
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Audiol. Otol., 09 January 2024
Sec. Tinnitus
Volume 1 - 2023 | https://doi.org/10.3389/fauot.2023.1302215
This article is part of the Research TopicTinnitus Tools and Protocols for Effective Clinical PracticeView all 11 articles
 Fabrice Bardy1,2*
Fabrice Bardy1,2* Laure Jacquemin3,4
Laure Jacquemin3,4 Cara L. Wong5
Cara L. Wong5 Michael R. D. Maslin1,2,6
Michael R. D. Maslin1,2,6 Suzanne C. Purdy1,2
Suzanne C. Purdy1,2 Hung Thai-Van7,8,9
Hung Thai-Van7,8,9Background: While there is no cure for tinnitus, research has shown that cognitive behavioral therapy (CBT) is effective in managing clinical sequelae. Although traditional CBT is labor-intensive and costly, new online consultations may improve accessibility. Moreover, there is promise in an engaging conversational agent, or a “chatbot,” delivering CBT in a conversation-like manner and allowing users to work through complex situations with the guidance of a virtual coach. Currently, there is little research examining a possible hybrid model using iCBT and tele consultation with a psychologist.
Methods: A randomized, 2 parallel-group trial was conducted to compare the clinical effectiveness of (1) iCBT delivered through a chatbot mobile app (i.e., Tinnibot only group) (2) Tinnibot combined with telepsychology (i.e., hybrid-intervention group). A total of 30 eligible adults with tinnitus were included. After an 8-week intervention period, participants were followed up for 2 months. The primary outcome measure, the Tinnitus Functional Index (TFI), and the secondary outcome measures, Hyperacusis Questionnaire (HQ), Generalized Anxiety Disorder 7-item (GAD-7), and Patient Health Questionnaire (PHQ-9), were assessed before treatment, post-treatment, and at follow-up.
Results: The TFI decreased significantly over time in both groups, with a trend for a larger improvement in the group that received telepsychology. At post-treatment, a clinically significant improvement was observed in 42% of the Tinnibot-only group and 64% of the hybrid-intervention group. At follow-up, this was 64% for both groups. The secondary outcome measures, PHQ-9 and GAD-7 improved significantly over time, but the HQ did not.
Discussion: Internet-based delivery of CBT is effective in decreasing tinnitus distress, and levels of anxiety and depression, which is more relevant today than ever in the context of a global pandemic that has challenged the delivery of face-to-face intervention. The addition of telepsychology might be beneficial, but not essential for the effectiveness of treatment. There is a need for further research to determine whether there is any relationship between the characteristics of tinnitus patients and the success of the different modes of delivery of therapy.
Tinnitus is the conscious perception of sound in the absence of corresponding external stimuli. It is a widely prevalent condition that affects approximately 10–15% of the civilian population, with 20% of those affected rating their tinnitus as moderate to severe (Baguley et al., 2013). While not all individuals with tinnitus are distressed by the sound, approximately two-thirds of tinnitus sufferers experience clinical depression, and 10% report a significant reduction in quality of life (Dawes et al., 2020; Boecking et al., 2021). Chronic tinnitus can also have debilitating effects on sleep, cognitive abilities, communication/social interaction, and sense of control. Currently, there is no cure for tinnitus, which makes tinnitus management both challenging and costly. However, there is a growing body of research that indicates that tinnitus-related distress can be alleviated by using cognitive behavioral therapy (CBT).
The cognitive-behavioral model of tinnitus distress purports that the distress experienced is not due to the psychophysical characteristics of the sound (e.g., perceived loudness) but is contributed to and maintained by the interaction between negative thoughts, emotions, attention and monitoring, safety behaviors, and beliefs about tinnitus (McKenna et al., 2014; Handscomb et al., 2020). This is similar to the cognitive behavior models of other mental health conditions such as depression and anxiety. McKenna et al. (2014) proposed a model of tinnitus distress suggesting that thinking of tinnitus in a negative way (e.g., “this noise will drive me crazy”) leads to feelings of distress, which in turn draws more attention toward the tinnitus causing the perception of it to be distorted. Increased attention creates more negative thoughts, while underlying beliefs and changes in behavior (e.g., avoiding situations for fear of making tinnitus worse) also enhance negative thinking, increasing distress and feeding back into the cycle.
To date, CBT has the most evidence of efficacy in reducing tinnitus distress (Cima et al., 2019). Through CBT, negative thoughts, emotions, and behaviors associated with tinnitus can be identified and changed. While CBT does not change the tinnitus sound itself, it can help to manage symptoms by reconceptualizing the sound to be less threatening. A recent Cochrane review including 28 studies, found that CBT led to significant improvements in tinnitus-related quality of life, and reductions in depression compared to audiological care, tinnitus retraining therapy, and other active treatments including relaxation, psychoeducation, and internet-based forums (Fuller et al., 2020).
Over the years, CBT has evolved to absorb components of mindfulness and acceptance, which has been termed the “third wave” of CBT. Mindfulness-based CBT interventions include Mindfulness-Based Cognitive Therapy (MBCT) and Acceptance and Commitment Therapy (ACT). In the context of tinnitus, mindfulness CBT interventions aim to disinhibit the tendency of trying to avoid unwanted tinnitus; instead, facilitating acceptance of it without promoting the need to change the content of related thoughts (Hayes et al., 2004). Thus, the addition of mindfulness complements CBT, emphasizing the importance of self-regulation and redirecting attention to the present moment, fostering openness and acceptance, and living in line with one's values (McKenna et al., 2017). The efficacy of combining treatments for tinnitus, such as CBT and MBCT, has been proven as more effective than monotherapies alone. While these findings are extremely promising, traditional delivery of CBT and MCBT interventions involving time with a trained psychologist is labor-intensive, costly, and has limitations in accessibility (Gander et al., 2011; Goldstein et al., 2015; Hoare et al., 2015; Bhatt et al., 2016; Stockdale et al., 2017; Henry et al., 2019).
To improve access to evidence-based tinnitus care, internet-based cognitive behavioral therapy interventions (iCBT) have been successfully implemented for tinnitus (Andersson et al., 2002; Beukes et al., 2018a,b) and shown to have effectiveness similar to face-to-face intervention (Fuller et al., 2020). There is also promise in an engaging conversational agent or a “chatbot” which delivers CBT in a conversation-like manner and allows users to work through complex situations with guidance from a virtual coach (Fitzpatrick et al., 2017). A randomized controlled trial of a fully automated chatbot (“Woebot”), delivering CBT to young adults with symptoms of depression and anxiety, found that those in the treatment group had significantly reduced depression after 2 weeks compared to an information-only control group (Fitzpatrick et al., 2017). Similarly, a mobile app-based CBT chatbot was found to significantly decrease the severity of panic disorder symptoms compared to an information-only control group (Oh et al., 2020). Finally, a chatbot called “Tinnibot” was development to deliver iCBT for individuals with tinnitus. The iCBT program is accessible via a mobile app offering psychoeducation, CBT exercises that are guided by an automated chatbot, MCBT exercises, and sound therapy. Unfortunately, despite demonstrated efficacy, online mental health interventions have comparably poorer adoption and adherence rates, which is thought to be due to the loss of human interactional quality in face-to-face CBT, crucial for success in complex situations (Donkin et al., 2013; Fitzpatrick et al., 2017).
There is currently no research to determine the potential benefit of incorporating telepsychology into a iCBT program for tinnitus delivered through a chatbot. Therefore, the current study aims to evaluate the difference in effectiveness of supplementing a newly developed tinnitus-specific iCBT program, provided through a chatbot known as “Tinnibot,” with the assistance of a video-psychoeducational psychologist. Specifically, the study will assess whether this combined approach yields greater improvements in tinnitus-related functioning compared to using Tinnibot alone.
A randomized, 2 parallel-group trial was performed between September 2020 and February 2021 to compare the clinical effectiveness of video consultation on top of iCBT delivered through a chatbot mobile app. The first group, known as the “Tinnibot only” group, received solely the iCBT program, while the second, dubbed the 'Hybrid' group, received a combination of iCBT and video calls with a clinical psychologist. The intervention period was 8 weeks, with assessments at pre-intervention, post-intervention, and 2 months follow-up.
The recruitment was completed via radio advertisement, articles on the university website, and advertisement flyers that were provided to audiology clinics in the Auckland area. Eligibility criteria included the age of 18 years or older, a mobile phone, and internet access.
Patients were excluded from the study if they met any of the following criteria: reporting a major medical or psychiatric disorder; experiencing pulsatile, objective, or unilateral tinnitus that had not been medically investigated by an Ear, Nose, Throat (ENT) specialist; currently undergoing any tinnitus treatment; or residing outside New Zealand during the time of the study. A total of 60 adults completed the initial screening questionnaire from which 30 eligible participants agreed to complete the study. Participants were alternately assigned to one of the two groups based on the order in which correspondence was received. The study was approved by the University of Auckland Human Participants Ethics Committee (reference 024482).
The iCBT program, “Tinnibot,” incorporates traditional CBT practices of identifying and challenging negative thoughts, behavior activation, and relaxation via conversations and exercises led by an automated chatbot; also, MCBT practices including exercises in mindfulness, acceptance, and gratitude. The mobile app also provided access to relaxing soundscapes that could be used by participants to create relaxing sound environments. Participants were instructed to engage with the virtual coach for 10 min per day over a period of 8 weeks. The “Hybrid” group with additional online counseling received 4 video calls of 30 min each over an 8-week period. Participants booked appointments with the psychologist through an online booking system available directly on the mobile app. Both groups were asked to check the notifications on their phone in order to access the content delivered through the app on their mobile phone. The clinical protocol can be found in Supplementary material 1.
Participants conducted a series of online questionnaires as part of the assessment battery (at pre-therapy, post-therapy, and 2 months follow-up). The assessment battery consisted of self-reported outcome measures that are related to areas that may be affected by tinnitus. All participants were invited for a video-call appointment at post-treatment to provide feedback about the smartphone application.
The Tinnitus Functional Index (TFI) was the primary outcome measure as it is a sensitive measure to treatment-related change in tinnitus distress (Meikle et al., 2012; Jacquemin et al., 2019). It is a questionnaire consisting of 25 items that are scored on a Likert scale from 0 to 10. The total score ranges from 0 to 100, with scores <25 indicating mild tinnitus, scores from 25 to 50 indicating significant tinnitus, and a score higher than 50 indicating severe tinnitus. A change on the TFI score of 13 points or more is considered to be clinically significant (Meikle et al., 2012).
Intervention effects on comorbidities of hyperacusis, anxiety, and/or depression were measured by the following questionnaires:
Tolerance of everyday sounds was assessed by means of the Hyperacusis Questionnaire (HQ) (Khalfa et al., 2002), as there is a large overlap in the prevalence of tinnitus and hyperacusis. This 14-item questionnaire has a total score ranging from 0 to 42, with a higher score indicating a more reduced sound tolerance.
The Patient Health Questionnaire (PHQ-9) was administered to indicate symptoms of depression. It is a nine-item questionnaire with a total score between 0 and 27 (Spitzer et al., 1999). Mild, moderate, moderately severe, and severe depression are indicated by cut points of 5, 10, 15, and 20 respectively.
The Generalized Anxiety Disorder 7-item (GAD-7) was filled out to quantify the level of anxiety. This seven-item questionnaire is scored between 0 and 21 (Spitzer et al., 2006). Scores of 5, 10, and 15 represent cut-offs for mild, moderate, and severe anxiety respectively.
The following questionnaires were also filled out by participants: Satisfaction with Life Scales (SLS), Cognitive Failures Questionnaire (CFQ), Insomnia Severity Index (ISI), Mindfulness Attention Awareness Scale (MAAS), Hearing Handicap Inventory for Adults–Screening version (HHIA-S), Tinnitus Handicap Inventory (THI) screening. However, they were not analyzed in the current manuscript as the goal was to measure the effectiveness of intervention in terms of tinnitus and its comorbidities of hyperacusis and related anxiety and depression. The study was conducted completely online without any in-person consultation during the COVID-19 pandemic. For this reason, we do not have details on participants clinical variables such as hearing status (pure-tone audiometry results).
The change over time in the primary outcome variable (TFI) and secondary outcome variables (HQ, PHQ9, and GAD7) were analyzed by repeated measures one-way analysis of variance (RM-ANOVA). In case the data were not normally distributed, outliers (>3.29 SD from the mean) were removed or the Friedman test was conducted. The RM-ANOVA was performed for the TFI, HQ, and PHQ-9 analyses, with one outlier being removed for the HQ and PHQ-9 data. The Friedman test was performed for the GAD-7 analyses. Data were analyzed using SPSS version 29.
A total of 28 participants completed the full experiment including 14 in the Tinnibot-only group and 14 in the hybrid group (i.e., Tinnibot plus online psychology). Hence, in each group, there was one drop-out. Both groups were well-balanced with regard to sex, had an average age of 57 years, mild symptoms of depression and anxiety, and no severe hyperacusis complaints (see Table 1). The mean TFI was higher in the hybrid group before intervention, but it was not significant (p < 0.125). The scores of HQ, PHQ9, and GAD7 between the two groups were not statistically different.
The TFI decreased significantly over time in both groups (p < 0.001) (Figure 1). The mean overall decrease in the TFI was 15.61 (T1-T0) and 1.96 (T2-T1). There was no significant difference between the groups (p > 0.05), although there was a trend for a larger TFI decrease in the group that received telepsychology (control group: T1-T0 = 11.24, T2-T1 = 3.10; hybrid group: T1-T0 = 19.99, T2-T1 = 0.81). At post-treatment, 42% of the Tinnibot-only group and 64% of the hybrid-intervention group had a clinically significant improvement (i.e., TFI difference >13). At follow-up, this was 64% for both groups. Figure 2 visualizes the change in TFI subscales, showing the smallest change on the auditory subscale, and the largest improvements for the relaxation, emotional, sense of control, and sleep subscales.
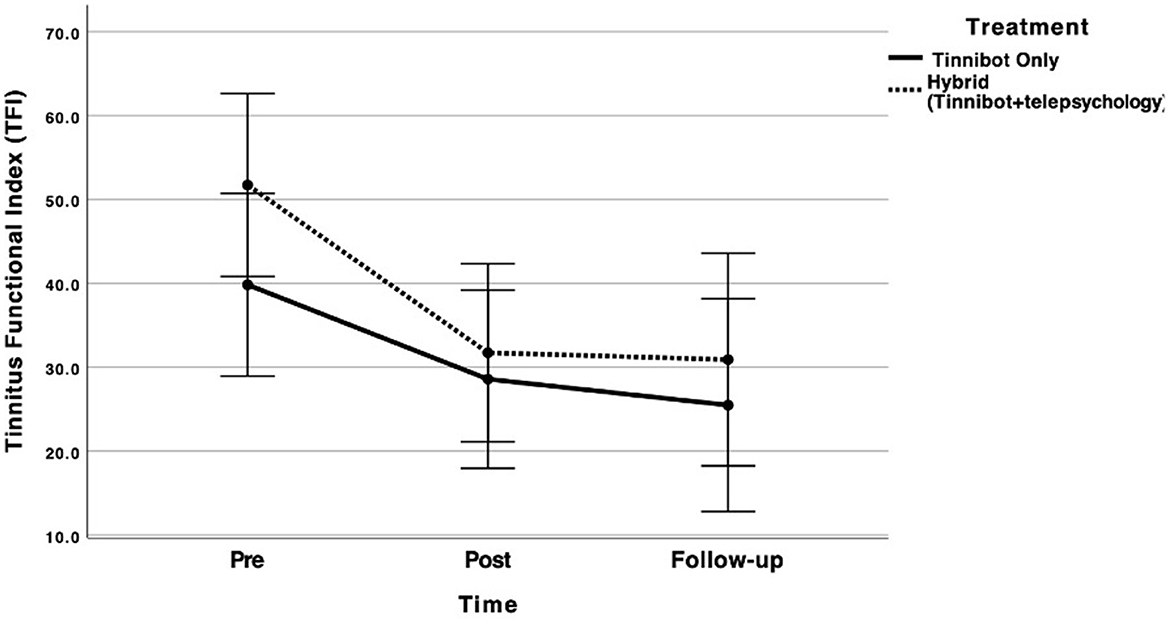
Figure 1. Mean scores on TFI over time for both groups: Tinnibot-only (dotted line) and hybrid-intervention group of Tinnibot with telepsychology (solid line). The error bars represent the 95% confidence intervals.
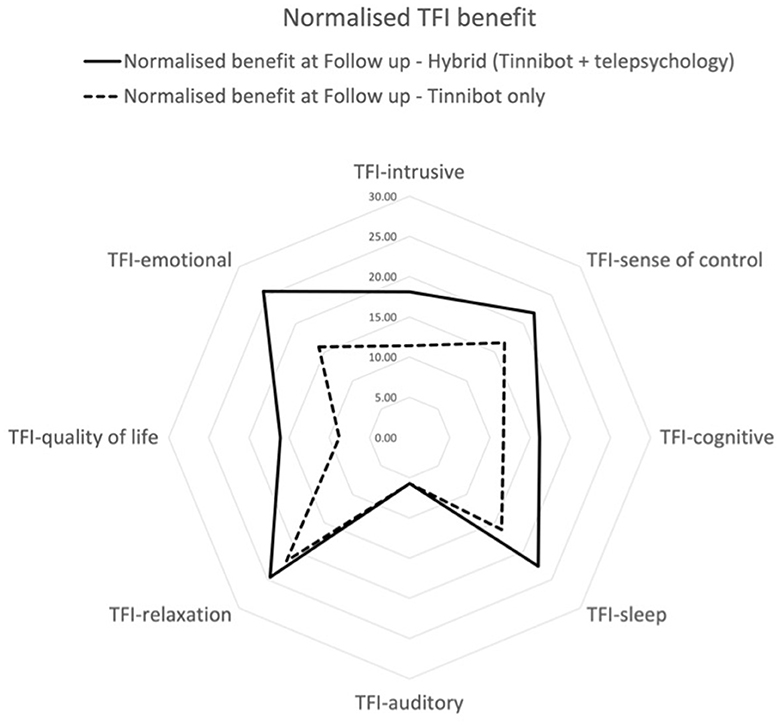
Figure 2. Mean normalized benefit for the TFI subscales at follow-up assessment for both groups: Tinnibot only (dotted line) and hybrid-intervention group of Tinnibot with telepsychology (solid line).
There was a significant decrease over time in the scores on the PHQ-9 (p < 0.001), but no significant difference was found between the groups (p > 0.05) (Figure 3). However, a trend was apparent for a larger decrease in the hybrid-intervention group (control group: T1-T0 = 1.21, T2-T1 = 1.00; tele group: T1-T0 = 1.85, T2-T1 = 0.54). Similarly, Figure 4 shows a significant decrease over time in the GAD-7 scores (p < 0.001). The intervention did not have a significant effect on the HQ (p > 0.05).
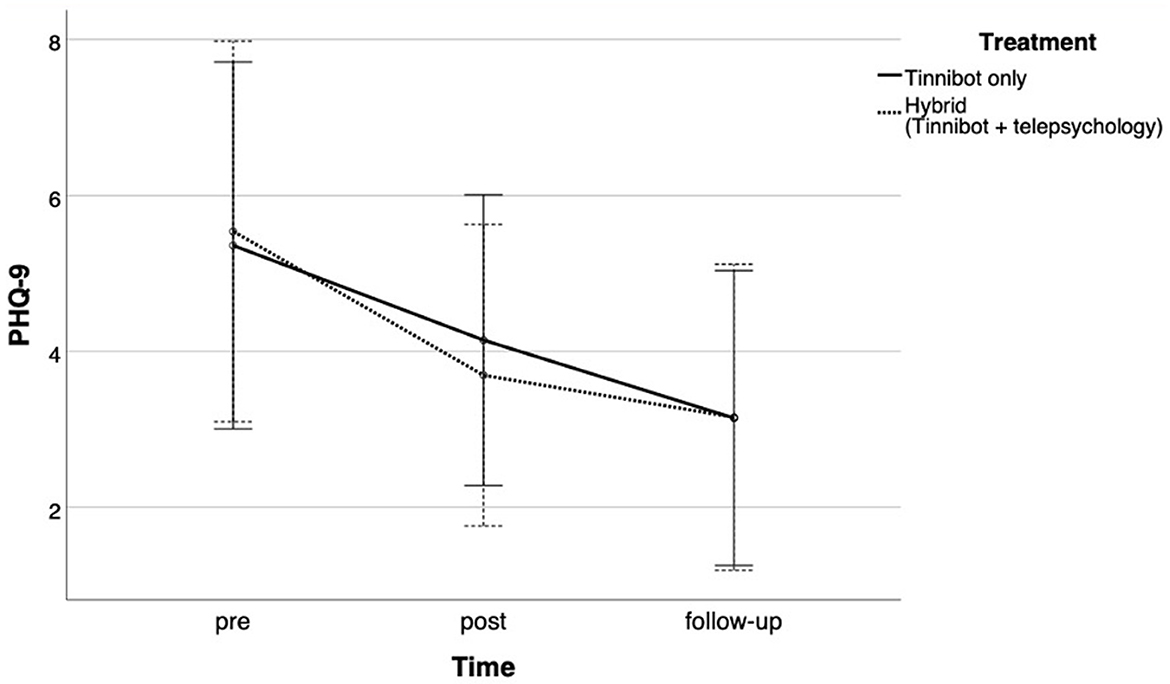
Figure 3. Mean scores on Patient Health Questionnaire (PHQ-9) over time for both groups: Tinnibot only (solid line) and hybrid-intervention group of Tinnibot with telepsychology (dotted line). The error bars represents the 95% confidence intervals.
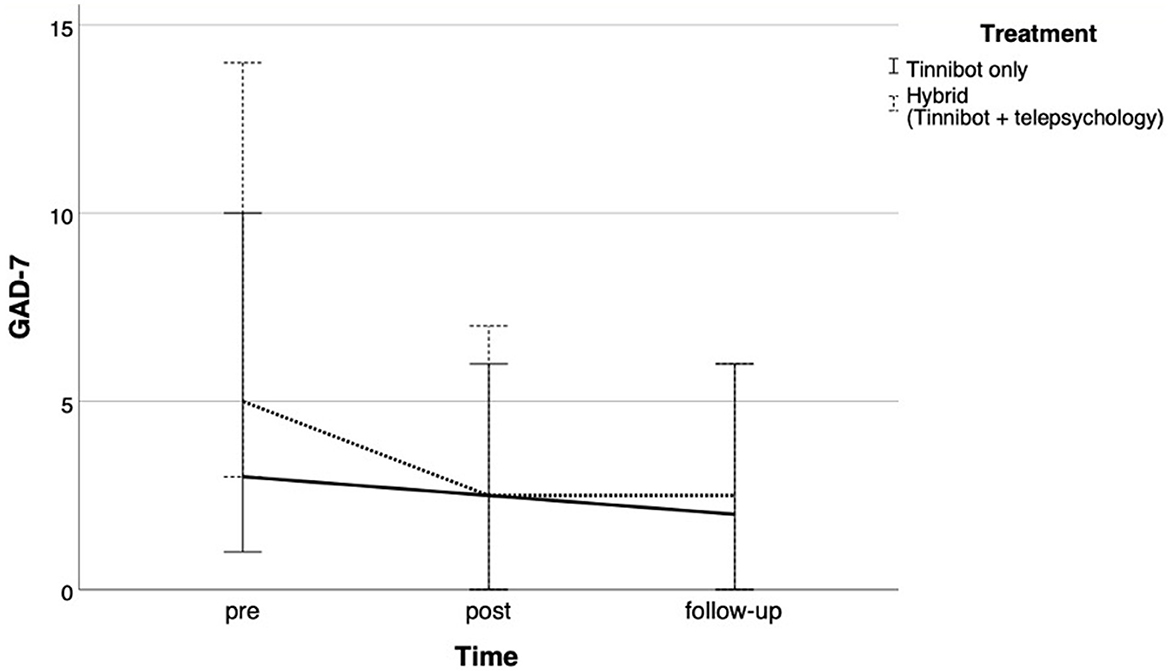
Figure 4. Mean scores on Generalized Anxiety Disorder 7-item (GAD-7) over time for both groups: Tinnibot only (solid line) and hybrid-intervention group of Tinnibot with telepsychology (dotted line). The error bars represents the 95% confidence intervals.
Table 2 shows the engagement with the mobile app during the 8-week program. There was a technical issue preventing tracking app engagement for 3 participants in the hybrid group. The total number of interactions changed significantly over time (p < 0.001), with an increase between week 1 and 8 and a decrease between week 8 and 16. Moreover, the total number of interactions was larger in the hybrid-intervention group, but this difference did not reach significance (p > 0.05) (Figure 5).
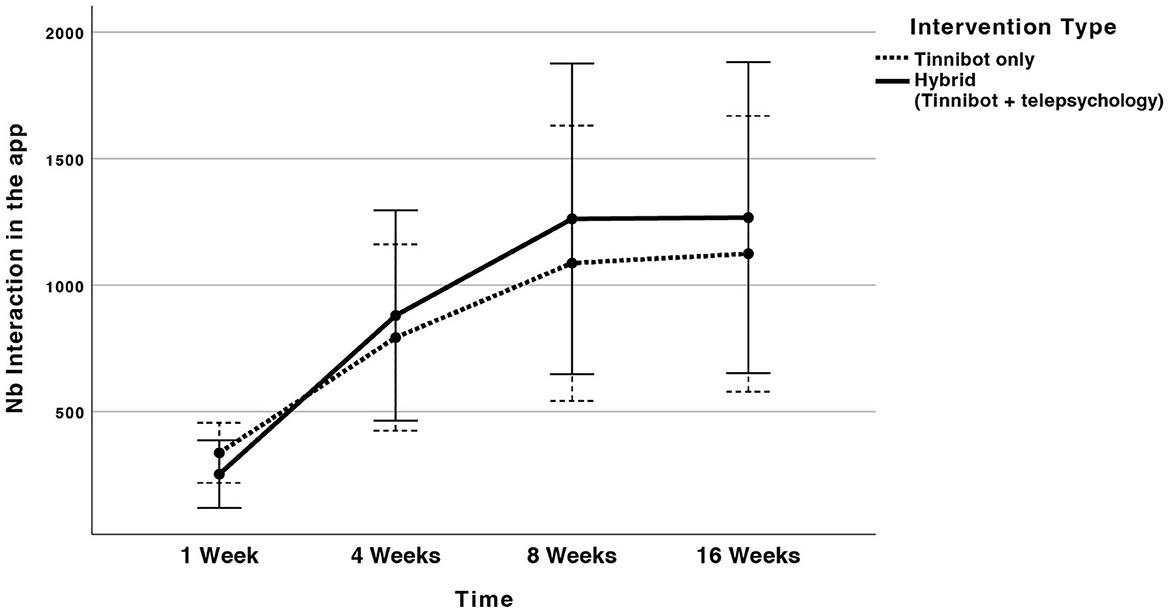
Figure 5. Mean number of interactions in the Tinnibot mobile app over time for both groups: Tinnibot only (solid line) and hybrid-intervention group of Tinnibot with telepsychology (dotted line). The error bars represents the 95% confidence intervals.
The aim of the current study was to determine if the addition of a video-psychoeducational psychologist, on top of a newly developed tinnitus-specific iCBT program provided by a chatbot mobile app (i.e., Tinnibot), would be more effective in improving tinnitus-related functioning, than Tinnibot alone. Participants were split into 2 groups of 14 participants. The first group received Tinnibot only. The second group received Tinnibot and 4 sessions of 30 min with a psychologist within 8 weeks. While both interventions led to a significant decrease in tinnitus distress measured by the TFI over time, there was no significant difference between the groups even though a trend toward a faster improvement for the hybrid-intervention group was found. At 8 weeks post-intervention, 6 out of 14 had a clinically significant decrease in TFI when provided with Tinnibot only, while 9 out of 14 had a clinically significant decrease in the hybrid-intervention group. However, at follow-up (16 weeks post-intervention), 9 out of 14 participants (~61%) showed a clinically significant decrease in tinnitus distress in both groups. Similar results could be found in terms of significant changes in symptoms of anxiety and depression (measured by the GAD-7 and PHQ-9 respectively). These findings are of particular relevance in current times, given the goal of providing new ways to access tinnitus intervention.
The current study replicated earlier studies showing iCBT to be effective in terms of decreasing tinnitus distress, anxiety, and depression. The hypothesis of the current study was that the addition of telepsychology would provide added benefits in terms of tinnitus distress compared to the digital therapy provided in isolation. While there was a trend in the current study for larger and faster improvements in the group with telepsychology, the interaction between intervention type (i.e., Tinnibot + telepsychology vs. Tinnibot only) and measurement time (i.e. pre-intervention, post-intervention, follow-up) was not statistically significant. It suggests that the addition of telepsychology did not lead to a significant difference in the primary outcome measure.
One limitation of the study to consider is the initial tinnitus severity among participants. Previous research has shown that tinnitus severity is a predictor of treatment benefit (Rodrigo et al., 2021), so this trend should be interpreted with caution, as the group with telepsychology had higher baseline scores on the TFI. In this regard, the current study support previous evidence for the efficacy of app-only treatments.
As internet-based interventions have shown barriers in terms of time, motivation, and engagement (Demoen et al., 2023), we hypothesized that the hybrid-intervention group would demonstrate an increase in engagement with the mobile app and a decrease in the number of dropouts because of the human interaction with a psychologist happening every 2nd week. There was no significant difference between the groups, however, though there was a trend toward a higher number of interactions with the Tinnibot mobile app when associated with telepsychology. This should be further investigated in future larger trials. It would also be interesting to compare adherence from app store users since clinical trial participants are in general more likely to adhere to an intervention (Andrade, 1998).
The auditory subscale of the TFI showed the smallest change, which is consistent with the fact that no hearing rehabilitation was provided to participants during the intervention. There is a need for further studies to investigate the impact of combining iCBT with audiological care on tinnitus distress. Also, there are suggestions in the literature that group therapy could lead to better results compared to individual treatment (Lourenco et al., 2023; Marks et al., 2023). Hence, online counseling in groups is another promising avenue to explore in future research.
The intervention in the current study had an innovative chatbot function, however, the study design did not allow us to make conclusions about its additional benefit, as a control group for this was not included in the study design. The intervention incorporated traditional CBT practices (i.e., identifying and challenging negative thoughts, behavior activation, and relaxation), as well as MCBT practices (i.e., exercises in mindfulness, acceptance, and gratitude). Hence, the question arises as to which of these components are crucial for therapeutic success. Further work on these topics is needed. In addition, more extensive studies are required to investigate if there are specific profiles that benefit most from telepsychology and whether it is feasible to predict who would benefit most based on a pre-assessment questionnaire. As the current sample had mainly mild symptoms of anxiety and depression, no conclusions can be drawn for tinnitus patients with a comorbidity of anxiety and/or depression. It could be that this group would benefit more from the hybrid-intervention approach of digital therapeutics and telehealth.
To our knowledge, this was the first study that investigated the benefit of human support in addition to a chatbot intervention in the context of tinnitus. This study showed that, in both groups (Tinnibot only or hybrid intervention with telepsychology), over 60% of the participants showed a clinically significant decrease in tinnitus distress 16 weeks after the start of the iCBT program. This positive result with iCBT is more relevant today than ever in the context of a global pandemic disturbing the delivery of face-to-face intervention. The addition of telepsychology might be beneficial, but not essential for the effectiveness of treatment. The cost-effectiveness of iCBT and iCBT combined with telepsychology should be investigated and compared to other current tinnitus treatment protocols. Moreover, further research should determine whether there is any relationship between the characteristics of tinnitus patients and the success of the different modes of delivery of therapy.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Auckland Health Research Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
FB: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Software, Writing—original draft, Writing—review & editing, Formal analysis. LJ: Formal analysis, Validation, Writing—original draft, Writing—review & editing. CW: Conceptualization, Funding acquisition, Investigation, Writing—original draft. MM: Conceptualization, Funding acquisition, Methodology, Writing—review & editing. SP: Funding acquisition, Writing—review & editing, Conceptualization, Investigation, Methodology. HT-V: Funding acquisition, Writing—review & editing, Formal analysis.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by the Eisdell Moore Centre project grant and by a grant from “Fondation pour l'Audition” at the “Institut de l'Audition de Paris” (FPA IDA09 and FPA IDA10).
FB is a co-founder of Odio Tech Pty Ltd., the company that developed the Tinnibot app. LJ is working as contractor for Odio Tech Pty Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fauot.2023.1302215/full#supplementary-material
Andersson, G., Strömgren, T., Ström, L., and Lyttkens, L. (2002). Randomized controlled trial of internet-based cognitive behavior therapy for distress associated with tinnitus. Psychosom. Med. 64, 810–816. doi: 10.1097/00006842-200209000-00014
Andrade, S. (1998). Compliance in the real world. Value Health 1, 171–173. doi: 10.1046/j.1524-4733.1998.130171.x
Baguley, D., Mcferran, D., and Hall, D. (2013). Tinnitus. Lancet 382, 1600–1607. doi: 10.1016/S0140-6736(13)60142-7
Beukes, E. W., Andersson, G., Allen, P. M., Manchaiah, V., and Baguley, D. M. (2018a). Effectiveness of guided internet-based cognitive behavioral therapy vs face-to-face clinical care for treatment of tinnitus: a randomized clinical trial. JAMA Otolaryngol. Head Neck Surg. 144, 1126–1133. doi: 10.1001/jamaoto.2018.2238
Beukes, E. W., Baguley, D. M., Allen, P. M., Manchaiah, V., and Andersson, G. (2018b). Audiologist-guided internet-based cognitive behavior therapy for adults with tinnitus in the united kingdom: a randomized controlled trial. Ear. Hear. 39, 423–433. doi: 10.1097/AUD.0000000000000505
Bhatt, J. M., Lin, H. W., and Bhattacharyya, N. (2016). Prevalence, severity, exposures, and treatment patterns of tinnitus in the United States. JAMA Otolaryngol. Head Neck Surg. 142, 959–965. doi: 10.1001/jamaoto.2016.1700
Boecking, B., Biehl, R., Brueggemann, P., and Mazurek, B. (2021). Health-related quality of life, depressive symptoms, anxiety, and somatization symptoms in male and female patients with chronic tinnitus. J. Clin. Med. 10, 2798. doi: 10.3390/jcm10132798
Cima, R. F. F., Mazurek, B., Haider, H., Kikidis, D., Lapira, A., Noreña, A., et al. (2019). A multidisciplinary European guideline for tinnitus: diagnostics, assessment, and treatment. HNO 67, 10–42. doi: 10.1007/s00106-019-0633-7
Dawes, P., Newall, J., Stockdale, D., and Baguley, D. M. (2020). Natural history of tinnitus in adults: a cross-sectional and longitudinal analysis. BMJ Open 10, e041290. doi: 10.1136/bmjopen-2020-041290
Demoen, S., Chalimourdas, A., Timmermans, A., Van Rompaey, V., Vanderveken, O. M., Jacquemin, L., et al. (2023). Effectiveness of telerehabilitation interventions for self-management of tinnitus: systematic review. J. Med. Internet Res. 25, e39076. doi: 10.2196/39076
Donkin, L., Hickie, I. B., Christensen, H., Naismith, S. L., Neal, B., Cockayne, N. L., et al. (2013). Rethinking the dose-response relationship between usage and outcome in an online intervention for depression: randomized controlled trial. J. Med. Internet Res. 15, e231. doi: 10.2196/jmir.2771
Fitzpatrick, K. K., Darcy, A., and Vierhile, M. (2017). Delivering cognitive behavior therapy to young adults with symptoms of depression and anxiety using a fully automated conversational agent (woebot): a randomized controlled trial. JMIR Ment. Health 4, e19. doi: 10.2196/mental.7785
Fuller, T., Cima, R., Langguth, B., Mazurek, B., Vlaeyen, J. W., and Hoare, D. J. (2020). Cognitive behavioural therapy for tinnitus. Cochr. Datab. Syst. Rev. 1, Cd012614. doi: 10.1002/14651858.CD012614.pub2
Gander, P. E., Hoare, D. J., Collins, L., Smith, S., and Hall, D. A. (2011). Tinnitus referral pathways within the National Health Service in England: a survey of their perceived effectiveness among audiology staff. BMC Health Serv. Res. 11, 162. doi: 10.1186/1472-6963-11-162
Goldstein, E., Ho, C. X., Hanna, R., Elinger, C., Yaremchuk, K. L., Seidman, M. D., et al. (2015). Cost of care for subjective tinnitus in relation to patient satisfaction. Otolaryngol. Head Neck Surg. 152, 518–523. doi: 10.1177/0194599814566179
Handscomb, L., Shorter, G. W., Hoare, D. J., and Hall, D. A. (2020). Evaluation of a cognitive behavioral model of tinnitus distress: a cross-sectional study using structural equation modeling. Ear. Hear 41, 1028–1039. doi: 10.1097/AUD.0000000000000826
Hayes, S. C., Follette, V. M., and Linehan, M. M. (2004). Mindfulness and Acceptance: Expanding the Cognitive-Behavioral Tradition. New York, NY, US: The Guilford Press.
Henry, J., Mcmillan, L., and Manning, C. (2019). Multidisciplinary tinnitus care. J. Nurse Practit. 15, 671–675. doi: 10.1016/j.nurpra.2019.07.017
Hoare, D. J., Broomhead, E., Stockdale, D., and Kennedy, V. (2015). Equity in provision of tinnitus services in United Kingdom National Health Service audiology departments. Eur. J. Pers. Centered Heathcare 3, 318–326. doi: 10.5750/ejpch.v3i3.984
Jacquemin, L., Mertens, G., Van De Heyning, P., Vanderveken, O. M., Topsakal, V., De Hertogh, W., et al. (2019). Sensitivity to change and convergent validity of the Tinnitus Functional Index (TFI) and the Tinnitus Questionnaire (TQ): clinical and research perspectives. Hear. Res. 382, 107796. doi: 10.1016/j.heares.2019.107796
Khalfa, S., Dubal, S., Veuillet, E., Perez-Diaz, F., Jouvent, R., and Collet, L. (2002). Psychometric normalization of a hyperacusis questionnaire. ORL J. Otorhinolaryngol. Relat. Spec. 64, 436–442. doi: 10.1159/000067570
Lourenco, M., Fuller, T. E., Ranson, S., Vlaeyen, J. W. S., and Cima, R. F. F. (2023). Better together group versus individual cognitive-behavioral therapy for tinnitus: a multiple-baseline single-case experimental design. Ear. Hear. 44, 167–178. doi: 10.1097/AUD.0000000000001261
Marks, E., Handscomb, L., and Remskar, M. (2023). “I can see a path forward now”: a qualitative investigation of online groups for tinnitus in the time of Covid-19. Int. J. Audiol. 62, 659–666. doi: 10.1080/14992027.2022.2063195
McKenna, L., Handscomb, L., Hoare, D. J., and Hall, D. A. (2014). A scientific cognitive-behavioral model of tinnitus: novel conceptualizations of tinnitus distress. Front. Neurol. 5, 196. doi: 10.3389/fneur.2014.00196
McKenna, L., Marks, E. M., Hallsworth, C. A., and Schaette, R. (2017). Mindfulness-based cognitive therapy as a treatment for chronic tinnitus: a randomized controlled trial. Psychother. Psychosom. 86, 351–361. doi: 10.1159/000478267
Meikle, M. B., Henry, J. A., Griest, S. E., Stewart, B. J., Abrams, H. B., Mcardle, R., et al. (2012). The tinnitus functional index: development of a new clinical measure for chronic, intrusive tinnitus. Ear. Hear. 33, 153–176. doi: 10.1097/AUD.0b013e31822f67c0
Oh, J., Jang, S., Kim, H., and Kim, J.-J. (2020). Efficacy of mobile app-based interactive cognitive behavioral therapy using a chatbot for panic disorder. Int. J. Med. Inform. 140, 104171. doi: 10.1016/j.ijmedinf.2020.104171
Rodrigo, H., Beukes, E. W., Andersson, G., and Manchaiah, V. (2021). Internet-based cognitive-behavioural therapy for tinnitus: secondary analysis to examine predictors of outcomes. BMJ Open 11, e049384. doi: 10.1136/bmjopen-2021-049384
Spitzer, R. L., Kroenke, K., and Williams, J. B. (1999). Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. Jama 282, 1737–1744. doi: 10.1001/jama.282.18.1737
Spitzer, R. L., Kroenke, K., Williams, J. B., and Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166, 1092–1097. doi: 10.1001/archinte.166.10.1092
Keywords: cognitive behavioral therapy, iCBT, telepsychology, digital therapeutics, telehealth, tinnitus, self-care
Citation: Bardy F, Jacquemin L, Wong CL, Maslin MRD, Purdy SC and Thai-Van H (2024) Delivery of internet-based cognitive behavioral therapy combined with human-delivered telepsychology in tinnitus sufferers through a chatbot-based mobile app. Front. Audiol. Otol. 1:1302215. doi: 10.3389/fauot.2023.1302215
Received: 26 September 2023; Accepted: 21 November 2023;
Published: 09 January 2024.
Edited by:
Jae-Jin Song, Seoul National University Bundang Hospital, Republic of KoreaReviewed by:
Petros Vlastarakos, University General Hospital Attikon, GreeceCopyright © 2024 Bardy, Jacquemin, Wong, Maslin, Purdy and Thai-Van. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fabrice Bardy, RmFicmljZS5iYXJkeUBhdWNrbGFuZC5hYy5ueg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.