- Faculty of Medicine and Health, School of Psychology, University of New England, Armidale, NSW, Australia
With the COVID-19 pandemic confronting health systems worldwide, medical practitioners are treating a myriad of physical symptoms that have, sadly, killed many thousands of people. There are signs that the public is also experiencing psychological trauma as they attempt to navigate their way through the COVID-19 restrictions impinging on many aspects of society. With unprecedented demand for health professionals' time, people who are unable to access face-to-face assistance are turning to smartphone apps to help them deal with symptoms of trauma. However, the evidence for smartphone apps to treat trauma is limited, and clinicians need to be aware of the limitations and unresolved issues involved in using mental health apps.
Introduction
Although many medical and allied health professionals are conducting telehealth sessions with patients and clients during the COVID-19 pandemic, the increased level of demand means that some people may not be able to access services in an adequate timeframe (1). In response, increasing numbers of sufferers are turning to digitized, automated options such as mobile applications (apps) (2). For people with symptoms of acute stress disorder, which if present for longer than a month is reclassified as posttraumatic stress disorder (PTSD) (3), mental health apps are potentially one way to access treatment and lessen the burden on primary health care.
It is no surprise that individuals are turning to digital options—over 5.2 billion people worldwide own a smartphone (4). When the COVID-19 situation rapidly worsened, downloads of mental health apps accelerated (2, 5). For example, the apps Calm and Headspace ranked two and three for worldwide revenue achieved in March 2020 for health and fitness apps in the Google Play store, achieving sales worth over US$1,149,000 and US$838,000, respectively (6). Around the world, there is other evidence that both authorities and people are turning to apps and other digital options in large numbers to cope with the trauma of COVID-19: in Australia (7), China (8), India (9), New Zealand (10), U.K. (11), U.S. (5), and others. However, we do not yet have accurate data on how many people are experiencing symptoms of PTSD as a result of COVID-19, nor how many are relying on smartphone apps to cope with these symptoms.
The Evidence for Treating Symptoms of Trauma With an APP
Best practice involves initially treating symptoms of trauma with specially administered psychological therapy, such as trauma-focused cognitive-behavioral therapy (CBT), eye movement desensitization and reprocessing (EMDR), cognitive processing therapy, narrative exposure therapy, or prolonged exposure therapy (12). If there is no or little improvement in symptoms as a result of these treatments, clinicians may explore pharmacological options, either as an adjunct to therapy or as a front line treatment if psychotherapy has been ineffective (13). If psychotropic medication is prescribed for PTSD, it will usually initially be an antidepressant, and mostly it will be a selective serotonin reuptake inhibitor (SSRI) or serotonin-norepinephrine reuptake inhibitor (SNRI) (12). However, the evidence for efficacy of pharmacological treatments of PTSD is less than that for psychological treatments (13), so further treatment options would be welcomed, especially with the anticipated worldwide surge in trauma-related presentations that may arise during and after the COVID-19 situation with both health workers and the general public (14–17).
The description of “antidepressant” for a class of drug is confusing because many antidepressants not only treat depression, but also anxiety (18). When pharmacological treatment is prescribed for anxiety or depression in the form of an antidepressant, it is has been done so for a medication that has been approved by government regulators in that country that have identified the medication as safe and efficacious. A digital antidepressant, therefore, can be thought of as any app, website or other digital tool that is specifically designed to treat symptoms of anxiety or depression. If this digital tool is a form of non-pharmaceutical medication, there is a need for these digital tools to have research behind them. Government regulators would not allow a pharmaceutical antidepressant to become available without research of efficacy, and using the term “digital antidepressant” is a reminder of how important it is to consider apps that claim to treat anxiety and depression symptoms as things that need to have research for their efficacy as well. The idea that a health professional could “prescribe” a mental health app (19) is attractive at this time because of the difficulties accessing face-to-face treatment, whether by telehealth or in-person. Medical practitioners are concerned about the welfare of their patients, and if their patients cannot access “human” help, they may seek out other options in the form of digital technology. However, clinicians should be aware of the evidence for mental health apps, and understand that a digital antidepressant may not produce the desired clinical outcomes.
Similarly, the above mentioned evidence-based psychotherapies for treating symptoms of trauma require the specialized skills of highly trained practitioners. To be effective, such practitioners have to be experts in recognizing the signs and symptoms of trauma, adapting their psychotherapy in response to changes in client presentation, and acting appropriately if their client's condition deteriorates, especially in response to a risk of self-harm or suicide. If a general practitioner or other health professional does not have such specialized training in the area of psychologically treating symptoms of trauma, they may have the mistaken belief that a mechanized version of psychotherapy is possible in an app without being aware that evidence may not exist for the app's effectiveness in treating trauma presentations.
Evidence for the efficacy and effectiveness of mental health apps is limited (20, 21). The research suffers from methodological deterrents (e.g., quality randomized controlled trials [RCTs] can be expensive and take years to run which is an impediment for the profit-driven app sector), heterogeneity across studies, no published replication studies to speak of, and a lack of independence (i.e., studies completed by researchers who have not had any association with the app) (22, 23). This last point is important and is illustrated through a comparison with chemical antidepressants.
The early evidence base for chemical antidepressants, which was largely established by pharmaceutical companies who developed these medications, showed far higher effect sizes and greater levels of statistical significance than more recent studies (24). The later studies have included a much greater proportion of independent trials by researchers who have no association with the medications being tested. Their results have demonstrated significantly less efficacious and effective outcomes (24). Using the Cochrane Bias Tool, it has been estimated that 82% of all previous published studies on antidepressant medications are at moderate or high risk of bias due to the involvement of pharmaceutical companies (24).
If the efficacy of mental health apps is to be free of the limitations affecting many drug trials, unbiased research is required while their development is still relatively young. In a recent review of the two major app stores, only 1% of apps that claimed to offer a therapeutic treatment for anxiety and depression had independent research to back-up claims of efficacy (25). That is, research that was conducted by individuals, institutions or organizations who were not involved in the development of the app, and who would not stand to gain financially or otherwise from it. This is not to discourage research by app developers—quite the contrary. More app developers also need to conduct research on their product because a huge proportion of publicly available apps have no research support whatsoever (22, 23). While much of the research conducted by those who have an association with the app may be of acceptable quality, it is important that independent research in this area is increased to further legitimize the evidence base and minimize concerns regarding bias.
There is less evidence for apps specifically treating symptoms of trauma. The principal research on this front has come from the U.S. Department of Veterans' Affairs (VA), developers of PTSD Coach (26) and a suite of other apps, most of which are specifically aimed at veterans or their families. At time of writing, no published evidence could be found for the efficacy or effectiveness of any individual app specifically designed to treat symptoms of trauma, other than those produced by VA (27, 28). This is despite hundreds of publicly available apps purporting to do this (28, 29), and the availability of a standardized framework for developing PTSD-focused apps that stipulates the importance of demonstrated efficacy (30). Without a more diverse evidence base, it is unknown to what extent people benefit when they attempt to manage trauma by using apps. Worse still, we do not know how much damage is being caused by misinformed and poorly developed apps.
Government Regulation
Examples of potential harm from an app include breaches of privacy, misuse of personal data, providing inappropriate advice (31), and poor app functionality leading to possible app failure at a critical emotional point for the user. It has also been found that for over 20% of publicly available apps claiming to treat symptoms of PTSD, their app store descriptions did not contain any specific PTSD evidence-based content (28). This is where government intervention is urgently required, but many governments are struggling to develop suitable regulations around mental health apps (32). Authorities such as the U.S. Food and Drug Administration are focused on removing apps that may cause harm (33). A recent report by the Australian Commission on Safety and Quality in Health Care (34) attempts to encompass a wider regulatory view of digital mental health resources founded on a “model of care” with “best available evidence and best practice” (p. 20).
However, these new standards in digital mental health care, which include mental health apps, are yet to be implemented. In the meantime, medical practitioners who are expecting an influx of trauma-related presentations in the wake of COVID-19, must use caution in directing patients toward apps to assist in managing symptoms of trauma.
Discussion
There is uncertainty about the effectiveness of many mental health apps (i.e., their ability to deliver beneficial treatments in a real world setting) and the most appropriate methods of examining this (35). The COVID-19 crisis brings to the fore the need for a centralized database of information for use by medical professionals, governments, therapists, researchers, and consumers (36). Clearly, there is a need to move beyond reliance on app store ratings and reviews, which may be inaccurate, ill-informed, or fake (37), to the requirement for app researchers to provide accessible and timely research evidence. While the time demands of the gold standard RCT can be an impediment to research, other methodologies that do not sacrifice scientific rigor and integrity can potentially be conducted on apps in a more timely manner (38). These include scalable single-case designs involving practicing clinicians working with researchers (36). In such a model, clinicians could contribute their findings to a centralized database that may continually be updated with results that occur from individuals using their app in real-world settings. The single-case methodology has the added advantage of being able to provide potentially more information on the characteristics of the individual than might otherwise be identified in larger RCT designs. This may in-turn lead to more informed hypotheses about how individual characteristics may impact on the effectiveness of a mental health app.
Other than the need for further research on efficacy and effectiveness, future development of apps for treating symptoms of trauma (and indeed for all apps treating mental illness generally) needs to take into account a number of factors, and there are many existing development blueprints that app developers can refer to (39–41). Building a mental health app on the foundations of an evidence-based framework is vital (42). There are several evidence-based frameworks that inform PTSD psychological treatments (as mentioned above), and it would seem plausible that such treatment interventions could be incorporated into an app. There needs to be expert input from qualified clinicians and/or researchers into the development of a mental health app—many apps claiming to treat symptoms of mental illness do not have such input (25, 43, 44). Given that the development of mobile mental health apps is still in its infancy, we are still not certain about the mechanisms of action of such apps, and therefore the level of importance of characteristics such as app design and usability is still being investigated. However, it would seem plausible to assume that a mental health app has to be easy to use, engaging, and aesthetically pleasing to be efficacious and effective (41), and therefore having the input from experienced app designers would seem to be a necessity. This is only a brief summary of necessary aspects of a successful mental health app, but even here it can be seen that many different aspects of development need to be considered before an app is able to make claims that it can successfully treat symptoms of trauma, or of any other mental illness.
Another concerning feature of around 40% of mental health apps is that they lack a publicly accessible privacy policy (45). Given the sensitive nature of people's mental health information, app developers need to pay more attention to this. One reason why app developers have been able to get away with this for so long is that there is no government regulation about the need for privacy policies for digital mental health resources. If government authorities can broaden and strengthen their oversight of this sector, protecting people's privacy will be as necessary a factor as ensuring that mental health apps do no harm to their users.
There are websites that clinicians (and consumers) can access for reviews and further information about choosing mental health apps, listed in Table 1. The rationale for providing the information in Table 1 is so that clinicians can become more informed about recommending appropriate apps for their patients and clients. We did not recommend specific apps, as that is not the purpose of this paper. Although lacking information on how to measure effectiveness, these websites are nevertheless useful resources for clinicians who need assistance identifying potentially suitable apps. While the current evidence base is lacking, it is hoped the COVID-19 crisis is a potential catalyst for ensuring that mental health apps have demonstrated effectiveness for treating specified mental health disorders, including PTSD-related trauma, into the future.
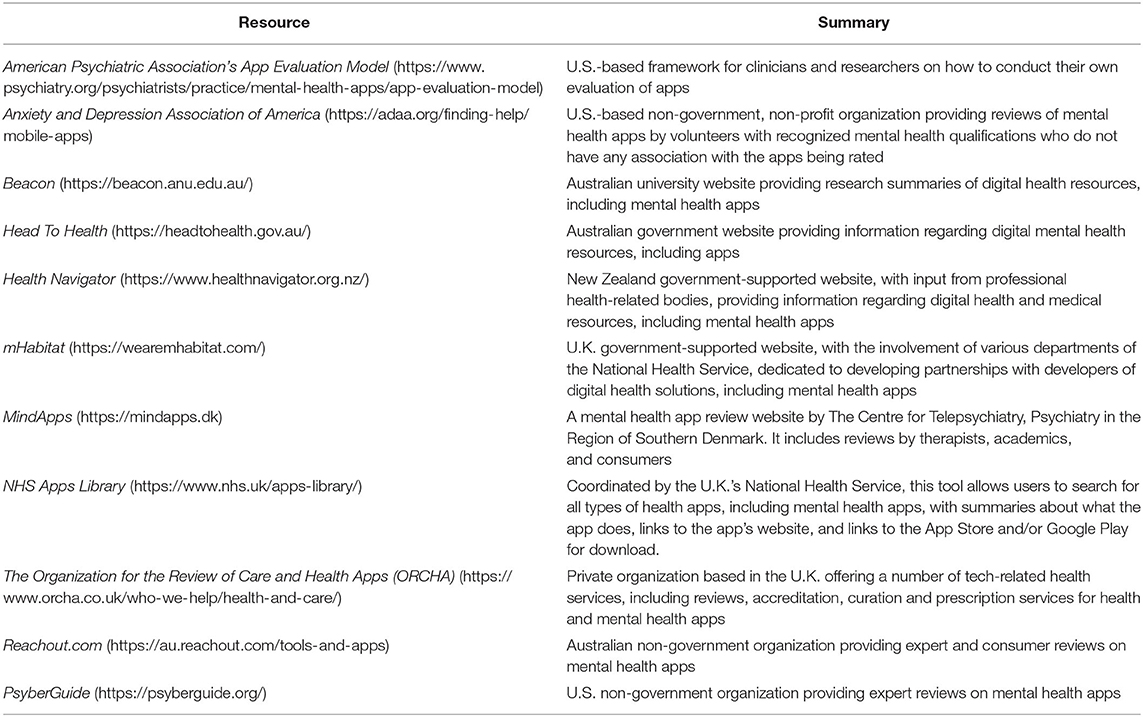
Table 1. Website resources for clinicians that provide reviews and further information on mental health apps for symptoms of trauma.
Data Availability Statement
All datasets analyzed in this study are included in the article/supplementary material.
Author Contributions
JM wrote the manuscript drafts. DD and WB provided proofreading and editing. All authors read and approved the final submitted version.
Funding
JM is in receipt of an Australian Government Research Training Program Stipend Scholarship. The provider of this funding has had no role in any proposed study design, collection or interpretation of data, writing manuscripts, or the decision to submit manuscripts for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Liu S, Yang L, Zhang C, Xiang Y-T, Liu Z, Hu S, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:e17–e8. doi: 10.1016/S2215-0366(20)30077-8
2. Basu T. The Coronavirus Pandemic is a Game Changer for Mental Health Care (2020). Available online at: https://www.technologyreview.com/2020/03/20/905184/coronavirus-online-therapy-mental-health-app-teletherapy/ (accessed April 11, 2020).
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders.- Fifth Edition (DSM-5). Arlington, VA: American Psychiatric Association (2013). p. 271–86. doi: 10.1176/appi.books.9780890425596
5. Heilweil R. Feeling Anxious About Coronavirus? There's an App for That. Niklas Heuveldop (2020). Available online at: https://www.vox.com/recode/2020/3/20/21185351/mental-health-apps-coronavirus-pandemic-anxiety (accessed August 5, 2020).
6. Statista. Leading Health and Fitness Apps in the Google Play Store Worldwide in March (2020). By revenue: Statista (2020). Available online at: https://www.statista.com/statistics/695697/top-android-health-apps-in-google-play-by-revenue/ (accessed April 11, 2020).
7. Koh D. New mental health program announced to support Australian healthcare workers during COVID-19. Healthcare IT News. (2020). Available online at: https://www.healthcareit.com.au/article/new-mental-health-program-announced-support-australian-healthcare-workers-during-covid-19 (accessed June 13, 2020).
8. Feng C. China's mental health counsellors reach out online to help those affected by coronavirus pandemic. South China Morning Post. (2020). Available online at: https://www.scmp.com/tech/apps-social/article/3077260/chinas-mental-health-counsellors-reach-out-online-help-those (accessed June 15, 2020).
9. Mukherjee J. We tried these 4 mental health apps to help us cope with stress during Covid-19 lockdown. News 18. (2020). Available online at: https://www.news18.com/news/buzz/we-tried-these-4-mental-health-apps-to-help-us-cope-with-stress-during-covid-19-lockdown-2553235.html (accessed June 13, 2020).
10. Mindfood. NZ Government releases apps to help with mental health during COVID-19 crisis. Mindfood. (2020). Available online at: https://www.mindfood.com/article/nz-government-releases-apps-to-help-with-mental-health-during-covid-19-crisis/ (accessed June 15, 2020).
11. Chowdhury H. Mental health apps downloaded more than 1m times since start of virus outbreak. The Telegraph. (2020). Available online from: https://www.telegraph.co.uk/technology/2020/05/16/mental-health-apps-downloaded-1m-times-since-start-virus-outbreak/ (accessed June 15, 2020).
12. Charney ME, Hellberg SN, Bui E, Simon N. Evidence-based treatment of posttraumatic stress disorder: an updated review of validated psychotherapeutic and pharmacological approaches. Harv Rev Psychiatry. (2018) 26:99–115. doi: 10.1097/HRP.0000000000000186
13. Psychotropic Expert Groups. Therapeutic Guidelines: Psychotropic. Melbourne: Therapeutic Guidelines Limited (2013).
14. Australian Government Department of Health. COVID-19:$48.1 Million for National Mental Health and Wellbeing Pandemic Response Plan (2020). Available online at: https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/covid-19-481-million-for-national-mental-health-and-wellbeing-pandemic-response-plan (accessed August 5, 2020).
15. Mougin S. Covid-19 debrief: Paris nurses, doctors reveal heavy toll on mental health. France 24. (2020). Available online at: https://www.france24.com/en/20200521-covid-19-debrief-nurses-and-doctors-share-feelings-and-feedback (accessed June 16, 2020).
16. Carthaus A. Coronavirus and mental health: “We are not made for social isolation”. DW News. (2020). Available online at: https://www.dw.com/en/coronavirus-and-mental-health-we-are-not-made-for-social-isolation/a-52971173 (accessed June 16, 2020).
17. Kallivayalil RA. COVID-19 and Mental Health: Working together in India. World Psychiatric Association. (2020). Available online at: https://www.wpanet.org/post/covid-19-and-mental-health-working-together-in-india (accessed June 16, 2020).
18. Jennings L. Antidepressants. In: Grossberg GT, Kinsella LJ, editors. Clinical Psychopharmacology for Neurologists - A Practical Guide. Cham: Springer (2018). p. 45–71. doi: 10.1007/978-3-319-74604-3_4
19. Byambasuren O, Sanders S, Beller E, Glasziou P. Prescribable mHealth apps identified from an overview of systematic reviews. NPJ Digit Med. (2018) 1:12. doi: 10.1038/s41746-018-0021-9
20. Orman J, O'Dea B. e-Therapy in primary care mental health. Aust J Gen Pract. (2018) 47:168–72. doi: 10.31128/AJGP-11-17-4410
21. Marshall JM, Dunstan DA, Bartik W. Clinical or gimmickal: the use and effectiveness of mobile mental health apps for treating anxiety and depression. Aust N Z J Psychiatry. (2020) 54:20–8. doi: 10.1177/0004867419876700
22. Firth J, Torous J, Nicholas J, Carney R, Rosenbaum S, Sarris J. Can smartphone mental health interventions reduce symptoms of anxiety? A meta-analysis of randomized controlled trials. J Affect Disord. (2017) 218:15–22. doi: 10.1016/j.jad.2017.04.046
23. Firth J, Torous J, Nicholas J, Carney R, Pratap A, Rosenbaum S, et al. The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials. World Psychiatry. (2017) 16:287–98. doi: 10.1002/wps.20472
24. Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. (2018) 391:1357–66. doi: 10.1016/S0140-6736(17)32802-7
25. Marshall JM, Dunstan DA, Bartik W. The digital psychiatrist: in search of evidence-based apps for anxiety and depression. Front Psychiatry. (2019) 10:831. doi: 10.3389/fpsyt.2019.00831
26. Kuhn E, Kanuri N, Hoffman JE, Garvert DW, Ruzek JI, Taylor CB. A randomized controlled trial of a smartphone app for posttraumatic stress disorder symptoms. J Consult Clin Psychol. (2017) 85:267–73. doi: 10.1037/ccp0000163
27. Owen JE, Kuhn E, Jaworski BK, McGee-Vincent P, Juhasz K, Hoffman JE, et al. VA mobile apps for PTSD and related problems: public health resources for veterans and those who care for them. Mhealth. (2018) 4:28. doi: 10.21037/mhealth.2018.05.07
28. Sander LB, Schorndanner J, Terhorst Y, Spanhel K, Pryss R, Baumeister H, et al. ‘Help for trauma from the app stores?’ A systematic review and standardised rating of apps for post-traumatic stress disorder (PTSD). Eur J Psychotraumatol. (2020) 11:1701788. doi: 10.1080/20008198.2019.1701788
29. Rodriguez-Paras C, Tippey K, Brown E, Sasangohar F, Creech S, Kum H-C, et al. Posttraumatic stress disorder and mobile health: app investigation and scoping literature review. JMIR Mhealth Uhealth. (2017) 5:e156. doi: 10.2196/mhealth.7318
30. Schellong J, Lorenz P, Weidner K. Proposing a standardized, step-by-step model for creating post-traumatic stress disorder (PTSD) related mobile mental health apps in a framework based on technical and medical norms. Eur J Psychotraumatol. (2019) 10:1611090. doi: 10.1080/20008198.2019.1611090
31. Hussain M, Al-Haiqi A, Zaidan AA, Zaidan BB, Kiah MLM, Anuar NB, et al. The landscape of research on smartphone medical apps: coherent taxonomy, motivations, open challenges and recommednations. Comput Methods Programs Biomed. (2015) 122:393–408. doi: 10.1016/j.cmpb.2015.08.015
32. Armontrout JA, Torous J, Cohen M, McNeil DE, Binder R. Current regulation of mobile mental health applications. J Am Acad Psychiatry Law. (2018) 46:204–11. doi: 10.29158/JAAPL.003748-18
33. US Food Drug Administration. Device Software Functions Including Mobile Medical Applications: U.S. Food and Drug Administration (2019). Available online from: https://www.fda.gov/medical-devices/digital-health/device-software-functions-including-mobile-medical-applications (accessed August 5, 2020).
34. Australian Commission on Safety and Quality in Health Care. National Safety and Quality Digital Mental Health Standards. Sydney, NSW (2020).
35. Lui JHL, Marcus DK, Barry CT. Evidence-based apps? A review of mental health mobile applications in a psychotherapy context. Prof Psychol Res Pract. (2017) 48:199–210. doi: 10.1037/pro0000122
36. Marshall JM, Dunstan DA, Bartik W. Smartphone psychology: new approaches toward safe and efficacious mobile mental health apps. Prof Psychol Res Pract. (2020) 51:214–22. doi: 10.1037/pro0000278
37. Xie Z, Zhu S. Appwatcher: unveiling the underground market of trading mobile app reviews. In: 8th ACM Conference on Security and Privacy in Wireless and Mobile Networks. New York. NY, New York: Association of Computing Machinery (2015). doi: 10.1145/2766498.2766510
38. Clough BA, Casey LM. Smart designs for smart technologies: research challenges and emerging solutions for scientist-practitioners within e-mental health. Prof Psychol Res Pract. (2015) 46:429–36. doi: 10.1037/pro0000053
39. Moshi MR, Tooher R, Merlin T. Suitability of current evaluation frameworks for use in the health technology assessment of mobile medical applications: a systematic review. Int J Technol Assess Health Care. (2018) 34:464–75. doi: 10.1017/S026646231800051X
40. Zelmer J, van Hoof K, Notarianni MA, van Mierlo T, Schellenberg M, Tannenbaum C. An assessment framework for e-mental health apps in Canada: results of a modified Delphi process. JMIR MHealth UHealth. (2018) 6:e10016. doi: 10.2196/10016
41. Bakker D, Kazantzis N, Rickwood D, Rickard N. Mental health smartphone apps: review and evidence-based recommendations for future developments. JMIR Mental Health. (2016) 3:e7. doi: 10.2196/mental.4984
42. Marshall JM, Dunstan DA, Bartik W. Apps with maps: a systematic review of the major app stores for anxiety and depression mobile apps with evidence-based frameworks. JMIR Mental Health. (2020) 7:e16525. doi: 10.2196/16525
43. Alyami M, Giri B, Alyami H, Sundrum F. Social anxiety apps: a systematic review and assessment of app descriptors across mobile store platforms. Evid Based Mental Health. (2017) 20:65–70. doi: 10.1136/eb-2017-102664
44. Shen N, Levitan M-J, Johnson A, Bender JL, Hamilton-Page M, Jadad AR, et al. Finding a depression app: a review and content analysis of the depression app marketplace. JMIR MHealth UHealth. (2015) 3:e16. doi: 10.2196/mhealth.3713
Keywords: smartphone apps, COVID-19, trauma, PTSD, mHealth, anxiety, Internet, mental health
Citation: Marshall JM, Dunstan DA and Bartik W (2020) Treating Psychological Trauma in the Midst of COVID-19: The Role of Smartphone Apps. Front. Public Health 8:402. doi: 10.3389/fpubh.2020.00402
Received: 06 May 2020; Accepted: 08 July 2020;
Published: 18 August 2020.
Edited by:
Gian Mauro Manzoni, University of eCampus, ItalyReviewed by:
Iva Georgieva, Institute for Advanced Study Varna, BulgariaYuen Yu Chong, The Chinese University of Hong Kong, China
Copyright © 2020 Marshall, Dunstan and Bartik. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jamie M. Marshall, am1hcnNoMjEmI3gwMDA0MDtteXVuZS5lZHUuYXU=
 Jamie M. Marshall
Jamie M. Marshall Debra A. Dunstan
Debra A. Dunstan Warren Bartik
Warren Bartik