- 1Department of Clinical Psychology and Experimental Psychopathology, University of Groningen, Groningen, Netherlands
- 2Department of Psychology, Catholic University Eichstaett-Ingolstadt, Ingolstadt, Germany
Introduction
Recently, prolonged grief disorder (PGD), a diagnosis characterized by severe, persistent and disabling grief, was formally included in the 11th revision of the International Classification of Diseases [ICD-11; (1): Table 1]. To meet PGDICD-11 criteria one needs to experience persistent and pervasive longing for the deceased and/or persistent and pervasive cognitive preoccupation with the deceased, combined with any of 10 additional grief reactions assumed indicative of intense emotional pain for at least six months after bereavement. Contrary to the 5th revision of the Diagnostical and Statistical Manual of Mental Disorders [DSM-5; (11)] and the 10th revision of the International Classification of Diseases [ICD-10; (12)], the ICD-11 only uses a typological approach, implying that diagnosis descriptions are simple and there is no strict requirement for the number of symptoms one needs to experience to meet the diagnostic threshold.
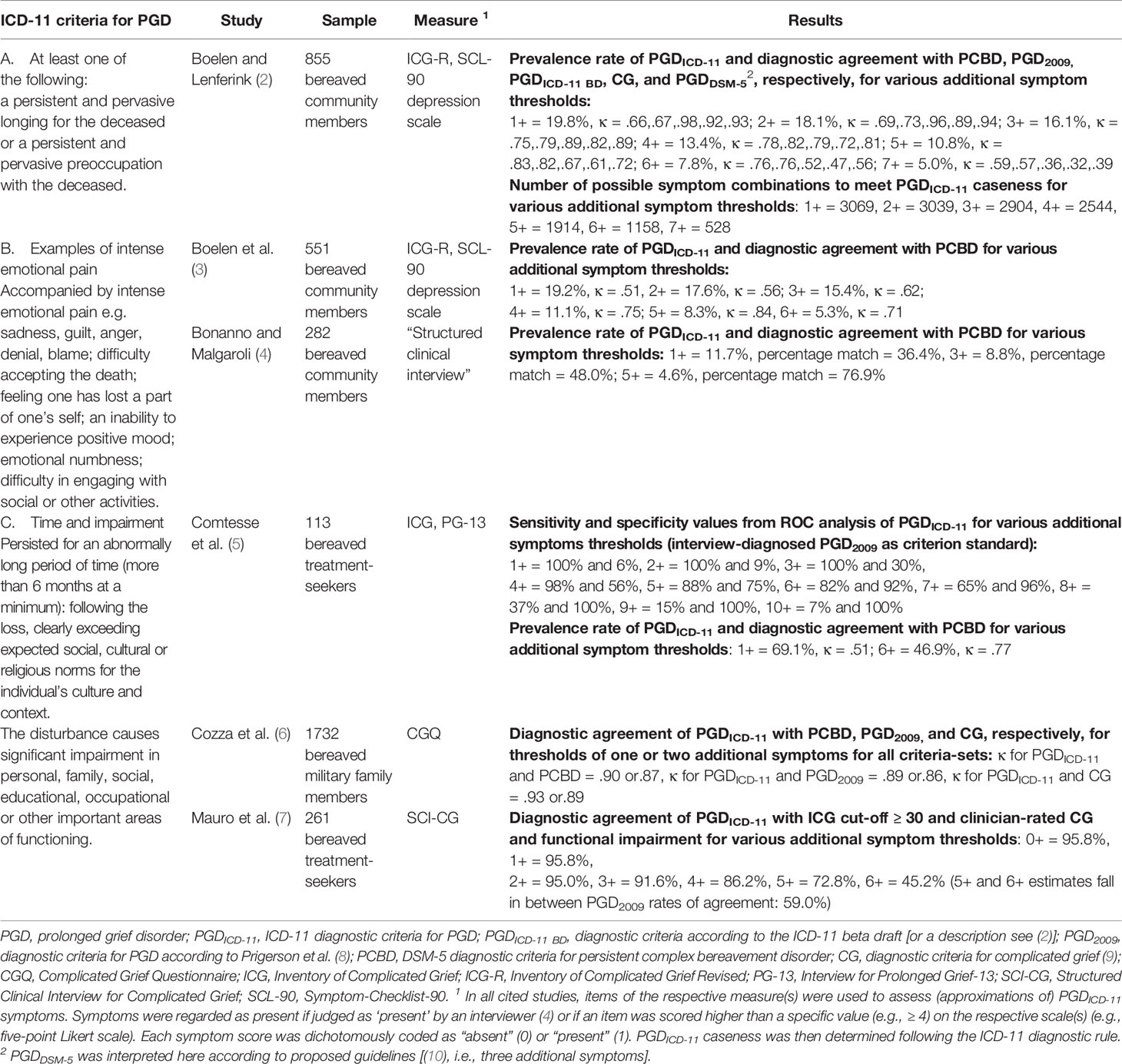
Table 1 Overview of ICD-11 diagnostic criteria for PGD and results of multiverse analyses of PGDICD-11.
Some researchers have argued that PGDICD-11’s typological approach is helpful, as it will lead to greater sensitivity in case identification in clinical practice and increased cross-cultural applicability (13). Others have highlighted that the typological approach allows for flexible diagnostic algorithms in research, so that PGDICD-11 criteria can be adapted to resemble the characteristics of both stricter and more lenient precursor criteria (14). In the current contribution, we take a different, complementary position. We highlight a series of challenges in using the PGD criteria for research purposes and discuss the application of a method that employs flexibility of PGDICD-11 diagnostic approach to address these challenges, which may help in working toward the unbiased, structured, and transparent identification of optimal criteria for disturbed grief.
A Critique of PGD ICD-11 for Research Purposes
A first challenge to researchers applying PGDICD-11 criteria is that they were completely new when first introduced and differed substantially from previously proposed diagnostic criteria sets (15). For example, PGDICD-11 contains multiple symptoms not found in any prior proposed criteria set, such as guilt, blame and the inability to experience positive mood [for a full criteria set comparison: (16)]. Furthermore, oft-used measures to assess disturbed grief responses, such as versions of the Inventory of Complicated Grief [e.g., ICG; (17)] do not fully assess PGDICD-11 criteria [6; for a recent review illustrating this point: (18)]. Therefore, the development of new, reliable and valid instruments is critical to assess the characteristics and validity of PGDICD-11 and determine for common research purposes [e.g., establishing prevalence, risk factors, treatment efficacy] who meets PGDICD-11 criteria. However, the typological approach in PGDICD-11 poses a substantial challenge to the development of such instruments.
First, the plain language used to formulate additional criteria makes it unclear what precisely each criterion implies. Single-word criteria “guilt,” “anger,” “denial,” and “blame” are particularly problematic. For example, “blame” could refer to self-blame or other-blame, blame for the death, or blame for something else. Since self-blame is much more prevalent in bereaved persons than blaming others (19) the interpretation of this criterion influences its prevalence. Moreover, blaming oneself for the death perpetuates disturbed grief, whereas blaming others for the death does not (20), so the characteristics and clinical correlates of this criterion may be very different depending on how it is interpreted [for a related discussion: (21)].
Second, even core criteria of “longing” and “preoccupation,” shared with most prior proposed grief disorders, are potentially problematic in their implementation. For example, it is unclear if a higher item-score threshold should be used to indicate that someone experiences persistent and pervasive longing, as it is the most frequently reported experience in bereavement (22), and, as a consequence, one of the least sensitive criteria in distinguishing those with and without disturbed grief (14). Preoccupation with the deceased is also already being interpreted differently by influential researchers in the grief field, with some viewing it as intrusive images about the death (23), and others as a process similar to grief rumination (24). While imagery and rumination are related processes, they are dissimilar in phenomenal characteristics, such as their duration, sensory experiences, and emotional correlates (25). The interpretation of this criterion will therefore have repercussions for what we regard as PGD.
Third, many key characteristics of PGDICD-11 (e.g., prevalence, classification, symptom heterogeneity) depend heavily on the chosen diagnostic algorithm. Pioneering research on characteristics of this disorder (with measures approximating actual criteria) used the minimal criteria as specified in the ICD-11 (i.e., at least one core criterion, and at least one additional criterion) in addition to the time and disability criteria (7, 26). It soon became apparent that applying these minimal criteria led to much higher prevalence rates for PGDICD-11 than for prior proposed criteria of PGD [PGD2009; (8)] and persistent complex bereavement disorder [PCBD; DSM-5, (10)]. This algorithm is thus relatively lenient, and applying it may lead to overdiagnosis and limited generalizability of findings on two of the most-studied grief disorder proposals (i.e., PGD2009; PCBD) to PGDICD-11 (14). This elicits the question: If the diagnostic algorithm directly derived from the ICD-11 text is too liberal, which diagnostic rules are then optimal for research?
Multiverse Analyses in Research on PGD ICD-11
In summary, a fundamental challenge for grief researchers in using the PGDICD-11 diagnosis is that its criteria are open for multiple interpretations and that the only diagnostic algorithm mapping one-on-one on the diagnosis description is too lenient. While the current criteria cannot easily be amended, their systematic investigation can make them more useful to researchers, for instance by providing a basis for achieving consensus on symptom interpretation, algorithms, and future PGD criteria. We propose that multiverse analyses can be particularly helpful in achieving such goals. Multiverse analyses typically consist of a procedure wherein one performs similar analyses across multiple datasets generated by making reasonable but variable choices on excluding, transforming and coding data (27). For example, when using a reaction time task with skewed data, one may perform analyses based on the median or the mean or analyze the data using parametric or non-parametric statistical tests. By comparing outcomes of multiple analyses, one can establish the degree of uncertainty about the conclusions one arrives at and the robustness of findings to arbitrary decisions made in data preparation and analysis. For example, one may discover that the direction and significance of effects is similar regardless of these decisions or that some decisions lead to significant effects, whereas others do not. The first scenario would allow for strong conclusions and the second scenario would signal caution is warranted in the interpretation of findings.
We advocate a similar but conceptually distinct procedure wherein empirical research examining the characteristics of PGDICD-11 systematically vary certain aspects of these criteria (e.g., using a more stringent cut-off for longing) or the diagnostic algorithm (e.g., varying the number of additional symptoms). A comparison of results obtained with multiple interpretations of criteria can help illuminate how robust specific results are dependent on multiple interpretations of the PGDICD-11 criteria. For example, one may be able to investigate the robustness of group differences between people with and without PGD on risk-factors and protective factors or treatment effectiveness (e.g., percentage with and without diagnosis after treatment) dependent on different interpretations of PGDICD-11. Additionally, critical information can be gathered on the influence of variations in symptom interpretations and algorithms on PGDICD-11 characteristics and how these characteristics compare to other proposed criteria sets [e.g., the newly developed PGD criteria for the upcoming text revision of DSM-5, (10)]. That is, multiverse analyses can be applied to shed light on a variety of clinically relevant characteristics of PGDICD-11 (e.g., retest and interrater reliability, specificity and sensitivity of classification, distinctiveness from other disorders, associations with functional impairment) when systematically modifying interpretations of its criteria.
Only a handful of studies have thus far applied such analyses, which have predominantly narrowly focused on examining characteristics of PGDICD-11 and their comparability against external standards when varying the number of additional criteria (see Table 1 for a summary). It has been observed that minimal PGDICD-11 criteria yield a similar prevalence as the relatively lenient Shear et al. criteria (9) for complicated grief (7), but almost two times higher prevalence than relatively strict PCBD criteria (2, 28, 29). Multiverse analyses in community samples demonstrated that similar prevalence estimates and good diagnostic agreement with PCBD and PGD2009 appears to be achieved with five additional criteria for PGDICD-11 [(2–4), cf. (7)]. Similarly, in treatment-seekers, minimal PGDICD-11 criteria correctly classified people against a relatively lenient standard of 30 or higher on the ICG (6, 7), yet as many as six additional symptoms were necessary to yield comparable prevalence and good diagnostic agreement with PGD2009 and PCBD (5). Moreover, one study demonstrated the influence of the number of additional symptoms on symptom heterogeneity, theoretically demonstrating that the number of ways to meet PGDICD-11 criteria ranges from 3.069 for one to 528 for seven additional symptoms (2). A less heterogeneous diagnosis is clearly preferable, as it would lead to less variability within groups of people meeting grief disorder criteria, making the distinction between these people more useful for research and practice (30). Taken together, these examples illustrate that the properties of PGDICD-11 depend on both the chosen diagnostic rule and the stringency of the comparison standard, and that the number of additional symptoms is critical in determining prevalence, clinical classification, and symptom profiles.
For future research, we recommend multiverse analyses varying not only the algorithm, but additionally symptom interpretations of single-item criteria and cognitive preoccupation and cut-offs for the presence of the longing criterion. We also advise to substantially expand the current focus of multiverse analyses of PGDICD-11 to establish the robustness of clinically-relevant findings (e.g., on treatment efficacy) and the variety of other aspects relevant to the validity of a diagnosis [for reviews: (13, 24)]. The latter includes - but is not limited to: reliability of classification [e.g., (31)], the structure of symptoms [e.g., (32)], distinctiveness from related disorders [e.g., (33)], and relationships with functional impairment [e.g., (34)]. We further advocate transparency in applying multiverse analyses and recommend: open access publication, data accessibility (e.g., through availability in repositories), fully specifying the origins and formulations of items used to assess PGDICD-11 and, if applicable, other disturbed grief criteria, and complete reporting of the variations of PGDICD-11 and outcomes under investigation.
Discussion
In the absence of clearly defined criteria and diagnostic rules for PGDICD-11, researchers should broadly apply structured methods to examine the characteristics of this disorder and compare it against past and future proposed grief disorders. Multiverse analyses can be a powerful tool to determine the validity and clinical usefulness of the PGDICD-11 criteria. By systematically varying the number of core and additional symptoms, the interpretation of symptoms, and the standards for meeting symptoms, we can evaluate how such decisions influence the characteristics of PGDICD-11, also in relation to different external standards. This will create a comprehensive research base enabling us to enhance our understanding of PGDICD-11 and of disturbed grief more generally. Creating this research base is no panacea: it cannot undo the inherent weaknesses of the PGDICD-11 criteria. However, the systematic evaluation of this information will help clarify under which circumstances diagnoses behave similarly or differently, providing a stepping stone to harmonize PGDICD-11 criteria with other criteria sets and to develop more optimal future disturbed grief criteria.
Author Contributions
All authors developed the ideas for this article. ME and HC wrote the first draft of the manuscript. RR contributed important intellectual content by providing critical revisions to the first draft.
Funding
ME was supported by a Netherlands Organization for Scientific Research (NWO) Veni grant [Grant ID: 016.veni195.113]. The funder did not play a role in the study design, the writing of the report or in the decision to submit the article for publication. RR was supported by a grant of Deutsche Forschungsgemeinschaft [Grant ID: RO2042/7-1]. The funder did not play a role in the study design, the writing of the report or the decision to submit the article for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. World Health Organization. ICD-11 beta draft website [Information]. (2018). Available at: https://icd.who.int/browse11/l-m/en (Accessed on 24th June 2020).
2. Boelen PA, Lenferink L IM. Comparison of six proposed diagnostic criteria sets for disturbed grief. Psychiatry Res (2020) 285:112786. doi: 10.1016/j.psychres.2020.112786
3. Boelen PA, Lenferink L IM, Smid GE. Further evaluation of the factor structure, prevalence, and concurrent validity of DSM-5 criteria for persistent complex bereavement disorder and ICD-11 criteria for prolonged grief disorder. Psychiatry Res (2019a) 3:206–10. doi: 10.1016/j.psychres.2019.01.006
4. Bonanno GA, Malgaroli M. Trajectories of grief: Comparing symptoms from the DSM-5 and ICD-11 diagnoses. Depress Anxiety (2020) 37:17–25. doi: 10.1002/da.22902
5. Comtesse H, Vogel A, Kersting A, Rief W, Steil R, Rosner R. When does grief become pathological? Evaluation of the ICD-11 diagnostic proposal for prolonged grief in a treatment-seeking sample. Eur J Psychotraumatol (2020) 11:1694348. doi: 10.1080/20008198.2019.1694348
6. Cozza SJ, Shear MK, Reynolds CF, Fisher JE, Zhou J, Maercker A, et al. Optimizing the clinical utility of four proposed criteria for a persistent and impairing grief disorder by emphasizing core, rather than associated symptoms. Psychol Med (2020) 50:438–45. doi: 10.1017/S0033291719000254
7. Mauro C, Reynolds CF, Maercker A, Skritskaya N, Simon N, Zisook S, et al. Prolonged grief disorder: Clinical utility of ICD-11 diagnostic guidelines. Psychol Med (2019) 49:861–7. doi: 10.1017/S0033291718001563
8. Prigerson HG, Horowitz MJ, Jacobs SC, Parkes CM, Aslan M, Goodkin K, et al. Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PloS Med (2009) 6:e1000121. doi: 10.1371/journal.pmed.1000121
9. Shear MK, Simon N, Wall M, Zisook S, Neimeyer R, Duan N, et al. Complicated grief and related bereavement issues for DSM-5. Depress Anxiety (2011) 28:103–17. doi: 10.1002/da.20780
10. American Psychiatric Association. View and comment on recently proposed changes to DSM–5. (2020). Available at: https://www.psychiatry.org/psychiatrists/practice/dsm/proposed-changes (Accessed on 24th of June 2020).
11. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. American Psychiatric Publishing: Arlington, VA (2013).
12. World Health Organization. ICD-10: international statistical classification of diseases and related health problems: tenth revision. 2nd ed. Geneva, Switzerland: World Health Organization (2004).
13. Killikelly C, Maercker A. Prolonged grief disorder for ICD-11: The primacy of clinical utility and international applicability. Eur J Psychotraumatol (2017) 8:1476441. doi: 10.1080/20008198.2018.1476441
14. Simon NM, Wall MM, Keshaviah A, Dryman MT, LeBlanc NJ, Shear MK. Informing the symptom profile of complicated grief. Depress Anxiety (2011) 28:118–26. doi: 10.1002/da.20775
15. Eisma MC, Lenferink L IM. Response to: Prolonged grief disorder for ICD-11: The primacy of clinical utility and international applicability. Eur J Psychotraumatol (2017) 8:1512249. doi: 10.1080/20008198.2018.1512249
16. Lenferink L IM, Boelen PA, Smid G, Paap M. The importance of harmonising diagnostic criteria sets for pathological grief. Brit J Psychiat (in press), 1–4. doi: 10.1192/bjp.2019.240
17. Prigerson HG, Maciejewski PK, Reynolds CF, IIIII, Bierhals AJ, Newsom JT, Fasiczka A, et al. Inventory of complicated grief: A scale to measure maladaptive symptoms of loss. Psychiatry Res (1995) 59:65–79. doi: 10.1016/0165-1781(95)02757-2
18. Treml J, Kaiser J, Plexnies A, Kersting A. Assessing prolonged grief disorder: A systematic review of assessment instruments. J Affect Disord (2020) 274:420–34. doi: 10.1016/j.jad.2020.05.049
19. Davis CG, Lehman DR, Wortman CB, Silver RC, Thompson SC. The undoing of traumatic life events. Pers Soc Psychol Bull (1995) 21:109–24. doi: 10.1177/0146167295212002
20. Eisma MC, Epstude K, Schut HAW, Stroebe MS, Simion A, Boelen PA. Upward and downward counterfactuals after loss: A multi-wave controlled longitudinal study. Behav Ther (in press). doi: 10.1016/j.beth.2020.07.007
21. Greene T. Blame, PTSD and DSM-5: An urgent need for clarification. Eur J Psychotraumatol (2018) 9:1468709. doi: 10.1080/20008198.2018.1468709
22. Maciejewski PK, Zhang B, Block SD, Prigerson HG. An empirical examination of the stage theory of grief. JAMA (2007) 297:716–23. doi: 10.1001/jama.297.7.716
23. Boelen PA, Smid GE. The Traumatic Grief Inventory Self-Report Version (TGI-SR): Introduction and preliminary psychometric evaluation. J Loss Trauma (2017) 22:196–212. doi: 10.1080/15325024.2017.1284488
24. Simon NM, Shear MK, Reynolds CF, Cozza SJ, Mauro C, Zisook S, et al. Commentary on evidence in support of a grief-related condition as a DSM diagnosis. Depress Anxiety (2020) 37:9–16. doi: 10.1002/da.22985
25. Speckens AE, Ehlers A, Hackmann A, Ruths FA, Clark DM. Intrusive memories and rumination in patients with post-traumatic stress disorder: A phenomenological comparison. Mem (2007) 15:249–57. doi: 10.1080/09658210701256449
26. Boelen PA, Lenferink L IM, Nickerson A, Smid GE. Evaluation of the factor structure, prevalence, and validity of disturbed grief in DSM-5 and ICD-11. J Affect Disord (2018) 240:79–87. doi: 10.1016/j.jad.2018.07.041
27. Steegen S, Tuerlinckx F, Gelman A, Vanpaemel W. Increasing transparency through a multiverse analysis. Perspect Psychol Sci (2016) 11:702–12. doi: 10.1177/1745691616658637
28. Boelen PA, Spuij M, Lenferink L II. Comparison of DSM-5 criteria for persistent complex bereavement disorder and ICD-11 criteria for prolonged grief disorder in help-seeking bereaved children. J Affect Disord (2019b) 250:71–8. doi: 10.1016/j.jad.2019.02.046
29. O’Connor M, Lasgaard M, Larsen L, Johannsen M, Lundorff M, Farver-Vestergaard I, et al. Comparison of proposed diagnostic criteria for pathological grief using a sample of elderly bereaved spouses in Denmark: Perspectives on future bereavement research. J Affect Disord (2019) 251:52–9. doi: 10.1016/j.jad.2019.01.056
30. Lenferink L IM, Eisma MC. 37.650 ways to have “persistent complex bereavement disorder” yet only 48 ways to have “prolonged grief disorder”. Psychiatry Res (2018) 261:88–9. doi: 10.1016/j.psychres.2017.12.050
31. Lichtenthal WG, Maciejewski PK, Demirjian CC, Roberts KE, First MB, Kissane DW, et al. Evidence of the clinical utility of a prolonged grief disorder diagnosis. World Psychiatry (2018) 17:364–5. doi: 10.1002/wps.20544
32. Golden A-M, Dalgleish T. Is prolonged grief distinct from bereavement-related posttraumatic stress? Psychiatry Res (2010) 178:336–41. doi: 10.1016/j.psychres.2009.08.021
33. Malgaroli M, Maccallum F, Bonanno G. Symptoms of persistent complex bereavement disorder, depression, and PTSD in a conjugally bereaved sample: A network analysis. Psychol Med (2018) 48:1–10. doi: 10.1017/S0033291718001769
Keywords: prolonged grief disorder, persistent complex bereavement disorder, complicated grief, criteria, algorithm, criticism, critique, multiverse analyses
Citation: Eisma MC, Rosner R and Comtesse H (2020) ICD-11 Prolonged Grief Disorder Criteria: Turning Challenges Into Opportunities With Multiverse Analyses. Front. Psychiatry 11:752. doi: 10.3389/fpsyt.2020.00752
Received: 24 February 2020; Accepted: 16 July 2020;
Published: 07 August 2020.
Edited by:
Birgit Wagner, Medical School Berlin, GermanyReviewed by:
Sebastian Trautmann, Medical School Hamburg, GermanyNadine Stammel, Freie Universität Berlin, Germany
Carina Heeke, Freie Universität Berlin, Germany
Copyright © 2020 Eisma, Rosner and Comtesse. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maarten C. Eisma, bS5jLmVpc21hQHJ1Zy5ubA==
 Maarten C. Eisma
Maarten C. Eisma Rita Rosner
Rita Rosner Hannah Comtesse
Hannah Comtesse