
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Anesthesiol. , 30 November 2022
Sec. Critical Care Anesthesiology
Volume 1 - 2022 | https://doi.org/10.3389/fanes.2022.975523
Background: Difficult airway has always been one of the greatest challenges for anesthesiologists. Patients with difficult airways and severe obstructive sleep apnea-hypopnea syndrome (OSAHS) often find themselves in life-threatening danger before their artificial airway is established and after their artificial airway is removed.
Case presentation: The study reported a case of nasal polyps shedding into the tracheal tube when nasotracheal intubation in a patient diagnosed with a difficult airway and OSAHS; the patient was being prepared for a transoral tonsillectomy under general anesthesia. The uniqueness of this case was that nasal polyps were scraped off using the tracheal tube during nasotracheal intubation, and detected in real-time; this ultimately prevented an airway foreign body obstruction. Reviewing the literature on intubation methods for difficult airways, awake endotracheal intubation guided by fiberoptic bronchoscopy remains to be the gold standard for airway management. Additionally, nasotracheal intubation can provide more operating space for oral surgery. In this case, the unexpected nasal polyp fell off into the tracheal tube during intubation, as is visualized on the following pictures. This fortunate event prevented the nasal polyp from falling into the trachea and bronchus.
Conclusion: It is necessary to rule out any nasal abnormalities in patients requiring nasotracheal intubation; otherwise, blind nasal intubation may be dangerous.
Difficult airway involves difficult ventilation and intubation, with the former as high as 5% and the latter as high as 8% [1]. Obstructive sleep apnea-hypopnea syndrome (OSAHS) patients have a higher incidence of difficult airways than other patients [2]. Airway management in these patients is a major challenge for anesthesiologists.When a patient presents with a difficult airway and OSAHS, preserved spontaneous breathing and awake tracheal intubation are the safest approaches for airway management [2]. In this case, awake nasotracheal intubation was required due to a small mouth opening and the need for transoral surgery. Reports of nasal polyps being scraped off during nasal intubation in difficult airway patients are rare, and reports of nasal polyps being found after shedding are even rarer. In this report, we share the experience of administering anesthesia in a difficult airway patient with OSAHS and findings of nasal polyps being scraped off by the tracheal tube. The symptoms at presentation were sore throat and snoring for over a year. Monitoring of sleep breathing and laryngoscopy were performed. Informed consent was obtained from the patient.
The patient was a 33-year-old man with a sore throat who reports of snoring while sleeping for more than 1 year upon consultation. He slept with a ventilator 1 month before presentation to the hospital. During this period, he received pharmacological treatments and weight-loss treatment, but the effect was not obvious. This made him anxious. Physical examination revealed the following: weight, 84 kg; height, 160 cm; body mass index, 32.8 kg/m2; American Society of Anesthesiology (ASA) III physical status classification. Airway assessment revealed the following: inter-incisor distance, 5 cm; Mallampati class III; a small jaw, bucktooth, and stubby neck. WBC 10.02 × 109/L, NE 81.9%.Monitoring the patient's sleep breathing indicated severe OSAHS and 50% minimum oxygen saturation. Laryngoscopy indicated chronic tonsillitis, bilateral tonsillar enlargement, and a nasopharyngeal polyp (there was no indication if it was on the left or right side). A bilateral tonsillectomy under general anesthesia was ordered to relieve the symptoms of OSAHS and sore throat. These information suggested that the patient had a difficult airway. Due to the small opening of the mouth and the need for surgery through an oral approach, nasal awake intubation was required. Vital signs revealed a body temperature of 36.2°C, respiration rate of 22 breaths/min, blood pressure of 131/78 mmHg, pulse of 79 bpm, and oxygen saturation of 96%.
The patient described right-sided nasal obstruction; hence, we suspected a nasopharyngeal polyp on the right side. Local anesthesia of the upper respiratory tract was performed before intubation, involving 10% ephedrine and 2% lidocaine nasal drops, 2% lidocaine larynx spray, ultrasound-guided superior laryngeal nerve block, and cricothyroid membrane puncture anesthesia with 2% lidocaine; a total of 200 mg of 2% lidocaine was administered. Remifentanil 0.1 μg/kg/min was administered through the patient's veins. Once the local anesthetic has taken full effect, the tracheal tube, with an inner diameter of 6.5 cm, was gently inserted into the oral cavity through the left nasal cavity, and then the fiberoptic bronchoscope was inserted into the tracheal tube. To our surprise, we found a polyp attached to the tracheal tube (presented on Figure 1). First, we removed the tracheal tube with the attached polyp. Moreover, considering that the left nasal cavity was unobstructed and we were aiming to achieve compression hemostasis, we once again attempted tracheal intubation guided by a fiberoptic bronchoscope through the left nasal cavity. The patient did not complain of discomfort before the tube reached the trachea. When the tube entered the trachea, the patient's heart rate increased by about 15%; hence, we immediately increased the anesthesia concentration with intravenous propofol (0.15 mg/kg), sufentanil (0.3 μg/kg), and cisatracurium (0.15 mg/kg). For the maintenance of anesthesia, 1–2% sevoflurane was inhaled, and 0.1–0.2 μg/kg/min remifentanil was injected to maintain the bispectral index (BIS) at 40–60. The intraoperative vital signs were stable.
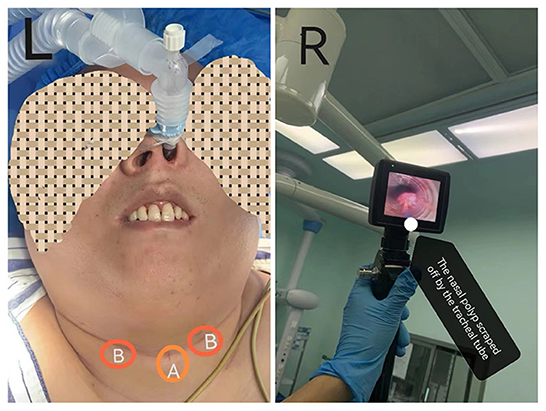
Figure 1. (L) Patient image after intubation. (A) The site of cricothyroid membrane puncturehe; (B) The site of superior laryngeal nerve block. (R) The nasal polyp scraped away by the tracheal tube.
Considering that the patient was prone to upper respiratory tract obstruction after surgery, the surgeon advised keeping the tracheal tube for 1 day. Therefore, after the surgery, the tracheal tube was not removed until the following day. The patient was discharged on the fourth postoperative day. Before discharge, he did not experience any apparent discomfort. He was satisfied with the results of surgical treatment. A visual timeline of this patient's anesthesia management is presented on Figure 2.
A difficult airway is a main topic of concern for anesthesiologists [1]. Patients with OSAHS have a higher incidence of difficult airways than other patients [2], and inappropriate airway planning or judgment errors may harm these patients [3]. Studies have shown that awake fiberoptic nasotracheal intubation (AFNI) guided by fiberoptic bronchoscopy can effectively avoid complications caused by tracheal intubation failure in OSAHS patients [4]. Therefore, patients with OSAHS often used AFNI [5]. This is a severe OSAHS patient with suspected difficult airway, awake tracheal intubation is certainly the safest way for him, but it might be more comfortable to try video-aided nasotracheal intubation.
Adequate upper airway anesthesia is important in patients with difficult airways requiring awake tracheal intubation; otherwise, the patient may not be able to tolerate intubation stimulation. Ultrasound has played an important role in the evaluation of a difficult airway [6], identification of the cricothyroid membrane puncture [7], and guidance of the superior laryngeal nerve block [8]. We took the following measures prior to surgery: adequate nasopharynx, oropharynx, and larynx surface anesthesia and ultrasound-guided superior laryngeal nerve block. The patient had a short neck; hence, we could not reach the cricothyroid membrane. Therefore, we located the puncture site for local anesthesia using an ultrasound and supplemented it with a small dose of remifentanil. With these measures, we achieved good cooperation from the patient during the intubation process.
Fiberoptic bronchoscopy is the gold standard for treating difficult airways [9], In recent years, video laryngoscopy was gradually recommended too [10]. In addition to local anesthesia, the use of small doses of sedative or analgesic drugs can achieve better patient cooperation [11, 12]. The combination of multiple measures can improve the chances of a successful intubation.
For oral surgery, nasal tracheal intubation can give doctors more room for operation. However, nasal intubation also has related complications, such as nasal bleeding, nasal pressure sore, increase risk of respiratory tract infection due to difficulty in disinfection of nasal cavity, etc.At the same time, the patient still has nasal polyps, and the his mouth opening can be put into the laryngoscope, and oral intubation may be able to meet the needs of the surgical operation. So our choice is debatable.For patients who must perform nasal intubation, how to avoid the occurrence of related complications [13]? First of all, it is necessary to exclude contraindications, such as skull base fracture or coagulation dysfunction. Secondly, do the necessary examination before intubation, especially nasopharyngoscopy to exclude nasal tumor, nasal stenosis or nasal septum deviation.Then, do nasal disinfection, reduce the risk of infection. Finally, the nasal surface anesthesia, contraction of nasal mucosa blood vessels, endotracheal tube cuff fully deflated and lubrication, softening catheter, take the patient's cooperation and so on equally important.
The strengths of this study inlcude adequate doctor-patient communication, adequate anesthesiologist-surgeon communication, adequate preoperative preparation, satisfactory surface anesthesia, and a perfect nerve block before intubation. The limitations of the study are as follows: laryngoscopy did not accurately describe the location of the nasopharyngeal polyp. So, we were only able to deduce from the patient's history that the nasal polyp was located on the right side. However, the nasal polyp being scraped off by the tracheal tube.we were unable to assess its original location and features further, because we have not used fiberoptic bronchoscope before the endotracheal tube went into the nasal cavity. Fortunately, we did not perform blind nasal intubation, which prevented the polyp from falling into the trachea and causing airway obstruction. At the same time, since the patient did not have massive nasal bleeding, the glottis was not difficult to expose.The patient had stable vital signs and no signs of discomfort during the entire duration of hospitalization.
In conclusion, if nasal abnormalities are not ruled out before nasal intubation, blind nasal intubation may be dangerous for patients.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
F-RB collected information and wrote the manuscript. SZ performed the anesthesia strategy. M-lY drafted the manuscript. All authors approved the final version.
We graciously thank the surgeons and the patient who supported us for this manuscript. We would also like to thank Editage for English language editing.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Heidegger T. Management of the difficult airway. N Engl J Med. (2021) 384:1836–47. doi: 10.1056/NEJMra1916801
2. Leong SM, Tiwari A, Chung F, Wong DT. Obstructive sleep apnea as a risk factor associated with difficult airway management - a narrative review. J Clin Anesth. (2018) 45:63–8. doi: 10.1016/j.jclinane.2017.12.024
3. Joffe AM, Aziz MF, Posner KL, Duggan LV, Mincer SL, Domino KB. Management of difficult tracheal intubation: a closed claims analysis. Anesthesiology. (2019) 131:818–29. doi: 10.1097/ALN.0000000000002815
4. Cabrini L, Baiardo Redaelli M, Ball L, Filippini M, Fominskiy E, Pintaudi M, et al. Awake fiberoptic intubation protocols in the operating room for anticipated difficult airway: a systematic review and meta-analysis of randomized controlled trials. Anesth Analg. (2019) 128:971–80. doi: 10.1213/ANE.0000000000004087
5. Ahmad I, El-Boghdadly K, Bhagrath R, Hodzovic I, McNarry AF, Mir F, et al. Difficult airway society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia. (2020) 75:509–28. doi: 10.1111/anae.14904
6. Gomes SH, Simões AM, Nunes AM, Pereira MV, Teoh WH, Costa PS, et al. Useful ultrasonographic parameters to predict difficult laryngoscopy and difficult tracheal intubation — a systematic review and meta-analysis. Front Med. (2021) 8:671658. doi: 10.3389/fmed.2021.671658
7. Kristensen MS, Teoh WH. Ultrasound identification of the cricothyroid membrane: the new standard in preparing for front-of-neck airway access. Br J Anaesth. (2021) 126:22–7. doi: 10.1016/j.bja.2020.10.004
8. Zhou C, Hu T, Fu J, Zhao X, Liu H, Guo H, et al. Ultrasound-guided superior laryngeal nerve block can reduce coughing scores, decrease the incidence of hypoxemia, and shorten examination times during bronchoscopy: a randomized controlled trial. J Clin Anesth. (2020) 63:109759. doi: 10.1016/j.jclinane.2020.109759
9. Johnston KD, Rai MR. Conscious sedation for awake fibreoptic intubation: a review of the literature. Can J Anaesth. (2013) 60:584–99. doi: 10.1007/s12630-013-9915-9
10. Alhomary M, Ramadan E, Curran E. Walsh SR. Videolaryngoscopy vs. fibreoptic bronchoscopy for awake tracheal intubation: a systematic review and meta-analysis. Anaesthesia. (2018) 73:1151–61. doi: 10.1111/anae.14299
11. Müller T, Cornelissen C, Dreher M. Nebulization versus standard application for topical anaesthesia during flexible bronchoscopy under moderate sedation - a randomized controlled trial. Respir Res. (2018) 19:227. doi: 10.1186/s12931-018-0926-5
12. Shah SV, Lacey O. A decade of using a remifentanil target-controlled infusion technique for awake fibreoptic intubations. Anaesthesia. (2021) 76:284–5. doi: 10.1111/anae.15226
Keywords: OSAHS, nasotracheal intubation, difficult airway, awake tracheal intubation, case report
Citation: Bai F-R, Zhang S and Yi M-l (2022) Case report: Nasal polyp exfoliated into the tracheal tube in a patient with a difficult airway during nasotracheal intubation. Front. Anesthesiol. 1:975523. doi: 10.3389/fanes.2022.975523
Received: 22 June 2022; Accepted: 17 October 2022;
Published: 30 November 2022.
Edited by:
Vincenzo Pota, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Francesco Coppolino, University of Campania Luigi Vanvitelli, ItalyCopyright © 2022 Bai, Zhang and Yi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ming-liang Yi, MTY4MjM3OTdAcXEuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.