
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 24 July 2019
Sec. Public Health Education and Promotion
Volume 7 - 2019 | https://doi.org/10.3389/fpubh.2019.00205
 Begashaw Melaku Gebresillassie1†
Begashaw Melaku Gebresillassie1† Yohannes Kelifa Emiru1*†
Yohannes Kelifa Emiru1*† Daniel Asfaw Erku1†
Daniel Asfaw Erku1† Amanual Getnet Mersha2†
Amanual Getnet Mersha2† Abebe Basazn Mekuria1†
Abebe Basazn Mekuria1† Asnakew Achaw Ayele1†
Asnakew Achaw Ayele1† Henok Getachew Tegegn1†
Henok Getachew Tegegn1†Purpose: Little is known about acceptance of provider-initiated HIV testing and counseling (PICT) as an intervention for prevention of mother to child transmission of HIV (PMTCT) in many parts of sub-Saharan Africa including Ethiopia. This study aimed at assessing the utilization and acceptance rate of PICT as an intervention for PMTCT among pregnant women attending University of Gondar referral and teaching hospital (UoGRTH), Ethiopia.
Methods: A hospital-based cross-sectional study was conducted on 364 pregnant women attending antenatal care clinic at UoGRTH through an interviewer-administered questionnaire. Frequencies, means, and percentages were used to report different variables. Univariate analysis and multivariate logistic regression analysis were used to come up with factors associated with acceptance of PICT services.
Results: Out of 364 respondents, 298 330 (81.7%) of them accepted provider-initiated HIV testing and counseling. Rural residency (AOR: 364, 95% CI: 2.17–6.34), higher educational status (AOR: 3.15, 95% CI: 1.86–6.82), planning of HIV test disclosure to male partners (AOR: 7.81, 95% CI: 3.17–13.14), and a higher average monthly income (AOR: 4.01, 95% CI: 2.32–7.61) were found to be strong predictors of acceptance of provider-initiated HIV testing and counseling.
Conclusions: The present study revealed a higher rate of acceptance of PICT among pregnant women. Enhancing access to and consistent use of antenatal care service among pregnant women and encouraging the active involvement of male partners are recommended to further increase the uptake of provider-initiated HIV testing and counseling.
Recently, children and adolescents have been given a higher priority for HIV preventive and treatment services owing to a higher prevalence of undiagnosed HIV infection in these population compared to adults (1). Mother-to-child transmission of HIV (MTCT) represents one of the biggest public health problem and continues to account for a considerable percentage of new cases of HIV infections among Ethiopian children (2). Only in 2012, more than 750,000 people were living with HIV with an estimated 37,600 were children, around 20,000 were newly infected and more than 22,000 were pregnant women (3). Without any interventions, the risk of HIV transmission from mother to child ranges from 5 to 10% during gestation, 10 to 20% during delivery, and 10 to 20% through infant feeding (4, 5). MTCT of HIV can be prevented through early detection of maternal HIV and administration of antiretroviral prophylaxis infection during pregnancy (6).
The national prevention of mother-to-child transmission of HIV (PMTCT) guideline of Ethiopia is based on the four-pronged approaches and promotes the integration of PMTCT and HIV counseling and testing services within the family planning and reproductive health services (7). Provider-initiated HIV counseling and testing (PICT) services are routinely provided freely to all pregnant women attending antenatal and post-natal services. In 2011, the proportion of pregnant women counseled and tested for MTCT in Ethiopia was 33.4%, and only 9.3% of infants born to HIV positive mothers received ARV prophylaxis for PMTCT (8). A number of factors have been identified which contribute to the low level of utilization of PICT services. Less frequent ANC attendance and follow up, a higher rate of home delivery and lost from follow up are some of the major reasons (9–13).
In order to reduce the number of infants with HIV infection, there has been a rapid and intensive scale-up of ARV prophylaxis and provider-initiated HIV counseling and testing (PICT) services in the country since 2005 (14). Yet, regardless of intensive interventions to scale-up, the coverage and utilization of PMTCT services in Ethiopia remains low. The aim of this study was to assess the utilization and acceptance rate of provider-initiated HIV testing and counseling (PICT) as an intervention for PMTCT of HIV among pregnant women attending antenatal clinic of University of Gondar teaching and referral hospital, northwest Ethiopia.
This was a hospital-based quantitative cross-sectional study conducted on 364 pregnant women attending antenatal care (ANC) clinic at University of Gondar Referral and Teaching Hospital (UoGRTH), Ethiopia. UoGRTH, the only referral center in the area with multiple specialized clinics including ANC follow up clinic, is located in Gondar town, northwest Ethiopia. The hospital provides ANC service for more than 15,000 pregnant women annually. The study was conducted from January 1 to March 30, 2018. This study was approved by the ethical review committee of School of Pharmacy, University of Gondar. Written informed consent was also secured from all the respondents before commencing this study.
All pregnant women attending ANC clinic of UoGRTH were taken as a source population and those pregnant mothers who visit the ANC clinic during the study period were our study population. We used a single population proportion formula taking into account a 95% confidence interval, 5% margin of error and 80% rate of acceptance and utilization of PICT (15) and 5% was considered for possible non-response rate to come up with a final sample size of 423. As per the information we got from Gondar university referral hospital Statistics and Information Office, an estimated number of 25 pregnant women visit the ANC clinic of UoGRTH on a daily basis. Hence, the proportion of pregnant women who will visit the ANC clinic during the data collection period was estimated to be 7. Accordingly, a systematic random sampling technique was utilized and every fourth pregnant woman available at the ANC clinic and who met the inclusion criteria during the 2-month data collection period were included. All pregnant women were interviewed in the waiting room before meeting with the doctor.
The data were collected performed five well-trained nurses working at ANC clinic via interviewer-administered questionnaire. Data collectors were trained intensively on contents of the questionnaire, data collection methods and ethical concerns by the principal investigator. The overall data completeness and consistency was checked by the principal investigator on a daily basis. The questionnaire was created by modifying items in three previously used instruments regarding the acceptance and utilization of PICT services (12, 15, 16) and items were thoroughly reviewed for relevance by a team of experts including obstetrics and gynecology specialists along with a reproductive health expert. The survey instrument was further validated by pre-testing on 25 pregnant women who were not included in the final analysis and relevant modifications were done before the start of final data collection. The final data collection tool included questions assessing demographic and pregnancy-related information including age, highest level of education, history and number of ANC visits, knowledge of PMTCT, and acceptability of PITC services, knowledge, and risk perception on HIV/AIDS, attitude toward PITC and perceived benefit of HIV test, and partner's feedback for HIV positive test result.
The final data collected were analyzed using Statistical Package for the Social Sciences (SPSS) software version 21.0 for Windows (SPSS Inc., Chicago, IL). Frequencies, means, and percentages were used to report different variables. Univariate analysis and multivariate logistic regression analysis were used to come up with factors associated with acceptance and utilization of PICT services. The results were adjusted for patients' demographic and pregnancy-related characteristics and OR with 95% CI were computed along with corresponding p-value (p < 0.05) as cut off points for determining statistical significance among different variables.
From a total of 423 pregnant women invited to participate, 364 of them completed the survey giving a response rate of 89.8%. The mean age of respondents was 26 years with a standard deviation of ± 5.0. Majority of the respondents were Orthodox Christians (87.6%) and urban residents (79.7%). About two-thirds (66.2%) of the subjects drawn in this study were in their third trimester of pregnancy. The socio-demographic and pregnancy-related characteristics of respondents are summarized in Table 1.
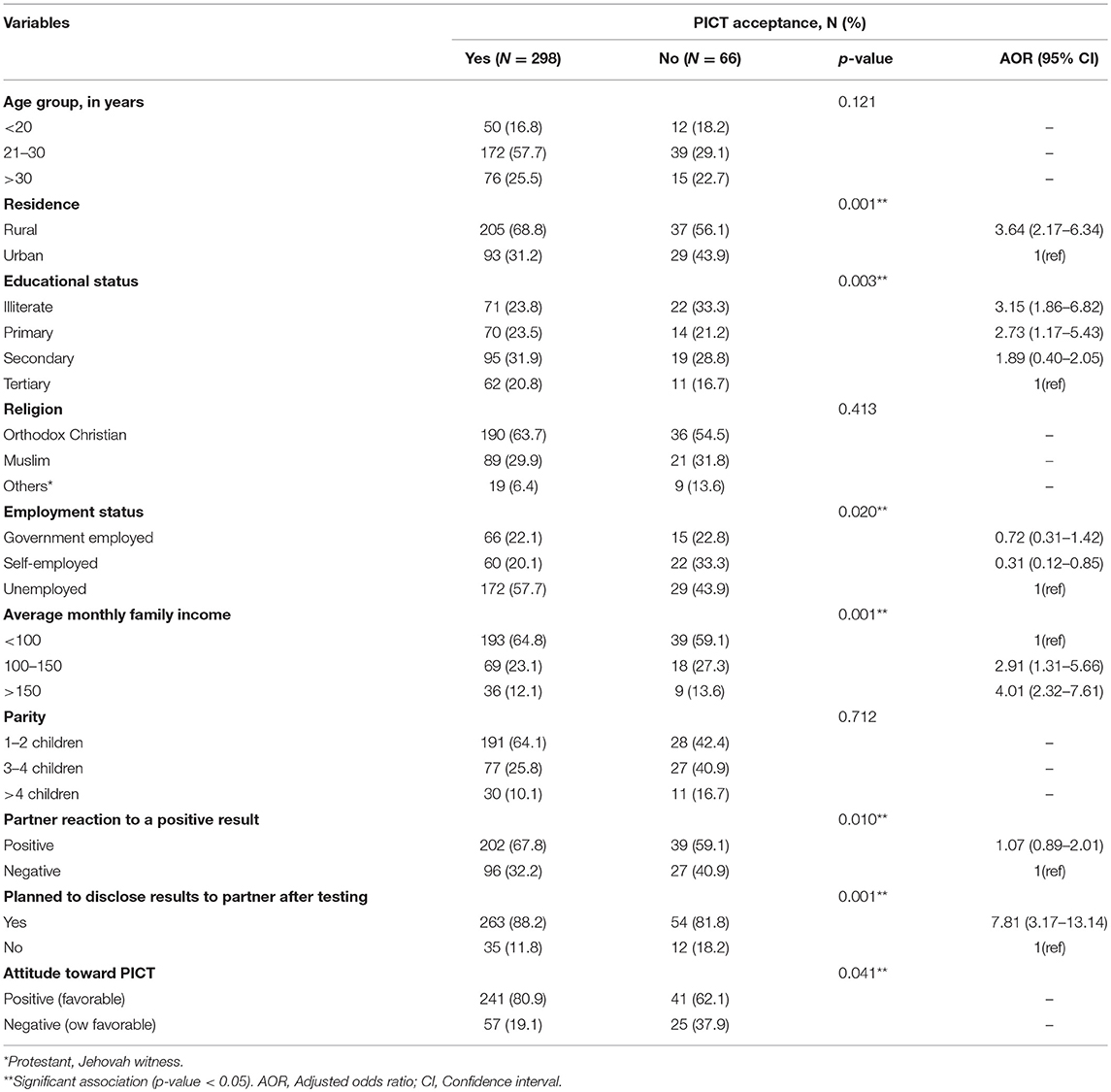
Table 1. Socio-demographic characteristics and factors associated with acceptance of PICT among respondents, 2018 (N = 364).
Protecting their children from getting the infection (64.4%) and concern for their own health (44.3%) were most frequent reasons given for accepting PICT, while anticipating the negative reaction from their partners for HIV test result (43.9%) and not being ready for conducting HIV test (33.3%) as the common reasons for not accepting PICT (Table 2).
Out of 364 respondents, 298 330 (81.7%) of them accepted provider-initiated HIV testing and counseling. Those variables that were significantly associated with acceptance of PICT in the bivariate analysis were further examined in multivariate logistic regression. Accordingly, residency, educational status, planning of HIV test disclosure to male partners, and average monthly income found to have a significant association in multivariate logistic regression analysis. Accordingly, the odds of acceptance of PICT was 3.64 times higher among rural residents as compared to urban residents (AOR: 364, 95% CI: 2.17–6.34). Pregnant women who had no formal education were 3.15 times more likely to accept PICT than those who attended tertiary education (AOR: 3.15, 95% CI: 1.86–6.82). Similarly, pregnant women who had average monthly income higher than 150 USD were 4.01 times more likely to accept PICT than those who had average monthly income of <100 USD (AOR: 4.01, 95% CI: 2.32–7.61). Respondents who planned to disclose their HIV status to their partners were 7.81 times (AOR: 7.81, 95% CI: 3.17–13.14) more likely to accept PICT than those who did not plan to disclose their results. No significant associations were found between PICT acceptance with age group, religion, marital status, and parity both in the bi-variant and multivariate logistic regression analysis.
In our study, the acceptance of PICT was 81.9%, which is comparable with the studies done in different regions of Ethiopia including Assossa (80.8%) (15), and Arba-Minch (74.4%) (17). However, a much lower acceptance rate of PICT was reported in Illubabor (27.0%) (18). The variation in acceptability of PICT is also pronounced in different parts of African countries with acceptability ranging from 79% in Zimbabwe, 88.3% in Cameroon, 95% in Botswana, 97% in Uganda and 99.9% in Zimbabwe (16, 19–22). The relatively higher acceptance rate in our study could be partially explained by the fact that most pregnant women consider that PICT as a standard care for PMTCT and due to the high availability and affordability of comprehensive HIV/AIDS care in the past couple of years through community sensitization and enhancing the accessibility of on-site rapid HIV testing.
Both bi-variant and multivariate regression analysis were done to identify factors associated with acceptance of PICT among women attending ANC follow up. Accordingly, Women who had no formal education were more likely to accept PICT than those who attended tertiary education. Similarly, the odds of acceptance of PICT was 3.64 times higher among rural residents as compared to urban residents. This could be partially explained by the fact that women who are illiterates or unschooled might accept PICT due to fear of the negative response from their physicians or health care providers and their relatively low possibility of asking their physicians regarding medical advice (23, 24). Furthermore, enhancing PICT acceptance may be achieved at the cost of pregnant women not knowing that PICT is optional, which might be also the case in our study (25). A similar study conducted in Botswana reported that about 68% of women felt that they could not refuse PICT (26).
Pregnant women who had a higher average monthly income were also more likely to accept PICT than those who had low average monthly income, which might be attributed to the fact that women with lower average monthly income are less able to make autonomous decisions as they are financially dependent and are not empowered economically. Furthermore, acceptance of PITC is increased as the number of ANC visits increases in our study, which corroborates with the finding of the study done in Zimbabwe (16). One possible explanation for this is the fact that frequent visit of health centers and close contact with health care providers increase the possibility of acquiring knowledge about PICT, PMTCT, and other preventive strategies. Moreover, women who did not plan to disclose their test results to their partner refused to test. This could be due to a number of reasons including fear of separation, cultural influence and anticipated lack of acceptance as reported in other similar studies (15).
The study has some limitations that should be taken into account while interpreting the results. As the study is cross-sectional and depends on self-reported assessment, underreporting is very likely. A larger-scale and multi-centered survey that includes more diverse participants is needed to provide more accurate findings. Regardless of the above limitations, the study provides useful information that will inform the implementation and consolidation of PICT to PMTCT Amhara and other regions of Ethiopia.
The present study revealed a higher level of utilization of PICT among pregnant women attending antenatal care clinic at University of Gondar referral and teaching hospital, Ethiopia. A higher number of antenatal care visits, urban residency, and a higher level of knowledge on prevention of mother to child transmission of HIV are associated with a higher acceptance rate of provider-initiated HIV testing and counseling. Enhancing access to and consistent use of antenatal care service among pregnant women is recommended to further increase the uptake of provider-initiated HIV testing and counseling. Physicians working in ANC clinics should promote and encourage the active involvement of partners during ANC services to reduce the trouble that pregnant women face to disclose their HIV test result. Further studies using mixed methods (both qualitative and quantitative approach) is recommended at a national level to come up with other factors associated with the acceptance and utilization of PICT.
This study was approved by the ethical review committee of School of pharmacy, University of Gondar with a reference number of SoP-UoG-134/2018. Written informed consent was also secured from all the respondents before commencing this study.
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
This research received no support from any funding agency in the public, commercial, or not-for-profit sectors.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors acknowledge the support of the School of Pharmacy and UoGRTH ANC clinic in facilitating the data collection process.
1. Global Update on HIV Treatment 2013. Results, Impact and Opportunities. Geneva: World Health Organization (2013).
2. World Health Organization. PMTCT Strategic Vision 2010–2015: Preventing Mother-to-Child Transmission of HIV to Reach the UNGASS and Millennium Development Goals. Geneva: World Health Organization (2010).
3. Doyle AM, Mavedzenge SN, Plummer ML, Ross DA. The sexual behaviour of adolescents in sub-Saharan Africa: patterns and trends from national surveys. Trop Med Int Health. (2012) 17:796–807. doi: 10.1111/j.1365-3156.2012.03005.x
4. Sabapathy K, Van den Bergh R, Fidler S, Hayes R, Ford N. Uptake of homebased voluntary HIV testing in sub-Saharan Africa: a systematic review and meta-analysis. PLoS Med. (2012) 9:e1001351. doi: 10.1371/journal.pmed.1001351
5. Suthar AB, Ford N, Bachanas PJ, Wong VJ, Rajan JS, Saltzman AK, et al. Towards universal voluntary HIV testing and counselling: a systematic review and meta-analysis of community-based approaches. PLoS Med. (2013) 10:e1001496. doi: 10.1371/journal.pmed.1001496
6. World Health Organization. Antiretroviral Drugs for Treating Pregnant Women and Preventing HIV Infection in Infants: Towards Universal Access. Geneva: World Health Organization (2006).
7. Ministry of Health of Federal Democratic Republic of Ethiopia, HIV/AIDS Prevention and Control Office. Guidelines for Prevention of Mother-to-child transmission of HIV in Ethiopia. Addis Ababa: Federal Ministry of Health (2007).
8. Ministry of Health of Federal Democratic Republic of Ethiopia. Health and Health Related Indicators. Addis Ababa: Federal Ministry of Health (2010).
9. Bajunirwe F, Muzoora M. Barriers to the implementation of programmes for the prevention of mother-to-child transmission of HIV: a cross sectional survey in rural and urban Uganda. AIDS Res Ther. (2005) 2:10. doi: 10.1186/2F1742-6405-2-10T
10. Kasenga F, Hurtig A, Emmelin M. HIV-positive women's experiences of a PMTCT programmeme in rural Malawi. Midwifery. (2010) 26:27–37. doi: 10.1016/j.midwif.2008.04.007
11. Chinkonde JR, Sundby J, Martinson F. The prevention of mother-to-child HIV transmission pogramme in Lilongwe, Malawi: why do so many women drop out. Reproduct Health Matters. (2009) 17:143–51. doi: 10.1016/S0968-8080(09)33440-0
12. Lerebo W, Callens S, Jackson D, Zarowsky C, Tommerman M. Identifying factors associated with the uptake of prevention of mother to child HIV transmission programme in Tigray region. Ethiopia: a multilevel modelling approach. BMC Health Services Res. (2014) 14:181. doi: 10.1186/1472-6963-14-181
13. Derebe G, Biadgilign S, Trivelli M, Hundessa G, Robi ZD, Gebre-Mariam M, et al. Determinant and outcome of early diagnosis of HIV infection among HIV-exposed infants in southwest Ethiopia. BMC Res Notes. (2014) 7:309. doi: 10.1186/1756-0500-7-309
14. Assefa Y, Jerene D, Lulseged S, Ooms G, Damme WV. Rapid scale-up of antiretroviral treatment in Ethiopia: successes and system-wide effects. PLoS Med. (2009) 6:e1000056. doi: 10.1371/journal.pmed.1000056
15. Solomon A, Awoke W, Asrat A. Acceptability of provider-initiated HIV testing as an intervention for prevention of mother to child transmission of HIV and associated factors among pregnant women attending at Public Health Facilities in Assosa town, Northwest Ethiopia. BMC Res Notes. (2015) 8:661. doi: 10.1186/s13104-015-1652-4
16. Perez F, Zvandaziva C, Engelsmann B, Dabis F. Acceptability of routine HIV testing (opt-out) in antenatal services in two rural district of Zimbabwe. J Acquir Immune Defic Syndr. (2005) 41:514–20. doi: 10.1097/01.qai.0000191285.70331.a0
17. Haddis M, Jerene D. Awareness of antenatal care clients on mother-to child- transmission (MTCT) of HIV infection and its prevention in Arba Minch. Ethiopian J Health Dev. (2006) 20:55–7. doi: 10.4314/ejhd.v20i1.10012
18. Kebede D, Alemayehu A, Biniam G, Wassie L, Yismaw D. Uptake and barriers of voluntary counselling and testing among antenatal care attendants, south west Ethiopia. Ethiopian J Health Sci. (2006) 16:71–81. Available online at: https://www.ajol.info/index.php/ejhs/article/viewFile/146119/135630
19. Kongnyuy EJ, Mbu ER, Mbopi-Keou FX, Fomulu N, Nana PN, Tebeu PM, et al. Acceptability of intrapartum HIV counselling and testing in Cameroon. BMC Pregnancy and Childbirth. (2009) 9:9. doi: 10.1186/2F1471-2393-9-9
20. Creek TL, Ntumy R, Seipone K, Smith M, Mogodi M, Smit M, et al. Successful introduction of routine opt-out HIV testing in antenatal care in Botswana. J Acquir Immune Defic Syndr. (2007) 45:102–7. doi: 10.1097/QAI.0b013e318047df88
21. Chandisarewa W, Stranix-Chibanda L, Chirapa E, Miller A, Simoyi M, Mahomva A, et al. Routine offer of antenatal HIV testing (“opt-out” approach) to prevent mother-to-child transmission of HIV in urban Zimbabwe. Bull World Health Organ. (2007) 85:843–50. doi: 10.2471/blt.06.035188
22. Homsy J, Kalamya JN, Obonyo J, Ojwang J, Mugumya R, Opio C, et al. Routine intrapartum HIV counselling and testing for prevention of mother-to-child transmission of HIV in a rural Ugandan Hospital. J Acquir Immune Defic Syndr. (2006) 42:149–54. doi: 10.1097/01.qai.0000225032.52766.c2
23. McQuoid M. Routine testing for HIV-ethical and legal implications. S Afr Med J. (2007) 97:416–20. Available online at: http://www.samj.org.za/index.php/samj/article/view/823/290
24. Rennie S, Behets F. Desperately seeking targets: the ethics of routine HIV testing in low income countries. Bull World Health Organ. (2006) 84:52–7. Available online at: https://www.scielosp.org/pdf/bwho/2006.v84n1/52-57/en
25. Ujiji OA, Rubenson B, Ilako F, Marrone G, Wamalwa D, Wangalwa G, et al. Is ‘opt-out HIV testing' a real option among pregnant women in rural districts in Kenya? BMC Public Health. (2011) 11:151. doi: 10.1186/1471-2458-11-151
Keywords: pregnant women, utilization, provider-initiated HIV testing and counseling, PMTCT, Ethiopia
Citation: Gebresillassie BM, Emiru YK, Erku DA, Mersha AG, Mekuria AB, Ayele AA and Tegegn HG (2019) Utilization of Provider-Initiated HIV Testing and Counseling as an Intervention for PMTCT Services Among Pregnant Women Attending Antenatal Clinic in a Teaching Hospital in Ethiopia. Front. Public Health 7:205. doi: 10.3389/fpubh.2019.00205
Received: 16 October 2018; Accepted: 09 July 2019;
Published: 24 July 2019.
Edited by:
Heather Honoré Goltz, University of Houston–Downtown, United StatesReviewed by:
Pradeep Nair, Central University of Himachal Pradesh, IndiaCopyright © 2019 Gebresillassie, Emiru, Erku, Mersha, Mekuria, Ayele and Tegegn. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yohannes Kelifa Emiru, am9obmtlbGlmYUBnbWFpbC5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.