- Department of Psychiatry, Shanghai Pudong New Area Mental Health Center, Tongji University School of Medicine, Shanghai, China
Background and Aim: There are important public health issues involving rehabilitation of patients living with schizophrenia in the community. The purpose of this study was to analyze the correlations between number of previous hospitalizations, living space and quality of family function in the rehabilitation of patients living with schizophrenia in the community. The study attempts to determine the potential ways to use beneficial factors in recurrent hospitalization for improving treatment and rehabilitation efforts for patients living with long-term chronic schizophrenia.
Methods: The study included 281 rehabilitations of patients living with schizophrenia in the community. A homemade general questionnaire was used to collect information about the number of previous hospitalizations and the living space of the participants. A family assessment device was used to evaluate the quality of family function of the patients.
Results: The number of previous hospitalizations of persons living with schizophrenia in the community was negatively correlated with the quality of family function (B = 0.063), and there was no statistical difference in the number of previous hospitalizations and the quality of family function of patients in different living spaces.
Conclusions: The number of previous hospitalizations had a negative impact on family function in the rehabilitation of patients living with schizophrenia in the community. Living space may not have a significant positive effect on family function or the number of previous hospitalizations.
Introduction
The course of schizophrenia is prolonged, the cure rate is low, the relapse and disability rates are high, and long-term treatment and rehabilitation are needed (1). Ninety percent of the more than 7.8 million persons living with schizophrenia in China live in the community; these people are the main target of community rehabilitation services (2). Persons living with schizophrenia suffer from cognitive impairment and recurrent conditions, so they may be repeatedly hospitalized (3). Some studies have found that an increased number of hospitalizations for persons living with schizophrenia increased the psychological burden on relatives (4). The provision of antipsychotic drugs alone cannot meet the economic, social, and psychological needs of persons living with schizophrenia (5). Clinical researchers believe that the treatment of schizophrenia requires drugs combined with psychological interventions (6). In addition, long-term hospitalization has been shown to greatly impair the social cognitive function of patients (7). Therefore, rehabilitation of persons living with schizophrenia in the community is currently a preferable approach (8).
Studies have shown that people living in densely populated and socially disordered areas are more likely to suffer from mental illness (9). Persons living with schizophrenia who have independent housing have a better quality of life and a better social and emotional network (10). Studies have found that the number of household members and floor space can predict patients' emotional health (11).
The prognosis of persons living with schizophrenia is closely related to their family function (12). Good family function can improve patient compliance and reduce the relapse rate (13). Persons living with schizophrenia have poor family function, insufficient social support, and less communication between family members (14). The family function of persons living with schizophrenia plays an important role in their rehabilitation (15). Good family function can reduce the relapse rate and improve the prognosis of schizophrenia (16). Additionally, family function has a positive regulatory effect on medication compliance in persons living with schizophrenia (17).
Repeated hospitalizations for persons living with schizophrenia will increase the patient's economic and psychological burden and will also increase the cost of government medical insurance (18). The present study analyzed the correlations between the number of hospitalizations of patients rehabilitating in the community, living space, and family function and provided a theoretical basis for reducing the hospitalization rate of persons living with schizophrenia.
Methods
Design and Procedures
A cross-sectional study was performed. The study included 281 rehabilitations of patients living with schizophrenia in the community. All participants were from community rehabilitation institutions under the Shanghai Pudong New Area Mental Health Center. The study lasted from May 2018 to August 2018, and sample evaluations were performed by professional clinical researchers.
Participants
The sample was originally recruited from persons living with schizophrenia in the community rehabilitation facility of the Shanghai Pudong New Area Mental Health Center. The following were the inclusion criteria: (1) met the diagnostic criteria for schizophrenia in the Tenth Edition of the International Statistical Classification of Diseases and Related Health Problems; (2) aged between 18 and 65; (3) were male or female; (4) had no history of head trauma, obvious intellectual disability, or other serious or uncontrolled stable physical illness; (5) had no current use (within the previous 3 months) of alcohol or drugs or a past history of dependence; and (6) had no obvious hallucinations or complaints.
Measures
A homemade questionnaire collected data on the number of previous hospitalizations and the personal living space of the patients. The number of previous hospitalizations was the number of times a patient was hospitalized in a psychiatric hospital from the first onset of schizophrenia and referred to the patient case for proofreading. According to Chinese traditional culture and customs, people with mental disorders usually live with their families. The personal living space was calculated as the total area of the patient's current house divided by the number of occupants.
Family Assessment Device
The family assessment device used in this study was a self-report scale that assessed family members' perceptions of family function (19). Previous studies have shown that these family assessment scales have good reliability and validity in the clinic (20). The total score for all items on the scale was the scale score (21). The higher the score was, the better the family structure and function (22). In most clinical studies, this score has a good degree of discrimination (23). Some studies have found that family assessment devices have good adaptability and sensitivity in mainland China (24).
Statistical Analysis
All results are expressed as the mean ± standard deviation. Statistical analysis was performed using the SPSS 21.0 (SPSS, Chicago, IL, USA) software package. Measurement data that met the normal distribution were compared using independent sample t-tests, rank-sum tests were used for data noncompliant with the normal distribution, and one-way ANOVA was used to compare multiple groups. Regression analysis was used to describe the correlations between variables. Statistical correlations between variables in the regression model were determined with p < 0.0001.
Results
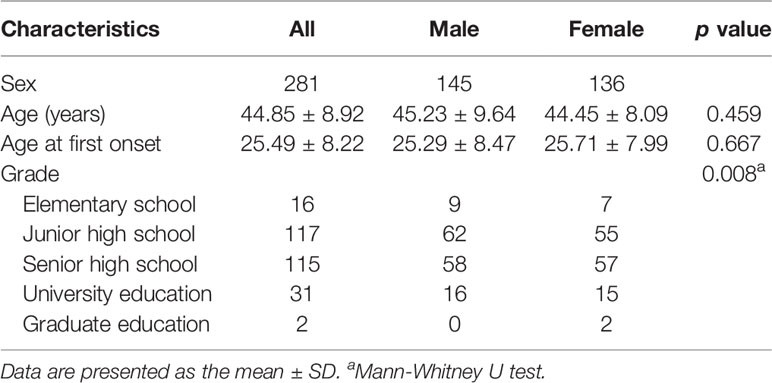
Table 1 is mainly a comparative study of the differences in sex, age, age at onset, and education. The patients of different sexes had significant differences in education (p < 0.01). There were no significant differences in the age at onset between males and females.
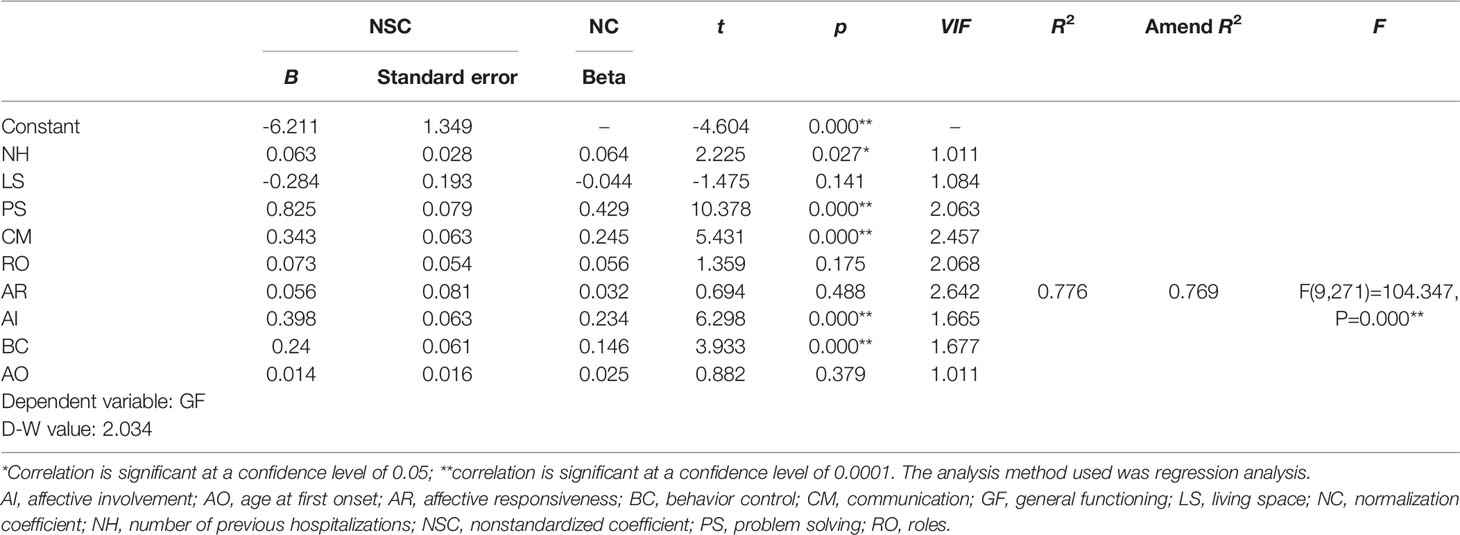
Table 2 shows that the number of previous hospitalizations, problem solving, communication, affective involvement, and behavior control had significant positive impacts on the general functioning score. However, living space, roles, affective responsiveness, and age at first onset did not affect general functioning.
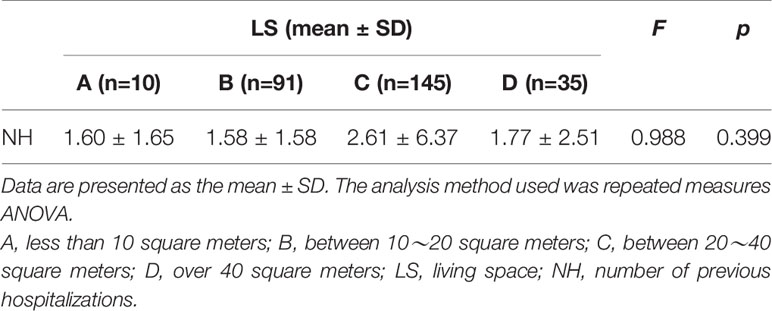
According to the analysis results provided in Table 3, there were no significant differences in the number of hospitalizations for persons living with schizophrenia in community rehabilitation based on different living spaces.
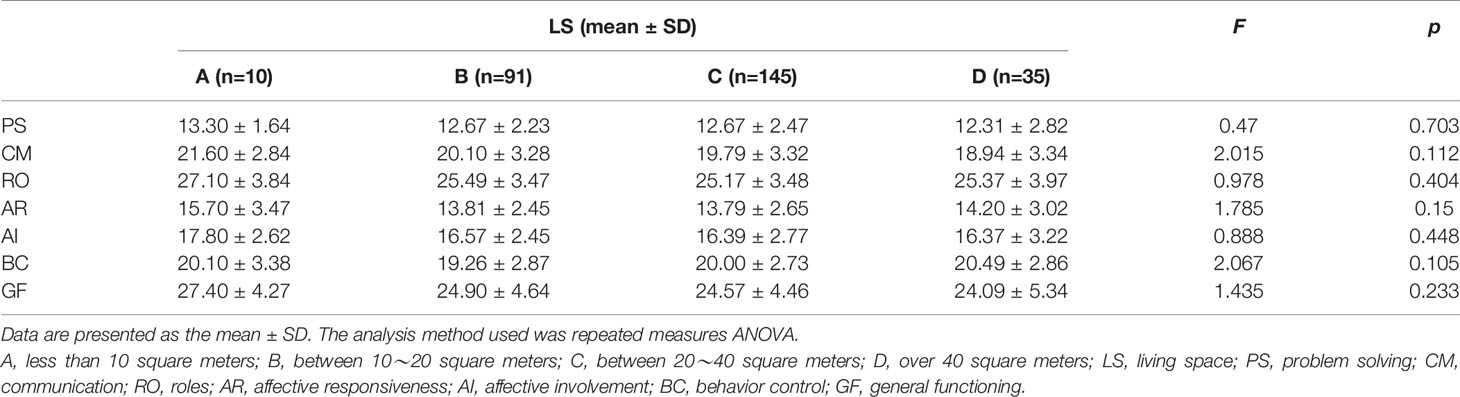
The analysis of variance results in Table 4 show that there was no statistically significant difference in family function among persons living with schizophrenia based on different living spaces, and there were no significant differences within each factor entry.
Discussion
This study mainly explored the correlations between the number of previous hospitalizations for rehabilitation of patients living with schizophrenia in the community and living space and family function. The study included 281 patients. The difference in educational level between persons living with schizophrenia of different sexes was significant. Sociological surveys have shown that the educational level of women in Shanghai, China, is higher than that of men (25). More than 70% of Shanghai women have a college education or above, and 11.1% of Shanghai women have a graduate education (26). Studies have found that males living with schizophrenia have more cognitive impairments in reasoning and problem solving, social cognition, processing speed, and working memory than females living with schizophrenia (27). The ovarian hormones progesterone and estrogen have good neurotrophic and neuroprotective effects and support reproductive function and cognitive health (28). Estrogen promotes higher cognitive functions by acting in brain regions such as the prefrontal cortex and the hippocampus (29). Therefore, women living with schizophrenia are more likely to continue their education than males with schizophrenia.
The family function behavior control scores were positively related to living space, showing that the larger the living space was, the lower was the behavior control mode. Patients living with schizophrenia in the community who are being rehabilitated have large emotional fluctuations and are prone to have negative emotions (30). Most persons living with schizophrenia cope with problems in a negative and evasive manner (31). Additionally, most persons living with schizophrenia have mild loneliness, and previous research has suggested that solitude makes people feel lonely (32). Therefore, subjects with a large living space may have a single problem-solving mode. The above results indicate that improvements in patient living space alone may not have a significant positive effect on improvements in family function.
There was an inverse correlation between the number of previous hospitalizations for persons living with schizophrenia and family function, such that as the number of previous hospitalizations increased, family function decreased. Previous studies have found that persons living with schizophrenia who were repeatedly hospitalized increased the burden on their families (33). Despite a better public understanding of schizophrenia in recent years, schizophrenia is still widely regarded as shameful for the patients' families and by the Chinese public (34, 35). With the increase in the number of hospitalizations, the stigma around the patients and their families will strengthen (36, 37). The above research results show that the number of previous hospitalizations for rehabilitation of patients living with schizophrenia in the community has a negative effect on family function. This study found that the roles and effective responsiveness scores for the rehabilitation of patients living with schizophrenia in the community were not related to general functioning and may be related to the clinical symptoms of schizophrenia (38, 39).
Shanghai's per capita living space is 36.7 square meters; approximately half of the patients in this study live below the Shanghai average (40). Table 4 shows that there were no statistically significant differences in the number of previous hospitalizations and family function of the patients based on different living spaces, further indicating that good living spaces had no significant positive effect on the rehabilitation of patients with schizophrenia in the community.
In summary, our study found that the number of previous hospitalizations of persons living with schizophrenia in the community has a negative impact on quality of family function and that there is no statistical difference in the number of previous hospitalizations and quality of family function of patients in different living spaces.
Data Availability Statement
All datasets generated for this study are included in the article/Supplementary Material.
Ethics Statement
The studies involving human participants were reviewed and approved by the Shanghai Pudong New Area Mental Health Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
HQ and XZ contributed to the conception and design of the present study. HQ recruited the patients and conducted the study. XF and BZ undertook the statistical analyses and wrote the first manuscript draft. All authors contributed to the data analysis and drafting and revision of the article, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Funding
This study was supported by the Shanghai Pudong Municipal Health Commission (PWRd 2017-05 and PWYgy2018-10) and the Shanghai Municipal Health Commission (201840372).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.00215/full#supplementary-material
References
1. De Picker LJ, Morrens M, Chance SA, Boche D. Microglia and brain plasticity in acute psychosis and schizophrenia illness course: a meta-review. Front Psychiatry (2017) 8:238. doi: 10.3389/fpsyt.2017.00238
2. Yeh Y-C, Yu X, Zhang C, Hao W, Du F, Liu D, et al. Literature review and economic evaluation of oral and intramuscular ziprasidone treatment among patients with schizophrenia in China. Gen Psychiatry (2018) 31(3):e100016. doi: 10.1136/gpsych-2018-100016
3. Gatov E, Rosella L, Chiu M, Kurdyak PA. Trends in standardized mortality among individuals with schizophrenia, 1993–2012: a population-based, repeated cross-sectional study. Cmaj (2017) 189(37):E1177–87. doi: 10.1503/cmaj.161351
4. Koutra K, Simos P, Triliva S, Lionis C, Vgontzas AN. Linking family cohesion and flexibility with expressed emotion, family burden and psychological distress in caregivers of patients with psychosis: A path analytic model. Psychiatry Res (2016) 240:66–75. doi: 10.1016/j.psychres.2016.04.017
5. Asher L, Patel V, De Silva MJ. Community-based psychosocial interventions for people with schizophrenia in low and middle-income countries: systematic review and meta-analysis. BMC Psychiatry (2017) 17(1):355. doi: 10.1186/s12888-017-1516-7
6. Patel V, Dan C, Parikh R, Charlson FJ, Whiteford H. Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities, 3rd edition. Lancet (2015) 387(10028):1672–85. doi: 10.1016/S0140-6736(15)00390-6
7. Fleischhacker WW, Arango C, Arteel P, Barnes TRE, Carpenter W, Duckworth K, et al. Schizophrenia - Time to Commit to Policy Change. Schizophr Bull (2014) 40 Suppl 3: (Suppl 3):S165–S94. doi: 10.1093/schbul/sbu006
8. Parker S, Hopkins G, Siskind D, Harris M, McKeon G, Dark F, et al. A systematic review of service models and evidence relating to the clinically operated community-based residential mental health rehabilitation for adults with severe and persisting mental illness in Australia. BMC Psychiatry (2019) 19(1):55. doi: 10.1186/s12888-019-2019-5
9. Segal SP, Baumohl J, Johnson E. Falling through the cracks: Mental disorder and social margin in a young vagrant population. Soc Problems (1977) 24(3):387–400. doi: 10.1525/sp.1977.24.3.03a00100
10. Hansson L, Middelboe T, Sørgaard K, Bengtsson-Tops A, Bjarnason O, Merinder L, et al. Living situation, subjective quality of life and social network among individuals with schizophrenia living in community settings. Acta Psychiatrica Scand (2002) 106(5):343–50. doi: 10.1034/j.1600-0447.2002.02346.x
11. Dunham A, Kinnear D, Allan L, Smiley E, Cooper SA. The relationship between physical ill-health and mental ill-health in adults with intellectual disabilities. J Intellectual Disability Res (2018) 62(5):444–53. doi: 10.1111/jir.12483
12. Wynn JK, Sugar C, Horan WP, Kern R, Green MF. Mismatch negativity, social cognition, and functioning in schizophrenia patients. Biol Psychiatry (2010) 67(10):940–7. doi: 10.1016/j.biopsych.2009.11.024
13. Rummel-Kluge C, Kissling W. Psychoeducation for patients with schizophrenia and their families. Expert Rev Neurother (2008) 8(7):1067–77. doi: 10.1586/14737175.8.7.1067
14. Raj EA, Shiri S, Jangam KV. Subjective burden, psychological distress, and perceived social support among caregivers of persons with schizophrenia. Indian J Soc Psychiatry (2016) 32(1):42. doi: 10.4103/0971-9962.176767
15. Podogrodzka-Niell M, Tyszkowska M. Stigmatization on the way to recovery in mental illness–the factors associated with social functioning. Psychiatr Pol (2014) 48(6):1201–11. doi: 10.12740/PP/20364
16. Onwumere J, Grice S, Kuipers E. Delivering cognitive-behavioural family interventions for schizophrenia. Aust Psychol (2016) 51(1):52–61. doi: 10.1111/ap.12179
17. Yang J, Ko Y-H, Paik J-W, Lee M-S, Han C, Joe S-H, et al. Symptom severity and attitudes toward medication: impacts on adherence in outpatients with schizophrenia. Schizophr Res (2012) 134(2-3):226–31. doi: 10.1016/j.schres.2011.11.008
18. Awad AG, Voruganti LN. The burden of schizophrenia on caregivers. Pharmacoeconomics (2008) 26(2):149–62. doi: 10.2165/00019053-200826020-00005
19. Sawant NS, Jethwani KS. Understanding family functioning and social support in unremitting schizophrenia: A study in India. Indian J Psychiatry (2010) 52(2):145. doi: 10.4103/0019-5545.64593
20. Byles J, Byrne C, Boyle MH, Offord DR. Ontario Child Health Study: reliability and validity of the general functioning subscale of the McMaster Family Assessment Device. Family Process (1988) 27(1):97–104. doi: 10.1111/j.1545-5300.1988.00097.x
21. Boterhoven de Haan KL, Hafekost J, Lawrence D, Sawyer MG, Zubrick SR. Reliability and validity of a short version of the general functioning subscale of the McMaster Family Assessment Device. Family Process (2015) 54(1):116–23. doi: 10.1111/famp.12113
22. Barney M, Max J. The McMaster family assessment device and clinical rating scale: Questionnaire vs interview in childhood traumatic brain injury. Brain Inj (2005) 19(10):801–9. doi: 10.1080/02699050400024961
23. Staccini L, Tomba E, Grandi S, Keitner GI. The evaluation of family functioning by the family assessment device: A systematic review of studies in adult clinical populations. Family Process (2015) 54(1):94–115. doi: 10.1111/famp.12098
24. Du N, Ran M-S, Liang S, SiTu M, Huang Y, Mansfield AK, et al. Comparison of family functioning in families of depressed patients and nonclinical control families in China using the Family Assessment Device and the Family Adaptability and Cohesion Evaluation Scales II. Ann Clin Psychiatry (2014) 26(1):47–56.
25. Li YH, Song GX, Yan Y, De Ding Z, Zhang HW. Study on age and education level and their relationship with fall-related injuries in Shanghai, China. Biomed Environ Sci (2013) 26(2):79–86. doi: 10.3967/0895-3988.2013.02.001
26. Chen Y, Geng W. Impact factors of marital satisfaction from female perspective:a Shanghai report. Shanghai Arch Psychiatry (2010) 22(z1):413–5.
27. Fanning JR, Bell MD, Fiszdon JM. Is it possible to have impaired neurocognition but good social cognition in schizophrenia? Schizophr Res (2012) 135(1-3):68–71. doi: 10.1016/j.schres.2011.12.009
28. Azcoitia I, Arevalo M-A, De Nicola AF, Garcia-Segura LM. Neuroprotective actions of estradiol revisited. Trends Endocrinol Metab (2011) 22(12):467–73. doi: 10.1016/j.tem.2011.08.002
29. Luine V, Frankfurt M. Interactions between estradiol, BDNF and dendritic spines in promoting memory. Neuroscience (2013) 239:34–45. doi: 10.1016/j.neuroscience.2012.10.019
30. Ventura J, Subotnik KL, Gitlin MJ, Gretchen-Doorly D, Ered A, Villa KF, et al. Negative symptoms and functioning during the first year after a recent onset of schizophrenia and 8 years later. Schizophr Res (2015) 161(2-3):407–13. doi: 10.1016/j.schres.2014.10.043
31. Deserno L, Heinz A, Schlagenhauf F. Computational approaches to schizophrenia: A perspective on negative symptoms. Schizophr Res (2017) 186:46–54. doi: 10.1016/j.schres.2016.10.004
32. Ludwig KA, Nye LN, Simmons GL, Jarskog LF, Pinkham AE, Harvey PD, et al. Correlates of loneliness among persons with psychotic disorders. Soc Psychiatry Psychiatr Epidemiol (2019). 10(3):1–11. doi: 10.1007/s00127-019-01789-5
33. Fallahi Khoshknab M, Sheikhona M, Rahgouy A, Rahgozar M, Sodagari F. The effects of group psychoeducational programme on family burden in caregivers of I ranian patients with schizophrenia. J Psychiatr Ment Health Nurs (2014) 21(5):438–46. doi: 10.1111/jpm.12107
34. Chen L, Zhao Y, Tang J, Jin G, Liu Y, Zhao X, et al. The burden, support and needs of primary family caregivers of people experiencing schizophrenia in Beijing communities: a qualitative study. BMC Psychiatry (2019) 19(1):75. doi: 10.1186/s12888-019-2052-4
35. Guan Z, Huang C, Wiley JA, Sun M, Bai X, Tang S. Internalized stigma and its correlates among family caregivers of patients diagnosed with schizophrenia in Changsha, Hunan, China. J Psychiatr Ment Health Nurs (2019). doi: 10.1111/jpm.12571
36. Yıldırım A, Hacıhasanoğlu Aşılar R, Camcıoğlu TH, Erdiman S, Karaağaç E. Effect of psychosocial skills training on disease symptoms, insight, internalized stigmatization, and social functioning in patients with schizophrenia. Rehabil Nurs (2015) 40(6):341–8. doi: 10.1002/rnj.195
37. Roberts LW, Bandstra BS. Addressing stigma to strengthen psychiatric education. (2012). Acad Psychiatry 36(5):347–50. In: Citeseer,. doi: 10.1176/appi.ap.12060118
38. Martin AK, Gibson EC, Mowry B, Robinson GA. Verbal initiation, suppression, and strategy use and the relationship with clinical symptoms in schizophrenia. J Int Neuropsychol Soc (2016) 22(7):735–43. doi: 10.1017/S1355617716000552
39. Yip K-S. The importance of subjective psychotic experiences: Implications on psychiatric rehabilitation of people with schizophrenia. Psychiatr Rehabil J (2004) 28(1):48. doi: 10.2975/28.2004.48.54
Keywords: previous hospitalizations, current living space, quality of family function, persons living with schizophrenia, community
Citation: Fan X, Zhao X, Zhu B and Qin H (2020) Retrospective Evaluation of the Correlation Between Previous Hospitalizations, the Type of Current Living Space, and Quality of Family Function. Front. Psychiatry 11:215. doi: 10.3389/fpsyt.2020.00215
Received: 30 December 2019; Accepted: 04 March 2020;
Published: 17 March 2020.
Edited by:
Helen Killaspy, University College London, United KingdomReviewed by:
Emilio Baliki Liociri Ovuga, Gulu University, UgandaFrances Louise Dark, Metro South Addiction and Mental Health Services, Australia
Copyright © 2020 Fan, Zhao, Zhu and Qin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongyun Qin, cWluaG9uZ3l1bjA3QDE2My5jb20=
 Xiwang Fan
Xiwang Fan Bingen Zhu
Bingen Zhu Hongyun Qin
Hongyun Qin