- 1Department of Public Health Sciences, Medical University of South Carolina, Charleston, SC, United States
- 2Arnold School of Public Health, University of South Carolina, Columbia, SC, United States
Background: On January 6, 2005, a train derailed in Graniteville, South Carolina, releasing nearly 60,000 kg of toxic chlorine gas. The disaster left nine people dead and was responsible for hundreds of hospitalizations and outpatient visits in the subsequent weeks. While chlorine gas primarily affects the respiratory tract, a growing body of evidence suggests that acute exposure may also cause vascular injury and cardiac toxicity. Here, we describe the incidence of cardiovascular hospitalizations among residents of the zip codes most affected by the chlorine gas plume, and compare the incidence of cardiovascular discharges in the years leading up to the event (2000–2004) to the incidence in the years following the event (2005–2014).
Methods: De-identified hospital discharge information was collected from the South Carolina Revenue and Fiscal Affairs Office for individuals residing in the selected zip codes for the years 2000 to 2014. A quasi-experimental study design was utilized with a population-level interrupted time series model to examine hospital discharge rates for Graniteville-area residents for three cardiovascular diagnoses: hypertension (HTN), acute myocardial infarction (AMI), and coronary heart disease (CHD). We used linear regression with autoregressive error correction to compare slopes for pre- and post-spill time periods. Data from the 2000 and 2010 censuses were used to calculate rates and to provide information on potential demographic shifts over the course of the study.
Results: A significant increase in hypertension-related hospital discharge rates was observed for the years following the Graniteville chlorine spill (slope 8.2, p < 0.001). Concurrent changes to CHD and AMI hospital discharge rates were in the opposite direction (slopes −3.2 and −0.3, p < 0.01 and 0.14, respectively). Importantly, the observed trend cannot be attributed to an aging population.
Conclusions: An unusual increase in hypertension-related hospital discharge rates in the area affected by the Graniteville chlorine spill contrasts with national and state-level trends. A number of factors related to the spill may be contributing the observation: disaster-induced hypertension, healthcare services access issues, and, possibly, chlorine-induced susceptibility to vascular pathologies. Due to the limitations of our data, we cannot determine whether the individuals who visited the hospital were the ones exposed to chlorine gas, however, the finding warrants additional research. Future studies are needed to determine the etiology of the increase and whether individuals exposed to chlorine are at a heightened risk for hypertensive heart disease.
Introduction
In the early morning hours of January 6, 2005, a freight train carrying three tank cars full of liquid chlorine derailed near the center of Graniteville, South Carolina, USA. One of the chlorine tanks ruptured in the accident, releasing nearly 60,000 kg of chlorine gas (1–3), which quickly overwhelmed workers on the graveyard shift at the nearby Avondale Mills textile plant. As the dense gas plume spread and settled in the valley, thousands of residents were exposed to the poisonous gas. A mass evacuation of the surrounding communities lasted for several days while emergency crews decontaminated the area, and photographs of the aftermath captured bleached and dead foliage and wildlife (4, 5). Ultimately, the disaster left nine people dead and was responsible for 72 hospitalizations and more than 840 emergency room and outpatient visits in the subsequent days (1, 2, 6, 7). Beyond the initial acute effects of chlorine gas, the results of public health-related screenings of exposed Graniteville residents demonstrated that the harmful pulmonary effects of exposure continued for months after the event (7, 8).
A substantial body of research has characterized the immediate effects of chlorine in animal models and humans (9–11). Following acute chlorine exposure, individuals are at risk for pulmonary edema, respiratory failure, and death by suffocation (9, 12). Consistent with the literature, studies of patient hospitalizations following the Graniteville train derailment confirmed the occurrence of frequent respiratory symptoms, and autopsies of the nine dead listed the primary cause of death as asphyxia or acute respiratory failure (1, 2). While the primary effects of acute exposure occur in the respiratory tract, a growing body of evidence suggests chlorine can also cause vascular injury and cardiac toxicity resulting in increased long-term cardiovascular risks (5, 13–15). In Graniteville, autopsies found eight of the nine dead suffered from cardiomegaly(7), and a study of lung function in the Avondale mill workers conducted 7 to 9 years after the event noted that 12% of subjects were unable to complete spirometry tests due to uncontrolled elevated blood pressure.
In addition to the health risks posed by chlorine gas exposure, a second threat to the cardiovascular health of the Graniteville community is “disaster-induced hypertension” (16). A number of studies conducted in the aftermath of natural and anthropogenic disasters have documented an increase in cardiovascular-related problems following the events. For example, following the 2011 earthquake and tsunami in Japan, Aoki et al. identified an increase in all types of cardiovascular disease events that lasted between 2 and 4 weeks and occurred in regions where radiation contamination was low (17). Similarly, researchers found a rise in cerebrovascular and heart disease hospitalizations and deaths after the World Trade Center Disaster in 2001 (18), and a 3-fold increase in acute myocardial infarctions in the 6 years following Hurricane Katrina (19). Activation of the sympathetic nervous system is postulated to be the primary driver of the phenomenon, likely due to disrupted circadian rhythms and psychological stress (20). Such activation of the sympathetic nervous system may, in turn, increases heart rate, blood pressure variability, and platelet activation (20).
Despite the documented risks to heart health, no studies to-date have investigated cardiovascular disease incidence in populations exposed to chlorine gas. Moreover, little is known about the long-term health effects of acute chlorine exposure, particularly cardiovascular disease. This study had two aims: (1) to describe the incidence of cardiovascular hospitalizations in the years surrounding the Graniteville chlorine spill, and (2) to determine whether there were significant changes in cardiovascular hospitalizations observed (at the population level) following the event.
Methods
Exposure Assessment
In a 2015 article, Jani et al. modeled the dispersion of the Graniteville chlorine plume using the Hazard Prediction and Assessment Capability (HPAC) modeling system, which incorporates topographical and meteorological data to optimize accuracy (3). This model was later validated with exposure indicator data (21). Using a geographical overlay of the published plume model, we selected seven zip codes that were most affected by the chlorine plume for our study area: 29801, 29816, 29828, 29829, 29834, 29850, and 29851. The plume area lies within Aiken County, SC and includes about 45,000 residents.
Outcome Data
De-identified hospital discharge information was collected from the South Carolina Revenue and Fiscal Affairs Office (SC RFA) for individuals residing in the selected zip codes. Data were available for the years 2000 through 2014 and captured discharges of the Graniteville residents from hospitals located in other states in addition to discharges from South Carolina hospitals. To protect patient confidentiality visit dates were limited to the year of hospital discharge, and patient age was provided in 5-year age categories. Records associated with the following ICD-9 codes were included in our analysis: acute myocardial infarction (AMI), ICD-9 code 410; hypertension, ICD-9 codes 401-404; and coronary heart disease (CHD) excluding AMI, ICD-9 codes 411-414, and 429.2. Selected records included both primary and secondary cardiovascular diagnoses, and individual patients were included more than once if s/he was discharged from the hospital multiple times with cardiovascular diagnoses. We were unable to assess repeated hospitalizations with this de-identified design. Admission records with multiple types of cardiovascular-related diagnoses were included in the statistics for each type of cardiovascular-related complaint (AMI, hypertension, or CHD).
Demographic Data
Population demographic information was collected for each zip code from the 2000 and 2010 U.S. Censuses (22). To assess whether shifting demographic characteristics played a role in the rate of cardiovascular hospital discharges, the population composition for 2000 and 2010 were compared. We were specifically interested in age, sex, and race variables, as cardiovascular disease is influenced by these factors.
Statistical Analysis
We used Microsoft Access (Redmond, WA) to store and query study data, and SAS 9.2 software (SAS Institute; Cary, NC) to calculate descriptive statistics and perform regression modeling. Summary statistics were calculated for each cardiovascular diagnosis by sex, payer type (Medicare/Medicaid, private insurance, or self-pay), visit type, race, and age categories. Mean annual rates of total and diagnosis-specific hospital discharges were calculated and stratified by sex and by age group. As dates of hospital visits were limited to the year of discharge, the rates calculated for 2005 included 5 days of “unexposed” time due to the chlorine disaster occurring on January 6, 2005.
We used a population-level interrupted time series design to compare trends in hospital discharge rates over time for the pre- and post-chlorine spill periods. To model trends in annual hospital discharge rates, linear regression with autoregressive error correction was used to adjust for serially correlated residuals (PROC AUTOREG in SAS) (23, 24). For each specified diagnosis, slopes and intercepts of the regression models were estimated for the time period leading up to the chlorine spill (2000–2004) and for the years following the event (2005–2014). In time series modeling, temporally variant covariates are most relevant (25). Therefore, population composition from the 2000 and 2010 censuses were compared to assess significant demographic shifts over the course of the study period. Any remaining unmeasured invariant covariates cannot confound these models because their effects would not vary between the pre- and post- exposure periods.
Ethical Considerations
Before receipt, all data were de-identified and aggregated to the yearly average by the SC RFA. This study was reviewed and approved by the Medical University of South Carolina's Institutional Review Board and the SC RFA data oversight committee. To further protect the privacy of area residents, the data presented are aggregated by zip codes or aggregated over the entire study area.
Results
We identified 13,275 hospital discharge records associated with one or more of the specified cardiovascular diagnostic codes between 2000 and 2014 in the study zip codes. Of all cardiovascular-related discharges, 5,669 (42.7%) included a primary or secondary diagnosis of CHD, 10,698 (80.6%) referenced hypertension diagnoses, and 1,046 (7.9%) cited an AMI diagnosis (Table 1). Men comprised the minority of hypertension-related discharges (42.2%), but represented the majority of visits for coronary heart disease (56.6%) and acute myocardial infarction (54.4%). Most of the patients seen were between the ages 65 and 74 (21.7%), followed closely by those aged 55 to 64 (21.3%) and 45 to 54 (19.6%). Only 1.1% of the hospital discharge records for our selected outcomes were for patients under the age of 25. Of those, most were related hypertension.
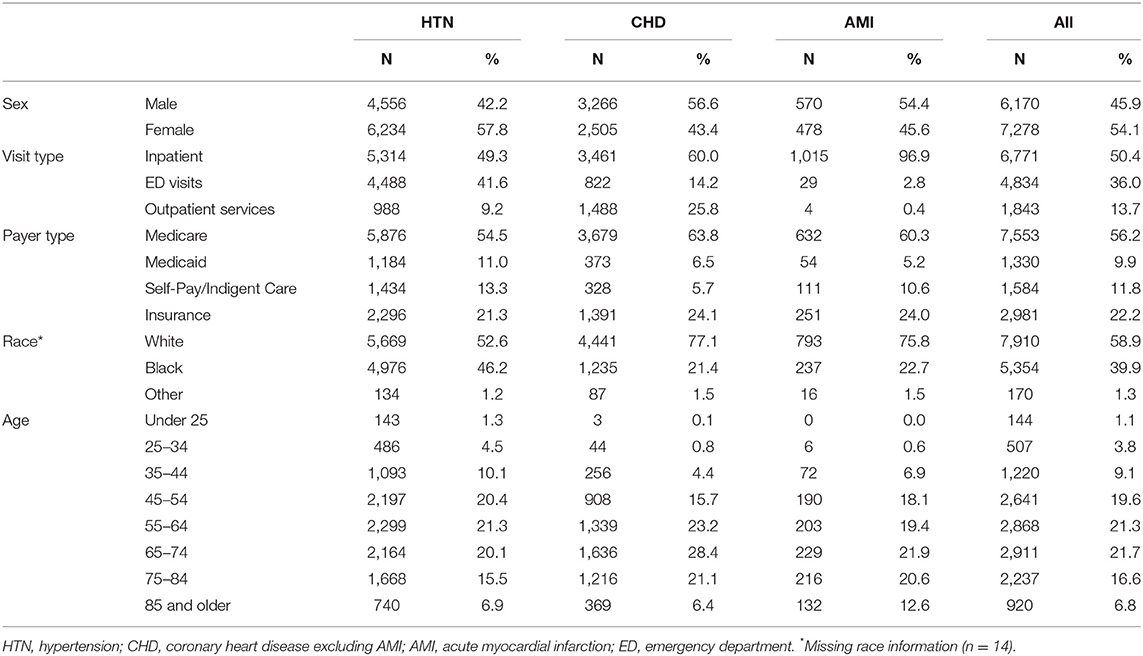
Table 1. Characteristics of cardiovascular hospital discharges by diagnosis (primary or secondary) among Graniteville-area residents for the years 2000–2014.
About half of the hypertension and CHD hospital discharge records were for inpatient visits (49.3% and 60.0%, respectively), while the almost all of the AMI-related discharges were for inpatient visits (96.9%). Emergency Department visits comprised 14.2% of the CHD visits 41.6% of hypertension visits, and 2.8% of AMI visits. The remaining records were for outpatient services, which included imaging, observation, and outpatient surgical procedures (9.2, 25.8, and 0.4% for hypertension, CHD, and AMI diagnoses, respectively).
Figure 1 illustrates the annual admission rates for our diagnoses of interest with the year of the chlorine accident noted with a dashed line to facilitate easy comparison of the pre/post disaster time periods. Upon examination of the annual trends in hospital discharge rates (Figure 1), we saw a pronounced increase in hypertension hospital discharges over time in contrast to small changes in CHD and AMI discharges. Rates of hypertension discharges rose from 120.7 per 10,000 in 2000 to 183.6 in 2014, an increase of 52%. At its peak in 2012, the rate was 219.5 per 10,000 which represents almost a 2-fold increase over the 2000 rate. A minor decrease in AMI rates was present over the study period: from 21.0 discharges per 10,000 persons to 15.6 per 10,000. This represents a 28% decrease. Rates of CHD-related hospital discharges experienced a marked declined over the study period, dropping from 118.3 per 10,000 persons in 2000 to 58.6 per 10,000 persons in 2014.
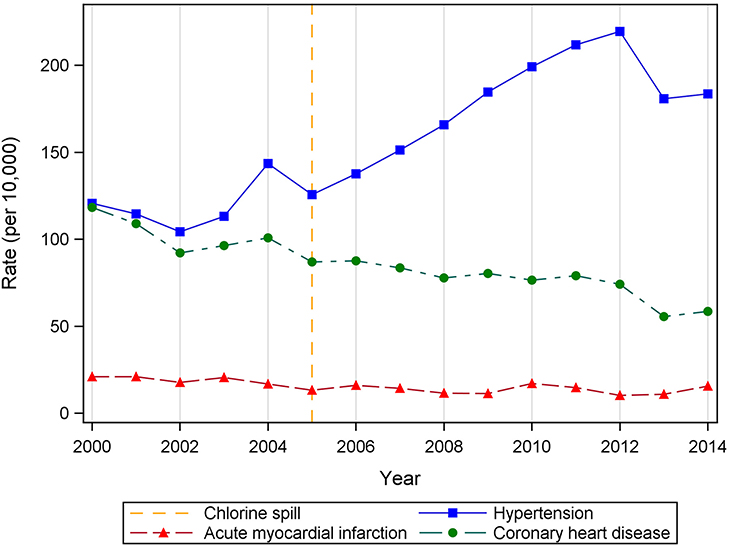
Figure 1. Annual rates of cardiovascular hospital discharges by diagnosis (primary or secondary) among Graniteville-area residents, 2000–2014.
Examination of annual discharge rates by diagnosis and visit type (Figure 2, dashed line represents the year of the chlorine disaster) showed the upward trend in hypertension-related discharges is largely attributable to emergency room visits. Emergency room discharge rates for hypertension more than doubled from 43.9 per 10,000 in 2004 to a high of 112.0 per 10,000 in 2012. A concurrent decrease was seen in CHD inpatient discharges, from 64.7 per 10,000 in 2004 to a low of 31.0 per 10,000 in 2013 (Figure S1, Supplementary Material). No notable changes in discharge rates by visit type were apparent among AMI-related hospital visits, as very few visits occurred in an outpatient or emergency room setting (Figure S2, Supplementary Material).
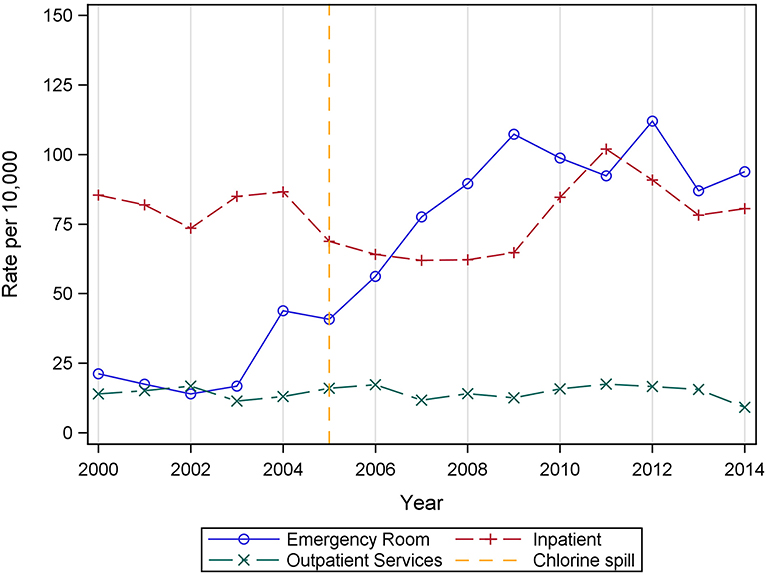
Figure 2. Annual rates of hospital discharges with a primary or secondary diagnosis of hypertension by visit type among Graniteville-area residents, 2000–2014.
When comparing the time periods before the chlorine spill (2000–2004) and after the event (2005–2014), the mean annual rates of hypertension associated discharges increased from 119.3 to 176.0 per 10,000 people (Table 2). In contrast, coronary heart disease and acute myocardial infarction-related discharges decreased in the years following the chlorine gas release, from 103.4 to 76.0 per 10,000 people and 19.4 to 13.5 per 10,000 people, respectively. This pattern held when stratified by sex, but a slightly different picture emerged when pre- and post-spill admission rates were examined by age group. For people 45 years of age and older, the overall trends persisted: mean annual hypertension-related discharge rates increased from the pre-spill period to the post-spill period, while CHD and AMI discharge rates decreased. However, shifts in the rates of cardiovascular discharges were more heterogeneous for Graniteville area residents under age 45. Among those under age 25, 25–34, and 35–44 years, most discharge rates either increased or remained the same for all three diagnoses, except for AMI in 25–34 year olds which decreased slightly from 2.9 to 2.7 discharges per 10,000 persons (Table 2).
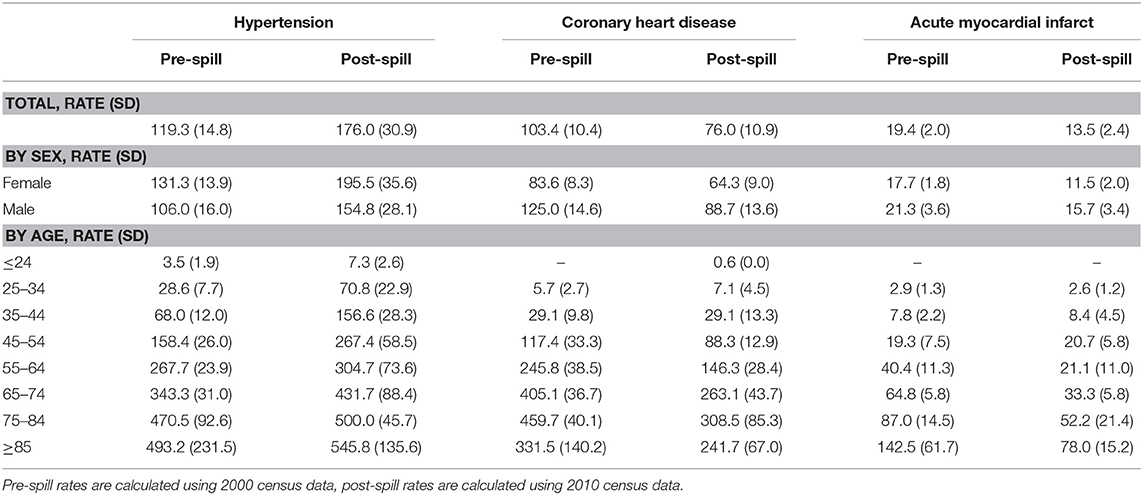
Table 2. Mean annual rates (per 10,000 population) of cardiovascular hospital discharges for Graniteville area residents by diagnosis, gender, and age for the time period leading up to (2000–2004) and following (2005–2014) the chlorine gas release.
Results of the linear regressions for time series data indicated that the post-spill time period was associated with a significant increasing trend for hypertension-related hospital discharges, 8.2 for 2005–2014 vs. 5.2 for 2000–2004 (Table 3). The pre-spill time period was not associated with a statistically significant trend. Hospital discharges with CHD diagnoses were statistically significantly decreasing over time, and the slope of the regression model was steeper in the pre-spill period (−4.8, p = 0.007) compared to the post-spill years (−3.2, p < 0.001). Rates of AMI hospital discharges also decreased over the pre-spill time period (−1.5, p = 0.03), but the slope for the post-chlorine spill period was not statistically significant (p = 0.14).
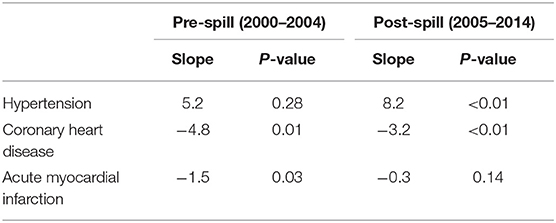
Table 3. Results of the linear regression analyses for annual rates of cardiovascular hospitalizations by diagnosis for the years leading up to the chlorine spill (2000–2004) and the years following the spill (2005–2014).
Discussion
We assessed three cardiovascular outcomes following a rare mass chlorine exposure event. Based on our analysis of administrative records, we were able to establish a temporal relationship between the chlorine spill and an increase in hypertension-related hospital discharges among residents of the area most impacted by the chlorine gas plume. However, due to the de-identified nature of our data source, we cannot say with any certainty whether the individuals who visited the hospital were also those exposed to chlorine. Future research is needed to clarify the etiology of the observed trend. To that end, we suggest three factors that may have contributed to the rise in hypertension hospitalizations and warrant attention: disaster-related hypertension, insufficient access to healthcare services, and chlorine-induced vascular damage.
The significant increasing trend in hypertension-related hospital discharges for the years 2005–2014 following the Graniteville train derailment and chlorine spill was surprising. Within our study population, concurrent changes in CHD and AMI hospital discharge rates were in the opposite direction. Furthermore, the upward trajectory contrasts with national trends in the prevalence of self-reported hypertension, which remained unchanged from 1999 to 2014, and in the number of inpatient discharges with a primary diagnosis of high blood pressure, which also remained static from 2000 to 2010 (26, 27). Within South Carolina, there was a minor increase in hypertension prevalence, from 28.8% in 2000 to 31.7% in 2009. But the incidence of heart disease hospitalizations has steadily declined over the same period, as have hospital visits for myocardial infarctions, specifically (28). It is important to note that the increasing trend cannot be attributed to an aging population because the demographic composition of the study population remained largely unchanged from 2000 to 2010 (Table 4), and within our dataset, the highest increases in hospital discharges following the chlorine spill were observed in younger age groups (<45 years).
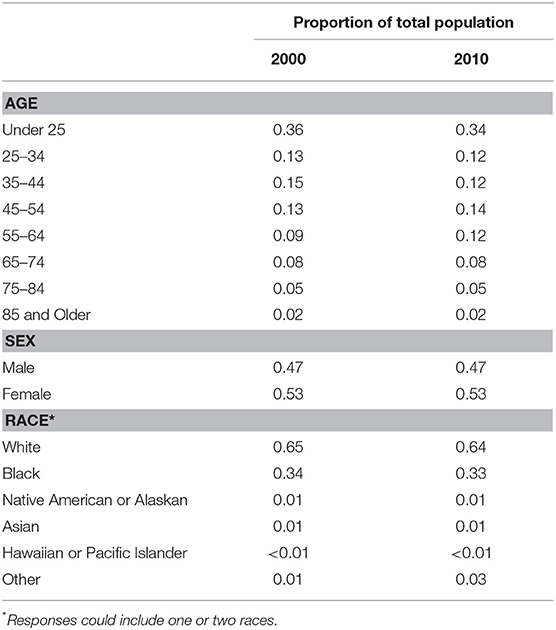
Table 4. Age, sex, and racial composition of the raniteville study population from the 2000 and 2010 censuses.
Limited access to healthcare services may have contributed to the observed rise in hypertension emergency room and hospital discharges. Within the hypertension diagnosis group, the greatest increase was seen in emergency department visits. Healthcare systems already taxed beyond capacity treating an influx of acute injuries during a disaster may be further overwhelmed by patients with exacerbated chronic conditions in the weeks and months following the event (29, 30). The phenomenon, known as a secondary surge, is consistent with descriptions of overbooked providers and insufficient medical resources in Graniteville during the recovery period (31). Further compounding the situation, the Avondale textile mill closed <2 years after the disaster, leaving more than 1,600 workers and their families without income or health insurance (32).
Disaster-related hypertension may also be independently influencing the observed trends in Graniteville cardiovascular hospital discharges. While the delayed onset of the increase is inconsistent with findings from studies conducted by Swerdel et al. and Nakamura et al., who noted an immediate increase in cardiovascular hospital discharges following Hurricane Sandy and the 2011 Japanese earthquake and tsunami, respectively (33, 34), other researchers have observed that cardiovascular effects of disasters may persist much longer. Aoki et al. found an increase of weekly occurrences of heart failure, acute coronary syndrome, stroke, and cardiopulmonary arrest in the three years following the Great East Japan Earthquake(17), Peters et al. observed a 3-fold increase in AMI incidence in the 6 year period following Hurricane Katrina (19), and Ohira et al. saw changes to blood pressure persisted for years among Japanese evacuees affected by the 2011 earthquake and tsunami (35). Although the specific biological mechanisms responsible for adverse cardiovascular symptoms following disasters are not fully understood, the effects may be further compounded by heightened susceptibility to vascular pathologies introduced by chlorine exposure among Graniteville residents.
Another factor which may be contributing to the unusual increase in hypertension-related hospital discharges is chlorine-induced systemic vascular damage among Graniteville residents exposed to the spill. As a member of the highly reactive halogen elements, chlorine readily forms hydrochloric (HCl) and hypochloric (HOCl) acids and oxygen free radicals when it comes into contact with water in the mucous membranes and alveolar spaces (11). The hydrolytic products exhaust stores of antioxidants, activate pro-inflammatory cells, and interfere with cell signaling (10, 36). As an example of the latter, chlorine has been shown to interfere with endothelial nitric oxide synthase (eNOS)-mediated signaling in animal models (37). Nitric oxide produced by eNOS regulates vasodilation and is responsible for maintaining vascular homeostasis; so disruption of this pathway results in increased susceptibility to hypertension and inflammation (37, 38). A second potential mechanism for chlorine-induced vascular disease is attributable to one of the products of chlorine's hydrolysis, HOCl. Hypochloric acid is known to react with low- and high-density lipoproteins (LDL and HDL) converting the molecules into pro-atherogenic compounds (39). Heightened vulnerability to chronic vascular dysfunction instigated by chlorine exposure may explain why the rise of related hospital discharges peaked years after the event. While the damage to lung epithelial tissue occurs within minutes of exposure, the systemic diffusion of pro-inflammatory cells and secondary reactive oxygen and chlorine species prolongs the physiological damage and may initiate biological processes with long-term health consequences (38).
Our study has important clinical significance. Elevated blood pressure may be involved with the risks associated with lung function and cardiovascular disease. Numerous population studies have shown that airflow restriction (as measured by forced expiratory volume in 1 s (FEV 1) or the FEV 1/forced vital capacity ratio) is a predictor of future risk of hypertension (40). Further, chronic obstructive pulmonary disease (COPD) has been associated with cardiovascular events (41), congestive heart failure, ischemic heart disease, arrhythmia, stroke, hypertension, and peripheral artery disease (42). This association is supported by research which demonstrates that airflow limitation is a predictor of future risks of hypertension and cardiovascular events (43). The 2017 American College of Cardiology (ACC)/American Heart Association (AHA) Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults, which provides an evidence-based approach to reduce CVD risk through lowering of blood pressure, redefined the lower threshold for systolic blood pressure to a target of <130 mm Hg to reduce the risk of several important outcomes including risk of myocardial infarction, stroke, heart failure, and major cardiovascular events(44, 45). The implications for a high risk population such as Graniteville is that these recommendations increase the number of individuals at risk from the lung effects on elevated blood pressure.
Our study also points toward an important public health problem. Individuals in disadvantaged communities are unlikely to receive regular routine health care and long-term follow up. This allows slowly developing but potentially life-threatening problems, such as hypertension, to go undetected for long periods of time. Even if such a problem is discovered, the individual may not be followed on a regular basis to ensure adequate long-term control. The lack of routine care also increases the probability that individuals in such communities will not be referred for mental health care if they develop symptoms of anxiety, depression or post-traumatic stress after a disaster. At the least, an effort to regularly assess blood pressures among potentially affected residents and to provide appropriate treatment referrals would likely be highly beneficial at relatively modest cost.
To our knowledge, this is the first study to examine temporal trends in cardiovascular hospitalizations following a mass chlorine exposure event. Use of a comprehensive administrative data set that included hospital discharges from other states in addition to South Carolina is a strength of our study. We were also able to avoid the need for extensive information on covariates with the use of a quasi-experimental interrupted time series design.
There are also limitations to this study As discussed earlier, we cannot say with certainty whether the individuals who visited the hospital were also those who were exposed to the chlorine gas plume or were directly impacted by the resulting disaster effects on the community. Further research is needed to determine if this is the case, and if so, what are the biologic mechanisms underlying the association. Additionally, our population-level design cannot assess disease etiology at an individual level, only at the population level, and we cannot discern which of disaster risk factors best explained the observed effects on CVD or whether their effects were synergistic. Further study is needed to assess whether these observed effects were caused by chlorine exposure, disaster-related stress, impaired healthcare services, and/or some yet unmeasured risk factor. Other limitations of our study design include limited statistical power and the potential for misclassification. Because our data was aggregated by year, there were only five time points available for the “pre-spill” period. Addresses used to select our study population were provided by patients and may not have been the address where the patient was located during the chlorine disaster. Additionally, only the year of discharge was available to us, so the “post-spill” time period included 5 days of “unexposed” time.
Conclusion
The utility of chlorine in diverse household and industrial applications ensures the chemical's ubiquity will persist. With domestic production of chlorine nearing 10 million metric tons annually, there continues to be real concern for another large industrial or transport accident (46). Indeed, the Department of Homeland Security included chlorine in one of its 15 “National Planning Scenarios” and lists chlorine among the “chemicals of concern” in the Chemical Facility Anti-Terrorism Standards (6 CFR Part 27) (47–49). Therefore, it would be prudent to improve our understanding of the persistent health effects from chlorine exposure so that we can be better prepared for future incidents involving chlorine.
Our study suggests that chlorine itself or stress associated with exposure to a chlorine disaster may be associated with later development of hypertension. Further research is needed to determine whether the residents of Graniteville exposed to chlorine or the resulting traumatic stress are at an increased risk for hypertension or other cardiovascular events, and if so, to elucidate the physiological processes responsible for systemic vascular damage. Nevertheless, this study is a small step toward identifying and characterizing an association that has the potential to cause considerable excess morbidity and costs to our healthcare system should another large-scale release of chlorine occur in the future.
Ethics Statement
This study was reviewed and approved by the Medical University of South Carolina Institutional Review Board and the South Carolina Revenue and Fiscal Affairs data oversight committee. Before receipt, all data were de-identified by the SC RFA, therefore the requirement of informed consent from individual subjects was waived by the IRB. To further protect the privacy of area residents, the data presented are in aggregate form.
Author Contributions
AH, JV, LI, and ES conceived and designed the study with statistical consultation with BC and AL. AH performed the analysis and took the lead in writing the manuscript with support from ES and JV. DL and ES also contributed to the interpretation of the results.
Funding
This study was partially supported through funding from the ATSDR (ATSDR grant 1E11TS000235-01: Rebuilding the Graniteville, SC Community through Public Health Communication and Tracking. Project Period: 09/30/2014 – 09/29/2015).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Our Graniteville community collaborators were instrumental in the public health activities related to this research. Louisiana Sanders and Anne Fulcher provided some excellent suggestions on the public health issues which were concerning this community. They had first suggested to us that there were some concerns with hypertension in the community, which proved to be valid. Chris Finney at the South Carolina Revenue and Fiscal Affairs office greatly assisted us with securing the data for this study. We would like to thank both Wilfried Karmaus and Dennis Ownby for their helpful comments on earlier versions of this paper. Danira Medunjanin was instrumental in coordinating the communication with the South Carolina Revenue and Fiscal Affairs office and between the authors regarding this and other related papers. We would like to acknowledge the contributions of Sacoby Wilson to the early development of the research questions assessed in this study and his leadership on a sister grant which contributed to this study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2019.00112/full#supplementary-material
Figure S1. Annual rates of hospital discharges with a primary or secondary diagnosis of coronary heart disease by visit type among Graniteville-area residents, 2000–2014.
Figure S2. Annual rates of hospital discharges with a primary or secondary diagnosis of acute myocardial infarction by visit type among Graniteville-area residents, 2000–2014.
References
1. Wenck MA, Van Sickle D, Drociuk D, Belflower A, Youngblood C, Whisnant MD, et al. Rapid assessment of exposure to chlorine released from a train derailment and resulting health impact. Public Health Rep. (2007) 122:784–92. doi: 10.1177/003335490712200610
2. Van Sickle D, Wenck MA, Belflower A, Drociuk D, Ferdinands J, Holguin F, et al. Acute health effects after exposure to chlorine gas released after a train derailment. Am J Emerg Med. (2009) 27:1–7. doi: 10.1016/j.ajem.2007.12.006
3. Jani D, Reed D, Feigley CE, Svendsen ER. Modeling an irritant gas plume for epidemiologic study. Int J Environ Health Res. (2016) 26:58–74. doi: 10.1080/09603123.2015.1020414
4. Abara W, Wilson S, Vena J, Sanders L, Bevington T, Culley J, et al. Engaging a chemical disaster community: lessons from Graniteville. Int J Environ Res Public Health. (2014) 11:5684–97. doi: 10.3390/ijerph110605684
5. Carlisle M, Lam A, Svendsen ER, Aggarwal S, Matalon S. Chlorine-induced cardiopulmonary injury. Ann N Y Acad Sci. (2016) 1374:159–67. doi: 10.1111/nyas.13091
6. Svendsen ER, Whittle NC, Sanders L, McKeown RE, Sprayberry K, Heim M, et al. GRACE: public health recovery methods following an environmental disaster. Arch Environ Occup Health. (2010) 65:77–85. doi: 10.1080/19338240903390222
7. Duncan MA, Drociuk D, Belflower-Thomas A, Van Sickle D, Gibson JJ, Youngblood C, et al. Follow-up assessment of health consequences after a chlorine release from a train derailment–Graniteville, SC, 2005. J Med Toxicol. (2011) 7:85–91. doi: 10.1007/s13181-010-0130-6
8. Clark KA, Chanda D, Balte P, Karmaus WJ, Cai B, Vena J, et al. Respiratory symptoms and lung function 8–10 months after community exposure to chlorine gas: a public health intervention and cross-sectional analysis. BMC Public Health. (2013) 13:945. doi: 10.1186/1471-2458-13-945
10. White CW, Martin JG. Chlorine gas inhalation: human clinical evidence of toxicity and experience in animal models. Proc Am Thorac Soc. (2010) 7:257–63. doi: 10.1513/pats.201001-008SM
11. CAMEO Chemicals. CHLORINE (CAS Number 7782-50-5). In: CAMEO Chemicals Version 2.7.1. Silver Spring, MD: U.S. National Oceanic and Atmospheric Administration, National Ocean Service, Office of Response and Restoration (2016). Available online at: https://cameochemicals.noaa.gov/chemical/2862 (accessed on December 16, 2016).
12. Hazardous Substances Data Bank. Chlorine (CASRN: 7782-50-5, UNII: 4R7X1O2820). In: TOXNET. Bethesda, MD: National Toxicology Information Program, National Library of Medicine (2016). Available online at: https://toxnet.nlm.nih.gov (accessed on December 18, 2016).
13. Suzuki S, Sakamoto S, Maniwa K, Saitoh A, Hirayama Y, Kobayashi H, et al. Fatal pulmonary arterial thrombosis associated with chlorine gas poisoning. Clin Appl Thromb Hemost. (2001) 7:356–8. doi: 10.1177/107602960100700420
14. Kose A, Kose B, Acikalin A, Gunay N, Yildirim C. Myocardial infarction, acute ischemic stroke, and hyperglycemia triggered by acute chlorine gas inhalation. Am J Emerg Med. (2009) 27:1022.e1–4. doi: 10.1016/j.ajem.2008.12.029
15. Zaky A, Bradley WE, Lazrak A, Zafar I, Doran S, Ahmad A, et al. Chlorine inhalation-induced myocardial depression and failure. Physiol Rep. (2015) 3:e12439. doi: 10.14814/phy2.12439
16. Nishizawa M, Hoshide S, Shimpo M, Kario K. Disaster hypertension: experience from the great East Japan earthquake of 2011. Curr Hypertens Rep. (2012) 14:375–81. doi: 10.1007/s11906-012-0298-z
17. Aoki T, Fukumoto Y, Yasuda S, Sakata Y, Ito K, Takahashi J, et al. The Great East Japan Earthquake Disaster and cardiovascular diseases. Eur Heart J. (2012) 33:2796–803. doi: 10.1093/eurheartj/ehs,288
18. Jordan HT, Stellman SD, Morabia A, Miller-Archie SA, Alper H, Laskaris Z, et al. Cardiovascular disease hospitalizations in relation to exposure to the September 11, 2001 World Trade Center disaster and posttraumatic stress disorder. J Am Heart Assoc. (2013) 2:e000431. doi: 10.1161/jaha.113.000431
19. Peters MN, Moscona JC, Katz MJ, Deandrade KB, Quevedo HC, Tiwari S, et al. Natural disasters and myocardial infarction: the six years after Hurricane Katrina. Mayo Clin Proc. (2014) 89:472–7. doi: 10.1016/j.mayocp.2013.12.013
20. Kario K. Disaster hypertension - its characteristics, mechanism, and management. Circ J. (2012) 76:553–62. doi: 10.1253/circj.CJ-11-1510
21. Jani DD, Wilson M, Wickliffe JK, Shaffer J, Middleton T, Rando R, et al. Assessment of an irritant gas plume model for epidemiologic study. Int J Environ Health Res. (2017) 27:276–92. doi: 10.1080/09603123.2017.1342226
22. U. S. Census Bureau. Zip Code Details Generated by Ashley Howell Using the American Fact Finder. Suitland-Silver Hill, MD: United States Census Bureau (2015).
23. Chipman JS. Efficiency of least-squares estimation of linear trend when residuals are autocorrelated. Econometrica. (1979) 47:115–28. doi: 10.2307/1912350
25. Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Belmont, CA: Wadsworth, Cengage Learning (2002).
26. Yoon SS, Fryar CD, Carrol MD. Hypertesion prevalence and control among adults: United States, 2011-2014. In: NCHS Data Brief, No 220. Hyattsville, MD: National Center for Health Statistics (2015). Available online at: https://www.cdc.gov/nchs/data/databriefs/db220.htm
27. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart Disease and Stroke Statistics-2016 update: a report from the American Heart Association. Circulation. (2016) 133:e38–360. doi: 10.1161/cir.0000000000000350
28. SC DHEC. Heart Disease and Stroke Prevention: Strengthening the Chain of Survival. Columbia, SC: South Carolina Department of Health and Environmental Control, Heart Disease and Stroke Prevention Division (2010).
29. Runkle JR, Brock-Martin A, Karmaus W, Zhang H, Svendsen ER. Secondary surge capacity: a framework for understanding long-term access to primary care among medically vulnerable populations in disaster recovery. Am J Public Health. (2012a) 102:e24–32. doi: 10.2105/AJPH.2012.301027
30. Runkle JR, Zhang H, Karmaus W, Brock-Martin A, Svendsen ER. Prediction of unmet primary care needs for the medically vulnerable post-disaster: an interrupted time-series analysis of health system responses. Int J Environ Res Public Health. (2012b) 9:3384–97. doi: 10.3390/ijerph9103384
31. Runkle JR, Zhang H, Karmaus W, Brock-Martin A, Svendsen ER. Long-term impact of environmental public health disaster on health system performance: experiences from the Graniteville, South Carolina chlorine spill. South Med J. (2013) 106:74–81. doi: 10.1097/SMJ.0b013e31827c54fc
32. Annang Ingram L, Tinago CB, Estrada R, Wilson S, Wright Sanders L, Bevington T, et al. Off the rails in rural South Carolina: a qualitative study of healthcare provider perspectives on the long-term health impact of the Graniteville train disaster. Rural Remote Health. (2016) 16:3906. Available online at: https://www.rrh.org.au/journal/article/3906
33. Nakamura M, Tanaka F, Nakajima S, Honma M, Sakai T, Kawakami M, et al. Comparison of the incidence of acute decompensated heart failure before and after the major tsunami in Northeast Japan. Am J Cardiol. (2012) 110:1856–60. doi: 10.1016/j.amjcard.2012.08.020
34. Swerdel JN, Janevic TM, Cosgrove NM, Kostis JB. The effect of Hurricane Sandy on cardiovascular events in New Jersey. J Am Heart Assoc. (2014) 3:e001354. doi: 10.1161/jaha.114.001354
35. Ohira T, Hosoya M, Yasumura S, Satoh H, Suzuki H, Sakai A, et al. Evacuation and risk of hypertension after the Great East Japan Earthquake: The Fukushima Health Management Survey. Hypertension. (2016) 68:558–64. doi: 10.1161/hypertensionaha.116.07499
36. Squadrito GL, Postlethwait EM, Matalon S. Elucidating mechanisms of chlorine toxicity: reaction kinetics, thermodynamics, and physiological implications. Am J Physiol Lung Cell Mol Physiol. (2010) 299:L289–300. doi: 10.1152/ajplung.00077.2010
37. Honavar J, Samal AA, Bradley KM, Brandon A, Balanay J, Squadrito GL, et al. Chlorine gas exposure causes systemic endothelial dysfunction by inhibiting endothelial nitric oxide synthase–dependent signaling. Am J Respir Cell Mol Biol. (2011) 45:419–25. doi: 10.1165/rcmb.2010-0151OC
38. Samal A, Honovar J, White CR, Patel RP. Potential for chlorine gas–induced injury in the extrapulmonary vasculature. Proc Am Thorac Soc. (2010) 7:290–3. doi: 10.1513/pats.201001-006S. M
39. Nicholls SJ, Hazen SL. Myeloperoxidase, modified lipoproteins, and atherogenesis. J Lipid Res. (2009) 50:S346–51. doi: 10.1194/jlr.R800086-JLR200
40. Engstrom G, Wollmer P, Valind S, Hedblad B, Janzon L. Blood pressure increase between 55 and 68 years of age is inversely related to lung function: longitudinal results from the cohort study 'Men born in 1914'. J Hypertens. (2001) 19:1203–8. doi: 10.1097/00004872-200107000-00004
41. Sin DD, Man SF. Chronic obstructive pulmonary disease as a risk factor for cardiovascular morbidity and mortality. Proc Am Thorac Soc. (2005) 2:8–11. doi: 10.1513/pats.200404-032MS
42. Mullerova H, Agusti A, Erqou S, Mapel DW. Cardiovascular comorbidity in COPD: systematic literature review. Chest. (2013) 144:1163–78. doi: 10.1378/chest.12-2847
43. Imaizumi Y, Eguchi K, Kario K. Lung disease and hypertension. Pulse. (2014) 2:103–12. doi: 10.1159/000381684
44. Reboussin DM, Allen NB, Griswold ME, Guallar E, Hong Y, Lackland DT, et al. Systematic review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. (2018) 71:2176–98. doi: 10.1016/j.jacc.2017.11.004
45. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. (2018) 71:e127–248. doi: 10.1016/j.jacc.2017.11.006
46. United States. “Chemical Data Reporting Database: Chlorine (7782-50-5)”. Washington, DC: US Environmental Protection Agency, Pollution Prevention and Toxics (2012).
47. Electronic Code of Federal Regulations. Electronic Code of Federal Regulations Part 27 - Chemical Facility Anti-Terrorism Standards. In: Department of Homeland Security, editor. Title 6: Domestic Security. Washington, DC: U.S. Government Publishing Office (2007).
48. Gussow L. Disaster Scenario: Tons of Chlorine Transported by U.S. Rail. Emerg Med. News. (2007) 29:12.
49. Jones R, Wills B, Kang C. Chlorine gas: an evolving hazardous material threat and unconventional weapon. West J Emerg Med. (2010) 11:151–6. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2908650/
Keywords: chlorine poisoning, chemical hazards release, disasters, hypertension cardiovascular disease, toxic gas exposure, disaster epidemiology
Citation: Howell AV, Vena JE, Cai B, Lackland DT, Ingram LA, Lawson AB and Svendsen ER (2019) Temporal Trends in Cardiovascular Hospital Discharges Following a Mass Chlorine Exposure Event in Graniteville, South Carolina. Front. Public Health 7:112. doi: 10.3389/fpubh.2019.00112
Received: 20 December 2018; Accepted: 17 April 2019;
Published: 08 May 2019.
Edited by:
Randy D. Kearns, University of New Orleans, United StatesReviewed by:
Mark A. Kirk, University of Virginia Health System, United StatesDagan Schwartz, Ben-Gurion University of the Negev, Israel
Copyright © 2019 Howell, Vena, Cai, Lackland, Ingram, Lawson and Svendsen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: John E. Vena, dmVuYUBtdXNjLmVkdQ==
 Ashley V. Howell
Ashley V. Howell John E. Vena1*
John E. Vena1* Daniel T. Lackland
Daniel T. Lackland