- 1Department of Child & Adolescent Psychiatry, Wuhan Mental Health Center, Tongji Medical College, Huazhong University of Science & Technology, Wuhan, China
- 2Department of Psychiatry, Tongji Hospital, Tongji Medical College, Huazhong University of Science & Technology, Wuhan, China
- 3School of Rehabilitation, Kunming Medical University, Kunming, China
Background: The limitations associated with antipsychotics in early-onset schizophrenia patients have stimulated more interest in psychological interventions in this population. Nevertheless, the isolated psychosocial interventions are unrealistic in a treatment success covering the complex array of symptoms, and the psychosocial interventions could be an adjunct treatment to the pharmacological treatment. It is necessary to find the benefits of psychological interventions with limited and targeted use of antipsychotics. Social cognition and interaction training (SCIT) was a program for social cognitive rehabilitation in adult schizophrenia. However, it is unclear how generalizable this is to early-onset patients.
Methods: The current study tested this hypothesis that combined SCIT and paliperidone was superior to paliperidone alone in treating early-onset schizophrenia patients on cognitive, functional, and symptom outcomes. Two hundred eight inpatients with schizophrenia aged 13 to 17 years old participated in a 24-week work intervention program. Patients completed a battery of measures administered at a pre-SCIT intervention baseline, 4, 8, 12, and 24 weeks post-SCIT, respectively.
Results: SCIT had significant added benefits above paliperidone for the speed of processing, attention/vigilance, and social cognition of the Chinese version of MATRICS consensus cognitive battery (MCCB) domains (p<0.05). The following logistic regression analysis on the exploration of the influential factors also confirmed the effects of SCIT. However, combined SCIT and paliperidone intervention had a null impact on social functioning and symptomatology.
Conclusions: The present study provides the first evidence that combined SCIT and paliperidone intervention has the potential to improve cognitive functions for the early-onset schizophrenia patients. The findings in the current study are suggestive of the extreme importance of SCIT as an adjunctive treatment in early-onset schizophrenia patients.
Introduction
Schizophrenia is a chronic, severe, and disabling illness that affects approximately 1% of individuals in the population, with onset usually during late adolescence or early adulthood (1). Youth who experience early-onset schizophrenia, defined by an onset before 18 years of age, often have impaired cognition involving both neuro-cognition and social cognition (2–4). These deficits highly correlated with loss of function in school, community, and social relationships (5, 6). As cognitive impairments remain an enduring and functionally disabling symptom of schizophrenia, it needs to find treatments to combat the cognitive deficits in younger persons with this condition (7).
Early-onset schizophrenia defined by an onset strictly before the age of 18 years (8). Patients with early-onset schizophrenia were less responsive to pharmacological treatment on cognitive deficits (9, 10). Furthermore, antipsychotics often have severe metabolic, neurological, and other side effects associated with significant premature mortality (11). The limitations associated with antipsychotic medication in early-onset schizophrenia patients have stimulated greater interest in psychological interventions in this population (12). Some aspects of social cognition had indicated to predict functional outcomes, and mediate the relationship between neuro-cognition and functional outcome in schizophrenia patients (13–15). The promise of social skills training focused on social cognition has been documented in schizophrenia patients (16).
Social cognition and interaction training (SCIT), which designed to increase the flexibility in attributional style and improve metacognition, is comprised of teaching individuals problem identification, goal setting, use of role-plays or behavioral rehearsal for successful social interaction, social modeling, and problem-solving (17). Contrary to other psychosocial interventions that focused on the specific social cognitive impairments to the exclusion of other domains (18), SCIT targets a broader range of social cognition, e.g., a theory of mind, social perception, social knowledge, attributional bias, and emotion processing (19). It indicated as a program for social cognitive rehabilitation in adult schizophrenia (20).
There is clear evidence that SCIT is a helpful intervention on social cognition in adults with schizophrenia (21), but it is unclear how generalizable this is to the early-onset patients. Such group of patients may have more severe social cognitive deficits, negatively influencing social, cognitive and psychological development (22), and having a worse prognosis and outcome (23, 24), which if alleviated might change the course of the disorder (25). Therefore, it is needed to confirm the degree to which SCIT is promising in youth with schizophrenia. Although delusions and catatonic symptoms occur less frequently, early-onset schizophrenia patients usually have hallucinations, thought disorder, and flattened affect. The isolated psychosocial interventions are unrealistic in a treatment success covering the complex array of symptoms, and the psychosocial interventions could be an adjunct treatment to the pharmacological interventions (26). The China Food and Drug Administration approved paliperidone extended-release for the treatments of adolescents with schizophrenia in 2017. Therefore, the specific objective of the current study was to examine the efficacy of combined SCIT and paliperidone on early-onset schizophrenia patients with a short duration of illness, the entire course of disease included previous episodes is no more than 4 years.
Since social cognition mediates the relationship between neuro-cognition and functional outcome, and negative symptoms also have a strong relationship with social cognitions (27), we expect that the combined SCIT and paliperidone improve cognitions along with social functioning and the symptomatology in the early-onset schizophrenia patients. In the current study, we used the MATRICS Consensus Cognitive Battery (MCCB) to estimate the patients’ cognition functions; the personal and social performance scale (PSP) to measure the social functioning; the scale for the assessment of Negative Symptoms (SANS) and the positive and negative syndrome scale (PANSS, total score) to assess the symptomatology. The current study hypothesized that combined SCIT and paliperidone were superior to paliperidone alone in treating early-onset schizophrenia patients on cognitive, functional, and symptom outcomes. This study will assist practitioners in understanding the psychosocial interventions with medications in early-onset schizophrenia patients.
Materials and Methods
Participants
Two hundred and eight inpatients with schizophrenia aged 13 to 17 years at the time of the study, who met the tenth version of the International Classification of Diseases (ICD-10) criteria for schizophrenia, were recruited from the Wuhan Mental Health Center, Tongji Medical College of Huazhong University of Science& Technology. Enrolled criteria were (1) meeting criteria for schizophrenia according to ICD-10; (2) no evidence of current or previous head injury, CNS disease, and other ICD-10 disorders; (3) right-handed with normal vision and hearing; (4) no history of antipsychotic use, or more than 2 weeks from the last drug treatment, and no long-acting injection of antipsychotic drugs. The excluded criteria were (1) with acute suicidal ideation or life-threatening, (2) severe, or unstable physical disorder; (3) had a history of substance or alcohol use disorder within six months before screening; (4) had an estimated IQ<70, as assessed by the Wechsler Intelligence Scale (Chinese version). Participants, to whom the doctor in charge deemed inappropriate for any other reason, were also excluded from the study. During the study intervention periods, some patients proceeded from wards to back home by the improvement of symptomatology, but they still need oral medication and rehabilitation training. All the participants under the investigation had the written and informed consent from the guardian. The ethics committee of the Wuhan Mental Health Centre, Tongji Medical College of Huazhong University of Science& Technology, approved the study protocol and informed consent procedures (KY20161617).
Study Design
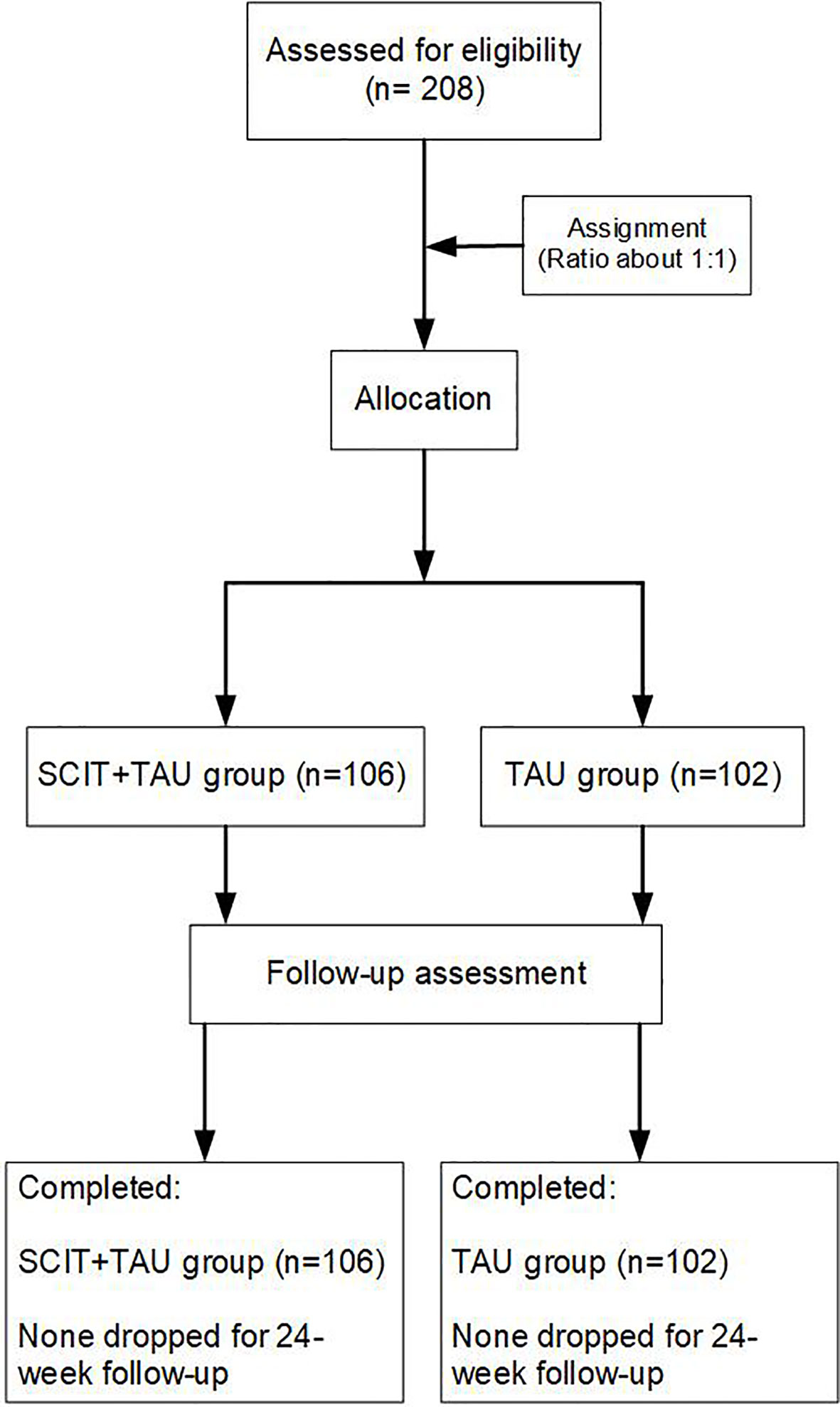
Patients screened for inclusion and exclusion criteria were randomized to either of the two groups on a 1:1 ratio. Patients who received SCIT plus paliperidone (paliperidone extended-release tablets, INVEGA®, 3 to 12 mg/day, Xian Janssen, Co. Ltd) enrolled in the SCIT+ paliperidone group (n=106). Those received paliperidone only were in the paliperidone group (n=102). More details are shown in Figure 1. Patients in SCIT plus paliperidone intervention were delivered for 5-8 patients at a time by a pair of clinicians, who trained to use SCIT by the developers of the intervention. There are 15 sub-groups in the SCIT+ paliperidone intervention group. Group leaders were psychologists and occupational therapists. Those in the groups received a 45- to 60-min training course once per week for 20 to 24 sessions. Patients’ social functioning and cognitive function were assessed by the personal and social performance scale (PSP) and the Chinese version of MATRICS consensus cognitive battery (MCCB) respectively; the scale measured their symptom severity for the assessment of Negative Symptoms (SANS) and the positive and negative syndrome scale (PANSS, total score). Patients completed measures of SANS, PANSS, and PSP at a pre-SCIT intervention baseline, 4, 8, 12, and 24 weeks post-SCIT, respectively, and MCCB at baseline and 24 weeks post-SCIT. Patients in the paliperidone group completed the same tests at the same time as those in the SCIT+ paliperidone group. The raters were well trained and had excellent interrater reliability; the raters were blind to the randomization.
Statistical Analysis
The sample size was calculated by PASS software 15.0.5. We used Pearson’s Chi test for the screening of the differences in gender ratio, education, dependant’s type, dependants’ education, family relationship, and relapse frequency between groups. One-way analysis of variance (ANOVA) performed for the analysis of each continuous variables between groups, such as age, paliperidone dosage, duration of the illness, SANS, PANSS and PSP at baseline and MCCB at baseline(Speed of processing, Attention/vigilance, Working memory, Verbal learning, Visual learning, reasoning and problem-solving, and Social cognition). The changes of MCCB, SANS, PANSS, and PSP were estimated by repeated-measures ANOVA, respectively, with the group (SCIT+ paliperidone vs paliperidone) as a between-group factor and time point (baseline vs follow-up) as a within-group factor.
To clarify the effects of SCIT on the early-onset schizophrenia patients, we performed binary logistic regression analysis to explore the potentially influential factors for improved cognition, social functioning, and symptoms. The logistic regression model is routinely used to evaluate the treatment effect on the responder status at the first time point of interest corresponding to the end of the study. The odds ratio means the character of the treatment effect adjusted for baseline. It was calculated by the Exp(β) in the SPSS software.
In the regression analysis, the full samples subdivided according to the median value of the variables identified as screening factors. The variables with p < 0.2 in the independence test (Chi-square and ANOVA tests) submitted to the regression analysis as the covariates, the effect sizes of MCCB cognition domains, SANS, PANSS total score, and PSP were the dependent respectively in the separate binary logistic regressions for the screening progress. The effect size calculated as (score at 24 weeks score at baseline)/pooled SD of baseline.
Results
Sociodemographic and Clinical Profiles of Participants
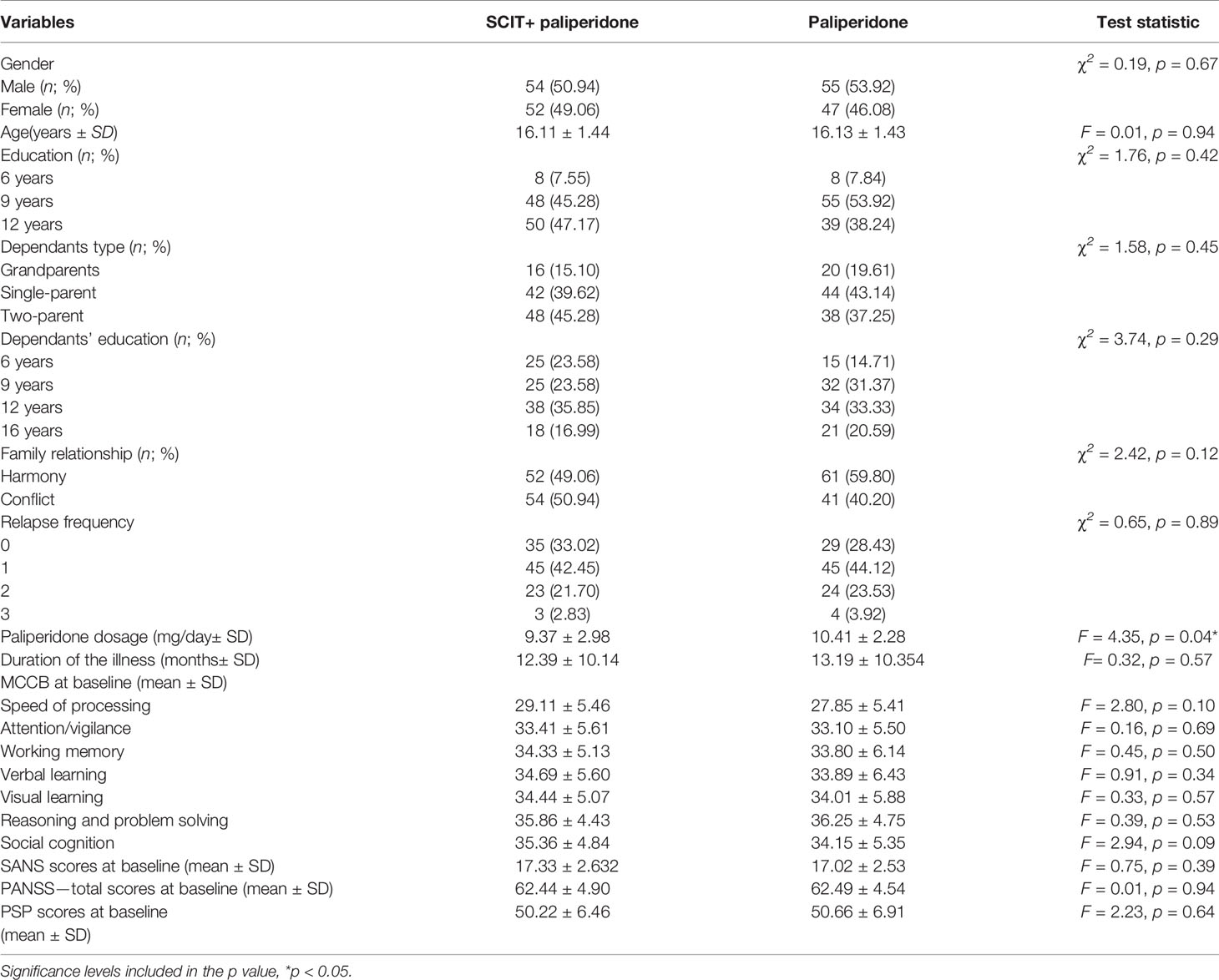
Two hundred and eight patients completed the study, 106 of them were in the SCIT+ paliperidone group, and 102 of them were in the paliperidone group. The demographic characteristics of the participants were in Table 1. Patients in the SCIT plus paliperidone group had not much significant difference from those in the paliperidone group, except for the higher paliperidone dosage in the paliperidone group (p<0.05, Table 1).
Effects of SCIT+ Paliperidone in the Change of Cognition, Social Functioning, and Symptom Severity
All the patients completed the 24-week study. During the study intervention periods, 85 patients in the SCIT+ paliperidone group and 79 patients in the paliperidone group proceeded from wards to back home. They still had routine outpatient visiting every once a week. In the MCCB test, the repeated-measures one-way ANOVA revealed a significant main effect of group for the speed of processing, attention/vigilance, and social cognition (p<0.05). Generally, both groups of treatments improved all the MCCB cognitive domains after 24-week intervention, but the SCIT+ paliperidone group had more sound effects than paliperidone group on the above domains (Table 2, Figure 2). Similarly, SANS and PANSS decreased, but PSP increased after 24 weeks of intervention in both groups. However, repeated-measures one-way ANOVA did not find significant differences between SCIT+ paliperidone and paliperidone group (Figure 3).
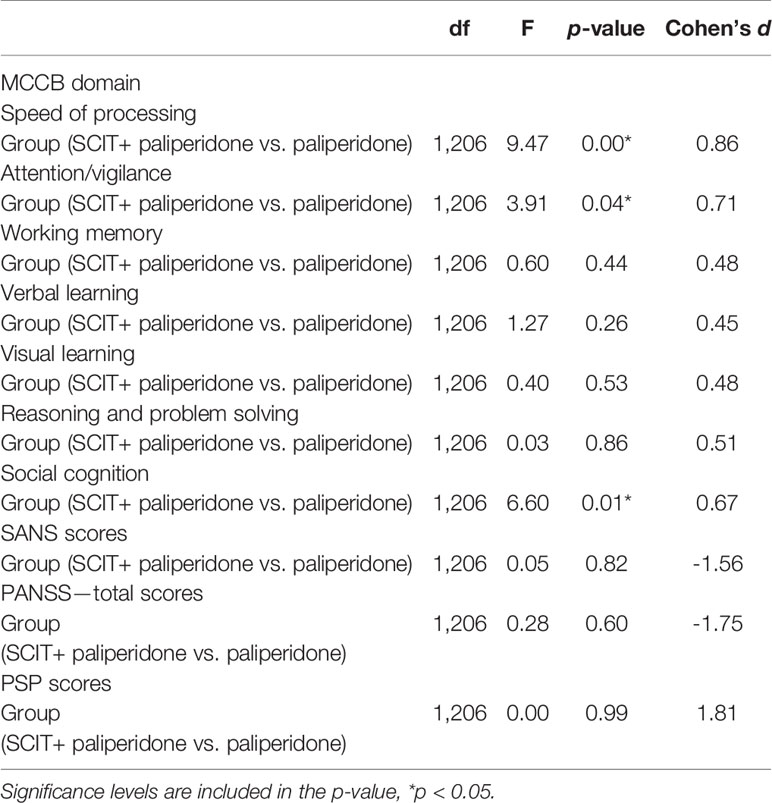
Table 2 Results of repeated ANOVA analysis on the measures of cognition, social functioning, and symptom severity.
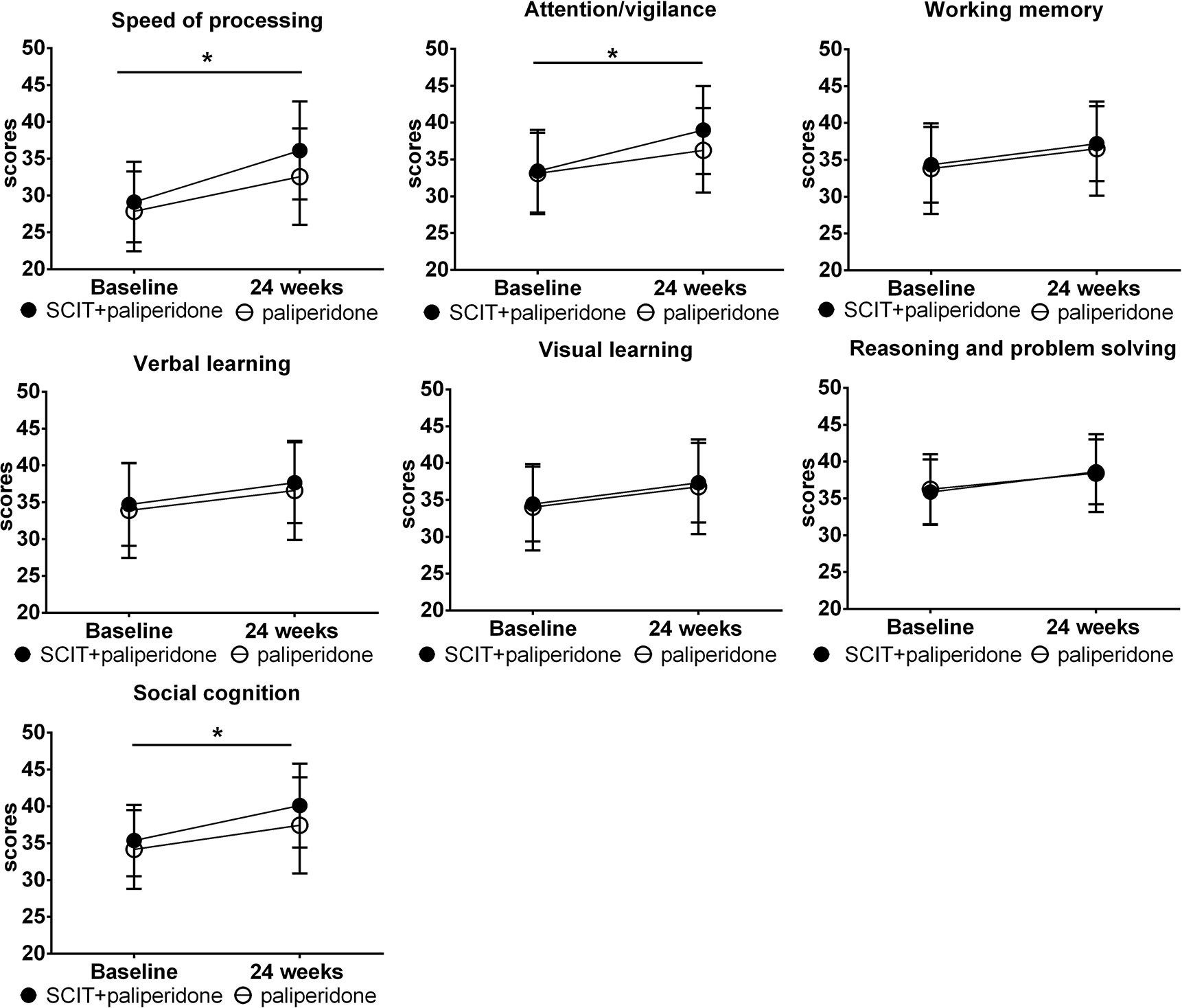
Figure 2 The comparison of changes in the scores of MCCB cognitive domains from baseline to the 24-week endpoint. Data are presented as mean ± SD. Significance levels are included in the p-value, *P < 0.05.
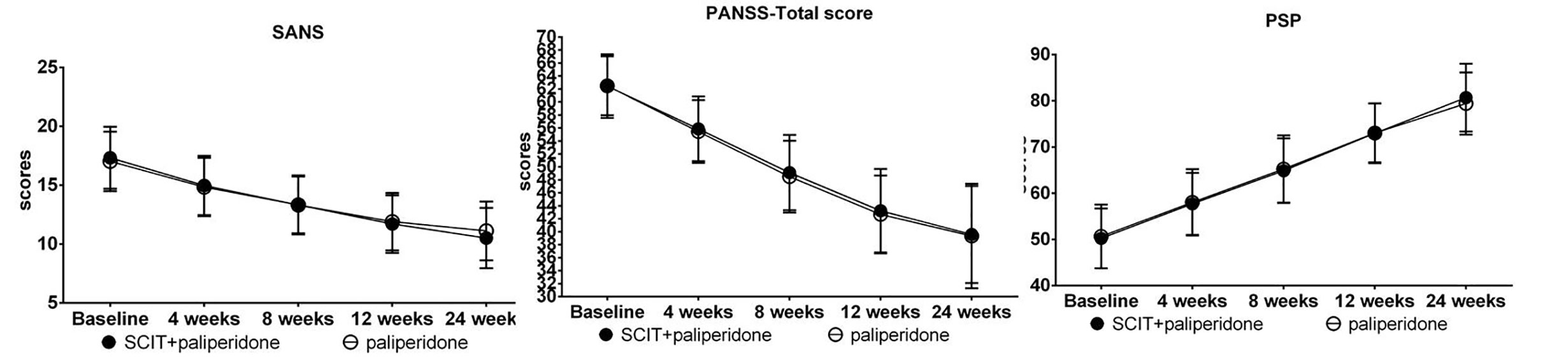
Figure 3 Comparison of changes in the scores of SANS, PANSS, and PSP from baseline to 4-week interim timepoint, 8-week interim timepoint, 12-week interim time point, and 24-week endpoint. Data are presented as mean ± SD.
Possible Influential Factors for the Improved Cognition, Social Functioning, and Symptoms
The results of logistic regression analysis also confirmed the effect of SCIT+ paliperidone. In the MCCB cognition domain, the multivariate analysis (binary logistic regression model) revealed that the speed of processing was associated with the speed of processing at baseline, attention/vigilance at baseline, working memory at baseline and group difference (SCIT+ paliperidone vs paliperidone). The maximum effect was in the SCIT+ paliperidone group. Patients in that group had a 2.89-folder higher chance to obtain improved speed of processing. Attention/vigilance was associated with the working memory at baseline, verbal learning at baseline, and group; the patients in the SCIT+ paliperidone group had a 6.38-folder higher chance to obtain improvement. Social cognition was also associated with visual learning at baseline, social cognition at baseline, and group; the patients in the SCIT+ paliperidone group had a 3.15-folder higher chance to obtain improvement. SANS was also associated with SANS at baseline, PSP at baseline, and group, patients in the SCIT+paliperidone group, had a 53.3% greater chance to obtain improvement. More other results in the logistic regression analysis displayed in Supplementary Table 1.
Discussion
In this study, we compared the early-onset schizophrenia patients’ performances in the SCIT plus paliperidone intervention with those in the only paliperidone intervention. None of the participants dropped out throughout the whole program, which suggested that SCIT and paliperidone appear to be feasible and well tolerated by patients with early-onset schizophrenia. Patients who received SCIT + paliperidone showed significant improvement in the speed of processing, attention/vigilance, and social cognition of MCCB domains relative to those with the only paliperidone. Those domains of neuro-cognition refers to the processes of linking and appraising information (28), which is a better predictor of functioning than the positive symptoms in schizophrenia patients (14). Those deficits have been associated with impairments in different domains of functional outcome such as global psychosocial functioning (29), community functioning (30), daily problem solving skills (31), job tenure (32), social skills (33), or independent living skills (34). However, results indicated that SCIT had no added benefits above paliperidone for enhancing the social functioning and clinical symptoms in the patients with early-onset schizophrenia.
We chose MCCB to estimate patients’ cognition, as it serves as the standard measure for cognitive studies, includes social cognition as one of the seven cognitive domains in schizophrenia (35). MCCB evidenced sensitivity to cognitive differences between adolescent healthy controls and adolescents with early-onset schizophrenia (36). The repeated-measures one-way ANOVA had found the significant differences in the change of the speed of processing, attention/vigilance, and social cognition in patients between the SCIT + paliperidone and paliperidone group. The following logistic regression analysis on the exploration of the influential factors also confirmed the effects of SCIT. Notably, most of them have the largest OR value, which means SCIT has a substantial impact on the improvements. Researchers have noted that the speed of processing and attention/vigilance in the MCCB was associated with the motivation (37). The accurate processing of socio emotive stimuli intimately integrated with neural systems related to motivation in the human brain (38), deficits in processing social stimuli harm motivation in patients with schizophrenia. Through this mechanism, it showed a negative influence on their functioning (39). SCIT could improve motivation in adult schizophrenia patients (40). Therefore, we suspect that the effects of SCIT on the cognitions measured by MCCB are due to its direct impact on the motivation of the early-onset schizophrenia patients.
We failed to find the similar effects of SCIT on the MCCB domains of working memory, verbal learning, visual learning, reasoning and problem-solving. The tasks of the above MCCB domains were possibly dependent on the individuals’ self-ability of perception, which impaired in the baseline of the study. SCIT has been reported to be effective in improving the ability to interact with social cues (41), but not emotion perception abilities to oneself (42).
The personal and social performance scale (PSP) scale is a reliable and valid instrument for assessing the social functioning of patients with schizophrenia during treatment (43). We used PSP to assess the patients’ social functioning from four main domains, such as socially useful activities, personal and social relationships, self-care, and disturbing and aggressive behavior. SCIT had no significant added benefits above paliperidone for facilitating remission of the social functioning. Previous studies had reported the social behaviors in the milieu had the most active associations with verbal learning, visual learning and memory, and reasoning and problem solving (14). However, neither of those MCCB domains obtained significant improvements in the SCIT plus paliperidone group compared with those in the paliperidone group. SCIT has reported improving the PSP scores in Chinese adult schizophrenia patients (44).
Nevertheless, we failed to find similar effects on the youth with schizophrenia. PSP has been proposed as particularly well sensitive to assess the social functioning outcomes in antipsychotic drug (45). Therefore, we suspected that the power of paliperidone might cover the net impacts of SCIT on the social functioning of early-onset schizophrenia patients.
Similarly, SCIT plus paliperidone intervention had null effects on the symptomatology of the early-onset schizophrenia patients. The lack of additive effects of SCIT on perception and executive functioning in the current study cannot help early-onset schizophrenia patients to detect social cues and understand the intentions while interacting with others, which in turn has no progress on negative and positive symptoms in schizophrenia (14). Moreover, The PANSS total score at baseline in our study was about 62.44 ± 4.903, which means those patients had mildly ill with higher function (46). SCIT has thought to have less impact on higher functioning patients (47). A relative more significant impact on social cognition than on social functioning and negative symptoms would be promising as SCIT improves social cognition through a combination of rehearsal-based “bottom-up” learning and acquisition strategies.
The early-onset schizophrenia patients usually mean less independence, more inadequate education (22); those also thought to influence the SCIT treatment effects. On the contrary, the logistic regression analysis in the current study revealed the impact of SCIT on early-onset patients was independent with those background characters, except for the cognition, social functioning, and symptomatology at the baseline. Moreover, there were more than 200 patients enrolled in this study; the sample size was large enough to have the power of avoiding a type II error. All of those have shown SCIT is feasible for use with and well-tolerated by early-onset schizophrenia patients in real-world settings.
The current study has several limitations. First, most of the patients in the present study were first-episode or have once relapse with the mean age of 16 years old, which increases the risk of diagnosis uncertainty, such as bipolar disorder in the future. Second, we only studied the treatment effect between baseline and 24-week interim assessments; we are not clear that those effects will last or change for a long time. Third, the SCIT acts as role-play with more than one facilitator, which was conducted by themselves (48), which has linked to several facets, including the theory of mind, emotion perception, and empathic ability (49). Therefore, there was an inherent probability for the children to understand the purpose of the training. Last, there is no active control in the current study, all the patients received paliperidone treatments, and we had not controlled for the dosages. However, research on the effects of antipsychotic medication on cognition is inconsistent, and pediatric psychotic disorders are scant. There is evidence that new atypical antipsychotic medications may have some positive effect on cognitive functioning, but there is no evidence that antipsychotic medication completely ameliorates cognitive impairments. Future study with a long-term follow-up and the more complicated situation is warranted.
In summary, the present study provides the first evidence that SCIT+ paliperidone intervention has the potential to improve cognitive functions for the early-onset schizophrenia patients. Our primary findings indicate that SCIT as an adjunctive treatment may facilitate remission of the schizophrenia symptoms in youth. Those changes could improve the long-term prognosis and psychosocial outcomes, which may also prevent some of the secondary difficulties associated with schizophrenia from being accrued, e.g., interruptions in education, reliance on welfare benefits, downwards socio-economic shift, and breakdown of relationships. This study could help to find how psychological interventions should be adapted for children and adolescents, the benefits of psychological interventions with limited and targeted use of antipsychotics, and the most effective timing for interventions during illness. Our study is the first report on a large number of young people with a relatively short duration of schizophrenia receiving individual cognitive remediation treatment early in their psychiatric history in China. The findings in the current study are suggestive of the extreme importance of social cognition training in early-onset schizophrenia patients.
Data Availability Statement
All datasets generated for this study are included in the article/supplementary material.
Ethics Statement
The studies involving human participants were reviewed and approved by The ethics committee of the Wuhan Mental Health Centre, Tongji Medical College of Huazhong University of Science & Technology (KY20161617). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author Contributions
JM and XZ were involved in the conceptualization and planning of the study. YL, KS, and DL were involved in the implementation of the trial. M-XC and XZ were responsible for the management of the trial, including the implementation of randomization procedures, data management, and drafting the manuscript. GL was responsible for the statistical analyses. All authors contributed to the article and approved the submitted version.
Funding
This work was financially supported by the critical project in the Wuhan health and Family Planning Commission to YL (grant WX17B15).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to express appreciation to the participants who devoted their time and effort to complete the study, as well as staff in the Wuhan Mental Health Centre who facilitated the completion of the study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.525492/full#supplementary-material
References
1. Asarnow JR, Tompson MC, McGrath EP. Annotation: childhood-onset schizophrenia: clinical and treatment issues. J Child Psychol Psychiatry (2004) 45(2):180–94. doi: 10.1111/j.1469-7610.2004.00213.x
2. Bell M, Tsang HW, Greig TC, Bryson GJ. Neurocognition, social cognition, perceived social discomfort, and vocational outcomes in schizophrenia. Schizophr Bull (2009) 35(4):738–47. doi: 10.1093/schbul/sbm169
3. Bellack AS, Schooler NR, Marder SR, Kane JM, Brown CH, Yang Y. Do clozapine and risperidone affect social competence and problem solving? Am J Psychiatry (2004) 161(2):364–7. doi: 10.1176/appi.ajp.161.2.364
4. Bismark AW, Thomas ML, Tarasenko M, Shiluk AL, Rackelmann SY, Young JW, et al. Relationship between effortful motivation and neurocognition in schizophrenia. Schizophr Res (2018) 193:69–76. doi: 10.1016/j.schres.2017.06.042
5. Brekke JS, Raine A, Ansel M, Lencz T, Bird L. Neuropsychological and psychophysiological correlates of psychosocial functioning in schizophrenia. Schizophr Bull (1997) 23(1):19–28. doi: 10.1093/schbul/23.1.19
6. Burns T, Patrick D. Social functioning as an outcome measure in schizophrenia studies. Acta Psychiatr Scand (2007) 116(6):403–18. doi: 10.1111/j.1600-0447.2007.01108.x
7. Combs DR, Adams SD, Penn DL, Roberts D, Tiegreen J, Stem P. Social Cognition and Interaction Training (SCIT) for inpatients with schizophrenia spectrum disorders: preliminary findings. Schizophr Res (2007) 91(1–3):112–6. doi: 10.1016/j.schres.2006.12.010
8. Dickerson F, Boronow JJ, Ringel N, Parente F. Social functioning and neurocognitive deficits in outpatients with schizophrenia: a 2-year follow-up. Schizophr Res (1999) 37(1):13–20. doi: 10.1016/s0920-9964(98)00134-0
9. Fett AK, Viechtbauer W, Dominguez MD, Penn DL, van Os J, Krabbendam L. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: a meta-analysis. Neurosci Biobehav Rev (2011) 35(3):573–88. doi: 10.1016/j.neubiorev.2010.07.001
10. Frazier JA, Giuliano AJ, Johnson JL, Yakutis L, Youngstrom EA, Breiger D, et al. Neurocognitive outcomes in the Treatment of Early-Onset Schizophrenia Spectrum Disorders study. J Am Acad Child Adolesc Psychiatry (2012) 51(5):496–505. doi: 10.1016/j.jaac.2012.02.001
11. Gold JM, Goldberg RW, McNary SW, Dixon LB, Lehman AF. Cognitive correlates of job tenure among patients with severe mental illness. Am J Psychiatry (2002) 159(8):1395–402. doi: 10.1176/appi.ajp.159.8.1395
12. Green MF, Kern RS, Heaton RK. Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr Res (2004) 72(1):41–51. doi: 10.1016/j.schres.2004.09.009
13. Green MF, Penn DL, Bentall R, Carpenter WT, Gaebel W, Gur RC, et al. Social cognition in schizophrenia: an NIMH workshop on definitions, assessment, and research opportunities. Schizophr Bull (2008) 34(6):1211–20. doi: 10.1093/schbul/sbm145
14. Harvey PD, Keefe RS, Patterson TL, Heaton RK, Bowie CR. Abbreviated neuropsychological assessment in schizophrenia: prediction of different aspects of outcome. J Clin Exp Neuropsychol (2009) 31(4):462–71. doi: 10.1080/13803390802251386
15. Heerey EA, Gold JM. Patients with schizophrenia demonstrate dissociation between affective experience and motivated behavior. J Abnorm Psychol (2007) 116(2):268–78. doi: 10.1037/0021-843x.116.2.268
16. Hollis C. Adult outcomes of child- and adolescent-onset schizophrenia: diagnostic stability and predictive validity. Am J Psychiatry (2000) 157(10):1652–9. doi: 10.1176/appi.ajp.157.10.1652
17. Holmen A, Juuhl-Langseth M, Thormodsen R, Melle I, Rund BR. Neuropsychological profile in early-onset schizophrenia-spectrum disorders: measured with the MATRICS battery. Schizophr Bull (2010) 36(4):852–9. doi: 10.1093/schbul/sbn174
18. Hooper SR, Giuliano AJ, Youngstrom EA, Breiger D, Sikich L, Frazier JA, et al. Neurocognition in early-onset schizophrenia and schizoaffective disorders. J Am Acad Child Adolesc Psychiatry (2010) 49(1):52–60. doi: 10.1097/00004583-201001000-00009
19. Juckel G, Morosini PL. The new approach: psychosocial functioning as a necessary outcome criterion for therapeutic success in schizophrenia. Curr Opin Psychiatry (2008) 21(6):630–9. doi: 10.1097/YCO.0b013e328314e144
20. Kanie A, Kikuchi A, Haga D, Tanaka Y, Ishida A, Yorozuya Y, et al. The Feasibility and Efficacy of Social Cognition and Interaction Training for Outpatients With Schizophrenia in Japan: A Multicenter Randomized Clinical Trial. Front Psychiatry (2019) 10:589. doi: 10.3389/fpsyt.2019.00589
21. Kayser N, Sarfati Y, Besche C, Hardy-Bayle MC. Elaboration of a rehabilitation method based on a pathogenetic hypothesis of “theory of mind” impairment in schizophrenia. Neuropsychol Rehabil (2006) 16(1):83–95. doi: 10.1080/09602010443000236
22. Kendler KS, Gallagher TJ, Abelson JM, Kessler RC. Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Arch Gen Psychiatry (1996) 53(11):1022–31. doi: 10.1001/archpsyc.1996.01830110060007
23. Kopelowicz A, Liberman RP, Zarate R. Recent advances in social skills training for schizophrenia. Schizophr Bull (2006) 32 Suppl 1(Suppl 1):S12–23. doi: 10.1093/schbul/sbl023
24. Kravariti E, Morris RG, Rabe-Hesketh S, Murray RM, Frangou S. The Maudsley early onset schizophrenia study: cognitive function in adolescents with recent onset schizophrenia. Schizophr Res (2003) 61(2–3):137–48. doi: 10.1016/s0920-9964(02)00291-8
25. Lay B, Blanz B, Hartmann M, Schmidt MH. The psychosocial outcome of adolescent-onset schizophrenia: a 12-year followup. Schizophr Bull (2000) 26(4):801–16. doi: 10.1093/oxfordjournals.schbul.a033495
26. Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel RR. What does the PANSS mean? Schizophr Res (2005) 79(2–3):231–8. doi: 10.1016/j.schres.2005.04.008
27. Meltzer HY, Rabinowitz J, Lee MA, Cola PA, Ranjan R, Findling RL, et al. Age at onset and gender of schizophrenic patients in relation to neuroleptic resistance. Am J Psychiatry (1997) 154(4):475–82. doi: 10.1176/ajp.154.4.475
28. Murray GK, Clark L, Corlett PR, Blackwell AD, Cools R, Jones PB, et al. Incentive motivation in first-episode psychosis: a behavioural study. BMC Psychiatry (2008) 8:34. doi: 10.1186/1471-244x-8-34
29. Oberman LM, Ramachandran VS. The simulating social mind: the role of the mirror neuron system and simulation in the social and communicative deficits of autism spectrum disorders. Psychol Bull (2007) 133(2):310–27. doi: 10.1037/0033-2909.133.2.310
30. Ochsner KN. The social-emotional processing stream: five core constructs and their translational potential for schizophrenia and beyond. Biol Psychiatry (2008) 64(1):48–61. doi: 10.1016/j.biopsych.2008.04.024
31. Oie M, Rund BR. Neuropsychological deficits in adolescent-onset schizophrenia compared with attention deficit hyperactivity disorder. Am J Psychiatry (1999) 156(8):1216–22. doi: 10.1176/ajp.156.8.1216
32. Ojeda N, Peña J, Sánchez P, Elizagárate E, Ezcurra J. Processing speed mediates the relationship between verbal memory, verbal fluency, and functional outcome in chronic schizophrenia. Schizophr Res (2008) 101(1–3):225–33. doi: 10.1016/j.schres.2007.12.483
33. Ostrom TM (1984). “The sovereignty of social cognition” In: Handbook of Social Cognition, Vol. 1. doi: 10.4324/9781315807102
34. Penn D, Roberts DL, Munt ED, Silverstein E, Jones N, Sheitman B. A pilot study of social cognition and interaction training (SCIT) for schizophrenia. Schizophr Res (2005) 80(2–3):357–9. doi: 10.1016/j.schres.2005.07.011
35. Penn DL, Roberts DL, Combs D, Sterne A. Best practices: The development of the Social Cognition and Interaction Training program for schizophrenia spectrum disorders. Psychiatr Serv (2007) 58(4):449–51. doi: 10.1176/ps.2007.58.4.449
36. Perkins DO, Gu H, Weiden PJ, McEvoy JP, Hamer RM, Lieberman JA. Predictors of treatment discontinuation and medication nonadherence in patients recovering from a first episode of schizophrenia, schizophreniform disorder, or schizoaffective disorder: a randomized, double-blind, flexible-dose, multicenter study. J Clin Psychiatry (2008) 69(1):106–13. doi: 10.4088/jcp.v69n0114
37. Pilling S, Bebbington P, Kuipers E, Garety P, Geddes J, Orbach G, et al. Psychological treatments in schizophrenia: I. Meta-analysis of family intervention and cognitive behaviour therapy. Psychol Med (2002) 32(5):763–82. doi: 10.1017/s0033291702005895
38. Puig O, Penades R, Baeza I, De la Serna E, Sanchez-Gistau V, Bernardo M, et al. Cognitive remediation therapy in adolescents with early-onset schizophrenia: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry (2014) 53(8):859–68. doi: 10.1016/j.jaac.2014.05.012
39. Remschmidt H. Early-onset schizophrenia as a progressive-deteriorating developmental disorder: evidence from child psychiatry. J Neural Transm (Vienna) (2002) 109(1):101–17. doi: 10.1007/s702-002-8240-3
40. Revheim N, Schechter I, Kim D, Silipo G, Allingham B, Butler P, et al. Neurocognitive and symptom correlates of daily problem-solving skills in schizophrenia. Schizophr Res (2006) 83(2–3):237–45. doi: 10.1016/j.schres.2005.12.849
41. Roberts DL, Combs DR, Willoughby M, Mintz J, Gibson C, Rupp B, et al. A randomized, controlled trial of Social Cognition and Interaction Training (SCIT) for outpatients with schizophrenia spectrum disorders. Br J Clin Psychol (2014) 53(3):281–98. doi: 10.1111/bjc.12044
42. Rus-Calafell M, Gutierrez-Maldonado J, Ortega-Bravo M, Ribas-Sabate J, Caqueo-Urizar A. A brief cognitive-behavioural social skills training for stabilised outpatients with schizophrenia: a preliminary study. Schizophr Res (2013) 143(2-3):327–36. doi: 10.1016/j.schres.2012.11.014
43. Stafford MR, Mayo-Wilson E, Loucas CE, James A, Hollis C, Birchwood M, et al. Efficacy and safety of pharmacological and psychological interventions for the treatment of psychosis and schizophrenia in children, adolescents and young adults: a systematic review and meta-analysis. PLoS One (2015) 10(2):e0117166. doi: 10.1371/journal.pone.0117166
44. Strauss GP, Granholm E, Holden JL, Ruiz I, Gold JM, Kelly DL, et al. The effects of combined oxytocin and cognitive behavioral social skills training on social cognition in schizophrenia. Psychol Med (2019) 49(10):1731–9. doi: 10.1017/s0033291718002465
45. Vaskinn A, Sundet K, Hultman CM, Friis S, Andreassen OA. Social problem-solving in high-functioning schizophrenia: specific deficits in sending skills. Psychiatry Res (2009) 165(3):215–23. doi: 10.1016/j.psychres.2007.11.009
46. Ventura J, Subotnik KL, Ered A, Gretchen-Doorly D, Hellemann GS, Vaskinn A, et al. The relationship of attitudinal beliefs to negative symptoms, neurocognition, and daily functioning in recent-onset schizophrenia. Schizophr Bull (2014) 40(6):1308–18. doi: 10.1093/schbul/sbu002
47. Voutilainen G, Kouhia T, Roberts DL, Oksanen J. Social Cognition and Interaction Training (SCIT) for Adults with Psychotic Disorders: A Feasibility Study in Finland. Behav Cognit Psychother (2016) 44(6):711–6. doi: 10.1017/s1352465816000151
48. Werry JS. Child and adolescent (early onset) schizophrenia: a review in light of DSM-III-R. J Autism Dev Disord (1992) 22(4):601–24. doi: 10.1007/bf01046330
Keywords: social cognition and interaction training, cognition, social functioning, symptomatology, early-onset schizophrenia
Citation: Li Y, Sun K, Liu D, Chen M-X, Li G, Ma J and Zhang X (2020) The Effects of Combined Social Cognition and Interaction Training and Paliperidone on Early-Onset Schizophrenia. Front. Psychiatry 11:525492. doi: 10.3389/fpsyt.2020.525492
Received: 09 January 2020; Accepted: 20 August 2020;
Published: 30 September 2020.
Edited by:
Jing Sun, Griffith University, AustraliaReviewed by:
Padmavati Ramachandran, Schizophrenia Research Foundation, IndiaMarek Michał Jarema, Institute of Psychiatry and Neurology (IPiN), Poland
Zhi-You Cai, Chongqing General Hospital, China
Copyright © 2020 Li, Sun, Liu, Chen, Li, Ma and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaofan Zhang, emhhbmd4aWFvZmFuQGh1c3QuZWR1LmNu; Jun Ma, MTcyODc3NTI0OUBxcS5jb20=
 Yichen Li1
Yichen Li1 Mo-Xian Chen
Mo-Xian Chen Xiaofan Zhang
Xiaofan Zhang