- Department of Anesthesiology, Lausanne University Hospital (CHUV), Lausanne, Switzerland
Introduction: Dorsal penile nerve block (DPNB) using anatomical landmarks remains the technique of choice for analgesia during circumcision. Ultrasound guidance has been shown to be safer and more effective. However, a recent study reported no differences between US-DPNB and DPNB in terms of analgesia. Thus, reverse US dorsal penile nerve block (RUS–PNB) has been developed, which is the image mirror of US-DPNB.
Aims: Comparison between RUS–PNB and DPNB in terms of efficacy, safety, and speed of execution.
Methods: This is a single-center retrospective study. Patients were all males, aged <16 years who underwent circumcision between 1 November 2019 and 31 December 2020. Exclusion criteria were undergoing another surgical procedure during the same operation, not undergoing a block, or refusing to participate. All patients received bupivacaine 0.5% using either DPNB or RUS-PNB. Data including demographic background information, doses of opioids used converted into an equivalent morphine dose per kilogram, different times taken for various medical acts, and complications were collected.
Results: A total of 139 patients were included. 45 (Group 1) underwent DPNB and 94 (group 2) underwent RUS–PNB. There were no differences in age, weight, height, or ASA scores between the groups. The per-operative morphine equivalent dose was Group 1; mean 0.5 mg/kg ± 0.2, Group 2; mean 0.2 mg/kg ± 0.2, with p < 0.001. The mean postoperative morphine equivalent dose, duration of anesthesia, and surgery were similar. The volume required was higher for Group 2; median 0.3 ml/kg than for Group 1; median 0.2 ml/kg. There were no complications, although two instances of block failures (4.7%) were observed in group 1 and three (3.3%) in group 2 (p = 0.653). This was due to the need for additional opioids during surgery.
Conclusion: The RUS–PNB technique is more efficient than the traditional DPNB method and does not require a longer procedure. It is likely that the incidence of complications is lower when the RUS-DPNB technique is employed, as the injection is performed “under vision” in contrast to the landmark method, which is carried out “blindly” as it results in fewer complications.
Introduction
Male circumcision is an operation to remove the foreskin from the penis. It is one of the most commonly performed surgical procedures worldwide (1). According to the World Health Organization, 30% of the world's male population over 15 years old has been circumcised for medical, religious, cultural, or social reasons (2). Historically, circumcision has been performed without anesthesia and is associated with significant per- and post-operative pain. However, when the procedure is performed without analgesia, there is a risk of increased sensitivity to pain in the future (3).
Local anesthesia has been shown to be effective and safe, preventing procedural pain in neonates and older children (4–7). However, circumcision is still frequently performed using inappropriate analgesic regimens, and there is significant variability in how medical centers perform surgery and initiate anesthesia (8).
One of the most commonly used methods is the combination of general anesthesia with local anesthesia of the nerves involved in sensory innervation of the penis. Techniques of varying efficacy have been described: eutectic mixture local anesthetic (EMLA®) cream (9) has been associated with cases of methemoglobinemia in newborns (10), circumferential infiltration (11) and caudal block—the latter, however, has the disadvantage of greater morbidity (12).
Of all the locoregional anesthesia techniques described, the dorsal penile nerve block (DPNB) remains the technique of choice because of its excellent analgesic efficacy. It is usually performed using the Dalens technique (13), which is based on the use of anatomical landmarks and involves two separate punctures and injections at the base of the penile root via the subpubic space that encloses the dorsal nerves of the penis (Figure 1) (14).
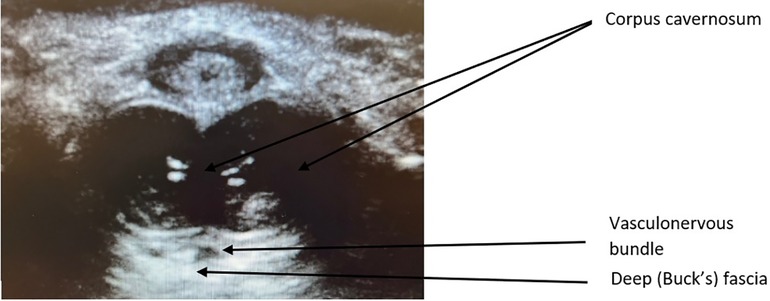
The use of ultrasound (US) Sonosite PX® (Fujifilm Sonosite Inc. United States) during DPNB (US–DPNB) was described by Sandeman (Figure 2) (6). The needle is inserted into the subpubic space, a triangle defined inferiorly by the deep penile fascia (Buck's fascia) enveloping the penile neurovascular bundle and the corpora cavernosa, superiorly by the pubic symphysis, and anteriorly by the membranous layer of the superficial fascia (Scarpa's fascia). The paired neurovascular structures lie immediately deep to the deep fascia of the penis on either side of the midline (6).

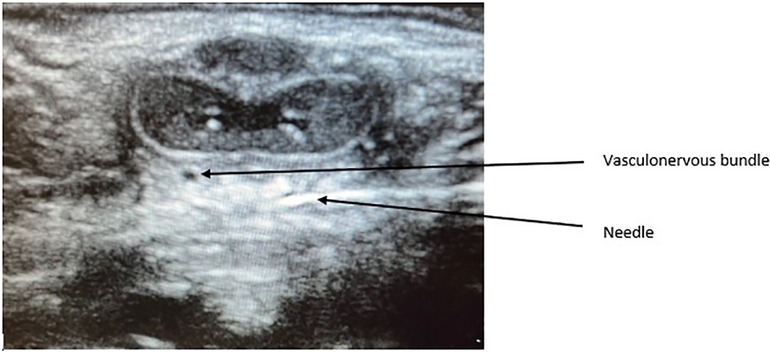
Figure 2. RUS-DPNB. The US probe placed at the root of the penis with the needle putted “in plane” technique.
Reverse US-DPNB (RUS-PNB) were first described by Rufini et al. (15). It is the mirror image of the US–DPNB. A linear US probe is positioned along the transverse plane of the penis, between its root and the scrota, angled slightly cranially towards the pubic symphysis. In this US visualization, the anatomical structures are mirrored. The deep penile fascia (Buck's fascia) and the superficial penile fascia (Dartos fascia) are visible below the corpora cavernosa. Arteries, veins, and the two dorsal nerves of the penis run above Buck's fascia. The procedure is carried out using a single injection after a negative aspiration test.
Our study aimed to compare RUS–PNB and DPNB in terms of efficacy, safety, and speed of execution.
Methods
We retrospectively analyzed a pediatric population of consecutive patients who underwent circumcision under general anesthesia using DPNB or RUS–PNB performed in Lausanne University Hospital's operating theatres by the Department of Pediatric Anesthesia physicians between 1 November, 2019, and 31 December, 2020.
The study population included all male patients under 16 years of age who underwent circumcision for phimosis or religious reasons under general anesthesia combined with either DPNB or RUS–PNB.
The needles were of varying sizes according to age, but with identical diameters and bevels. For those aged between 0 and 10 years, the needle size was 25 mm, while for those over the age of 10, the needle size was 50 mm.
The assignment of patients to either group was dependent on the anesthetist in charge of the patient's preference for analgesic technique.
We excluded patients who underwent another surgical procedure during the same operation, those who did not undergo a block, and those who refused or whose legal representative refused consent to participate in the study.
We collected data including demographic background information, the doses of opioids used converted into an equivalent morphine dose per kilogram (16) the different times taken for various medical acts, and complications. Any intraoperative need for additional boluses of fentanyl or the injection of a local anesthetic by a surgeon was considered block failure.
Increased arterial pressure or heart rate guided opioid injections during surgery. In the postoperative period, these indicators were supplemented by an assessment based on adjusted pain scores that help manage patients' comfort using opioids.
Ethics
This study was approved on April 14th 2022 by the Human Research Ethics Committee of the Canton of Vaud (CERV-VD 2021-01139), Av. de Chailly 23, 1012 Lausanne (Switzerland). Chairperson Prof. Dominique Sprumont.
The penile block procedure
All patients in the sample were induced with inhalational anesthesia using sevoflurane and nitrous oxide. After induction, a peripheral intravenous (IV) catheter was inserted for fluid maintenance and IV medication. Patients received IV fentanyl (1 mcg/kg), and ventilation was assisted using either a face mask or laryngeal mask. The blocks are designed to target the same structures, but with different approaches, which are described in detail below.
DPNB (group 1)
Patients were anesthetized using the technique described by Dalens (13, 17), which uses anatomical landmarks for guidance. Both sides of the dorsal base of the penis were infiltrated with a bolus of 0.1 ml/kg (0.2 ml/kg total) of bupivacaine 0.5%, using a Pajunk SonoPlex 22G needle.
RUS–PNB (group 2)
The anesthetist identified the corpus spongiosum, the two-corpus cavernosum, and the vasculonervous bundle surrounded by Buck's fascia using a Fujifilm Sonosite PX® L19-5 probe with maximum resolution in the superficial field (19–5 MHz) (Figure 3). The anesthetist then infiltrated this bundle with a single bolus of bupivacaine 0.5% using a Pajunk SonoPlex 22G needle (Figure 4).
During the procedure, the children received paracetamol, nonsteroidal anti-inflammatory drugs (NSAIDs), and ondansetron. IV fentanyl (1 mcg/kg) was administered at the discretion of the anesthetist in charge if the block proved insufficient. At the end of the procedure, the patient was transferred to the pediatric intensive care unit. The nurses titrated IV morphine (50 mcg/kg) until the child was comfortable.
Statistical methods
Categorical variables (ASA score, paracetamol, NSAIDs, and complications) were summarized using the frequency and percentage of each category. Comparisons between the two groups were performed using Fisher's exact test. Continuous variables were summarized using their means and standard deviations or using their medians and inter-quartile ranges (reported as lq–uq) and min–max. The comparison was made using a Student's t-test or a Wilcoxon test. A statistically significant difference was deemed to have occurred when the p-value was less than 0.05.
Results
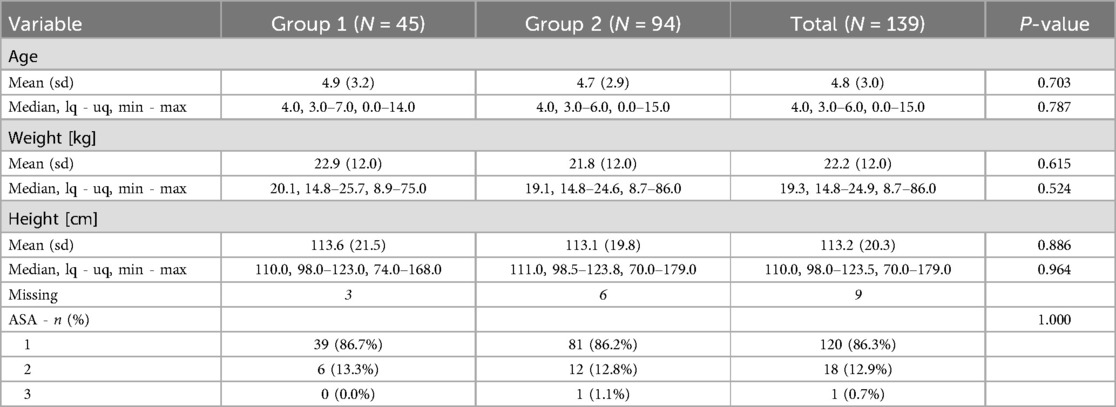
Our sample included 139 patients: 45 patients (group 1) underwent DPNB procedures and 94 (group 2) underwent RUS–PNB procedures. Overall, there were no significant differences in age (mean = 4.8 years ± 3.0, weight; mean = 22.2 kgs ± 12.0, height; mean = 113.2 cm ± 20.3, ASA score = 1, 86.3%; ASA 2 = 12.9%; ASA 3 = 0.7%) between the two groups (Table 1).
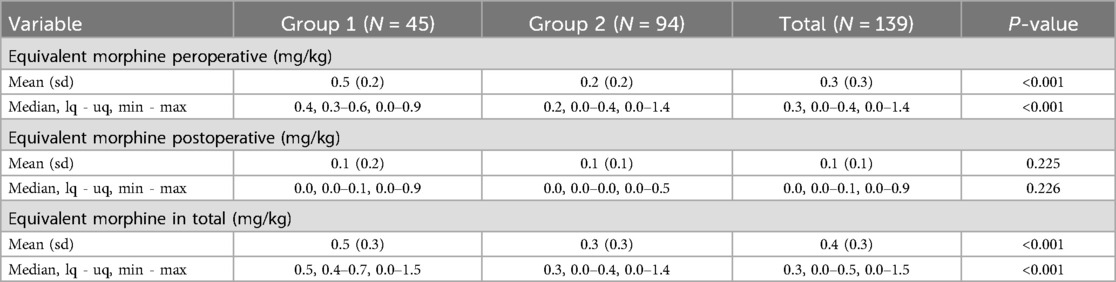
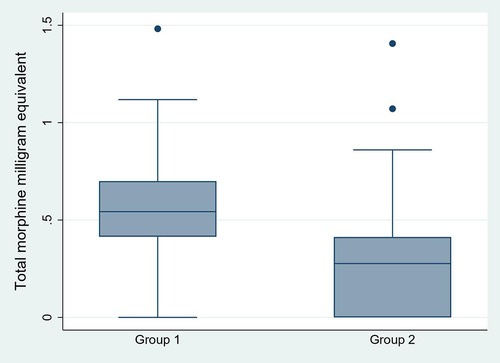
Group 1's mean per-operative morphine equivalent dose was 0.5 mg/kg ± 0.2, compared to 0.2 mg/kg ± 0.2 for Group 2, with p < 0.001. The mean post-operative morphine equivalent dose was the same for both groups: 0.1 mg/kg ± 0.2 (Table 2; Figure 5). Baseline analgesic drug use for paracetamol (Group 1, 100%; Group 2, 98.9%) and NSAIDs (Group 1, 90.9%; Group 2, 94.6%) showed no significant differences between the two groups, and these were administered according to our departmental guidelines.
The volume required for the block was slightly higher for Group 2; median 0.3 ml/kg (range 0.1–1.4) than for Group 1 median 0.2 ml/kg (range 0.2–0.5). The mean durations of anesthesia (Group 1 = 12.5 min ± 4.4; Group 2 = 13.3 min ± 5.5) and surgery (Group 1 = 18.5 min ± 6.6; Group 2 = 16.2 min ± 4.9) were similar.
There were no complication, although two instances failure of block failures (4.7%) were observed in group 1 and three (3.3%) in group 2. This was due to the need for additional opioids during surgery.
Discussion
The procedure is carried out using a single injection following a negative aspiration test. The two techniques of penile block target the same structure namely the vasculonervous bundle surrounded by Buck's fascia. However, the landmark technique is a blind dorsal approach, in contrast to the RUS-PNB technique, which is ventral and under vision. On one side, there is only one puncture, while on the other side there are two.
The present study revealed that the RUS–PNB procedures in our pediatric surgery unit required less perioperative morphine than the DPNB procedures. Thus, RUS-PNB was more efficient, although a greater volume of local anesthesia was needed to perform the block in the RUS–PNB group. The use of this block is relatively new, and its minimum efficient volume is not yet known. In this instance, a volume of 0.2 ml/kg was employed, although this was considerably below the maximum authorized dose of 0.5 ml/kg for bupivacaine (0.5%). As with axillary block, experience, time, and further studies should reduce this volume to a more realistic minimum. It is likely that the minimum effective volume for penile block is lower than the doses used in our cohort, and future studies will have to determine this.
Surprisingly, the duration of surgery was not affected by performing a RUS–PNB procedure. This could be explained by the fact that the anesthetists who performed these blocks had a lot of experience with this technique and that RUS–PNB is easier to perform because it requires only one puncture.
However, the results of studies examining this block are inconsistent. Over the last few decades, US guidance has been shown to be quicker, safer, and more effective than landmark guidance for performing most blocks. Sandeman's article on penile block noted that US guidance had higher block success rates, shorter block onset times, used smaller total doses of local anesthetic, showed better assessment of local anesthetic spread, and reduced complications (6). This led to comparative studies between US–DPNB and DPNB. However, a recent study by Teukens et al. (18) found no differences between the two techniques in terms of analgesia, but the induction of anesthesia was significantly longer in the US–DPNB group.
In this context, Rufini (15) developed the RUS-PNB. Therefore, our study aimed to investigate differences in the efficacy of intraoperative analgesia. The differences found in our study could be explained by the different nerves involved in the two techniques. Teukens' US-DPNB procedure targets the dorsal nerve, which originates from the pudendal nerve. In the RUS–PNB procedure, the block also targets branches of the perineal nerve, which innervates the ventral part of the penis. The difference would, therefore, not be due to the technique (US or landmark guidance), but rather to the different nerves targeted. However, to the best of our knowledge, no studies to date have compared the efficacies of RUS–PNB and DPNB (18).
Additionally, a discrepancy was observed in the volume of administration between the two groups. This difference is minimal and is likely attributable to the lesser experience of anesthetists under US guidance than landmark guidance, where meticulous hydrodissection results in an increase in the volume administered, though not at the targeted site for analgesia.
In terms of the reliability of these anesthetic procedures, it should be noted that this study was retrospective and included only 139 patients. Further studies are required to assess the potential of this block. As the analgesic technique used was at the discretion of the anesthetist performing the block, there could also have been a selection bias. This might explain why the two groups in the sample were of unequal sizes. However, we corrected this in our statistical analysis. Finally, several different anesthetists performed the blocks, which could have introduced bias into the way the blocks were performed.
Conclusion
The RUS–PNB technique is more efficient than the traditional DPNB method and does not require a longer procedure. It is likely that the incidence of complications is lower when the RUS-PNB technique is employed, as the injection is performed “under vision” in contrast to the landmark method, which is carried out “blindly” as it results in fewer complications.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Human Research Ethics Committee of the Canton of Vaud (CERV-VD 2021-01139), Av. de Chailly 23, 1012 Lausanne (Switzerland). Chairperson Prof. Dominique Sprumont. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin because the study focuses on the analysis of information already available in the patient's electronic record. No information on the medium- or long-term follow-up of these patients was requested.
Author contributions
EC-P: Investigation, Methodology, Writing – original draft, Writing – review & editing. TS: Data curation, Software, Writing – original draft, Writing – review & editing. SM: Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors declare that there was no assistance with the article, financial support, conflicts of interest or presentation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. American Academy of Pediatrics Task Force on Circumcision. Male circumcision. Pediatrics. (2012) 130(3):e756–85. doi: 10.1542/peds.2012-1990
2. Weiss H, World Health Organization, Joint United Nations Programme on HIV/AIDS, London School of Hygiene and Tropical Medicines. Male Circumcision: Global Trends and Determinants of Prevalence, Safety, and Acceptability. Geneva: World Health Organization: UNAIDS (2008). p. 35.
3. Taddio A, Katz J, Ilersich AL, Koren G. Effect of neonatal circumcision on pain response during subsequent routine vaccination. Lancet. (1997) 349(9052):599–603. doi: 10.1016/S0140-6736(96)10316-0
4. Nguyen TT, Kraft E, Nasrawi Z, Joshi M, Merianos D. Avoidance of general anesthesia for circumcision in infants under 6 months of age using a modified plastibell technique. Pediatr Surg Int. (2019) 35(5):619–23. doi: 10.1007/s00383-019-04452-x
5. Brady-Fryer B, Wiebe N, Lander JA. Pain relief for neonatal circumcision. Cochrane Database Syst Rev. (2004) 2004(4):CD004217. doi: 10.1002/14651858.CD004217.pub2
6. Sandeman DJ, Dilley AV. Ultrasound guided dorsal penile nerve block in children. Anaesth Intensive Care. (2007) 35(2):266–9. doi: 10.1177/0310057X0703500217
7. Sandeman DJ, Reiner D, Dilley AV, Bennett MH, Kelly KJ. A retrospective audit of three different regional anaesthetic techniques for circumcision in children. Anaesth Intensive Care. (2010) 38(3):519–24. doi: 10.1177/0310057X1003800317
8. Rossi S, Buonocore G, Bellieni CV. Management of pain in newborn circumcision: a systematic review. Eur J Pediatr. (2021) 180(1):13–20. doi: 10.1007/s00431-020-03758-6
9. Taddio A, Stevens B, Craig K, Rastogi P, Ben-David S, Shennan A, et al. Efficacy and safety of lidocaine-prilocaine cream for pain during circumcision. N Engl J Med. (1997) 336(17):1197–201. doi: 10.1056/NEJM199704243361701
10. Stang HJ, Snellman LW, Condon LM, Conroy MM, Liebo R, Brodersen L, et al. Beyond dorsal penile nerve block: a more humane circumcision. Pediatrics. (1997) 100(2):E3. doi: 10.1542/peds.100.2.e3
11. Chambers FA, Lee J, Smith J, Casey W. Post-circumcision analgesia: comparison of topical analgesia with dorsal nerve block using the midline and lateral approaches. Br J Anaesth. (1994) 73(4):437–9. doi: 10.1093/bja/73.4.437
12. Ecoffey C, Lacroix F, Giaufré E, Orliaguet G. Courrèges P, Association des Anesthésistes Réanimateurs Pédiatriques d'Expression Française (ADARPEF). Epidemiology and morbidity of regional anesthesia in children: a follow-up one-year prospective survey of the French-Language Society of Paediatric Anaesthesiologists (ADARPEF). Paediatr Anaesth. (2010) 20(12):1061–9. doi: 10.1111/j.1460-9592.2010.03448.x
13. Dalens B, Vanneuville G, Dechelotte P. Penile block via the subpubic space in 100 children. Anesth Analg. (1989) 69(1):41–5. doi: 10.1213/00000539-198907000-00008
14. Brown TC, Weidner NJ, Bouwmeester J. Dorsal nerve of penis block–anatomical and radiological studies. Anaesth Intensive Care. (1989) 17(1):34–8. doi: 10.1177/0310057X8901700108
15. Rufini P, Cumbo S, Caccavale AR, Azzari C, Germini F, L'Erario M, et al. Reversed ultrasound-guided dorsal penile nerve block in children: a retrospective study. Paediatr Anaesth. (2022) 32(9):1076–7. doi: 10.1111/pan.14502
16. Patanwala AE, Duby J, Waters D, Erstad BL. Opioid conversions in acute care. Ann Pharmacother. (2007) 41(2):255–66. doi: 10.1345/aph.1H421 Erratum in: Ann Pharmacother. 2007 Mar;41(3):531.17299011
17. Van Zundert A. Penile dorsal nerve block for penile surgery. Acta Anaesthesiol Belg. (1985) 36(1):41–6. doi: 10.13140/RG.2.1.3257.1289
18. Teunkens A, Van de Velde M, Vermeulen K, Van Loon P, Bogaert G, Fieuws S, et al. Dorsal penile nerve block for circumcision in pediatric patients: a prospective, observer-blinded, randomized controlled clinical trial for the comparison of ultrasound-guided vs landmark technique. Paediatr Anaesth. (2018) 28(8):703–9. doi: 10.1111/pan.13429
Keywords: regional anesthesia, pediatric, circumcision, penile block, ultrasound, landmark
Citation: Christophel-Plathier E, Saucy T and Mauron S (2024) Comparison of penile block using the reverse US-guided nerve block or landmark guidance during circumcision in pediatric population: a retrospective study. Front. Anesthesiol. 3:1433770. doi: 10.3389/fanes.2024.1433770
Received: 7 June 2024; Accepted: 12 August 2024;
Published: 12 September 2024.
Edited by:
André Van Zundert, The University of Queensland, AustraliaReviewed by:
Ece Yamak Altinpulluk, Morphological Madrid Research Center, SpainJohn Samuel Wiener, Duke University, United States
Copyright: © 2024 Christophel-Plathier, Saucy and Mauron. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: E. Christophel-Plathier, ZW1lbGluZS5jaHJpc3RvcGhlbEBjaHV2LmNo
 E. Christophel-Plathier
E. Christophel-Plathier T. Saucy
T. Saucy