- 1Department of Psychology, California State University, Long Beach, Long Beach, CA, United States
- 2Department of Psychology, University of South Carolina, Columbus, SC, United States
- 3College of Nursing, University of South Carolina, Columbus, SC, United States
- 4MAP Centre for Urban Health Solutions, St. Michael's Hospital, Unity Health, Toronto, ON, Canada
- 5Department of Psychology, University of California, Los Angeles, Westwood, CA, United States
Early paternal involvement in infant care is beneficial to child and maternal health, and possibly for paternal mental health. The purpose of the present study was to examine the relationship between fathers’ involvement in early infant parenting and their depressive symptoms during the infant’s first year in a sample of 881 low-income Black, Hispanic, and White fathers recruited from five sites in the United States (urban, mixed urban/suburban, rural). Home interviews at 1 month after birth assessed three concepts based on prior research and community input: (1) time spent with the infant, (2) parenting self-efficacy, (3) material support for the baby. Paternal depressive symptoms at 1, 6, and 12 months after the birth of a child were assessed with the Edinburgh Postpartum Depression Scale. Generalized estimating equations tested whether the three indicators of father involvement at 1 month after birth predicted lower subsequent paternal depressive symptoms controlling for social and demographic variables. For fathers, greater time spent with the infant, parenting self-efficacy, and material support were all significantly associated with lower paternal depressive symptoms during the first year. When risk of depression (scores > 9) was examined, only parenting self-efficacy among fathers was associated with higher likelihood of clinical depression. Findings have implications for future research on mechanisms linking paternal involvement and paternal mental health, and for possible paid paternal leave policies in the future.
Introduction
Paternal depressive symptoms following the birth of a child are now a topic of increasing interest (1, 2). Estimates from three meta-analyses indicate that approximately 8 to 10 percent of men experience depression during the transition period to parenting and during early fatherhood (3–5), with the highest prevalence at 3 to 6 months after birth (3, 4). The prevalence of prenatal and postnatal depression among fathers is approximately twice as high as the prevalence of depression among men in general (6). The substantial proportion of fathers experiencing postpartum depression has important implications not only for fathers, who deserve attention, but also for maternal and child health and well-being (7, 8). Fathers often exert a strong influence on family life and functioning (9), and paternal depressive symptoms have been associated with adverse child and maternal mental health outcomes such as depression and psychiatric disorders (4, 10–13). The present study incorporates fathers and their experiences into our understanding of the family unit during the time following a birth.
One factor that is implicated in the phenomenon of paternal depression is low levels of paternal involvement with children (14). The meaning and characterization of paternal involvement has evolved over the past few decades with early perspectives emphasizing the father’s role as a moral teacher and provider (15–17) to more contemporary perspectives emphasizing the importance of actual time fathers are involved in the different domains of accessibility, engagement, and responsibility (16, 18). Accessibility reflects the fathers’ presence and availability to the child irrespective of the type or quality of actual interactions. Engagement reflects the ways in which fathers directly interact with the child including time spent in activities such as caregiving and play. Responsibility reflects involvement with supervisory parenting activities such as scheduling medical appointments and choosing a daycare. The present study focuses specifically on more contemporary paternal involvement constructs that incorporate paternal engagement and responsibility for the infant.
Previous research has demonstrated that greater paternal involvement is associated with positive family outcomes. Specifically, greater paternal involvement has been associated with lower maternal depressive symptoms (19, 20) and higher maternal life satisfaction (19). During infancy, greater paternal involvement has also been associated with lower rates of infant mortality (21), more secure father-child attachment (22), lower likelihood of infant cognitive delay (23) and higher child IQ at three years of age (24). In addition, investigators have shown that paternal depression, maternal depression, and the amount of time fathers spend interacting with their children during infancy reduces child behavioral problems in kindergarten (25). The conceptualization of fatherhood used in the current study may be limited to fathers in Western cultures. What constitutes acceptable levels of paternal involvement may also differ depending on cultural background (26, 27). Even given these cultural differences, previous research clearly demonstrates that paternal involvement may play an important role in adjustment for the mother and the child.
To our knowledge, no study has examined the link between early paternal involvement and later paternal depressive symptoms following the birth of a child. Previous studies have examined the associations between father involvement and depressive symptoms using cross-sectional study designs. One study of preteen sons of nonresidential Black fathers found that lower paternal involvement was cross-sectionally associated with higher levels of paternal depressive symptoms in controlled analyses [e.g., (28)]. Furthermore, a recent study reported that fathers who were depressed were more withdrawn when playing with their infants in comparison to non-depressed fathers (29), and were more likely to neglect their children (30). Another study reported that paternal depressive symptoms were not associated with paternal involvement such as caregiving and play time (31). Thus, it is not known whether father involvement in early infancy has protective benefits with respect to later paternal depressive symptoms, during the year following a child’s birth.
Based on previous conceptualizations of father involvement, this study focused on three aspects of involvement – the amount of time fathers spent with the infant, parenting self-efficacy, and the father’s provision of material support for the baby– in predicting paternal depression over the first year after the birth of a child.
Time Spent With New Infant
Fathers who are unable to spend enough time with the infants may be at increased risk of feelings of sadness or dissatisfaction over the early years of their children’s lives—especially in the first year when infants grow and change so much (32). Time spent with their children may be particularly relevant for low-income fathers, as these fathers emphasize the importance of “being there” for their children even when direct contact is infrequent due to social, economic, and other barriers (33). Many fathers also view the provider role as providing material support such as money and supplies, in addition to spending time with their children (33). Although the amount of time that fathers spend with their children does not reflect the nature and quality of father-child interactions (16), the amount of time fathers spend with their infants is a more objective indicator of father accessibility and a precondition for types of father involvement. Several previous investigators have assessed time that fathers were engaged with their infants. However, few have examined the associations of time spent with infants and paternal (or any family member’s) health-related outcomes (17, 34).
Parenting Self-Efficacy
Parenting self-efficacy, or self-confidence, which reflects a father’s ability to care for offspring, is an important determinant of paternal involvement (17, 35). To our knowledge, no study has evaluated whether parenting self-efficacy is related to depressive symptoms over time in low-income fathers from racially and ethnically diverse backgrounds. One longitudinal study of 86 fathers from the first trimester to 6 months after the birth of a child found that greater parenting self-efficacy was correlated with lower depressive symptoms (36). Cross-sectionally, parenting self-efficacy has been positively associated with father involvement (37, 38). Self-efficacy is important because it may increase a father’s level of involvement, which in turn may lead to stable parenting, and better paternal mental health outcomes. Thus, the present study incorporated a self-efficacy measure of father involvement to further our understanding of paternal well-being in this longitudinal study.
Material Support
Consistent with a historical perspective on fathers (17), scholars have argued that the procurement of economic resources and being a provider for the family are also important (39), and especially when fathers and mothers are not in an ongoing marital or close relationship. Others have noted the importance of financial support as being a form of paternal involvement within the responsibility domain (18) and have suggested that provision of material support by fathers is critical aspect of father involvement (40).
The present study extends our understanding of how early father involvement relates to paternal depressive symptoms longitudinally within a large, racially and ethnically diverse sample of low-income fathers. While it is expected that parenting self-efficacy, time spent with infant, and provision of material support are intercorrelated to some extent, these concepts reflect distinct aspects of paternal involvement. Therefore, in this study, we evaluated whether time spent with a new infant, parenting self-efficacy, and material support at 1 month after the birth of a child are associated with paternal depressive symptoms over the first 12 months of parenting among fathers, an understudied population. Specifically, it was hypothesized that 1 month after the birth of a child, more time spent with infants, greater parenting self-efficacy, and more material support provided for the child would predict fewer depressive symptoms in fathers over the first year after a child’s birth.
Methods
Community Child Health Network Procedure
The Community Child Health Network (CCHN) is a multi-site network of interdisciplinary researchers funded by the Eunice Kennedy Shriver National Institute of Child and Health Development to investigate biopsychosocial mechanisms underlying racial/ethnic disparities in maternal and child health (41). Researchers used community-based participatory research methods, which involves collaborations with members of the community through every phrase of research from planning to dissemination in order to examine risk and resilience in low-income mothers and fathers in five sites across the United States (Los Angeles, California; Washington, D.C.; Baltimore, Maryland; Lake County, Illinois; several rural counties in North Carolina). The first three sites (Los Angeles, Washington D.C., and Baltimore) were urban environments, Lake County was a suburban environment, and the counties in North Carolina were rural sites. Researchers received IRB approval at each study site.
Mothers were recruited in the hospital after the birth of their child in four sites (Los Angeles, Lake County, Baltimore, and Washington D.C.) and in prenatal clinics in one site (North Carolina). Mothers were eligible if they were African American, Latina, or non-Hispanic White. Fathers were interviewed only if the mothers gave permission to the researchers to contact the fathers. Then, fathers were approached and invited to participate in the study. All procedures for mothers and fathers were approved by the various hospital and university institutions, and informed consent procedures were followed to enroll fathers and mothers into the study. Recruiters and interviewers were trained staff and research assistants from the partnered academic and community institutions.
Mothers and fathers were interviewed separately in their homes at 1 month (T1), 6 months (T2), and 12 months after the birth of a child (T3) [For further details on CCHN study, see (41, 42)]. The current study focuses on the subset of fathers who completed interviews at 1 month (T1) and 12 months (T3) after their child’s birth.
Participants
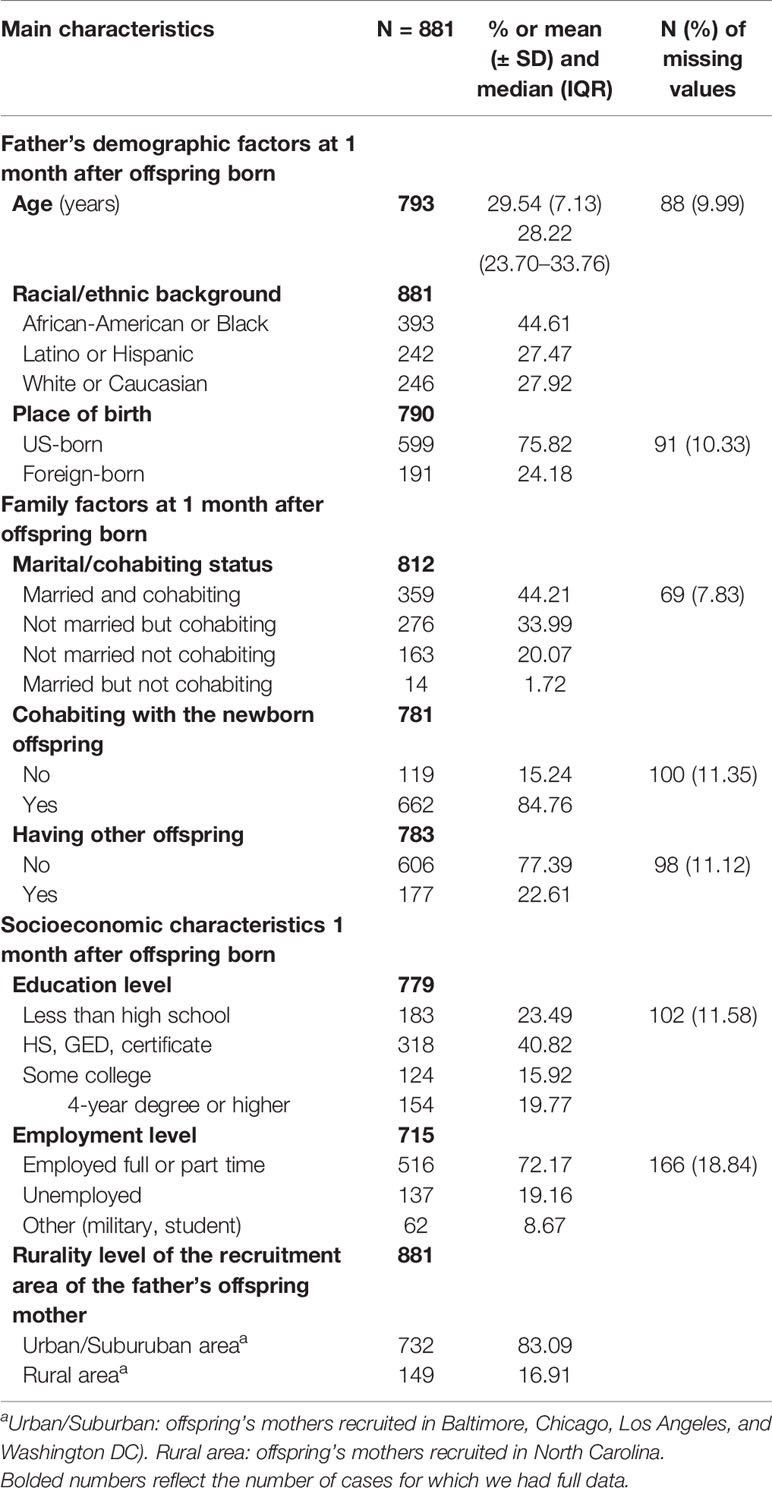
At 1 month (T1), 2,510 mothers agreed to participate. Of these, 1,923 gave permission to contact fathers and of those, 1,758 fathers agreed to participate. This group was comprised of fathers from diverse racial/ethnic backgrounds, however, due to small subgroup sizes, multi-racial fathers (n = 38), Asian-American and Pacific Islander fathers (n = 14), and fathers for whom race/ethnicity was missing and could not be determined (n = 37) were dropped from analyses leaving a sample size of 1,669. Of these, 53 percent (n = 881) completed the T3 depressive symptoms measure. Thus, the final sample size is 881 fathers. Descriptive characteristics including age, racial/ethnic background, marital and cohabitation status, levels of education, employment status, and site are reported in Table 1.
Analyses were conducted to determine whether there were any significant differences between the 881 Black, Latino, and White fathers in the current study who completed the T3 depressive symptoms measure and the 788 Black, Latino, and White fathers who did not. Independent samples t-tests revealed no significant differences between these groups of fathers on employment status, whether the father had prior children, parenting self-efficacy, time spent with infant, material support for the baby, or depressive symptoms at T1 or T2. However, fathers who completed the T3 depressive symptoms measure were significantly older (t (1,181) = 3.68, p <.001) and had more years of education (t (1,313) = 3.24, p <.01), compared to fathers who did not complete the T3 measure of depressive symptoms. Chi-square analyses found that fathers who were White (X2 (2, N = 1,669) = 16.79, p <.001), from Chicago (X2 (4, N = 1,659) = 36.03, p <.001), married to their baby’s mother (X2 (1, N = 1,467) = 26.89, p <.001), and cohabiting with their baby’s mother (X2 (1, = 1,413) = 16.21, p <.001) were significantly more likely to complete the T3 depressive symptoms measure than Black fathers, fathers from Los Angeles, unmarried fathers, and non-cohabiting fathers, respectively.
Measures
Demographic Data
Several socio-demographic characteristics were considered in this study as covariates including race/ethnicity, paternal age, place of birth (foreign-born vs. U.S. born), marital and cohabitation status with the baby’s mother, cohabitation status with the baby, level of education, employment status, and type of recruitment site (rural vs. not rural).
Father Involvement Measures
The measures for fathers were designed by a CCHN subcommittee of researchers and community partners including experts on father research. The work was informed by the Fragile Families and Child Well-Being Study, a longitudinal birth cohort study that followed nearly 4,900 families in large U.S. cities between 1998 and 2000 (43). All father measures used in this study were adapted from instruments in the Fragile Families and Child Well-Being study and provided to CCHN by members of the FFCWS team. Following review by a CCHN community-partnered measurement subcommittee and piloting a subset of items were used in this study.
Time Spent With Infant
Fathers responded to four items about the time they spent with their infants: 1) On an average weekday from Monday to Friday, do you spend any waking hours with [BABY]? 2) On an average weekday from Monday to Friday, do you spend time alone with [BABY]? 3) On an average weekend day meaning Saturday and Sunday, do you spend any waking hours with [BABY]? 4) On an average weekend day meaning Saturday and Sunday, do you spend time alone with [BABY]? Responses to each question were 0 (no) or 1 (yes) and were summed. Scores range from 0 to 4 and a higher score indicates more time spent with the infant.
Parenting Self-Efficacy
Paternal self-efficacy in parenting tasks was measured with six items. This scale was adapted from the FFCWS. In the present study, fathers were asked “how confident or comfortable you feel when you” 1) hold baby, 2) put baby to sleep, 3) wash or bathe baby, 4) change baby’s diaper, 5) feed baby, and 6) soothe baby when he/she is upset. Responses range from 1 (not at all) to 4 (very much). Responses were averaged with higher scores indicative of greater parenting self-efficacy. Cronbach’s alpha coefficient for these items for the full sample of fathers at 1 month was.68.
Material Support
A total of 10 items were used to measure the degree of material support fathers provided for their baby. Fathers reported how often they provided a) baby clothing, b) medicine for baby, c) baby furniture or equipment, d) childcare items, such as diapers, baby wipes, e) food, f) babysitting, g) money, h) health insurance, i) toys, and j) other. Possible responses were 0 (no), 1 (yes, occasionally), and 2 (yes, regularly). Scores were summed and range from 0 to 20. Higher scores reflect greater material support. Cronbach’s alpha was.77.
Depressive Symptoms Measures
The primary outcome was the fathers’ depressive symptoms scores, which were measured with the 10-item Edinburgh Postpartum Depression Scale administered at 1, 6, and 12 months after the birth of the child. This scale was originally designed for use with mothers but has been validated in fathers (44) as well as racial/ethnic minorities (45). Responses range from 0 (no, not at all) to 3 (yes, quite a lot). The response values were summed into an overall score, which in our study population ranged from 0 to 20. Higher scores indicate greater depressive symptoms. This scale had good reliability at T1 (Cronbach’s alpha = .78) and T3 (Cronbach’s alpha = 80).
Depressive symptoms were also examined in exploratory analyses using a cutoff for likely depressive illness. Researchers have used different scale cut-offs to indicate possible or probable diagnosis of depression including over 8 (46), over 9 (44, 47), and over 10 (48). In the current study, the most conventional cut-off score of ≥ 9 was used.
Data Analysis Plan
All analyses were performed at a 95% confidence interval using Stata Software (version 16). First, descriptive statistics were computed for demographic and socioeconomic characteristics as well as the fathers’ parenting involvement measures and depression scores. Second, we conducted preliminary analyses of the associations between the main three father involvement measures and depression values over the one-year follow-up period using the Generalized estimating equation [GEE; (49)] which accounts for repeated measures. Some study variables had incomplete or missing data (see Supplementary Table 1), ranging from 8% (marital and cohabitation status) to depressive symptoms at T2 (25%). Hence, we imputed missing values using Multiple Imputation (MI) via chained equations (50). We compared the distribution and proportion of the observed, imputed, and completed values (51) which showed good appropriateness of the imputed values (see examples of the comparison in Supplementary Figures 1–3, and Supplementary Tables 2–8). Third, we repeated the analysis with the imputed data to test the associations between each of the father’s parenting involvement measures (material support, parenting self-efficacy, and time spent with infant) with the continuous depression scale scores and the dichotomous depression cut-off (≥ 9). These data are presented and discussed in the present paper. We fitted the GEE models with the Gaussian family, Identity link, and exchangeable correlation with robust covariance when the EPDS scale scores were analyzed as outcomes. We fitted the GEE models with Binomial family, Logit link, and exchangeable correlation with robust covariance when the nine-cut-off values of the EPDS scale were analyzed as an outcome. We adjusted the crude association (Model 1) for each fathers parenting measures with the depression outcomes (EPDS score and nine-cut-off of EPDS scale values) in the following core adjusted models: Model 2, adjusted for age, and racial/ethnic background; Model 3, added the marital/cohabiting status, and having other offspring; Model 4, introduced educational level; Model 5, added rurality level of the recruitment area of the father’s offspring mother. Due to multi-collinearity, in Adjusted Model 6, we replaced the marital/cohabiting status variable of Model 5 with cohabiting status with the new-born offspring. In Model 7, we substituted the educational level variable of Model 5 with employment status. Finally, in Model 8, we replaced the race/ethnicity variable of Model 5 with place of birth. We performed these variable substitutions as these variables are too highly correlated to include in the same model. Further, each of the substituted variables may have different confounding effects on the assessed association.
Finally, we tested potential interaction effects between three parenting involvement measures using three-way interaction terms (Material support*Self-efficacy*Time spent with Infant). Since the interaction terms were not statistically significant (p > 0.05), we present the final models without interaction factors.
Results
Descriptive Statistics of Main Study Variables
Table 2 displays the descriptive statistics for the parental involvement measures and depression symptoms scores variables. On average, fathers had relatively high score values on parenting self-efficacy (M = 3.61, SD = .46), with scores reflecting that fathers feel “pretty much” to “very much” confident or comfortable in executing new-born offspring’s tasks. For the provision of material support to the newborn, the mean was 14.29 (SD = 3.97), showing that fathers provided support for the infant between occasionally and regularly. The majority of fathers (63%) reported spending waking hours with their children on weekdays and weekends and alone time with their children on weekdays and weekends. The average father’s scores on the depressive symptoms’ scales over the first year of parenting ranged from 3.71 at 1 month to 4.07 at 12 months after the child was born. Based on the cut-off of 9, the percentage of fathers with scores suggestive of clinical depression was 10%, 15%, and 12% at T1, T2, and T3, respectively.
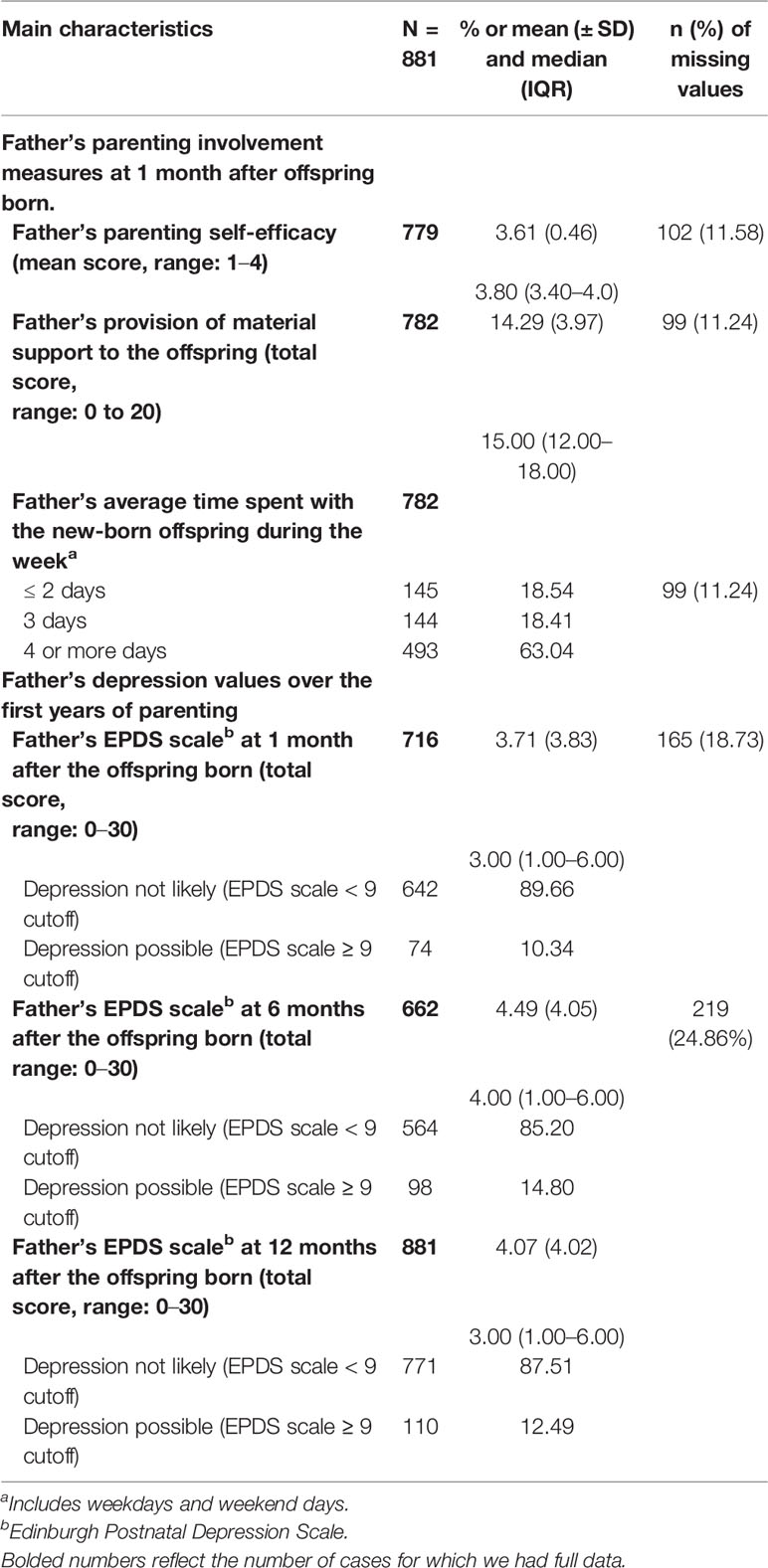
Table 2 Descriptive Characteristics of fathers’ parenting measures scores and depression symptoms scores (observed data).
Correlations Between Father Involvement Variables
Pearson’s correlation coefficients showed significant but weak associations among the father involvement variables. Greater parenting self-efficacy was positively correlated with greater provision of tangible support (r = .18) and more time spent with the infant (r = .18). In addition, greater tangible support was also associated with more time spent with infant (r = .18).
Fathers’ Parenting Self-Efficacy and Depressive Symptoms Scores
The unadjusted and adjusted associations of fathers’ parenting self-efficacy scores at 1 month after the offspring born with their depression scores (EPDS scale, range 0–20) over the first year of parenting are presented in Table 3. A one-point increase in the fathers’ self-efficacy score was significantly associated with lower values of the EPDS scale, even when adjusted for age, racial/ethnic background, marital/cohabiting status, having other offspring, educational level, and rurality level of the recruitment area of the father’s offspring mother (Table 3, Model 5=Adjusted coefficient and 95% CI: −1.652, −2.203 to −1.101). Similar results were observed when accounting for cohabiting with the new-born offspring (Table 3, Model 6), employment status (Table 3, Model 7), and place of birth (Table 3, Model 8).
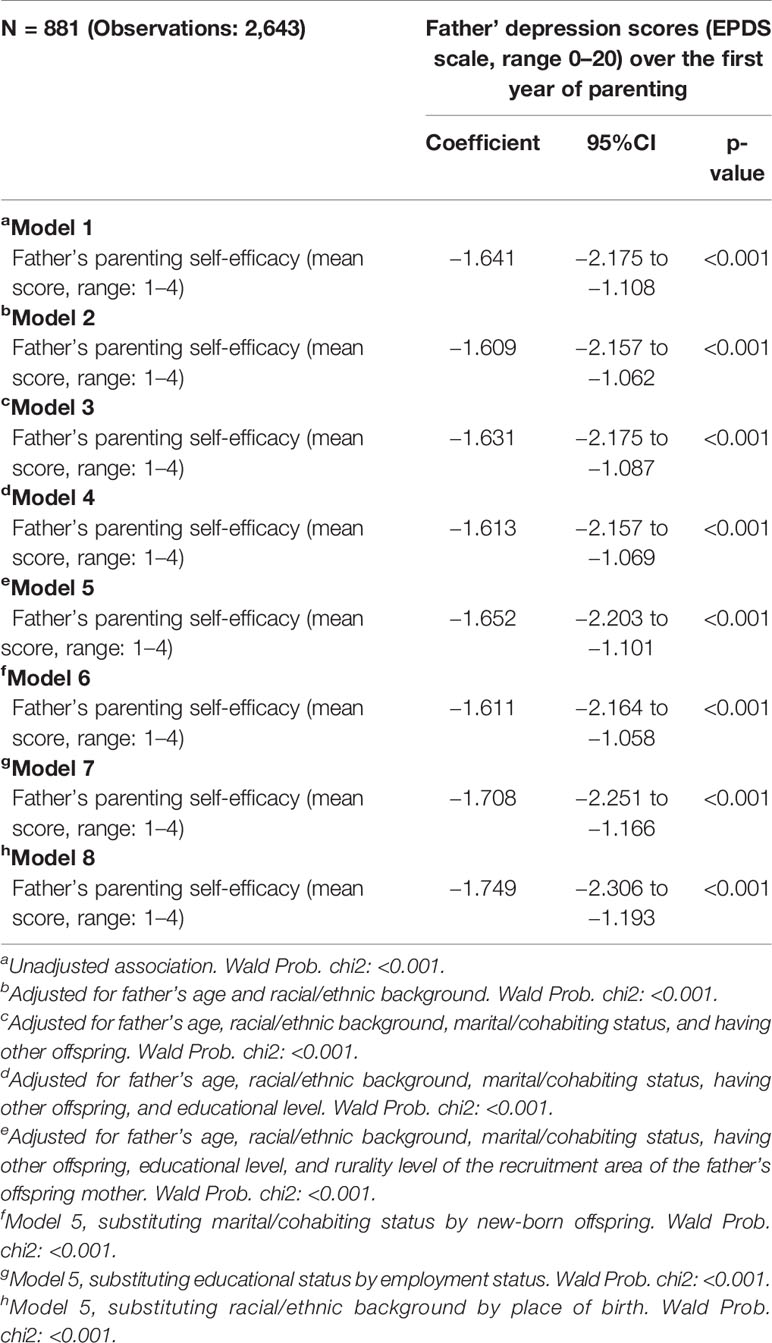
Table 3 Unadjusted and adjusted associations between father’s parenting self-efficacy with depression scores (EPDS scale) over the first year of parenting (completed imputed data).
Fathers’ Time Spent With the Newborn During the Week and Depressive Symptoms Scores
Table 4 shows the unadjusted and adjusted association between time spent with the new-born during the week at 1 month after the offspring born and depression scores over the first years of parenting. After adjusting for age, racial/ethnic background, marital/cohabiting status, having other offspring, educational level, and rurality level of the recruitment area of the offspring mother, spending 4-days or more with the new-born child was significantly associated with lower depression scores (Table 4, model 5=Adjusted coefficient and 95% CI: −0.647, −1.274 to −0.021). Although this association was smaller in effect size when accounting for cohabiting status with the baby (Table 4, model 6), it remained significant when controlling for employment (Table 4, model 7), and place of birth (Table 4, model 8).
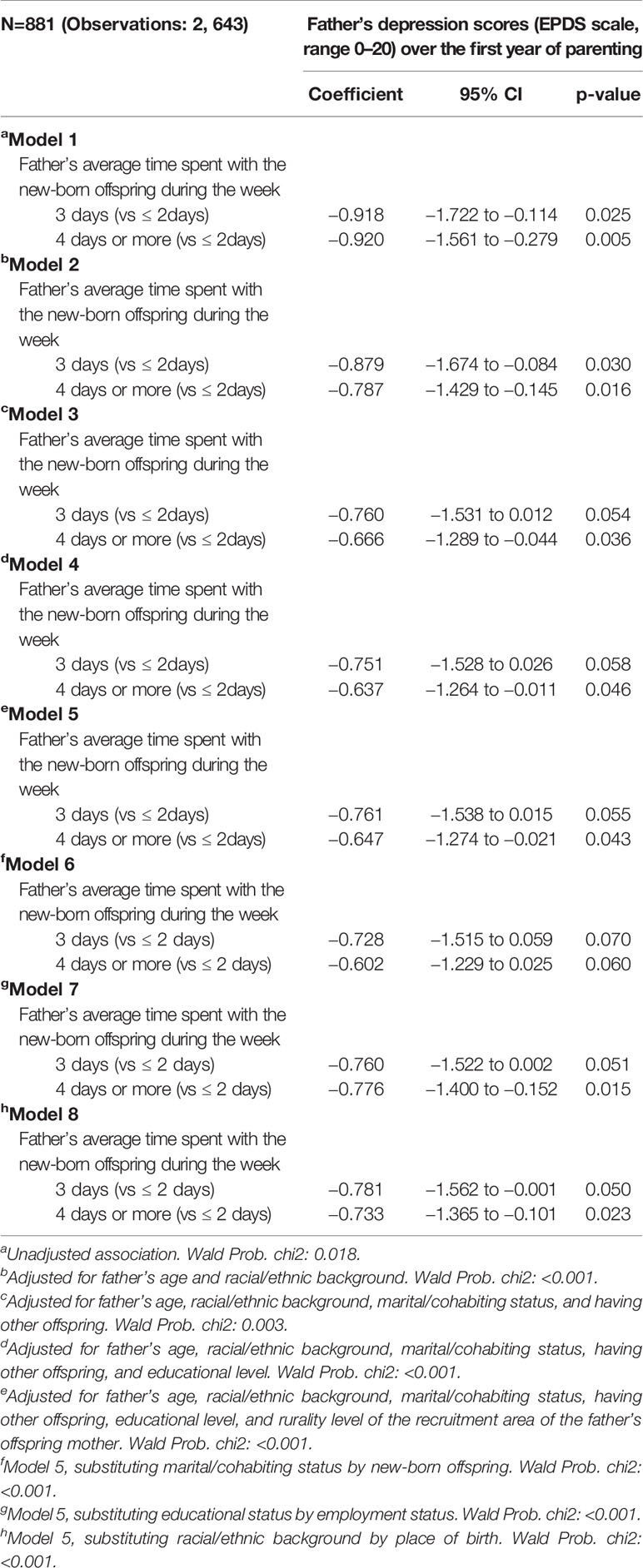
Table 4 Unadjusted and adjusted associations between the father’s average time spent with the new-born offspring during the week with depression scores (EPDS scale) over the first year of parenting (completed imputed data).
Fathers’ Provision of Material Support to the Newborn and Depressive Symptoms Scores
Table 5 displays the unadjusted and adjusted associations of fathers’ provision of material support score at 1 month after the offspring born with their depression scores (EPDS scale, range 0–20) over the first year of parenting. Greater material support was associated with lower depressive symptoms after accounting for age and racial/ethnic background (Table 5, model 2, coefficient and 95% CI: −0.109 to −0.172 to −0.046), marital/cohabiting status and having other children (Table 5, model 3, coefficient and 95% CI: −0.086, −0.146 to −0.025), educational level (Table 5, model 4, coefficient and 95% CI: −0.080, −0.142 to −0.019), and rurality level of the recruitment area (Table 5, model 5, coefficient and 95% CI: −0.081, −0.143 to −0.020). Similar estimations were observed when accounting for cohabiting with the new-born offspring (Table 5, model 6), employment status (Table 5, model 7), and place of birth (Table 5, model 8).
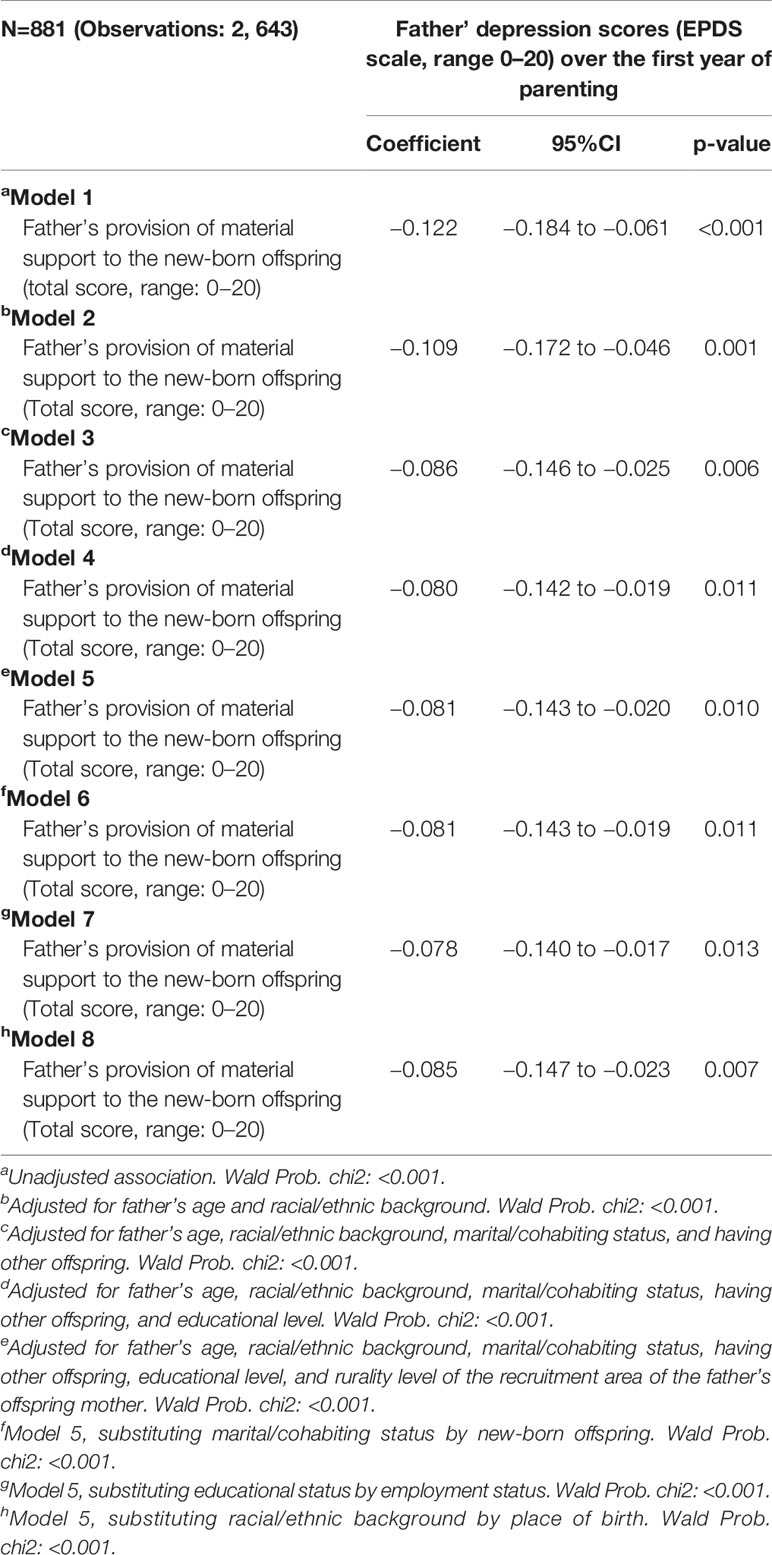
Table 5 Unadjusted and adjusted associations between father’s provision of material support to the offspring with depression scores (EPDS scale) over the first year of parenting (completed imputed data).
Father Involvement Measures and the Likelihood for Depression
Figure 1 displays the unadjusted and adjusted association of father parenting self-efficacy scores in executing new-born offspring’s tasks (Figure 1A), provision of material support to the new-born child (Figure 1B) and spent four or more days per week with their new-born child (Figure 1C) with the likelihood of depression using the apriori cutpoint (EPDS score: ≥ 9) over the first years of parenting. After controlling for all demographic, family, and socioeconomic factors, as well as rurality status of the recruitment area of the offspring mother, only higher values of father parenting self-efficacy scores were negatively associated with the likelihood of depression over the first year of parenting (Figure 1A). Father’s provision of material support to the new-born offspring and time spent with the new-born were not statistically significant after controlling for the covariates (Figures 1B, C).
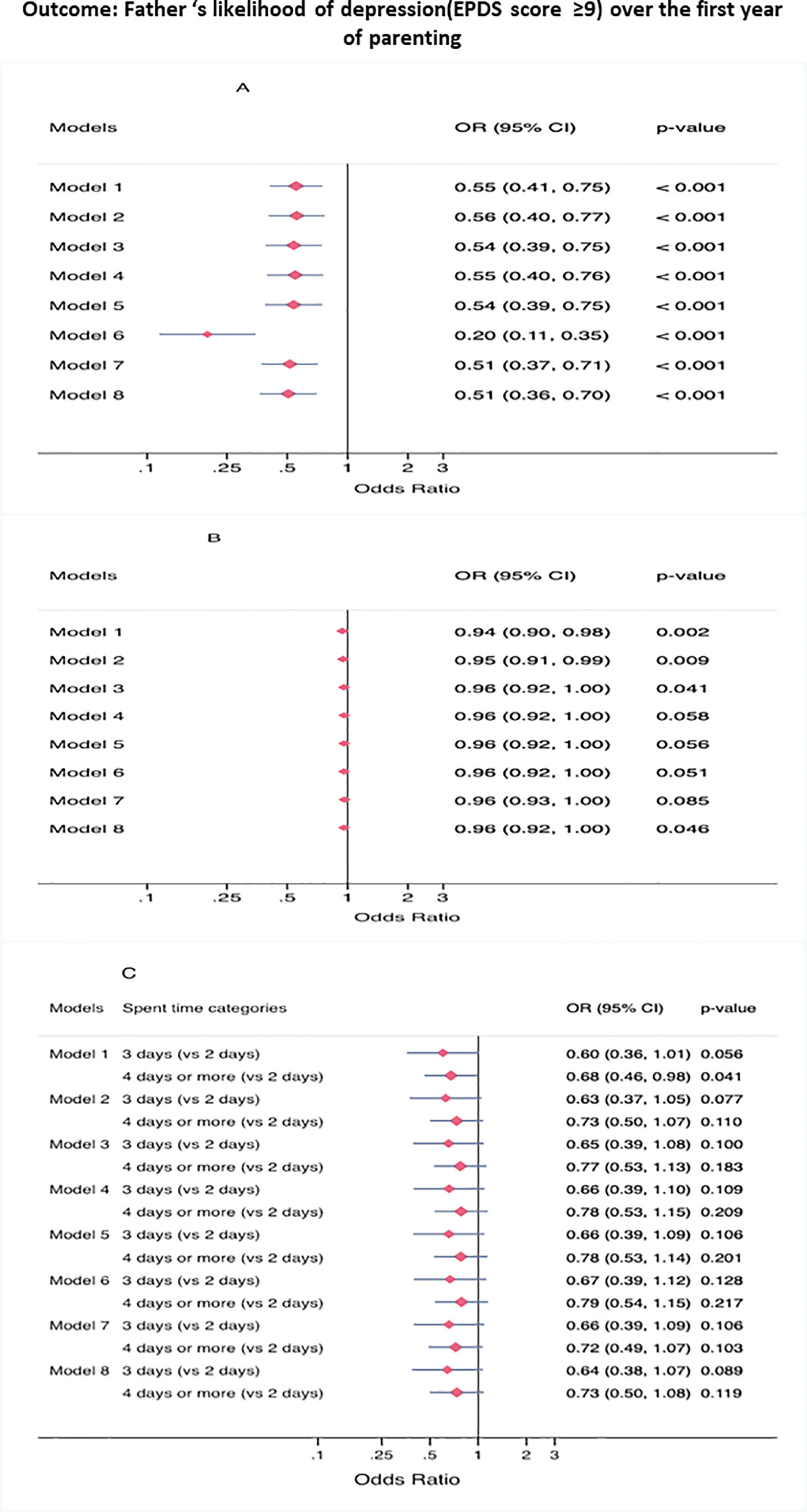
Figure 1 (A) Exposure: parenting self-efficacy, (B) Exposure: provision of material support, (C) Exposure: father's weekly time spent with the new-born. Unadjusted and adjusted associations of Father’s parenting self-efficacy, fathers’ provision of material support to the new-born, father’s average time spent with the new-born during the week with the EPDS scale ≥ 9 cut-off over the first year of parenting (completed imputed data, N=881, observations: 2,643). Model 1: Unadjusted association. Model 2: Adjusted for father's age and racial/ethnic background. Model 3: Adjusted for father's age, racial/ethnic background, marital/cohabiting status, and having other offspring. Model 4: Adjusted for father's age, racial/ethnic background, marital/cohabiting status, having other offspring, and educational level. Model 5: Adjusted for father's age, racial/ethnic background, marital/cohabiting status, having other offspring, educational level, and rurality level of the recruitment area of the father's offspring mother. Model 6: Model 5, substituting marital/cohabiting status by new-born offspring. Model 7: Model 5, substituting educational status by employment status. Model 8: Model 5, substituting racial/ethnic background by place of birth.
Discussion
This study examined the correspondence between early paternal involvement with a newborn infant at one month after birth and paternal depressive symptoms nearly one year later within a community sample of low-income and ethnically diverse fathers from five areas of the U.S. We found that fathers who spent more time with their infants, had greater parenting self-efficacy, and provided more material support for the baby one month after the birth reported significantly lower depressive symptoms when the child was one year of age. To the best of our knowledge, this study is the first to show longitudinal associations between greater perceived parenting self-efficacy and lower depressive symptoms, and specifically in low SES fathers from diverse racial/ethnic backgrounds. These findings suggest that paternal involvement is an important predictor of father’s mental health during the transition to fatherhood. Thus, parental involvement is an important for these men who were present at one month after birth, even though significant portions of them did not live with and were not married to the baby’s mother.
Parenting self-efficacy may be related to depressive symptoms as a result of higher parenting satisfaction. Previous research has shown that greater parenting self-efficacy is associated with greater parenting satisfaction in fathers (52), and has been associated with lower prevalence of paternal depressive symptoms (53). Fathers who feel competent as parents may therefore be more satisfied in their roles, and as a result, have fewer depressive symptoms. Research in fathers has also shown that when fathers rate their infants as less “fussy,” they report fewer depressive symptoms (54, 55), although other researchers have not replicated these findings (56). Additional research is needed to identify the underlying mechanisms through which greater parenting self-efficacy is associated with lower paternal depressive symptoms. Nonetheless, these findings suggest that it may be beneficial to foster the development of fathers’ parenting skills during prenatal and postnatal visits, as suggested by Salonen and colleagues (57). This may be particularly important for first time fathers who may have low parenting self-efficacy. Different online intervention programs have been successful in increasing parenting self-efficacy in fathers (58, 59). Adapting these programs and making them culturally sensitive and accessible to fathers from diverse racial/ethnic and socioeconomic backgrounds may be useful in reducing paternal depressive symptoms.
Regarding the link between parenting self-efficacy and parental depression, Jones and Prinz (60) note that “it is not altogether clear whether parenting self-efficacy functions consistently as an antecedent or contributor to parental depression, as a consequence of parental depression, or in a transactional relationship with parental depression. On the one hand, low parenting self-efficacy can contribute to maternal vulnerability for depression. Alternatively, depression can lead to lower maternal parenting self-efficacy” (p. 352). Although this was written with regard to mothers, it applies equally to fathers. Future research in this area should better understand the complex nature of their association.
Spending more time with a child one month after his or her birth was associated in this study with fewer paternal depressive symptoms nearly one year later. A potential explanation for this relationship may be related to employment. Fathers who work more hours and make more money spend less time with their child (61) and working more hours has been associated with greater paternal depressive symptoms (62, 63). Another study found that fathers who were better able to cope with major stressors in their life, such as work, spent more time with their kids (64). However, we accounted for employment status in our analysis and the observed associations between time spent with the newborn infant and lower father’s depression symptoms at one year remained significant.
Fathers who provided more material support in the form of diapers, toys, clothing, and food at one month after the birth of their baby had lower depressive symptoms at one year later. These findings held even after controlling for socioeconomic status and family factors such cohabitation with the child and with the child’s mother. Considerable research has demonstrated that the provider role is an important identity for father’s perceptions of themselves as well as mother’s perceptions of fathers (33, 39, 65–67). As a result, fathers who are less able to provide support, typically measured in the form of money, may have poor self-image, resulting in depressed mood. There is some evidence to support this as previous research indicated that fathers who were less able to provide economic support reported more depressive symptoms (68, 69). Previous research also demonstrates that when fathers provide greater financial and instrumental support, their children engage in fewer behavior problems (70, 71), which, in turn, may be associated with lower paternal depressive symptoms. Another reason why material support may be associated with fewer depressive symptoms is that material support is a type of social support well known to be beneficial not only to recipients but also to those providing it (72–74). A longitudinal study with over 700 families from diverse racial/ethnic backgrounds demonstrated bi-directional effects between paternal depressive symptoms and child behavior problems [e.g., internalizing behaviors, externalizing behaviors; (75)]. Thus, while paternal depressive symptoms affect children’s well-being, children’s well-being also affects paternal depressive symptoms.
There are a number of important implications for public health policies given the findings reported in this study. For example, greater time spent with the infant was associated with lower depressive symptoms, which has implication for designing policies to support opportunity to spend more time with their children without penalizing fathers who work. One avenue for increased time spent with kids may be paid paternal leave. Paid paternal leave for fathers of young children may be beneficial for the entire family unit (76). Research has shown that fathers in countries with more paternal paid leave spend significantly more time with their children (77) and fathers who take longer leave when their children are born spend more time on child-related tasks 9 months later (78). In light of the results of the current study, paid leave may also play a role in decreasing levels of paternal depressive symptoms, although more research is needed to elucidate this link and associated mechanisms.
There may several pathways linking early paternal involvement to later depressive symptoms in fathers. Specifically, lower depressive symptoms have been associated with changes in hormonal and neural functioning (79) and increased oxytocin levels (80). Oxytocin, known as the “love hormone” due to its links with social bonding and reproduction, increases in fathers following the birth of the child and after father-child interactions (81). Although we did not assess actual father-child interactions in our study, fathers who spend more time with their infants may have been engaging in positive interactions that affect hormonal and neural functioning, which may protect against future depressive symptoms. Furthermore, while the current study did not assess father-infant attachment, it may play a significant role in paternal mental health. Previous studies have demonstrated that stronger infant-parent attachment is associated with many positive outcomes for the child (82) and fathers feel valued when they have stronger attachments with their young children (83). In addition, father-infant attachment is associated with greater father involvement (84). Future research is needed to better elucidate these potential mechanisms.
The current study is not without limitations. Although we assessed different domains of involvement, we did not directly assess engagement with the child or quality of engagement in any way. Several research studies have shown that the quality and nature of time spent with the child is important for child well-being among non-resident fathers (85, 86). In addition, this study did not control for factors related to the child’s mother (e.g., maternal depression, serious health problems) that may have contributed to father’s depression, which was beyond the scope of this study and can be examined in future. A large body of research has shown that paternal depressive symptoms are associated with greater maternal depression (10) and poorer relationship quality (87, 88), and thus future research is warranted on this topic. The current study design also does not permit causal inferences although longitudinal data with temporal precedence were used. Although we used a repeated measure analysis approach to account for associations between depressive symptoms within subjects at different timepoints, we did not control for fathers’ depressive symptoms during pregnancy or history of depression as this information was not collected. Thus, there is the possibility that some fathers were already depressed before their child born, and a reverse causality may be present such that their depression led to lower involvement at 1 month. Finally, the fathers in this study only participated if the researchers received consent from the mother. Although the findings may not be generalizable to fathers in other socioeconomic and cultural settings, this study is among the first studies to involve a relatively large community sample of low-income fathers from diverse racial/ethnic backgrounds.
In conclusion, this study demonstrates that greater paternal involvement may benefit paternal mental health in low income ethnically and racially diverse fathers. Specifically, greater involvement in the form of time spent with the newborn, parenting self-efficacy, and ability to provide material support were all implicated as aspects of fathering that predicted lower depressive symptoms in fathers, and self-efficacy predicted risk of depressive disease. More research is needed to address these important constructs of father involvement to better understand how to improve paternal mental health and overall wellbeing. This study suggests that these factors associated with depression in fatherhood may be addressed by increasing skills in parenting, improving or enhancing ways for fathers to spend time with their children, as well as enabling fathers to provide material support for their children. Future researchers should consider designing and testing interventions to assess the impact of paid paternal leave and increases in parenting self-efficacy skills on paternal depression in ethnically diverse populations.
Data Availability Statement
Publicly available datasets were analyzed in this study. These data can be found here: https://dash.nichd.nih.gov/study/1649.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Review Boards for Johns Hopkins University, University of California, Los Angeles, Cedars-Sinai Medical Center, University of North Carolina, Northshore University Health System, Evanston Northwestern Healthcare Research Institute, Georgetown University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
OB, DW, DA, CD, and CM-L all contributed to the writing of this manuscript. CD and CCHN collected the original data. DW and DA wrote the Introduction. OB wrote the Methods section. CM-L wrote the Results sections. OB and CD wrote the Discussion section. CM-L conducted the statistical analysis of the paper.
Funding
This article is a product of the Child Community Health Research Network (CCHN). The CCHN was supported through cooperative agreements with the Eunice Kennedy Shriver National Institute of Child Health and Human Development (U HD44207, U HD44219, U HD44226, U HD44245, U HD44253, U HD54791, U HD54019, U HD44226-05S1, U HD44245-06S1, R03 HD59584) and the National Institute for Nursing Research (U NR008929). For more information on CCHN network sites, see https://www.nichd.nih.gov/research/supported/Pages/cchn.aspx. DA was supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under award number K23MD013899.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.578688/full#supplementary-material
References
1. Bamishigbin ON, Dunkel Schetter C, Guardino CM, Stanton AL, Schafer P, Shalowitz MU, et al. Risk, resilience, and depressive symptoms in low-income African American fathers. Cult Divers Ethnic Minor Psychol (2017) 23:70–80. doi: 10.1037/cdp0000088
2. Hammarlund K, Andersson E, Tenenbaum H, Sundler AJ. We are also interested in how fathers feel: A qualitative exploration of child health center nurses’ recognition of postnatal depression in fathers. BMC Pregnancy Childb (2015) 15:290. doi: 10.1186/s12884-015-0726-6
3. Cameron EE, Sedov ID, Tomfohr-Madsen L. Prevalence of paternal depression in pregnancy and the postpartum: An updated meta-analysis. J Affect Disord (2016) 206:189–203. doi: 10.1016/j.jad.2016.07.044
4. Paulson JF, Bazemore SD. Prenatal and postpartum depression in fathers and its association with maternal depression: A meta-analysis. JAMA (2010) 303:1961–9. doi: 10.1001/jama.2010.605
5. Rao W, Zhu X, Zong Q, Zhang Q, Hall BJ, Ungvari GS, et al. Prevalence of prenatal and postpartum depression in fathers: A comprehensive meta-analysis of observational studies. J Affect Dis (2020) 263:491–9. doi: 10.1016/j.jad.2019.10.030
6. Ferrari AJ, Somerville AJ, Baxter AJ, Norman R, Patten SB, Vos T, et al. Global variation in the prevalence and incidence of major depressive disorder: A systematic review of the epidemiological literature. Psychol Med (2013) 43:471–81. doi: 10.1017/S0033291712001511
7. Bond MJ. The missing link in MCH: Paternal involvement in pregnancy outcomes. Am J Mens Health (2010) 4:284–6. doi: 10.1177/1557988310384842
8. Lu MC, Jones L, Bond MJ, Wright K, Pumpuang M, Maidenberg M, et al. Where is the F in MCH? Father involvement in African American families. Ethnic Dis (2010) 20:S2–49.
9. Day RD, Lamb ME. Conceptualizing and measuring father involvement: Pathways, problems, and progress. In: Day RD, Lamb ME, editors. Conceptualizing and Measuring Father Involvement. Mahwah, New Jersey: Lawrence Eribaum Associates (2004). p. 1–15.
10. Goodman JH. Paternal postpartum depression, its relationship to maternal postpartum depression, and implications for family health. J Adv Nurs (2004) 45:26–35. doi: 10.1046/j.1365-2648.2003.02857.x
11. Saxbe DE, Dunkel Schetter C, Guardino CM, Ramey SL, Shalowitz MU, Thorp J, et al. Sleep quality predicts persistence of parental postpartum depressive symptoms and transmission of depressive symptoms from mothers to fathers. Ann Behav Med (2016) 50:862–75. doi: 10.1007/s12160-016-9815-7
12. Ramchandani P, Stein A, Evans J, O’Connor TG, the ALSPAC study team. Paternal depression in the postnatal period and child development: A prospective population study. Lancet (2005) 365:2201–5. doi: 10.1016/S0140-6736(05)66778-5
13. Ramchandani PG, Stein A, O’Connor TG, Heron J, Murray L, Evans J. Depression in men in the postnatal period and later child psychopathology: A population cohort study. J Am Acad Child Adolesc Psychiatry (2008) 47:390–8. doi: 10.1097/CHI.0b013e31816429c2
14. Coates EE, Phares V. Predictors of paternal involvement among nonresidential, Black fathers from low-income neighborhoods. Psychol Men Masculinities (2014) 15:138–51. doi: 10.1037/a0032790
15. Atkinson MP, Blackwelder SP. Fathering in the 20th century. J Marriage Fam (1993) 55:975–86. doi: 10.2307/352777
16. Lamb ME. The history of research on father involvement: An overview. Marriage Fam Rev (2000) 29:23–42. doi: 10.1300/J002v29n02_03
17. Lamb ME, Pleck JH, Charnov EL, Levine JA. A biosocial perspective on paternal behavior and involvement. In: Lancaster JB, Altmann J, Rossi AS, Sherrod LR, editors. Parenting Across the Lifespan: Biosocial Dimensions. Abingdon, Oxon: Aldine Publishing Co (1987). p. 111–42.
18. Cabrera NJ, Tamis-LeMonda CS, Bradley RH, Hofferth S, Lamb ME. Fatherhood in the twenty-first century. Child Dev (2000) 71:127–36. doi: 10.1111/1467-8624.00126
19. Mallette JK, Futris TG, Oshri A, Brown GL. Paternal support and involvement in unmarried fragile families: Impact on long-term maternal mental health. Fam Proc (2019) 59:789–806. doi: 10.1111/famp.12456
20. Maselko J, Hagaman AK, Bates LM, Bhalotra S, Biroli P, Gallis JA, et al. Father involvement in the first year of life: Associations with maternal mental health and child development outcomes in rural Pakistan. Soc Sci Med (2019) 237:112421. doi: 10.1016/j.socscimed.2019.112421
21. Alio AP, Mbah AK, Kornosky JL, Wathington D, Marty PJ, Salihu HM. Assessing the impact of paternal involvement on racial/ethnic disparities in infant mortality rates. J Community Health (2011) 36:63–8. doi: 10.1007/s10900-010-9280-3
22. Caldera YM. Paternal involvement and infant-father attachment: A Q-set study. Fathering (2004) 2:191–210. doi: 10.3149/fth.0202.191
23. Bronte-Tinkew J, Carrano J, Horowitz A, Kinukawa A. Involvement among resident fathers and links to infant cognitive outcomes. J Fam Issues (2008) 29:1211–44. doi: 10.1177/0192513X08318145
24. Yogman MW, Kindlon D, Earls F. Father involvement and cognitive/behavioral outcomes of preterm infants. J Am Acad Child Psy (1995) 34:58–66. doi: 10.1097/00004583-199501000-00015
25. Mezulis AH, Hyde JS, Clark R. Father involvement moderates the effect of maternal depression during a child’s infancy on child behavior problems in kindergarten. J Fam Psychol (2004) 18:575–88. doi: 10.1037/0893-3200.18.4.575
26. Glass J, Owen J. Latino fathers: The relationship among machismo, acculturation, ethnic identity, and paternal involvement. Psychol Men Masc (2010) 11:251–61. doi: 10.1037/a0021477
27. Madhavan S, Townsend NW, Garey AI. Absent breadwinners’: Father–child connections and paternal support in rural South Africa. J South Afr Stud (2008) 34:647–63. doi: 10.1080/03057070802259902
28. Davis RN, Caldwell CH, Clark SJ, Davis M. Depressive symptoms in nonresident African American fathers and involvement with their sons. Pediatrics (2009) 124:1611–8. doi: 10.1542/peds.2009-0718
29. Sethna V, Murray L, Netsi E, Psychogiou L, Ramchandani PG. Paternal depression in the postnatal period and early father–infant interactions. Parenting (2015) 15:1–8. doi: 10.1080/15295192.2015.992732
30. Lee SJ, Taylor CA, Bellamy JL. Paternal depression and risk for child neglect in father-involved families of young children. Child Abuse Negl (2012) 36:461–9. doi: 10.1016/j.chiabu.2012.04.002
31. Planalp EM, Braungart-Rieker JM. Determinants of father involvement with young children: Evidence from the ECLS-B. J Fam Psychol (2016) 30:135–46. doi: 10.1037/fam0000156
32. Eggebeen DJ, Knoester C. Does fatherhood matter for men? J Marriage Fam (2001) 63:381–93. doi: 10.1111/j.1741-3737.2001.00381.x
33. Randles J. The means to and meanings of “being there” in responsible fatherhood programming. J Fam Relat (2020) 69:7–20. doi: 10.1111/fare.12376
34. Cooksey EC, Fondell MM. Spending time with his kids: Effects of family structure on fathers’ and children’s lives. J Marriage Fam (1996) 58:693–707. doi: 10.2307/353729
35. McBride BA, Schoppe SJ, Ho M, Rane TR. Multiple determinants of father involvement: An exploratory analysis using the PSID-CDS data set. In: Day RD, Lamb ME, editors. Conceptualizing and Measuring Father Involvement. Mahwah, New Jersey: Lawrence Eribaum Associates (2004). p. 321–40.
36. Pinto TM, Figueiredo B, Pinheiro LL, Canário C. Fathers’ parenting self-efficacy during the transition to parenthood. J Reprod Infant Psychol (2016) 34:343–55. doi: 10.1080/02646838.2016.1178853
37. Shorey S, Ang L, Goh EL, Gandhi M. Factors influencing paternal involvement during infancy: a prospective longitudinal study. J Adv Nurs (2019) 75:357–67. doi: 10.1111/jan.13848
38. de Montigny F, Lacharite C, Devault A. Transition to fatherhood: Modeling the experience of fathers of breastfed infants. J Adv Nurs Sci (2012) 35:E11–22. doi: 10.1097/ANS.0b013e3182626167
39. Christiansen SL, Palkovitz R. Why the “good provider” role still matters: Providing as a form of paternal involvement. J Fam Issues (2001) 22:84–106. doi: 10.1177/019252401022001004
40. Hill CV, Lynne-Landsman SD, Boyce CA. Maternal and child health disparities: Considering the influence of fathers. Am J Public Health (2012) 102:S164–5. doi: 10.2105/AJPH.2012.300792
41. Ramey SL, Schafer P, DeClerque JL, Lanzi RG, Hobel C, Shalowitz M, et al. The preconception stress and resiliency pathways model: A multi-level framework on maternal, paternal, and child health disparities derived by community-based participatory research. Matern Child Health J (2015) 19:707–19. doi: 10.1007/s10995-014-1581-1
42. O’Campo P, BeLue R, Borenstein H, Reed-Vance M, Lanzi RG, Schafer P, et al. Issues and solutions for collecting biological specimen in longitudinal studies: Experience from the Community Child Health Network Research Network. J Health Care Poor Underserved (2016) 27:339–51. doi: 10.1353/hpu.2016.0021
43. Reichman NE, Teitler JO, Garfinkel I, McLanahan SS. Fragile families: Sample and design. Child Youth Serv Rev (2001) 23:303–26. doi: 10.1016/S0190-7409(01)00142-6
44. Matthey S, Barnett B, Kavanagh DJ, Howie P. Validation of the Edinburgh Postnatal Depression Scale for men, and comparison of item endorsement with their partners. J Affect Disord (2001) 64:175–84. doi: 10.1016/S0167-0327(00)00236-6
45. Tandon SD, Cluxton-Keller F, Leis J, Le HN, Perry DF. A comparison of three screening tools to identify perinatal depression among low-income African American women. J Affect Dis (2012) 136:155–62. doi: 10.1016/j.jad.2011.07.014
46. Cox JL, Chapman G, Murray D, Jones P. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in non-postnatal women. J Affect Disord (1996) 39:185–9. doi: 10.1016/0165-0327(96)00008-0
47. Usuda K, Nishi D, Okazaki E, Makino M, Sano Y. Optimal cut-off score of the Edinburgh Postnatal Depression Scale for major depressive episode during pregnancy in Japan. Psychiat Clin Neuros (2017) 71:836–42. doi: 10.1111/pcn.12562
48. Edmondson OJ, Psychogiou L, Vlachos H, Netsi E, Ramchandani PG. Depression in fathers in the postnatal period: Assessment of the Edinburgh Postnatal Depression Scale as a screening measure. J Affect Dis (2010) 125:365–8. doi: 10.1016/j.jad.2010.01.069
49. Zeger SL, Liang KY, Albert PS. Models for longitudinal data: A generalized estimating equation approach. Biometrics (1988) 44:1049–60. doi: 10.2307/2531734
50. White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med (2011) 30:377–99. doi: 10.1002/sim.4067
51. Eddings W, Marchenko Y. Diagnostics for multiple imputation in Stata. SJ (2012) 11:353–67. doi: 10.1177/1536867X1201200301
52. Hudson DB, Elek SM, Fleck MO. First-time Mothers; and Fathers’ transition to parenthood: Infant care self-efficacy, parenting satisfaction, and infant sex. Issues Compr Pediatr Nurs (2001) 24:31–43. doi: 10.1080/0180/014608601300035580
53. Salonen AH, Kaunonen M, Åstedt-Kurki P, Järvenpää AL, Isoaho H, Tarkka MT. Parenting satisfaction during the immediate postpartum period: Factors contributing to mothers’ and fathers’ perceptions. J Clin Nurs (2010) 19:1716–28. doi: 10.1111/j.1365-2702.2009.02971.x
54. Davé S, Nazareth I, Sherr L, Senior R. The association of paternal mood and infant temperament: A pilot study. Br J Dev Psychol (2005) 23:609–21. doi: 10.1348/026151004X22962
55. Pesonen AK, Räikkönen K, Strandberg T, Keltikangas-Järvinen L, Järvenpää AL. Insecure adult attachment style and depressive symptoms: Implications for parental perceptions of infant temperament. Infant Ment Health J (2004) 25:99–116. doi: 10.1002/imhj.10092
56. Hanington L, Ramchandani P, Stein A. Parental depression and child temperament: Assessing child to parent effects in a longitudinal population study. Infant Behav Dev (2010) 33:88–95. doi: 10.1016/j.infbeh.2009.11.004
57. Salonen AH, Kaunonen M, Åstedt-Kurki P, Järvenpää AL, Isoaho H, Tarkka MT. Parenting self-efficacy after childbirth. J Adv Nurs (2009) 65:2324–36. doi: 10.1111/j.1365-2648.2009.05113.x
58. Hudson DB, Campbell-Grossman C, Fleck MO, Elek SM, Shipman A. Effects of the new fathers network on first-time fathers’ parenting self-efficacy and parenting satisfaction during the transition to parenthood. Issues Compr Pediatr Nurs (2003) 26:217–29. doi: 10.1080/01460860390246687
59. Salonen AH, Kaunonen M, Åstedt-Kurki P, Järvenpää AL, Isoaho H, Tarkka MT. Effectiveness of an internet-based intervention enhancing Finnish parents’ parenting satisfaction and parenting self-efficacy during the postpartum period. Midwifery (2011) 27:832–41. doi: 10.1016/j.midw.2010.08.010
60. Jones TL, Prinz RJ. Potential roles of parental self-efficacy in parent and child adjustment: A review. Clin Psychol Rev (2005) 25:341–63. doi: 10.1016/j.cpr.2004.12.004
61. Yeung WJ, Sandberg JF, Davis-Kean PE, Hofferth SL. Children’s time with fathers in intact families. J Marriage Fam (2001) 63:136–54. doi: 10.1111/j.1741-3737.2001.00136.x
62. Kleppa E, Sanne B, Tell GS. Working overtime is associated with anxiety and depression: The Hordaland Health Study. J Occup Environ Med (2008) 50:658–66. doi: 10.1097/JOM.0b013e3181734330
63. Nakata A. Work hours, sleep sufficiency, and prevalence of depression among full-time employees: A community-based cross-sectional study. J Clin Psychiat (2011) 72:605–14. doi: 10.4088/JCP.10m06397gry
64. Grossman FK, Pollack WS, Golding E. Fathers and children: Predicting the quality and quantity of fathering. Dev Psychol (1988) 24:82–91. doi: 10.1037/0012-1649.24.1.82
65. Alio AP, Lewis CA, Scarborough K, Harris K, Fiscella K. A community perspective on the role of fathers during pregnancy: A qualitative study. BMC Pregnancy Childb (2013) 13:60. doi: 10.1186/1471-2393-13-60
66. Cazenave NA. Middle-income Black fathers: An analysis of the provider role. Fam Coord (1979), 28:583–93. doi: 10.2307/583522
67. Cohen TF. What do fathers provide? Reconsidering the economic and nurturant dimensions of men as parents. In: Hood JC, editor. Research on Men and Masculinities Series, Vol. 4, Men, Work and Family. Thousand Oaks, CA: Sage Publications, Inc (1993). p. 1–22.
68. Anderson EA, Kohler JK, Letiecq BL. Predictors of depression among low-income, nonresidential fathers. J Fam Issues (2005) 26:547–67. doi: 10.1177/0192513X04272753
69. Bielawska-Batorowicz E, Kossakowska-Petrycka K. Depressive mood in men after the birth of their offspring in relation to a partner’s depression, social support, fathers’ personality and prenatal expectations. J Reprod Infant Psychol (2006) 24:21–9. doi: 10.1080/02646830500475179
70. Black MM, Dubowitz H, Starr RH Jr. African American fathers in low income, urban families: Development, behavior, and home environment of their three-year-old children. Child Dev (1999) 70:967–78. doi: 10.1111/1467-8624.00070
71. Choi JK, Pyun HS. Nonresident fathers’ financial support, informal instrumental support, mothers’ parenting, and child development in single-mother families with low income. J Fam Issues (2014) 35:526–46. doi: 10.1177/0192513X13478403
72. Brown SL, Nesse RM, Vinokur AD, Smith DM. Providing social support may be more beneficial than receiving it: Results from a prospective study of mortality. Psychol Sci (2003) 14:320–7. doi: 10.1111/1467-9280.14461
73. Krause N, Herzog AR, Baker E. Providing support to others and well-being in later life. J Gerontol (1992) 47:300–11. doi: 10.1093/geronj/47.5.P300
74. Inagaki TK, Haltom KEB, Suzuki S, Jevtic I, Hornstein E, Bower JE, et al. The neurobiology of giving versus receiving support: The role of stress-related and social reward-related neural activity. Psychosom Med (2016) 78:443–53. doi: 10.1097/PSY.0000000000000302
75. Gross HE, Shaw DS, Moilanen KL, Dishion TJ, Wilson MN. Reciprocal models of child behavior and depressive symptoms in mothers and fathers in a sample of children at risk for early conduct problems. J Fam Psychol (2008) 22:742–51. doi: 10.1037/a0013514
76. Alio AP, Bond MJ, Padilla YC, Heidelbaugh JJ, Lu M, Parker WJ. Addressing policy barriers to paternal involvement during pregnancy. Matern Child Health J (2011) 15:425–30. doi: 10.1007/s10995-011-0781-1
77. Boll C, Leppin J, Reich N. Paternal childcare and parental leave policies: Evidence from industrialized countries. Rev Econ Househ (2014) 12:129–58. doi: 10.1007/s11150-013-9211-z
78. Nepomnyaschy L, Waldfogel J. Paternity leave and fathers’ involvement with their young children: Evidence from the American Ecls–B. Community Work Fam (2007) 10:427–53. doi: 10.1080/13668800702575077
79. Bakermans-Kranenburg MJ, Lotz A, Dijk KA, van IJzendoorn M. Birth of a father: Fathering in the first 1,000 days. Child Dev Perspect (2019) 13:247–53. doi: 10.1111/cdep.12347
80. Scantamburlo G, Hansenne M, Fuchs S, Pitchot W, Marechal P, Pequeux C, et al. Plasma oxytocin levels and anxiety in patients with major depression. Psychoneuroendocrinology (2007) 32:407–10. doi: 10.1016/j.psyneuen.2007.01.009
81. Abraham E, Feldman R. The neurobiology of human allomaternal care; implications for fathering, coparenting, and children’s social development. Physiol Behv (2018) 3:25–34. doi: 10.1016/j.physbeh.2017.12.034
82. Ranson K, Urichik LJ. The effect of parent–child attachment relationships on child biopsychosocial outcomes: A review. Early Child Dev Care (2008) 178:129–52. doi: 10.1080/03004430600685282
83. Bretherton I, Lambert JD, Golby B. Involved fathers of preschool children as seen by themselves and their wives: Accounts of attachment, socialization, and companionship. Attach Hum Dev (2005) 7:229–51. doi: 10.1080/14616730500138341
84. Brown GL, Mangelsdorf SC, Neff C. Father involvement, paternal sensitivity, and father– child attachment security in the first 3 years. J Fam Psychol (2012) 26:421–30. doi: 10.1037/a0027836
85. Adamsons K, Johnson S. An updated and expanded meta-analysis of nonresident fathering and child well-being. J Fam Psychol (2013) 27:589–99. doi: 10.1037/a0033786
86. Amato PR, Gilbreth JG. Nonresident fathers and children’s well-being: A meta-analysis. J Marriage Fam (1999) 61:557–73. doi: 10.2307/353560
87. de Montigny F, Girard ME, Lacharité C, Dubeau D, Devault A. Psychosocial factors associated with paternal postnatal depression. J Affect Disord (2013) 150:44–9. doi: 10.1016/j.jad.2013.01.048
Keywords: fathers, depressive symptoms, paternal involvement, parenting self-efficacy, low-income fathers, community-based participatory research
Citation: Bamishigbin ON Jr, Wilson DK, Abshire DA, Mejia-Lancheros C and Dunkel Schetter C (2020) Father Involvement in Infant Parenting in an Ethnically Diverse Community Sample: Predicting Paternal Depressive Symptoms. Front. Psychiatry 11:578688. doi: 10.3389/fpsyt.2020.578688
Received: 30 June 2020; Accepted: 25 August 2020;
Published: 23 September 2020.
Edited by:
Susan Garthus-Niegel, Dresden University of Technology, GermanyReviewed by:
Susanne Knappe, Technical University Dresden, GermanyFreya Thiel, Technische Universität Dresden, Germany
Copyright © 2020 Bamishigbin, Wilson, Abshire, Mejia-Lancheros and Dunkel Schetter. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Olajide N. Bamishigbin Jr, b2xhamlkZS5iYW1pc2hpZ2JpbkBjc3VsYi5lZHU=
 Olajide N. Bamishigbin Jr
Olajide N. Bamishigbin Jr Dawn K. Wilson2
Dawn K. Wilson2 Demetrius A. Abshire
Demetrius A. Abshire Christine Dunkel Schetter
Christine Dunkel Schetter