- 1Clinical Psychology and Psychotherapy, Department of Psychology, Bielefeld University, Bielefeld, Germany
- 2vivo international, Konstanz, Germany
- 3Department of Clinical Psychology and Biopsychology, Catholic University Eichstätt-Ingolstadt, Eichstätt, Germany
Background: In low- and middle-income countries (LMIC), the mismatch between the number of individuals needing and those receiving treatment for alcohol use disorders (AUD) is substantial. In order to provide suggestions for the scaling up of effective service provision we systematically reviewed the current evidence on the effectiveness of AUD-focused psychosocial interventions in LMIC.
Methods: We used a systematic review methodology following the PRISMA guidelines. Twelve electronic databases listing published and grey literature were searched and only randomized-controlled trials (RCTs) were included. Where possible, effect sizes were calculated using Hedges' g indices.
Results: Twenty-one RCTs conducted in 15 different LMIC between 1992 and 2018 fulfilled inclusion criteria. Most studies employed brief one-on-one interventions facilitated by trained primary care staff. Eighty-six percent of RCTs based their interventions on the principles of motivational interviewing (MI) with the majority supplementing MI-based interventions with alcohol-tailored elements of cognitive-behavioral therapy (CBT). The remaining RCTs employed CBT-components exclusively. Just over 40% of studies included in quantitative analyses (n=17) yielded an at least medium-sized effect (g≥.50) of the respective intervention compared to alcohol-related and unrelated control conditions or waiting list. Only half of the trials implementing the widely applied MI-based approaches (or MI-based approaches blended with CBT-elements) were superior to their respective control conditions.
Conclusion: To date, a relatively small number of RCTs investigating AUD-focused treatments has been conducted in LMIC. The majority of between condition effect size estimates were small and no type of intervention can clearly be recommended over another. No RCTs were conducted in conflict-affected areas in LMIC although they would merit particular attention since AUD is often linked to trauma-related mental health disorders. More RCTs in LMIC are required and alternatives to MI-based approaches should be investigated. This systematic review summarizes properties of effective interventions and provides implications for future research.
Introduction
Excessive alcohol use and the resulting consequences pose a major challenge to health systems globally, and particularly to those of low- and middle-income countries [LMIC; defined according to World Bank country classification (1)]. The most recent World Health Organization (WHO) status report on alcohol and health (2) found that, although most alcohol per capita is consumed in wealthier countries, the alcohol-attributable burden of disease (3) per unit of consumed alcohol is higher in LMIC [e.g. (4, 5)]. A higher burden of disease implies higher morbidity and mortality risks due to diseases for which alcohol has a detrimental effect, including cardiovascular diseases, cirrhosis of the liver, neuropsychiatric disorders, and unintentional injuries. In developing settings poor living conditions and limited access to health care can perpetuate and exacerbate such medical conditions and thus further increase the burden of disease (3, 6). Other factors strongly associated with a higher burden of disease include risky and potentially harmful patterns of drinking (e.g. drinking to intoxication, drinking in public places) which were found to be more prevalent in LMIC compared to upper middle- and high-income countries with comparable levels of consumption (7, 8). Furthermore, unrecorded alcohol consumption (i.e., home-made alcohol, illegal alcohol products, or alcohol not officially made for human consumption) is widespread in LMIC, and Rehm and colleagues (9) presume detrimental health consequences beyond the impact of ethanol alone.
Although individuals with severe alcohol-related problems or alcohol dependence are at the highest risk of experiencing such alcohol-attributable harm, the burden on health care and social systems resulting from non-dependent, but harmful or hazardous use, is assumed to be even greater with the majority of alcohol-related problems attributable to this group of drinkers. This is not surprising since harmful or hazardous drinkers simply constitute the much larger group within a population [e.g. (10)]. The WHO defines hazardous drinking as “pattern of alcohol consumption that increases the risk of harmful consequences for the user or others,” and harmful alcohol use as “alcohol consumption that results in consequences to physical and mental health” (11).
Epidemiological research from LMIC has revealed very high prevalence rates of hazardous, harmful, or dependent drinking, reaching up to 28% in Tanzania (12), 22% in India (13), 40% in Namibia (14), 31% in Ethiopia (15), and 21% in Uganda (16). Studies predominantly used male, random or convenience samples from the general population. Special concern has been raised about alcohol consumption among LMIC-populations affected by conflict and/ or forced displacement (17) where even higher rates of risky drinking have been found, though the evidence base is still generally weak [for reviews see: (18–20)]. More recent epidemiological studies investigating prevalences of hazardous drinking among refugees, internally displaced persons (IDP) and former IDPs found high rates of 23% in Nepal (21), 28% in Georgia (22), and 32% (23), respectively 46% (24) in Northern Uganda.
While the alcohol-attributable health and economic burden placed upon affected populations is significant, the strains related to social harm are just as immense. From an economic perspective, impaired health is resulting in the loss of productivity of affected individuals thereby contributing to the persistence of poverty of whole regions (3, 25, 26). Furthermore, financial problems due to alcohol consumption and stigmatization are adverse effects not limited to the individual drinker, but directly affecting his or her family as well. Often, families of alcohol abusers are unable to pay for their children’s education, experience undernutrition, lack other essential needs, and experience marginalization and isolation (27–30).
Beyond impacting the family’s material needs, alcohol abuse has detrimental effects on the mental health of the drinkers themselves and of the individuals living with them. Proximal effects of drinking, such as impaired cognitive functioning and emotional lability, act as potential facilitators of tension and conflict within families (31, 32). Moreover, research including some studies from LMIC, frequently suggests associations between alcohol abuse and comorbid psychopathology such as depression, anxiety disorders, suicidal ideation, and posttraumatic stress disorder [PTSD; (5, 33–35)]. Various pathways have been hypothesized to explain this relationship linking hazardous drinking to the development, maintenance and exacerbation of psychological problems [e.g. (36)]. Moreover, studies have shown high levels of psychological distress among family members of alcohol abusers as well as dysfunctional family dynamics including multiple forms of violent behavior. In several LMIC-based studies, alcohol-related symptoms are among the most consistently found risk factors for intimate partner violence [IPV; e.g. (37–40)] and violence against children (41). In ongoing and post-conflict areas the relationship between excessive drinking and domestic violence seems to be magnified (42), which is particularly detrimental for LMIC-settings where the majority of the world’s most violent crises are currently taking place (43). This relationship has emerged even in studies controlling for traumatic experiences and psychopathologies in male respondents [in Sri Lanka (44) and Uganda (45, 46)].
High prevalence rates and severe negative consequences indicate the urgent need for alcohol-focused interventions in LMIC-settings as well as their scientific evaluation. With the launch of the Mental Health Gap Action Programme [mhGAP; (47)] in 2008 the WHO drew attention to the substantial mismatch between the number of people needing treatment and those receiving treatment for alcohol use disorders (AUD) in low-resource contexts. In fact, among all mental disorders, globally, the treatment gap for AUD was found to be the widest with nearly 80% of affected individuals remaining untreated (47), most of them residing in LMIC. This finding was replicated in a more recent cross-sectional study conducted in four LMIC where the population-level treatment gap was estimated to be between 94.9% and 97.2% for AUD (48). The research base on the efficacy of alcohol treatments delivered in high income countries (HIC) is quite substantial with numerous studies evaluating screening and brief intervention (SBI) programs; a concept involving systematic screening procedures plus structured interventions of short duration [1–4 sessions (11)]. Counseling approaches based on motivational enhancement, in particular, have been extensively examined and are recommended as first-line interventions by WHO’s mhGAP for implementation in routine health-care settings, though evidence on their effectiveness is mixed [for reviews see e.g. (49, 50)]. The most commonly used rationale is the principle of motivational interviewing (MI) which was first proposed by Miller in 1983 and then further elaborated by Miller and Rollnick in 1991 and constitutes a “guiding style for enhancing intrinsic motivation to change” (51). In further research, a number of elements were found to be recurring features in effective brief interventions. These features, represented by the acronym FRAMES: Feedback, Responsibility, Advice, Menu, Empathic, and Self-efficacy (52, 53), have subsequently been used by the WHO-affiliated brief alcohol interventions and are still referenced by brief interventions today. Other common interventions applied in HIC-trials include simple structured advice, cognitive behavioral therapy, or giving out leaflets on alcohol consumption [e.g. (54)].
Despite the evident global health significance of the issue, there is a lack of comprehensive review-level data regarding the effectiveness of AUD-focused interventions in LMIC. There are plenty of reviews condensing findings from high-income countries [e.g. (55–59)] with few including some data from trials based in developing and transitional countries [e.g. (60–65)]. However, as alcohol researchers have emphasized [e.g. (66, 67)], findings derived from HIC may not be generalizable to LMIC settings due to a number of reasons, including context-specific health issues, structural differences regarding the availability of resources, variations in drinking patterns and types of alcohol, and the severity of alcohol-related symptoms and consequences. A small number of reviews focused exclusively on alcohol treatments in LMIC, however, these do not include effect size calculations or do not describe systematic literature searches (66, 68). Furthermore, such reviews are divergent in scope as they focus on LMIC within specific geographical regions such as Sub-Sahara Africa (69, 70) or solely on middle-income countries (71). Others address wider spectrums of mental (72) or substance use disorders in general (73, 74) with alcohol being only one aspect. To our knowledge, reviews on alcohol intervention trials based in conflict-torn populations are, to date, nonexistent with only a few authors trying to raise awareness on the topic [e.g. (18, 24, 75, 76)]
With this review we aim to give an updated comprehensive overview of the currently implemented psychosocial interventions, its components, and their current state of evidence to serve as an orientation for practitioners as well as for future intervention trials. Therefore, the objective of the present study is to systematically review treatment trials aiming to reduce hazardous and harmful drinking and alcohol-related symptoms in LMIC and to summarize the evidence regarding their effectiveness.
Methods
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (77) [see Supplementary Figure 1 for the PRISMA checklist]. We did not preregister this systematic review, however, we had a predefined review question, search strategy, inclusion and exclusion criteria, and risk of bias assessment strategy following the Cochrane guidelines for systematic reviews of interventions (78).
Search Strategy and Inclusion/Exclusion Criteria
The search for eligible intervention studies was undertaken in the electronic databases PsychINFO, PubMed, PSYNDEX, Web of Science, Google Scholar, Cochrane Library (CENTRAL) using combinations of the following search terms: alcohol OR drink* AND treatment OR intervention OR program OR therapy AND “low- and middle-income countr*” OR “low-income countr*” OR “middle-income countr*” OR “developing countr*” OR “post-conflict” OR war OR “post-war”. In order to avoid the potential for publication bias an explicit search for grey literature (i.e., unpublished reports, master and dissertation theses) was conducted in the following databases using the same search terms described above: DissOnline, DART-Europe, EthOS, OATD, ProQuest, and Open Grey. Furthermore, prospective trial registration databases (Clinicaltrials.gov, ISRCTN Registry, INEBRIA, WHOLIS, PACTR) were searched for intervention research projects that fit the purpose of the review in terms of intervention focus and outcomes in order to overcome time-lag bias. Authors of such projects were contacted requesting any conference contributions, unpublished reports or manuscripts in preparation or under review they would be willing to provide. There were no limitations regarding the publication dates of the studies. The search was conducted up to August 5th, 2019.
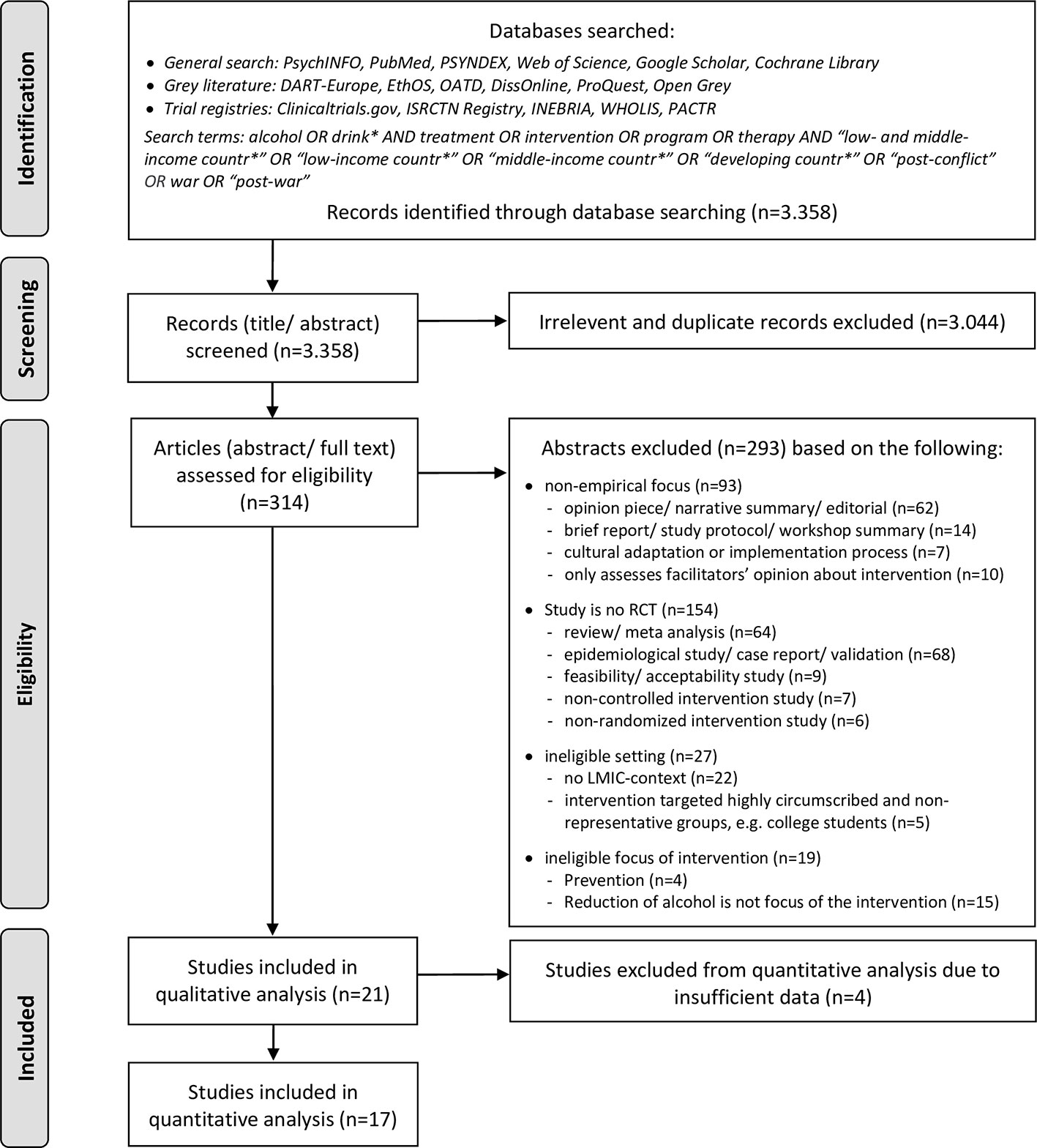
The inclusion criteria were oriented along the PICOS (populations, interventions, comparators, outcomes, study designs) elements. Regarding the populations (P), the studies had to address individuals identified as hazardous or harmful drinkers through systematic clinical screening procedures. Due to the fact that many studies defined lower but not upper limits for their screening instruments (even if explicitly aiming at hazardous or harmful and not dependent drinkers) we were unable to exclude studies whose samples included dependent drinkers. Therefore, we decided during the process that determining dependent drinking as an excluding factor was not practicable, although we had previously considered this restriction. The presence of comorbid disorders (including abuse of other substances apart from alcohol) was not an exclusion criterion. Our aim was to identify intervention studies that recruited participants in primary health care, social care, or community-based settings in LMIC. We excluded treatment trials which targeted highly circumscribed subgroups that did not represent general LMIC populations, mainly particularly privileged groups such as university students. In terms of interventions (I), we applied the following inclusion criteria: psychosocial intervention specifically aiming to reduce consumption of alcohol, implemented in a low- or middle-income country [according to World Bank country classification (1)]. Interventions applied within other health programs (i.e., reproductive health programs, HIV-programs) were not excluded from the present review as long as the intervention focus included the reduction of alcohol use and respective outcomes were assessed. The simultaneous treatment of other drugs was also not an exclusion criterion as long as participants were also screened and treated for hazardous alcohol use. We excluded intervention trials targeting the “alcogenic environment” instead of individuals. For example, programs controlling availability or promotion of alcohol or trials evaluating the establishment of new policies were excluded from the present review. There were no restrictions regarding the type of comparison conditions (C). In terms of outcomes (O), eligible studies had to include at least some quantity- or frequency measure of alcohol consumption or a standardized scale assessing alcohol-related symptoms. Regarding study designs (S), we only included randomized-controlled trials, including pilot- and cluster-RCTs as the objective of the current review was to identify the best clinical evidence available for outpatient alcohol intervention components in LMIC. A total of 3.358 articles were identified from electronic database searching. As a first step, titles and abstracts were screened to remove irrelevant reports as well as duplicates, leading to 314 eligible abstracts. In a second step, these were analyzed against a priori set inclusion and exclusion criteria. In the event the information in the abstract was insufficient to determine inclusion or exclusion, the full text was retrieved and scanned. The final determination of whether a study met the eligibility criteria was made by two authors (MP, VE). Disagreements about whether a study was to be included were resolved by discussion. After analysis of the abstracts and/ or full texts, 293 studies were excluded. Most of them were non-empirical reports, non-RCTs or were excluded because of their non-LMIC setting (see Figure 1 for details). The search resulted in a total number of 21 intervention studies. One study was a multicenter trial which applied the same research design and intervention in 10 different countries of which six were LMIC (79). We refer to it as one study throughout the text unless stated otherwise. An overview of the selection process is presented in Figure 1.
Data Extraction and Analysis
Data was extracted on selected study-level characteristics for each primary study. Investigators were contacted to request data not available within the publications. Due to the heterogeneity of outcome assessments used across the studies and due to the large disparity regarding settings of recruitment, severity of alcohol-related symptoms, intervention intensities, and facilitators’ backgrounds, skill levels and trainings, combining outcomes into pooled effect sizes or other meta-analytic measures was not feasible. Instead, for studies which allowed us to do so, we calculated effect sizes based upon the most frequently applied outcome variables. These were grouped into two main categories: (1) alcohol-related symptoms using standardized assessment scales [i.e. Alcohol Use Disorder Identification Test, AUDIT (80) or Alcohol, Smoking and Substance Involvement Screening Test, ASSIST (81)] and (2) alcohol amount consumed per defined unit (i.e., grams of ethanol consumed within a set time frame, typically per day or per drinking day). In the event a study reported more alcohol-related outcomes beyond these categories, preference was given to the dependent variable belonging to (1) or (2) in order to increase uniformity. When a study reported outcomes from both main categories we calculated effect sizes for both of them. We used the continuous outcome that was most similar to one of the two main categories (e.g. number of days or times alcohol was drunk within a certain time frame) only for studies that did not report outcomes categorizable into any of the two categories and where no relevant data was available after contacting the authors and grouped them under (3) other outcomes. To further improve comparability between effect size values we only included outcomes assessed on either one or both of the most frequently used follow-up (FU) time points, which were 3 and 6 months post-enrollment or -intervention. Consequently, shorter or longer assessment points (4–8 weeks, available in three studies; 12 months, available in three studies) were not considered for quantitative analyses.
Whenever possible, we calculated two types of effect size values for each study: within-condition effect sizes comparing pre- and posttreatment means in the intervention groups to assess main effects of intervention over time, and between-condition effect sizes comparing intervention and comparison groups on group x time interaction effects. We further segregated effect sizes according to comparison condition. Comparison conditions were categorized into control groups that did not focus on alcohol use in any way (alcohol-unrelated control groups; e.g. interview assessments only, nutrition intervention, wellness promotion, routine medical care) and those that did provide some information or advice concerning drinking (alcohol-related control groups; e.g. psycho-education on hazardous alcohol use, education leaflets informing about responsible drinking, simple advice to cut down on drinking, personalized feedback on AUDIT-score). For studies which employed different experimental add-on conditions (e.g. MI-based intervention in one group and MI-based intervention complemented by cognitive-behavioral techniques in the other group), we included both conditions in the effect size calculations.
According to Lakens’ (82), effect sizes for correlated or dependent measurements (within-condition effect sizes) and independent measurements (between-condition effect sizes) should be computed as Hedges' g indices. Lakens (82) recommends the use of Hedge’s g over Cohen’s d as the Bessel-correction makes it a less biased measure in the estimation of the population variance. Following Lakens suggestion we used Hedge’s gav for within-treatment-condition and Hedge’s gs for between-condition effect sizes. Hedge’s gav uses the average standard deviation as a standardizer while Hedge’s gs uses the pooled standard deviation. All effect sizes were calculated using Lakens’ (83) calculation sheet for effect sizes. For the interpretation of Hedge’s g coefficients the commonly used benchmarks (84) of small (d ≥ .20), medium (d ≥ .50), and large (d ≥ .80) as well as very large [d ≥ 1.30; (85)] effect sizes were applied. Where numeric information required for the calculation of effect sizes was insufficient or not available in the published article or by contacting the authors (e.g. missing standard deviations) we excluded the study from the quantitative, but not qualitative analysis. Regarding missing participant data, we employed the type of data that was available in the published articles for calculation of effect sizes. If both intention-to-treat and complete case data were available preference was given to intention-to-treat data.
Assessment of Methodological Quality
Assessment of risk of bias was guided by the Cochrane Collaboration’s Risk of Bias Tool [CCRBT; (86)]. The tool suggests different domains of potential bias: selection bias (adequacy of randomization and allocation concealment), performance bias (blinding of participants), detection bias (blinding of outcome assessment), attrition bias (amount, nature or handling of incomplete outcome data), and reporting bias (due to selective outcome reporting). The assessment involves categorizing studies as having a low, high, or unclear risk of bias in these areas using the set of criteria listed within the tool. As blinding of intervention facilitators is virtually impracticable in trials involving behavioral interventions, within the category of performance bias we only assessed risk of bias regarding the extent to which subjects knew about their allocation and the potential bias associated with this knowledge. For studies where treatment manuals were used intervention procedures described in studies were cross-checked for adherence to the procedures described in the respective manuals.
Results
Study Characteristics
Twenty-one studies met our inclusion criteria. Years of publication ranged between 1992 (79) and 2018 (87) with 18 articles published in or after 2010.
Countries and Settings
The interventions were implemented in 15 different LMIC. Although the trial settings were quite diverse, the majority of alcohol interventions were integrated into routine primary care services or were conducted within established health promotion or disease prevention programs at community health centers.
Participants
Across all studies, a total of 6.488 participants were randomized to the trial conditions with total sample sizes per study ranging from 75 to 1,196 participants. Out of the studies that reported their participants’ mean age the youngest sample was 21.8 years old [SD=2.6; (88)] and the oldest sample’s average age was 42.0 years [SD=11.4; (89)]. The subjects of two trials (10%) were males only, three trials (15%) recruited only females, and the remaining 16 trials (76%) included subjects of both sexes.
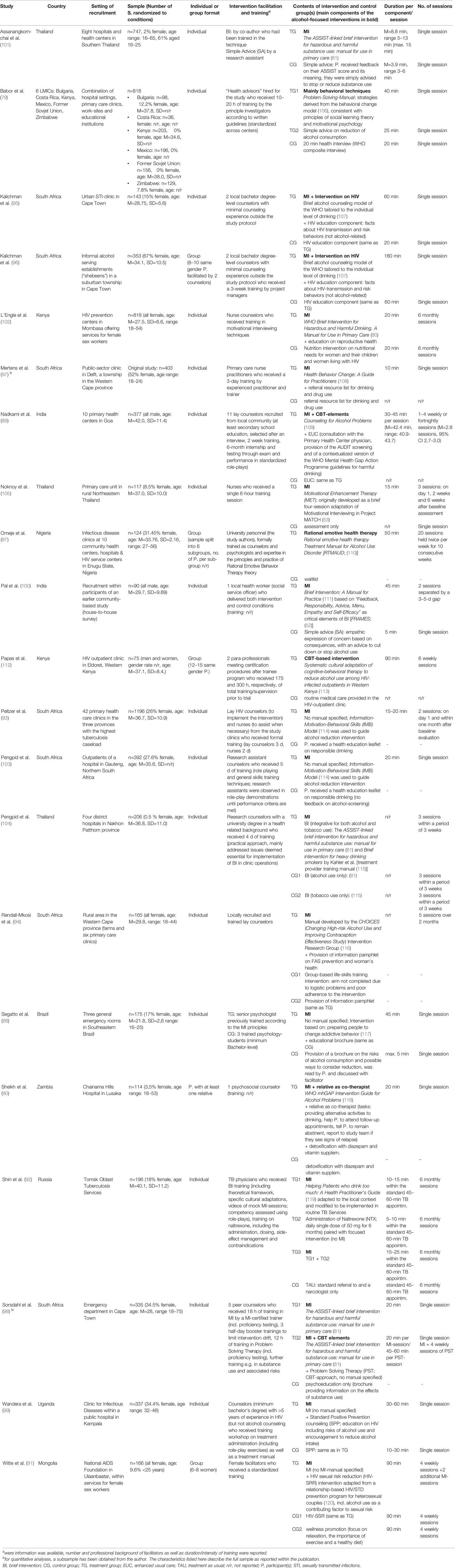
Apart from the wide range of general inclusion criteria there was also substantial variation across the studies regarding their alcohol-related eligibility criteria. The majority of studies used interviewer-administered standardized self-report instruments, mostly AUDIT and ASSIST, however, studies were not consistent with regard to applied cut-off-scores. The diversity of alcohol-related inclusion criteria accounted for a rather heterogeneous overall sample in terms of symptom severity. The samples of six studies either completely (90, 91) or partially [40% (88), 63% (92), 73.2% (93), and “about 50%” (94)] consisted of alcohol-dependent individuals. In eight studies, dependent drinking is neither controlled for nor explicitly addressed, although the respective samples are likely to include dependent drinkers as the studies either used lower but no upper screening limits (95–99), did not specify a cut-off score at all (87), or used an upper score potentially including dependent drinkers (100). The remaining seven studies employed procedures attempting to rule out the presence of alcohol-dependence among participants by either adhering to the upper cut-off scores proposed in the screening tool manuals (89, 101–104) or determining clinical judgment of alcohol dependence as an excluding factor (79, 105). An overview of countries, settings and sample characteristics is given in Table 1 as well as in Supplementary Table 1.
Intervention Characteristics
Lengths and Intensities
All but one study evaluated interventions that qualified as “brief” (1–4 sessions) or “moderate” length (5–7 sessions) following Babor’s (11) definition. With 20 group therapy sessions, the study by Omeje et al. (87) qualifies as “intensive” treatment and thus is by far the study with the highest intervention exposure which must be kept in mind when interpreting the results. For the 17 studies employing individual therapy formats the number of sessions in the treatment groups ranged from one to six sessions with nine interventions consisting of a single session only. Individual sessions lasted between 10 and 60 min, while total intervention exposure time over all sessions ranged from 10 min (97) to approximately 4 h (98). Four trials used group therapy formats (87, 91, 96, 112) with the number of sessions in the treatment groups ranging from 1 to 20 sessions and total intervention exposure time over all sessions ranging from 3 h (96) to 16 h and 40 min (87).
Therapeutic Components
The majority of trials (n=18) based their interventions on the principles of MI with most of them explicitly referring to Miller and Rollnick’s MI-rationale (117, 121). MI-based treatments varied with regard to specific techniques, arrangement of components, and intensities. Miller and Rollnick (122) emphasize that MI was not a technique in and of itself and neither was there a step-by-step script to follow when employing it. Accordingly, MI-based interventions were not structured into consecutive components but into communication styles and core skills. However, in order to systemize the elements emerging from the 18 trials using elements of MI, we categorize them into four components comprising the most frequently used topics as well as corresponding techniques. First, the strategy of providing participants with a personalized feedback on the result of alcohol related screening and illustrating its meaning was used in the majority of trials [e.g. (89, 91) and all ASSIST-based interventions]. Miller and Rollnick (122) emphasize that personalized feedback was not an essential component of MI, although widely assumed as such. Second, the provision of structured information about alcohol use generally plays a major role in all MI-based trials. In all trials, participants in the experimental groups received general psychoeducation about the consequences of alcohol on physical and mental health, either verbally within the counseling setting [e.g. (98)] or in the form of written material [e.g. (88)]. In trials that embedded MI-based treatments into other health programs, the information component was often specific for alcohol consumption in relation to the respective health issue, such as education on how alcohol affects communication skills and sexual behaviors and increases risk for HIV or sexually transmitted infections [STI; e.g. (91, 99)]. The third component is also found in all MI-based trials in this review and includes the elicitation of the participant’s ambivalence, participant-perceived importance of and confidence in achieving the behavior change, and the subsequent enhancement of all three states. To facilitate these objectives, a variety of structured techniques were employed across the studies with the aim of evoking the participant’s own motivation to reduce drinking and confidence in succeeding (“change talk”). These include (group) discussions about pros and cons of change [e.g. (105)], role-plays to practice how to behave in alcohol-related “high-risk situations” (96), or the explicit recognition of prior attempts to cut down (99). Finally, the fourth component frequently employed across the 18 MI-based trials comprises techniques helping participants to plan their behavior change in detail and set specific and appropriate goals. Examples are the development of a “habit-breaking plan” (102), helping participants identify their personal aim (e.g. reduced drinking vs. abstinence) and planning measurable goals in changing drinking behavior [e.g. (105)]. Furthermore, Miller and Rollnick (51) emphasize the “cooperative and collaborative partnership between patient and clinician” as a key principle and foundation necessary for the therapeutic skills and styles to have an effect. To account for that, most MI-based studies in this review used expressions such as “client-centered” [e.g. (99)] to describe their facilitators’ general attitude toward the participants, “empathic counseling style” [e.g. (105)] as a method to establish good rapport, and “reflective listening” [e.g. (99)] or “open-ended questioning” [e.g. (89)] as communication styles to be employed by the practitioners.
Among the 18 studies employing an MI-based approach, only six used it as stand-alone intervention without any further additional components (88, 97, 100, 101, 104, 105), while the remaining used the MI-based approach as one method and blended it with other treatment components extending beyond the scope of MI. Two studies (89, 98) delivered cognitive and behavioral components within their MI-frameworks, with examples being problem-solving, drink refusal skills training, and handling of peer pressure or difficult emotions. The interventions conducted by Peltzer et al. (93) and Pengpid et al. (103) were informed by the Information-Motivation-Behavioral Skills (IMB) model (114) which integrated behavioral (but not cognitive) elements into the MI-framework, namely “behavioral skills related to preventive actions” (not further specified) (103). One study enhanced the MI-based intervention through administration of the opiate antagonist Naltrexone for the prevention of relapse (92) and one established the active integration of a close family member into the intervention (90). Furthermore, some studies combined their MI-based intervention with non-alcohol-related psychosocial interventions for health topics such as TB (92, 93), reproductive health for female sex workers (102), or HIV (91, 96, 99).
Three trials did not or did not explicitly describe employing elements of MI. One of them was the WHO multinational study that conducted a brief intervention based on a problem-solving model using mainly behavioral techniques (79). The study by Papas and colleagues (112) exclusively applied a cognitive-behavioral approach without explicitly mentioning motivational elements. Finally, in the study by Omeje et al. (87) the authors used an adaptation of Ellis’ rational emotive behavior therapy (123) which, apart from cognitive and behavioral elements, included “emotive” techniques such as satiric songs related to alcohol and other humorous methods with the intention of generating feelings that help to challenge and change dysfunctional attitudes toward drinking. Almost all studies implemented manualized intervention approaches.
Intervention Facilitators
Most interventions were conducted by trained lay counselors such as nurses, clinic staff, health workers, or other paraprofessionals, most of them with no or only minimal prior experience in counseling. Some trials formally required the facilitators to have at least a secondary school or a university degree. The majority of studies specified their training procedures. Among those, training intensities ranged widely from 6 h to 300 h or even a 6-month-trainee-program followed by formalized certification procedures (89). Fourteen trials offered weekly, bi-weekly, or monthly supervision to the facilitators, mostly conducted by the project’s principle investigators, clinical supervisors, or peer lay counselors.
Comparison Conditions
Apart from a non-alcohol vs. alcohol-focus, the comparison conditions differed greatly regarding their intensities and modalities. Only three studies employed active comparison conditions representing state-of-the-art alcohol interventions (89, 98, 104) and five studies compared the experimental intervention with minimal interventions using the simple provision of advice concerning the reduction of drinking. Other comparison conditions consisted of the treatment considered as “usual care” in the facilities where the study was conducted such as referrals to physicians, the delivery of written material on alcohol consumption, nutrition or wellness promotion interventions, medical detoxification, and assessment-only. For detailed information about the characteristics of intervention and control conditions including manuals and facilitators see Table 1 as well as Supplementary Table 1.
Duration of Trials and Retention Rates
Across the 21 trials, post-treatment assessment time points of alcohol-related measures were reported referring either to post-enrollment (n=9) or post-intervention (n=12). They were conducted anywhere from 1-month to 12-months post-enrollment or -treatment, with most trials conducting assessments at least two points in time. Most studies assessed participants at either 3 or 6 months after enrollment or intervention. The median reported retention rate was 80% (range: 39%–93%) for 3-months FU-assessments in the experimental groups and 84.5% (range: 54%–97%) in controls. For 6-months FU-assessments the median reported retention rate was 74% (range: 59%–98%) in the experimental groups and 85% (range: 56%–96%) among the control groups. Attrition rates typically increase with trial duration. Interestingly, this was not the case here, since out of the eight studies reporting retention rates for both 3-months and 6-months FU-assessments five studies (95, 96, 99, 103, 105) had higher retention rates at the 6-months FUs compared to the 3-months FUs. The same was true for all three 12-months FU-assessments compared with the 6-months (102, 103) and 3-months (94) FU assessments of the respective studies. See Table 2 for an overview of trial durations and retention rates for studies included in quantitative analyses.
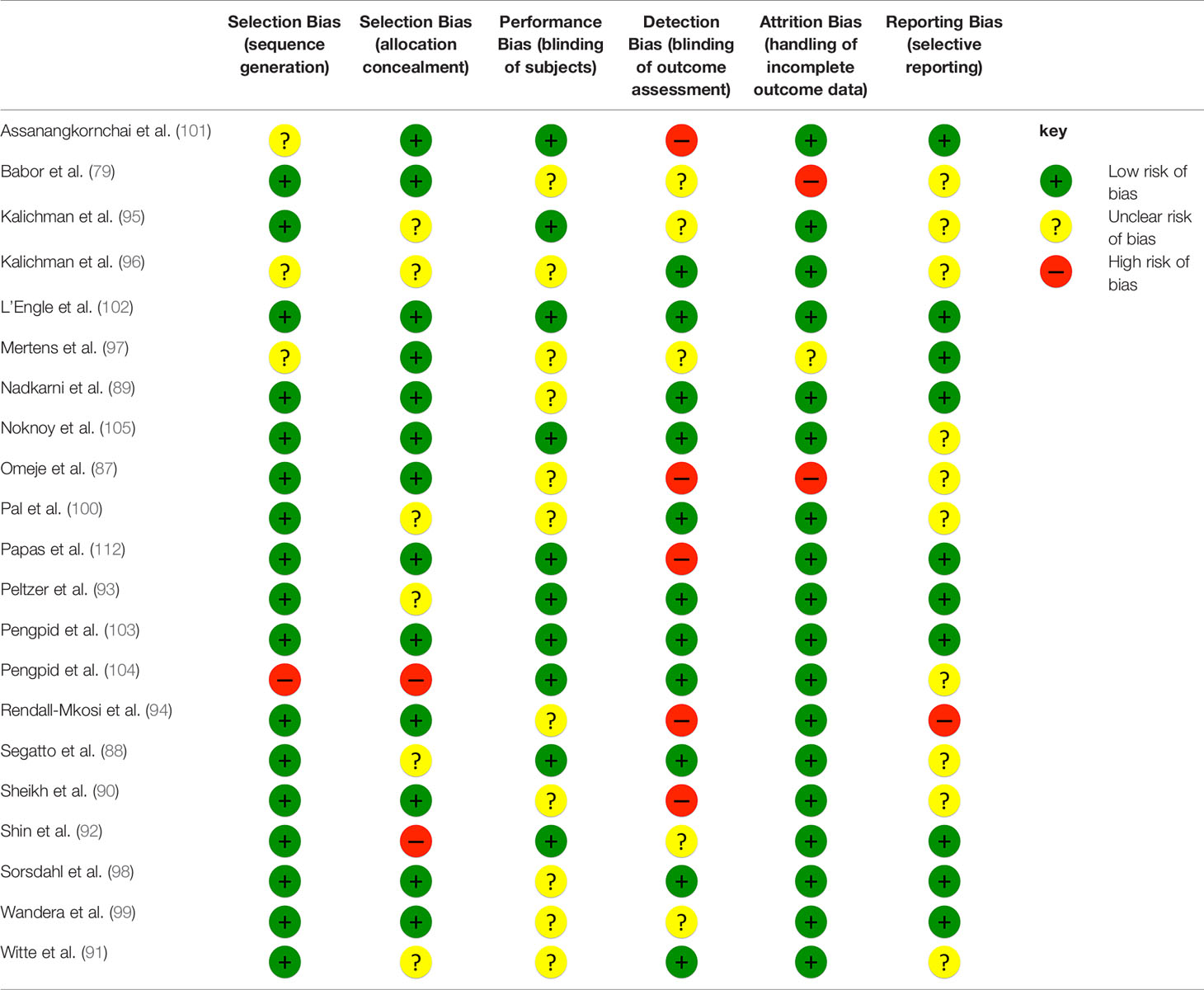
Risk of Bias
The methodological quality of the included RCTs was variable. For some cases an unfavorable rating has to be put into perspective, since trials were conducted over a 25-year period. An overview of all risk of bias judgments is displayed in Table 3 and a detailed version including reasons for ratings can be found in Supplementary Table 2.
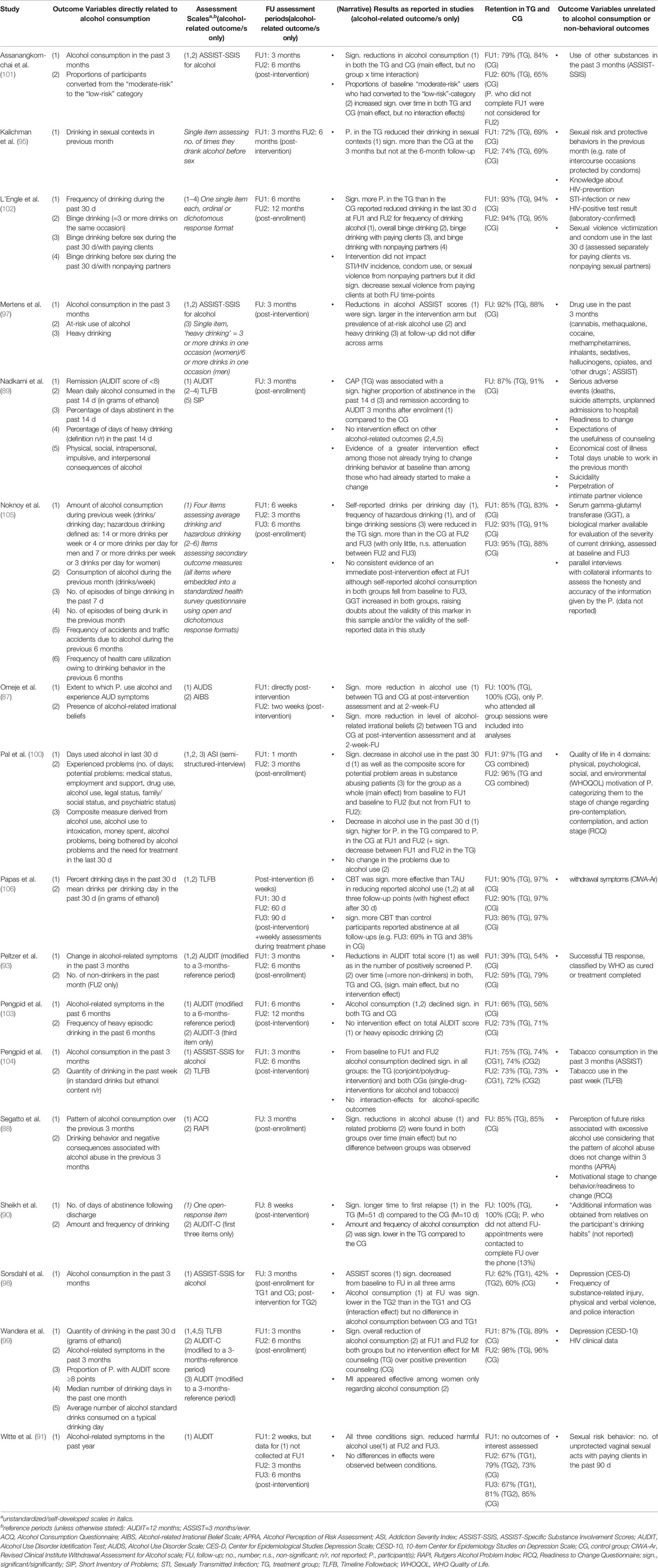
Outcome Measures
The included studies employed a wide variety of outcome measures. Effects were reported on more than 30 different alcohol-related outcome variables, including measures of frequency, amount and patterns of alcohol consumption, alcohol-related symptoms, binge drinking occasions, dependency symptoms, alcohol-related irrational beliefs, and problems resulting from drinking. These were measured using about 20 different assessment instruments including standardized clinical screening tools, timeline-followback interview assessments (TLFB), and self-developed scales. The most frequently employed instruments were the AUDIT and the ASSIST, both measuring frequency, amount and patterns of alcohol consumption, and alcohol-related symptoms. For details on measured outcome variables and applied instruments see Table 2 and Supplementary Table 1.
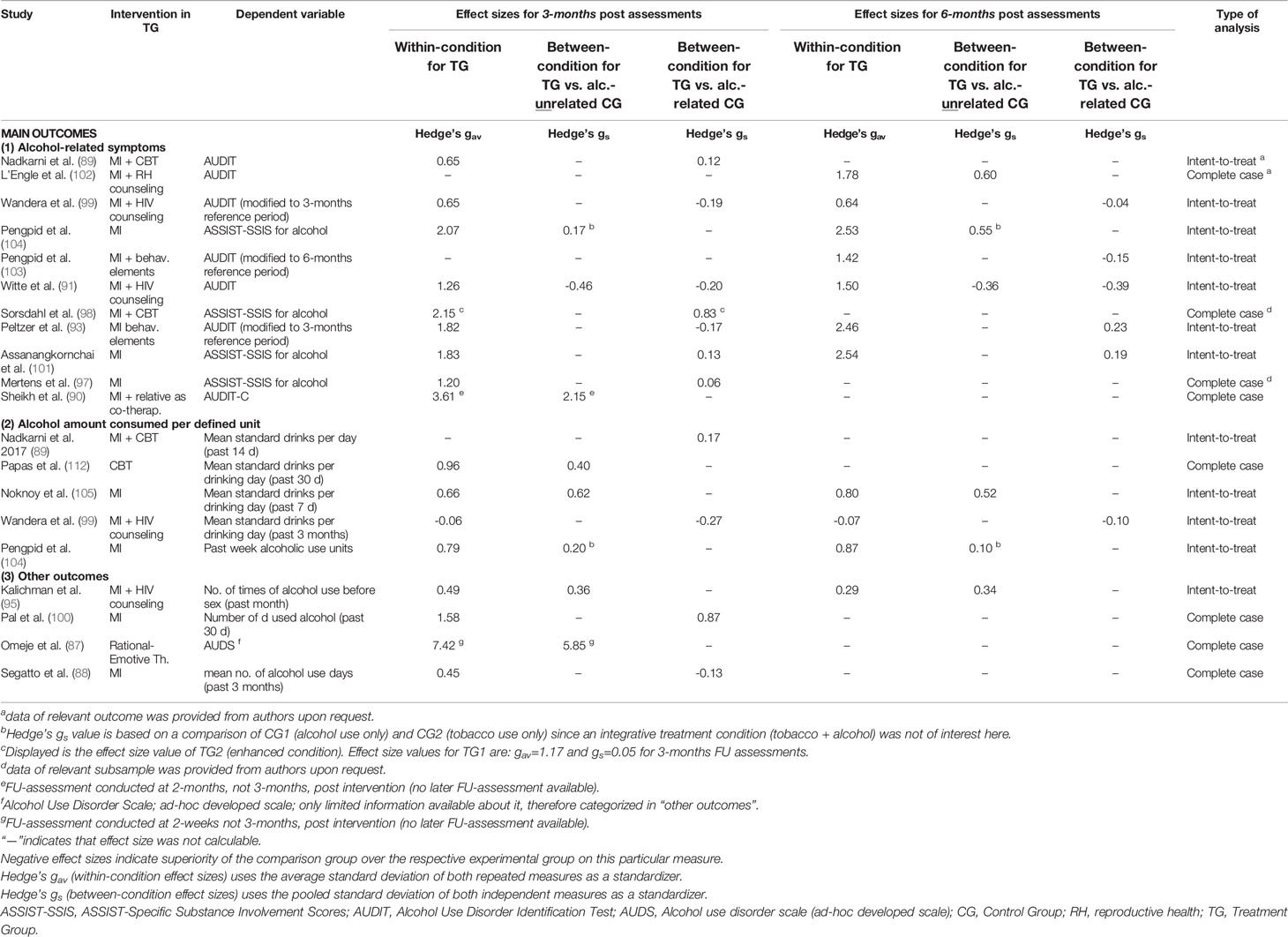
Main Results of Quantitative Analyses: Effect Sizes
Among the 17 studies included in the quantitative analyses 11 reported outcomes from the category alcohol-related symptoms, five from the category alcohol amount consumed per defined unit, and three studies reporting outcomes from both main categories. Four studies reported none of the two measures and therefore entered analyses with other alcohol-related outcomes (see Table 4 for details). In terms of assessment time points, 14 studies reported a 3-month FU and nine studies reported 6-month FU measurements, and eight studies reported both. Only two studies did not assess outcomes at any of the two time points and therefore entered analyses with their 2-month (90) and 2-week (87) FU assessments instead. Enhanced treatment conditions relevant for this review were conducted only by Sorsdahl et al. (98) and the respective results of this condition were utilized for effect size calculations. Positive effect sizes indicate that the intervention was more effective than the control condition in reducing alcohol-related symptoms and vice versa for negative effect sizes. All effect sizes are displayed in Table 4.
Alcohol-Related Symptoms
Among the 11 intervention trials which reported an outcome from the category alcohol-related symptoms, all 11 within effect size values (Hedge’s gav) indicated positive effects for the treatment conditions with the majority of effect size values being larger than gav>1.0. This was the case for both, 3-months (range: 0.65–3.61) and 6-months (range: 0.64–2.54) FU-assessments compared to baseline.
Between-group effect sizes (Hedge’s gs) comparing the focus intervention with an alcohol-unrelated control group (n=3 studies) ranged widely for the 3-months FU-assessment. We found a superiority of the control group for Witte et al. (91) (gs= −.46), no effect for Pengpid et al. (104) (gs = .17), and a very large between-group effect for Sheikh et al. (90) (gs = 2.15). In the case of Pengpid et al. (104), however, the intervention effect increased toward a medium sized effect measured on the ASSIST scale 6-months post-intervention (gs = .55).
Comparisons with alcohol-related control groups revealed negative to small between-condition effect size values at 3-months (n = 6; range: −.20 to .15) and 6-months (n = 5; range: −.39 to .23) FU-assessments with the highest value (gs = .23) calculated for Peltzer et al.’s (93) intervention at their 6-months FU.
Alcohol Amount Consumed Per Defined Unit
Based on five RCTs that measured the amount of alcohol consumption per defined unit within-condition effect sizes ranged from gav = −.06 to 0.96 at 3-months FU and from gav = −.07 to .87 at 6-months FU.
The studies comparing their interventions to alcohol-unrelated control conditions found small to medium between-condition effect sizes (range: 0.20–0.62) at 3-months FU-assessment. The highest effect was calculated for Noknoy and colleagues (gs = 0.62) (105). The effect remained notable at 6-months FU-assessment (gs = 0.52).
The two RCTs contrasting their interventions against alcohol-related comparison conditions at 3-months (89) and 3- and 6-months FU-assessments (99) found either no group x time interaction effects (gs = 0.17) (89) or depicted a negative effect representing the superiority of the respective control group (gs = −0.27) at 3-months FU-assessment that subsided at 6 months (gs = −0.10) (99).
Other Outcomes
Four studies employed alcohol-related endpoints that could not be allocated to either of our two main outcome categories (87, 88, 95, 100). Calculations of within-condition effect sizes yielded a range from gav = 0.45 to 1.58 at 3-months FU. For the study conducted by Omeje et al. (87), only a 2-week FU assessment was available, producing a very large within-condition effect size-value of gav= 7.42 on a self-developed AUD scale. Of these studies, only Kalichman et al. (95) provided data at the 6-months FU point with an effect size value of gav = 0.29 for number of times of alcohol use before sex in the past month.
For the two studies that compared their intervention to an alcohol-unrelated control condition, we calculated small, but stable between-condition effect sizes of gs = .36 (3-months FU) and gs = .34 (6-months FU) for Kalichman et al. (95) and a very large effect of gs = 5.85 (2-weeks FU) for Omeje et al. (87). For the two studies with alcohol-related comparison conditions we found no effect for Segatto et al. on their dependent variable mean number of alcohol use days in the past 3 months (88), but calculated a large effect size value of gs = .87 based on the results of Pal et al.’s study at the 3-months FU-assessment (100).
Trends of Effect Size Values Across Multiple Assessment Points
Among studies where we were able to calculate between-condition effect size values for two FU-assessments (n=7 studies), the effect increased from FU1 to FU2 for Pengpid et al. (104) (small effect to medium effect) and Peltzer et al. (93) (negative effect to small effect) both reporting on alcohol-related symptoms. The effect size decreased from a small effect to no effect for the second outcome of Pengpid et al. (104). For the other studies the effect remained within the same Cohen’s d category (91, 95, 99, 101, 105).
Narrative Results and Studies Without Numeric Data
As part of the qualitative analysis, we extracted the results as reported within the study publications in addition to calculating effect sizes. All narrative results as reported by the 17 studies included in quantitative analyses can be found in Table 2. For four studies (79, 92, 94, 96) we were unable to calculate effect sizes as the necessary information was neither provided within the publications nor after contacting the authors. Due to the lack of numeric data the results of these four studies are only summarized as reported by the authors in Supplementary Table 3.
Discussion
Summary of Main Results
The present systematic review identified 21 randomized-controlled trials conducted in 15 different LMIC. Generally, methodological quality of the included studies was found to be adequate. Studies included female and male participants who screened as hazardous, harmful, or potentially dependent drinkers. The treatments were predominantly brief interventions provided by trained paraprofessionals in primary care settings. Four studies provided group therapy while all others conducted individual therapy sessions and there was great variation in total intervention exposure and primary outcome measures between the trials. In order to facilitate comparability regarding the effectiveness of interventions we calculated effect-sizes for the 17 studies where sufficient information was available using Hedge’s gav for within the respective treatment condition and Hedge’s gs for between-condition effects.
Effect Sizes
The majority of within-condition Hedge’s gav -values were ≥.8 at both 3-months (n=10 out of 17 effect size values) and 6-months (n=8 out of 11 effect size values) FU assessments. From this perspective, the vast majority of interventions had a large to very large positive impact on alcohol-related outcomes. However, looking at between-condition effect sizes, this impression is relativized as Hedge’s gs -values were generally much smaller. Large and very large effects occurred only in four studies (87, 90, 98, 100) and only at the short-term FU assessment point. What is striking about the studies by Sorsdahl et al. (98) and Pal et al. (100) is that their interventions achieved large between-condition effect sizes although contrasted with alcohol-related comparison procedures. Pal et al. (100) employed an MI-based approach as stand-alone intervention against routine medical care while, in the case of Sorsdahl et al. (98), only the condition in which ASSIST-linked-MI was enhanced with Problem Solving Therapy (an additional CBT component) yielded a differential effect over control (psycho-education only) while ASSIST-linked-MI alone did not. The extremely large between-condition effect size values found by Omeje et al. (87) (gs = 5.85) and Sheikh et al. (90) (gs = 2.15) have to be put into perspective. In addition to having methodological limitations such as high risk of attrition bias (all participants who missed one or more therapy sessions were excluded from analyses) and a self-administered ad-hoc developed scale as the primary outcome, Omeje et al. (87) employed the intervention with by far the highest treatment exposure of 20 group sessions of rational emotive health therapy and compared it to a waitlist control group condition. On top of that, the authors chose a very short period of 2 weeks for their only FU assessment. In Sheikh et al. (90), although formally stating only one therapeutic contact of 20 min, the very intensive involvement of the participants’ relatives as co-therapists designated to monitor the participant’s consumption as well as the option to seek support from the study team in case of relapses extend the intervention exposure far beyond the actual counseling session. Moreover, the control group received medical detoxification only.
For the longer-term FU time point, 11 studies reported data after 6 months with only three achieving medium-sized between-condition effects (Pengpid et al. (104) using ASSIST-linked-brief intervention, L’Engle et al. (102) using WHO Brief Intervention for alcohol use, and Noknoy et al. (105) using motivational enhancement therapy). All three studies compared their interventions to alcohol-unrelated control conditions. In summary, among the 17 studies that entered quantitative analyses only six revealed small to medium between-condition effect size values 6 months later. An additional five reported medium to large between-condition effect sizes 3 months after intervention but did not assess subjects at later time points. Our results suggest a modest impact of psychosocial interventions for alcohol-related problems in LMIC.
Comparison Conditions
Continuing to consider the nature of comparison conditions to further disentangle the results, it is notable that among the 10 studies with at least small between-condition effect-size values in favor of the experimental group, only three employed active control groups with an alcohol-focus (93, 98, 100). For the remaining seven studies with at least small Hedge’s gs values the effect sizes corresponded to a comparison between intervention and alcohol-unrelated control group procedures, such as routine medical care, mixed content educational components, or assessment only. Moreover, looking at the seven studies where between-condition effect size values were below .20 or negative, all of them employed alcohol-related comparison groups. Effect size results therefore suggest that as soon as the topic of alcohol is addressed in the control group procedure (e.g. expression of concern about drinking habit and simple advice to cut down, verbal or paper-based information/ psycho-education) there appears to be little to no difference between the conditions regarding their potential for reducing harmful alcohol use in participants. In general it seems that, at least within the rather short re-assessment interval of up to 6 months as investigated in the current review, many different control group procedures (including assessment-only) can lead to consumption-related behavior change.
Similarly, previous reviews on alcohol-focused interventions in HIC [e.g. (56, 61)] have also identified significant reductions in alcohol consumption in assessment-only or minimal-treatment (e.g. simple advice) control groups. Factors that have been postulated to possibly contribute to change in control groups are regression to the mean (124), the Hawthorne effect (change in behavior because subjects know they are being studied), and reactivity to assessment [e.g. (58, 125)]. The latter appears especially plausible for short interventions because their assessment processes often last longer than the actual counseling session and similarly focus on alcohol and effects of drinking. In addition, assessments in populations with low education and literacy rates, as are often found in LMIC, are usually done via one-on-one interview. This entails that the mere setting can resemble an intervention and therefore may (unintentionally) actuate unspecific effect mechanisms such as the therapeutic relationship, increase of attention on the problem, or evocation of motivation e.g. via feelings of guilt or remorse; especially since alcohol use and its effects are addressed during the assessment.
Interventions
Taking a closer look at the employed interventions, among the 10 studies with at least small positive between-condition effect size values eight employed at least one component of MI (90, 93, 95, 98, 100, 102, 104, 105). The two non-MI studies were the study by Omeje et al. (87) (rational emotive health therapy) which has methodological problems (see above) and Papas et al. (112) who conducted a CBT-based multi-session group intervention. Although promising, we are unable to draw conclusions regarding the effectiveness of pure CBT-interventions in LMIC from only one study. On the other hand, among the seven studies where between-condition effect-size values were below .20 or negative, all employed a MI-component as well (88, 89, 91, 97, 99, 101, 103). Taken together, the current evidence regarding MI-based interventions in LMIC is by far not as clear as one would expect considering its wide-spread use in therapeutic practice and scientific trials in LMIC settings. In sum, MI-based approaches or enhanced MI-based approaches were almost as often not effective as they were effective. This finding, however, matches conclusions drawn from comprehensive reviews summing up data from high income settings [e.g. (57)]. The authors similarly failed to find compelling evidence to support one psychosocial treatment targeting alcohol abuse over another. Nevertheless, some conclusions and recommendations concerning the features of interventions for practice and future study can be derived based on the current findings.
Properties of Effective Interventions
The heterogeneity of the studies’ settings and populations complicates the process of identifying intervention elements and properties that seem to be associated with positive outcomes regarding alcohol consumption for a majority of examined individuals. Starting with the framework conditions, evidence regarding the most effective dose of intervention input is inconclusive. One review that investigated alcohol-focused interventions conducted in primary care settings in predominantly high-income countries found brief multi-contact interventions to be more effective than other intensities, including brief single contact interventions (126). This matches the evidence found in the current review. Among the eight studies that conducted brief multi-contact interventions of 2–6 sessions, six showed an effectiveness of their experimental group in terms of between-condition effect sizes (93, 100, 102, 104, 105, 112), while only two did not (89, 91). For single-session interventions the ratio was nearly opposite with only two studies showing effectiveness of their interventions over the respective control condition (95, 98), while five did not (88, 97, 99, 101, 103). This is again excluding the trials by Sheikh et al. (90) and Omeje et al. (87), whose interventions appear to be extremely effective, but contain characteristics and methodological issues making them less comparable to all other studies.
Other reviews such as Moyer et al. (62) or Kaner et al. (61) who compare brief alcohol interventions in treatment-seeking and non-treatment-seeking populations or in primary care settings, respectively, argue in favor of brief interventions by concluding that there was no significant advantage of more extended treatments over shorter and even single-session inputs on alcohol reduction. In the current review among the 17 studies with calculable effect sizes eight studies had overall treatment exposures of <45 min. For those eight studies, the ratio of effective vs. non-effective interventions was 3:5 while it was 7:2 for the studies with overall treatment durations of ≥45 min making the longer interventions appear more effective. However, except Omeje et al. (87), practically all of the studies within this review can still be considered short-term interventions as the trials with the longest overall individual counseling exposure reported 120 (102) and 150 min (89). The finding that the majority of these interventions were effective is an important message, especially for low-resource settings within LMIC, where extensive treatment programs may not be a realistic option.
Another aspect that needs consideration is the delivery mode of the interventions. While the authors of the four studies that employed group-based interventions (87, 91, 96, 112) did not explain the reasoning behind their decision for the format, the most obvious factors appear to be cost- and resource efficiency and practicability. Whereas there is some quite promising evidence on CBT in groups for the treatment of hazardous drinking [e.g. (127, 128)], only very limited data can be applied to the question of whether group-delivered MI is effective. The few researchers who have attempted to illuminate the topic have named potential benefits and mechanisms such as direct feedback through peers (129) or positive reinforcement of behavior change by group members (130), however, they remain hesitant to recommend group-based MI and argue in favor of a combined approach (group + individual) instead. Review-level data investigating delivery mode of MI as a moderator is scarce with the existing literature yielding no statistically significant differences between group and individual facilitation among the small number of primary studies available (131). In the present review, a benefit of the group-based approach compared to active control was found for both CBT-infused interventions (87, 112) and for one (96) out of the two MI-based interventions. In any case, given the many potential advantages of group therapy programs for at-risk drinkers in LMIC this therapy modality merits more research attention.
It is fairly difficult to distill the active components of the interventions that have demonstrated good effectiveness, as the great majority of trials in this review used approaches based on MI. However, stand-alone MI-based approaches were rarely used, reflecting the circumstance that combining MI-elements with other interventions for hazardous drinking, usually behavioral or cognitive-behavioral in nature, has become quite common in HIC-settings and this seems to have been transferred to LMIC-settings. By focusing in detail on one research project which has combined MI with CBT, Moyers and Houck (132) have reflected on this widespread practice. They found that combined treatments produce outcomes that are often, but not always, superior to “pure” MI and state that the common rationale for combining MI with other treatment approaches was to help engage patients into the more complex CBT techniques. In the current review, including only the trials that entered quantitative analyses, three out of six MI-only interventions (100, 104, 105), both CBT-only interventions (87, 112), and two out of the four MI+CBT-interventions (93, 98) produced at least small between-condition effect sizes. Only Sorsdahl et al. (98) directly compared their MI-based intervention with the same MI-based intervention blended with CBT and found the combined treatment condition to be by far superior (gs = .83 for the MI+CBT intervention compared to gs = .05 for the MI-only condition). However, for Pal et al.’s study (100) an about equally high between-condition effect size value of gs = .87 was calculated for their two-session MI-based intervention without any CBT enhancement. Hence, even when attaching more weight to the studies by Sorsdahl et al. (98) and Pal et al. (100) (which seems legitimate as their interventions were the only ones yielding large between-condition effect size values when contrasted to alcohol-related comparison procedures), we end with a draw between MI-only and a CBT-blended MI-based intervention. Taken together, based on the trials included in the present review, the question of whether MI-only, or enhanced MI-based approaches should be first-line interventions to reduce alcohol-consumption and related symptoms in LMIC-settings cannot be conclusively answered.
The reduction in drinking among controls as found in many studies in the present review [e.g. (91, 93, 101)] might support the conclusion that mere FU could be recognized as a factor favoring change; a phenomenon which has already been recognized decades ago [e.g. (133, 134)]. As an implication for LMIC-settings it can be derived that beneficial effects might already arise from low-threshold, yet mandatory arrangements such as regular brief assessments of individuals combined with continuous communication and psychoeducation regarding alcohol use which could be pragmatically integrated into health care or other community-based services.
On a related note, monitoring seems to be a helpful mechanism to maintain behavior change as demonstrated in the study by Sheikh et al. (90) where a close relative, such as a participant’s spouse, was designated as co-therapist whose task it was to support the study participant’s abstinence (e.g. by helping him/her to avoid places where alcohol is available) and to arrange an additional appointment with the study team if they observed any signs of relapse in the patients. Apparently, this strategy was successful with remarkable results regarding effectiveness (Hedge’s gs=2.15) and retention (100%) at 8 weeks post-intervention. However, an intervention that interferes with the patient’s social system in a way that dysfunctional processes may eventuate seems ethically concerning, especially without controlling or studying these during or beyond the study period. There are similarities with the community reinforcement approach [CRA (135)] that also acknowledges the role of the social environment in the treatment of alcohol problems, or Behavioral Couples Therapy [BCT (136)] that involves both, the partner and the help-seeking individual into treatment. However, while in BCT and CRA the relationship to the spouse or relative(s) is closely monitored, in Sheikh et al.’s (90) intervention there is no mention about any specialized training or supervision for the relatives who act as co-therapists. Taken together, therapeutic techniques systematically utilizing social normative influence by partners, relatives, or significant others seem to offer some potential regarding the reduction of alcohol consumption in certain constellations. When employing such techniques, supervision structures for individuals within the patients’ social contexts who are involved in the intervention provision have to be considered.
In terms of facilitators the majority of interventions in this review (67%) were conducted by trained and supervised paraprofessionals. The practice of lay counselors conducting mental health interventions is backed up by an emerging number of researchers arguing that common practice elements such as MI-based counseling, psychoeducation, and even more complex techniques such as cognitive restructuring can be taught to personnel trained in other professions such as primary care staff who can then effectively apply them and improve the coverage in settings where no formal mental health infrastructure exists (73, 137, 138).
Recommendations for Future Research
Given the inconclusive picture we attained regarding the effectiveness of components used in alcohol-focused interventions in LMIC, dismantling trials and dissemination studies seem warranted in order to determine the differential effectiveness of the specific treatment elements.
A rather complex issue emerging from epidemiological research in LMIC is the topic of gender, with differential findings for prevalence rates. This includes generally higher rates found in men [e.g. (24, 139)], differences in drinking motives [e.g. coping motives predicting average alcohol intake for dependent women, but not men (140)], and psychiatric comorbidities [e.g. relationship between comorbid PTSD and alcohol dependence for men but not women (141)]. These findings appear to indicate that interventions should also be gender-sensitive. In most studies in this review, the vast majority of participants were male, with only three studies investigating all-female cohorts and only one mixed-sample study with more women than men. Among these four, two studies found their interventions to be effective (96, 102). Wandera and colleagues (99), whose sample was mixed but predominantly male, found their intervention to be effective for female participants only. Furthermore, female samples examined by the RCTs included in the present review were often extraordinary groups, such as female sex workers (91, 102), possibly due to the fact that hazardous drinking in LMIC is generally more prevalent in males. Hence, such samples may entail some particular risk factors and treatment approaches not best suited for women from the general population (e.g. particular emphasis on alcohol use in the context of HIV risk). Overall, sex-specific evidence in this review is inconclusive as most studies either did not report any gender-specific outcomes at all or were unable to examine whether findings differed by gender or not due to excessive gender imbalances in their cohorts [e.g. (97, 101, 105)]. With regard to the gendered nature of alcohol-related problems in LMIC, prospective alcohol intervention research should account for gender differences and power their samples accordingly.
Moreover, in order to more holistically capture the impact of interventions against excessive alcohol consumption, future trials in LMIC should consider including socially and systemically relevant outcomes, such as the impact of male drinking on intimate partner violence, violence against children, and other adverse effects on families such as stigmatization. In their RCT conducted in India, Satyanarayana et al. (142) found that an integrated cognitive-behavioral intervention targeting IPV perpetration among alcohol-dependent men was able to reduce violence against women and even improve mental health outcomes among participants’ wives and children in addition to having positive effects on alcohol-related problems. While the exacerbation of domestic violence with the involvement of alcohol is also found in HIC, women’s economic dependence and limited social opportunities relative to men are much more pronounced in LMIC and limit the viability of women exiting relationships in which alcohol consumption and violence become excessive (143). To date, research investigating the effectiveness of integrated treatment programs on both outcomes is optimistic but mostly HIC-based [e.g. (144)]. Therefore, the assessment of domestic violence in future alcohol intervention research in LMIC would be of particular importance and may document effects of the interventions beyond the reduction of AUD-symptoms.
None of the studies matching our inclusion criteria conducted their interventions in a conflict or post-conflict setting, which is in line with statements by authors of recent reviews [e.g. (18, 19)]. Therefore, we are unable to draw conclusions about intervention implementability and success in this particular context. However, research in populations affected by conflict points out some contextual factors that are likely to be relevant when trying to provide alcohol interventions in conflict or post-conflict settings. These include higher levels of traumatic exposure, higher prevalence rates of mental health disorders [e.g. (145)], and most likely also a higher density of daily stressors compared to more stable settings (e.g. impoverishment, ongoing insecurity, and impaired social cohesion within communities). Ezard, Debakre, and Catillon (146), who piloted an alcohol-focused brief intervention in a refugee camp in Thailand, additionally noted a “pervasive sense of hopelessness and dispossession” that potentially limited people’s motivation toward behavior change and therefore might have prevented positive treatment outcomes. Given that alarming prevalences of risky alcohol use in conflict-affected civilian populations have been reported (18–20) and given the empirically robust link between alcohol use and aggression [e.g. (42, 45)] it seems crucial to extend the current body of intervention research toward conflict and post-conflict societies.
As a further step beyond the efficacy of interventions, future studies in LMIC should also take important public health issues such as barriers to treatment access, cost-effectiveness, and long-term effects into consideration when evaluating interventions as those are factors relevant for the dissemination and routine-implementation of treatment programs.
Limitations of the Included Studies
The studies included in this review have several limitations regarding their designs and contents: First, FU periods were rather short, with only three studies reporting FU assessments later than 6 months posttreatment. Consequently, for most interventions no conclusions about their long-term effectiveness could be drawn. Future studies should consider longer FU periods as well as multiple assessment points in order to more clearly measure the sustainability of treatment effects. Second, attrition rates were quite high in some trials which may have limited the studies’ power to detect between-group differences. Future intervention studies in LMIC contexts are advised to allocate more effort and resources toward developing FU procedures which better match the specific setting of the target population. For instance, instead of relying on phone calls researchers could consider the use of local partners to collect detailed location descriptions of the participants’ homes in the event of informal living conditions to reduce attrition between the end of treatment and FU. Third, almost all studies reviewed here relied solely on self-report outcome data which can bring along problems such as memory effects or social desirability, with the latter being prone to variation by group allocation, especially in non-blinded trials. Experience with objective measures in LMIC-contexts is lacking. Consequently the use of measures of recent alcohol consumption in the form of breathalyzers or biomarkers, as well as collateral informants in an attempt to validate self-report-measures should be considered where feasible. Fourth, even though all the trials were RCTs, risk of bias assessment revealed some potential threats to internal validity, such as unclear or deficient sequence generation in four studies, unclear or inadequate allocation concealment in eight studies, and either unclearly or non-blinded outcome assessment in nine studies. However, most RCTs were rather strong on external validity, since they were conducted in naturalistic settings. This includes the choice of locations for service provision, such as primary health centers or hospitals, and the choice of personnel. Fifth, not all studies employed manualized interventions. For those studies this limits the possibility of monitoring treatment fidelity as well as replicability. Sixth, 14 trials in this review (87, 88, 90–100, 112) either included alcohol-dependent individuals only, reported a high proportion of dependent drinkers within their sample, or did not actively attempt to exclude alcohol dependent individuals, while the remaining seven studies did. Although, traditionally, hazardous and harmful, yet non-dependent drinkers have been the target for alcohol brief intervention research, the assumption that the interventions might not be effective in alcohol-addicted individuals has been questioned [e.g. (63, 147, 148)]. In this review, only two out of the 21 studies statistically controlled for a potential moderating effect of baseline drinking level on their outcomes: Nadkarni et al. (89) who included participants with an AUDIT score between 12–19 found no evidence of effect moderation by baseline AUDIT score; and Kalichman et al. (96), whose only inclusion criterion was “alcohol consumption in the previous month”, noted that those who were at the least risk for problem drinking demonstrated the greatest reductions in alcohol use. As these two studies either excluded dependent drinkers (89) or potentially included an unknown number of dependent drinkers (96) we are unable to clarify the debate of whether or not dependent drinkers in LMIC can statistically benefit from alcohol-focused brief interventions. However, among the 10 studies in the current review with effect sizes above .20 only three excluded dependent drinkers from their interventions (102, 104, 105), while all others did not explicitly do so. This suggests that brief alcohol interventions can also be effective when alcohol-addicted individuals are among the participants. Future studies should differentiate more clearly between persons with risky non-dependent drinking patterns and persons with alcohol dependence using reliable measurements. Such a classification would allow for differential analyses on the effectiveness of interventions.
Seventh, it is concerning that, among the 14 studies in this review that potentially or intentionally included alcohol-dependent individuals, only two (94, 98) reported that appropriate measures were in place in the event a participant experienced serious withdrawal symptoms such as seizures, deliria, or other medical complications. Accordingly, the availability of medical staff on site or at least the potential to quickly refer patients to appropriate treatment should be mandatory when dealing with potentially dependent participants, particularly in areas where formal emergency care units or rehabilitation centers may not be available. Eighth, the important question of how to deal with the previously mentioned high comorbidity rates between alcohol-related disorders and depressive, anxiety, and trauma-related disorders was bypassed in many studies in this review, either by excluding individuals exhibiting symptoms of such disorders or by not assessing other psychopathology besides AUD at all. Apart from Sorsdahl et al. (98), who found that their alcohol intervention also reduced depressive symptoms, none of the remaining studies controlled for comorbidities within their analyses. Being aware of such symptomatology is important, as these comorbidities may be associated with poorer treatment responses (149). Ninth and finally, when referring to MI it is important to keep in mind that only some studies employ it as it has initially been proposed and elaborated by Miller and Rollnick (117). Most of the RCTs in this review use elements of MI or MI-based interventions such as the WHO ASSIST-linked brief intervention for hazardous and harmful substance use (81) which are adapted versions of the original format.
Limitations of the Present Systematic Review
The present systematic review has several limitations. First, it is important to note some methodological factors when interpreting the reported effect sizes. All four high between-condition effect sizes might have been inflated since they were calculated from completer-only and not imputed values with the study by Sorsdahl et al. (98) yielding considerable attrition (38% and 58% in the treatment groups and 40% in the control group). Further, the study by Omeje et al. (87) only included completers of all 20 therapy sessions into their analyses while conducting only one very short-term FU assessment (two weeks post-intervention). Additionally, as this review gives preference to standardized assessment scales and/ or standard drinks per day as outcomes, where available we used these measures for effect size calculations. Only for four studies we had to use other variables depicting alcohol consumption (87, 88, 95, 100). For these studies it has to be kept in mind that the outcomes are less commonly-utilized scales lacking comprehensive validation studies and thus results might be less reliable. Furthermore, Hedge’s g does not take pretest differences into account. As the majority of authors reported no differences between groups at baseline, we do not assume a strong bias occurred in this regard. Second, the heterogeneity of the included studies precluded the pooling of outcomes in a meta-analytic manner. Instead, we based our analysis of evidence on the calculation and descriptive comparison of unpooled effect size values. Third, our literature search was limited to studies published in the English language. Apart from a potential selection bias due to language, this additionally entails the risk of publication bias, as significant results are more likely to be published in English-language journals (150). Fourth, due to our selection of search terms, the word ,alcohol’ had to be included in the title, abstract or key words of articles and therefore it cannot be completely ruled out that we failed to identify intervention studies in LMIC which, for example, used alcohol consumption as a secondary outcome. Also, though unlikely, we may have missed records as we did not search for each LMIC included in the World Bank country classification list separately. Finally, we only included randomized-controlled trials which can be seen as a strength of this review, but also entails the risk of disregarding findings originating from other designs such quasi-experimental studies.
Conclusions
This systematic review further supports the emerging evidence base demonstrating that the use of pragmatic psychosocial interventions can effectively reduce hazardous and harmful alcohol use in low-resource settings. Apart from the complete dearth of intervention research in LMIC-regions affected by conflict, the research gap is increasingly being addressed, with many studies presenting pioneering and promising work on this endeavor.
In summary, the following aspects can be derived from existing research: (1) multiple contact interventions seem to work better than single contact interventions and (2) interventions with sessions of 45 min or longer were on average more effective than those with shorter sessions. However, overall individual counseling intensity across all sessions was still short in virtually all studies (≤150 min). Also, (3) group interventions do not seem to be less effective when compared to individual interventions. (4) The finding that just over 50% of those studies using MI-based approaches yielded a notable treatment effect compared to control entails the necessity of considering alternatives to MI-based approaches which should be tested in future trials. (5) The additional value of therapeutic components applied to enhance MI-based interventions, such as cognitive techniques, remains inconclusive and (6) the finding that, often, assessment or even mere monitoring of alcohol-related symptoms may already reduce drinking cannot be ignored. Finally, (7) in most cases interventions were conducted by trained paraprofessionals suggesting this as a feasible concept in LMIC. However, evaluations of the delivery model itself, including details on an adequate intensity of training and supervision of lay counselors, are lacking.
The RCTs of the current review have provided us with a valuable knowledge base, however, there is room for the improvement of service provision and accompanying research in LMIC settings. We therefore would like to encourage the generation of more research in order to enhance and strengthen the implementation of evidence-based, sustainable and accessible interventions targeting alcohol abuse in LMIC settings.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding author.
Author Contributions
MP, VE, and FN contributed to the conception and design of the review. MP and VE conducted the study selection. MP extracted the data from the selected articles, conducted the data analysis, and drafted the manuscript with supervision from VE. MP and VE contributed to the interpretation of data. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Neele Bormann for assisting with literature search and formatting and Justin Preston for language editing. We also acknowledge the financial support of the German Research Foundation (DFG) and the Open Access Publication Fund of Bielefeld University for the article processing charge.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.00768/full#supplementary-material
References
1. World Bank. World Bank country and lending groups, country classification. Washington (DC): World Bank (2019). Available at: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
2. WHO. Global status report on alcohol and health 2018. Geneva: World Health Organization (WHO) (2018). p. 392, Available at: http://www.who.int/substance_abuse/publications/global_alcohol_report/en/.
3. Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet (2009) 373:2223–33. doi: 10.1016/S0140-6736(09)60746-7
4. Connor JP, Hall W. Alcohol burden in low-income and middle-income countries. Lancet (2015) 386:1922–4. doi: 10.1016/S0140-6736(15)00236-6
5. Patel V. Alcohol Use and Mental Health in Developing Countries. Ann Epidemiol (2007) 17:87–92. doi: 10.1016/j.annepidem.2007.01.019
6. Room R, Mäkelä P, Schmidt L, Rehm J. Alcohol, Health Disparities and Development. Geneva: World Health Organization (2006).
7. Rehm J, Rehn N, Room R, Monteiro M, Gmel G, Jernigan D, et al. The global distribution of average volume of alcohol consumption and patterns of drinking. Eur Addict Res (2003) 9:147–56. doi: 10.1159/000072221
8. Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction (2003) 98:1209–28. doi: 10.1159/000072221
9. Rehm J, Kanteres F, Lachenmeier DW. Unrecorded consumption, quality of alcohol and health consequences. Drug Alcohol Rev (2010) 29:426–36. doi: 10.1111/j.1465-3362.2009.00140.x
10. Babor TF, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham K, et al. Alcohol: No Ordinary Commodity - Research and Public Policy. 2nd ed. Oxford, UK: Oxford University Press (2010).
11. Babor TF, Campbell R, Room R, Sauners J. Lexicon of Alcohol and Drug Terms. Geneva: World Health Organization (1994).
12. Francis JM, Weiss HA, Mshana G, Baisley K, Grosskurth H, Kapiga SH. The epidemiology of alcohol use and alcohol use disorders among young people in Northern Tanzania. PLoS One (2015) 10:e0140041. doi: 10.1371/journal.pone.0140041
13. Ghosh S, Samanta A, Mukherjee S. Patterns of alcohol consumption among male adults at a slum in Kolkata, India. J Heal Popul Nutr (2012) 30:73–81. doi: 10.3329/jhpn.v30i1.11279
14. Seth P, Glenshaw M, Sabatier JHF, Adams R, Du Preez V, DeLuca N, et al. AUDIT, AUDIT-C, and AUDIT-3: Drinking patterns and screening for harmful, hazardous and dependent drinking in Katutura, Namibia. PLoS One (2015) 10:e0120850. doi: 10.1371/journal.pone.0120850
15. Teferra S, Medhin G, Selamu M, Bhana A, Hanlon C, Fekadu A. Hazardous alcohol use and associated factors in a rural Ethiopian district: A cross-sectional community survey. BMC Public Health (2016) 16:218. doi: 10.1186/s12889-016-2911-6
16. Kullgren G, Alibusa S, Birabwa-Oketcho H. Problem drinking among patients attending primary healthcare units in Kampala, Uganda. Afr J Psychiatry (2009) 12:52–8. doi: 10.4314/ajpsy.v12i1.30279
17. UNHCR and WHO. Rapid Assessment of Alcohol and Other Substance Use in Conflict-affected and Displaced Populations: A Field Guide. Geneva: UNHCR (2008). p. 50, Available at: http://www.who.int/mental_health/emergencies/unhcr_alc_rapid_assessment.pdf?ua=1.
18. Ezard N. Substance use among populations displaced by conflict: A literature review. Disasters (2012) 36:533–57. doi: 10.1111/j.1467-7717.2011.01261.x
19. Lo J, Shultz P, Ezard N, Roberts B. A systematic review on harmful alcohol use among civilian populations affected by armed conflict in low- and middle-income countries. Subst Use Misuse (2017) 52:1494–510. doi: 10.1080/10826084.2017.1289411
20. Weaver H, Roberts B. Drinking and displacement: a systematic review of the influence of forced displacement on harmful alcohol use. Subst Use Misuse (2010) 45:2340–55. doi: 10.3109/10826081003793920
21. Luitel NP, Jordans M, Murphy A, Roberts B, McCambridge J. Prevalence and Patterns of Hazardous and Harmful Alcohol Consumption Assessed Using the AUDIT among Bhutanese Refugees in Nepal. Alcohol Alcohol (2013) 48:349–55. doi: 10.1093/alcalc/agt009
22. Roberts B, Murphy A, Chikovani I, Makhashvili N, Patel V, McKee M. Individual and community level risk-factors for alcohol use disorder among conflict-affected persons in Georgia. PLoS One (2014) 9:e98299. doi: 10.1371/journal.pone.0098299
23. Roberts B, Felix Ocaka K, Browne J, Oyok T, Sondorp E. Alcohol disorder amongst forcibly displaced persons in northern Uganda. Addict Behav (2011) 36:870–3. doi: 10.1016/j.addbeh.2011.03.006
24. Ertl V, Saile R, Neuner F, Catani C. Drinking to ease the burden: A cross-sectional study on trauma, alcohol abuse and psychopathology in a post-conflict context. BMC Psychiatry (2016) 16:202. doi: 10.1186/s12888-016-0905-7
25. Chung W, Chun H, Lee S. Socioeconomic Costs of Alcohol Drinking in Korea. J Prev Med Public Heal (2006) 39:21–9.
26. Thavorncharoensap M, Teerawattananon Y, Yothasamut J, Lertpitakpong C, Thitiboonsuwan K, Neramitpitagkul P, et al. The economic costs of alcohol consumption in Thailand, 2006. BMC Public Health (2010) 10:323. doi: 10.1186/1471-2458-10-323
27. Gmel G, Ph D, Rehm J, Ph D. Harmful alcohol use. Alcohol Res Heal (2003) 27:52–62. doi: 10.7748/ns.29.36.17.s22
28. World Health Organization. Burden and socio-economic impact of alcohol: The Bangalore study. New Delhi: WHO, Regional Office for South-East Asia (2006). Available from https://apps.who.int/iris/handle/10665/204856
29. Navarro HJ, Doran CM, Shakeshaft AP. Measuring costs of alcohol harm to others: A review of the literature. Drug Alcohol Depend (2011) 114:87–99. doi: 10.1016/j.drugalcdep.2010.11.009
30. Room R. Stigma, social inequality and alcohol and drug use. Drug Alcohol Rev (2005) 24:143–55. doi: 10.1080/09595230500102434
31. Fillmore MT. Acute alcohol-induced impairment of cognitive functions: Past and present findings. Int J Disabil Hum Dev (2007) 6:115–26. doi: 10.1515/IJDHD.2007.6.2.115
32. Sayette MA, Wilson GT, Elias MJ. Alcohol and aggression: a social information processing analysis. J Stud Alcohol (1993) 54:399–407. doi: 10.15288/jsa.1993.54.399
33. Debell F, Fear NT, Head M, Batt-Rawden S, Greenberg N, Wessely S, et al. A systematic review of the comorbidity between PTSD and alcohol misuse. Soc Psychiatry Psychiatr Epidemiol (2014) 49:1401–25. doi: 10.1007/s00127-014-0855-7
34. Hickie IB, Koschera A, Davenport TA, Naismith SL, Scott EM. Comorbidity of common mental disorders and alcohol or other substance misuse in Australian general practice. Med J Aust (2001) 175:31–6. doi: 10.5694/j.1326-5377.2001.tb143787.x
35. Lai HMX, Cleary M, Sitharthan T, Hunt GE. Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990-2014: A systematic review and meta-analysis. Drug Alcohol Depend (2015) 154:1–13. doi: 10.1016/j.drugalcdep.2015.05.031
36. Haller M, Chassin L. Risk pathways among traumatic stress, posttraumatic stress disorder symptoms, and alcohol and drug problems: A test of four hypotheses. Psychol Addict Behav (2014) 28:841–51. doi: 10.1037/a0035878
37. Gage AJ. Women’s experience of intimate partner violence in Haiti. Soc Sci Med (2005) 61:343–64. doi: 10.1016/j.socscimed.2004.11.078
38. Jewkes R, Levin J, Penn-Kekana L. Risk factors for domestic violence: Findings from a South African cross-sectional study. Soc Sci Med (2002) 55:1603–17. doi: 10.1016/S0277-9536(01)00294-5
39. Koenig MA, Lutalo T, Zhao F, Nalugoda F, Wabwire-Mangen F, Kiwanuka N, et al. Domestic violence in rural Uganda: Evidence from a community-based study. Bull World Health Organ (2003) 81:53–60. doi: 10.1590/S0042-96862003000100011
40. Zaleski M, Pinsky I, Laranjeira R, Ramisetty-Mikler S, Caetano R. Intimate partner violence and alcohol consumption. Rev Saude Publica (2010) 44:53–9. doi: 10.1590/S0034-89102010000100006
41. Catani C, Schauer E, Neuner F. Beyond individual war trauma: Domestic violence against children in Afghanistan and Sri Lanka. J Marital Fam Ther (2008) 34:165–76. doi: 10.1111/j.1752-0606.2008.00062.x
42. Stark L, Ager A. A systematic review of prevalence studies of gender-based violence in complex emergencies. Trauma Violence Abus (2011) 12:127–34. doi: 10.1177/1524838011404252
43. Heidelberg Institute for International Conflict Research. Conflict Barometer 2017. Heidelberg: University of Heidelberg (2017).
44. Sriskandarajah V, Neuner F, Catani C. Predictors of violence against children in Tamil families in northern Sri Lanka. Soc Sci Med (2015) 146:257–65. doi: 10.1016/j.socscimed.2015.10.010
45. Saile R, Neuner F, Ertl V, Catani C. Prevalence and predictors of partner violence against women in the aftermath of war: A survey among couples in Northern Uganda. Soc Sci Med (2013) 86:17–25. doi: 10.1016/j.socscimed.2013.02.046
46. Saile R, Ertl V, Neuner F, Catani C. Does war contribute to family violence against children? Findings from a two-generational multi-informant study in Northern Uganda. Child Abus Negl (2014) 38:135–46. doi: 10.1016/j.chiabu.2013.10.007
47. World Health Organization. mhGAP: mental health gap action programme: scaling up care for mental, neurological and substance use disorders. Geneva: World Health Organization (2008), 44.
48. Rathod SD, De Silva MJ, Ssebunnya J, Breuer E, Murhar V, Luitel NP, et al. Treatment Contact Coverage for Probable Depressive and Probable Alcohol Use Disorders in Four Low- and Middle-Income Country Districts: The PRIME Cross-Sectional Community Surveys. PLoS One (2016) 11:e0162038. doi: 10.1371/journal.pone.0162038
49. Foxcroft DR, Coombes L, Wood S, Allen D, Almeida Santimano NML. Motivational interviewing for alcohol misuse in young adults. Cochrane Database Syst Rev (2014) 8:CD007025. doi: 10.1002/14651858.CD007025.pub2
50. Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: A meta-analytic review. Alcohol Alcohol (2006) 41:328–35. doi: 10.1093/alcalc/agl016
51. Rollnick S, Miller WR, Butler CC. Motivational interviewing in health care: Helping patients change behavior. Applications of motivational interviewing. New York: The Guilford Press (2008).
52. Miller W, Sanchez V. “Motivating young adults for treatment and lifestyle change”. In: Howard G, editor. Issues in alcohol use and misuse by young adults. Notre Dame: University of Notre Dame Press. (1994) p. 211–21.
53. Miller W, Zweben A, DiClemente CC, Rychtarik RG. Motivational enhancement therapy manual- a clinical research guide for therapists treating individuals with alcohol abuse and dependence. Rockville, Maryland: National Institute on Alcohol Abuse and Alcoholism (1992).
54. Kaner EFS, Dickinson HO, Beyer F, Pienaar E, Schlesinger C, Campbell F, et al. The effectiveness of brief alcohol interventions in primary care settings: A systematic review. Drug Alcohol Rev (2009) 28:301–23. doi: 10.1111/j.1465-3362.2009.00071.x
55. Ballesteros J, Duffy JC, Querejeta I, Ariño J, González-Pinto A. Efficacy of brief interventions for hazardous drinkers in primary care: systematic review and meta-analyses. Alcohol Clin Exp Res (2004) 28:608–18. doi: 10.1097/01.ALC.0000122106.84718.67
56. Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: a review. Addiction (1993) 88:315–35. doi: 10.1111/j.1360-0443.1993.tb00820.x
57. Hunt GE, Siegfried N, Morley K, Sitharthan T, Cleary M. Psychosocial treatment programs for people with both severe mental illness and substance misuse. Cochrane Database Syst Rev (2013) 10:226–8. doi: 10.1002/14651858.CD001088.pub3
58. McCambridge J, Kypri K. Can simply answering research questions change behaviour? Systematic review and meta analyses of brief alcohol intervention trials. PLoS One (2011) 6:e23748. doi: 10.1371/journal.pone.0023748
59. Tanner-Smith EE, Lipsey M. Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. J Subst Abuse Treat (2015) 51:1–18. doi: 10.1016/j.jsat.2014.09.001
60. Bertholet N, Daeppen, Wietlisback J, Fleming V, Burnand B M. Reduction of Alcohol Consumption by Brief Alcohol Intervention in Primary Care. Arch Intern Med (2005) 165:986–95. doi: 10.1001/archinte.165.9.986
61. Kaner E, Beyer FR, Muirhead C, Campbell F, Pienaar ED, Bertholed N, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev (2018) 2. doi: 10.1002/14651858.CD004148.pub4
62. Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction (2002) 97:279–92. doi: 10.1046/j.1360-0443.2002.00018.x
63. Saitz R. Alcohol screening and brief intervention in primary care: Absence of evidence for efficacy in people with dependence or very heavy drinking. Drug Alcohol Rev (2010) 29:631–40. doi: 10.1111/j.1465-3362.2010.00217.x
64. Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. Behavioral Counseling Interventions in Primary Care To Reduce Risky / Harmful Alcohol Use by Adults: A Summary of the Evidence for the U.S. Ann Intern Med (2004) 140:557–80. doi: 10.7326/0003-4819-140-7-200404060-00017
65. Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med (1997) 12:274–83. doi: 10.1046/j.1525-1497.1997.012005274.x
66. Babor TF, Robaina K, Nilssen P, Kaner E, Li Q. Rapid Review of Current Evidence for Health Promotion Actions for Hazardous and Harmful Alcohol Use, with Specific Reference to Low- and Middle-Income Countries. Geneva: World Health Organization, Mainstreaming Project, Division of Non-communicable Diseases (2011).
67. O’Donnell A, Anderson P, Newbury-Birch D, Schulte B, Schmidt C, Reimer J, et al. The impact of brief alcohol interventions in primary healthcare: A systematic review of reviews. Alcohol Alcohol (2014) 49:66–78. doi: 10.1093/alcalc/agt170
68. Benegal V, Chand PK, Obot IS. Packages of care for alcohol use disorders in low- and middle-income countries. PLoS Med (2009) 6:e10000170. doi: 10.1371/journal.pmed.1000170
69. Carrasco MA, Esser MB, Sparks A, Kaufman MR. HIV-Alcohol Risk Reduction Interventions in Sub-Saharan Africa: A Systematic Review of the Literature and Recommendations for a Way Forward. AIDS Behav (2016) 20:484–503. doi: 10.1007/s10461-015-1233-5
70. Peltzer K. Brief Intervention of Alcohol Problems in Sub-Saharan Africa: A Review. J Psychol Afr (2009) 19:415–22. doi: 10.1080/14330237.2009.10820310
71. Joseph J, Basu D. Efficacy of Brief Interventions in Reducing Hazardous or Harmful Alcohol Use in Middle-Income Countries: Systematic Review of Randomized Controlled Trials. Alcohol Alcohol (2017) 52:56–64. doi: 10.1093/alcalc/agw054
72. Patel V, Araya R, Chatterjee S, Chisholm D, Cohen A, De Silva M, et al. Treatment and prevention of mental disorders in low-income and middle-income countries. Lancet (2007) 370:991–1005. doi: 10.1016/S0140-6736(07)61240-9
73. van Ginneken N, Tharyan P, Lewin S, Rao GN, Meera SM, Pian J, et al. Non-Specialist Health Worker Interventions for the Care of Mental, Neurological, and Substance-Abuse Disorders in Low- and Middle-Income Countries. Cochrane Database Syst Rev (2013) 11. doi: 10.1002/14651858.CD009149.pub2
74. Salwan J. Katz CL. A review of substance use disorder treatment in developing world communities. Ann Glob Heal (2014) 80:115–21. doi: 10.1016/j.aogh.2014.04.010
75. Ertl V. Excessive Alcohol Use In Crisis-affected Societies: A Weak Spot of Global Mental Health Research and Practice. Int Soc Trauma Stress Stud - Stress (2016).
76. Roberts B, Ezard N. Why are we not doing more for alcohol use disorder among conflict-affected populations? Addiction (2015) 110:889–90. doi: 10.1111/add.12869
77. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann Intern Med (2009) 151:264–70. doi: 10.1371/journal.pmed.1000097
78. Higgins J, Green S. Cochrane handbook for systematic reviews of interventions version 5.0.2. The Cochrane Collaboration (2009). Available at: www.cochrane-handbook.org.
79. Babor TF, Grant M. Programme on substance abuse: Project on identification and management of alcohol-related problems. Report on Phase II. A randomized clinical trial of brief interventions in primary health care. Geneva: World Health Organization (1992).
80. Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorder Identification Test (AUDIT) - Guidelines for Use in Primary Care. 2nd ed. Geneva: World Health Organization (2001).
81. Humenuik R, Henry-Edwards S, Poznyak V, Monteiro M. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST). Geneva: World Health Organization (2010).
82. Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front Psychol (2013) 4:863. doi: 10.3389/fpsyg.2013.00863
83. Lakens D. (2013). Data Sheet 1 (XLSX document). Available at: http://openscienceframework.org/project/ixGcd/.
85. Rosenthal JA. Qualitative Descriptors of Strength of Association and Effect Size. J Soc Serv Res (1996) 21:37–59. doi: 10.1300/J079v21n04
86. Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (2011) 343:d5928. doi: 10.1136/bmj.d5928
87. Omeje JC, Otu MS, Aneke AO, Adikwu VO, Nwaubani OO, Chigbu EF, et al. Effect of Rational Emotive Health Therapy on Alcohol Use among Community-dwelling, HIV-positive Patients. Med (Baltimore) (2018) 97:e11688. doi: 10.1097/MD.0000000000011688
88. Segatto ML, Andreoni S, de Souza e Silva R, Diehl A, Pinsky I. Brief motivational interview and educational brochure in emergency room settings for adolescents and young adults with alcohol-related problems: a randomized single-blind clinical trial. Rev Bras Psiquiatr (2011) 33:225–33. doi: 10.1590/S1516-44462011005000004
89. Nadkarni A, Weobong B, Weiss HA, McCambridge J, Bhat B, Katti B, et al. Counselling for Alcohol Problems (CAP), a lay counsellor-delivered brief psychological treatment for harmful drinking in men, in primary care in India: a randomised controlled trial. Lancet (2017) 389:186–95. doi: 10.1016/S0140-6736(16)31590-2
90. Sheikh WA, Paul R, Banda H, Agath K, Luty J. Impact of brief relapse prevention intervention in patients with alcohol dependence in Zambia. J Subst Use (2017) 22:113–7. doi: 10.3109/14659891.2015.1090494
91. Witte SS, Altantsetseg B, Aira T, Riedel M, Chen J, Potocnik K, et al. Reducing sexual HIV/STI risk and harmful alcohol use among female sex workers in Mongolia: A randomized clinical trial. AIDS Behav (2011) 15:1785–94. doi: 10.1007/s10461-011-9984-0
92. Shin S, Livchits V, Connery HS, Shields A, Yanov S, Yanova G, et al. Effectiveness of alcohol treatment interventions integrated into routine tuberculosis care in Tomsk, Russia. Addiction (2013) 108:1387–96. doi: 10.1111/add.12148
93. Peltzer K, Louw J, Matseke G, Zuma K, McHunu G, Tutshana B, et al. Screening and brief interventions for hazardous and harmful alcohol use among patients with active tuberculosis attending primary public care clinics in South Africa: Results from a cluster randomized controlled trial. BMC Public Health (2013) 13:699. doi: 10.1186/1471-2458-13-699
94. Rendall-Mkosi K, Morojele N, London L, Moodley S, Singh C, Girdler-Brown B. A randomized controlled trial of motivational interviewing to prevent risk for an alcohol-exposed pregnancy in the Western Cape, South Africa. Addiction (2013) 108:725–32. doi: 10.1111/add.12081
95. Kalichman SC, Simbayi LC, Vermaak R, Cain D, Jooste S, Peltzer K. HIV/AIDS Risk Reduction Counseling for Alcohol Using Sexually Transmitted Infections Clinic Patients in Cape Town, South Africa. JAIDS J Acquir Immune Defic Syndr (2007) 44:594–600. doi: 10.1097/QAI.0b013e3180415e07
96. Kalichman SC, Simbayi LC, Vermaak R, Cain D, Smith G, Mthebu J, et al. Randomized trial of a community-based alcohol-related HIV risk-reduction intervention for men and women in Cape Town South Africa. Ann Behav Med (2008) 36:270–9. doi: 10.1007/s12160-008-9067-2
97. Mertens JR, Ward CL, Bresick GF, Broder T, Weisner CM. Effectiveness of nurse-practitioner-delivered brief motivational intervention for young adult alcohol and drug use in primary care in South Africa: A randomized clinical trial. Alcohol Alcohol (2014) 49:430–8. doi: 10.1093/alcalc/agu030
98. Sorsdahl K, Stein DJ, Corrigall J, Cuijpers P, Smits N, Naledi T, et al. The efficacy of a blended motivational interviewing and problem solving therapy intervention to reduce substance use among patients presenting for emergency services in South Africa: A randomized controlled trial. Subst Abuse Treat Prev Policy (2015) 10:46. doi: 10.1186/s13011-015-0042-1
99. Wandera B, Tumwesigye NM, Nankabirwa JI, Mafigiri DK, Parkes-Ratanshi RM, Kapiga S, et al. Efficacy of a Single, Brief Alcohol Reduction Intervention among Men and Women Living with HIV/AIDS and Using Alcohol in Kampala, Uganda: A Randomized Trial. J Int Assoc Provid AIDS Care (2016) 16:276–85. doi: 10.1177/2325957416649669
100. Pal HR, Yadav D, Mehta S. Mohan I. A comparison of brief intervention versus simple advice for alcohol use disorders in a North India community-based sample followed for 3 months. Alcohol Alcohol (2007) 42:328–32. doi: 10.1093/alcalc/agm009
101. Assanangkornchai S, Nima P, McNeil EB, Edwards JG. Comparative trial of the WHO ASSIST-linked brief intervention and simple advice for substance abuse in primary care. Asian J Psychiatr (2015) 18:75–80. doi: 10.1016/j.ajp.2015.09.003
102. L’Engle KL, Mwarogo P, Kingola N, Sinkele W. Weiner DH. A Randomized Controlled Trial of a Brief Intervention to Reduce Alcohol Use Among Female Sex Workers in Mombasa, Kenya. J Acquir Immune Defic Syndr (2014) 67:446–53. doi: 10.1097/QAI.0000000000000335
103. Pengpid S, Peltzer K, Skaal L, Van Der Heever H. Screening and brief interventions for hazardous and harmful alcohol use among hospital outpatients in South Africa: Results from a randomized controlled trial. BMC Public Health (2013) 13:644. doi: 10.1186/1471-2458-13-644
104. Pengpid S, Peltzer K, Puckpinyo A, Viripiromgool S, Thamma-Aphiphol K, Suthisukhon K, et al. Screening and concurrent brief intervention of conjoint hazardous or harmful alcohol and tobacco use in hospital out-patients in Thailand: a randomized controlled trial. Subst Abuse Treat Prev Policy (2015) 10:22. doi: 10.1186/s13011-015-0018-1
105. Noknoy S, Rangsin R, Saengcharnchai P, Tantibhaedhyangkul U, McCambridge J. RCT of effectiveness of motivational enhancement therapy delivered by nurses for hazardous drinkers in primary care units in Thailand. Alcohol Alcohol (2010) 45:263–70. doi: 10.1093/alcalc/agq013
106. Babor TF, Ritson EB, Hodgson RJ. Alcohol-Related Problems in the Primary Health Care Setting: a review of early intervention strategies. Br J Addict (1986) 81:23–46. doi: 10.1111/j.1360-0443.1986.tb00291.x
107. Babor TF, de la Fuente JR, Saunders J, Grant M. The Alcohol Use Disorders Identification Test (AUDIT): Guidelines for use in Primary Health Care. Geneva: World Health Organization (1992).
108. Rollnick S, Mason P, Butler C. Health Behavior Change: A Guide for Practitioners. New York: Churchill Livingston (1999).
109. Nadkarni A, Velleman R, Dabholkar H, Shinde S, Bhat B, Mccambridge J, et al. The systematic development and pilot randomized evaluation of counselling for alcohol problems, a lay counselor-delivered psychological treatment for harmful drinking in primary care in India: The PREMIUM study. Alcohol Clin Exp Res (2015) 39:522–31. doi: 10.1111/acer.12653
110. Hammels D, Yalom V. Instructor"s Manual for Rational Emotive Behavior Therapy for Addictions With Albert Ellis. Mill Valley, CA: Psychotherapy.net (2009).
111. Pal H, Yadav D, Singh AK. Brief Intervention: A Manual for Practice. New Delhi, India: National Drug Dependence Treatment Centre, All India Institute of Medical Sciences (2005).
112. Papas RK, Sidle JE, Gakinya BN, Baliddawa JB, Martino S, Mwaniki MM, et al. Treatment outcomes of a stage 1 cognitive-behavioral trial to reduce alcohol use among human immunodeficiency virus-infected out-patients in western Kenya. Addiction (2011) 106:2156–66. doi: 10.1111/j.1360-0443.2011.03518.x
113. Papas RK, Sidle JE, Martino S, Baliddawa JB, Songole R, Omolo OE, et al. Systematic cultural adaptation of cognitive-behavioral therapy to reduce alcohol use among HIV-infected outpatients in Western Kenya. AIDS Behav (2010) 14:669–78. doi: 10.1007/s10461-009-9647-6
114. Fisher JD, Fisher JD, Fisher WA. Changing AIDS - Risk Behavior Changing AIDS-Risk Behavior. Psychol Assess (1992) 111:455–74. doi: 10.1037/0033-2909.111.3.455
115. Kahler CW, Metrik J, LaChance HR, Ramsey SE, Abrams DB, Monti PM, et al. Addressing Heavy Drinking in Smoking Cessation Treatment: A Randomized Clinical Trial. J Consult Clin Psychol (2008) 76:852–62. doi: 10.1037/a0012717
116. Ingersoll K, Floyd L, Sobell M, Velasquez MM. Reducing the risk of alcohol-exposed pregnancies: a study of a motivational intervention in community settings. Pediatrics (2003) 111:1131–5.
117. Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. New York: Guilford Press (1991).
118. WHO. mhGAP Intervention Guide for Mental, Neurological and Substance Use Disorders in non-Specialized Health Settings. Geneva: World Health Organization (2008).
119. National Institute on Alcohol Abuse and Alcoholism and National Institute of Health. Helping Patients Who Drink Too Much - a Clinicans Guide. Bethesda, MD: U.S. Department of Health an Human Services (2005).
120. El-Bassel N, Witte SS, Gilbert L, Wu E, Chang M, Hill J, et al. The Efficacy of a Relationship-Based HIV/STD Prevention Program for Heterosexual Couples. Am J Public Health (2003) 93:963–9. doi: 10.2105/AJPH.93.6.963
121. Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York: Guilford Press (2002).
122. Miller WR, Rollnick S. Ten things that motivational interviewing is not. Behav Cognit Psychother (2009) 37:129–40. doi: 10.1017/S1352465809005128
123. Ellis AE, Grieger RM. Handbook of rational-emotive therapy, Vol. 2. New York: Springer Publishing Company (1986).
124. Finney JW. Regression to the mean in substance use disorder treatment research. Addiction (2007) 103:42–52. doi: 10.1111/j.1360-0443.2007.02032.x
125. Kypri K, Langley JD, Saunders JB, Cashell-Smith ML. Assessment may conceal therapeutic benefit: Findings from a randomized controlled trial for hazardous drinking. Addiction (2007) 102:62–70. doi: 10.1111/j.1360-0443.2006.01632.x
126. Jonas DE, Garbutt JC, Brown JM, Amick HR, Brownley KA, Council CL, et al. Screening, Behavioral Counseling, and Referral in Primary Care To Reduce Alcohol Misuse. Rockville, Maryland: Agency for Healthcare Research and Quality (2012).
127. Marques ACP, Formigoni MLO. Comparison of individual and group cognitive-behavioral therapy for alcohol and / or drug-dependent patients. Addiction (2001) 96:835–46. doi: 10.1080/09652140020050951
128. Sobell LC, Sobell MB, Agrawal S. Randomized Controlled Trial of a Cognitive-Behavioral Motivational Intervention in a Group Versus Individual Format for Substance Use Disorders. Psychol Addict Behav (2009) 23:672–83. doi: 10.1037/a0016636
129. LaBrie JW, Pedersen ER, Lamb TF, Quinlan T. A campus-based motivational enhancement group intervention reduces problematic drinking in freshmen male college students. Addict Behav (2007) 32:889–901. doi: 10.1016/j.addbeh.2006.06.030
130. Foote J, DeLuca A, Magura S, Warner A, Grand A, Rosenblum A, et al. A group motivational treatment for chemical dependency. J Subst Abuse Treat (1999) 17:181–92. doi: 10.1016/S0740-5472(99)00003-3
131. Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL. A meta-analysis of motivational interviewing: twenty-five years of empirical studies. Res Soc Work Pract (2010) 20:137–60. doi: 10.1177/1049731509347850
132. Moyers TB, Houck J. Combining Motivational Interviewing With Cognitive-Behavioral Treatments for Substance Abuse: Lessons From the COMBINE Research Project. Cognit Behav Pract (2011) 18:38–45. doi: 10.1016/j.cbpra.2009.09.005
133. Elvy GA, Wells JE, Baird KA. Attempted Referral as Intervention for Problem Drinking in the General Hospital. Br J Addict (1988) 83:83–9. doi: 10.1111/j.1360-0443.1988.tb00455.x
134. Heather N, Campion PD, Neville RG, Maccabe D. Evaluation of a controlled drinking minimal intervention for problem drinkers in general practice (the DRAMS scheme). J R Coll Gen Pract (1987) 37:358–63.
135. Meyers RJ, Smith JE. Clinical Guide to Alcohol Treatment: The Community Reinforcement Approach. New York: The Guilford Press (1995).
136. Epstein EE, McCrady BS. Behavioral couples treatment of alcohol and drug use disorders: Current status and innovations. Clin Psychol Rev (1998) 18:689–711. doi: 10.1016/S0272-7358(98)00025-7
137. Murray LK, Dorsey S, Haroz E, Lee C, Alsiary MM, Haydary A, et al. Bolton P. A Common Elements Treatment Approach for Adult Mental Health Problems in Low- and Middle-Income Countries. Cognit Behav Pract (2014) 21:111–23. doi: 10.1016/j.cbpra.2013.06.005
138. Strosahl KD, Robinson PJ. Adapting empirically supported treatments in the era of integrated care: A roadmap for success. Clin Psychol Sci Pract (2018) 25:1–19. doi: 10.1111/cpsp.12246
139. Ezard N, Thiptharakun S, Nosten F, Rhodes T, McGready R. Risky alcohol use among reproductive-age men, not women, in Mae la refugee camp, Thailand, 2009. Confl Health (2012) 6:7. doi: 10.1186/1752-1505-6-7
140. Lehavot K, Stappenbeck CA, Luterek JA, Kaysan D, Simpson TL. Gender Differences in Relationships among PTSD Severity, Drinking Motives, and Alcohol Use in a Comorbid Alcohol Dependence and PTSD Sample. Psychol Addict Behav (2015) 28:42–52. doi: 10.1037/a0032266.Gender
141. Kozarić-Kovačić D, Ljubin T, Grappe M. Comorbidity of posttraumatic stress disorder and alcohol dependence in displaced persons. Croat Med J (2000) 41:173–8.
142. Satyanarayana VA, Nattala P, Selvam S, Pradeep J, Hebbani S, Hegde S, et al. Integrated Cognitive Behavioral Intervention Reduces Intimate Partner Violence Among Alcohol Dependent Men, and Improves Mental Health Outcomes in their Spouses: A Clinic Based Randomized Controlled Trial from South India. J Subst Abuse Treat (2016) 64:29–34. doi: 10.1016/j.jsat.2016.02.005
143. Bourey C, Williams W, Bernstein EE, Stephenson R. Systematic review of structural interventions for intimate partner violence in low- and middle-income countries: Organizing evidence for prevention health behavior, health promotion and society. BMC Public Health (2015) 15:1165. doi: 10.1186/s12889-015-2460-4
144. Kraanen FL, Vedel E, Scholing A, Emmelkamp PMG. The comparative effectiveness of Integrated treatment for Substance abuse and Partner violence (I-StoP) and substance abuse treatment alone: a randomized controlled trial. BMC Psychiatry (2013) 13:189. doi: 10.1186/1471-244X-13-189
145. Morina N, Akhtar A, Barth J, Schnyder U. Psychiatric disorders in refugees and internally displaced persons after forced displacement: A systematic review. Front Psychiatry (2018) 9:433. doi: 10.3389/fpsyt.2018.00433
146. Ezard N, Debakre A, Catillon R. Screening and brief intervention for high-risk alcohol use in Mae La refugee camp, Thailand: A pilot project on the feasibility of training and implementation. Interv Int J Ment Heal Psychosoc Work Couns Areas Armed Confl (2010) 8:223–32. doi: 10.1097/WTF.0b013e3283413134
147. Guth S, Lindberg SA, Badger GJ, Thomas CS, Rose GL, Helzer JE. Brief Intervention in Alcohol-Dependent Versus Nondependent Individuals. J Stud Alcohol Drugs (2008) 69:243–50. doi: 10.15288/jsad.2008.69.243
148. Heather N. Breaking new ground in the study and practice of alcohol brief interventions. Drug Alcohol Rev (2010) 29:584–8. doi: 10.1111/j.1465-3362.2010.00204.x
149. Ouimette PC, Brown PJ, Najavits LM. Course and treatment of patients with both substance use and posttraumatic stress disorders. Addict Behav (1998) 23:785–95. doi: 10.1016/S0306-4603(98)00064-1
Keywords: alcohol, addiction, intervention, treatment, low- and middle-income country, systematic review
Citation: Preusse M, Neuner F and Ertl V (2020) Effectiveness of Psychosocial Interventions Targeting Hazardous and Harmful Alcohol Use and Alcohol-Related Symptoms in Low- and Middle-Income Countries: A Systematic Review. Front. Psychiatry 11:768. doi: 10.3389/fpsyt.2020.00768
Received: 10 May 2020; Accepted: 20 July 2020;
Published: 07 August 2020.
Edited by:
Otto Lesch, Medical University of Vienna, AustriaReviewed by:
Antoni Gual, Hospital Clínic de Barcelona, SpainGeorgios Demetrios Kotzalidis, Sapienza University of Rome, Italy
Copyright © 2020 Preusse, Neuner and Ertl. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Melissa Preusse, bWVsaXNzYS5wcmV1c3NlQHVuaS1iaWVsZWZlbGQuZGU=
 Melissa Preusse
Melissa Preusse Frank Neuner
Frank Neuner Verena Ertl
Verena Ertl