- 1Department of Human Nutrition, Foods, and Exercise, Virginia Tech, Blacksburg, VA, United States
- 2Extension, University of Wyoming, Lander, WY, United States
- 3Translational Biology, Medicine, and Health, Department of Human Nutrition, Foods, and Exercise, Virginia Tech, Blacksburg, VA, United States
Introduction: A number of effective physical activity programs for older adults exist, but are not widely delivered within community settings, such as the Cooperative Extension System. The purpose of this paper was to determine if an evidence-based intervention (EBI) developed in one state Extension system could be scaled-out to a new state system.
Methods and results: The RE-AIM (reach, effectiveness, adoption, implementation, maintenance) framework was used to guide an iterative evaluation of three translational stages. Stage 1: Before program adoption, Extension health educators were surveyed and interviewed to assess physical activity programming perceptions and factors that may influence their decision to attend training or deliver the program in practice. Results indicated that a virtual, scalable training protocol would be necessary and that training needed to include hands-on instruction and be catered to those who were less confident in physical activity program delivery. Stage 2: Training attendees were surveyed pre- and post-training on factors related to the adoption-decision making process and contacted post-training to assess program delivery status. Training did not influence perceptions of the program, intent to deliver, or confidence in delivering the program. Stage 3: During program implementation, the program was evaluated through the RE-AIM framework by surveying across three key stakeholder groups: (1) program participants, (2) potential delivery personnel, and (3) Extension administrators. Findings indicate that the program has the potential to reach a large and representative proportion of the target audience, especially in rural areas. However, adoption and implementation rates among Extension health educators and community partners were low and data collection for effectiveness, implementation, and maintenance was a challenge.
Conclusion: Overall, the results indicate initial struggles to translating and evaluating the program in a large, rural state. Implications for practice include making system-level changes to increase physical activity program adoption rates among Extension health educators and improve data collection and program evaluation through this community-based organization. More work is needed to identify infrastructure support and capacity to scale-out EBIs.
Introduction
Delivering (and sustaining) evidence-based interventions (EBI) in community practice is challenging. One challenge is that delivery personnel have to select an intervention and ensure its fit within the mission, values, and resources of the system they are delivering (1). County-based delivery personnel in the land-grant university Cooperative Extension Service (Extension) have the autonomy to select open-access (i.e., open to all, without restriction due to sex, socioeconomic status, or, more notably, health condition) interventions for their county residents (2). One target audience for whom Extension professionals provide services is older adults. As only 12% of this population is meeting physical activity recommendations, and new efforts within Extension are geared toward promoting physical activity (3–5), it is necessary to understand existing programs, their impacts, and how to scale-out interventions (6) across Extension state systems. Scale-out is “a deliberate effort to broaden the delivery of an EBI. Scale-out is an extension of scale-up and uniquely refers to the deliberate use of strategies to implement, test, improve, and sustain an EBI as it is delivered to new populations and/or through new delivery systems that differ from those in effectiveness trials.” [(6) p. 3].
One way that Extension has been challenged at scale-out is that rather than scaling core elements of “what works,” new or unique programs are introduced to the system. This is evidenced by a recent systematic review of open-access physical activity interventions for older adults which found that 17 unique open-access physical activity programs were offered by Extension professionals (7). In addition to duplicated efforts, both the fidelity to the underlying evidence-based program principles and the impact of these open-access interventions on older adult physical activity levels is underreported (7).
In order for this process of scale-out to be successful, information about how and why the intervention works is needed, as much as whether the intervention worked or not (6, 8, 9). Notably, there are three types of scale-out: EBI scaled-out to (1) the same population through a different system, (2) different population, same delivery system, and (3) different population and different delivery system (6). However, while the national Extension system is “one delivery system,” the structure of each state may be somewhat unique. In addition, while “older adults” may be one population, older adults from one state may experience different barriers and facilitators to program adherence when compared to older adult population in a different state. Therefore, the degree to which an EBI can be scaled-out from one state Extension system to another is difficult to discern.
One way to understand scale-out of EBI from one state system to another is to use pragmatic data collection. Pragmatism focuses on “issues and data relevant for making decisions and taking action [10, p.257].” This type of evaluation is especially useful in community settings that may not have substantial research funding, and can move beyond evaluating intervention effectiveness and determine for whom, where, when, why, and how an intervention is working in a given context (11). The RE-AIM (reach, efficacy, adoption, implementation, maintenance) framework can be used to systematically capture perceptions, decision making, and impacts (8, 9, 12, 13).
Using these key considerations, researchers and practitioners can iteratively engage to reflect on successes and failures related to adoption and implementation through a participatory approach (1). Collecting pragmatic measures within a participatory approach is crucial to understand how and why an evidence-based intervention may be delivered outside of the context in which it was developed. Taken together, the research question was: Can an EBI developed in one state Extension system be scaled-out to a new state system? Capturing this context-driven work is essential to understanding why and how interventions are adopted, implemented, and maintained within delivery systems so they can be scaled-out to reach broader populations.
Materials and Methods
Design
As recently proposed by members of the National Working Group on RE-AIM Planning and Evaluation Framework (14), the RE-AIM framework was applied across three stages of implementation: before adoption, during adoption, and during program implementation; herein called the scaling-out process. First, before the program was adopted, a mixed-methods design based on RE-AIM was used to capture perceptions of Extension health educators who could deliver the program in practice. Second, during program adoption, a pre- and post-training survey based on RE-AIM adoption was used to understand delivery personnel's adoption-decision making process. Finally, as the program was implemented, it was comprehensively evaluated through RE-AIM, including pre/post and cross-sectional measures, depending on outcome.
In addition to the planning and evaluation framework, an adapted participatory process model was used to guide this work. Figure 1 [adapted from Estabrooks et al. 15] details the contextual considerations that influenced each stage of the process. Notably, there were challenges in visually representing the iterative process of contextual considerations and responses. While the work here is presented in stages, it is important to note that these processes are continuous steps in order to ensure that the researchers, Extension health educators, and community partners engaged in a reflective and action-oriented manner. This study was approved by the University of Wyoming (stage 1) and Virginia Tech (stages 2 and 3) Institutional Review Boards.
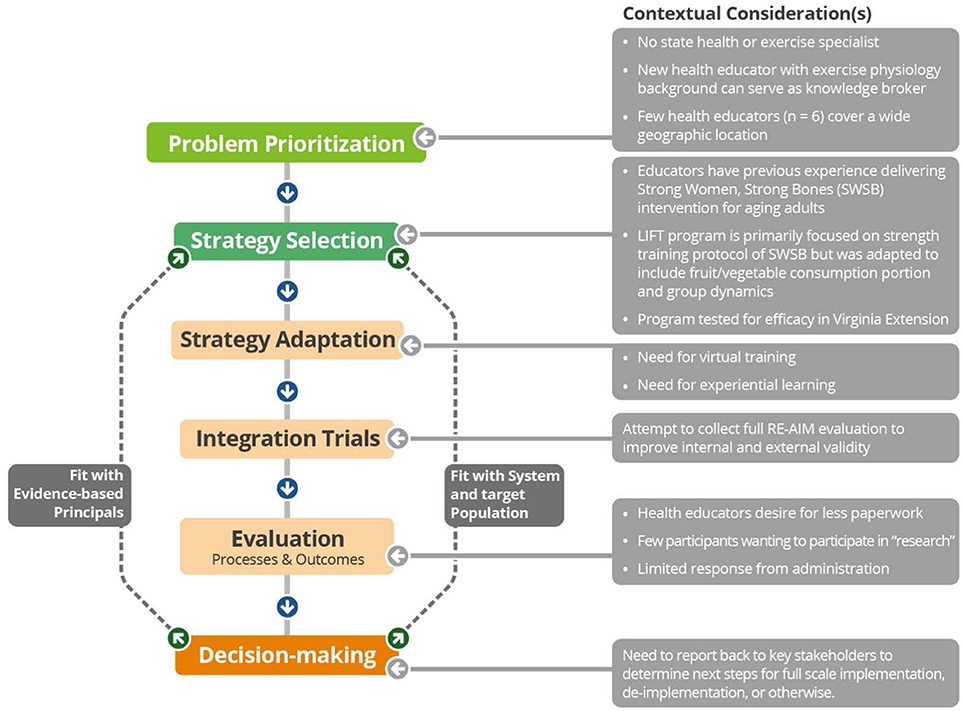
Figure 1. Integrated research-practice partnership model with contextual considerations leading to translational solutions.
Setting
Wyoming is a large, rural state with a small population (579,315). Ten Extension health educators cover the state's 23 counties and the Wind River Indian Reservation (by stage 2 of this research, only six health educators were employed in the state). These educators have a broad reach, interacting with over 40,000 participants per year. In Wyoming, there is no Extension health or physical activity specialist. When a new county-based Extension health educator (with a background in physical activity promotion and research) was hired by University of Wyoming Extension (UWE), the educator contacted the Virginia Cooperative Extension (VCE) Exercise Specialist to inquire about potential research partnerships. The new county-based Extension health educator served as a knowledge broker (i.e., an intermediary between researchers and stakeholders who facilitates knowledge transfer between these parties) (16). In alignment with the integrated research-practice process (IRPP) model, this setting and work identified that the lack of a health specialist and the small number of Extension health educators covering the state were problems to be addressed in order to successfully implement a physical activity intervention (see Figure 1: problem prioritization).
Program Development and Description
Lifelong Improvements through Fitness Together (LIFT) (17, 18) was adapted from two programs: Stay Strong Stay Healthy (19) and Activity for the Ages (20). LIFT combines the evidence-based behavioral strategies (goal setting, self-monitoring, and group dynamics) from Activity for the Ages with the evidence-based strength training protocol from Stay Strong Stay Healthy (18) and Strong Women, Strong Bones (also delivered by Extension professionals) (21). Since LIFT was adapted and tested specifically in Virginia, it was unknown whether the packaged LIFT program could be scaled-out to a new Extension state system (see Figure 1: strategy selection).
Stage 1: Before Adoption
Before offering a LIFT training, the exercise specialist and UWE knowledge broker conducted a pragmatic concurrent, transformative mixed-methods [i.e., equal emphasis on the quantitative and qualitative findings 22] study. To aid in replicability, the survey and interview guide can be found in Appendices A and B. Briefly, 67% of the eligible Extension health educators completed the online survey. Overall, participants were middle-aged Caucasian females; more demographic characteristics are displayed in Table 1. Health educators reported a range of comfort for delivering physical activity (from moderately to very comfortable). While none of the Extension health educators were currently delivering physical activity programs, three (50%) were thinking about offering a physical activity program (contemplation phase) (23). Finally, most of the survey respondents (n = 5) indicated that they would be interested in receiving training (either in person or via webinar) on delivery and evaluation of the LIFT program.
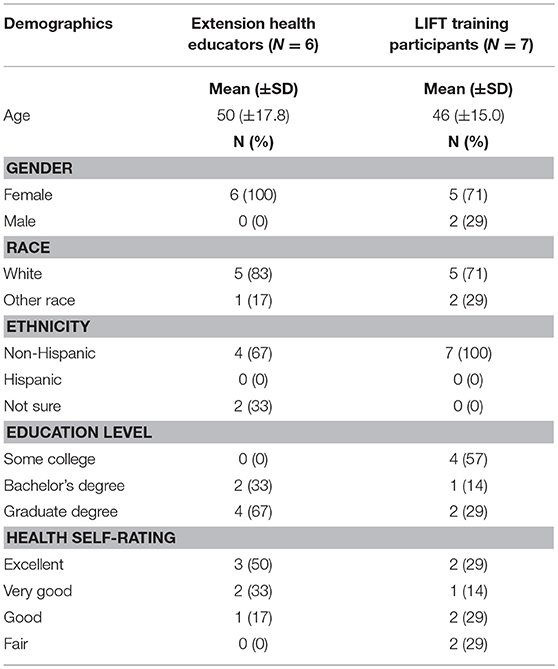
Table 1. Extension health educator characteristics compared to LIFT training participant characteristics.
Thematic coding of the two interviews yielded 349 meaning units reporting perceived barriers (n = 115 meaning units) and facilitators (n = 157) for delivering physical activity programs and types of programs delivered (n = 71). See Table 2 for coding, frequencies, and example meaning units. For barriers, interviewees expressed that their workload was too high to incorporate additional types of programming and their focus was on nutrition. They also mentioned that delivering the Strong Women, Strong Bones program (which was previously implemented through UWE) was too time consuming. As for facilitators, interviewees had positive perceptions of physical activity recommendations and benefits and had enjoyed the Strong Women, Strong Bones training. Community partners were mentioned as a source of physical activity program delivery. While a lack of facilities came up as a barrier, the presence of facilities (e.g., schools, fairgrounds, and walking paths) was also mentioned as a facilitator. Finally, regarding types of programs delivered, interviewees indicated that they were not currently delivering any physical activity programs. Rather, physical activity was promoted through incorporating topics, such as “sit less, move more” in other programming.
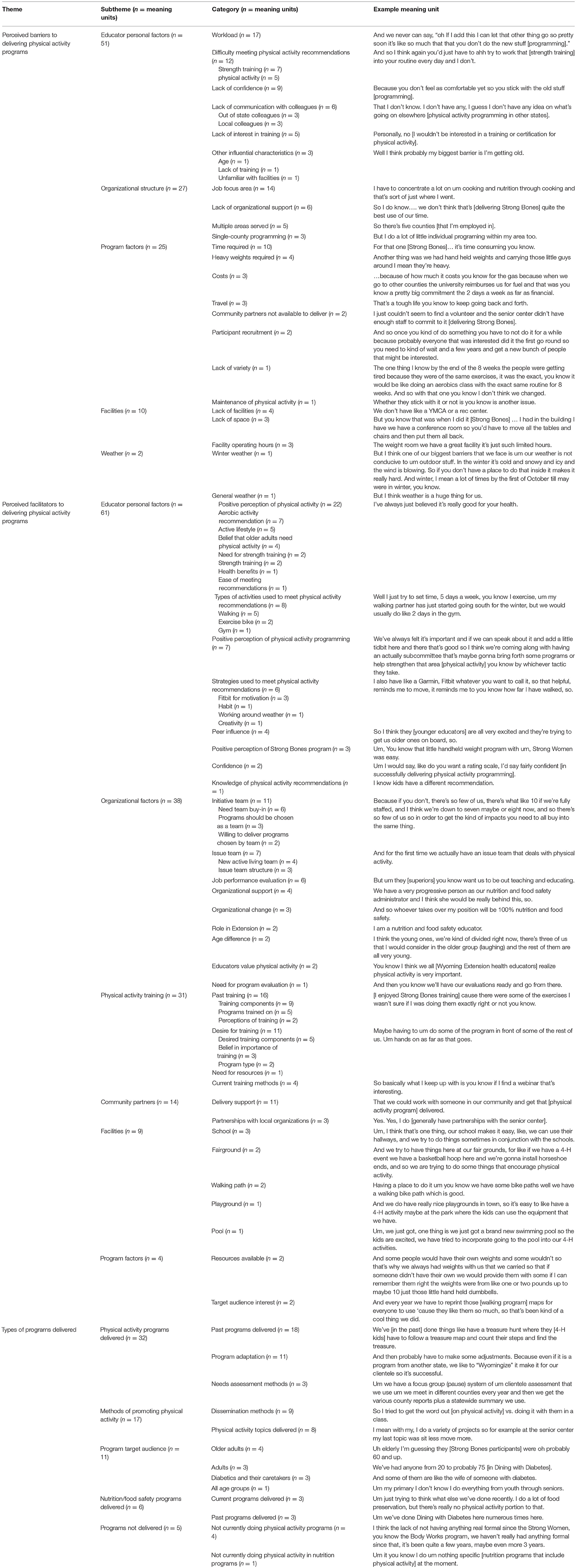
Table 2. Qualitative results of Extension health educators' perceptions of physical activity programs (n = 2 interviewees).
Stage 2: During Adoption (Training)
Based on the results of Stage 1, the research team decided that there was a need for a scalable training protocol (i.e., one that was feasible across the entire 97,818 square miles of Wyoming) designed to target Extension health educators who were less confident in delivering physical activity programs and include hands-on instruction and teach-back. LIFT training was created as a 4 h “live” virtual format based on evidence-based methods on training (24, 25), learner-centered teaching (26), and program adoption rates (27). Training included detailed descriptions of program principles and opportunities for experiential learning (e.g., practicing and receiving feedback on the exercises and fitness assessments). Additionally, the training was made available to Extension health educators' community partners (e.g., staff from senior centers and other health organizations) to promote a delivery model that would address the time requirement barrier; Extension health educators were encouraged to attend training with their community partners so they could offer support with implementation and evaluation. See Figure 1: strategy adaptation.
In alignment with Extension practices, pragmatic recruitment and feedback methods (e.g., listserv email invites and post-training surveys) were used. Nine participants completed the initial LIFT training in September 2017: the knowledge broker, one Extension health educator, and seven community partners (including one retired Extension health educator). Following this training, additional community partners expressed interest in the training, and the research team offered another training in December 2017 to four community partners.
Of the thirteen total training participants, nine (69%) completed surveys. Of the seven who completed pre-training surveys, trainees were predominantly middle-aged Caucasian females. All participants (100%) were very or completely confident in meeting physical activity recommendations. While all participants (100%) reported high physical activity levels through the International Physical Activity Questionnaire (IPAQ), only 57% reported meeting strength training guidelines. Pre-training, participants agreed that they intended to deliver LIFT and to include LIFT in a plan of work; mean values were both 4.00 (+0.707). The Wilcoxon signed-rank test showed that post-training surveys did not detect a statistically significant change in intent to deliver LIFT (Z = 0.000, p = 1.000) or inclusion of LIFT in a plan of work (Z = −0.447, p = 0.655).
The program characteristic that influences the adoption-decision making process of highest importance was “The program has been successful when tested in community settings” (mean rating of 4.00 = very important). While the majority of the factors (73%) had a mean rating between 3.00 and 3.99 (moderately important), four factors rated as only “somewhat important”: “I do not feel that the program is part of my job responsibility,” “I do not feel comfortable delivering the program,” “I am not physically active, so do not feel comfortable delivering a physical activity program,” and “I do not have the expertise that is needed to deliver the program.” By February 2018 (5 months after the first training and 2 months after the second), three LIFT programs were being delivered through UWE, and the comprehensive evaluation was initiated. Due to this low initial implementation rate, a survey for trainees who both did and did not implement the program was added to the measures for adoption.
Stage 3: During Implementation
Participants and Recruitment
The final step in this research was to evaluate both the individual-level impact and the system-level delivery of LIFT through the RE-AIM framework. The evaluation included three levels of respondents in an attempt to collect data on all RE-AIM dimensions: reach and effectiveness (LIFT participants), adoption and implementation (delivery personnel, i.e., both Extension health educators and community partners), and system-level maintenance (UWE administrators). LIFT participants were recruited through senior centers (including participants in Strong Bones programs), newspaper articles, flyers, and word of mouth. Extension health educators and community partners were contacted via email after the LIFT training to complete a brief online survey. Extension administrators (N = 3) were also contacted via email to complete a brief online survey.
Data Collection and Analysis
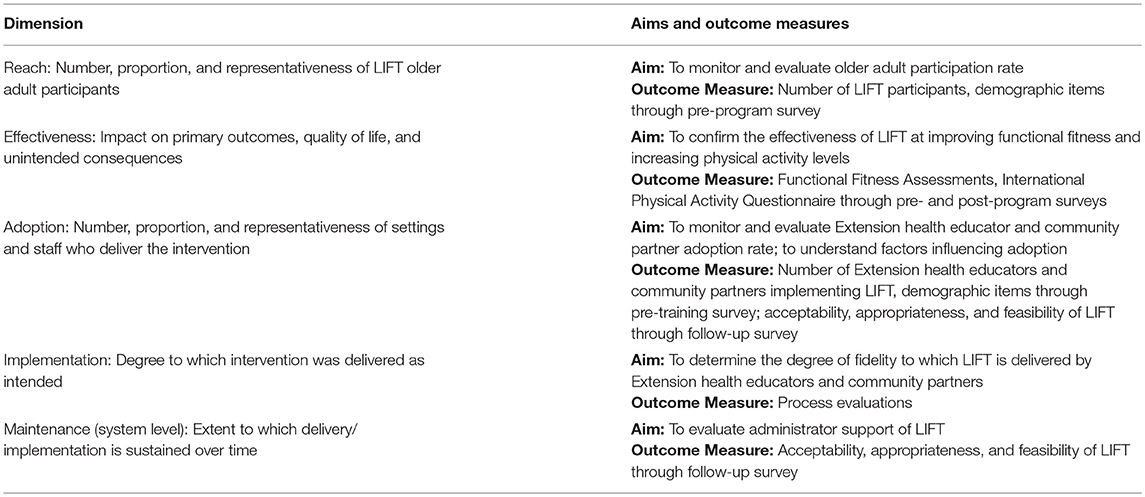
Data were collected on all RE-AIM dimensions except for individual-level maintenance, which was outside the scope of this work (see Figure 1: integration trials). Measures for each dimension were as follows (see Table 3 for detailed aims and outcome measures):
Reach
LIFT participants completed baseline surveys including demographic items used to calculate reach (proportion and representativeness).
Effectiveness
The pre- and post-program surveys included IPAQ items to assess whether participants were meeting physical activity recommendations (28). A validated seven-item test associated with performing everyday activities independently (29) was completed at baseline and post-program, as an additional outcome of LIFT is improving functional fitness.
Adoption
The primary adoption indicator was the total number and representativeness of those trained on LIFT program (including both Extension health educators and community partners). In addition, all those eligible to deliver the LIFT program were asked to complete a survey assessing: (1) acceptability, appropriateness, and feasibility (30) of implementing LIFT (on a 5-point Likert scale; 1-completely disagree, 5-completely agree), and (2) their current stage of change category (23) based on the 6-point scale of 1- “I am not considering delivering LIFT in my county at all” to 6- “I have been delivering LIFT for 6 months of more.” Demographic items were not included to create a short survey that decreased respondent burden.
Implementation
This was assessed through process evaluations designed for delivery personnel to self-report the extent to which the program was delivered as intended and capture adaptations made during program delivery. The process evaluations contained five categories: warm-up activity, group-dynamics strategy, exercises, cool down, and overall program delivery.
Maintenance
As a proxy measures for system-level maintenance, administrator perceptions were sought related to: (1) acceptability, appropriateness, and feasibility (30) of LIFT; (2) the importance of RE-AIM factors for LIFT [e.g., “The program has potential to attract/recruit a group of participants that is representative of the residents of Wyoming (reach); LIFT has been previously tested in community settings (effectiveness): 1-not at all important, 5-very important], and (3) whether they supported educators in delivering LIFT (yes or no with reasons why or why not). Demographic items were also not included in this survey.
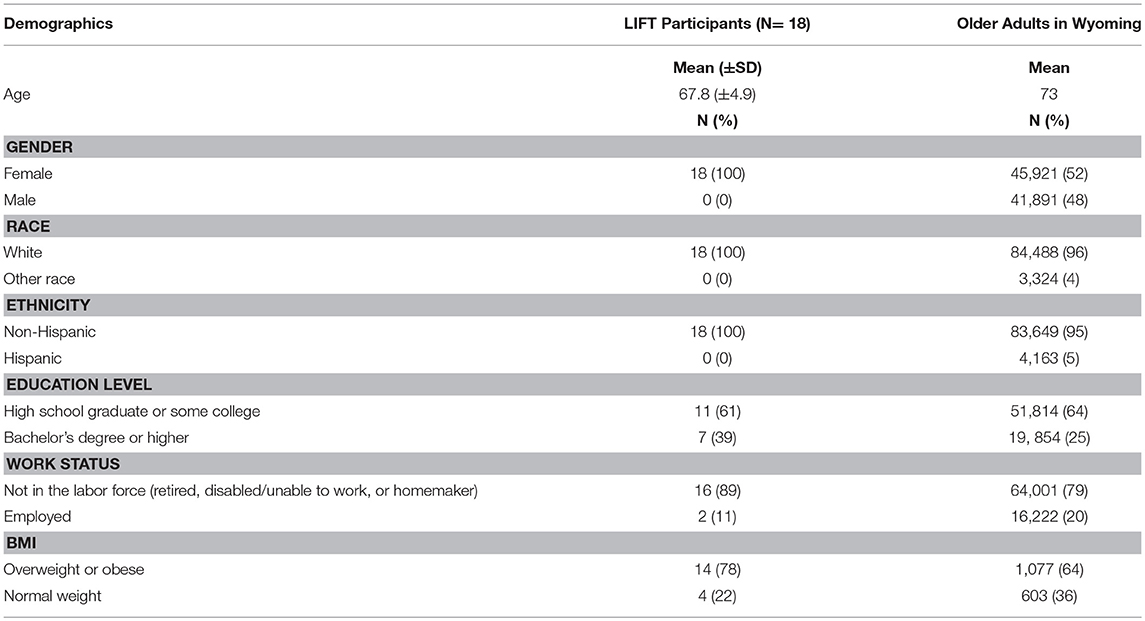
Means and standard deviations of continuous variables and frequencies and proportions of nominal variables were calculated for the overall sample. Representativeness was calculated by comparing demographics (age, gender, race, ethnicity, education level, and work status) of LIFT participants to all older adults (age 65 and older) in Wyoming (city or county level census data was not available) (31). As raw data was not available for education level or work status, frequencies were calculated by using census data percentages and totals. Representativeness of BMI was calculated by comparing LIFT participants to the sub-sample of older adults in Wyoming (age 65 and older) who were selected and responded to the Behavioral Risk Factor Surveillance System (BRFSS) survey. A one-sample t-test was used to compare mean age; Fisher's exact test was used to compare categorical variables due to the small sample size.
Results
Reach
Forty-eight participants attended the LIFT classes. However, only 37 individuals agreed to the research portion of this work. Of the 37 who agreed to be research participants, 18 completed pre-program surveys. These participants had a mean (±SD) age of 67.8 (±4.9) years, were predominantly retired (78%), and were Caucasian females (100%). Participants had a mean (±SD) BMI of 29.9 (±7.0) with seven (39%) classified as obese, seven (39%) classified as overweight, and four (22%) classified as normal weight. For each of the three delivery locations, proportion of LIFT participants was calculated as 17 out of 1,480 adults age 65 or older (1%) in Lander, 12 out of 35 (34%) in Pavillion, and 8 out of 281 (3%) in Guernsey. When comparing the representativeness of LIFT participants to older adults in Wyoming, there were no significant differences in terms of race (p = 1.000), ethnicity (p = 1.000), employment status (p = 1.000), education level (p = 0.297), and BMI (p = 0.324). There was a significant difference in age and gender: LIFT participants were younger (t = −4.385, p = 0.000) and more likely to be female (p = 0.000) (see Table 4).
Effectiveness
Of the 37 LIFT research participants, 10 completed both pre- and post-program functional fitness assessments. There was a statistically significant increase in the 30 s chair stand test (t = −2.673, p = 0.028) and no significant difference in any of the other tests (balance station, 30 s arm curl, 2 min step test, chair sit and reach, back scratch, and eight food up and go). As only five participants completed both pre- and post-program surveys, changes in physical activity levels were not included in this report.
Adoption
Proportion of delivery agents was calculated for both Extension health educators and community partners. Of the six Extension health educators employed at the time who were invited to the training, one delivered LIFT for an adoption rate of 17%. Of the two Extension health educators who attended training, one delivered LIFT for an adoption rate of 50%. However, the other Extension health educator who attended training indicated through the follow-up email 2 months post-training that she was planning on delivering LIFT but had not yet scheduled a session; she also recruited community partners to attend the second LIFT training and assisted one of the community partners with completing evaluations when she delivered the program.
Of the eleven community partners who attended training, two delivered LIFT for an adoption rate of 18%. Representativeness of those who delivered LIFT compared to those who attended the training but did not deliver LIFT was not calculated, as demographic data from the pre-training survey was only available for one of the educators who delivered LIFT. Demographics of those invited to attend LIFT training (the six Extension health educators) were compared to the demographics of those who attended LIFT training (both Extension health educators and community partners) and completed the pre-training survey (see Table 1). Due to the small sample sizes, representativeness was not calculated.
One of the 13 training attendees and none of the four Extension health educators who did not attend training completed follow-up surveys. Due to the low response rate, survey results are not included.
Implementation
One of the two eligible delivery personnel completed process evaluations. One other educator completed the process evaluations, but these data were not eligible for inclusion in analysis as she was also the knowledge broker (i.e., a research team member with the potential to bias responses) (32). Results from the one educator indicated that the program was overall delivered as intended 100% of the time, although adaptations were made to program components: the warm-up was delivered with 63% fidelity, group dynamics-based activities 75%, strength training exercises 100%, and cool-down 69%. Due to the small sample size, these data should be interpreted with caution.
Maintenance
One of the three administrators completed the surveys; due to the low response rate, administrator survey results are also not included.
Discussion
Results of this work indicated initial struggles in scaling-out a previously tested Extension EBI to Wyoming Extension. All three stages were equally important in capturing the challenges and facilitators of the LIFT EBI scale-out; however, a lack of compliance with data completion (see Figure 1: evaluation processes and outcomes) highlights challenges of a pragmatic approach to data collection (e.g., without large funds for systematic evaluation). This is notable as the researchers were also from within the Extension system, and therefore, aligned evaluation with standards of practice. Therefore, translational solutions (Figure 1) are yet to be determined. However, there were notable observations and implications, by stage, to be shared.
Stage 1: Before Adoption
In order to improve physical activity program adoption rates among Extension health educators, system-wide changes are needed. While it appears that the UWE organizational structure supports physical activity programming (e.g., interviewees mentioned a newly developed Active Living issue team tasked with choosing physical activity programs to deliver), educators face barriers to adopting these programs, including role clarity, traditional delivery models, and organizational culture.
Physical activity is not explicitly included as a focus area of Extension health educators' work. Including “physical activity promotion” in Extension health educators' job descriptions and changing position titles to be more inclusive of physical activity could help educators prioritize physical activity programming and de-implement other work duties that are not evidence-based (33). In addition, physical activity programming is fairly new as an Extension target area and Extension educators (in both health and other disciplines) not aware of this change may not support physical activity programming among their colleagues. Interviewees also mentioned a lack of communication with colleagues, both those on their initiative team as well as educators in neighboring states, which makes program dissemination difficult (34). Future work should investigate the usefulness of a dissemination network of Extension state specialists that assists educators in staying informed of evidence-based physical activity promotion efforts taking place nationwide (34).
In addition to role clarity within the system, Extension professionals need guidance on how to leverage volunteers and community members to engage participants across a disperse region. That is, novel approaches for program delivery may be necessary to increase the penetration of an intervention across a state system, particularly a large rural one. For example, interview respondents mentioned time required for program delivery as a barrier to Strong Women, Strong Bones (and LIFT requires a similar time commitment); adaptations to the delivery model may encourage adoption. They also mentioned a lack of funds to cover fuel to reach geographically disparate communities. A train-the-trainer delivery model may help Extension health educators to adopt the program and then turn it over to community partners, as has been done by Washburn and colleagues for their version of LIFT (35). To address lack of time as a barrier, Extension health educators also need training on evidence-based programming; this training could encourage them to adopt existing structured, evidence-based programs instead of developing their own programming (36). Future studies should explore the effects on program adoption rates when these system-level changes are made.
Finally, the culture of the organization and the state can also affect physical activity program adoption. Wyoming is a politically conservative state with an individualistic and independent culture. This culture can impede health promotion efforts, as observed in the tobacco control efforts of the 2000s: “We are independent, we're rugged, we'll smoke if we want to, and do not want any government folks trying to tell us how to live healthier and live longer” (37). This belief can be a barrier to adoption of any program with health behavior change as an outcome. To encourage adoption of physical activity interventions, it may be necessary to shift this mindset within the system.
Stage 2: During Adoption
Although perceptions of the LIFT training were positive, participating in training did not change attendees' predictors of implementation, stage of change, or positive intent to deliver both the LIFT program and physical activity programming in general. This may be because those who attended already planned on delivering LIFT (e.g., intent to incorporate physical activity into existing programming and intent to deliver LIFT both had a mean rating of 4 (agree) both before and after training). As these are the top predictors of program implementation, it was expected that program implementation rates following training would be high. However, only 2 months had passed since the second LIFT training, so it is possible that those who attended training will deliver LIFT once they have determined a location, community partners, etc., as intent to deliver LIFT was high post-training. The optimal length of time post-training to assess implementation status is unknown; other studies of Extension-delivery physical activity programs have assessed delivery status after 1 year (Ramalingam et al., in preparation) or annually for 5 years (38). Overall, through this iterative work, attempts were made to include perceptions of delivery agents to “begin with the end in mind (39)”; however, in this study, these efforts to align the intervention with the pull of the system (40) did not lead to strong adoption or implementation. More work is needed to determine what factors would lead to higher implementation rates.
More work is needed to understand the adoption-implementation gap among community partners that occurred following the LIFT training. Training attendees had positive perceptions of the training and intentions to deliver LIFT post-training. Without responses to the follow-up survey, it is difficult to understand perceptions of the program or implementation barriers that occurred. Future research on system-level changes to promote physical activity programming through Extension, training on evidence-based programming for Extension health educators, physical activity program delivery methods that decrease educator time commitment, and barriers to community partner program implementation are needed to address low adoption and implementation rates.
Stage 3: During Implementation
Extension is an open-access entity that values pragmatic outcomes; stringent collection of empirical data is more novel to this system and its personnel. Therefore, the magnitude of effect and fit of LIFT within the system is yet to be determined. Furthermore, it was difficult to determine if the program was implemented with fidelity; changes are needed to encourage or incentivize collecting these data from delivery personnel (41, 42). While self-report process evaluations seem easy and manageable, observations may be necessary to monitor program delivery. However, these observations require intense resources (travel, time), so the longevity of this approach may not be feasible. Future work is needed to determine how to train for and monitor high quality delivery.
Although effectiveness, adoption, and implementation data were challenging to collect, there were positive outcomes in terms of reach. First, LIFT demonstrated a strong reach among eligible older adults, particularly in small communities (e.g., 34% of older adults (12 participants) from one community participated). In terms of representativeness, LIFT participants were more likely to be female; however, this is also not surprising as the Wyoming Extension system had previously delivered Strong Women, Strong Bones (21). The program was eventually called “Strong Bones” to be more inclusive but more females participated. One advantage of LIFT is that it is available and promoted to both men and women, similar to the Stay Strong, Stay Healthy program of Extension in Missouri and, more recently, Kansas (19, 43). Although previous research demonstrated that older adults prefer to exercise with other older adults (44, 45), new research shows that gender-segregated classes do not produce better adherence or physical activity outcomes when compared to classes of similar age but mixed-gender (46). From a practical perspective, some older adults may prefer gender segregated classes (44), but LIFT will continue to be offered to all aging adults due to its open-access policy (7).
Limitations
The most prominent limitation of this work is the small sample size for empirical data. However, in pragmatic settings large sample sizes are not always available; the purpose of this work was to report process and outcome data in order to aid in replicability and understanding the process of scaling an intervention that was adapted specifically for Extension. Due to low survey response rates, perceptions of LIFT that influence adoption and system level maintenance were not captured. These data may have offered insight into reasons for LIFT not being adopted and implemented (e.g., low perceived acceptability, appropriateness, or feasibility among community partners, Extension health educators, or UWE administrators) and predicted institutionalization of the program. Future work should consider other methods of collecting data to determine perceptions of LIFT and potentially adapt the program to improve adoption and implementation rates. The sample sizes for each portion of this study were small as they were limited by the organization structure of UWE (i.e., only three administrators and six Extension health educators serve the entire state). However, these educators have a large reach, as they cover the entire state and are tasked with providing community-based education to all Wyomingites.
Finally, strategies to partner with delivery personnel could have been better used to enhance buy-in and ensure a good fit between LIFT and UWE as a delivery system (47). The research team did not fully employ an IRPP in UWE, as the LIFT program was developed through an IRPP in VCE. As there were challenges with translating LIFT from Virginia to Wyoming, in the future employing a new, state-specific IRPP is recommended to address potential program adaptations and enhance program sustainability.
This is the first study to follow the scaling-out of an Extension intervention for Extension professionals by Extension professionals that did not include place-based adaptations. For example, Sequin et al. used Extension as a dissemination model for the Strong Women, Strong Bones intervention but were not Extension professionals themselves (48). In another example, a statewide walking program was translated to a new state but the state made place-based adaptations before launching the intervention (1, 49). Reports like this one are needed to show the challenges, successes, and next steps to translating evidence-based interventions across state lines within the national system as well as to other community-based entities that partner with Extension.
Conclusion
Applying a planning and evaluation framework (e.g., RE-AIM) has the potential to improve transparency and translation of best practices into community settings. However, many settings do not have the resources to capture these iterative, pragmatic data. The results of this study suggest that system-level changes are needed to increase physical activity program adoption rates among Extension health educators, reduce system-level barriers (e.g., role clarity, lack of time or transportation funds), and leverage partnerships to ensure programs can reach those most in need of intervention. Collecting ongoing effectiveness data will be a challenge, and pragmatic ways to indicate a public health impact need to be developed (and match systems' capacity, interest, and value). These improvements in community-based and community-driven data collection may improve reach, effectiveness, adoption, implementation, and maintenance of interventions within Extension.
Availability of Data and Materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions
LB and SH conceived of the study, and participated in its design and coordination. LB led the manuscript preparation. NR contributed to data collection and analysis. TS contributed to data analysis. All authors read, contributed to, and approved the final manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2018.00357/full#supplementary-material
References
1. Harden S, Johnson SB, Almeida F, Estabrooks P. Improving physical activity program adoption using integrated research-practice partnerships: an effectiveness-implementation trial. Transl Behav Med. (2017) 7:28–38. doi: 10.1007/s13142-015-0380-6
2. United, States Department of Agriculture,. Civil Rights Compliance Review Guide: Extension Programs. Washington, DC; n.d. Available online at: https://agsci.psu.edu/diversity/civil-rights-compliance-training/civil-rights-compliance-review-guide-extension-programs
3. United States Department of Agriculture,. The Farm Bill 2015. Washington, DC (2015). Available online at: https://nifa.usda.gov/farm-bill
4. United States Department of Agriculture,. NIFA Strategic Plan FY2014–FY2018 2015. Washington, DC (2015). Available online at: https://nifa.usda.gov/resource/nifa-strategic-plan-fy2014-fy2018
5. Braun B, Bruns K, Cronk L, Kirk Fox L, Koukel S, Le Menestrel S, et al. Cooperative Extension's National Framework for Health and Wellness. Washington, DC: United States Department of Agriculture (2014).
6. Aarons G, Sklar M, Bustanski B, Benbow N, Hendricks Brown C. “Scaling-out” evidence-based interventions to new populations or new health care delivery systems. Implement Sci. (2017) 12:111. doi: 10.1186/s13012-017-0640-6
7. Balis L, Strayer T, Ramalingam N, Wilson M, Harden S. Open-access physical activity programs for older adults: a pragmatic and systematic review. Gerontologist5 (2018) gnx195. doi: 10.1093/geront/gnx195
8. Whitelaw N. System change and organizational capacity for evidence-based practices: lessons from the field. Generations J Am Soc Aging (2010) 34:43–50.
9. Wilcox S, Dowda M, Leviton LC, Bartlett-Prescott J, Bazzarre T, Campbell-Voytal K, et al. Active for life: final results from the translation of two physical activity programs. Am J Prev Med. (2008) 35:340–51. doi: 10.1016/j.amepre.2008.07.001
10. Glasgow R. What does it mean to be pragmatic? Pragmatic methods, measures, and models to facilitate research translation. Health Educ Behav. (2013) 40:257–65. doi: 10.1177/1090198113486805
11. Glasgow R, Estabrooks P. Pragmatic applications of RE-AIM for health care initiatives in community and clinical settings. Prev Chron Dis. (2018) 15:1–7. doi: 10.5888/pcd15.170271
12. Glasgow R, Vogt T, Boles S. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health (1999) 9:1322–7.
13. Glasgow RE, Nelson CC, Strycker LA, King DK. Using RE-AIM metrics to evaluate diabetes self-management support interventions. Am J Prev Med. (2006) 30:67–73. doi: 10.1016/j.amepre.2005.08.037
14. Harden S, Smith M, Smith-Ray R, Ory M, Estabrooks P, Glasgow R. RE-AIM in clinical, community, and corporate settings: perspectives, strategies, and recommendations to enhance public health impact. Front Public Health (2018) 6:71. doi: 10.3389/fpubh.2018.00071
15. Estabrooks P, Harden S, Almeida F, Hill J, Johnson S, Greenaward M. Translating evidence-based principles into sustained programs through integrated research practice partnerships. Exerc Sport Sci Rev. (forth coming).
16. Bornbaum C, Kornas K, Peirson L, Rosella L. Exploring the function and effectiveness of knowledge brokers as facilitators of knowledge translation in health-related settings: a systematic review and thematic analysis. Implement Sci. (2015) 10:162. doi: 10.1186/s13012-015-0351-9
17. Wilson ML, Strayer T, Davis R, Harden SM. Informed adaptations of a strength-training program through a research-practice partnership. Front Public Health (2018) 6:58. doi: 10.3389/fpubh.2018.00058
18. Wilson ML, Strayer III T, Davis R, Harden SM. Use of an integrated research-practice partnership to improve outcomes of a community-based strength-training intervention for older adults: reach and effect of lifelong improvements through fitness together (LIFT). Int J Environ Res Public Health (2018) 15:237. doi: 10.3390/ijerph15020237
19. Ball S, Gammon R, Kelly P, Cheng A-L, Chertoff K, Kaume L, et al. Outcomes of stay strong, stay healthy in community settings. J Aging Health (2013) 25:1338–97. doi: 10.1177/0898264313507318
20. Estabrooks P, Fox E, Doerksen S, Bradshaw M, King A. Participatory research to promote physical activity at congregate-meal sites. J Aging Phys Act. (2005) 13:121–44. doi: 10.1123/japa.13.2.121
22. Creswell J, Plano Clark V. Designing and Conducting Mixed Methods Research. Los Angeles, CA: Sage (2011).
23. Prochaska J, DiClemente C. The Transtheoretical Approach: Crossing Traditional Boundaries of Change. Homewood, IL: Dorsey Press (1984).
24. Proctor E, Landsverk J, Baumann A, Mittman B, Aarons G, Brownson R, et al. The implementation research institute: training mental health implementation researchers in the United States. Implement Sci. (2013) 8:105.doi: 10.1186/1748-5908-8-105
25. Nebeker C, Lopez-Arenas A. Building research integrity and capacity (BRIC): an educational initiative to increase research literacy among community health workers and promotores. J Microbiol Biol Educ. (2016) 17:41–5. doi: 10.1128/jmbe.v17i1.1020
26. Weimar M. Learner-Centered Teaching: Five Key Changes to Practice. San Francisco, CA: Jossey-Bass (2013).
27. Salas E, Tannenbaum S, Kraiger K, Smith-Jentsch K. The science of training and development in organizations: what matters in practice. Psychol Sci Public Interest (2012) 13:74–101. doi: 10.1177/1529100612436661
28. Craig C, Marshall A, Sjostrom M, Bauman A, Booth M, Ainsworth B, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. (2003) 35:1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB
29. Rikli R, Jones CJ. Development and validation of a functional fitness test for community-residing older adults. J Aging Phys Act. (1999) 7:129–61.
30. Weiner B, Lewis C, Stanick C, Powell B, Dorsey C, Clary A, et al. Psychometric assessment of three newly developed implementation outcome measures. Implement Sci. (2017) 12:108. doi: 10.1186/s13012-017-0635-3
31. United States Census Bureau,. American Fact Finder 2016. Washington, DC (2016). Available online at: https://factfinder.census.gov/faces/nav/jsf/pages/community_facts.xhtml?src=bkmk#
32. McCambridge J, Witton J, Elbourne D. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol. (2014) 67:267–77. doi: 10.1016/j.jclinepi.2013.08.015
33. Harden S, Lindsay A, Everette A, Gunter K. Systematic review of physical activity objectives in extension strategic plans: findings and implications for improved public health impact. J Ext. (2016) 54.
34. Strayer III T, Kennedy L, Balis L, Ramalingam N, Wilson M, Harden SM. Cooperative extension gets moving, but how? Exploration of extension health educators' sources and channels for information-seeking practices. BMC Health Serv Res. (forth coming).
35. Washburn L, Cornell C, Phillips M, Felix H, Traywick L. Strength training in community settings: impact of lay leaders on program access and sustainability for rural older adults. J Phys Act Health (2014) 11:1408–14. doi: 10.1123/jpah.2013-0007
36. Peña-Purcell N, Bowen E, Zoumenou V, Schuster E, Boggess M, Manore M, et al. Extension professional's strengths and needs related to nutrition and health programs. J Ext. (2012) 50.
37. The Center for Tobacco Policy Research. The Wyoming Profile: A Review of Wyoming's Tobacco Prevention & Control Program. St. Louis, MO: Saint Louis University Prevention Research Center (2003).
38. Estabrooks PA, Bradshaw M, Dzewaltowski DA, Smith-Ray RL. Determining the impact of Walk Kansas: applying a team-building approach to community physical activity promotion. Ann Behav Med. (2008) 36:1–12. doi: 10.1007/s12160-008-9040-0
39. Klesges L, Estabrooks P, Dzewaltowski D, Bull S, Glasgow R. Beginning with the application in mind: designing and planning health behavior change interventions to enhance dissemination. Ann Behav Med. (2005) 29:66–75. doi: 10.1207/s15324796abm2902s_10
40. Lavis JN, Lomas J, Hamid M, Sewankambo NK. Assessing country-level efforts to link research to action. Bull World Health Organ. (2006) 84:620–8. (41): doi: 10.2471/BLT.06.030312
41. Ahn S, Smith ML, Altpeter M, Belza B, Post L, Ory MG. Methods for streamlining intervention fidelity checklists: an example from the chronic disease self-management program. Front Public Health (2015) 2:294. doi: 10.3389/fpubh.2014.00294
42. Lambert JD, Greaves CJ, Farrand P, Cross R, Haase AM, Taylor AH. Assessment of fidelity in individual level behaviour change interventions promoting physical activity among adults: a systematic review. BMC Public Health (2017) 17:765. doi: 10.1186/s12889-017-4778-6
43. K-State Research Extension,. Stay Strong, Stay Healthy. Manhattan, KS: Kansas State University (2018). Available online at: https://www.k-state.edu/staystrong/
44. Beauchamp M, Carron A, McCutcheon S, Harper O. Older adults' preferences for exercising alone versus in groups: considering contextual congruence. Ann Behav Med. (2007) 33:200–6. doi: 10.1080/08836610701310037
45. Dunlop W, Beauchamp M. Birds of a feather stay active together: a case study of an all-male older adult exercise program. J Aging Phys Act. (2013) 21:222–32. doi: 10.1123/japa.21.2.222
46. Beauchamp M, Dunlop W, Ruissen G, Estabrooks P, Harden S, Wolf S, et al. GrOup based physical Activity for oLder adults (GOAL) randomized controlled trial: exercise adherence outcomes. Heath Psychol. (forthcoming).
47. Israel B, Eng E, Schulz A, Parker E. Methods in Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass (2005).
48. Seguin RA, Heidkamp-Young E, Kuder J, Nelson ME. Improved physical fitness among older female participants in a nationally disseminated, community-based exercise program. Health Educ Behav. (2012) 39:183–90. doi: 10.1177/1090198111426768
Keywords: RE-AIM, physical activity, cooperative Extension system, implementation science, translation
Citation: Balis LE, Strayer TE III, Ramalingam N and Harden SM (2018) Beginning With the End in Mind: Contextual Considerations for Scaling-Out a Community-Based Intervention. Front. Public Health 6:357. doi: 10.3389/fpubh.2018.00357
Received: 28 August 2018; Accepted: 21 November 2018;
Published: 10 December 2018.
Edited by:
Melody Goodman, New York University, United StatesReviewed by:
Cassandra Arroyo, Barnes-Jewish Hospital, United StatesAnna J. DeRuyter, Washington University in St. Louis, United States
Deborah Paone, Independent Researcher, Minneapolis, United States
Copyright © 2018 Balis, Strayer, Ramalingam and Harden. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Laura E. Balis, bGJhbGlzQHV3eW8uZWR1
 Laura E. Balis
Laura E. Balis Thomas E. Strayer III
Thomas E. Strayer III NithyaPriya Ramalingam
NithyaPriya Ramalingam Samantha M. Harden
Samantha M. Harden