
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Anesthesiol. , 06 December 2022
Sec. Cardiothoracic Anesthesiology
Volume 1 - 2022 | https://doi.org/10.3389/fanes.2022.987378
A 50-year-old women presented with a history of fatigue after activities. Transthoracic echocardiography showed a 2.8 cm dilatation at the ostium of the left coronary artery and a 7.1 × 7.4 cm cyst-like aneurysm at the upper back of the left atrium, interlinking an anomalous fistula from the left coronary artery to the right atrial appendage, accompanied by moderate mitral and tricuspid regurgitation. Cardiac 3D-computed tomography confirmed the diagnosis of a ruptured aortic sinus aneurysm (RASA) and a giant left coronary artery aneurysm fistula to the right atrium. A transesophageal echocardiogram and surgical vision confirmed these findings. Surgeries, including RASA repair, coronary artery bypass grafting, and mitral and tricuspid valvuloplasty, were then performed. The procedures proceeded successfully, and the patient fully recovered and was discharged home.
Coronary artery anomaly (CAA) is a common cause of sudden cardiac death, a congenital disease relating to the abnormal coronary origin, course, and termination [1]. Coronary artery fistula (CAF) is an abnormally terminated CAA with a low prevalence (0.2–0.6%) and is usually detected incidentally during the diagnostic examination for ischemic heart diseases [2]. Ischemic symptoms of CAF are caused by coronary steal where coronary blood flows into low-pressure areas of the fistula (e.g., right ventricle, right atrium, pulmonary artery, or coronary sinus), resulting in distal myocardium ischemia. The latest data show that CAF accounts for 0.32% of total coronary anomalies in Southwest China as determined by angiography [3]. In particular, a giant left coronary artery aneurysm that connects by fistula to the right atrium accompanied by a ruptured aortic sinus aneurysm (RASA) has been rarely reported. Notably, even asymptomatic coronary fistulas can lead to severe complications, such as endocarditis, coronary aneurysms, myocardial infarction, or cardiac arrest. Therefore, catheter-based closure or surgical therapy is often needed for coronary fistulae.
A 50-year-old woman presented to a community clinic due to fatigue after activities and was primarily diagnosed with a giant left coronary artery aneurysm. On admission, she reported not to have had previously received any surgery or special medication. She had no history of hypertension, diabetes, Kawasaki disease, or a family history of heart disease. Physical examination revealed a left-inferior enlargement of the cardiac border. The electrocardiogram showed sinus rhythm, T-wave changes, premature atrial contractions, and left ventricular hypervoltage. Blood pressure was normal and maintained at 100–120/70–80 mmHg. There were grades 3 to 6 systolic murmurs in the auscultatory mitral area. Chest x-ray showed left atrioventricular enlargement and right coronary artery calcification. Transthoracic echocardiography (TTE) indicated a 7.1 × 7.4 cm cyst-like aneurysm at the upper back of the left atrium, which originated from the left coronary artery, detoured to the left posteriorly, and broke into the right atrial appendage, accompanied by moderate mitral and tricuspid regurgitation (Figures 1A–C). Concurrently, the left coronary artery ostium dilated up to 2.8 cm, and the possibility of RASA should be further precluded. Then, cardiac three-dimensional computed tomography (3D-CT) was recommended to reconstruct the aneurysm. Cardiac 3D-CT revealed RASA of the left coronal sinus and an aneurysm-like fistula connecting the left main coronary artery with the right atrium, squeezing the right pulmonary vein and the left atrium (Figure 2).
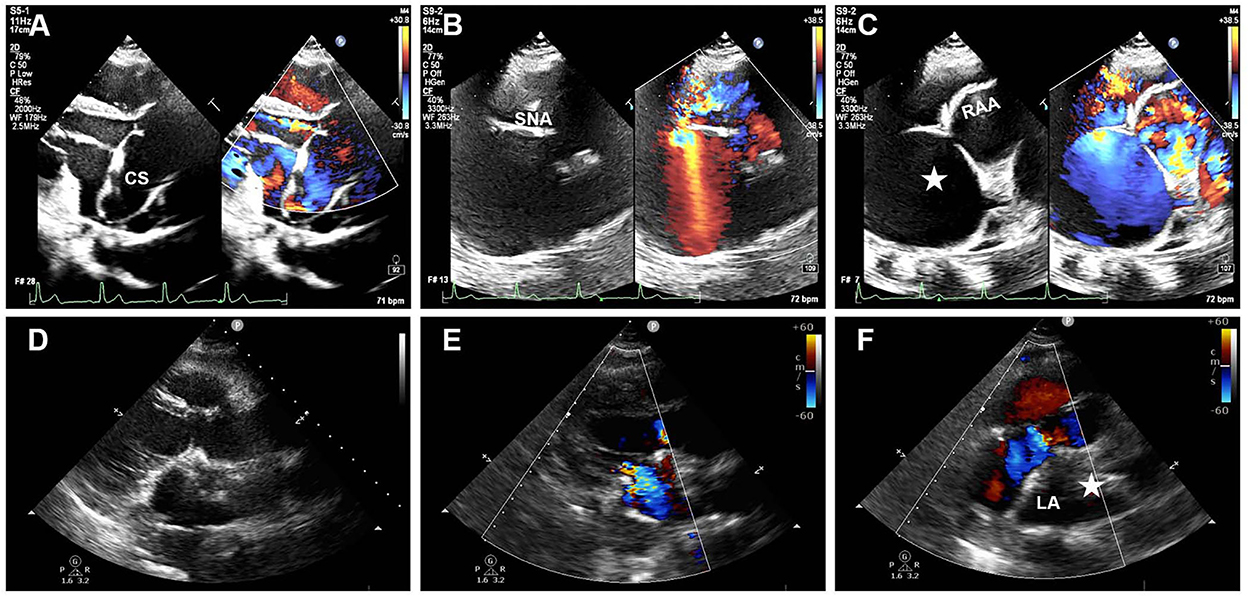
Figure 1. Pre- and postoperative TTE images. (A) Pre-TTE parasternal long-axis view reveals dilated left coronary sinus (CS). (B) Color Doppler imaging with systolic aliased flow in the sinus node artery (SNA). (C) Apical four-chamber view shows a 7.1 × 7.4 cm giant aneurysm (white star) fistula into the right atrial appendage (RAA). (D–F) Post-TTE shows a hypoechogenic mass of collapsed aneurysm (white star) in the posterior of the left atrium (LA).
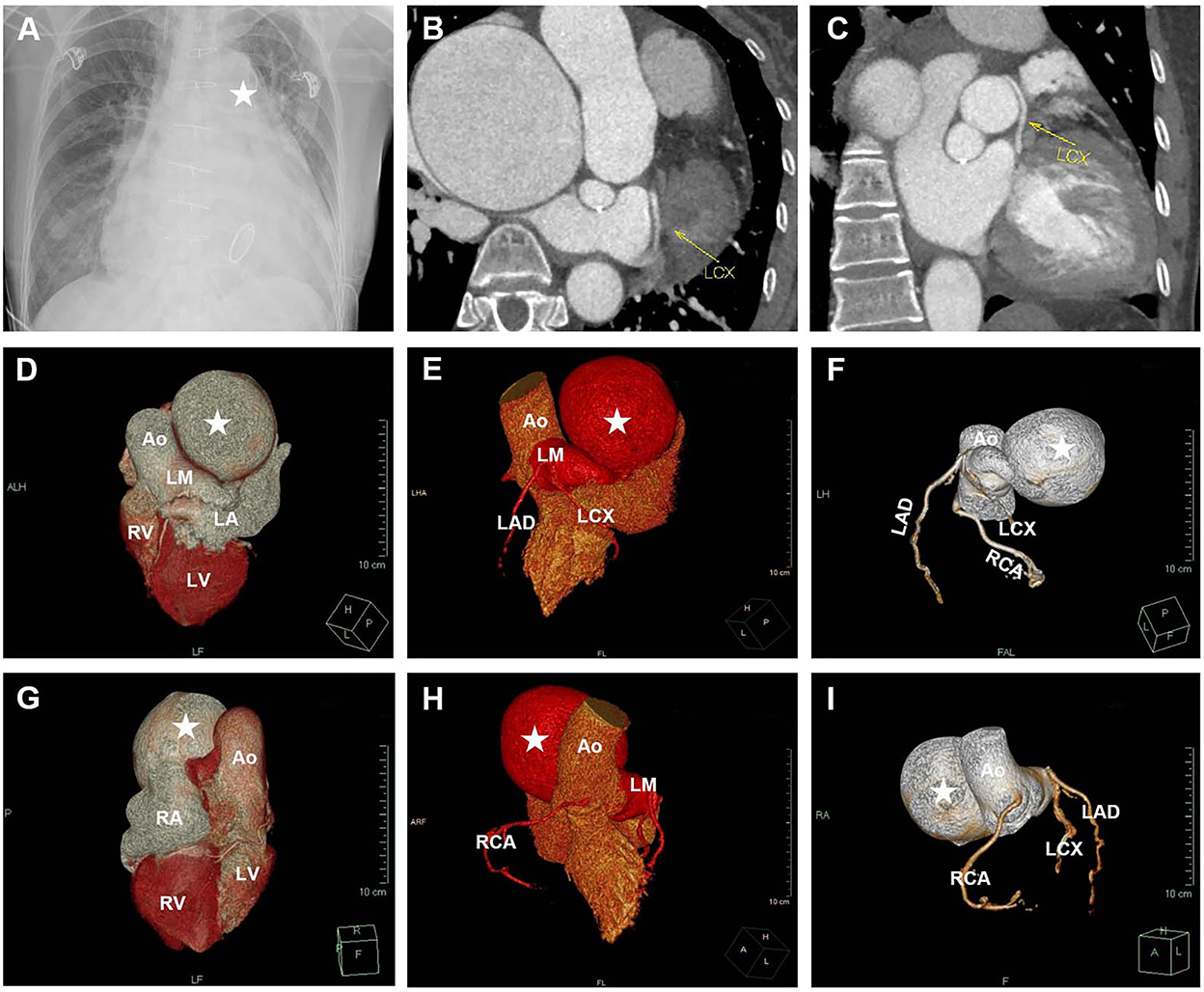
Figure 2. Multimodality image examination. (A) Chest X-ray shows a mass (white star) abutting the left atrium border. (B,C) Cardiac CT reveals a giant aneurysm in the distal left coronary artery. (D–I) Cardiac 3D-CT indicated that the origin and course of coronary arteries were normal. The left coronary sinus sent out a thick blood vessel branch, connecting a giant left main (LM) coronary artery aneurysm (white star) fistula to the right atrium. AO, aorta; LAD, left anterior descending; LCX, left circumflex; RCA, right coronary artery; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.
During the operation, a transesophageal echocardiogram (TEE) and surgical vision confirmed these findings (Figure 3, Supplementary Videos 1–3). Under cardiopulmonary bypass, the patient underwent RASA repair, coronary artery bypass grafting (great saphenous vein graft to the left anterior descending and circumflex branches), mitral and tricuspid valvuloplasty, and temporary pacemaker implantation. Following the operation, TEE confirmed that there was no flow in the fistula at the right atrium, and the aneurysm in the posterior wall of the left atrium collapsed. Intraoperative hemodynamics were stable without obvious malignant arrhythmia. The patient fully recovered and was discharged home 14 days after the operation. At the follow-up 1 month after surgery, the electrocardiogram and myocardial injury markers were all normal. Postoperative TTE revealed normal systolic and diastolic function with a hypoechoic collapsed aneurysm mass in the posterior of the left atrium (Figures 1D–F).
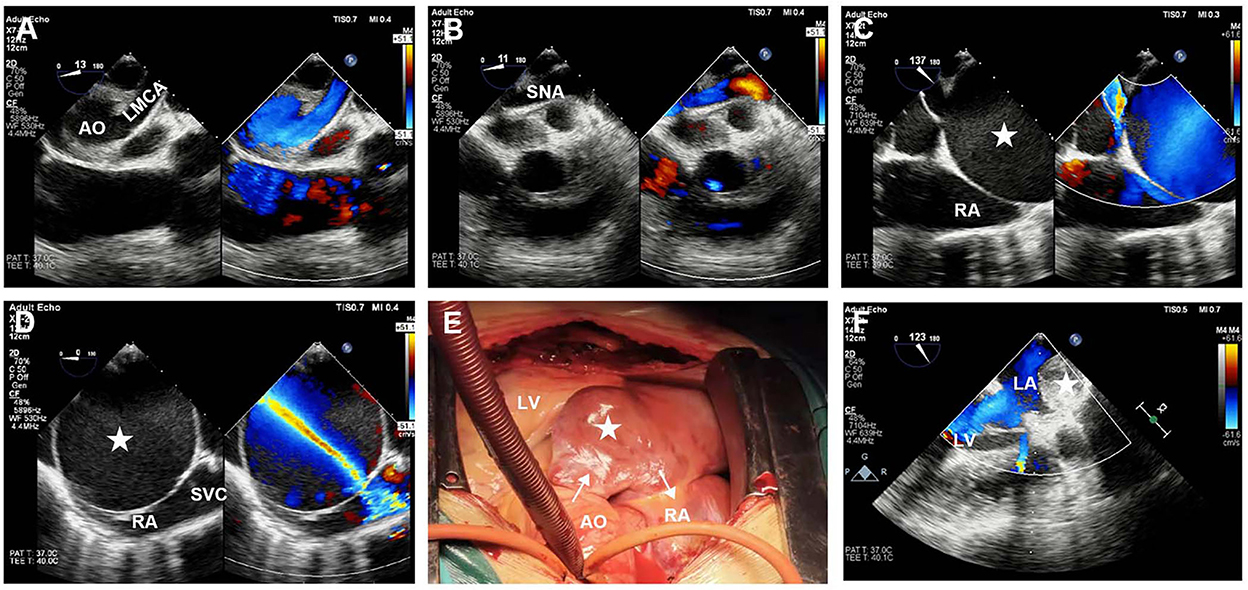
Figure 3. Intraoperative TEE and surgical images. (A) Pre-TEE shows an aneurysmal dilation of left main coronary artery (LMCA) origin. (B) Color Doppler imaging with systolic aliased flow in the sinus node artery (SNA). (C,D) Pre-TEE bicaval view reveals an aneurysm-like fistula from the left main coronary to the right atrium (RA), which is adjacent to the superior vena cava (SVC). (E) A collapsed left coronary aneurysm under cardiopulmonary bypass. (F) Post-TEE long-axis view reveals a collapsed aneurysm in the posterior of the left atrium. The white star represents the aneurysm.
Of all types of CAF, a left coronary fistula to the right atrium with a giant left coronary aneurysm is rare [4]. It has been reported that 90% of CAFs originate from the right coronary artery, of which only 0.2% are accompanied by giant coronary aneurysms (> 4 times the normal diameter) [5]. CAF often has no specific clinical manifestations, with or without angina pectoris and cardiac murmur, which are closely affected by the location and size of the fistula. Although optimal treatment for CAF remains controversial, transcatheter closure of the fistula, surgical resection of the aneurysm, and bypass grafting of the coronary artery are the most common approaches [6]. Multimodal imaging and functional testing often play vital roles in the diagnosis of CAFs. Specifically, coronary angiography and cardiac CT are universal methods for diagnosing and tracking the anatomical abnormalities of the coronary arteries. However, coronary angiography is invasive, and CT often misses tiny breaks. In the present case study, we proved that TTE and TEE are necessary and sufficient to determine the complex anatomy of a coronary fistula and its relationship to adjacent structures and can be used for preoperative, intraoperative, and postoperative assessments. Echocardiography has the advantages of being noninvasive, real-time, and inexpensive, especially in the detection of fistula rupture and location by color Doppler. It is worth noting that the echocardiographic images of this patient need to be differentiated from images of the three-atrial heart, because the apical four-chamber view of TTE may easily mistake the aneurysm wall for the right atrial septum and mistake the fistula for the septal hole.
The original contributions presented in the study in the are included article/Supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Ethics Management Committee of West China Hospital of Sichuan University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
WX, JL, and HS conceived the presented idea. WX, WL, and LT wrote the manuscript. WX made the videos. WL and LT drew the figures. JL and HS revised the manuscript. All authors have read and approved the final version of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fanes.2022.987378/full#supplementary-material
Supplementary Video 1. Mid-esophageal four-chamber view demonstrating an aneurysmal dilation of the left coronary sinus of the aorta with moderate mitral and tricuspid regurgitation.
Supplementary Video 2. Mid-esophageal bicaval view showing an aneurysmal fistula drain into the right atrium.
Supplementary Video 3. Mid-esophageal long-axis view revealing a collapsed aneurysm in the posterior of the left atrium.
1. Gentile F, Castiglione V, De Caterina R. Coronary artery anomalies. Circulation. (2021) 144:983–96. doi: 10.1161/CIRCULATIONAHA.121.055347
2. Han JS, Overgaard C. Left main coronary artery to right atrium fistula causing acute cardiac failure and arrest. JACC Cardiovasc Interv. (2021) 14:e197–8. doi: 10.1016/j.jcin.2021.05.030
3. Jiang X, Zhou P, Wen C, Yin Z, Liu T, Xu M, et al. Coronary anomalies in 11,267 southwest Chinese patients determined by angiography. Biomed Res Int. (2021) 2021:6693784–91. doi: 10.1155/2021/6693784
4. Brussee H, Gasser R. Images in clinical medicine. Fistula connecting the left main coronary artery with the right atrium in a marathon runner. N Engl J Med. (2002) 346:904. doi: 10.1056/NEJMicm980664
5. Wang L, Wang J, Cheng TO, Xie M, Wang X, Song Y, et al. Giant left coronary artery aneurysms: Review of the literature and report of a rare case diagnosed by transthoracic echocardiography. Int J Cardiol. (2015) 189:267–71. doi: 10.1016/j.ijcard.2015.04.082
Keywords: rupture of aortic sinus aneurysm, coronary artery aneurysm, right atrium fistula, transesophageal echocardiogram (TEE), transthoracic echocardiography (TTE)
Citation: Xiong W, Long W, Tang L, Liu J and Song H (2022) Case report: Ruptured aortic sinus aneurysm with left coronary artery aneurysm-right atrial fistula. Front. Anesthesiol. 1:987378. doi: 10.3389/fanes.2022.987378
Received: 06 July 2022; Accepted: 15 November 2022;
Published: 06 December 2022.
Edited by:
Martina Crivellari, San Raffaele Hospital (IRCCS), ItalyReviewed by:
Chiara Maria Marta Gerli, San Raffaele Hospital (IRCCS), ItalyCopyright © 2022 Xiong, Long, Tang, Liu and Song. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haibo Song, cGRhc29uZ2hhaWJvQDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.