- 1Anesthesia Department, Faculty of Medicine, Ain Shams University, Cairo, Egypt
- 2Dow Medical College, Dow University of Health Sciences, Karachi, Pakistan
- 3Department of Anaesthesia, Sandwell and West Birmingham Hospitals (SWBH), Birmingham, United Kingdom
- 4Department of Anesthesiology, Louisiana State University Health Sciences Center at Shreveport, Shreveport, LA, United States
- 5Department of Anesthesiology, Creighton University School of Medicine, Phoenix, AZ, United States
- 6Department of Pharmacology, Toxicology, and Neurosciences, Louisiana State University Health Sciences Center at Shreveport, Shreveport, LA, United States
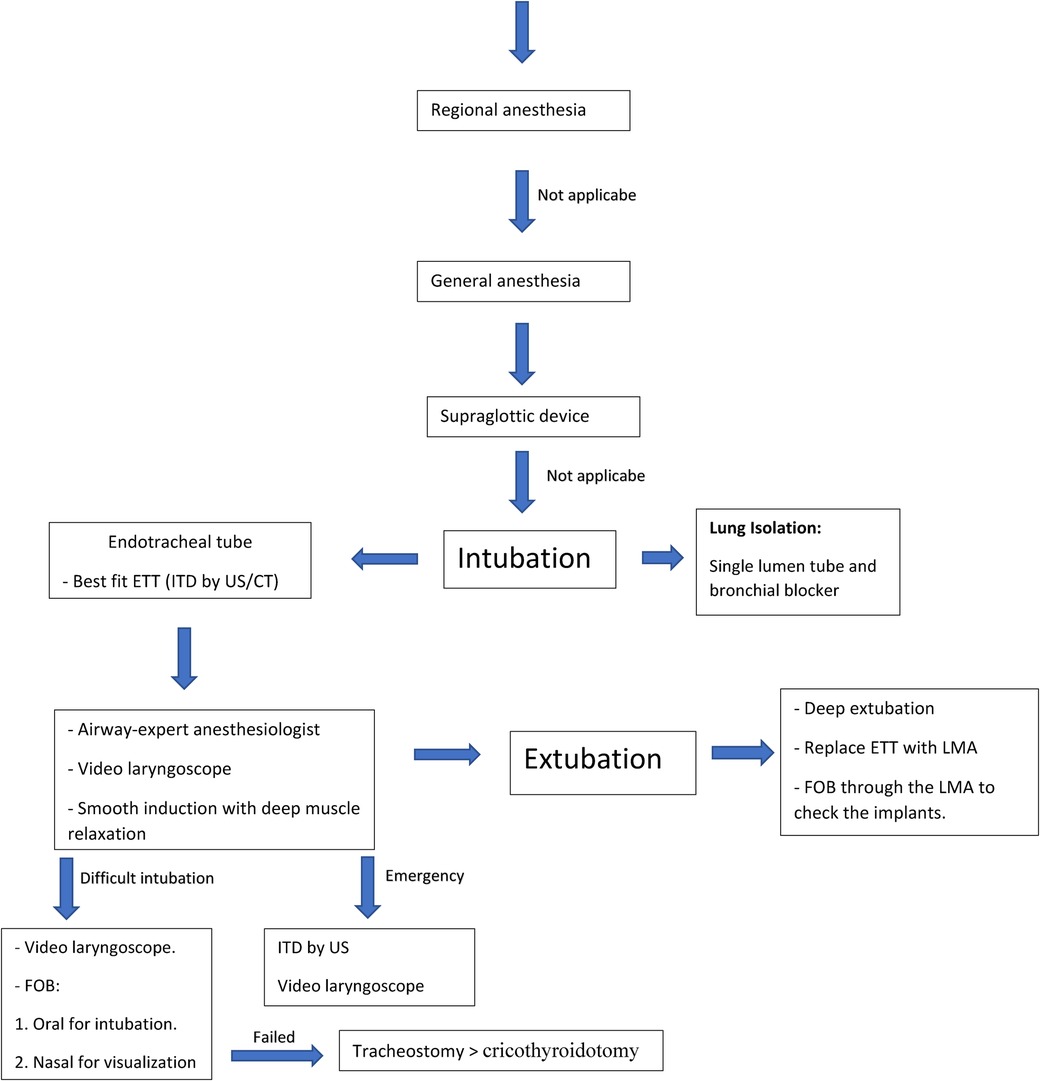
Vocal fold implants (VFI) are used to manage glottis insufficiency, restore proper vocal cord functioning, and prevent aspiration. Implants with different physical properties are made from various materials. Patients with VFI present challenging airways. Perioperative physicians should recognize several considerations when confronting airway management in the setting of VFI. A preoperative assessment of patients with a VFI by a multidisciplinary team specialized in airway management is crucial. The best-fitting endotracheal tube and intubation technique can minimize the risk of implant displacement. The present investigation provides different options for airway management in the setting of VFI and describes solutions for special situations such as lung isolation and difficult intubation. An algorithm is presented as a visual tool to help anesthesiologists who encounter such patients for safe airway management while preserving the VFI.
Introduction
Vocal fold implants (VFI) are used to manage glottis insufficiency (GI), restore proper vocal cord functioning, and prevent aspiration. Patients with VFI present uncommon challenges for anesthesiologists who deal with their airways. The major risk during endotracheal intubation is displacing the VFI, which can instantly obstruct the airway and threaten the life of the patient. Another risk is the loss of phonation. Moreover, the VFI causes changes in the vocal folds making them more prone to injury during airway instrumentation.
Therefore, recognizing and planning for this unique situation are key issues in safe airway management. Perioperative physicians should recognize several considerations when confronting such a situation. To date, no review articles have discussed the proper airway management for such patients with VFI. This review aims to evaluate the airway of patients with VFI and tailor the optimal plan for airway management while preserving the implant in place.
VFI
History of VFI
The therapeutics of vocal cord insufficiencies remained unknown over the past centuries. In 1911, Brunings (1) first described paraffin injection of a patient’s vocal folds under general anesthesia through a direct laryngoscopy to substantially ameliorate and restore the voice of the patient. Many new types and techniques have been implemented since then. In 1962, Godfrey Edward Arnold used Teflon in injection laryngoplasty (IL). However, Teflon was discontinued due to its postoperative granuloma formation as a disastrous complication (2). Over time, various materials have been used for IL, such as gel foam, carboxymethylcellulose, collagen, hyaluronic acid, calcium hydroxyapatite, and autologous fat (3). Correspondingly, in 1915, Erwin Payr proposed the idea of realigning the vocal fold with a surgical intervention called medialization laryngoplasty or thyroplasty. Payr created a cartilaginous flap from the thyroid ala to medialize the laryngeal fold, thus introducing alteration to a laryngeal framework to medialize the vocal cords. This method gained notability in 1974 when Isshiki et al. proposed the technique of thyroplasty to alter the laryngeal framework and restore normal laryngeal function. The method of Isshiki et al. (5) involved inserting of a solid implant, i.e., a silicon wedge, through a window in the thyroid cartilage. Montgomery, titanium, silicone, and layered Gore-Tex are common materials for thyroplasty implants (4). Recently, medialization thyroplasty has been established for medializing the vocal fold and reducing the glottis gap.
Indications for VFI
Laryngeal framework surgeries and IL are interventions used to manage GI and restore proper vocal cord functioning. GI is described as partial closure of vocal cords when phonating, resulting in inappropriate air leakage and vibration loss (6). Rationally, there are two types of GI causes, namely, paralytic and non-paralytic. The paralytic causes include vocal cord paralysis and paresis (6).
The primary indication for vocal cord implants in adults is unilateral vocal fold paralysis (7). Nouraei et al. (8) surveyed unilateral vocal fold immobility showing an incidence of 5.13 per 100,000 annually. Medialization thyroplasty is regarded as the gold standard method for gap reduction between the vocal folds in such cases (9).
The non-paralytic causes of GI may include traumatic injury to the neck, nerve injury, tumors, inflammation, and neurological conditions such as Parkinson's disease in adults (6). Bilateral vocal cord paralysis is a congenital idiopathic condition that ranks second among laryngeal malformations in pediatric patients (10). Perpetuity in the conditions often requires surgical interventions such as cordotomy, arytenoidectomy, and thyroplasty (11).
Types of vocal cord implants
Injection laryngoplasty
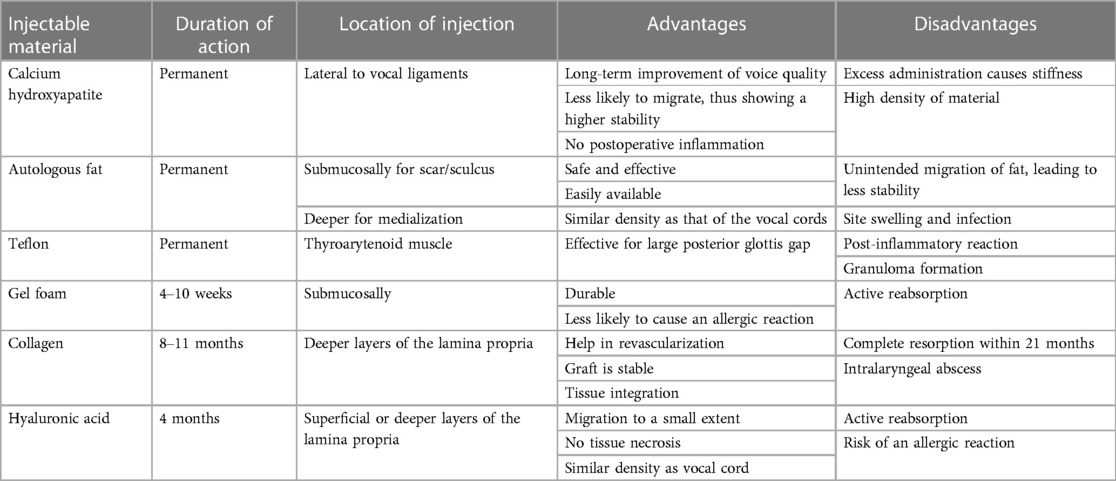
VFI has two main processes, namely, IL (liquid implants) and thyroplasty (solid implants). Transcutaneous IL is a minimally invasive technique characterized by injecting a biodegradable material into the paralyzed vocal cord with the help of endoscopic visualization (12). The injectable substances involved are either permanent materials, such as calcium hydroxyapatite autologous fat and Teflon, or temporary substances, such as gel foam, collagen, and hyaluronic acid. Each material possesses contrasting characteristics based on the duration of action and stability (Table 1) (13–19).
Medialization thyroplasty
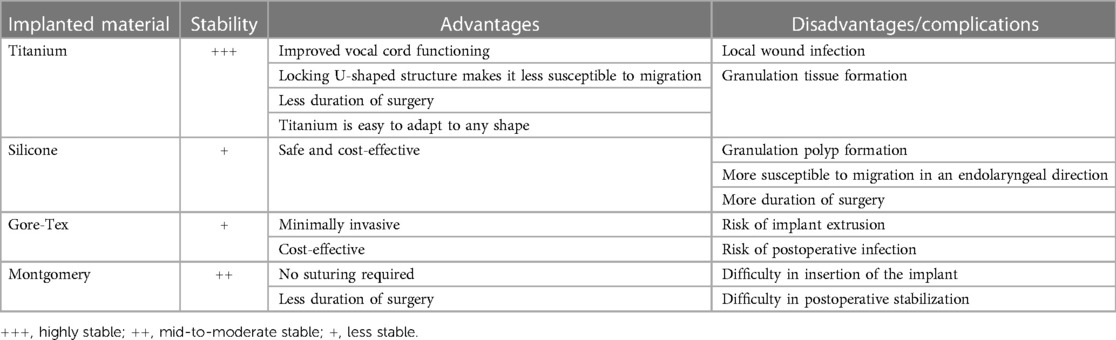
In 1974, Isshiki et al. proposed the idea of thyroplasty, which involves cutting and reshaping the thyroid cartilage to cure laryngeal insufficiencies. Thyroplasty is widely accepted and frequently observed to medialize the vocal cords and improve all kinds of glottis insufficiencies (20, 21). Techniques to perform medialization thyroplasty have improved over the recent years, and better materials for implants have been discovered. Various implants are used to fix the vocal folds medially during thyroplasty. These implants come in different sizes and materials, and the most commonly used implants are Montgomery, titanium, hand-carved silicone, or layered Gore-Tex (Table 2) (22).
Although silicon vocal cord implants are commonly used with desirable outcomes, new research has found that silicone implants do not adhere to the thyroid cartilage and have a higher risk of migration into an endolaryngeal direction, reducing the stability and being undesirable for future surgeries and intubations (23).
A novel titanium vocal cord implant is a safe and much better option to achieve desirable outcomes. Titanium vocal cord implants are extremely durable due to their U-shaped structure, which firmly adheres to the thyroid cartilage and resists migration (24).
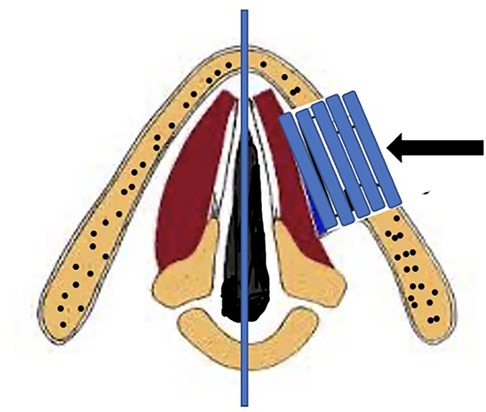
A minimally invasive vocal cord medialization technique is the use of Gore-Tex implants (Figure 1), which are commonly preferred for unilateral vocal cord paralysis. A study by Giovanni et al. (25) evaluated the results of vocal cord medialization using Gore-Tex implants and found that only one out of the 13 cases undergoing the procedure showed migration, while all had improved vocal functionally. Another literature review attributed the causes of Gore-Tex extrusion to large size used and coincident hematoma, especially in women (26). Therefore, the anesthesiologist should pay attention to the type of implant used.
Montgomery vocal cord implants (Figure 2) have been designed over recent years for an effective and practical treatment of unilateral laryngeal nerve palsy. A study by Laccourreye et al. (27) found that no adverse reaction was observed in 79.8% of cases and displacement was observed in only 2% of cases, thus showing a satisfactory response regarding stability.
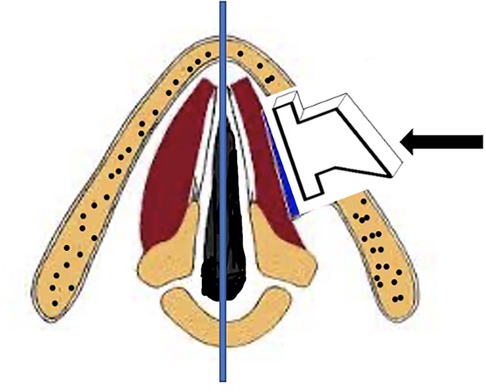
Figure 2. Larynx: post-medialization using a patient-specific, customized implant (arrow: pre-sized implant).
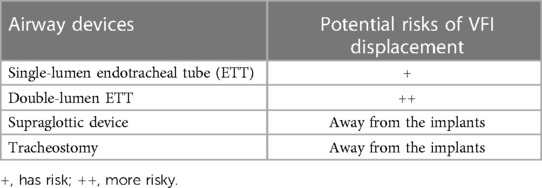
Airway management
Safe airway management is one of the crucial steps in the anesthetic management of any surgery. In the setting of VFI, airway management is more complicated because it poses higher risks and requires a careful approach to secure the airway without displacing the implants. Therefore, regional anesthesia should be a safer alternative if applicable for patients without contraindications. In case general anesthesia is inevitable, the new generations of supraglottic devices might be a wise choice to avoid encountering the implants (28) (Table 3). However, a definite plan for tracheal intubation should be always ready (Algorithm 1).
Multidisciplinary team
The multidisciplinary team involving airway-expert anesthesiologists, laryngologists, and radiologists enables a comprehensive airway assessment of such patients. The team should inform the patient about the potential risks of tracheal intubation, which may displace the VFI (29). Therefore, informed consent should be obtained, and the plan in case of implant displacement should be discussed with the patient, especially if immediate revision medialization laryngoplasty is involved.
Preoperative airway assessment
After the conventional anesthetic preoperative assessment of the patients, airway examination should be twofold. First, the anesthesiologist should obtain a meticulous history of the implant (type, duration, revision of implantation). As mentioned, the stability of the VFI and, consequently, the risk of displacement differ based on its type. Second, in addition to identifying the signs of difficult ventilation, the airway examination should involve visualization of the implant and an objective measurement of the internal transverse diameter (ITD) of the trachea for choosing the best-fitting endotracheal tube (ETT).
Visualization of the VFI
It is imperative to perform a preoperative flexible bronchoscope to evaluate VFI status (30). The laryngologist should document the status of the implants and report any related complications. Preoperative bronchoscopy also helps prepare the plan of endotracheal intubation and prevents encountering any unanticipated difficult airway.
Radiological assessment of the airway
Neck imaging by x-ray may help detect any metalwork in the airway. However, a neck computed tomography is more sensitive to show the characteristic imaging appearances of various implants (e.g., in case no reports of the VFI are available) and any related complications (31). The radiologist would be of great benefit here.
Best-fitting ETT
Proper selection of an ETT is vital to avoid a narrower size with more resistance and a larger one with more potential damage. The risk factors of the potential damage involve the type of ETT [double-lumen tube (DLT) and reinforced tubes may be more traumatic] and the type of surgery that necessitates positional change (and subsequently alteration of the tube position) (32). In addition, magnetic resonance imaging study of the vocal folds after medialization laryngoplasty demonstrated a three-dimensional structural change in the vocal folds. A recent study revealed a reduced medial-lateral dimension of the vocal fold and a 70% more stretch of the coronal plane (33). Moreover, after medialization thyroplasty, the glottic aperture becomes narrower in a non-compliant way because of the implant. These structural changes may make the vocal fold prone to injury during tracheal intubation much more than in the normal population.
Therefore, it is imperative to measure the ITD of the trachea to choose the best-fitting tube by relating ITD with the outer diameter of the tube and not the internal diameter of the tube, which is usually used for size measurement and smaller than the outer diameter of the tube. A study utilized the magnetic resonance image to measure the internal diameter of the trachea at the cricoid cartilage and found that it was more than the outer diameter of the best-fitting ETT by 0.1–1.7 mm (34). Neck ultrasound and computed tomography of the neck have comparable efficacy in measuring the internal diameter of the trachea (35, 36) (Figure 3).
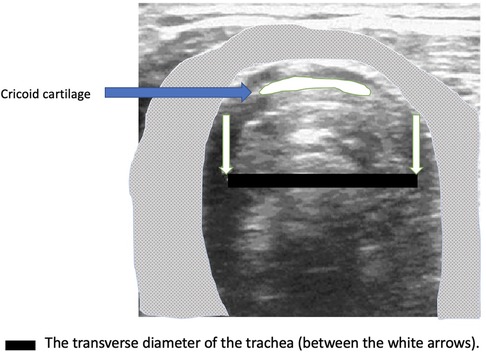
Figure 3. Measurement of the internal tracheal diameter by ultrasound (the anesthesiologist should put the linear probe of the ultrasound at the cricoid cartilage while the patient is in a sniffing position).
Intraoperative considerations
Attendance of the laryngologist throughout the operation, especially during tracheal intubation and extubation, is highly recommended.
Minimizing the number of intubation attempts and inserting the ETT away from the implant site may help decrease its potential contact with the implant. This necessitates that the anesthesiologist responsible for endotracheal intubation should be an airway expert. Attenuating the airway response to intubation and extubation should be considered to avoid bucking and coughing, which may lead to the displacement of unstable implants or injectable materials (37). Therefore, using neuromuscular blocking drugs and the confirmation of adequate paralysis with a nerve stimulator or quantitative neuromuscular monitoring prior to intubation is of utmost importance.
It is recommended to use a video laryngoscope, which can provide a better glottic view than the conventional laryngoscope (38). In addition, cautious inflation of the endotracheal cuff and continuous monitoring of the cuff pressure throughout the operation is paramount. Inadvertent syringe inflation may increase the cuff pressure and, subsequently, the volume to two times the internal diameter of the trachea, which could threaten the implant (39).
Tracheal extubation
Deep extubation and then ETT replacement with a laryngeal mask airway before emergence may reduce the stress forces of the implant and decrease respiratory complications. In addition, the laryngeal mask airway allows the passing of the fiber-optic bronchoscope (FOB) to assess the implant after the extubation (40). Therefore, it is possible to document the VFI status and then remove the laryngeal mask airway after full emergence from anesthesia.
Special consideration
Emergency intubation
In emergency intubation, there is no time for a comprehensive airway evaluation. Therefore, the anesthesiologist can utilize the ultrasound (more familiar and feasible) to measure the ITD of the trachea. Using a video laryngoscope and directing the ETT away from the implant side should be the proper technique. Examining the VFI with the FOB before extubation is crucial to show the implant status.
Single-lung ventilation
One-lung ventilation can be achieved using a DLT or bronchial blockers. However, the DLT poses higher risks of airway injury and the possibility of displacing the VFI (41). Therefore, isolating the lung with a bronchial blocker through a single-lumen tube would likely be a safer technique in this case (42, 43). Moreover, using the non-intubation technique (bronchial blocker via the laryngeal mask airway) may be a novel solution for lung isolation, which avoids the potential injury of the VFI with the ETT in selected patients (44).
Difficult intubation
Difficult intubation in the setting of the VFI poses a complicated challenge. Tracheal tube introducer (bougie), which is associated with a high incidence of airway injury, should be avoided (45). In the setting of awake intubation, using oral FOB is the gold standard (46). However, on railroading the ETT on the FOB, the FOB cannot visualize the area outside the ETT where it encounters the VFI. To avoid this blind spot, two options may be helpful. The first option is combining the oral FOB with a nasal FOB to visualize the tube while passing through the airway (47). The second option is replacing the FOB with video laryngoscopy for tracheal intubation, which has the same efficacy in awake intubation and provides better visualization of the glottic view (48).
Deep extubation may not be a proper technique in case of difficult intubation. Therefore, inserting a nasal FOB before emergence can visualize the ETT on removal and assess the implant position. Finally, in the case of the surgical airway, tracheostomy is more distant from the implant than the cricothyroidotomy. After securing the difficult airway, airway examination with FOB is important to detect any coincident implant displacement as we mentioned before extubation.
Future directions
One of the innovations in airway management is artificial intelligence. Implementing the artificial intelligence model can decrease the incidence of unexpectedly difficult airways by detecting accurately its morphological features (49).
The preoperative airway assessment may benefit from using nasal and virtual endoscopy, which improves the diagnostic accuracy of the various airway anatomical challenges (50). The former can be used by the anesthesiologist in awake patients, which may be very helpful in case of emergency intubation. The latter should improve the interpretation of the computed tomography images and guide a competent airway plan in such a situation.
The most interesting is the advances in the supraglottic airway devices with enhanced protection against aspiration which may be comparable to the ETT (51). In the management of patients with VFI, using these devices would avoid contact with the implant. In addition, the new generation facilitates using a flexible bronchoscopy, which can assist in the diagnosis of unexpected challenges, especially in difficult airways.
Conclusion
Airway management in the setting of VFI necessitates the cooperation of the multidisciplinary team to set a proper plan. The preoperative airway assessment should be shared between the laryngologist, radiologist, and anesthesiologist to visualize the implant and measure the internal transverse tracheal diameter to choose the best-fitting ETT. Attending an airway-expert anesthesiologist is crucial in managing and minimizing the risk of VFI displacement. Endotracheal intubation should be avoided whenever possible in patients with vocal cord implants. However, if it is necessary, ensuring deep muscle relaxation prior to intubation is very crucial. Video laryngoscope may be more helpful than both the conventional laryngoscope and the FOB for better visualization of the glottis. Deep extubation by replacing the ETT with a laryngeal mask airway and using FOB to check the implant status are medicolegally important. In addition to the challenges, awake intubation and emergency intubation mandate further management to save the airway and keep the implant in place., As regards single-lung ventilation isolating the lung with a bronchial blocker through a single-lumen ETT would likely be a safer technique than the sizable DLT.
Author contributions
IS, WM, AD, and IG wrote the manuscript. IU, OV, EC, and AK contributed to the revision and editing of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer AE declared a past co-authorship with IS to the handling editor at the time of the review.
IS declared that he was an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ETT, endotracheal tube; FOB, fiber-optic bronchoscope; FBI, fiber-optic intubation; GI, glottis insufficiency; IL, injection laryngoplasty; ITD, internal transverse diameter; VFI, vocal fold implants.
References
1. Brunings W. Uber eine neue behandlungsmethode der rekurrenslahmung. Verh Detsch Laryngol. (1911) 18:93–151.
2. Kasperbauer JL. Injectable Teflon for vocal cord paralysis. Otolaryngol Clin North Am. (1995) 28(2):317–23. doi: 10.1016/S0030-6665(20)30546-6
3. Salinas JB, Chhetri DK. Injection laryngoplasty: techniques and choices of fillers. Curr Otorhinolaryngol Rep. (2014) 2(2):131–6. doi: 10.1007/s40136-014-0038-9
4. Crolley V, Gibbins N. One hundred years of external approach medialisation thyroplasty. J Laryngol Otol. (2017) 131:1–7. doi: 10.1017/S0022215116010033
5. Isshiki N, Morita H, Okamura H, Hiramoto M. Thyroplasty as a new phonosurgical technique. Acta Otolaryngol. (1974) 78(1–6):451–7. doi: 10.3109/00016487409126379
6. Onwordi L. N., Al Yaghchi C. Airway glottic insufficiency. In StatPearls. Treasure Island, FL: StatPearls Publishing (2021).
7. Carroll TL. Unilateral vocal fold paralysis: practice essentials, history of the procedure, problem. Medscape. Available at: https://emedicine.medscape.com/article/863779-overview (Accessed November 28, 2021).
8. Nouraei SAR, Middleton SE, Butler CR, Sandhu GS. An estimation of the population incidence of adult unilateral vocal fold mobility impairment in England. Logopedics Phoniatrics Vocology. (2015) 40(2):93–4. doi: 10.3109/14015439.2014.902497
9. Chao TN, Mahmoud A, Rajasekaran K, Mirza N. Medialisation thyroplasty with tensor fascia lata: a novel approach for reducing post-thyroplasty complications. J Laryngol Otol. (2018) 132(4):364–7. doi: 10.1017/S0022215118000300
10. Xu W. Congenital disorders of the larynx. In: Atlas of strobolaryngoscopy. Singapore: Springer (2019). doi: 10.1007/978-981-13-6408-2_3
11. Li Y, Garrett G, Zealear D. Current treatment options for bilateral vocal fold paralysis: a state-of-the-art review. Clin Exp Otorhinolaryngol. (2017) 10(3):203–12. doi: 10.21053/ceo.2017.00199
12. Hamdan A-L, Mokarbel R, Dagher W. Medialization laryngoplasty for the treatment of unilateral vocal cord paralysis: a perceptual, acoustic and stroboscopic evaluation. J Med Liban. (2004) 52(3):136–41.16432970
13. Tsai YT, Tsai MS, Chang GH, Lee LA, Yang MY, Yang YH, et al. Patient-related factors of medialization laryngoplasty with autologous thyroid cartilage. Healthcare (Basel). (2020) 8(4):521. doi: 10.3390/healthcare8040521
14. Kwon T-K, An S-Y, Ahn J-C, Kim KH, Sung M-W. Calcium hydroxylapatite injection laryngoplasty for the treatment of presbylaryngis: long-term results. Laryngoscope. (2010) 120(2):326–9. doi: 10.1002/lary.20749
15. Khadivi E, Akbarian M, Khazaeni K, Salehi M. Outcomes of autologous fat injection laryngoplasty in unilateral vocal cord paralysis. Iran J Otorhinolaryngol. (2016) 28(86):215–9.27429951
16. Salmerón-González E, García-Vilariño E, Llópez-Carratalá I, Collado-Martin D, María Perolada-Valmaña J, Armengot-Carceller M. Augmentation of scarred vocal folds with centrifuged and emulsified autologous fat grafts. Otolaryngol Head Neck Surg. (2020) 163(6):1226–31. doi: 10.1177/0194599820932836
17. Hsiung MW, Woo P, Minasian A, Schaefer Mojica J. Fat augmentation for glottic insufficiency. Laryngoscope. (2000) 110(6):1026–33. doi: 10.1097/00005537-200006000-00026
18. Schramm VL, May M, Lavorato AS. Gelfoam paste injection for vocal cord paralysis: temporary rehabilitation of glottic incompetence. Laryngoscope. (1978) 88(8 Pt 1):1268–73. doi: 10.1288/00005537-197808000-00007
19. Zeitels SM, Lombardo PJ, Chaves JL, Faquin WC, Hillman RE, Heaton JT, et al. Vocal fold injection of absorbable materials: a histologic analysis with clinical ramifications. Ann Otol Rhinol Laryngol. (2019) 128(3_suppl):71S–81S. doi: 10.1177/0003489418805503
20. Schneider-Stickler B, Gaechter J, Bigenzahn W. Long-term results after external vocal fold medialization thyroplasty with titanium vocal fold medialization implant (TVFMI). Eur Arch Otorhinolaryngol. (2013) 270(5):1689–94. doi: 10.1007/s00405-013-2416-1
21. Anderson TD, Spiegel JR, Sataloff RT. Thyroplasty revisions: frequency and predictive factors. J Voice. (2003) 17(3):442–8. doi: 10.1067/s0892-1997(03)00080-8
22. Frost A, Mirza N. Gore-Tex implant extrusion following revision medialization thyroplasty: case report and review of the literature. World J Otorhinolaryngol Head Neck Surg. (2022) 8:213–6. doi: 10.1016/j.wjorl.2020.08.001
23. Van Ardenne N, Vanderwegen J, Van Nuffelen G, De Bodt M, Van de Heyning P. Medialization thyroplasty: vocal outcome of silicone and titanium implant. Eur Arch Otorhinolaryngol. (2011) 268(1):101–7. doi: 10.1007/s00405-010-1327-7
24. Friedrich G. Titanium vocal fold medializing implant: introducing a novel implant system for external vocal fold medialization. Ann Otol Rhinol Laryngol. (1999) 108(1):79–86. doi: 10.1177/000348949910800112
25. Giovanni A, Vallicioni JM, Gras R, Zanaret M. Clinical experience with Gore-Tex for vocal fold medialization. Laryngoscope (1999) 109 (2 Pt 1), 284–8. doi: 10.1097/00005537-199902000-00020
26. Watanabe K, Hirano A, Honkura Y, Kashima K, Shirakura M, Katori Y. Complications of using Gore-Tex in medialization laryngoplasty: case series and literature review. Eur Arch Otorhinolaryngol. (2019) 276:255–61. doi: 10.1007/s00405-018-5204-0
27. Laccourreye O, Sharkawy L, Holsinger C, Hans S, Ménard M, Brasnu D. Thyroplasty type I with Montgomery implant among native French language speakers with unilateral laryngeal nerve paralysis. Laryngoscope. (2005) 115:1411–7. doi: 10.1097/01.mlg.0000168059.12949.a6
28. Sip M, Dabrowska A, Prucnal K, Puslecki M, Klosiewicz T. Supraglottic devices—future or everyday life? Disaster Emerg Med J. (2017) 2(2):74–83. doi: 10.5603/DEMJ.2017.0015
29. Ayala MA, Patterson MB, Bach KK. Late displacement of a Montgomery thyroplasty implant following endotracheal intubation. Ann Otol Rhinol Laryngol. (2007) 116(4):262–4. doi: 10.1177/000348940711600407
30. Heikkinen M, Mäkinen K, Penttilä E, Qvarnström M, Kemppainen T, Löppönen H, et al. Incidence, risk factors, and natural outcome of vocal fold paresis in 920 thyroid operations with routine pre-and postoperative laryngoscopic evaluation. World J Surg. (2019) 43(9):2228–34. doi: 10.1007/s00268-019-05021-y
31. Vachha BA, Ginat DT, Mallur P, Cunnane M, Moonis G. “Finding a voice”: imaging features after phonosurgical procedures for vocal fold paralysis. Am J Neuroradiol. (2016) 37(9):1574–80. doi: 10.3174/ajnr.A4781
32. Lim H, Kim JH, Kim D, Lee J, Son JS, Kim DC, et al. Tracheal rupture after endotracheal intubation-a report of three cases. Korean J Anesthesiol. (2012) 62(3):277. doi: 10.4097/kjae.2012.62.3.277
33. Zhang Z, Wu L, Gray R, Chhetri DK. Three-dimensional vocal fold structural change due to implant insertion in medialization laryngoplasty. PLoS One. (2020) 15(1):e0228464. doi: 10.1371/journal.pone.0228464
34. Al-Mazrou KA, Abdullah KM, Ansari RA, Abdelmeguid ME, Turkistani A. Comparison of the outer diameter of the ‘best-fit’ endotracheal tube with MRI-measured airway diameter at the cricoid level. Eur J Anaesthesiol. (2009) 26:736–9. doi: 10.1097/EJA.0b013e32832aaccd
35. Altun D, Orhan-Sungur M, Ali A, Özkan-Seyhan T, Sivrikoz N, Çamcı E. The role of ultrasound in appropriate endotracheal tube size selection in pediatric patients. Pediatric Anesthesia. (2017) 27(10):1015–20. doi: 10.1111/pan.13220
36. Jain K, Gupta N, Yadav M, Thulkar S, Bhatnagar S. Radiological evaluation of airway—what an anaesthesiologist needs to know! Indian J Anaesth. (2019) 63(4):257. doi: 10.4103/ija.IJA_488_18
37. Bock JM, Lee JH, Robinson RA, Hoffman HT. Migration of Cymetra after vocal fold injection for laryngeal paralysis. Laryngoscope. (2007) 117(12):2251–4. doi: 10.1097/MLG.0b013e3181462a16
38. Hirabayashi Y, Hoshijima H, Kuratani N. Efficacy of glidescope video laryngoscope in difficult airways: a meta-analysis of randomized controlled trials. Masui. (2013) 62(8):996–1002.23984585
39. Bernet V, Dullenkopf A, Maino P, Weiss M. Outer diameter and shape of paediatric tracheal tube cuffs at higher inflation pressures. Anaesthesia. (2005) 60:1123–8. doi: 10.1111/j.1365-2044.2005.04359.x
40. Suppiah RK, Rajan S, Paul J, Kumar L. Respiratory and hemodynamic outcomes following exchange extubation with laryngeal mask airway as compared to traditional awake extubation. Anesth Essays Res. (2016) 10(2):212–7. doi: 10.4103/0259-1162.174469
41. Campos J. Lung isolation. In: Slinger P, editor. Principles and practice of anesthesia for thoracic surgery. Cham: Springer (2019). p. 247–58. doi: 10.1007/978-3-030-00859-8_16
42. Bhandary SP, Shehata IM, Richter E, Klopman M. Lung isolation in the setting of vocal cord implantation. J Cardiothorac Vasc Anesth. (2022) 36(8 Pt B):3129–30. doi: 10.1053/j.jvca.2021.10.034
43. Shehata IM, Elhassan A, Zaman B, Viswanath O. Challenge of lung isolation in patients with vocal cord implants. Anesth Pain Med. (2022) 12(1). doi: 10.5812/aapm.123370
44. Cao XH, Zhang W, Huang L, Hu ZY. Use of the bronchial blocker via laryngeal mask airway for one-lung ventilation in children undergoing thoracoscopic surgery: a randomized controlled study. Authorea. (2020). doi: 10.22541/au.160139711.19979243
45. Shehata IM, Hashim RM. Pneumomediastinum, pneumothorax, pneumoperitoneum, and subcutaneous emphysema complicating extubation of a difficult airway using an airway exchange catheter: is oxygen insufflation innocent?: a case report. A&A Practice. (2020) 14(7):e01228. doi: 10.1213/XAA.0000000000001228
46. Langeron O, Bourgain JL, Francon D, Amour J, Baillard C, Bouroche G, et al. Difficult intubation and extubation in adult anaesthesia. Anaesthesia Crit Care Pain Med. (2018) 37(6):639–51. doi: 10.1016/j.accpm.2018.03.013
47. Gorlin A, Susarla SM, Chatburn J, Jiang Y. Use of a second fiberoptic bronchoscope to guide oral fiberoptic intubation in 2 patients with existing vocal cord injury. J Oral Maxillofac Surg. (2011) 69(2):546–50. doi: 10.1016/j.joms.2010.09.012
48. Jiang J, Ma DX, Li B, Wu AS, Xue FS. Videolaryngoscopy versus fiberoptic bronchoscope for awake intubation—a systematic review and meta-analysis of randomized controlled trials. Ther Clin Risk Manag. (2018) 14:1955–63. doi: 10.2147/TCRM.S172783
49. Cuendet GL, Schoettker P, Yüce A, Sorci M, Gao H, Perruchoud C, et al. Facial image analysis for fully automatic prediction of difficult endotracheal intubation. IEEE Trans Biomed Engineering. (2015) 63(2):328–39. doi: 10.1109/TBME.2015.2457032
50. Myatra SN, Dhawan I, D’Souza SA, Elakkumanan LB, Jain D, Natarajan P. Recent advances in airway management. Indian J Anaesth. (2023) 67(1):48–55. doi: 10.4103/ija.ija_26_23
51. Priya H, Sripriya R, Ravishankar M, Karthikeyan P, Charulatha R. Baska mask is non-inferior to tracheal tube in preventing airway contamination during controlled ventilation in elective nasal surgeries: a randomised controlled trial. Indian J Anaesth. (2021) 65(8):586. doi: 10.4103/ija.IJA_237_21
Keywords: vocal fold implants, airway management, anesthesia, endotracheal intubation, ultrasound
Citation: Shehata IM, Masood W, Daebis A, Gamal I, Urits I, Viswanath O, Cornett EM and Kaye AD (2023) Airway management considerations in patients with vocal fold implants. Front. Anesthesiol. 2:1209229. doi: 10.3389/fanes.2023.1209229
Received: 20 April 2023; Accepted: 2 October 2023;
Published: 3 November 2023.
Edited by:
Hong Liu, UC Davis Health, United StatesReviewed by:
Christian Bohringer, UC Davis Medical Center, United StatesMasood Mohseni, Iran University of Medical Sciences, Iran
Amaresh Vydyanathan, Montefiore Medical Center, United States
© 2023 Shehata, Masood, Daebis, Gamal, Urits, Viswanath, Cornett and Kaye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Islam Mohammad Shehata aXNsYW0uc2hlaGF0YUBtZWQuYXN1LmVkdS5lZw==
 Islam Mohammad Shehata
Islam Mohammad Shehata Waniyah Masood
Waniyah Masood Ahmad Daebis
Ahmad Daebis Islam Gamal
Islam Gamal Ivan Urits4
Ivan Urits4 Elyse M. Cornett
Elyse M. Cornett