
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 06 May 2020
Sec. Addictive Disorders
Volume 11 - 2020 | https://doi.org/10.3389/fpsyt.2020.00352
This article is part of the Research TopicNeurobiological Biomarkers for Developing Novel Treatments of Substance and Non-Substance AddictionView all 45 articles
 Qiuping Huang1,2,3
Qiuping Huang1,2,3 Ying Li3
Ying Li3 Shucai Huang4
Shucai Huang4 Jing Qi5
Jing Qi5 Tianli Shao1,2
Tianli Shao1,2 Xinxin Chen1,2
Xinxin Chen1,2 Zhenjiang Liao1,2
Zhenjiang Liao1,2 Shuhong Lin1,2
Shuhong Lin1,2 Xiaojie Zhang1,2
Xiaojie Zhang1,2 Yi Cai6
Yi Cai6 Hongxian Chen1,2*
Hongxian Chen1,2*Background: Chinese college students are at high risk of sleep problems, and smartphone use is common among this population. However, the relationship between smartphone use characteristics and sleep problems in Chinese college students has been inadequately studied. In this preliminary study, we examined the association of poor sleep quality with smartphone use in a sample of Chinese college students from a health vocational college in Changsha, China.
Methods: A total of 439 college students completed a self-report questionnaire containing the Pittsburgh Sleep Quality Index (PSQI) and questions regarding demographic information, psychosocial factors, physical health, smartphone use characteristics, and mobile phone addiction (MPA).
Results: The results showed that the prevalence of poor sleep quality (PSQI > 7) in Chinese college students was 9.8%. In multiple logistic regression analysis, poor sleep quality was significantly associated with male gender (OR: 2.80, P: 0.022), not having good physical health (OR: 2.61, P: 0.020), headache (OR: 2.47, P: 0.014), more severe depressive symptoms (OR: 2.17, P: 0.049), > four years of smartphone use (OR: 3.38, P: 0.001), > five hours of daily smartphone use (OR: 2.19, P: 0.049), and more severe inability to control MPA craving (OR: 2.04, P: 0.040).
Conclusion: Our findings suggest that excessive smartphone use and MPA are associated with poor sleep quality in a sample of Chinese college students from a health vocational college. Because of the limited sample representativeness and cross-sectional design of this study, large-scale prospective representative studies are warranted to confirm these associations.
College students are at considerably high risk for sleep problems. Worldwide, the prevalence of insomnia in university students has been found to be 18.5%, much higher than the 7.4% rate in the general population (1). A cross-national survey reported an overall 10.4% prevalence of severe or extreme nocturnal sleeping problems in undergraduate university students during the previous month, with the lowest seen in Thailand (3.0%) and the highest in Indonesia (32.9%) (2). Chinese university students are also at increased risk of sleep problems; for example, 25.7% of university students have sleep problems, a rate two to three times that of the general Chinese population (7.4-15.0%) (1, 3, 4). Evidence from empirical studies has shown that sleep disturbance is a major risk factor for a variety of physical and mental morbidities and increased mortality, including obesity, cardiovascular diseases, depression, and cognitive impairment (5–10). For students, sleep disorder is also significantly associated with poor academic performance and elevated risk of suicidal behaviors (11, 12).
A diversity of factors have been reported to be associated with sleep problems in university students, such as smoking, academic failure, depression, anxiety, and stress (13–16). In recent years, because of the rapid development of communications and information technologies, smartphone use has been very popular in young people, particularly university students. While smartphone use has made our lives more convenient, it also has negative effects on the health of users. For example, in the international literature, sleep problems in university students and adolescents have been significantly associated with mobile phone addiction (MPA) and various measures of problematic smartphone use, including long duration of smartphone usage, late-night smartphone use, bedtime smartphone use, and excessive use of a smartphone (17–23). In addition, there is evidence that smartphone overuse impairs cognition via its negative influences on mood and sleep (24).
In China, there have been a few studies examining the relationship between smartphone use and sleep problems in university students. Similar associations of sleep problems with MPA, long-term smartphone use, smartphone use before going to bed, and sleeping near the phone, have been reported (25–30). A prospective cohort study of Chinese college students has shown that long-time mobile phone use predicts sleep disturbances, and there is a bidirectional relationship between the duration of phone use and various sleep outcomes (25). Thus, results from both international and Chinese studies suggest that both some characteristics of smartphone use (i.e., duration of phone use, bedtime smartphone use, et al.) and MPA are involved in the etiology of the sleep problems of university students. However, it remains unknown which type of smartphone use variables (i.e., long duration of phone use versus MPA) is the strongest predictor of sleep problems, because these prior studies seldom examined the association of sleep problems with the two types of variables simultaneously. The relative contributions of the two groups of variables to sleep problems are potentially important, because these data may inform the level of intervention intensity required (i.e., health education vs. psychotherapy) if we want to address the sleep problems of university students via reducing problematic smartphone use.
Changsha is a major municipality in central-south China with a total population of 7,918,100, of which 672,000 are university students from its 51 universities. Due to societal concern about the misuse of smartphones by university students, our research team focuses on the prevention of MPA and its association with health problems in university campuses. To facilitate the design of a large-scale municipality-wide study on smartphone use and sleep health in university students of Changsha, China, a preliminary study was carried out to investigate the prevalence of poor sleep quality in a sample of Chinese college students, with a particular focus on its associated smartphone use factors. We hypothesized that long time phone use, high expense, and MPA would be negatively correlated with sleep quality in Chinese college students.
This cross-sectional study was conducted in May 2016. By using cluster sampling, all college students of the ten classes of the Department of Pharmacy, Changsha Health Vocational College, were invited to participate in this study. Students who were unwilling to join the study and had severe physical illnesses were excluded.
The study protocol was approved by the Institutional Review Board of Changsha Health Vocational College. Written consent was obtained from all participants, as well as their headteachers and parents, when necessary.
We used a self-administered questionnaire to collect demographic information and data on psychosocial factors, physical health, smartphone use characteristics, and MPA. Before starting the study, the questionnaire was tested with a small sample of college students, and it was finalized after the pilot study.
Demographic data collected included gender, age, place of origin (rural vs. urban), and self-rated level of family income (good, fair, poor).
Psychosocial factors were depression and social support. In China, the University Personality Inventory (UPI) is the most widely used scale for assessing the mental health of college students (31). It consists of 60 items that assess a wide variety of psychopathological symptoms that an individual may have experienced in the previous year. Nevertheless, the administration time of UPI is a little long, and, therefore, it is not suitable for an epidemiological survey. Importantly, the factor structure of UPI in Chinese college students varies across studies (32–34), making it difficult to explain the test results of UPI. After expert consultation, we decided to use 12 items of the UPI to operationally construct a scale of depressive symptoms (SDS): poor appetite (item 1), feeling pessimistic (item 13), distracted (item 14), or restless (item 23), having suicidal thoughts (item 25), no interest in anything (item 26), a lack of judgment (item 29), good mood (item 35, reverse-scored), or lack of confidence (item 38), and feeling self-abased (item 44), physically exhausted (item 46), and hesitant (item 52). Because these items corresponded to the symptomatology of major depression according to DSM-IV criteria (35), SDS was defined in this manner. To avoid the overlap of the insomnia symptoms of depression and the outcome of our study, sleep quality, item 16 of the UPI (frequent insomnia) was not included in the SDS. All items were answered on a binary (yes/no, rated 1/0) scale. The total score of SDS ranged between 0 and 12, with a higher score denoting more severe depression. In our sample of college students, the internal consistency of SDS was satisfactory (Cronbach's α coefficient: 0.751).
We used two subscales of the Social Support Rating Scale (SSRS) to assess the level of social support: subjective social support and utilization of social support. Developed by Shuiyuan Xiao in 1986, the SSRS has good reliability and validity (36). A higher total score in each subscale represents a higher level of social support (37).
Two questions were used to evaluate physical health: “During the past year, did you often feel that you were in good physical health?” and “During the past year, did you often suffer from headaches?” Respondents who answered “yes” were categorized as having good physical health or headaches.
Smartphone use-related variables included length of smartphone use (years), smartphone charge per month (Yuan), duration of daily smartphone use and mobile internet use (hours), and MPA. MPA was assessed with the validated Chinese Mobile Phone Addiction Index (MPAI), which has 17 items and gauges four dimensions of MPA: inability to control cravings (ICC), feeling anxious and lost (FAL), withdrawal or escapism (WE), and productivity loss (PL) (38, 39). Each item of the MPAI is rated on a five-point Likert scale, from 1=never to 5=always. Higher scores indicate greater severity of MPA.
The primary outcome of the present study, sleep quality, was assessed with the validated Chinese Pittsburgh Sleep Quality Index (PSQI) (40, 41). The PSQI has 18 items,and its total score varies between zero and 21, with a higher score indicating poorer sleep quality. In China, a total score of eight or more is indicative of poor sleep quality (42).
Respondents were categorized into subgroups according to demographic, psychosocial, physical health, and phone use characteristics. Prevalences of poor sleep quality in the whole sample and in different subgroups of college students were calculated. Chi-square (χ2) test and Fisher's exact test were used to compare poor sleepers and normal sleepers between subgroups. Multicollinearity of independent variables was tested prior to the formal analysis. We found a very low degree of multicollinearity among independent variables because the Variance Inflation Factor values of all independent variables ranged from 1.02 to 1.16, substantially below the critical threshold of 10. Multiple logistic regression with a backward stepwise entry of all significant factors in univariate analysis was used to identify factors associated with poor sleep quality. Odds ratio (OR) and 95% confidence intervals (CIs) were generated for each variable. The statistical significance level was set at p < 0.05 (two-sided). SPSS software version 20.0 package was used for all analyses.
A total of 443 college students were invited to participate in the study, and all agreed. Four students were excluded due to an incomplete questionnaire, so the final sample consisted of 439 completers. The average age of the 439 college students was 18.8 years (standard deviation [SD]: 1.7, range: 15-24), and 86.8% were female. The mean length of smartphone use was 3.9 years (SD: 2.3). Detailed socio-demographic and smartphone use characteristics are displayed in Table 1.
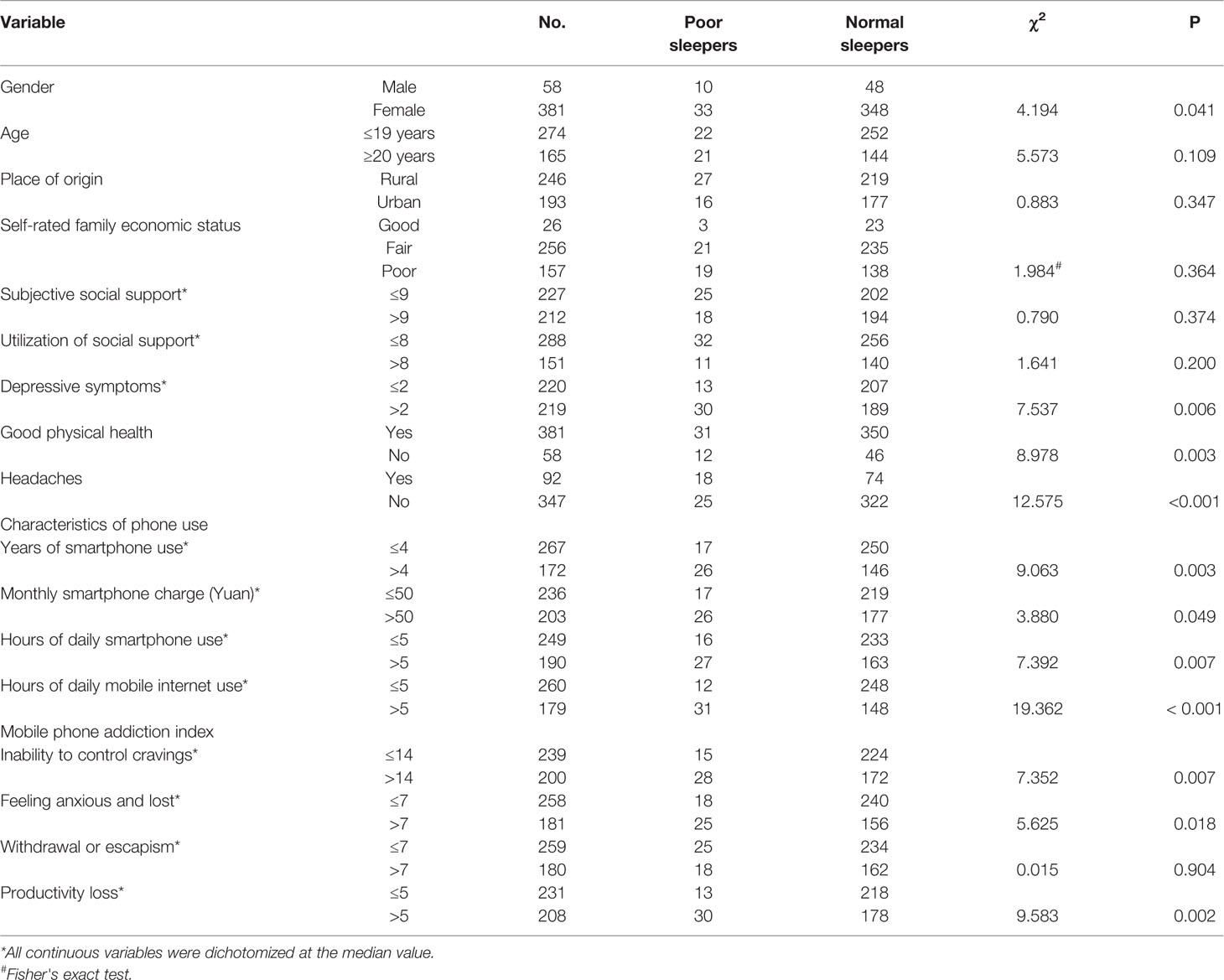
Table 1 Socio-demographic and smartphone use characteristics of college students and comparison between poor sleepers and normal sleepers by variable.
The mean PSQI score was 4.5 (SD: 2.3). A total of 43 students (9.8%) had poor sleep quality (PSQI > 7). Results from Chi-square tests and Fisher's exact test (Table 1) show that poor sleepers were more likely to be male students (P=0.041), not to have good physical health (P=0.003), to suffer from headaches (P < 0.001), to have more severe depressive symptoms (as indicated by a score of two or more, P=0.006), to have been using a smartphone for more than four years (P=0.003), to pay a monthly phone charge of 50 Yuan or more (P=0.049), to use the phone for more than five hours per day (P=0.007), to use mobile internet for more than five hours per day (P < 0.001), and to have more severe MPA in terms of ICC (P=0.007), FAL (P=0.018), and PL (P=0.002).
Multivariable logistic regression analysis (Table 2) show that poor sleep quality in college students was significantly associated with male gender (OR: 2.80, P: 0.022), not having good physical health (OR: 2.61, P: 0.020), headaches (OR: 2.47, P: 0.014), more severe depressive symptoms (OR: 2.17, P: 0.049), > four years of smartphone use (OR: 3.38, P: 0.001), > five hours of daily smartphone use (OR: 2.19, P: 0.049), and more severe ICC (OR: 2.04, P: 0.040).
According to the statistics provided by the China Internet Network Information Center (CNNIC), by June 2019, the number of internet users in China was 854 million, and 847 million (99.1%) used mobile phones to access the internet. Of the total internet users, 41.5% were 10–29 years old, and 26% were students (the largest group) (43). Therefore, Chinese adolescents and young adults such as college students are the most vulnerable group to problematic smartphone use. To the best of our knowledge, our study is one of the very few to examine associations of poor sleep quality with smartphone use characteristics and MPA. We found that nearly one-tenth (9.8%) of the Chinese college students reported poor sleep quality and that poor sleep quality was significantly associated with male gender, not having good physical health, headaches, more severe depressive symptoms, >four years of smartphone use, >five hours of daily smartphone use, and more severe ICC of MPA.
The 9.8% prevalence of poor sleep quality revealed in our sample of college students is exactly the same as that of college students in Anhui, a central province in China (44) but lower than that of Chinese university students (25.7%) and the general population (15.0%) reported by two meta-analytic reviews (3, 4). The lower rate of poor sleep quality in this study might be related to the lower level of academic stress in college students of a health vocational college compared to college students of general universities. However, due to differences in sample characteristics (i.e., percentage of male students) and assessments of sleep problem (i.e., PSQI vs. Athens Insomnia Scale) across existing studies, the relatively low prevalence of poor sleep quality does not necessarily mean a low risk of sleep problems in our sample of college students. Considering the many negative health effects associated with sleep problems and the very large number of Chinese college students, this 9.8% prevalence figure suggests that the sleep problems of college students still deserve preventive and clinical attention.
Overall, the significant associations between poor sleep quality and poor physical health (as indicated by not having good physical health and headache) and depression are consistent with prior studies (45–47). These could be explained by the complex reciprocal relationships between sleep disorders and pain, chronic conditions, and depression (46, 48–50). For example, poor physical and mental health would cause insomnia, and insomnia would exacerbate physical and mental health problems.
Numerous studies have confirmed the female predisposition to sleep problems in various populations, including college students, young adults, and adults (51–55), but we found a significantly elevated risk of poor sleep quality in male compared to female students. This unexpected phenomenon might be related to some unknown male-specific stressors, because, in most Chinese health vocational colleges, male students are the minority group, usually accounting for less than 5% of the total students. Nevertheless, since the sample size of male students is small (n=58), further investigation is warranted to validate this finding.
Our findings on the significant relationships between poor sleep quality and excessive smartphone use (as indicated by more years of smartphone use and more hours of daily smartphone use) and more MPA-associated ICC are generally in line with existing international and Chinese studies, despite the different measures of smartphone overuse and MPA used (17–23, 25–30). The difference between this study and other studies is that excessive smartphone use and MPA simultaneously contributed to the poor sleep quality of college students. Although the long-term effect of smartphone use on health remains unclear, the identified association between more years of smartphone use and poor sleep quality in our study might suggest a cumulative adverse effect of smartphone use on sleep.
Several mechanisms have been proposed to explain the negative effect of smartphone use on sleep. First, long-time phone use directly reduces the user's time spent on sleep, in particular bedtime smartphone use, resulting in insufficient sleep. Second, some phone users prefer to browse mobile websites before bed. Inappropriate content on these websites may make the users feel tension and excitement, leading to difficulties in initiating sleep. Third, excessive smartphone use may affect sleep via some physiological and psychological pathways (27, 56). For example, exposure to the light of smartphone screens and radiation from the phone during bedtime could influence the onset time and secretion of melatonin, which in turn causes sleep-wake rhythm disorders (25, 57). Fourth, morphological evidence from an fMRI study has confirmed alterations in gray matter volume and white matter integrity in college students with MPA (58); we speculate that MPA would affect sleep via several neurobiological pathways, which need to be further understood.
As a preliminary study, some limitations are unavoidable. First, this is a cross-sectional study, so the significant associations of poor sleep with poor physical health, depression, unhealthy smartphone use, and MPA found are not, strictly speaking, causal relationships. The influences of these factors on sleep need to be examined by prospective longitudinal studies. Second, our sample of college students was recruited from one health vocational college only, so the sample representativeness is very limited. Caution is needed when generalizing our findings to students of other colleges and universities. Third, although the internal consistency of our measure of depression was satisfactory and its items were believed to mirror depressive symptoms, empirical data on its validity were still unavailable in this study. Studies using common depression scales are warranted to examine the sleep–smartphone use associations. Fourth, our assessment of perceived physical health was based on only a single question, which may be unable to capture all dimensions of physical well-being. Fifth, there are no clinical diagnoses of mobile phone addiction, and the results from MPA assessment can only indicate the severity of phone addiction. Sixth, there are some other limitations, such as inadequate controlling of other variables associated with poor sleep, such as anxiety, and no assessment of the contents browsed on the phone before falling asleep, which could influence sleep quality.
In summary, in this sample of Chinese college students from a health vocational college in Changsha, China, one out of every ten have poor sleep quality, and poor sleep quality is significantly associated with poor physical health, depression, excessive smartphone use, and MPA. Given the common use of smartphones in Chinese colleges and the association of this use with sleep problems, administrators and health workers at Chinese colleges should pay more attention in terms of research and interventions to problematic smartphone use among students. Further investigation is justified into whether reducing smartphone use and MPA can improve the sleep quality of Chinese college students. Nevertheless, because of the limited sample representativeness and cross-sectional design of this study, large-scale prospective representative studies are warranted to confirm these associations.
All datasets generated for this study are included in the article/supplementary material.
The studies involving human participants were reviewed and approved by the Institutional Review Board of Changsha Health Vocational College. The patients/participants provided their written informed consent to participate in this study.
All authors made substantial contributions to this study. QH and HC conceptualized and designed the research. XZ, JQ, and SL prepared the assessment tools. TS, ZL, and XC performed the experiments. YC and YL undertook the statistical analysis. QH and SH wrote the first draft of the manuscript and contributed to the final manuscript. All authors critically reviewed content and approved the final version for publication.
This work was supported by the National Natural Science Foundation of China (81971249), the National Basic Research Program of China (2015CB553504), and the National Research Program of China (2016YFC0800908-Z02).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors would like to thank all the participating teachers and students from the Department of Pharmacy, Changsha Health Vocational College, for their cooperation. The first author, QH, is grateful to colleagues in the Department of Pharmacy, Dr. Yongwang Yan, Prof. Zhihui Wang, Liping Wang, Qiaoping Lu, and Xiaoyan Wang, for their support during the period of the study.
1. Jiang XL, Zheng XY, Yang J, Ye CP, Chen YY, Zhang ZG, et al. A systematic review of studies on the prevalence of insomnia in university students. Public Health (2015) 129(12):1579–84. doi: 10.1016/j.puhe.2015.07.030
2. Peltzer K, Pengpid S. Nocturnal sleep problems among university students from 26 countries. Sleep Breath (2015) 19:499–508. doi: 10.1007/s11325-014-1036-3
3. Li L, Wang YY, Wang SB, Zhang L, Li L, Xu DD, et al. Prevalence of sleep disturbances in Chinese university students: a comprehensive meta-analysis. J Sleep Res (2018) 27(3):e12648. doi: 10.1111/jsr.12648
4. Cao XL, Wang SB, Zhong BL, Zhang L, Ungvari GS, Ng CH, et al. The prevalence of insomnia in the general population in China: A meta-analysis. PloS One (2017) 12(2):e0170772. doi: 10.1371/journal.pone.0170772
5. Li Y, Zhang X, Winkelman JW, Redline S, Hu FB, Stampfer M, et al. Association between insomnia symptoms and mortality: a prospective study of U.S. men. Circulation (2014) 129(7):737–46. doi: 10.1161/CIRCULATIONAHA.113.004500
6. Sofi F, Cesari F, Casini A, Macchi C, Abbate R, Gensini GF. Insomnia and risk of cardiovascular disease: a meta-analysis. Eur J Prev Cardiol (2014) 21(1):57–64. doi: 10.1177/2047487312460020
7. Benedict C, Hallschmid M, Lassen A, Mahnke C, Schultes B, Schioth HB, et al. Acute sleep deprivation reduces energy expenditure in healthy men. Am J Clin Nutr (2011) 93(6):1229–36. doi: 10.3945/ajcn.110.006460
8. Li L, Wu C, Gan Y, Qu X, Lu Z. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry (2016) 16(1):375. doi: 10.1186/s12888-016-1075-3
9. Fortier-Brochu E, Morin CM. Cognitive impairment in individuals with insomnia: clinical significance and correlates. Sleep (2014) 37(11):1787–98. doi: 10.5665/sleep.4172
10. Zhong BL, Liu TB, Chan SSM, Jin D, Hu CY, Dai J, et al. Common mental health problems in rural-to-urban migrant workers in Shenzhen, China: prevalence and risk factors. Epidemiol Psychiatr Sci (2018) 27(3):256–65. doi: 10.1017/S2045796016001141
11. Lee YJ, Park J, Kim S, Cho SJ, Kim SJ. Academic performance among adolescents with behaviorally induced insufficient sleep syndrome. J Clin Sleep Med (2015) 11(1):61–8. doi: 10.5664/jcsm.4368
12. Becker SP, Dvorsky MR, Holdaway AS, Luebbe AM. Sleep problems and suicidal behaviors in college students. J Psychiatr Res (2018) 99:122–8. doi: 10.1016/j.jpsychires.2018.01.009
13. Almojali AI, Almalki SA, Alothman AS, Masuadi EM, Alaqeel MK. The prevalence and association of stress with sleep quality among medical students. J Epidemiol Glob Health (2017) 7(3):169–74. doi: 10.1016/j.jegh.2017.04.005
14. Schlarb AA, Classen M, Grunwald J, Vogele C. Sleep disturbances and mental strain in university students: results from an online survey in Luxembourg and Germany. Int J Ment Health Syst (2017) 11:24. doi: 10.1186/s13033-017-0131-9
15. Gaultney JF. The prevalence of sleep disorders in college students: impact on academic performance. J Am Coll Health (2010) 59(2):91–7. doi: 10.1080/07448481.2010.483708
16. Basdav J, Haffejee F, Puckree T. Impact of headaches on university students in Durban, South Africa. Springerplus (2016) 5(1):1679. doi: 10.1186/s40064-016-3372-1
17. Gladius J, Sowmiya K, Vidya D, Archana L, Roseline F. A study of mobile phone usage on sleep disturbance, stress and academic performance among medical students in Tamil Nadu. Int J Community Med Public Health (2018) 5(1):365–8. doi: 10.18203/2394-6040.ijcmph20175814
18. Amra B, Shahsavari A, Shayan-Moghadam R, Mirheli O, Moradi-Khaniabadi B, Bazukar M, et al. The association of sleep and late-night cell phone use among adolescents. J Pediatr (Rio J) (2017) 93(6):560–7. doi: 10.1016/j.jped.2016.12.004
19. Tamura H, Nishida T, Tsuji A, Sakakibara H. Association between Excessive Use of Mobile Phone and Insomnia and Depression among Japanese Adolescents. Int J Environ Res Public Health (2017) 14(7):701. doi: 10.3390/ijerph14070701
20. Exelmans L, Van den Bulck J. Bedtime mobile phone use and sleep in adults. Soc Sci Med (2016) 148:93–101. doi: 10.1016/j.socscimed.2015.11.037
21. Demirci K, Akgonul M, Akpinar A. Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. J Behav Addict (2015) 4(2):85–92. doi: 10.1556/2006.4.2015.010
22. Lee JE, Jang SI, Ju YJ, Kim W, Lee HJ, Park EC. Relationship between Mobile Phone Addiction and the Incidence of Poor and Short Sleep among Korean Adolescents: a Longitudinal Study of the Korean Children & Youth Panel Survey. J Korean Med Sci (2017) 32(7):1166–72. doi: 10.3346/jkms.2017.32.7.1166
23. Sahin S, Ozdemir K, Unsal A, Temiz N. Evaluation of mobile phone addiction level and sleep quality in university students. Pak J Med Sci (2013) 29(4):913–8. doi: 10.12669/pjms.294.3686
24. Wilmer HH, Sherman LE, Chein JM. Smartphones and Cognition: A Review of Research Exploring the Links between Mobile Technology Habits and Cognitive Functioning. Front Psychol (2017) 8:605. doi: 10.3389/fpsyg.2017.00605
25. Liu S, Wing YK, Hao Y, Li W, Zhang J, Zhang B. The associations of long-time mobile phone use with sleep disturbances and mental distress in technical college students: a prospective cohort study. Sleep (2019) 42(2):1–10. doi: 10.1093/sleep/zsy213
26. Li L, Mei S, Niu Z. Influences of smartphone addiction and negative affect on sleep quality among university students. Chin J Public Health (2016) 32(5):646–9.
27. Liu Q, Zhou Z, Yang X, Kong F, Niu G, Fan C. Mobile phone addiction and sleep quality among Chinese adolescents: A moderated mediation model. Comput Hum Behav (2017) 72(C):108–14. doi: 10.1016/j.chb.2017.02.042
28. Wang H, Rao J, Ye Y, Zhang S, Dong X. Correlation between mobile phone use and sleep quality among college students of a university in Guangzhou City. Pract Prev Med (2016) 23(4):429–33.
29. Shen C, Dai J, Zhou Y, Sheng Q, Wang Z, Cai S, et al. Influence of cell phone overuse on sleep quality among university students in Jiangsu. Chin J Sch Health (2015) 36(5):708–710, 714. doi: 10.16835/j.cnki.1000-9817.2015.05.021
30. Liao Y, Yang L, Wu C, Chai J, Mei S. The influence of cell phone dependence on sleep disorders in a university students. Chin J Sch Health (2016) 37(2):303–5. doi: 10.16835/j.cnki.1000-9817.2016.02.045
31. Yu L, Cai L. Review on the application of the University Personality Inventory in China and abroad. Prof Circle (2007) 53:158–9.
32. Zheng L, Wang J. An examination on the factor structure of a mental health screener in a sample of more than 10000 university students. J Xi'an Shiyou University: Soc Sci Edition (2007) 16(1):91–6.
33. Zhang J, Lanza S, Zhang M, Su B. Structure of the University Personality Inventory for Chinese College Students. Psychol Rep (2015) 116(3):821–39. doi: 10.2466/08.02.PR0.116k26w3
34. Su B, Zhang W. An analysis on the factor structure of the University Personality Inventory. Chin J Sch Health (2015) 36(6):920–2. doi: 10.16835/j.cnki.1000-9817.2015.06.041
35. American-Psychiatric-Association. Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: American-Psychiatric-Association (2000).
36. Xiao S. Theoretical basis and research application of Social Support Rating Scale. J Clin Psychiatry (1994) 4(2):98–100.
37. Gu W, Xu YM, Zhong BL. Health-related quality of life in Chinese inpatients with lung cancer treatedin large general hospitals: across-sectional study. BMJ Open (2018) 8(4):e019873. doi: 10.1136/bmjopen-2017-019873
38. Huang H, Niu L, Zhou C, Wu H. Reliability and Validity of Mobile Phone Addiction Index for Chinese College Students. Chin J Clin Psychol (2014) 22(5):835–8. doi: 10.16128/j.cnki.1005-3611.2014.05.062
39. Leung L. Linking Psychological Attributes to Addiction and Improper Use of the Mobile Phone among Adolescents in Hong Kong. J Children Media (2008) 2(2):93–113. doi: 10.1080/17482790802078565
40. Liu XC, tang MQ, Hu L, Wang AZ, Wu HX, Zhao GF, et al. Reliability and validility of the Pittsburgh sleep quality index. Chin J Psychiatry (1996) 29(2):103–7.
41. Buysse DJ, Reynolds CF .3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res (1989) 28(2):193–213. doi: 10.1016/0165-1781(89)90047-4
42. Zhang HS, Xu YM, Zhu JH, Zhong BL. Poor sleep quality is significantly associated with low sexual satisfaction in Chinese methadone-maintained patients. Med (Baltimore) (2017) 96(39):e8214. doi: 10.1097/MD.0000000000008214
43. CNNIC. The 44th China Statistical Report on Internet Development. Beijing: China Internet Network Information Center (2019).
44. Tao S, Wu X, Zhang Y, Zhang S, Tong S, Tao F. Effects of Sleep Quality on the Association between Problematic Mobile Phone Use and Mental Health Symptoms in Chinese College Students. Int J Environ Res Public Health (2017) 14(2):185. doi: 10.3390/ijerph14020185
45. Tran DP, Spierings EL. Headache and insomnia: their relation reviewed. Cranio (2013) 31(3):165–70. doi: 10.1179/crn.2013.026
46. Koyanagi A, Garin N, Olaya B, Ayuso-Mateos JL, Chatterji S, Leonardi M, et al. Chronic conditions and sleep problems among adults aged 50 years or over in nine countries: a multi-country study. PloS One (2014) 9(12):e114742. doi: 10.1371/journal.pone.0114742
47. Isaac F, Greenwood KM. The relationship between insomnia and depressive symptoms: genuine or artifact? Neuropsychiatr Dis Treat (2011) 7:57–63. doi: 10.2147/NDT.S16267
48. Roberts RE, Duong HT. Depression and insomnia among adolescents: a prospective perspective. J Affect Disord (2013) 148(1):66–71. doi: 10.1016/j.jad.2012.11.049
49. Finan PH, Goodin BR, Smith MT. The association of sleep and pain: an update and a path forward. J Pain (2013) 14(12):1539–52. doi: 10.1016/j.jpain.2013.08.007
50. Zhong BL, Chen SL, Tu X, Conwell Y. Loneliness and Cognitive Function in Older Adults: Findings From the Chinese Longitudinal Healthy Longevity Survey. J Gerontol B Psychol Sci Soc Sci (2017) 72(1):120–8. doi: 10.1093/geronb/gbw037
51. Tsai LL, Li SP. Sleep patterns in college students: gender and grade differences. J Psychosom Res (2004) 56(2):231–7. doi: 10.1016/S0022-3999(03)00507-5
52. Zhang B, Wing YK. Sex differences in insomnia: a meta-analysis. Sleep (2006) 29(1):85–93. doi: 10.1093/sleep/29.1.85
53. Fatima Y, Doi SA, Najman JM, Mamun AA. Exploring Gender Difference in Sleep Quality of Young Adults: Findings from a Large Population Study. Clin Med Res (2016) 14(3-4):138–44. doi: 10.3121/cmr.2016.1338
54. Madrid-Valero JJ, Martinez-Selva JM, Ribeiro do Couto B, Sanchez-Romera JF, Ordonana JR. Age and gender effects on the prevalence of poor sleep quality in the adult population. Gac Sanit (2017) 31(1):18–22. doi: 10.1016/j.gaceta.2016.05.013
55. Tang J, Liao Y, Kelly BC, Xie L, Xiang YT, Qi C, et al. Gender and Regional Differences in Sleep Quality and Insomnia: A General Population-based Study in Hunan Province of China. Sci Rep (2017) 7:43690. doi: 10.1038/srep43690
56. Ikeda K, Nakamura K. Association between mobile phone use and depressed mood in Japanese adolescents: a cross-sectional study. Environ Health Prev Med (2014) 19(3):187–93. doi: 10.1007/s12199-013-0373-3
57. Wood AW, Loughran SP, Stough C. Does evening exposure to mobile phone radiation affect subsequent melatonin production? Int J Radiat Biol (2006) 82(2):69–76. doi: 10.1080/09553000600599775
Keywords: poor sleep quality, smartphone use, mobile phone addiction, college students, association
Citation: Huang Q, Li Y, Huang S, Qi J, Shao T, Chen X, Liao Z, Lin S, Zhang X, Cai Y and Chen H (2020) Smartphone Use and Sleep Quality in Chinese College Students: A Preliminary Study. Front. Psychiatry 11:352. doi: 10.3389/fpsyt.2020.00352
Received: 03 February 2020; Accepted: 07 April 2020;
Published: 06 May 2020.
Edited by:
Yanhui Liao, Sir Run Run Shaw Hospital, ChinaReviewed by:
Bao-Liang Zhong, Wuhan Mental Health Center, ChinaCopyright © 2020 Huang, Li, Huang, Qi, Shao, Chen, Liao, Lin, Zhang, Cai and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongxian Chen, c2hlbmh4MjAxOEBjc3UuZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.