- 1Public Service Research Group, University of New South Wales, Sydney, NSW, Australia
- 2Centre for Primary Health Care and Equity, University of New South Wales, Sydney, NSW, Australia
- 3South Eastern Sydney Local Health District, New South Wales Department of Health, Sydney, NSW, Australia
Background: Waterpipe tobacco smoking is a traditional method of tobacco use, especially in the Eastern Mediterranean Region (EMR), but its prevalence is growing worldwide, especially among young people. Although often perceived as less harmful than other methods of tobacco use because the smoke passes through water, accumulating evidence shows harmful effects and that some smokers become addicted. Interventions that deglamourise and denormalise use have been recommended but little is known about the range and impact of different health prevention and promotion interventions.
Methods: A scoping review of literature was undertaken to explore the breadth of literature and assess the range and impact of community based health promotion interventions for waterpipe smoking. Searches were conducted in Medline, Embase, CINAHL, Psychinfo, and the Cochrane database of systematic reviews. Interventions were classified using a health promotion framework and data extracted on the aspects of prevention/promotion addressed; key strategies employed, evidence of effectiveness or impact on behavior change as well as barriers to implementation and perceived success factors.
Results: Ten studies were included in the review. They include brief interventions to increase quit rates; community campaigns to raise awareness and increase knowledge; web based health education and skill development to increase perceived risks and intention to quit; as well as studies that evaluated product labeling and opportunities for policy interventions to create healthy environments.
Conclusions: The evidence base is small but growing. Brief interventions for waterpipe users, community campaigns, and web based tailored information can modify perceptions of addiction and increase intentions to quit. Product labeling may be an effective policy tool to curb waterpipe smoking. A range of policy interventions have been identified but not evaluated.
Background
Waterpipe smoking is a traditional method of tobacco use, practiced originally in the Middle East but becoming increasingly popular worldwide, particularly among young people and women (1, 2). Recent estimates of the rapid increase in waterpipe use across the world suggest a very high prevalence among school and university students in Middle Eastern countries, as well as among groups of Middle Eastern descent in western countries including the USA and Australia (3). Although often perceived as less harmful than other types of tobacco use because the smoke passes through water, there is growing evidence of health risks and harm associated with toxicity, associations with lung cancer, periodontal disease and other conditions, as well as the development of dependence in some users (2–4).
Systematic reviews of interventions addressing waterpipe use have largely focused on behavioral and treatment interventions with very limited attention to health promotion and prevention (5, 6). Despite growing consensus that waterpipe smoking is a public health issue and calls from the World Health Organization for action to intervene (7) little is known about how best to deliver health promotion interventions that can increase awareness of potential harm and improve community capacity for action. A recent review of interventions for waterpipe smoking cessation (5) concluded that evidence-based information about waterpipes' addictive and harmful properties should be developed and disseminated in order to deglamourize and denormalize its use. Ward et al. (8) have also argued that programs need to address the unique features of waterpipe smoking e.g., its cultural significance, social uses, and intermittent use pattern as well as the characteristics and motivations of users who want to quit.
We conducted a scoping review to identify and describe the range of literature on health promotion initiatives and to assess evidence of impact and the key mechanisms, barriers and enablers to implementation. Specific questions were:
• What types of community based health promotion interventions for waterpipe smoking have been trialed?
• What aspects of prevention do they seek to address and what mechanisms for change are employed?
• Which of these have been shown to be effective, for which population groups/communities and in which contexts?
Methods
The review follows the scoping methodology outlined by Arksey and O'Malley (9). Consistent with this methodology, the review was conducted in 5 steps. Step 1 involved developing the research questions; Step 2 identifying relevant studies; Step 3 selecting studies; Step 4 charting data; and Step 5 collating, summarizing and reporting results. A project team consisting of health promotion practitioners, policy makers and researchers was established to develop the research question and oversee the study.
Search Strategy
A comprehensive search strategy and set of search terms is contained in Supplementary File 1. Search terms included “waterpipe” or “narghile” or “arghile” or “shisha” or “goza” or “narkeela” or “hookah” or “hubble bubble” AND a combination of “health promotion” or “health intervention” or “health education” or “social marketing” or “health knowledge” (see Supplementary File 1). Searches were conducted in April 2016 in Medline, Embase, CINAHL, Psychinfo and the Cochrane database of systematic reviews. Hand searching of key journals and citations from key papers was also conducted.
Inclusion Criteria for Study Selection
Studies of health promotion interventions, using the WHO health promotion definition (10) (http://www.who.int/topics/health_promotion/en/) were included. Studies that focused on treatment interventions, attitudes and prevalence, studies not in English, and gray literature were excluded.
Charting Data
Two authors (RK, KG) extracted data. Details of the study population and context, aims and methods, intervention strategies, mechanisms if available, key success factors and barriers to implementation, and impacts were recorded. Studies were classified across the spectrum of health promotion (11) see the Northern Territory Health Promotion Framework) from medical approaches such as brief intervention that focus on individuals, through behavioral approaches that aim to improve knowledge and skills, to socio-environmental activities that focus on creating healthy communities, settings, and environments. Formal quality assessment was not conducted, consistent with the scoping review methodology and because of the small numbers of papers and heterogeneity of topics and study types.
Results
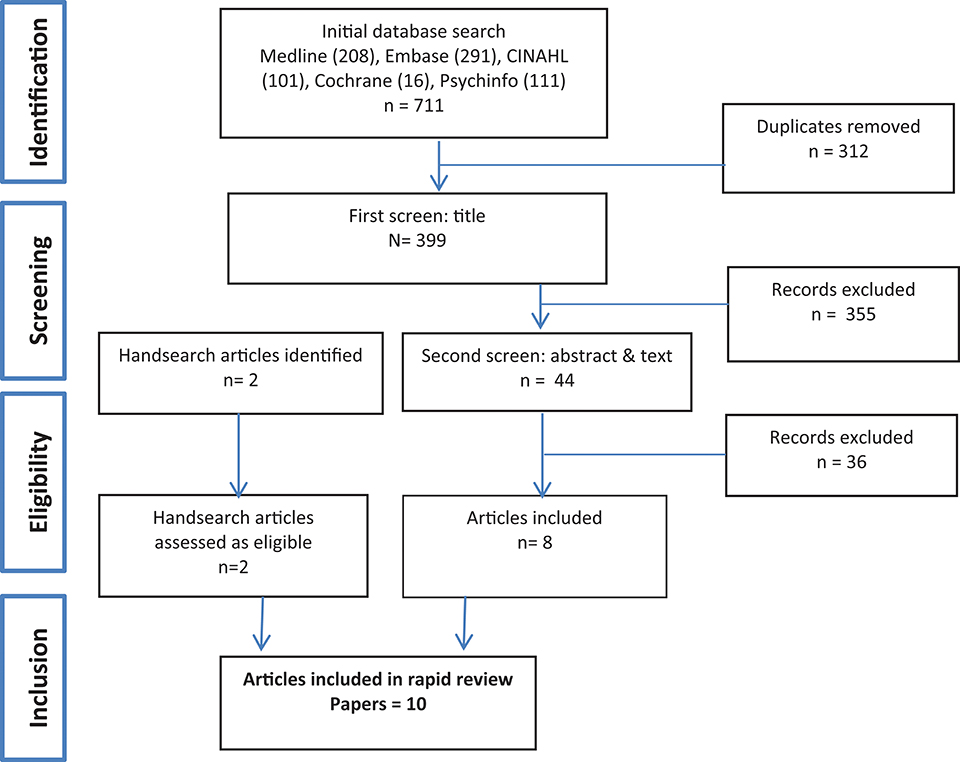
The initial search identified 711 references, of which 312 duplicates were removed, leaving 399 papers that were subject to first screen title review (Figure 1). A further 388 papers that did not meet our criteria were excluded. Many of these were papers reporting on various aspects of prevalence; health knowledge, perceptions, and behaviors; treatments and policies related to waterpipe control. Ten studies were included in the final review.
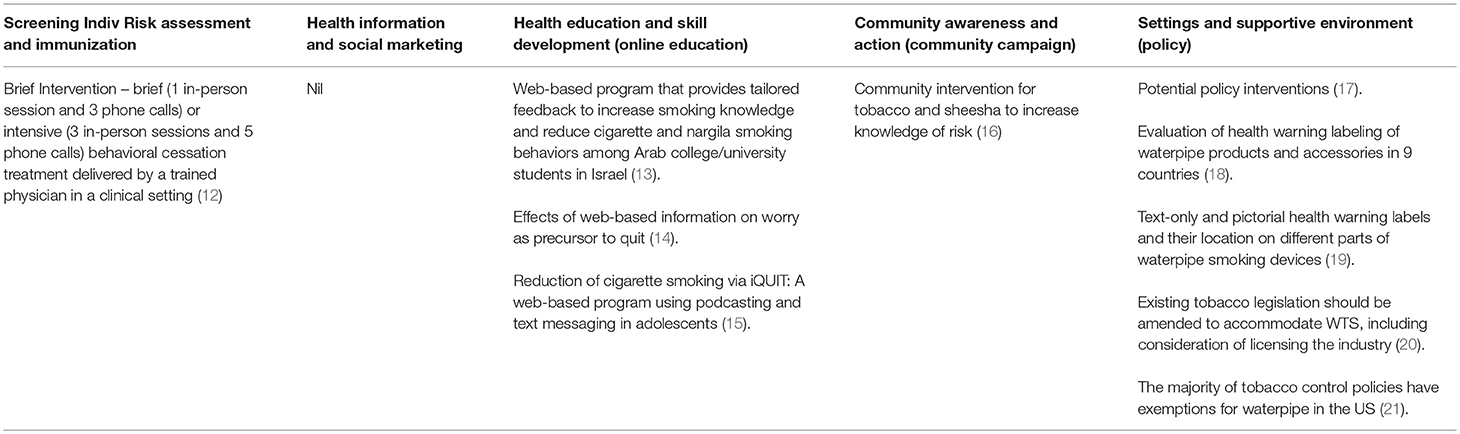
As shown in Table 1, included articles were: a study of a brief behavioral intervention to increase quit rates (12); three studies examining web based health education and skill development initiatives to increase cessation as well as perceived risks and intention to quit (13–15); a community education campaign to raise awareness and increase knowledge (16); as well as five studies that evaluated product labeling or implementation of tobacco control legislation as policy opportunities to create healthy environments (17–21).
Intervention Characteristics
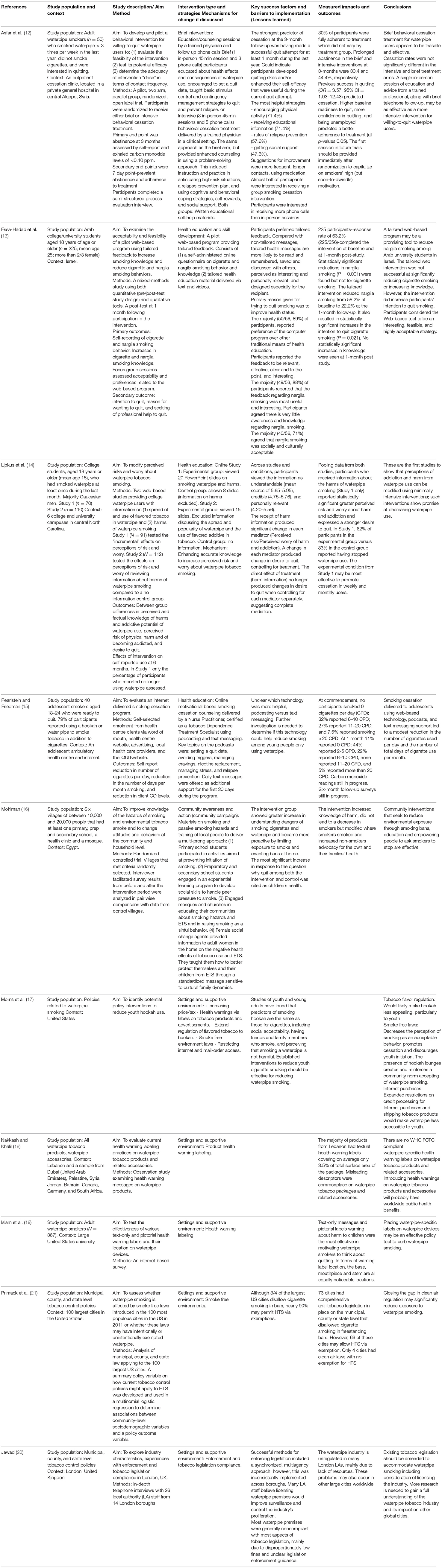
Table 2 describes the characteristics of studies. As shown, Asfar‘s (12) randomized controlled trial tested the feasibility and potential efficacy of brief interventions for waterpipe smoking cessation for willing-to-quit adults who had smoked waterpipe >3 times per week in the last year (but not cigarettes), comparing brief and more intensive interventions delivered by a trained physician in a clinical setting in Syria. Both the brief and more intensive interventions resulted in prolonged abstinence and brief interventions were as effective as more intensive interventions for willing to quit waterpipe users.
Three web based educational interventions targetting adolescents and university students in Israel and the United States who smoked cigarettes and waterpipe also showed some success. Essa-Hadad et al. (13) found that a web-based program providing tailored feedback to increase smoking knowledge and reduce cigarette and waterpipe smoking behaviors among Arab college/university students in Israel was highly acceptable to participants. The program significantly reduced waterpipe smoking from 58.2% at baseline to 22.2% at the 1-month follow-up, and while it did not result in a reduction to cigarette smoking, or increase knowledge, it was found to influence participants' intention to quit cigarettes. Lipkus (14) studied an online education intervention among American college students who had smoked waterpipe at least once in the last month. It successfully modified perceived risks, increased worry about waterpipe smoking and resulted in a reported reduction in waterpipe smoking among some participants. Pearlstein (15) found that an online motivational based smoking cessation program “iQUIT”delivered over a 6 month period to adolescents who reported smoking both cigarettes and waterpipe, using web-based technology, podcasts, and text messaging support, yielded a modest reduction in the number of cigarettes used per day and the number of total days of cigarette use per month. Reductions in waterpipe use were not reported.
A randomized controlled trial of a multi-pronged community intervention in six Egyptian villages by Mohlman (16) delivered education and training to women, students, and religious leaders to improve knowledge of harm related to smoking and second hand smoke and to change behavior and attitudes to waterpipe. While the intervention did not lead to a decrease in smoking (tobacco or waterpipe), it did increase knowledge of harm, modified where smokers smoked and increased non-smokers advocacy for their own and their families' health.
The remaining five studies addressed aspects of tobacco control policies for creating supportive environments to curb waterpipe use. Morris (17) identified a number of regulatory and policy levers that may result in making waterpipe smoking less appealing and available to young people. Among these were regulating tobacco flavorings to enforce removal of sweetners and additives; implementing smoke free laws to decrease the perception of smoking as acceptable, promote cessation, discourage initiation and prevent reinforcement of a community norm; and expanding restrictions on credit processing for internet purchases and shipping tobacco products to make them less accessible to youth. Nakash (18) evaluated health warning labeling practices on waterpipe tobacco products in Lebanon, Dubai, Palestine, Syria, Jordan, Bahrain, Canada, Germany, and South Africa. A lack of appropriate health warning labels on waterpipe tobacco products and accessories, misleading descriptors, and misreporting of tar and nicotine labels were identified. Islam (19) surveyed students in a large university in the United States to test the effectiveness of text-only and pictorial health warning labels and their location on waterpipe devices. Warnings about harm to children were found to be the most effective in motivating waterpipe smokers to think about quitting. The base, mouthpiece and stem were seen by participants as equally noticeable locations. Primack (21) evaluated municipal, county, and state level smoke free laws introduced in the 100 most populous cities in the United States in 2011 to assess whether waterpipe smoking is included or been intentionally or unintentionally exempted. Sixty-nine of Seventy Three cities were found to allow HTS via exemption. Jawad (20) explored industry characteristics, experiences with enforcement and tobacco legislation compliance in London through in-depth telephone interviews with 26 local authority (LA) staff from 14 boroughs. He found low levels of compliance with all forms of regulation due to disproportionately low fines and unclear legislation enforcement guidance.
Study Populations
Interventions targeted different population groups. The brief intervention specifically targeted ready-to-quit adult waterpipe smokers who did not smoke cigarettes. Web based educational programs targeted students and young people who smoked waterpipe as well as cigarettes. The community intervention targeted whole communities in six Muslim villages in Pakistan but specifically young people, religious leaders and women as the change agents. Policy and legislative changes deliver messages and create safe environments for whole populations. The studies reported here were conducted in the United States, UK, Lebanon, Dubai (United Arab Emirates), Palestine, Syria, Jordan, Bahrain, Canada, Germany, and South Africa.
Outcomes
Motivational and behavioral outcomes were assessed in relation to: increased periods of abstinence in adults (12); increasing worry and intention to quit waterpipe among university students (14); and reductions in waterpipe smoking among young people (13, 14). In the community study, Mohlman (16) found increases in knowledge, advocacy and protective behaviors but no reductions to waterpipe smoking behaviors. Studies of product labeling or tobacco control legislation were not linked to behavioral outcomes so their impacts remain unknown.
Mechanisms for Change
Only one study specifically assessed the impact of strategies on a mechanism for change. Lipkus (14) found that the receipt of harm information produced significant change in perceived risk as well as perceived worry of harm and addiction, and each was associated with changes in desire to quit. Thus the authors conclude that strategies targeting cognitive and emotional responses to harm and addiction can be modified and that these emotional changes underlie intentions which are proximal to behavioral changes.
Discussion
The evidence base relating to the impact of health promotion programs on individual and community change is very small. The majority of studies (5/10) focused on the policy and legislative environment and few of these measured impact on outcomes related to smoking. Only one brief intervention was identified, one community level intervention and three health education programs targeting young people. There is a gap in studies trialing health information and social marketing strategies. The only reference to work in this area identified in our search was a major campaign launched in Turkey in 2014 which included television and radio advertisements, outdoor materials, brochures, handouts, newspaper inserts, internet and social media strategies, but although an evaluation was planned it had not yet been reported (TMPD 2014).
Overall, this review indicates that behavioral health promotion interventions have been successful in raising awareness of smoking harm and increasing concern and worry as a precursor to quit in both youth (14) and community populations (16) and directly influencing waterpipe smoking behavior (12, 13). Unfortunately Pearlstein (13) did not report waterpipe smoking outcomes separately from cigarettes so it is unclear whether waterpipe practices were affected.
Both adults and young people are important target audiences. Young people are the fastest growing users of waterpipe (1) and since American data suggest that most adults become addicted during adolescence (17) increasing intention to quit among young people is important. As a practice that is often done at home in some communities, influencing parents to take action to protect children is also an important vehicle for change. The community level study reported here (16) sought to influence mothers' behavior to limit family exposure to smoke, with some success. Further work might explore potential for influencing the behavior of fathers as parents and role models.
Web based information strategies appear to be an appropriate way of providing information to young people. In the studies reviewed here, young people reported preference for these over traditional education methods and valued tailored information and feedback which they perceived as interesting and personally relevant. Health messages were more likely to be read and remembered, saved and discussed with others when tailored to their specific interests. Improving health status was a relevant message for young people since the primary reason given for trying to quit smoking was to improve their health (13).
Few studies reported on the mechanisms they sought to influence, but it is clear that each of the interventions aimed to provide participants with personal resources to bring about change in some aspect of the rules or reasoning through which people understood, undertook and experienced smoking waterpipe. According to Lacouture (22) a mechanism is hidden but real, is an element of reasoning and reactions of agents in regard to the resources available in a given context to bring about changes through the implementation of an intervention, and evolves within an open space-time and social system of relationships. The combination of strategies employed as part of the brief interventions for adults, examined by Asfar (12), sought to reframe people's understanding of harm (I might become addicted, get sick, or die if I continue to smoke waterpipe), induce an emotional response (some level of concern or fear as a precursor to quitting) and instill a cognitive response to controlling emotions associated with quitting (I can make a plan and stick to it even when things feel tough).
Similarly educational interventions for young people sought to enhance their understanding of harm by tailoring information to their questions and to shift the sense of glamor associated with smoking that has been reported in a number of studies (5, 23). Interventions aimed to increase doubt, induce worry and subvert perceptions that smoking means “fitting in” and “being cool.” This might enable adolescents to resist peer pressure to take up smoking and find other less harmful ways of fitting in. The community intervention used a combination of these mechanisms and in addition sought to engage religious leaders to provide authority and endorse the message for people who might feel connected to smoking as a cultural practice (smoking is not necessarily an expression of my culture). The intervention also sought to engage women's sense of responsibility in protecting children by encouraging them to intervene in practices that expose their children and family members to smoke.
Most anti-tobacco legislation in the countries included in the studies reviewed in this paper allowed waterpipe smoking venues via exemption and that compliance was poor with most forms of regulation due to legal uncertainties and low levels of fines applied. Learning from international experience and exploring potential for work at the municipal, regional or state levels is warranted. Smoke free laws may be an important step in shifting community norms. Further investigation of the suitability of labeling on products is another area in which studies indicate potential for impacting young people's knowledge of harm. Price levers may also be used to decrease affordability, especially among young people who are significantly more price sensitive than adults. While this review showed that evidence of impact of policy and regulatory interventions is limited and previous studies have highlighted the multiple challenges involved in waterpipe control (24), recent policy guidance from the World Health Organization indicates a range of policy interventions and suggested actions for regulators to control waterpipe use in signatory countries (7). These extend from the types of interventions identified in studies included in this review (product labeling, price levers, smoke free laws, taxation) to include prohibitions on manufacturers from making health claims related to sheesha products; training for health and other workers; adaptation of existing advertising to address the specific context of internet based vending; modification of waterpipe products to minimize harms; and the extension of existing tobacco surveillance and monitoring systems to include waterpipe. There is evidence that some countries are beginning to call attention to addressing loopholes in legislation, including countries in the Middle East and some states in Australia.
Multipronged approaches addressing multiple mechanisms seem well placed to address the specific practices of waterpipe smoking which differ from cigarette smoking in that they are associated with sociability and relaxation rather than stress, are perceived as less harmful than other forms of tobacco use, may be seen as part of cultural practices, and for some groups start at home.
There are a number of potential limitations to this review. While we conducted a comprehensive search using key databases and hand searching, it is possible that some papers may have been missed. In addition only papers in English were included which means there could be other relevant papers. Gray literature was beyond the scope of this review and it may be that there is evidence of program impacts in evaluation and other technical reports, not available here.
Conclusion
Brief interventions for waterpipe users, community campaigns and web based tailored information can modify perceptions of addiction and harm, increase worry and intention to quit. Product labeling may be an effective policy tool to curb waterpipe smoking. A range of policy interventions have been identified but not evaluated. There is great scope to trial many of these interventions in different contexts. Attention to mechanisms for change including those related to gender/family and social roles, culture, age, and emotions could aid implementation. Co-design of interventions with people from specific target groups may enhance the appropriateness of nuanced messages and therefore increase acceptability and the likely uptake of interventions.
Author Contributions
KG, RK, LW, MH, MS, MK, KT, and JM designed the study. KG and RK designed the review methods, ran the black literature searches and conducted the analyses. LW and MH identified further literature. KG and RK extracted data. KG drafted the manuscript. All authors read and were involved in critically revising the manuscript and all authors have approved the final manuscript.
Funding
This project was funded by the South East Sydney Local Health District.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2018.00308/full#supplementary-material
References
1. Akl EA, Gunukula SK, Aleem S, Obeid R, Jaoude PA, Honeine R, et al. The prevalence of waterpipe tobacco smoking among the general and specific populations: a systematic review. BMC Public Health (2011) 11:244. doi: 10.1186/1471-2458-11-244
2. Maziak W, Talev ZB, Bahelah R, Islam F, Jaber R, Auf R, et al. The global epidemiology of waterpipe smoking. Tobacco Control (2015) 24:i3–12. doi: 10.1136/tobaccocontrol-2014-051903
3. Akl EA, Gaddam S, Gunukula SK, Honeine R, Jaoude PA, Irani J. The effects of waterpipe tobacco smoking on health outcomes: a systematic review. Int J Epidemiol. (2010) 39:834–57. doi: 10.1093/ije/dyq002
4. Wang LW, He E, Ghosh D, O Day R, Jones G, Subbiah R., et al. Severe carbon monoxide poisoning from waterpipe smoking: a public health concern. Med J Aust. (2015) 202:446–7. doi: 10.5694/mja14.01264
5. Maziak W, Jawad M, Jawad S, Ward KD, Eissenberg T, Asfar T. Interventions for waterpipe smoking cessation. Cochr Database Syst Rev. (2015) 2015:CD005549. doi: 10.1002/14651858.CD005549.pub3
6. Tee GH, Hairi NN, Nordin F, Choo WY, Chan YY, Kaur G, et al. Systematic review on international practices in controlling waterpipe tobacco smoking. Asian Pac J Cancer Prev. (2015) 16:3659–65. doi: 10.7314/APJCP.2015.16.9.3659
7. World Health Organisation. Advisory Note: Waterpipe Tobacco Smoking: Health Effects, Research Needs and Recommended Actions by Regulators−2nd edition. WHO Study Group on Tobacco Product Regulation (2015).
8. Ward KD, Siddiqi K, Ahluwalia JS, Alexander AC, Asfar T. Waterpipe tobacco smoking: the critical need for cessation treatment. Drug Alcohol Depend. (2015) 153:14–21. doi: 10.1016/j.drugalcdep.2015.05.029
9. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
10. WHO. WHO Health Promotion Definition. Available online at http://www.who.int/topics/health_promotion/en/ (Accessed 1 May, 2017).
11. Northern Territory Government Health Promotion Framework. Department of Health Darwin, 2013. Available online at http://digitallibrary.health.nt.gov.au/prodjspui/bitstream/10137/881/1/Northern%20Territory%20Health%20Promotion%20Framework.pdf (Accessed 1 May, 2017).
12. Asfar T, Al Ali R, Rastam S, Maziak W, Ward KD. Behavioral cessation treatment of waterpipe smoking: the first pilot randomized controlled trial. Addict Behav. (2014) 39:1066–74. doi: 10.1016/j.addbeh.2014.02.012
13. Essa-Hadad J, Linn S, Rafaeli S. A web-based program to increase knowledge and reduce cigarette and nargila smoking among Arab university students in Israel: mixed-methods study to test acceptability. J Med Internet Res. (2015) 17:e39. doi: 10.2196/jmir.2988
14. Lipkus IM, Eissenberg T, Schwartz-Bloom RD, Prokhorov AV, Levy J, et al. Affecting perceptions of harm and addiction among college waterpipe tobacco smokers. Nicotine Tobacco Res. (2011) 13:599–610. doi: 10.1093/ntr/ntr049
15. Pearlstein I, Friedman S. Reduction of cigarette smoking via iQUIT: a web-based program using podcasting and text messaging in adolescents. J Adolesc Health (2009) 1:S24. doi: 10.1016/j.jadohealth.2008.10.055
16. Mohlman MK, Boulos DNK, El Estouhy M, Radwan G, Makambi K, Jillson I, et al. A randomized, controlled community-wide intervention to reduce environmental tobacco smoke exposure. Nicotine Tobacco Res. (2013) 15:1372–81. doi: 10.1093/ntr/nts333
17. Morris DS, Fiala SC, Pawlak R. Opportunities for policy interventions to reduce youth hookah smoking in the United States. Prevent Chronic Dis Res Pract Policy (2012) 9:120082. doi: 10.5888/pcd9.120082
18. Nakkash RT, Khalil J. Health warning labelling practices on narghile (shisha,hookah) waterpipe tobacco products and related accessories. Tobacco Control (2010) 19:235–9. doi: 10.1136/tc.2009.031773
19. Islam F, Salloum RG, Nakkash R, Maziak W, Thrasher JF. Effectiveness of health warnings for waterpipe tobacco smoking among college students. Int J Public Health (2016) 61:709–15. doi: 10.1007/s00038-016-0805-0
20. Jawad M. Legislation enforcement of the waterpipe tobacco industry: a qualitative analysis of the London experience. Nicotine Tobacco Res. (2014) 16:1000–8. doi: 10.1093/ntr/ntu022
21. Primack B, Hopkins M, Hallett C, Carroll M, Zeller M, Dachille K, et al. US health policy related to hookah tobacco smoking. Am J Public Health (2012) 102: e47–51. doi: 10.2105/AJPH.2012.300838
22. Lacouture A, Breton E, Guichard A, Riddle V. The concept of mechanism from a realist approach: A scoping review to facilitate its operationalization in public health program evaluation. Implement Sci. (2015) 10:153 doi: 10.1186/s13012-015-0345-7
23. Nakkash RT, Khalil J, Affifi RA. The rise in narghile (shisha, hookah) waterpipe tobacco smoking: A qualitative study of perceptions of smokers and non smokers. BMC Public Health (2011) 11:315. doi: 10.1186/1471-2458-11-315
Keywords: waterpipe, smoking, health promotion, health intervention, tobacco control
Citation: Gardner K, Kearns R, Woodland L, Silveira M, Hua M, Katz M, Takas K and McDonald J (2018) A Scoping Review of the Evidence on Health Promotion Interventions for Reducing Waterpipe Smoking: Implications for Practice. Front. Public Health 6:308. doi: 10.3389/fpubh.2018.00308
Received: 14 June 2018; Accepted: 05 October 2018;
Published: 05 November 2018.
Edited by:
Harshad Thakur, Tata Institute of Social Sciences, IndiaReviewed by:
Sankalp Das, Baptist Health South Florida, United StatesIffat Elbarazi, United Arab Emirates University, United Arab Emirates
Copyright © 2018 Gardner, Kearns, Woodland, Silveira, Hua, Katz, Takas and McDonald. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Karen Gardner, a2FyZW4uZ2FyZG5lckB1bnN3LmVkdS5hdQ==
 Karen Gardner
Karen Gardner Rachael Kearns
Rachael Kearns Lisa Woodland3
Lisa Woodland3