- Department of Neuroscience, School of Medicine, University of Turin, Turin, Italy
The role of childhood trauma in the development of borderline personality disorder (BPD) in young age has long been studied. The most accurate theoretical models are multifactorial, taking into account a range of factors, including early trauma, to explain evolutionary pathways of BPD. We reviewed studies published on PubMed in the last 20 years to evaluate whether different types of childhood trauma, like sexual and physical abuse and neglect, increase the risk and shape the clinical picture of BPD. BPD as a sequela of childhood traumas often occurs with multiple comorbidities (e.g. mood, anxiety, obsessive-compulsive, eating, dissociative, addictive, psychotic, and somatoform disorders). In such cases it tends to have a prolonged course, to be severe, and treatment-refractory. In comparison with subjects who suffer from other personality disorders, patients with BPD experience childhood abuse more frequently. Adverse childhood experiences affect different biological systems (HPA axis, neurotransmission mechanisms, endogenous opioid systems, gray matter volume, white matter connectivity), with changes persisting into adulthood. A growing body of evidence is emerging about interaction between genes (e.g. FKBP5 polymorphisms and CRHR2 variants) and environment (physical and sexual abuse, emotional neglect).
Introduction
Borderline personality disorder (BPD) is a severe and heterogeneous disorder characterized by chronic instability, with episodes of severe affective and impulsive dyscontrol, interpersonal and identity disturbances (1). Patients with BPD show a marked emotional sensitivity with the incapacity to modulate intense emotional responses and inadequate return to emotional baseline (2).
The prodromal signs and symptoms that prelude to later personality pathology are already present in very young age, in particular in adolescence (3), meaning that BPD does not abruptly emerge during adulthood.
Prevalence rate of BPD in non-psychiatric population is ranged between 0.7 and over 5% (4, 5) while in clinical settings reaches 10% of all psychiatric outpatients and 15–20% of inpatients (6). BPD is characterized by severe functional impairment, intense use of health services, medications, and a suicide rate of 10–50 times higher than the rate in the general population (7).
Psychodynamic theories suggested that BPD arises from precocious distortions in object relations (8) and characteristic patterns of attachment (9), inducing an intolerance of aloneness, hypersensitivity to environmental stimuli, expectation of detached and hostility from other, and loss of positive memories of dyadic relationship (10).
From early attachment experiences, subjects gain important information about their identity and abilities to regulate inner experiences and behavioral strategies for maintaining proximity to others. Aggression or neglect from caregivers may be experiences contributing to compromise a realistic and balanced view of self and others (10). So, an insecure model of attachment with caregivers is internalized and could be at the origin of the expectancies for future relationships characterized by abuse or rejection (11). BPD occurs in a precocious context of intolerance toward the manifestations of private emotions during childhood (12). So, children exposed to these unfavorable conditions are unable to recognize, regulate, and tolerate emotional responses and they fluctuate between extreme emotional lability and emotional inhibition. In 30% up to 90% of cases BPD is associated with abuse and neglect in childhood and these percentages are significantly higher than those registered in other personality disorders (13–15). Some authors proposed affect regulation difficulties as central mediator in the relationship between childhood trauma and BPD (16). Interpersonal dysfunctions are a result of early scarcity of emotional closeness or responsibility from caregivers in early childhood (17).
Similarly to other psychiatric disorders, the most acknowledged etiopathogenetic theory of BPD suggested that this disturbance was produced by the interaction of biological and psychosocial factors (17–19), in particular biologically based vulnerabilities (temperamental features, genetic polymorphisms) and adverse environment (traumas) during childhood or adolescence. These traumatic experiences could be also associated to neuromorphological abnormalities and to neuroendocrine changes (i.e. hypothalamic-pituitary axis (HPA) activation) that are observed in patients with early BPD and abuse/neglect history (20).
The aim of this review is to provide an updated overview on different types of traumatic events (sexual and physical abuse, neglect, and bullying) that combined with temperamental, genetic, and neurobiological factors may contribute to early manifestations of BPD.
We searched in Pubmed database studies focused on borderline symptoms and disorder in adolescents up to 20 years old, published between 2000 and 2021 and using the following terms: (borderline personality disorder) AND (child OR adolescent OR teen OR young) AND (trauma OR abuse OR maltreatment OR neglect OR bullying) AND (temperament) AND (environment) AND (epigenetic factors OR neuroimaging OR neurobiology) AND (suicide OR self-injury) AND (cPTSD). Eligibility status for articles was defined by the initial screening of trials on the basis of title and abstract. Papers that passed the initial screening were further selected on the basis of a careful examination of the full manuscript content. The review considered only articles written in English. We included the following type and number of studies: 30 longitudinal, 12 retrospective, 9 cross-sectional, 1 randomized controlled trials. Assessment instruments more commonly used in the trials were: the Borderline Personality Features Scale for Children (BPFS-C) and a recently developed parent report version of the same measure (BPFS-P); the Revised Diagnostic Interview for Borderlines (DIB-R); the Child Interview for DSM-IV Borderline Personality Disorder (CI- BPD); the Child Interview for DSM-IV Borderline Personality Disorder. Number of studies participants ranged between 12 and 7,771. Age of patients ranged between 9 and 21 years. Five studies included only females. Participants were mainly Caucasian.
Factors Associated to Early Onset of BPD: Temperamental Traits and Environmental Context
Temperamental Factors
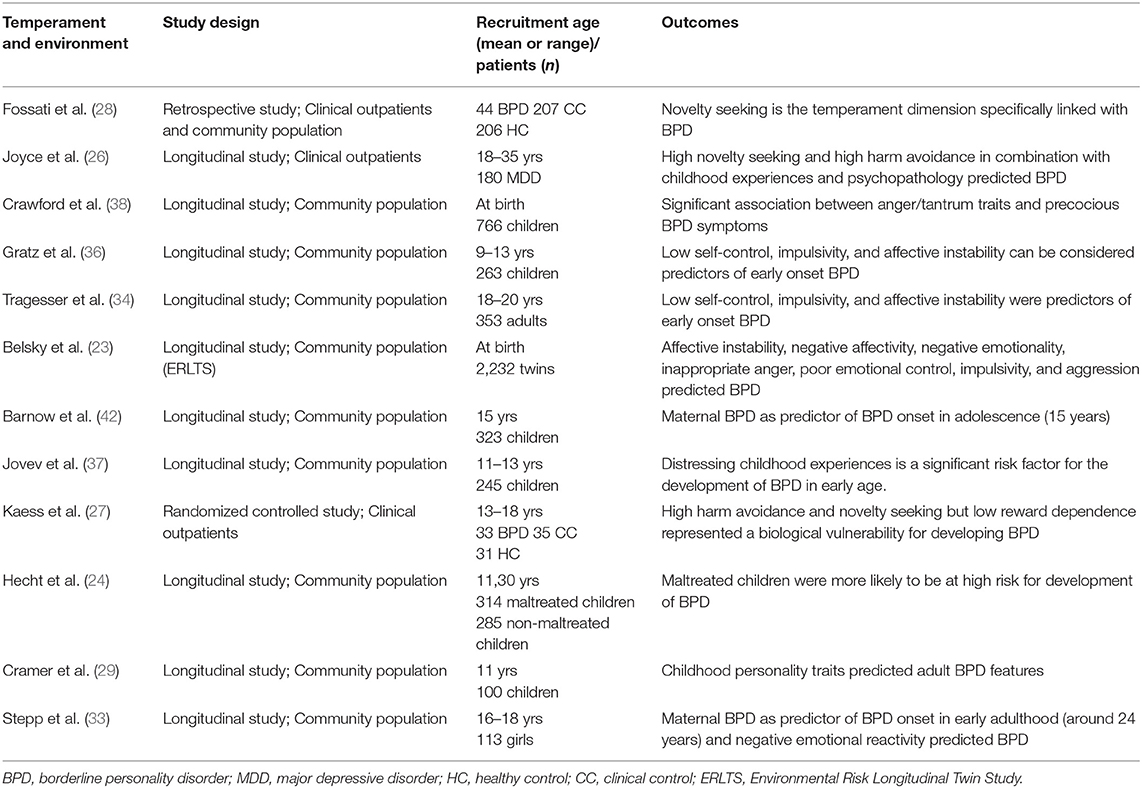
Intrapsychic factors, including temperamental characteristics and personality traits in childhood and adolescence, must be investigated to recognize predictors of BPD at an early phase (3). There is a general consensus that temperamental vulnerabilities combined with childhood adversities play a role in the development of BPD traits (12, 21, 22). Researchers identified several temperamental traits in children or adolescents, including affective instability, negative affectivity, negative emotionality, inappropriate anger, poor emotional control, impulsivity, and aggression, that could predispose to borderline personality disorder (3, 23, 24). Model proposed by Cloninger for personality pathology underlines the role of temperamental characteristics in BPD development (25). Some authors found that high harm avoidance and novelty seeking (in combination with childhood traumatic experiences and adolescent psychopathology) can be considered predictive of early onset BPD (26). In a randomized controlled study that compared 33 BPD adolescents with 35 clinical controls and 31 healthy subjects, it was observed that high harm avoidance and novelty seeking, together with low reward dependence represented a vulnerability for BPD onset (27).
In particular, novelty seeking is the temperament dimension that was specifically linked with BPD and differentiated BPD patients from non-clinical patients, patients without personality disorders (PDs), and patients with other PDs (including diagnoses of cluster B disorders) (28).
Among other temperamental traits, aggression at a very juvenile age was associated with precocious onset of BPD (24, 29, 30). Vaillancourt et al. found in a prospective study performed in 484 children and adolescents that aggression was a predictor for the early diagnosis of BPD (at 14 years) with some gender differences. In particular, relational aggression was the main predictor in boys, while physical aggression was the strongest predictor in girls. The same authors suggested that negative emotionality, in terms of negative affectivity and poor emotional control, was another temperamental trait often associated to early BPD (31). Several studies designed to evaluate how negative emotionality and other traits, such as affiliation, constraint, and agency, might impact onset of BPD showed that negative emotionality and low constraint predicted onset of BPD at younger age (32, 33), as well as the association of negative affectivity with impulsivity and lower sociability in childhood (34, 35).
Two different longitudinal studies by Gratz and Tragesser identified that three tightly connected traits—low self-control, impulsivity, and affective instability—can be considered predictors of early onset BPD (34, 36). One study investigated the impact of the temperamental trait of anger on precocious BPD (37). Crawford and colleagues showed a significant association between anger trait and early BPD symptoms in a large sample of 766 children who were followed for 20 years (38).
Available data sustained the hypothesis that temperamental factors may increase vulnerability for the development of BPD, but they are not sufficient to predict this disorder and need to interact with environmental negative factors to induce it. Several investigations indicated that the interaction of temperamental vulnerabilities with environmental experiences [i.e., distressing childhood experiences within the context of the family (12, 22)] is a significant risk factor for the development of BPD in early age (21, 37).
Environmental Factors
Environmental factors that have been identified as predisposing conditions for early BPD encompass familial maltreatments (abuse and neglect), psychopathology of family members, and parent-child conflicting relationship. It has been supposed that the development of cognition and affectivity, the integration of thinking and emotions, and the ability to discern emotional states are disturbed by early trauma with consequent post-traumatic reactions, dissociation, and alexithymia (39).
Children who suffer maltreatments may infer negative characteristics of themselves and others and deduce that they are intrinsically unacceptable and deserve maltreatment. This assumption may lead to see themselves as “helpless, unlovable, or weak and to view other people as dangerous, rejecting, or unavailable”. So, abused children may internalize negative perception about themselves, others, and about relationships with other people (40).
Childhood familial maltreatments may foster BPD through insecure attachment. Abused children tend to “blame themselves for their maltreatment when the perpetrator is an attachment figure” (41). In particular, more severe and chronic experiences of maltreatment may produce a negative image of oneself with consequent expectation to be abandoned (i.e., attachment anxiety) and a simultaneous negative perception of others as unworthy of being trusted (i.e., attachment avoidance) (40). Some studies showed that primarily attachment anxiety, rather than avoidance (more related to father's maltreatment), plays a role in the relation between child maltreatment and the development of precocious BPD symptoms.
Findings from studies focused on maternal psychopathology emphasize the importance of considering the diagnosis of BPD in mother as predictor of BPD onset in adolescence (around 15 years of age) (42). Maternal externalizing disorders, characterized by poor impulse-control, rule breaking, aggression, and impulsivity were significantly associated with early BPD in offspring (43). Maternal anxiety and depression during pregnancy predict early BPD in sons or daughters. (44).
Among familial relationships, role confusions and disoriented behaviors in parent-child relationship were found in patients with early BPD symptoms, in particular self-injuries in adolescence (45). Moreover, dysfunctional familial relationships characterized by induction of guilt, psychological control, and triangulation (children who have a role of mediator in the parental marital conflicts), were observed in large samples of adolescents with severe behavioral and emotional disorders who had already showed BPD symptoms in childhood (46).
Studies on temperamental and environmental factors associated to early onset BPD are presented in Table 1.
Traumatic Experiences and Early Onset of BPD
The hypothesis that early traumatic life experiences foster the development of BPD received increasing scientific validation. In particular, early traumas work as triggers for the evolution of several BPD characteristics, such as affect instability, emotion dysregulation, and self-destructive behaviors (47). Traumatic events play a central role as they seem to impair the ability of mentalizing or symbolizing emotions (48, 49), especially in early phases of life. A recent study on this focus (50) suggested that the adverse childhood experiences (ACEs) involving emotional and physical trauma, parental mental illness, and exposure to poverty in early stages of life were the strongest predictor of BPD symptoms in 14–19-year-old subjects, even when parental psychopathology and poverty were excluded from the analysis. In particular, this study found that ACEs in preschool age were particularly impacting on early development of borderline personality features.
In accordance with diathesis–stress theories of borderline etiology (13), precocious traumatic experiences in terms of abuse and neglect and inherited vulnerability (specific temperamental traits and genetic polymorphisms) play a synergistic role to foster borderline personality features. In this perspective, we cannot consider single predisposing factors to early BPD as point insults that produce the disorder by themselves, but rather as overlapping factors that added to other environmental or biological conditions contribute to the genesis of the disorder. Moreover, there is a cumulative effects of traumatic experiences: children who had experienced more than one type of abuse and maltreatment perpetrated across developmental periods had significantly higher severity of borderline personality features (24, 51–53).
We will discuss below available evidences on this issue, conceiving trauma in terms of abuse or neglect conducts from parents and peers that contributed to early development of borderline pathology. Verbal, emotional, physical, and sexual abuse, together with emotional and physical neglect, and chronic exposure to peer victimization were identified as potential factors that increase the risk for early BPD.
Some studies that will be reported in the following paragraphs are the same described in the previous section (temperamental factors and environmental factors) as authors investigated the role and interaction of different risk factors in early BPD onset.
Sexual Abuse
Sexual abuse is defined as “any sexual act to which the victim did not consent, could not consent, or was pressured or manipulated into consenting” (54).
Most of studies showed a significant association between childhood sexual abuse (CSA) and onset of BPD at very young age (33, 50, 55–61). Nevertheless, this evidence was not replicated in all studies. In fact, Hect et al. (24) did not find a relationship between BPD and sexual abuse. This result should be interpreted considering the study limitations: a small sample size and the possibility that consequences of sexual abuse may manifest after the middle-childhood period, which was the timespan analyzed in Hect's study. Findings from several investigations suggested that adolescents with BPD have a history of sexual trauma more frequently than both healthy adolescents (57) and non-BPD psychiatric patients (58).
In BPD adolescents some authors found a higher rate of sexual abuse-related events, than in depressed and healthy control adolescents (55). In addition, sexual abuse events were significantly associated to suicidal conducts in youths with BPD (62). Psychological burden of CSA experiences does not decrease with the disclosure. On the contrary, this can be a delicate period with increased risk of suicide and development of personality disorders (60). In particular, a cohort study that compared the presence of several psychiatric diagnoses in adolescents who had been victims of CSA, reported that BPD was the only diagnosis not present at all before the disclosure of CSA experience, but it was found in the first year, and its rate drastically increased in the second year after the first registered CSA experience (61). These findings supported the specificity of the relationship between precocious sexual abuse experiences and early BPD onset.
Sexual abuse was found the only one, among different types of abuses (e.g. neglect, physical, and sexual abuse), to reach an independent significant relation with early BPD development in a study performed in a sample of adolescent females with BPD, compared with a clinical control group with mixed psychiatric diagnoses (59). Precocious sexual abuse could alter clinical manifestations and worsen the course of BPD. Some authors observed a significant relationship between sexual abuse and psychotic-like experiences in young patients with borderline personality features (63) and a more severe general clinical picture in BPD patients with prolonged childhood sexual abuse than subjects who had not experienced these traumas (50, 64). Moreover, adolescent BPD females who did not remit four years after initial presentation of symptoms were significantly more likely to have self-reported childhood sexual abuse, concomitant depressive symptoms, or substance use disorder (56). On the other hand, BPD symptoms significantly improved from ages 16 to 18 among BPD adolescent girls who did not report experiences of sexual abuses (33).
Physical and Verbal Abuse
Physical abuse consists of “the non-accidental infliction of physical injury on the other person (e.g., bruises, welts, burns, choking, and broken bones), while verbal abuse involves some sort of verbal interaction that causes a person's emotional harm (e.g. blaming, criticism, judging, and name-calling)” (24). Several studies found a relationship between physical or verbal abuse and BPD development (23, 24, 37, 59, 65).
Children who were physically maltreated developed more BPD symptoms at age 12 compared to non-maltreated peers and were especially vulnerable if they had relatives with psychiatric disorders (23). Harsh treatment and inherited vulnerability seem to play a synergistic role to foster borderline personality features. Not only family history, but also children temperamental characteristics can facilitate manifestation of BPD symptoms if physical abuse is suffered: children with a low level of the temperamental trait of affiliation who were physically abused showed an earlier onset and a higher severity of BPD symptoms (37). The relationship between perpetrated maltreatments and temperament is complex and debated: maltreatment could promote the onset of BPD in patients who had a biological vulnerability (specific temperamental traits). Nevertheless, it is also possible that precocious and repeated familial maltreatments influence at least some of the temperamental features related to BPD. Timing of measurement of temperamental features constitutes a limitation as it is hard to distinguish temperamental traits in personality of adult patients.
The effect of physical trauma affects many domains of personality, such as affective dysregulation, identity diffusion, disturbed relationships, and self-harm. Physically abused children presented higher scores on each domain in comparison with a non-maltreated children control group. Moreover, they had higher overall borderline trait scores and were more likely to be recognized as individuals at high risk for BPD (24).
Not all studies are consistent about the specific relationship between physical abuse and early BPD development. Infurna et al. (59) found a significant association between physical abuse from father and BPD onset when univariate regression was used, while this association was lost when results were analyzed by means of a multivariate regression model, including other types of abuse experiences. Biskin et al. (56) found no difference between BPD and clinical comparison groups on self-reports of physical abuse.
As regards the effects of verbal abuse, data are limited. Some authors suggested that the impact of harsh speech can be traumatic as well as physical abuse. Johnson et al. (65) found that children who experienced verbal abuse from mother were more prone to borderline, narcissistic, obsessive-compulsive, and paranoid PDs in adolescence or early adulthood compared to subjects who did not experience verbal abuse.
Neglect
In the context of caregiving, neglect is a kind of abuse characterized by “failure to supervise the child properly, leading to physical or emotional harm” (65). Neglect concept includes physical neglect, which is the failure to meet adequately the physical needs of children, and emotional neglect, which is represented by emotional detachment by the caregivers to the requests for attention and care of children (66).
The association between neglect and early BPD development was reported by several studies (24, 37, 57, 59, 67, 68). The most significant findings showed that: adolescents with BPD and concomitant depression had significantly higher rates of neglect than healthy controls (57); physical neglect was associated with BPD features onset at an earlier age (24); the combination between specific temperamental features and physical/emotional neglect may speed up the onset of BPD and antisocial personality disorder (ASPD) symptoms (37); and neglect from both parental figures was reported more often among BPD adolescents in comparison with other clinical populations (59).
The impact of specific kinds of neglect (i.e. childhood supervision neglect and maternal withdrawal) was investigated in two studies (67, 68). Childhood supervision neglect, including the failure to set limits, to attend to misbehavior, to know child's whereabouts and friends, was associated with higher risk for Cluster B personality disorders in adolescence and early adulthood (67). Maternal withdrawal in infancy, a kind of neglect in which mother creates physical and verbal distance from her baby, was a robust predictor of both BPD symptoms and self-injuries or suicidality in adolescence (68).
Bullying
“Bullying is a systematic abuse of power and is defined as aggressive behavior or intentional harm doing by peers that is carried out repeatedly and involves an imbalance of power, either actual or perceived, between the victim and the bully” (69).
Bullying includes both physical and verbal acts of aggression or indirect bully victimization denoted by social exclusion (70, 71). In a psychological perspective, victimization may affect upon inner working models that pertain the relationships, disturbing the capacity to trust and interact with others in a correct manner, and leading to unstable relationships, distort perceptions, and emotional dysregulation (72).
Several studies reported that being bullied during the period of primary school is a strong predictor of early BPD onset (73, 74) approximately up to 2–6 years after the bullying conducts (73). Feelings of loneliness, anger, and loss of trust that are due to victimization by peers were frequently described by victims of bullying who had developed BPD in young age and were observed also during experimental social trust games (75, 76).
Wolke and colleagues (73) conducted one study in order to explore the association between peer victimization and BPD symptoms. Authors considered peer victimization during primary school as a potential predictor of the disorder's onset at about 12 years and observed that children who were exposed to chronic bullying (at 8 and 10 years) had an augmented risk of BPD symptoms with a dose-response relationship. Children who experienced relational and repeated peer victimization had seven times increased risk to early BPD symptoms compared to those that were not bullied. In our previous investigation aimed to identify which factors are independently associated to early onset of BPD, we found that earlier onset of BPD is associated to traumatic experiences, including abuse, neglect, and dysfunction in household environment. A significant traumatic condition that was identified in our analysis of early BPD risk factors is bully victimization (74). Studies on precocious traumas (sexual abuse, physical/verbal abuse, neglect, bullying) and early onset BPD are displayed in Table 2.
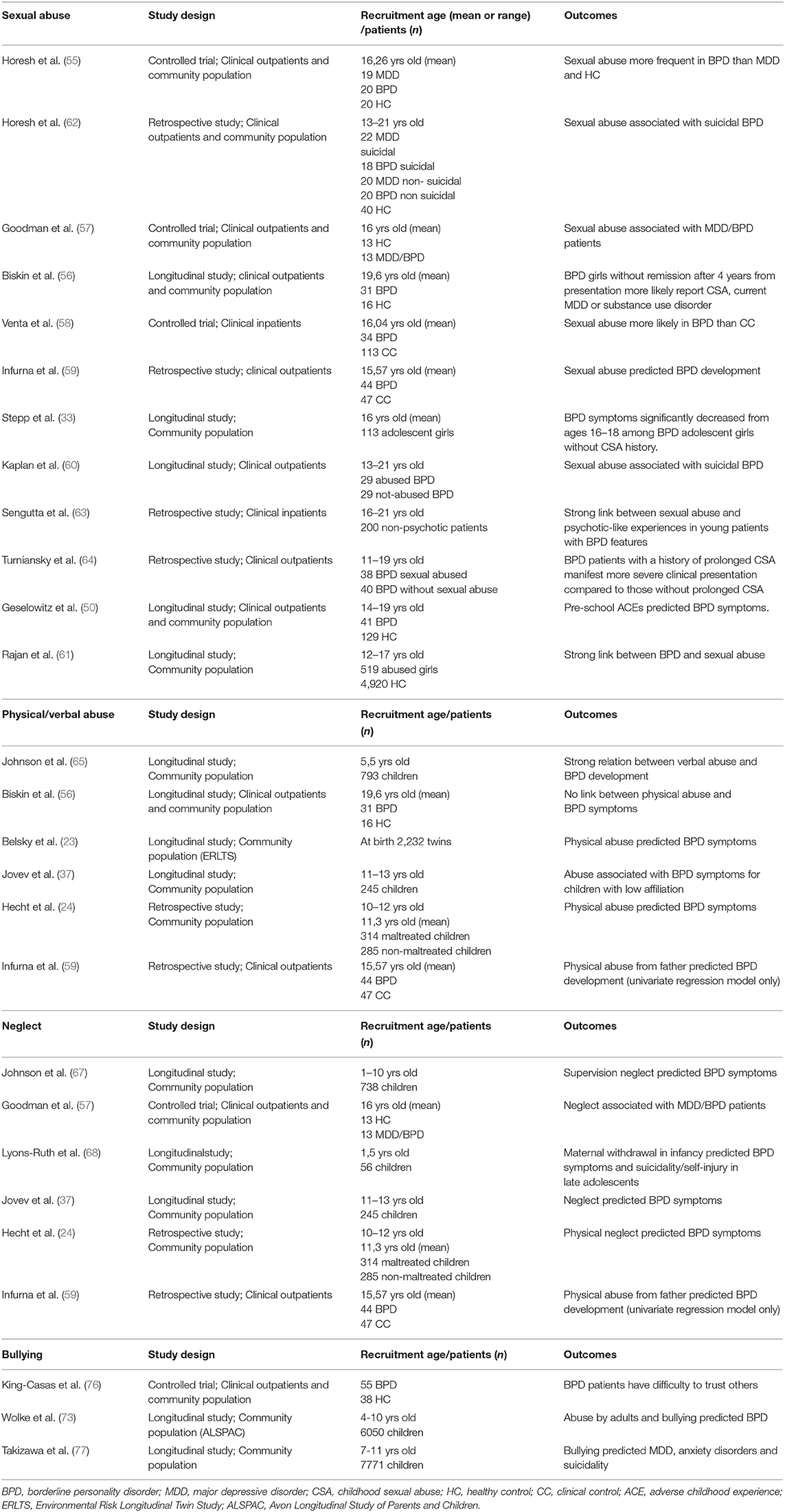
Table 2. Studies on precocious traumas (sexual abuse, physical/verbal abuse, neglect, and bullying) and early onset BPD.
Neurobiology, Neuro-Morphology and Epigenetic in Early Trauma and BPD
There is a general consensus in retaining that alterations in several biological systems and brain anatomical features are related to traumas in childhood and to early BPD. Some authors have examined the effect of early stressful events on biological systems in order to identify biomarkers that could be involved in BPD vulnerability. These markers might allow an early detection of individuals at high risk for BPD (2).
Precocious traumatic experiences lead to chronic “hyperarousal” of the hypothalamic-pituitary- adrenal axis (HPA), resulting in higher levels of cortisol. Several investigators found an increase of cortisol levels (urinary, salivary, and blood) in patients with BPD, hallmarking HPA activation (78–80). The cortisol hyper-stimulation of the hippocampus can generate a distorted interpretation of signals from the environment as constant menaces, therefore sending this danger signals to amygdala, that modulates fear and aggression (20). Intense emotional responses to small stress with a greater latency for returning to baseline conditions are common in young BPD patients. Moreover, over-functioning of the prefrontal cortex generates loss of rationality, reasoning, and decision- making capacity in BPD patients (20, 81).
With regards to neuroimaging investigations, several preclinical studies have delineated the effects of early stressors on specific brain regions. Corpus callosum and other myelinate areas are potentially vulnerable to the impact of early exposure to higher levels of stress hormones, that suppress glial cell division crucial for myelination (82) and determine a reduced size of the corpus callosum (83, 84). These results were confirmed in clinical investigations. De Bellis and colleagues observed the reduction of volume of corpus callosum size in children with a history of abuse and post-traumatic stress disorder (PTSD) (85). Reduction of the corpus callosum size may lead to a diminished communication between the hemispheres, with an increased hemispheric laterality (82).
The association between decreased hippocampal volume, early traumatic events, and development of psychiatric disorders in early phases of life was also investigated (86, 87). In particular, an average of 16% reduction in hippocampal volume bilaterally was seen in BPD females with a history of childhood victimization (88). Some authors observed a direct proportional correlation between the amount of volume reduction in the mentioned areas and severity of trauma exposure in childhood (89). In addition to the volumetric reduction that was observed in corpus callosum, hippocampus, and prefrontal cortex, some abnormalities in activity were found in amygdala, in particular in BPD females with traumatic experiences in childhood (90).
Despite the detrimental consequences of child maltreatment on developmental processes, some subjects show resilience, with low level of psychopathology, while others develop severe disorders. Gene-environment interaction model can help us to better understand the role of trauma on genetic predisposition to develop early BPD. An interconnection between genes and environment in relation to behavior was firstly reported by Caspi et al. (91). In particular, authors observed that maltreated children who developed conduct disorder and antisocial personality disorder had a genotype that resulted in low levels of monoamine oxidase A (MAOA) expression (92).
Some studies evaluated how serious life events (SLE) (i.e., physical abuse, rape, and childhood sexual abuse—CSA) interact with polymorphisms of genes in producing behavioral patterns characteristic of BPD. In BPD patients trauma was found associated with a decrease or an increase of impulsivity depending on the genotype: lower impulsivity after SLE was associated to SS and SL genotypes and higher impulsivity was associated to LL carriers of the long/short (L/S) polymorphism of the serotonin transporter promoter (5-HTTLPR) (93). Interactions between trauma and the rs4680 COMT polymorphism involved in dopaminergic functioning (COMT Val158Met) was also evaluated. Results reported that the Val/Val genotype (but not the Val/Met and Met/Met genotypes) was associated with lower impulsive aggression in BPD (94).
Martin Blanco and colleagues (95) performed a study aimed to study the interaction of HPA genetic polymorphisms and childhood trauma in BPD. Authors found that two FKBP Prolyl Isomerase 5 (FKBP5) alleles (rs3798347-T and rs10947563-A) were more frequent in BPD subjects who experienced physical abuse and emotional neglect and two Corticotropin-releasing factor receptor 2 (CRHR2) variants (rs4722999-C and rs12701020-C) were more common in BPD subjects sexually and physically abused (95). These findings can suggest that childhood trauma modulates the onset of this disorder (92).
In order to better understand the influence of the environment on gene, some epigenetic studies were performed. Perroud et al. (96) investigated epigenetic changes of serotonin 3A receptor (5-HT3AR) in patients with childhood maltreatment and several psychiatric disorders. They found that epigenetic modification of 5-HT3AR was related to a history of childhood maltreatment and more severe psychiatric disorders, including BPD, in adulthood (96). Another study showed a higher methylation of glucocorticoid receptor gene NR3C1 in patients with BPD and childhood traumas (97).
Studies on neurobiological, neuro-morphological, and epigenetic factors in early onset BPD are described in Table 3.
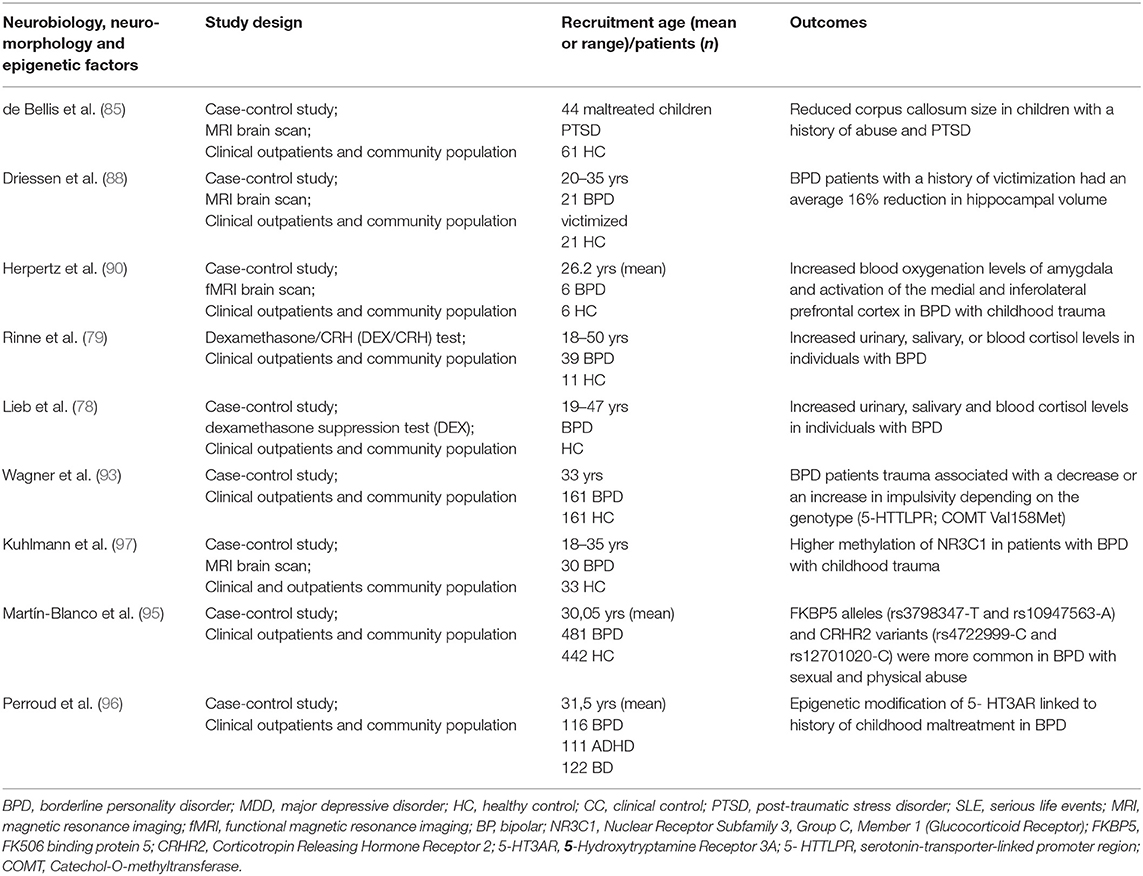
Table 3. Studies on neurobiological, neuro-morphological, and epigenetic factors in early onset BPD.
BPD and Complex PTSD: Recent Traumatic Experiences Could Reactivate Precocious Traumas?
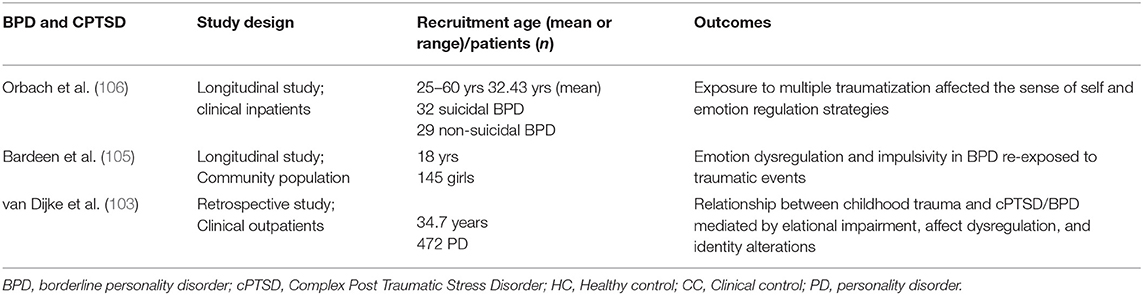
Repeated traumatic events provoked by caregivers or intimate partners involve the risk of developing a constellation of psychiatric symptoms. Complex Post Traumatic Stress Disorder (cPTSD) was originally conceptualized to indicate the reaction to multiple, perpetrated traumatic events with onset in early life (98). More recently the diagnosis of cPTSD referred to a “clinical syndrome following experiences of interpersonal traumatic victimization and is characterized by difficulties in emotion regulation, interpersonal relationships, and self-concept” (99). So, cPTSD shows some overlapping with BPD, including dissociative symptoms, dysregulation of emotions, self and relational disturbances (100). In fact, chronic precocious traumatic experiences often result in more pervasive disorders than simple PTSD with impairment in attachment style and in the ability to modulate emotions. Trauma can produce its effects on behavioral, emotional, physiologic, and neuroanatomical levels. Assaults lead to hyperarousal states that can interfere with right judgment of the relationships and situations. Later stressors tend to be experienced by victims of trauma as a reactivation of the precocious traumatic experiences (101).
Prolonged and repeated traumas, particularly in early life, promote a chronic inability to modulate emotions, that can result in behavioral patterns characteristic of BPD, such as disturbed relationships, substance abuse, and self-injuries behaviors, in which precocious traumatic events are re-enacted over time (102).
Despite the great interest in this topic, systematic investigations focused on the relationship between precocious traumas, present traumatic experiences, complex post traumatic disorder and BPD psychopathology are still scarce. One of the main reasons is that complex PTSD has been proposed by several investigators, but has been included as an official diagnosis only very recently in ICD-11. So, only now well-defined diagnostic criteria are available for PTSD and BPD in DSM- 5 and for cPTSD in ICD-11. A comparison of these criteria in clinical samples will allow to identify more clearly differences and similarities of these psychopathological constructs.
One study was performed in order to determine whether patterns of affective dysregulation, relational impairment, and identity alterations, mediate the relationship between exposure to interpersonal traumatic stressors in childhood and present clinical symptoms in a sample of adults diagnosed with severe cPTSD/BPD. Results of the study demonstrated that the relationship between childhood exposure to trauma and cPTSD/BPD symptoms in adulthood was mediated by the three factors: relational impairment, affect dysregulation, and identity alterations (103). Some authors hypothesized that emotion dysregulation and impulsivity in BPD may increase vulnerability to be re-exposed to traumatic events due to high appraisal of threat, diminished coping resources, increased exposure to risky situations, and intense emotional responding peri-traumatically (104, 105). Exposure to multiple traumatization affected the sense of self and emotion regulation strategies (106). These key alterations of personality can evolve into BPD or cPTSD. Emotional dysregulation may also increase the tendency to perceive new events as threatening and traumatic (107).
Studies on BPD and complex PTSD are presented in Table 4.
Conclusions
On the basis of the results discussed in the previous sections, we can conclude that the interaction of temperamental, environmental, and genetic factors with early traumatic experiences can promote onset of BPD in young age. Available data suggested that experiences of abuse, neglect, and bully victimization in childhood, temperamental traits of impulsive aggression and negative affectivity interacting with dysfunctional familial environment, volumetric and functional abnormalities in fronto-limbic areas associated to precocious trauma and specific polymorphisms of genes (MAOA; 5-HTTLPR; FKBP5; CRHR2; 5HTTR; COMT) characterize subjects at high risk to develop BPD. In accordance with our preliminary model of risk factors in early BPD (3), the effect of the interaction of different risk factors is more decisive than the separate effects of single factors in early development of BPD. So, the effects of traumatic experiences are enhanced when the dysfunctional familial environment that produces traumas interacts with the child's innate temperamental traits or specific genetic polymorphisms.
The mechanisms of interaction of different predisposing factors are only partially known and further studies are required to understand which factors have an independent effect and which produce their action as mediators or modulators.
Author Contributions
All authors provided their contribution to collection and analysis of data and preparation of manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association (2013).
2. Cattane N, Rossi R, Lanfredi M, Cattaneo A. Borderline personality disorder and childhood trauma: exploring the affected biological systems and mechanisms. BMC Psychiatry. (2017) 17:221. doi: 10.1186/s12888-017-1383-2
3. Bozzatello P, Bellino S, Bosia M, Rocca P. Early detection and outcome in borderline personality disorder. Front Psychiatry. (2019) 10:710. doi: 10.3389/fpsyt.2019.00710
4. Barnow S, Herpertz SC, Spitzer C, Stopsack M, Preuss UW, Grabe HJ, et al. Temperament and character in patients with borderline personality disorder taking gender and comorbidity into account. Psychopathology. (2007) 40:369–78. doi: 10.1159/000106467
5. Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the wave 2 national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. (2008) 69:533–45. doi: 10.4088/jcp.v69n0404
6. Skodol AE, Gunderson JG, Pfohl B, Widiger TA, Livesley WJ, Siever LJ. The borderline diagnosis I: psychopathology, comorbidity, and personality structure. Biol Psychiatry. (2002) 51:936–50. doi: 10.1016/s0006-3223(02)01324-0
7. American Psychiatric Association. Practice guideline for the treatment of patients with borderline personality disorder. Am J Psychiatry. (2001) 158(Suppl. 10):1–52.
8. Kernberg O. Borderline personality organization. J Am Psychoanal Assoc. (1967) 15:641–85. doi: 10.1177/000306516701500309
9. Bowlby J. Attachment and Loss: Volume II Separation: Anxiety and anger. London: The international psycho- analytical library (1973) vol. 95, p. 1–429.
10. Critchfield KL Levy KN Clarkin JF Kernberg OF. The relational context of aggression in borderline personality disorder: using adult attachment style to predict forms of hostility. J Clin Psychol. (2008) 64:67–82. doi: 10.1002/jclp.20434
11. Fonagy P. Male perpetrators of violence against women: an attachment theory perspective. J Appl Psychoanal Stud. (1999) 1:7–27. doi: 10.1023/A:1023074023087
12. Linehan MM. Dialectical behavior therapy for treatment of borderline personality disorder: implications for the treatment of substance abuse. NIDA Res Monogr. (1993) 8:279–92.
13. Battle CL, Shea MT, Johnson DM, Yen S, Zlotnick C, Zanarini MC, et al. Childhood maltreatment associated with adult personality disorders: Findings from the collaborative longitudinal personality disorders study. J Pers Disord. (2004) 18:193–211. doi: 10.1521/pedi.18.2.193.32777
14. Yen S, Shea MT, Battle CL, Johnson DM, Zlotnick C, Dolan-Sewell R, et al. Traumatic exposure and posttraumatic stress disorder in borderline, schizotypal, avoidant, and obsessive-compulsive personality disorders: findings from the collaborative longitudinal personality disorders study. J Nerv Ment Dis. (2002) 190:510–8. doi: 10.1097/00005053-200208000-00003
15. Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Prediction of the 10-year course of borderline personality disorder. Am J Psychiatry. (2006) 163:827–32. doi: 10.1176/ajp.2006.163.5.827
16. van Dijke A, Ford JD, van der Hart O, van Son M, van der Heijden P, Bühring M. Affect dysregulation in borderline personality disorder and somatoform disorder: differentiating under- and over-regulation. J Pers Disord. (2010) 24:296–311. doi: 10.1521/pedi.2010.24.3.296
17. Hughes AE, Crowell SE, Uyeji L, Coan JA. A developmental neuroscience of borderline pathology: emotion dysregulation and social baseline theory. J Abnorm Child Psychol. (2012) 40:21–33. doi: 10.1007/s10802-011-9555-x
18. Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: elaborating and extending Linehan's theory. Psychol Bull. (2009) 135:495–510. doi: 10.1037/a0015616
19. Leichsenring F, Leibing E, Kruse J, New AS, Leweke F. Borderline personality disorder. Lancet. (2011) 377:74–84. doi: 10.1016/S0140-6736(10)61422-5
20. Mainali P, Rai T, Rutkofsky IH. From child abuse to developing borderline personality disorder into adulthood: exploring the neuromorphological and epigenetic pathway. Cureus. (2020) 12:e9474. doi: 10.7759/cureus.9474
21. Bornovalova MA, Gratz KL, Delany-Brumsey A, Paulson A, Lejuez CW. Temperamental and environmental risk factors for borderline personality disorder among inner-city substance users in residential treatment. J Pers Disord. (2006) 20:218–31. doi: 10.1521/pedi.2006.20.3.218
22. Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, et al. Axis I comorbidity of borderline personality disorder. Am J Psychiatry. (1998) 155:1733–9. doi: 10.1176/ajp.155.12.1733
23. Belsky DW, Caspi A, Arseneault L, Bleidorn W, Fonagy P, Goodman M, et al. Etiological features of borderline personality related characteristics in a birth cohort of 12-year-old children. Dev Psychopathol. (2012) 24:251–65. doi: 10.1017/S0954579411000812
24. Hecht KF, Cicchetti D, Rogosch FA, Crick N. Borderline personality features in childhood: the role of subtype, developmental timing and chronicity of child maltreatment. Dev Psychopathol. (2014) 26:805–15. doi: 10.1017/S0954579414000406
25. Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Arch Gen Psychiatry. (1993) 50:975–90. doi: 10.1001/archpsyc.1993.01820240059008
26. Joyce PR, McKenzie JM, Luty SE, Mudler RT, Carter JD, Sullivan PF, et al. Temperament, childhood environment and pyschopathology as risk factors for avoidant and borderline personality disorders. Aust N Z J Psychiatry. (2003) 37:756–64. doi: 10.1080/j.1440-1614.2003.01263.x
27. Kaess M, Resch F, Parzer P, von Ceumern-Lindenstjerna IA, Henze R, Brunner R. Temperamental patterns in female adolescents with borderline personality disorder. J Nerv Ment Dis. (2013) 201:109–15. doi: 10.1097/NMD.0b013e31827f6480
28. Fossati A, Donati D, Donini M, Novella L, Bagnato M, Maffei C. Temperament, character, and attachment patterns in borderline personality disorder. J Pers Disord. (2001) 15:390–402. doi: 10.1521/pedi.15.5.390.19197
29. Cramer P. Childhood precursors of adult borderline personality disorder features: a longitudinal study. J Nerv Ment Dis. (2016) 204:494–9. doi: 10.1097/NMD.0000000000000514
30. Underwood MK, Beron KJ, Rosen LH. Joint trajectories for social and physical aggression as predictors of adolescent maladjustment: internalizing symptoms, rule-breaking behaviors, and borderline and narcissistic personality features. Dev Psychopathol. (2011) 23:659–78. doi: 10.1017/S095457941100023X
31. Vaillancourt T, Brittain HL, McDougall P, Krygsman A, Boylan K, Duku E, et al. Predicting borderline personality disorder symptoms in adolescents from childhood physical and relational aggression, depression, and attention-deficit/hyperactivity disorder. Dev Psychopathol. (2014) 26:817–30. doi: 10.1017/S0954579414000418
32. Lenzenweger MF, Cilcchetti D. Toward a developmental psychopathology approach to borderline personality disorder. Dev Psychopathol. (2005) 17:893–8. doi: 10.1017/s095457940505042x
33. Stepp SD, Scott LN, Jones NP, Whalen DJ, Hipwell AE. Negative emotional reactivity as a marker of vulnerability in the development of borderline personality disorder symptoms HHS public access. Dev Psychopathol. (2016) 28:213–24. doi: 10.1017/S0954579415000395
34. Tragesser SL, Solhan M, Brown WC, Tomko RL, Bagge C, Trull TJ. Longitudinal associations in borderline personality disorder features: diagnostic interview for borderlines-revised (DIB-R) scores over time. J Pers Disord. (2010) 24:377–91. doi: 10.1521/pedi.2010.24.3.377
35. Stepp SD, Olino TM, Klein DN, Seeley JR, Lewinsohn PM. Unique influences of adolescent antecedents on adult borderline personality disorder features. Pers Disord Theory, Res Treat. (2013) 4:223–9. doi: 10.1037/per0000015
36. Gratz KL, Tull MT, Reynolds EK, Bagge CL, Latzman RD, Daughters SB, et al. Extending extant models of the pathogenesis of borderline personality disorder to childhood borderline personality symptoms: The roles of affective dysfunction, disinhibition, and self- and emotion-regulation deficits. Dev Psychopathol. (2009) 21:1263–91. doi: 10.1017/S0954579409990150
37. Jovev M, Mckenzie T, Whittle S, Simmons JG, Allen NB, Chanen AM. Temperament and maltreatment in the emergence of borderline and antisocial personality pathology during early adolescence. J Can Acad Child Adolesc Psychiatry. (2013) 22:220–9.
38. Crawford TN, Cohen PR, Chen H, Anglin DM, Ehrensaft M. Early maternal separation and the trajectory of borderline personality disorder symptoms. Dev Psychopathol. (2009) 21:1013–30. doi: 10.1017/S0954579409000546
39. Craparo G, Faraci P, Fasciano S, Carrubba S, Gori A. A factor analytic study of the boredom proneness scale (BPS). Clin Neuropsychiatry. (2013) 10:164. doi: 10.1037/t32164-000
40. Godbout N, Briere J, Sabourin S, Lussier Y. Child sexual abuse and subsequent relational and personal functioning: the role of parental support. Child Abuse and Neglect. (2014) 38:317–25. doi: 10.1016/j.chiabu.2013.10.001
41. Barker-Collo SL. Adult reports of child and adult attributions of blame for childhood sexual abuse: predicting adult adjustment and suicidal behaviors in females. Child Abuse and Neglect. (2001) 25:1329–41. doi: 10.1016/s0145-2134(01)00278-2
42. Barnow S, Aldinger M, Arens EA, Ulrich I, Spitzer C, Grabe HJ, et al. Maternal transmission of borderline personality disorder symptoms in the community-based Greifswald family study. J Pers Disord. (2013) 27:806–19. doi: 10.1521/pedi_2012_26_058
43. Conway CC, Hammen C, Brennan PA. Adolescent precursors of adult borderline personality pathology in a high-risk community sample. J Pers Disord. (2015) 29:316–33. doi: 10.1521/pedi_2014_28_158
44. Stepp SD, Whalen DJ, Scott LN, Zalewski M, Loeber R, Hipwell AE. Reciprocal effects of parenting and borderline personality disorder symptoms in adolescent girls. Dev Psychopathol. (2014) 26:361–78. doi: 10.1017/S0954579413001041
45. Lyons-Ruth K, Brumariu LE, Bureau JF, Hennighausen K, Holmes B. Role confusion and disorientation in young adult-parent interaction among individuals with borderline symptomatology. J Pers Disord. (2015) 29:641–62. doi: 10.1521/pedi_2014_28_165
46. Vanwoerden S, Kalpakci A, Sharp C. The relations between inadequate parent-child boundaries and borderline personality disorder in adolescence. Psychiatry Res. (2017) 257:462–71. doi: 10.1016/j.psychres.2017.08.015
47. Herzog JI, Schmahl C. Adverse childhood experiences and the consequences on neurobiological, psychosocial, and somatic conditions across the lifespan. Front Psychiatry. (2018) 9:420. doi: 10.3389/fpsyt.2018.00420
48. Gabbard GO. Psychodynamic Psychiatry in Clinical Practice. 4th ed. Washington, DC: Amer Psychiatric Pub Inc (2014).
49. Gunderson JG. Borderline Personality Disorder: A Clinical Guide. Washington, DC: American Psychiatric Publishing Inc (2008). p. 22–41.
50. Geselowitz B, Whalen DJ, Tillman R, Barch DM, Luby JL, Vogel A. Preschool age predictors of adolescent borderline personality symptoms. J Am Acad Child Adolesc Psychiatry. (2021) 60:612–22. doi: 10.1016/j.jaac.2020.07.908
51. Guzder J, Paris J, Zelkowitz P, Marchessault K. Risk factors for borderline pathology in children. J Am Acad Child Adolesc Psychiatry. (1996) 35:26–33. doi: 10.1097/00004583-199601000-00009
52. Winsper C, Zanarini M, Wolke D. Prospective study of family adversity and maladaptive parenting in childhood and borderline personality disorder symptoms in a non-clinical population at 11 years. Psychol Med. (2012) 42:2405–20. doi: 10.1017/S0033291712000542
53. Ibrahim J, Cosgrave N, Woolgar M. Childhood maltreatment and its link to borderline personality disorder features in children: a systematic review approach. Clin Child Psychol Psychiatry. (2018) 23:57–76. doi: 10.1177/1359104517712778
54. Steine IM, Harvey AG, Krystal JH, Milde AM, Grønli J, Bjorvatn B, et al. Sleep disturbances in sexual abuse victims: a systematic review. Sleep Med Rev. (2012) 16:15–25. doi: 10.1016/j.smrv.2011.01.006
55. Horesh N, Ratner S, Laor N, Toren P. A comparison of life events in adolescents with major depression, borderline personality disorder and matched controls: a pilot study. Psychopathology. (2008) 41:300–6. doi: 10.1159/000141925
56. Biskin RS, Paris J, Renaud J, Raz A, Zelkowitz P. Outcomes in women diagnosed with borderline personality disorder in adolescence. J Can Acad Child Adolesc Psychiatry. (2011) 20:168–74.
57. Goodman M, Hazlett EA, Avedon JB, Siever DR, Chu K-W, New AS, et al. Anterior cingulate volume reduction in adolescents with borderline personality disorder and co-morbid major depression. J Psychiatr Res. (2011) 45:803–7. doi: 10.1016/j.jpsychires.2010.11.011
58. Venta A, Robyn Kenkel-Mikelonis B. Carla Sharp B. A preliminary study of the relation between trauma symptoms and emerging BPD in adolescent inpatients. Bull Menninger Clin. (2012) 76:130–46. doi: 10.1521/bumc.2012.76.2.130
59. Infurna MR, Brunner R, Holz B, Parzer P, Giannone F, Reichl C, et al. The specific role of childhood abuse, parental bonding, and family functioning in female adolescents with borderline personality disorder. J Pers Disord. (2016) 30:177–92. doi: 10.1521/pedi_2015_29_186
60. Kaplan C, Tarlow N, Stewart JG, Aguirre B, Galen G, Auerbach RP. Borderline personality disorder in youth: the prospective impact of child abuse on non-suicidal self-injury and suicidality. Compr Psychiatry. (2016) 71:86–94. doi: 10.1016/j.comppsych.2016.08.016
61. Rajan G, Syding S. Ljunggren · Gunnar, Wändell · Per, Wahlström L, Philips B, et al. Health care consumption and psychiatric diagnoses among adolescent girls 1 and 2 years after a first-time registered child sexual abuse experience: a cohort study in the Stockholm Region. Eur Child Adolesc Psychiatry. (2020) 1:3. doi: 10.1007/s00787-020-01670-w
62. Horesh N, Nachshoni T, Wolmer L, Toren P A. comparison of life events in suicidal and nonsuicidal adolescents and young adults with major depression and borderline personality disorder. Compr Psychiatry. (2009) 50:496–502. doi: 10.1016/j.comppsych.2009.01.006
63. Sengutta M, Gawe da Ł, Moritz S, Karow A. The mediating role of borderline personality features in the relationship between childhood trauma and psychotic-like experiences in a sample of help- seeking non-psychotic adolescents and young adults. Eur Psychiatry. (2019) 56:84–90. doi: 10.1016/j.eurpsy.2018.11.009
64. Turniansky H, Ben-Dor D, Krivoy A, Weizman A, Shoval G. A history of prolonged childhood sexual abuse is associated with more severe clinical presentation of borderline personality disorder in adolescent female inpatients-a naturalistic study. Child Abuse Negl. (2019) 98:104222. doi: 10.1016/j.chiabu.2019.104222
65. Johnson JG, Cohen P, Smailes EM, Skodol AE, Brown J, Oldham JM. Childhood verbal abuse and risk for personality disorders during adolescence and early adulthood. Compr Psychiatry. (2001) 42:16–23. doi: 10.1053/comp.2001.19755
66. Hildyard KL, Wolfe DA. Child neglect: developmental issues and outcomes. Child Abuse and Neglect. (2002) 26:679–95. doi: 10.1016/s0145-2134(02)00341-1
67. Johnson JG, Smailes EM, Cohen P, Brown J, Bernstein DP. Associations between four types of childhood neglect and personality disorder symptoms during adolescence and early adulthood: findings of a community-based longitudinal study. J Pers Disord. (2000) 14:171–87. doi: 10.1521/pedi.2000.14.2.171
68. Lyons-Ruth K, Bureau J-F, Holmes B, Easterbrooks A, Brooks NH. Borderline symptoms and suicidality/self-injury in late adolescence: prospectively observed relationship correlates in infancy and childhood. Psychiatry Res. (2013) 206:273–81. doi: 10.1016/j.psychres.2012.09.030
69. Gredler GR. Bullying at school: what we know and what we can do. Psychol Sch. (2003) 40:140–42. https://doi.org/10.1002/pits.10114
70. Crick NR, Grotpeter JK. Children's treatment by peers: victims of relational and overt aggression. Dev Psychopathol. (1996) 8:367–80. doi: 10.1017/S0954579400007148
71. Wolke D, Woods S, Bloomfield L, Karstadt L. The association between direct and relational bullying and behaviour problems among primary school children. J Child Psychol Psychiatry Allied Discip. (2000) 41:989–1002. doi: 10.1111/1469-7610.00687
72. Staebler K, Renneberg B, Stopsack M, Fiedler P, Weiler M, Roepke S. Facial emotional expression in reaction to social exclusion in borderline personality disorder. Psychol Med. (2011) 41:1929–38. doi: 10.1017/S0033291711000080
73. Wolke D, Schreier A, Zanarini MC, Winsper C. Bullied by peers in childhood and borderline personality symptoms at 11 years of age: A prospective study. J Child Psychol Psychiatry Allied Discip. (2012) 53:846–55. doi: 10.1111/j.1469-7610.2012.02542.x
74. Bozzatello P, Rocca P, Bellino S. Trauma and psychopathology associated with early onset BPD: an empirical contribution. J Psychiatr Res. (2020) 131:54–9. doi: 10.1016/j.jpsychires.2020.08.038
75. Stassen Berger K. Update on bullying at school: science forgotten? Dev Rev. (2007) 27:90–126. doi: 10.1016/J.DR.2006.08.002
76. King-Casas B, Sharp C, Lomax-Bream L, Lohrenz T, Fonagy P, Read Montague P. The rupture and repair of cooperation in borderline personality disorder. Science. (2008) 321:806–10. doi: 10.1126/science.1156902
77. Takizawa R, Maughan B, Arseneault L. Adult health outcomes of childhood bullying victimization: evidence from a five-decade longitudinal British birth cohort. Am J Psychiatry. (2014) 171:777–84. doi: 10.1176/appi.ajp.2014.13101401
78. Lieb K, Rexhausen JE, Kahl KG, Schweiger U, Philipsen A, Hellhammer DH, et al. Increased diurnal salivary cortisol in women with borderline personality disorder. J Psychiatr Res. (2004) 38:559–65. doi: 10.1016/j.jpsychires.2004.04.002
79. Rinne T, de Kloet ER, Wouters L, Goekoop JG, DeRijk RH, van den Brink W. Hyperresponsiveness of hypothalamic-pituitary-adrenal axis to combined dexamethasone/corticotropin-releasing hormone challenge in female borderline personality disorder subjects with a history of sustained childhood abuse. Biol Psychiatry. (2002) 52:1102–12. doi: 10.1016/s0006-3223(02)01395-1
80. Wingenfeld K, Driessen M, Adam B, Hill A. Overnight urinary cortisol release in women with borderline personality disorder depends on comorbid PTSD and depressive psychopathology. Eur Psychiatry. (2007) 22:309–12. doi: 10.1016/j.eurpsy.2006.09.002
81. Lupien SJ, Maheu F, Tu M, Fiocco A, Schramek TE. The effects of stress and stress hormones on human cognition: implications for the field of brain and cognition. Brain Cogn. (2007) 65:209–37. doi: 10.1016/j.bandc.2007.02.007
82. Lanius RA, Vermetten E, Pain C. The impact of early life trauma on health and disease: the hidden epidemic. The impact of early life trauma on health and disease: the hidden epidemic. Psychol Med. (2010) 41:665. doi: 10.1017/S0033291710002564
83. Berrebi AS, Fitch RH, Ralphe DL, Denenberg JO, Friedrich VL, Denenberg VH. Corpus callosum: region-specific effects of sex, early experience and age. Brain Res. (1988) 438:216–24. doi: 10.1016/0006-8993(88)91340-6
84. Teicher MH, Ito Y, Glod CA, Andersen SL, Dumont N, Ackerman E. Preliminary evidence for abnormal cortical development in physically and sexually abused children using EEG coherence and MRI. Ann N Y Acad Sci. (1997) 821:160–75. doi: 10.1111/j.1749-6632.1997.tb48277.x
85. de Bellis MD, Keshavan MS, Clark DB, Casey BJ, Giedd JN, Boring AM, et al. Developmental traumatology part II: brain development. Biol Psychiatry. (1999) 45:1271–84. doi: 10.1016/s0006-3223(99)00045-1
86. Bremner JD, Randall P, Vermetten E, Staib L, Bronen RA, Mazure C, et al. Magnetic resonance imaging-based measurement of hippocampal volume in posttraumatic stress disorder related to childhood physical and sexual abuse—a preliminary report. Biol Psychiatry. (1997) 41:23–32. doi: 10.1016/s0006-3223(96)00162-x
87. Stein MB, Koverola C, Hanna C, Torchia MG, McClarty B. Hippocampal volume in women victimized by childhood sexual abuse. Psychol Med. (1997) 27:951–9. doi: 10.1017/s0033291797005242
88. Driessen M, Herrmann J, Stahl K, Zwaan M, Meer S, Hill A, et al. Magnetic resonance imaging volumes of the hippocampus and the amygdala in women with borderline personality disorder and early traumatization. Arch Gen Psychiatry. (2000) 57:1115–22. doi: 10.1001/archpsyc.57.12.1115
89. Irle E, Lange C, Sachsse U. Reduced size and abnormal asymmetry of parietal cortex in women with borderline personality disorder. Biol Psychiatry. (2005) 57:173–82. doi: 10.1016/j.biopsych.2004.10.004
90. Herpertz SC, Dietrich TM, Wenning B, Krings T, Erberich SG, Willmes K, et al. Evidence of abnormal amygdala functioning in borderline personality disorder: a functional MRI study. Biol Psychiatry. (2001) 50:292–8. doi: 10.1016/s0006-3223(01)01075-7
91. Caspi A, McCray J, Moffitt TE, Mill J, Martin J, Craig IW, et al. Role of genotype in the cycle of violence in maltreated children. Science. (2002) 297:851–4. doi: 10.1126/science.1072290
92. Bulbena-Cabre A, Bassir Nia A, Perez-Rodriguez MM. Current knowledge on gene-environment interactions in personality disorders: an update. Curr Psychiatry Rep. (2018) 20:74. doi: 10.1007/s11920-018-0934-7
93. Wagner S, Baskaya Ö, Lieb K, Dahmen N, Tadić A. The 5-HTTLPR Polymorphism modulates the association of serious life events (SLE) and impulsivity in patients with borderline personality disorder. J Psychiatr Res. (2009) 43:1067–72. doi: 10.1016/j.jpsychires.2009.03.004
94. Wagner S, Baskaya Ö, Dahmen N, Lieb K, Tadić A. Modulatory role of the brain-derived neurotrophic factor Val 66Met polymorphism on the effects of serious life events on impulsive aggression in borderline personality disorder. Genes, Brain Behav. (2010) 9:97–102. doi: 10.1111/j.1601-183X.2009.00539.x
95. Martín-Blanco A, Ferrer M, Soler J, Arranz MJ, Vega D, Calvo N, et al. The role of hypothalamus–pituitary–adrenal genes and childhood trauma in borderline personality disorder. Eur Arch Psychiatry Clin Neurosci. (2016) 266:307–16. doi: 10.1007/s00406-015-0612-2
96. Perroud N, Zewdie S, Stenz L, Adouan W, Bavamian S, Prada P, et al. Methylation of serotonin receptor 3A in ADHD, Borderline personality, and bipolar disorders: Link with severity of the disorders and childhood maltreatment. Depress Anxiety. (2016) 33:45–55. doi: 10.1002/da.22406
97. Kuhlmann A, Bertsch K, Schmidinger I, Thomann PA, Herpertz SC. Morphometric differences in central stress-regulating structures between women with and without borderline personality disorder. J Psychiatry Neurosci. (2013) 38:129–37. doi: 10.1503/jpn.120039
98. Herman JL. Complex PTSD: a syndrome in survivors of prolonged and repeated trauma. J Trauma Stress. (1992) 5:377–91. https://doi.org/10.1002/jts.2490050305
99. World Health Organization. International Statistical Classification of Diseases and Related Health Problems 11th ed. Geneva: World Health Organization (2020).
100. Brewin CR, Cloitre M, Hyland P, Shevlin M, Maercker A, Bryant RA, et al. A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clin Psychol Rev. (2017) 58:1–15. doi: 10.1016/j.cpr.2017.09.001
101. van der Kolk BA. The trauma spectrum: the interaction of biological and social events in the genesis of the trauma response. J Trauma Stress. (1988) 1:273–90. https://doi.org/10.1002/jts.2490010302
102. van der Kolk BA, Hostetler A, Herron N, Fisler R. Trauma and the development of borderline personality disorder. Psychiatr Clin North Am. (1994) 17:715–30.
103. van Dijke A, Hopman JAB, Ford JD. Affect dysregulation, psychoform dissociation, and adult relational fears mediate the relationship between childhood trauma and complex posttraumatic stress disorder independent of the symptoms of borderline personality disorder. Eur J Psychotraumatol. (2018) 9:1400878. doi: 10.1080/20008198.2017.1400878
104. Frías Á, Palma C. Comorbidity between post-traumatic stress disorder and borderline personality disorder: a review. Psychopathology. (2015) 48:1–10. doi: 10.1159/000363145
105. Bardeen JR, Kumpula MJ, Orcutt HK. Emotion regulation difficulties as a prospective predictor of posttraumatic stress symptoms following a mass shooting. J Anxiety Disord. (2013) 27:188–96. doi: 10.1016/j.janxdis.2013.01.003
106. Orbach I, Mikulincer M, Gilboa-Schechtman E, Sirota P. Mental pain and its relationship to suicidality and life meaning. Suicide Life Threat Behav. (2003) 33:231–41. doi: 10.1521/suli.33.3.231.23213
Keywords: abuse, borderline personality disorder, etiopathogenesis, early onset, comorbidity, trauma
Citation: Bozzatello P, Rocca P, Baldassarri L, Bosia M and Bellino S (2021) The Role of Trauma in Early Onset Borderline Personality Disorder: A Biopsychosocial Perspective. Front. Psychiatry 12:721361. doi: 10.3389/fpsyt.2021.721361
Received: 06 June 2021; Accepted: 09 August 2021;
Published: 23 September 2021.
Edited by:
Maria Muzik, University of Michigan, United StatesReviewed by:
Jessica Riggs, University of Michigan, United StatesMadhavi Latha Nagalla, Pine Rest Christian Mental Health Services, United States
Copyright © 2021 Bozzatello, Rocca, Baldassarri, Bosia and Bellino. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Silvio Bellino, silvio.bellino@unito.it
 Paola Bozzatello
Paola Bozzatello Paola Rocca
Paola Rocca Lorenzo Baldassarri
Lorenzo Baldassarri Marco Bosia
Marco Bosia Silvio Bellino
Silvio Bellino