitus intrusiveness, promotes habituation to tinnitus and distracts attention from tinnitus (Henry et al., 2008; Newman and Sandridge, 2012). It has, however, also been speculated that the effects of sound therapy on tinnitus improvement may be facilitated by counseling and not necessarily by the sound stimulation itself (Mackenna and Irwin, 2008).
As hearing loss is a common comorbidity of tinnitus (Baguley et al., 2013), hearing aids are frequently used for the management of tinnitus (Surr et al., 1999; Kochkin and Tyler, 2008; Trotter and Donaldson, 2008; Searchfield et al., 2010). It has been discussed that the beneficial effects on tinnitus from hearing aids may be related to amplified volume of external sounds which may mask the tinnitus sound or refocus attention on alternative auditory stimuli that are unrelated to the tinnitus sound (Del Bo and Ambrosetti, 2007; Hoare et al., 2014a). Nonetheless, there is not sufficient evidence to support or refute the hypothesis that hearing aids are beneficial as a standard treatment for tinnitus (Hoare et al., 2014a; Sereda et al., 2018).
Due to association between hearing loss and tinnitus, devices that combine the benefits of amplification and sound stimulation have become increasingly popular. Most modern hearing aids have integrated sound generators that can deliver customized sounds and/or various noise signals to the individual with tinnitus. Several clinical studies have shown both short- and long-term beneficial effects of combination devices on treatment of tinnitus (Sweetow and Sabes, 2010; Johansen et al., 2014; Sweetow et al., 2015a; Tyler et al., 2017; Sanders et al., 2023). However, it has been difficult to disentangle whether the benefits are due to sound-therapy use, amplification, device use in general or other placebo effects. Randomized controlled trials that included combination devices and amplification-only devices concluded that both are effective for tinnitus treatment (Oz et al., 2013; Henry et al., 2015, 2017). Henry et al. (2017) further concluded that there is insufficient evidence that one type of device offers greater relief from tinnitus than the other.
The mixed findings are likely related to sound therapy, amplification-only or combination devices not being effective for everyone. Not everyone is equally responsive to a given treatment, and some people experience tinnitus relief with these interventions while others do not (Sweetow and Sabes, 2010; Tyler et al., 2017). People have individual preferences for auditory stimuli selected for providing tinnitus relief (Henry et al., 2004) and liking of the sound stimulation may also play a role (Jørgensen, 2022). Furthermore, positive effects on tinnitus-related distress may be related to combination strategies (amplification, sound therapy and counseling).
The primary aims of this study were to explore (1) the effects of sound therapy on tinnitus-related distress when participants choose a selection of the three sounds they want implemented in a combination device and (2) relationship between improvement in tinnitus outcome and sound-therapy use, amplification-only use, and total device use time. A secondary aim was to explore what types of sounds were the most preferred and used in real life.
Ethical clearance for conducting the study was obtained from the Research Ethics Committee of the Capital Region of Denmark (case no. 21070949).
Twenty participants, four with normal hearing and 16 with various degrees of hearing loss, were included in the study. Out of the 16 participants with hearing loss, seven were experienced hearing aid users. That is, 13 participants were first-time hearing aid users at the start of the study. Participants signed up for the study with tinnitus, and not hearing loss, as the primary complaint. However, the better-ear four-frequency pure-tone average (4fPTA) revealed that nine of the participants who were not hearing aid users at the time had some degree of hearing loss. Four participants had previously tried fractal-tone sound therapy—two were experienced hearing aid users who tried it as a special program in own hearing aids, one with hearing loss who tried it in borrowed hearing aids, and one with normal hearing who tried it in a previous study. For an overview of participants' personal and clinical characteristics, please see Table 1. Participants' audiograms are depicted in Figure 1.
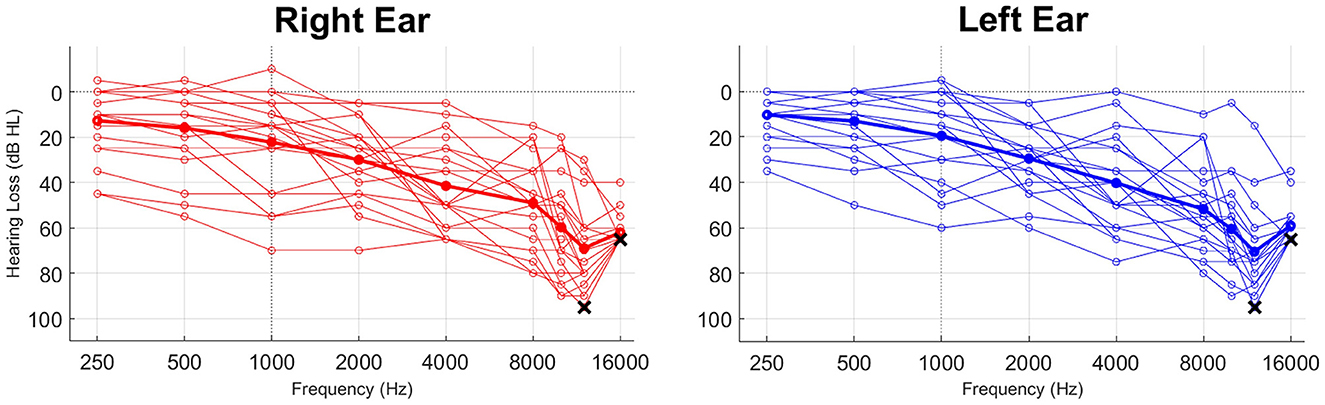
Figure 1. Participant audiograms. The bold lines represent average audiograms across all participants. All participants had some degree of hearing loss in high frequencies (>8 kHz). Two participants could not detect any sound at 12 kHz and fifteen participants could not detect any sound at 16 kHz. This figure shows the highest presented levels for these participants (95 dB HL at 12 kHz and 65 dB HL at 16 kHz)—depicted by the black x.
The inclusion criteria were: ≥18 years of age, chronic tinnitus (experienced for more than 6 months), tinnitus handicap inventory (THI) score between 18 and 70, and willingness to commit to the required tasks and study duration. The participants were recruited via (1) a database of participants by conducting a search for the ones who matched the inclusion criteria and (2) an announcement on the company intranet. The announcement stated that participants with bothersome tinnitus (buzzing or ringing in the ears) were needed for a tinnitus study that investigated the potential benefits of sound therapy over 12 months. The announcement further stated that participants would be required to come to the laboratory three times in the beginning of the study and four times over the course of the year following device fitting.
All the candidates for the study were emailed a Microsoft Forms link to the THI questionnaire, which they were asked to complete up to 2 days prior to Visit 1. If they did not submit it before arrival, they were given the opportunity to complete the questionnaire at the laboratory. If participants filled out questionnaires in the laboratory, they were given the space to do so without interference from the audiologist—this is the case for all the subsequent visits as well.
The participants were informed about the study orally and in writing. Before the trial commenced, the participants gave their written informed consent.
The study consisted of seven visits to the laboratory (Widex HQ, Lynge, Denmark). The 1-year field trial commenced at Visit 3. The study flow is depicted in Figure 2 and each part of the study is described in detail below.
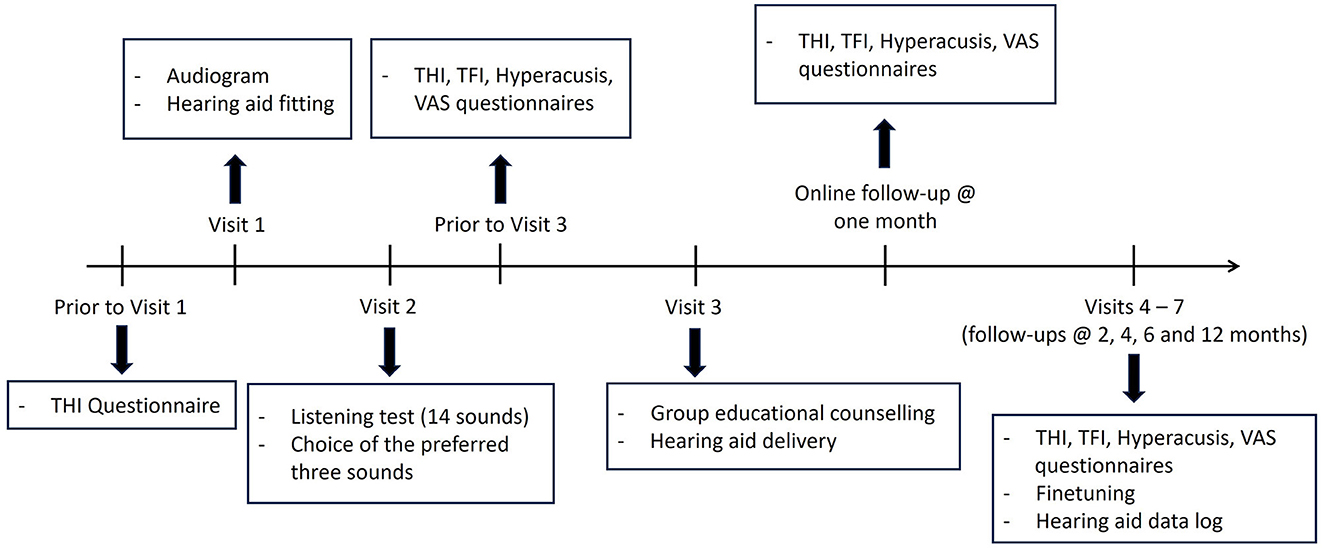
Figure 2. The study flow. THI, tinnitus handicap inventory; TFI, tinnitus functional index; VAS, visual analog scale.
At the first visit, participants underwent anamnesis followed by audiometry which included both air conduction (between 250 and 16,000 Hz) and bone conduction (between 500 and 4,000 kHz). Participants were then fitted bilaterally with MOMENT 440 RIC 312 hearing aids. The hearing aids were fitted to the participant's hearing loss using Compass GPS (version 4.4) according to the fitting recommendations (Schmidt, 2018). Hearing aid finetuning, if needed, was done based on the audiologist's clinical experience. Verification of fitting outcomes was not performed. The participants who had normal hearing at frequencies < 8 kHz were fitted with a flat 15 dB hearing loss. Receivers and ear tips were selected according to the recommendations in the fitting software. The participants did not start wearing the hearing aids until after Visit 3 (see below).
Visit 2 occurred ~1 month after the first visit. At the second visit, the sound-therapy programs were added to the fitted hearing aids, and the participants were asked to listen to all available sounds consisting of six fractal tones, two nature sounds, and six soundscapes (combination of fractal tones and nature sounds), for ~1–3 min each. The microphone by default was on for sound therapy programs, hence amplification within the program was based on the hearing loss. The 14 sounds were presented in a random order. Using visual analog scales (VAS), participants were asked to rate how much they liked listening to the sound (1 = not at all, 10 = very much) and how relaxing the sound was to listen to (1 = not relaxing at all, 10 = very relaxing). All participants rated at least three sounds as ≥5 on both liking and relaxation.
Once all the sounds had been evaluated, participants were asked to choose their three favorite sounds and describe the reasons behind their choice. Then, they listened to each of these sounds for 10 min and afterwards rated on a scale from 1 (not at all) to 10 (very much) how relaxed they felt while listening to the sounds, if the sounds made them feel good, and how aware and annoyed they were by their tinnitus while listening to the sounds. The three final programs consisting of the participants' three favorite sounds were included in the fitted hearing aids that were delivered at Visit 3. The microphone in the three programs was turned off for the two participants who had normal hearing at frequencies < 8 kHz. The volume of the sound-therapy programs was based on the audiogram. If needed, the volume of the tones was adjusted such that the sound could be the most optimal for the user. The universal (amplification-only) program was always the default one.
Two days prior to the laboratory visit, all participants were e-mailed a pdf attachment with THI, tinnitus functional index (TFI) questionnaire, hyperacusis questionnaire and baseline VAS questionnaire assessing relaxation, concentration, mood and tinnitus over the past week. The THI and TFI questionnaires were selected due to their widespread use in evaluating tinnitus outcomes. Additionally, the VAS questions were administered to assess aspects that were not covered by the two aforementioned questionnaires. As there was a 3-month time span between Visit 1 and Visit 3, THI was administered again here as the baseline for the longitudinal trial. The VAS questions and scales are presented in the Supplementary Table 1. The participants submitted the completed questionnaires either via e-mail or when they arrived at the laboratory. They were given an opportunity to fill out the questionnaires at this visit if they did not submit them before coming to the laboratory.
Visit 3 was a group session, participants attended in groups of 6–7 persons. During this visit, participants received group educational counseling regarding the etiologies of tinnitus, relation between tinnitus and stress, the purpose of sound stimulation and how to use the sound therapy and amplification. The counseling session lasted 1.5 h. Participants were then handed the hearing aids fitted at Visit 1 and 2 and were asked to listen to any of the sound-therapy programs for 2–4 h per day but at least 2 h per day. If participants had a hearing loss, they were further instructed that they should also use the amplification-only program for at least 8 h a day. The 13 participants who had not used amplification before were advised to start with 4 h of daily amplification use and increase gradually to ≥8 h during the first month. All participants received a remote control that they could use to adjust the volume of sound therapy, independent of amplification. After 1 week, the responsible audiologist followed up with the participants to ensure that they were using the hearing aids as instructed.
Participants were e-mailed the THI, TFI, Hyperacusis and VAS questionnaires as pdf attachments 1 month after receiving the hearing aids (Visit 3). The participants then either e-mailed back the completed questionnaire or mailed/dropped off to the physical address. VAS questions were the same ones as administered prior to Visit 3 (Supplementary Table 1).
Participants were e-mailed the THI, TFI, Hyperacusis and VAS questionnaires as pdf attachments 2 days before the follow-up visit. Participants came to the laboratory for a follow-up ~2, 4, 6, and 12 months after receiving their hearing aids (Visit 3). At these visits, participants submitted the completed questionnaires that they either filled out at home up to 2 days before arrival or in the laboratory. The participants were further asked about their experience with the hearing aids and sound therapy so far. If needed, adjustments to the fitting or sound-therapy programs were done. In some cases, the order of the programs was changed to address the participant's preferences. Eleven participants required the microphones to be turned off in at least one sound-therapy program as they found that too much sound was provided by the microphone—they preferred to only hear the sound therapy and not amplification. Hearing aid log data including the wear time and percentage of time spent in each program were captured at each follow-up visit. At the 2-month follow-up, it was revealed that eleven participants had not used the sound therapy for 2–4 h per day as recommended. For these participants, instruction of sound therapy use, to help with tinnitus-related distress, was reinforced.
The sample size of twenty participants is in line with other explorative studies that investigated longitudinal effects of sound therapy on tinnitus-related outcomes (Sweetow and Sabes, 2010; Herzfeld et al., 2014; Sweetow et al., 2015b; Tyler et al., 2017).
Mixed-effects linear regression with random effects of participant ID was used to assess the effect of time on the outcome variables. The reference time category was baseline. Hearing loss was included as a covariate, as the changes in tinnitus outcomes may be related to the degree of hearing loss. The residuals were visually inspected to ensure they fit an approximately normal distribution and meet the homoscedasticity criterion. When homoscedasticity was violated, regression with robust standard errors was conducted.
Spearman correlation analyses were performed to assess the relationship between improvement in the tinnitus outcome variables and sound-therapy, amplification, and total device use. The improvement values were calculated as the difference between each post-baseline assessment and the baseline assessment. The longitudinal improvements in each individual outcome and device use values were averaged within each participant for correlation analyses.
No adjustments for multiple comparisons were done; the Althouse (2016) guidelines were followed instead. These guidelines state that, rather than controlling for multiple comparison, the best approach is to (1) describe what was done; (2) report effect sizes, confidence intervals, and p-values; and (3) let readers use their own judgment about the relative weight of the conclusions.
Interval data are presented as mean ± standard deviation, unless otherwise noted.
P < 0.05 was considered significant.
All the statistical analyses were done in Stata (v. 15, StataCorp, College Station, TX, USA).
Sixteen participants successfully completed the 1-year trial. Four participants dropped out after the 2-month follow-up. Of these, three participants had some degree of hearing loss, one was experienced hearing aid user, and none had previous sound therapy experience. Two participants dropped out because they did not feel that sound therapy was helping them—one with normal hearing and one experienced hearing aid user. These participants managed their tinnitus better with other strategies. Two participants stopped responding and we failed to reach them despite multiple attempts. All the available data were analyzed, including the dropouts up until the point they decided to stop the trial.
The VAS ratings for the three preferred sounds at Visit 2 were 7.7 ± 1.0 for liking and 7.5 ± 1.4 for relaxation. Sound preferences varied between participants and the most common reasons given for preferences were that the sound was relaxing, calming, comfortable or distracted from tinnitus (see Supplementary Table 2). The fractal tones were selected as the preferred sounds in 42% of cases (chosen at least once by twelve participants), soundscapes were selected in 36% of cases (chosen at least once by thirteen participants) and nature sounds were selected in 22% of cases (chosen at least once by nine participants). After listening to the selected sounds for 30 min collectively, the participants rated them high on the relaxation (7.7 ± 1.3, range: 5–10), feeling good (7.7 ± 1.3, range: 5–9), reduction of tinnitus awareness (7.1 ± 1.6, range: 3–10) and reduction of tinnitus annoyance (7.0 ± 1.5, range: 3–9) scales. Ratings for concentration were somewhat lower: 5.7 ± 1.6, range: 2–8. The high ratings for relaxation, feeling good, reduction of tinnitus awareness and annoyance are in line with participants' descriptors for why they chose these sounds.
Figure 3 shows how participants used their devices, with more detailed statistics shown in Supplementary Table 3. Both sound-therapy and total device use tended to increase after the 2-month follow-up, although this change was not significant. The device and sound-therapy use declined after the 6-month follow-up. This decline in use did not occur for amplification-only. For most of the wear time, the device was used for the sole purpose of amplification (~55% of time). However, when participants listened to sound therapy, fractal tones were the most often listened to on a group level (see Figure 3; Supplementary Table 3).
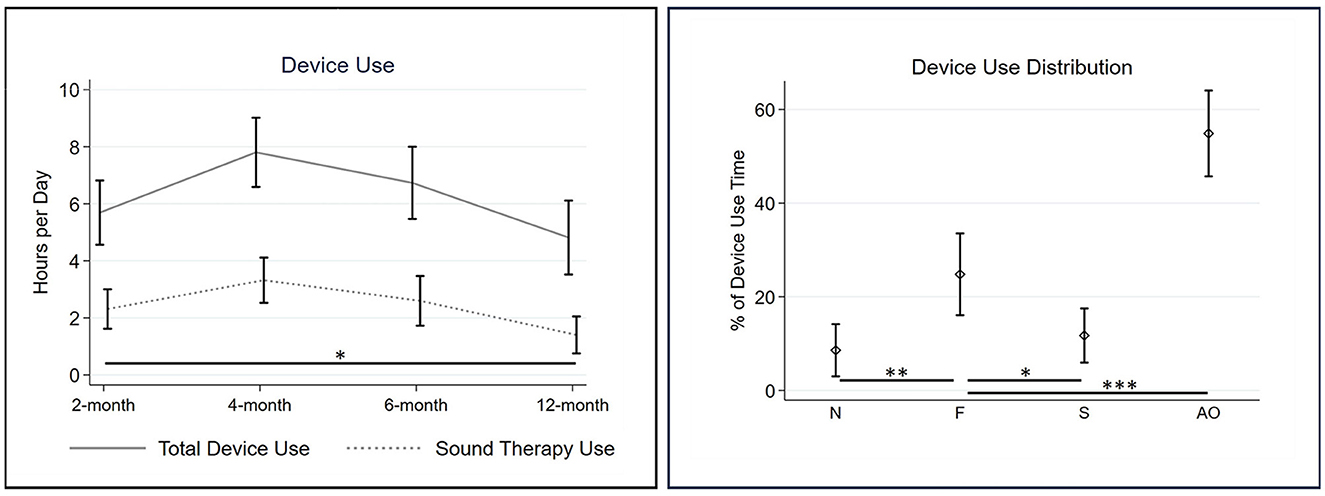
Figure 3. Device use based on hearing aid log data. The (left) shows the number of hours that the device and sound therapy were used as captured at the four follow-up visits. The (right) shows the proportion of time participants listened to nature sounds (N), fractal tones (F), combination soundscapes (S) or used the device for amplification only (AO) over the entire wear time. The error bars represent standard errors of the mean. Significant differences relative to the reference category in the regression model are denoted by asterisks (*P < 0.05; **P < 0.01; ***P < 0.001).
Participants showed significant improvement in THI at the 1-month follow-up and continued improving until the 4-month follow-up where the scores plateaued (Figure 4, detailed statistics in Supplementary Table 4). TFI scores tended to improve at the 1-month follow-up, but the improvement achieved significance at the 2-month follow-up. Clinically meaningful improvement on the THI scale is seven points (Zeman et al., 2011), whereas on the TFI scale, it is 13 points (Meikle et al., 2012). On average, such an improvement occurred already at 1 month on the THI scale (7.1 ± 6.4, range: −4 to 20), whereas it occurred at 4 months on the TFI scale (17.4 ± 13.3, range: 1.6–45.6). The maximum improvement in TFI was also at 4 months, whereas in THI it was at 6 months (12.4 ± 14.7, range: −6 to 56). Tinnitus awareness, annoyance, loudness, relaxation, concentration and mood significantly improved at the 4-month follow-up. This effect persisted throughout the 12-month follow-up for tinnitus awareness, annoyance and relaxation (see Figure 5, detailed statistics in Supplementary Table 4).

Figure 4. THI and TFI scores at baseline and the five follow-ups. Lower scores indicate better ratings. The error bars indicate standard errors of the mean. Significant improvements at follow-up visits relative to baseline are denoted by asterisks (**P < 0.01; ***P < 0.001). BL, baseline; 1-M, 1-month follow-up; 2-M, 2-month follow-up; 4-M, 4-month follow-up; 6-M, 6-month follow; 12-M, 12-month follow-up.
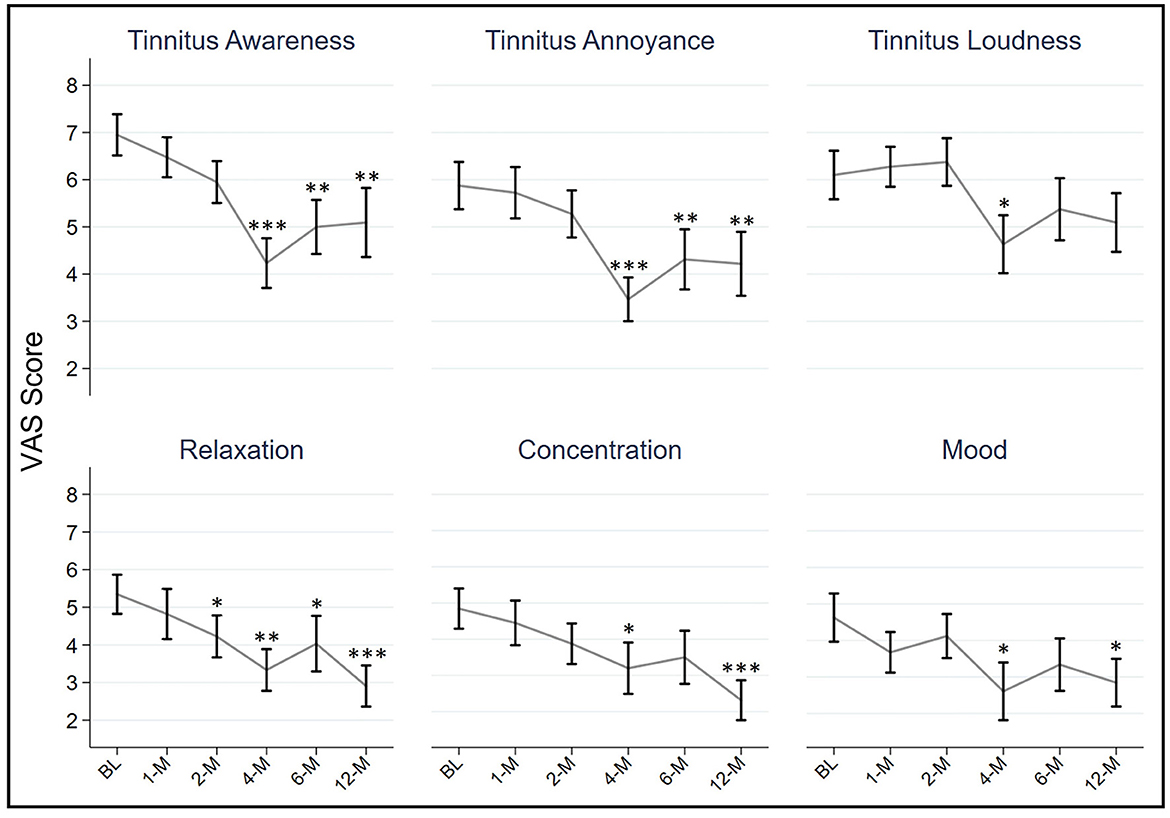
Figure 5. VAS scores for tinnitus awareness, tinnitus annoyance, tinnitus loudness, relaxation, concentration and mood. Lower scores indicate better ratings. The error bars indicate standard errors of the mean. Significant improvements at follow-up visits relative to baseline are denoted by asterisks (*P < 0.05; ** P < 0.01; ***P < 0.001). BL, baseline; 1-M, 1-month follow-up; 2-M, 2-month follow-up; 4-M, 4-month follow-up; 6-M, 6-month follow; 12-M, 12-month follow-up.
Improvements in THI, TFI and tinnitus annoyance were correlated with sound-therapy use but not with amplification-only use or total device use (see Table 2; Figure 6). There was a borderline significant correlation between improvement in TFI and total device use time (P = 0.05)—attributed mainly to sound-therapy use time, as the correlation with amplification-only was non-significant. There was also a borderline significant correlation (P = 0.05) between improvement in relaxation and sound-therapy use. Improvements in other tinnitus outcomes were not related to sound-therapy, amplification, or total device use. The improvements in tinnitus were not related to the type of sound therapy participants listened to the most (see detailed statistics in Supplementary Table 5).
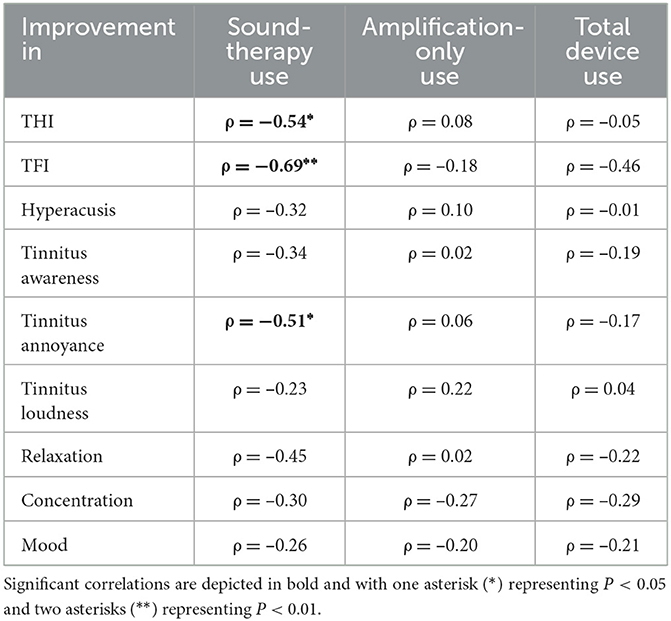
Table 2. Spearman correlations between improvement in the measured tinnitus outcome and sound-therapy use, amplification-only use, and total device use.
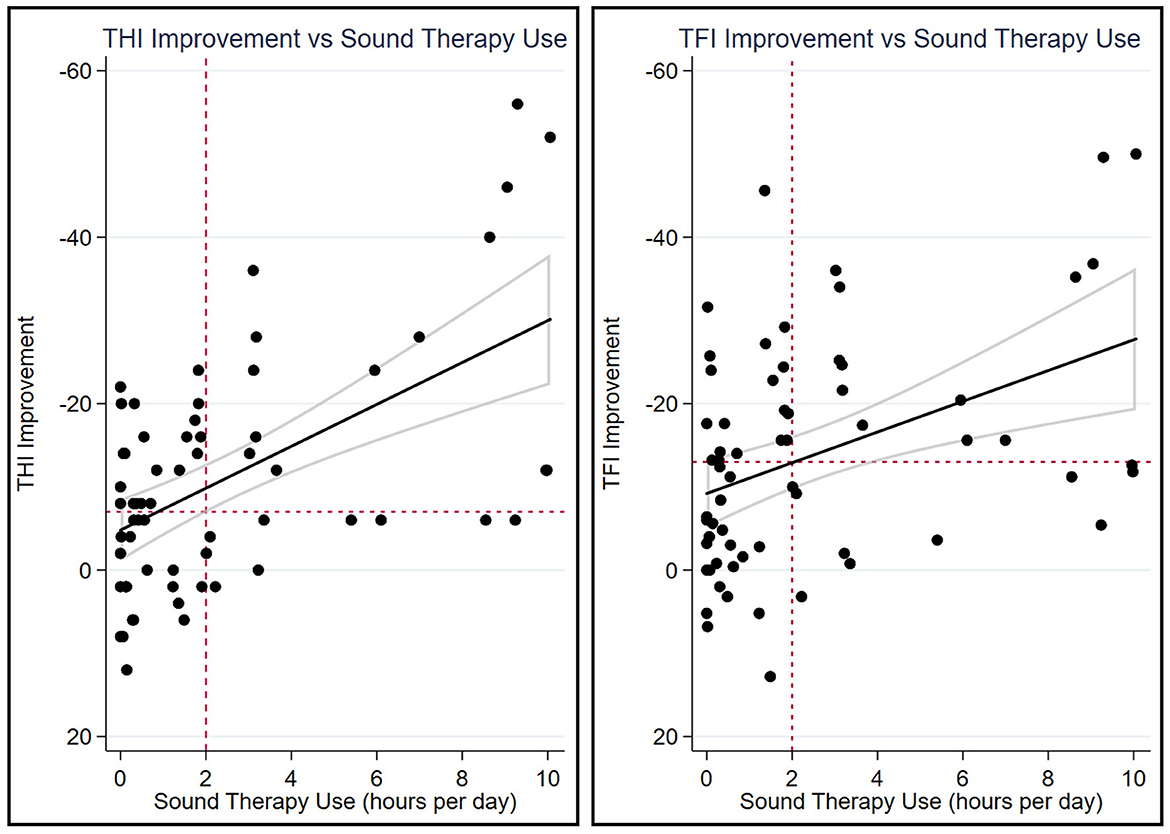
Figure 6. Scatter plot of THI improvement (left) and TFI improvement (right) vs. sound-therapy use. Datapoints from all measurement points (2, 4, 6, and 12 months) are plotted, although the correlation analyses were done on average improvement vs. average sound-therapy use. The black diagonal lines are the lines of best fit and the areas outlined by gray lines depict the 95% confidence intervals of the lines of best fit. The horizontal dashed lines denote the clinically meaningful improvement of seven points in THI and 13 points in TFI. The vertical dashed lines denote the instructed minimum 2 h per day listening time.
In Figure 6, it can be seen that, in many cases, participants did not listen to the sound-therapy programs at least 2 h per day as instructed. The hearing aid log data revealed that 13, 7, 11, and 12 participants used sound-therapy programs < 2 h per day at 2-, 4-, 6-, and 12- month follow-ups, respectively. It should be noted that those who used sound therapy at least 2 h per day at any of the four measurement points (N = 11) rated the three sounds at Visit 2 as 7.3 ± 0.6 across the five assessments after listening to the sounds for 30 min. On the other hand, those who used sound therapy < 2 h per day at all the measurement points (N = 8) rated the sounds as 6.5 ± 1.0 after the 30-min listening task (difference: 0.8, 95% CI: −1.6, −0.03; P = 0.04, t-test). This suggests that those who like the sounds in a first listening session are also more likely to use them consistently and, in turn, achieve the benefit associated with sound therapy use. However, the differences are not large, so ruling out sound therapy based on a short listening session is unlikely to make clinical sense.
The results of the current study indicate that a combination device together with counseling is effective for treatment of tinnitus. These results are in line with previous studies that investigated the effects of combination devices on tinnitus distress (Sweetow and Sabes, 2010; Herzfeld et al., 2014; Johansen et al., 2014; Stocking and Stecker, 2016; Henry et al., 2017; Tyler et al., 2017; Sanders et al., 2023). The effects of the combination device in this study are already evident after 1 month of treatment but peak at 4 months. Further, we showed that the experienced improvements in THI, TFI and tinnitus annoyance are associated with sound-therapy use but not with amplification-only or total device use time. Sweetow et al. (2015b) found that when sound therapy was delivered via hearing aids without amplification together with instructional counseling, tinnitus distress was significantly alleviated. On the other hand, when only instructional counseling was given, improvements in tinnitus distress were not observed. Similarly, Jørgensen et al. (2022) conducted a study investigating the effect of long-term (2-months) sound therapy delivered via hearing aids with no amplification and no tinnitus counseling and found that the sound-therapy intervention reduced THI scores. Although sound therapy in the current work was often accompanied by amplification due to the microphone being turned on, the previous findings together with our correlation results indicate that sound therapy seems to play a pivotal role in easing tinnitus distress with a combination device.
The improvements in THI (12.4) and TFI (17.4) scores are lower in this study compared to what was previously observed in studies utilizing combination devices (Herzfeld et al., 2014; Johansen et al., 2014; Sweetow et al., 2015a; Stocking and Stecker, 2016; Henry et al., 2017; Tyler et al., 2017). The previous studies observed a reduction of 18–30 points in THI and 26–28 points in TFI. A potential reason for lower improvement scores in our study could be the lower baseline THI (37) and TFI (46) scores in comparison to the aforementioned studies that had baseline average THI scores in the range of 49–51 and average TFI scores in the range of 53–62. It has previously been demonstrated that the magnitude of improvement in THI is related to baseline THI scores—the patients that show greater degree of tinnitus show a greater reduction in comparison to those that have lower baseline THI scores (Henry et al., 2006; Newman and Sandridge, 2012; Johansen et al., 2014). The sample size in our study is too small to explore the relationship between the degree of improvement and baseline THI scores as only eight participants had a score that was at least moderate (≥38). Another reason for lower degree of improvement in the current study could be that counseling and hearing aid delivery were done in group sessions, rather than individually as done in previous studies. When participants came back for the 2-month follow-up and instruction on sound-therapy use was reinforced, it was evident that this played a role in improvement of tinnitus-related outcomes at the 4-month follow-up, where the improvement on various scales spiked. It should also be noted that we included all the participants in our analyses, even if they did not use the sound therapy as instructed. But it is clear from the correlation analyses that the degree of measured benefit on THI and TFI is tied to sound-therapy use. Those that used the sound therapy more hours per day experienced more benefit. This relationship has been observed before (Jin et al., 2022). Hence, the non-compliant participants in our study likely pulled the average down.
In line with THI and TFI improvements, the VAS scores for tinnitus awareness, annoyance and loudness were improved. Furthermore, participants' wellbeing—as measured by VAS scores for relaxation, concentration and mood—improved as well. Other than the relaxation score which already improved at the 2-month follow-up, the VAS scores reached a significant improvement at the 4-month follow-up. Here, as mentioned earlier, it seems that the reinforcement of instruction on sound therapy use at the first physical follow-up at 2 months after the hearing aid delivery was effective. We also observed that the average hours of sound-therapy and device use peaked at the 4-month follow-up. The improvements in tinnitus-related VAS outcomes persisted throughout the 12-month period, although for tinnitus loudness the effect at 12-months was slightly above the significance level. This may be because, although the combination-device can alleviate distress related to tinnitus, the loudness of the tinnitus is more constant.
Both sound-therapy and overall device use were significantly lower at 12-months relative to the 2-month follow-up. This decrease may be related to participants experiencing their tinnitus distress reduce over time and no longer feeling the need to use the device. In fact, although the sound-therapy use was decreased, this did not seem to have a detrimental effect on the tinnitus outcomes at 12 months. Considering that most participants had some degree of hearing impairment, the overall device use was particularly low (6.2 h per day on average). This could be because most participants signed up for the study due to problems with tinnitus and not due to problems with hearing. Although it was discovered that most had a hearing loss, they likely did not feel it as severe enough to warrant a greater use of the device.
The participants in the current study had varying preferences of sounds and sound types, and while the fractal tones were used the most (likely due to being the most selected sound-therapy programs), the type of sound did not influence tinnitus outcomes. From this, it is clear that one size does not fit all, and it is important to offer a variety of sounds for tinnitus relief and let the user choose the most optimal ones based on how relaxing, calming or comfortable they are. It seems important that the user likes the sound and can see the potential benefit. We observed that participants who did not use sound therapy at least 2 h per day rated the final chosen sounds at Visit 2 lower than the participants who used the sound therapy as advised (as measured during at least one follow-up visit).
In addition to improvements in THI, TFI and tinnitus annoyance being related to sound-therapy use, there was a borderline significant relationship between improvement in relaxation and sound-therapy use. This relationship is particularly interesting as the most frequent descriptor for the chosen sounds is that they were “relaxing.” This could be another indicator of the importance of choosing the sounds that induce the desired effect already after brief listening.
The most general clinical implication of this study is that offering sound therapy to people suffering due to tinnitus can alleviate some of the associated distress. However, it is important that the sound therapy is accompanied by counseling and that the user chooses the sound they prefer and like from a variety of available sounds. Information about how to use the sound therapy and the benefits of using it as advised should be clearly explained. Not everyone is equally prone to adhere to treatment or benefit from it. But it seems that rating the sounds favorably already at the fitting visit may play a role in people using it in real life (which is paramount to getting benefit from the treatment).
The key limitation of the current study is the lack of a control condition. Tinnitus is susceptible to placebo effect and counseling. Further, many sound-therapy programs also included the amplification component, and it is not possible to conclude whether the improvement was due to sound therapy alone or to the combination of sound therapy and amplification. Nonetheless, the multiple measures over a 1-year period provide a novel view of a combination sound therapy intervention for treatment of tinnitus. The significant correlation between the use of sound therapy and the reduction in tinnitus handicap is suggestive of a positive effect of sound therapy, but a future randomized controlled trial should be conducted to allow for detangling of the effect of sound therapy from effects of amplification, counseling, placebo, and time itself.
The study sample is relatively small and heterogeneous—probable cause of tinnitus and tinnitus characteristics varied, some participants had hearing loss while others did not, and some were experienced hearing aid users while others were new to hearing aids. As such, the intervention varied accordingly (e.g., some participants had microphone turned on, while others had it off). This reflects clinical practice and heterogeneity seen in clinics. Our main inclusion criterion was the presence of bothersome tinnitus, and we did not consider hearing loss or hearing aid experience to be relevant for this exploratory study. In a recent study, Sanders et al. (2023) showed that the effect of sound therapy implemented in hearing aids was comparable between new and experienced hearing aid users, hence limiting our sample to one sub-group likely would not have affected the outcome. Future investigations should look into whether the experienced benefit is different based on the degree of hearing loss or tinnitus etiology. Case-series methodology could have been another viable strategy to manage the heterogeneity of the participants in this study (Nikles, 2015). This “N = 1” method treats each participant as their own control, and it includes detailed aspects of individual responses. Consequently, it requires fewer participants than randomized controlled trials. However, for data to be analyzed on such individual basis, the study must be properly designed. This type of study design and analysis could be useful in future research investigating individual response to sound therapy.
At least seven participants did not use sound therapy as advised at any given follow-up. Considering the link between sound-therapy use and improvement in tinnitus outcomes, future randomized-control trials should address the individual predictors of sound-therapy use. If we can predict who is likely to not use sound therapy, then we can better help these individuals by trying to improve the process so that it is acceptable to them or look for alternative approaches to alleviate their tinnitus distress.
This explorative study showed that sound therapy implemented in a combination device together with instructional counseling can be an effective method to manage tinnitus-related distress. The improvements in tinnitus outcomes were correlated with sound-therapy use, but not with total device or amplification only use. Hence, it seems that sound therapy plays a fundamental role in alleviating tinnitus related distress. As the current study did not have a control condition, it is not possible to separate the effect of sound therapy alone from effects of amplification, counseling, placebo, and time itself. Hence, a randomized controlled trial allowing for isolation of the effect of sound therapy is warranted.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and ethical clearance was obtained by the Research Ethics Committee of the Capital Region of Denmark (case no. 21070949). The participants provided their written informed consent to participate in this study.
DL: Formal analysis, Writing – original draft, Writing – review & editing, Visualization. SC: Conceptualization, Data curation, Investigation, Writing – review & editing. DP: Conceptualization, Investigation, Writing – review & editing. JN: Conceptualization, Writing – review & editing. LB: Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors thank Ronny Hannemann for his valuable input on the manuscript.
DL, SC, DP, JN, and LB were employed by WS Audiology.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fauot.2024.1322596/full#supplementary-material
Althouse, A. D. (2016). Adjust for multiple comparisons? It's not that simple. Ann. Thorac. Surg. 101, 1644–1645. doi: 10.1016/j.athoracsur.2015.11.024
Axelsson, A., and Sandh, A. (1985). Tinnitus in noise-induced hearing loss. Br. J. Audiol. 19, 271–276. doi: 10.3109/03005368509078983
Baguley, D., McFerran, D., and Hall, D. (2013). Tinnitus. Lancet 382, 1600–1607. doi: 10.1016/S0140-6736(13)60142-7
Baguley, D. M. (2002). Mechanisms of tinnitus. Br. Med. Bull. 63, 195–212. doi: 10.1093/bmb/63.1.195
Barozzi, S., Del Bo, L., Crocetti, A., Dyrlund, O., Passoni, S., Zolin, A., et al. (2016). A comparison of nature and technical sounds for tinnitus therapy. Acta. Acust. United Acust. 102, 540–546. doi: 10.3813/AAA.918971
Biswas, R., Lugo, A., Akeroyd, M. A., Schlee, W., Gallus, S., and Hall, D. A. (2022). Tinnitus prevalence in Europe: a multi-country cross-sectional population study. Lancet Reg. Health 12:100250. doi: 10.1016/j.lanepe.2021.100250
Davis, A., Paki, B., and El Refaie, A. (2000). “Epidemiology of tinnitus,” in Tinnitus Handbook, ed R. S. Tyler (San Diego, CA: Singular, Thomson Learning).
Del Bo, L., and Ambrosetti, U. (2007). Hearing aids for the treatment of tinnitus. Brain Res. 166, 341–345. doi: 10.1016/S0079-6123(07)66032-4
Gallus, S., Lugo, A., Garavello, W., Bosetti, C., Santoro, E., Colombo, P., et al. (2015). Prevalence and determinants of tinnitus in the Italian adult population. Neuroepidemiology 45, 12–19. doi: 10.1159/000431376
Henry, J. A., Frederick, M., Sell, S., Griest, S., and Abrams, H. (2015). Validation of a novel combination hearing aid and tinnitus therapy device. Ear Hear. 36, 42–52. doi: 10.1097/AUD.0000000000000093
Henry, J. A., McMillan, G., Dann, S., Bennett, K., Griest, S., Theodoroff, S., et al. (2017). Tinnitus management: randomized controlled trial comparing extended-wear hearing aids, conventional hearing aids, and combination instruments. J. Am. Acad. Audiol. 28, 546–561. doi: 10.3766/jaaa.16067
Henry, J. A., and Rheinsburg, B. T Z. (2004). Comparison of custom sounds for achieving tinnitus relief. J. Am. Acad. Audiol. 15, 585–598. doi: 10.3766/jaaa.15.8.6
Henry, J. A., Schechter, M. A., Zaugg, T. L., Griest, S., Jastreboff, P. J., Vernon, J. A., et al. (2006). Outcomes of clinical trial: tinnitus masking versus tinnitus retraining therapy. J. Am. Acad. Audiol. 17, 104–132. doi: 10.3766/jaaa.17.2.4
Henry, J. A., Zaugg, T. L., Myers, P. J., and Schechter, M. A. (2008). Using therapeutic sound with progressive audiologic tinnitus management. Trends Amplif. 12, 188–209. doi: 10.1177/1084713808321184
Herzfeld, M., Ciurlia-Guy, E., and Sweetow, R. (2014). Clinical trial on the effectiveness of widex zen therapy for tinnitus. Hear. Rev. 10.
Hoare, D. J., Edmondson-Jones, M., Sereda, M., Akeroyd, M. A., and Hall, D. (2014a). Amplification with hearing aids for patients with tinnitus and co-existing hearing loss. Cochr. Database Syst. Rev. 2014, CD010151. doi: 10.1002/14651858.CD010151.pub2
Hoare, D. J., Searchfield, G. D., Refaie, A. E., and Henry, J. A. (2014b). Sound therapy for tinnitus management: practicable options. J. Am. Acad. Audiol. 25, 62–75. doi: 10.3766/jaaa.25.1.5
Humes, L. E. (2019). The World Health Organization's hearing-impairment grading system: an evaluation for unaided communication in age-related hearing loss. Int. J. Audiol. 58, 12–20. doi: 10.1080/14992027.2018.1518598
Jastreboff, P. J., and Hazell, J. W. (1993). A neurophysiological approach to tinnitus: clinical implications. Br. J. Audiol. 27, 7–17. doi: 10.3109/03005369309077884
Jin, I., Choi, S., and Ku, M. (2021). Notched and nonnotched stimuli are equally effective at the mixing-point level in sound therapy for tinnitus relief. J. Am. Acad. Audiol. 32, 420–425. doi: 10.1055/s-0041-1728701
Jin, I., Choi, S., Ku, M., Sim, Y., and Leeb, T. (2022). The impact of daily hours of sound therapy on tinnitus relief for people with chronic tinnitus: a randomized controlled study. J. Speech Lang. Hear. Res. 65, 3079–3099. doi: 10.1044/2022_JSLHR-21-00651
Johansen, J. D., Skellgaard, P. H., and Caporali, S. (2014). Effect of counseling, amplification and fractal tones in tinnitus management. J. Commun. Disord. Deaf Stud. Hear. Aids 2:1000124. doi: 10.4172/2375-4427.1000124
Jørgensen, M. L. (2022). Exploring Innovative Hearing Aid Techniques for Tinnitus Treatment Lyngby: Technical University of Denmark.
Jørgensen, M. L., Hyvärinen, P., Caporali, S., and Dau, T. (2022). The short and long-term effect of sound therapy on visual attention in chronic tinnitus patients. Audiol. Res. 12, 493–507. doi: 10.3390/audiolres12050050
Khalfaa, S., Dubalb, S., Veuilleta, E., Perez-Diazb, F., Jouventb, R., and Colleta, L. (2002). Psychometric normalization of a hyperacusis questionnaire. J. Otorhinolaryngol. Relat. Spec. 64, 436–442. doi: 10.1159/000067570
Kochkin, S., and Tyler, R. (2008). Tinnitus treatment and the effective of hearing aids: hearing care professional perceptions. Hear. Rev. 15, 14–18.
Krick, C. M., Grapp, M., Daneshvar-Talebi, J., Reith, W., Plinkert, P. K., and Bolay, H. V. (2015). Cortical reorganization in recent-onset tinnitus patients by the Heidelberg Model of Music Therapy. Front. Neurosci. 9, 1–9. doi: 10.3389/fnins.2015.00049
Kuk, F., Peeters, H., and Lau, C. C. (2010). The efficacy of fractal music employed in hearing aids for tinnitus management. Hear. Rev. 17, 32–42.
Liu, H., Zhang, J., Yang, S., Wang, X., Zhang, W., Li, J., et al. (2021). Efficacy of sound therapy interventions for tinnitus management: a protocol for systematic review and network meta-analysis. Medicine 100, 1–14. doi: 10.1097/MD.0000000000027509
Mackenna, L., and Irwin, R. (2008). Sound Therapy for tinnitus – sacred cow or idol worship?: an investigation of the evidence. Audiol. Med. 6, 16–24. doi: 10.1080/16513860801899389
Makar, S. K., Mukundan, G., and Gore, G. (2017). Treatment of tinnitus: a scoping review. Int. Tinnitus J. 21, 144–156. doi: 10.5935/0946-5448.20170027
McCormack, A., Edmondson-Jones, M., Somerset, S., and Hall, D. (2016). A systematic review of the reporting of tinnitus prevalence and severity. Hear. Res. 337, 70–79. doi: 10.1016/j.heares.2016.05.009
Meikle, M. B., Henry, J. A., Griest, S. E., Stewart, B. J., Abrams, H. B., McArdle, R., et al. (2012). The tinnitus functional index: development of a new clinical measure for chronic, intrusive tinnitus. Ear Hear. 33, 153–176. doi: 10.1097/AUD.0b013e31822f67c0
Newman, C. W., and Sandridge, S. A. (2012). A comparison of benefit and economic value between two sound therapy tinnitus management options. J. Am. Acad. Audiol. 126–138, 126–138. doi: 10.3766/jaaa.23.2.7
Nikles, J. (2015). “What are N-of-1 trials?,” in The Essential Guide to N-of-1 Trials in Health, eds J. Nikles and G. Mitchell (Dordrecht: Springer). doi: 10.1007/978-94-017-7200-6_2
Oz, I., Arslan, F., Hizal, E., Erbek, S. H., Eryaman, E., Senkal, O. A., et al. (2013). Effectiveness of the combined hearing and masking devices on the severity and perception of tinnitus: a randomized, controlled, double-blind study. J. Otorhinolaryngol. Head Neck Surg. 75, 211–220. doi: 10.1159/000349979
Sanders, P. J., Nielsen, R. M., Jensen, J. J., and Searchfield, G. D. (2023). Hearing aids with tinnitus sound support reduce tinnitus severity for new and experienced hearing aid users. Front. Audiol. Otol. 1:1238164. doi: 10.3389/fauot.2023.1238164
Schmidt, E. (2018). The Widex Fitting Rationale for Evoke, Vol. 38. WidexPress. Available online at: https://www.widex.biz/axapta/documents/9%20502%204866%20001%2001.pdf
Searchfield, G. D., Kaur, M., and Martin, W. H. (2010). Hearing Aids as adjunct to counseling: tinnitus patients who choose amplification do better than those who don't. Int. J. Audiol. 49, 574–579. doi: 10.3109/14992021003777267
Sereda, M., Davies, J., and Hall, D. A. (2017). Pre-market version of a commercially available hearing instrument with a tinnitus sound generator: feasibility of evaluation in a clinical trial. Int. J. Audiol. 56, 286–294. doi: 10.1080/14992027.2016.1254822
Sereda, M., Xia, J., El Refaie, A., Hall, D. A., and Hoare, D. J. (2018). Sound therapy (using amplification devices and/or sound generators) for tinnitus in adults. Cochr. Database Syst. Rev. 2018:CD013094. doi: 10.1002/14651858.CD013094
Stocking, C. T., and Stecker, N. A. (2016). Efficacy of the individual components of a tinnitus management protocol. Audiology 18326. Retrieved from: https://www.audiologyonline.com
Surr, R. K., Kolb, J. A., Cord, M. T., and Garrus, N. P. (1999). Tinnitus Handicap Inventory (THI) as a hearing aid outcome measure. J. Am. Acad. Audiol. 10, 489–495. doi: 10.1055/s-0042-1748538
Sweetow, R. W., Fehl, M., and Ramos, P. M. (2015a). Do tinnitus patients continue to use amplification and sound therapy post habilitation? Hear. Rev. 21.
Sweetow, R. W., Kuk, F., and Caporali, S. (2015b). A controlled study on the effectiveness of fractal tones on subjects with minimal need for amplification. Hear. Rev. 22.
Sweetow, R. W., and Sabes, J. H. (2010). Effects of acoustical stimuli delivered through hearing aids on tinnitus. J. Am. Acad. Audiol. 21, 461–473. doi: 10.3766/jaaa.21.7.5
Trotter, M. I., and Donaldson, I. (2008). Hearing aids and tinnitus therapy: a 25-year experience. J. Laryngol. Otol. 122, 1052–1056. doi: 10.1017/S002221510800203X
Tunkel, D. E., Bauer, C. A., Sun, G. H., Rosenfeld, R. M., Chandrasekhar, S. S., Cunningham, E. R., et al. (2014). Clinical practice guideline: tinnitus. Otolaryngol. Head Neck Surg. 151, S1–S40. doi: 10.1177/0194599814545325
Tyler, R. S., Deshpande, A. K., Lau, C. C., and Kuk, F. (2017). The effectiveness of the progression of Widex zen tinnitus therapy: a pilot study. Am. J. Audiol. 26, 283–292. doi: 10.1044/2017_AJA-16-0009
Keywords: tinnitus, sound therapy, fractal tones, amplification, combination device
Citation: Lelic D, Caporali S, Parker D, Nielsen J and Balling LW (2024) Impact of a combination sound therapy on tinnitus distress: an exploratory one-year longitudinal study. Front. Audiol. Otol. 2:1322596. doi: 10.3389/fauot.2024.1322596
Received: 16 October 2023; Accepted: 14 February 2024;
Published: 05 March 2024.
Edited by:
Alicja Natalia Malicka, La Trobe University, AustraliaReviewed by:
Michelle Loeliger, La Trobe University, AustraliaCopyright © 2024 Lelic, Caporali, Parker, Nielsen and Balling. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dina Lelic, ZGluYS5sZWxpY0B3c2EuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.