- 1Unit of Psychiatry, Institute of Translational Medicine, Faculty of Health Sciences, University of Macau, Macau, China
- 2Center for Cognition and Brain Sciences, University of Macau, Macau, China
- 3Department of Psychiatry, Southern Medical University Nanfang Hospital, Guangdong-Hong Kong-Macao Greater Bay Area Center for Brain Science and Brain-Inspired Intelligence, Guangdong, China
- 4Department of Social Medicine and Health Management, School of Public Health, Jilin University, Changchun, China
- 5The National Clinical Research Center for Mental Disorders & Beijing Key Laboratory of Mental Disorders, Beijing Anding Hospital & the Advanced Innovation Center for Human Brain Protection, Capital Medical University, Beijing, China
- 6Global and Community Mental Health Research Group, Department of Psychology, University of Macau, Macau, China
- 7Division of Psychiatry, School of Medicine, University of Western Australia, Perth, WA, Australia
- 8The University of Notre Dame Australia, Fremantle, WA, Australia
Background: Sleep disturbance is common in perinatal and postnatal women, but the epidemiology of sleep problems is highly variable in these populations. This was a meta-analysis that examined the prevalence of poor sleep quality and its correlates among perinatal and postnatal women.
Methods: A systematic search of both international and Chinese databases (PubMed, EMBASE, PsycINFO, Web of Science, CNKI, and Wangfang) was performed. Studies with data on sleep quality measured by the Pittsburgh Sleep Quality Index (PSQI) were included.
Results: Forty-two studies were included for analyses. The prevalence of poor sleep quality was 54.2% (95% CI: 47.9–60.5%) in perinatal and postnatal women, with 44.5% (95% CI: 37.6–51.6%) in perinatal women and 67.2% (95% CI: 57.6–75.5%) in postnatal women. The pooled total PSQI score was 7.54 ± 0.40 (95% CI: 6.75–8.33), while the average PSQI component scores varied from 0.13 ± 0.04 for use of sleeping medication to 1.51 ± 0.17 for habitual sleep efficiency. Maternal age, study site, survey year, comorbidity, PSQI cut-off value, and quality assessment score had significant moderating effects on the prevalence of poor sleep quality.
Conclusion: Given the negative impact of poor sleep quality on health outcomes and well-being, regular screening for poor sleep quality and effective interventions should be conducted for this population.
Introduction
The perinatal and the postpartum period are critical time-windows for women because of the changes in their physiology, social situation, and psychological well-being, all of which influences sleep quality (1). Sleep problems, such as poor sleep quality and sleep disturbance, often occur in perinatal and postnatal women. For instance, 14–76% of expectant mothers experience clinically significant insomnia symptoms (2, 3), while the figure increases up to 87.5% in postpartum women (4). The wide- ranging prevalence across studies are partly due to different sample demographic characteristics, sampling methods, and assessment tools. In addition, the definition of the perinatal period is inconsistent, which leads to bias due to exposure misclassification. It usually refers to the period before and after delivery, which usually begins at the 20th to 28th week of gestation and ends 1 to 4 weeks after childbirth (5). Some researchers even classify the perinatal period as the whole pregnancy and 1 year postpartum (6). In China, perinatal time is defined as the period that starts at the 28th week of pregnancy and ends 1 week after delivery (7).
Women experience changes in sleep patterns and increased levels of tiredness after childbirth (8). For example, postnatal women usually sleep less and worse during the early days following child delivery than during pregnancy and/or other time periods of reproductive age (9). Consequently, after delivery, women often reported more daytime napping, decreased total sleep time, and poorer sleep efficiency compared with late pregnancy (10), all of which affects sleep quality. In addition, some demographic and clinical characteristics are significantly associated with poor sleep quality (11, 12). For perinatal women, advanced maternal age, fluid retention, anemia, discomfort (e.g., uncomfortable sleeping positions), and body pain, as well as mood disturbance (e.g., depressive symptoms), were correlates of sleep disturbances and quality (13–15). As for postnatal new mothers, family/social support, postpartum stress, demands from the infant (i.e., nighttime feeding and care), physical changes, and bed sharing/sleeping with the infant affects sleep quality (16–18). In addition, parity was another potential factor, as multipara women usually have less efficient sleep than nulliparas women from prepregnancy until 3 months postpartum (19). Moreover, compared to vaginal deliveries, caesarean sections were associated with poorer sleep quality and more frequent nighttime awakenings (20). Poor sleep quality could lead to negative physical and mental health outcomes (21). For example, poor sleep quality in pregnancy may increase the chances of preterm birth and longer labor (22, 23) and increase the risk of depression and suicidal ideation during pregnancy and the postnatal period (6, 24).
In order to allocate health resources and reduce the negative impact of poor sleep quality on health outcomes, it is important to understand its pattern and associated factors. Some studies have examined the prevalence of poor sleep quality, but the findings were mixed. Sedov et al. (1) conducted a meta-analysis of sleep quality during pregnancy and found that 45.7% of pregnant women experienced poor sleep quality and gestational age was a moderating factor. However, postpartum women were excluded, and only English databases were searched, restricting the generalizability of the findings.
Sleep quality, defined as an individual's subjective perception about his or her sleep (25), could be measured by both objective [e.g., polysomnography (PSG) and actigraphy (25)] and subjective methods [e.g., sleep diary and standardized instruments, such as the Pittsburgh Sleep Quality Index (PSQI)]. The PSQI is a widely used questionnaire on sleep quality in the past month (26). It has been translated and validated in many populations, such as in Chinese (27), Japanese (28), Korean (29), French (30), Kurdish (31), Portuguese (32), Serbian (33), Hungarian (34), and Persian (35). The psychometric properties of the PSQI–Chinese version is satisfactory, with the Cronbach's alpha of 0.734 (27). The PSQI total score ranges from 0 to 21, with higher scores indicating poorer sleep quality. The most commonly used cut-off value for poor sleep quality is 5 (26).
Study aim
The aim of this meta-analysis was to examine the prevalence of poor sleep quality in perinatal and postpartum women and investigate its associated moderators. Following previous meta-analysis and empirical studies (1, 36, 37), associated moderators of poor sleep quality in perinatal and postpartum women were preidentified. In order to reduce heterogeneity caused by different measures, only studies using PSQI were included.
Methods
Literature Search
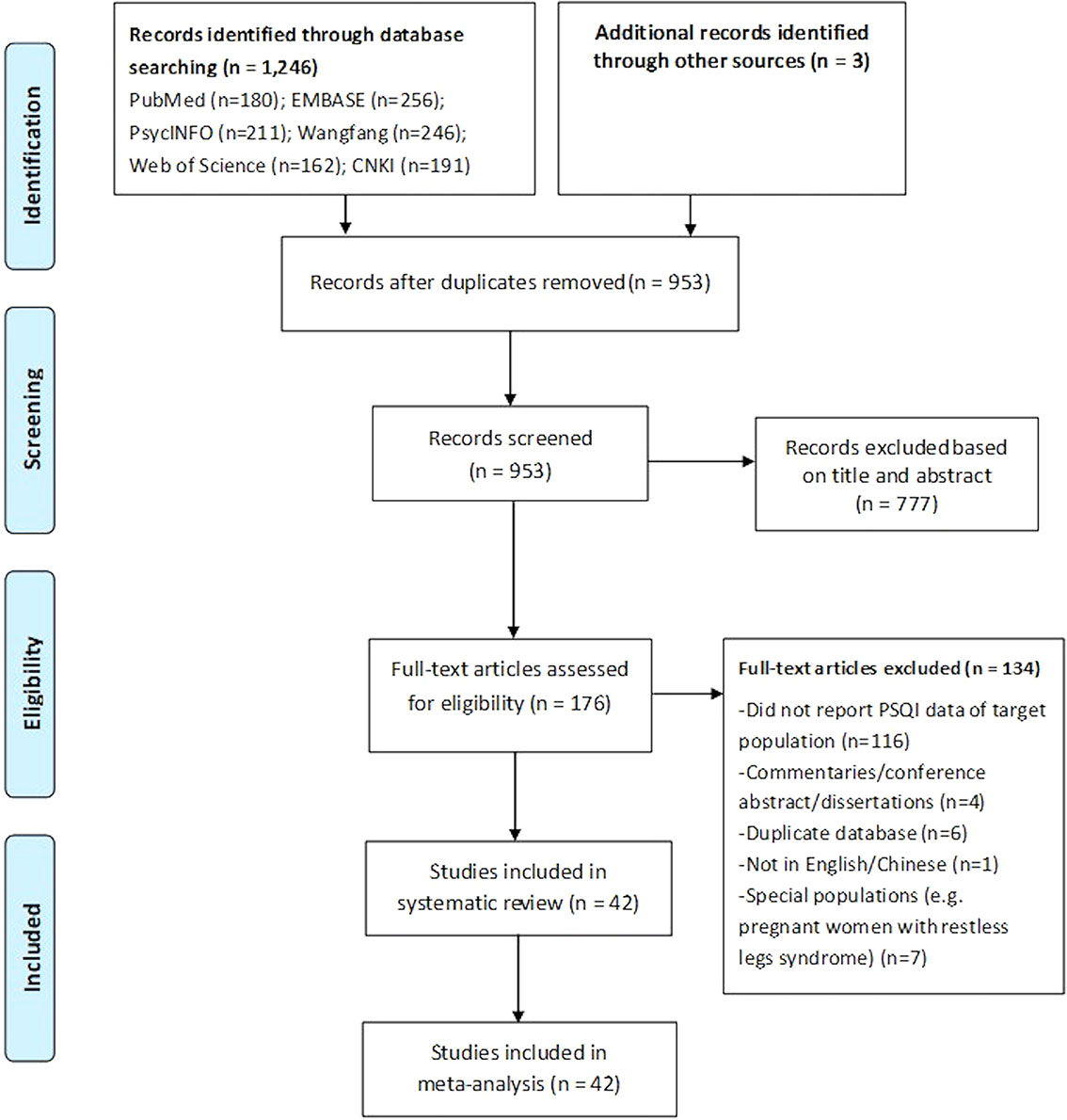
This meta-analysis was conducted according to the guidance of the preferred reporting items for systematic reviews and meta-analyses (PRISMA). Three investigators (YY, WL, TJM) independently and systematically conducted a literature search in PubMed, EMBASE, PsycINFO, Web of Science, CNKI, and Wangfang from their inception dates until 28th March 2019, using the following search words: (postpartum, postnatal, perinatal, maternal, Pittsburgh Sleep Quality Index, and PSQI. The PROSPERO registration number of this study is: CRD42019139366.
Study Criteria
Following previous studies (38, 39), the perinatal period was defined as occurring from the 28th week of gestation to 1 week postnatal, and the postpartum period was defined as occurring from the 2nd week postnatal to 1 year. Original studies that fulfilled the following criteria were included: (1) papers published in English or Chinese; (2) cross-sectional, longitudinal, or cohort studies (only baseline data of cohort studies were extracted); (3) focusing on perinatal and/or postpartum women; (4) reporting data on sleep quality as measured by PSQI; (5) having data on PSQI score or the prevalence of poor sleep quality, or relevant data that could generate the prevalence of poor sleep quality. Articles including perinatal and/or postpartum women with severe sleep problems, such as restless legs syndrome (RLS) or obstructive sleep apnea (OSA), were excluded as their inclusion may lead to significant selection bias and an overestimation of the prevalence of poor sleep quality.
Data Extraction and Quality Assessment
After duplicates were removed, the same three investigators independently screened all titles and abstracts of relevant publications and then reviewed all full texts for eligibility. Relevant data were extracted using a standardized data collection sheet, such as the first author, publication year, study design, location, sample size, mean age, depressive/anxiety status, comorbidities, PSQI cut-off value, PSQI score, and prevalence of poor sleep quality. Any disagreement was discussed and resolved by a consultation with a senior investigator (YTX).
Quality assessment was conducted by the same three authors independently using Parker's quality evaluation tool for epidemiological studies (40), with six domains: definition of the target population, representativeness of the study sample, sampling method, response rate, definition of the target symptom or diagnosis, and validation of the assessment instrument.
Statistical Analyses
Comprehensive Meta-Analysis Program 2.0 (CMA 2.0, http://www.meta-analysis.com/) was used to analyze data. Considering various sampling methods and sample size across studies, the random-effects model was utilized in all analyses. Heterogeneity was tested by the Q and I2 statistics (an I2 of > 50% or a P value of < 0.10 was considered as significant heterogeneity) (41). In order to explore potential sources of heterogeneity, we conducted subgroup, meta-regression, and sensitivity analyses according to the following variables (42): continent, study site (multicenter vs. single site), hospital type (general vs. specialized), publication year (categorized by median splitting method), PSQI cut-off, maternal age, survey year, and quality assessment score. Publication bias was assessed using funnel plot and the Begg's regression model (43). Statistical significance in this study was set at P < 0.05 (two-tailed).
Results
Literature Search and Study Characteristics
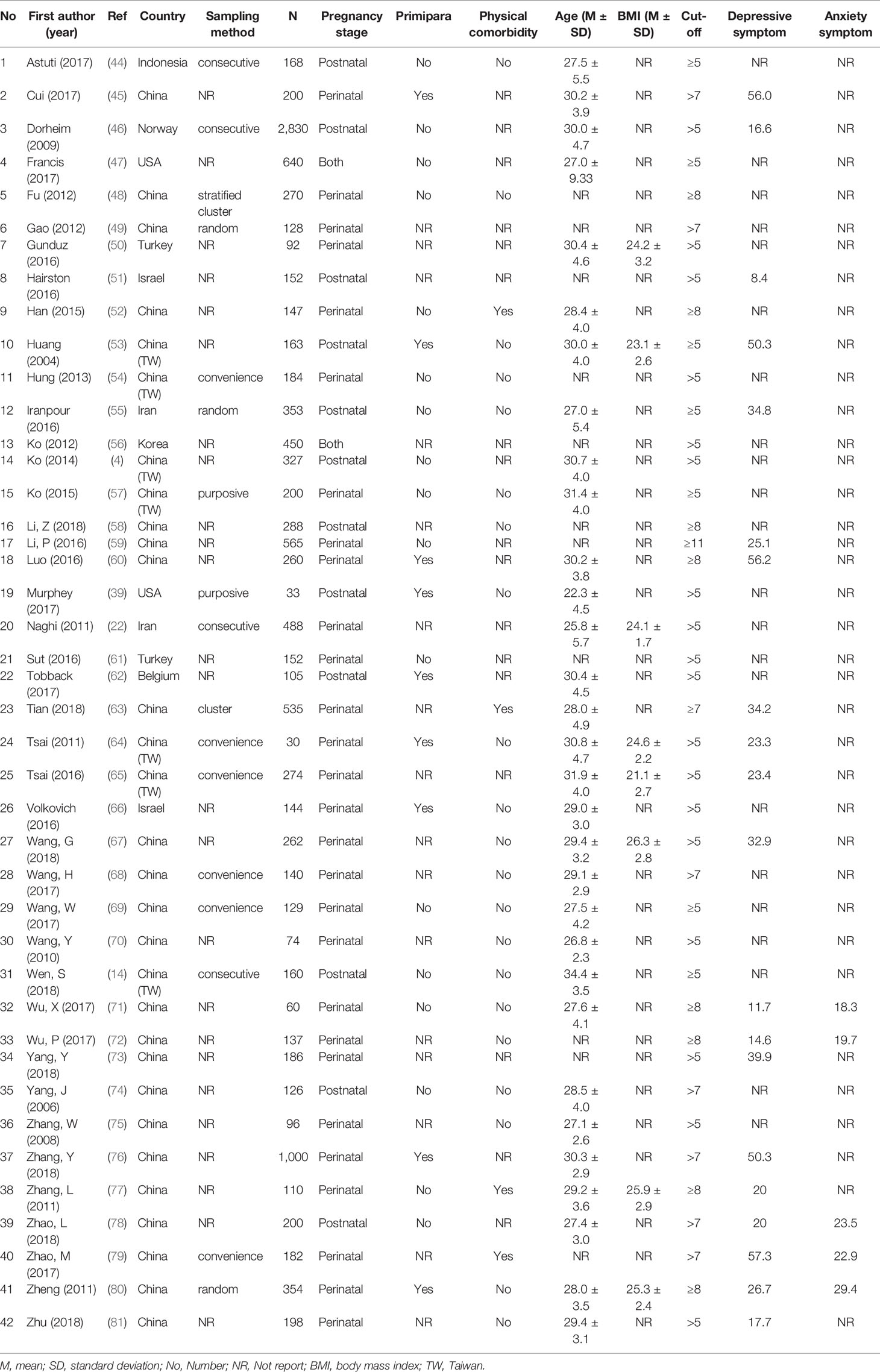
The PRISMA flowchart of literature search and selection is shown in Figure 1. Altogether, 1,249 relevant articles were identified. Of them, 777 were excluded by reviewing titles and abstracts. After full texts were read for eligibility, 42 studies covering 12,592 individuals were included for analyses. Of them, 28 studies reported prevalence of poor sleep quality in perinatal women, 12 reported data in postnatal women, and 2 studies included both the populations. Table 1 displays the characteristics of the included studies. The total sample size varied from 30 to 2,830. Most of the studies were conducted in Asia (n = 36), followed by Europe (n = 4), and North America (n = 2). More than half (n = 23) of the studies were conducted in one study site, and half (n = 21) recruited patients without physical comorbidities (i.e., pregnancy hypertension, heart disease, or diabetes). Twenty studies reported data of depressive symptoms, and five reported percentage of anxiety symptoms. Seven studies utilized the Center for Epidemiologic Studies Depression Scale (CES-D) to assess participant's depressive symptoms, seven used Edinburgh Postnatal Depression Scale (EPDS), four used Self-Rating Depression Scale (SDS), while the remaining two used Hospital Anxiety and Depression Scale (HADS). Regarding anxiety symptoms, three studies utilized the Self-Rating Anxiety Scale (SAS), and two used HADS. The percentage of participants with depressive symptoms ranged from 8.4 to 57.3%, while the corresponding figure for anxiety symptoms ranged from 18.3 to 29.4%.
Prevalence of Poor Sleep Quality in Perinatal and Postnatal Women
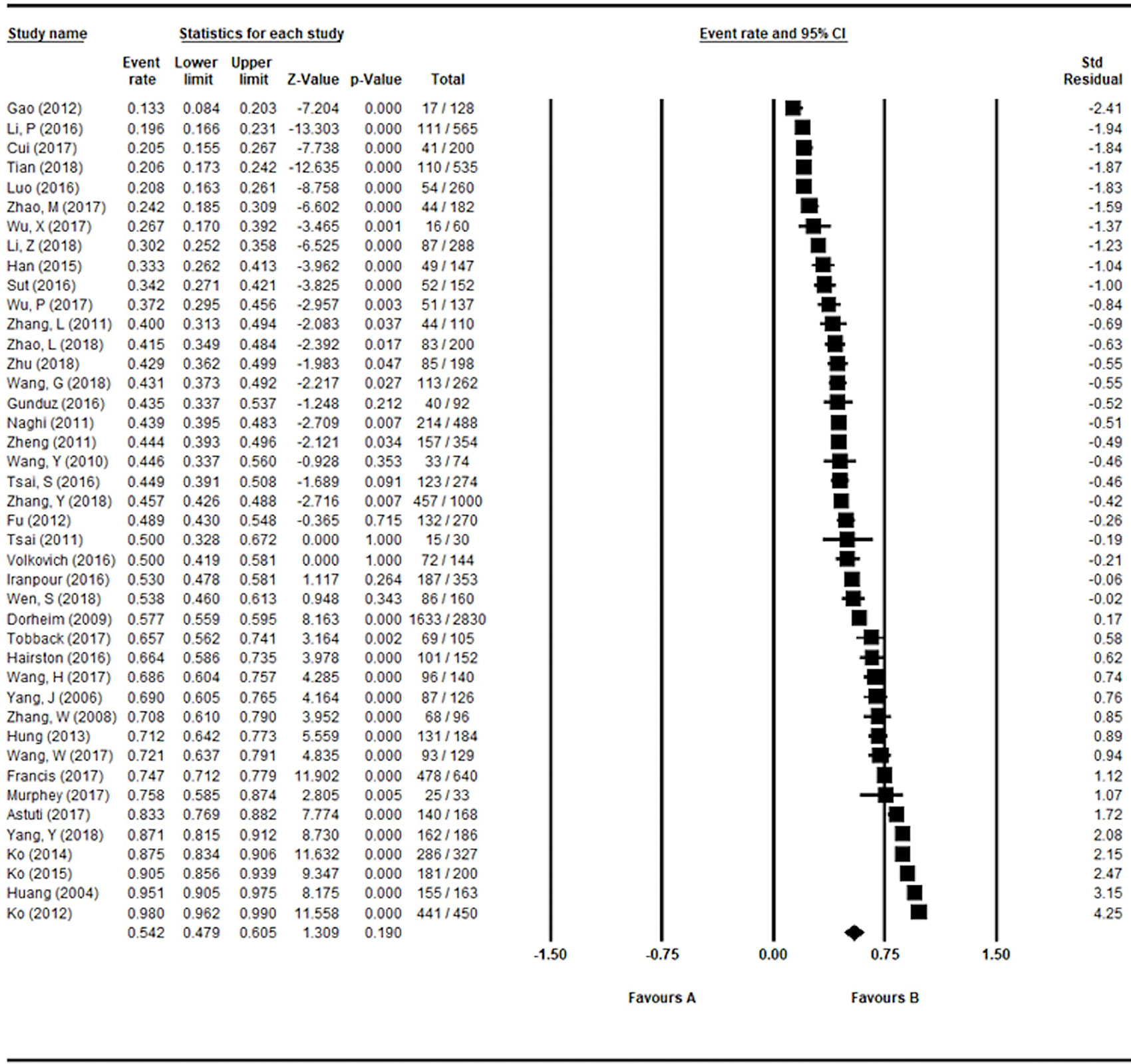
The pooled prevalence of poor sleep quality based on the 42 studies was 54.2% (95% CI: 47.9–60.5%; I2: 97.5%) as shown in Figure 2, while the corresponding figure was 44.5% (95% CI: 37.6–51.6%; I2: 96.4%) in perinatal women and 67.2% (95% CI: 57.6–75.5%; I2: 96.5%) in postnatal women.
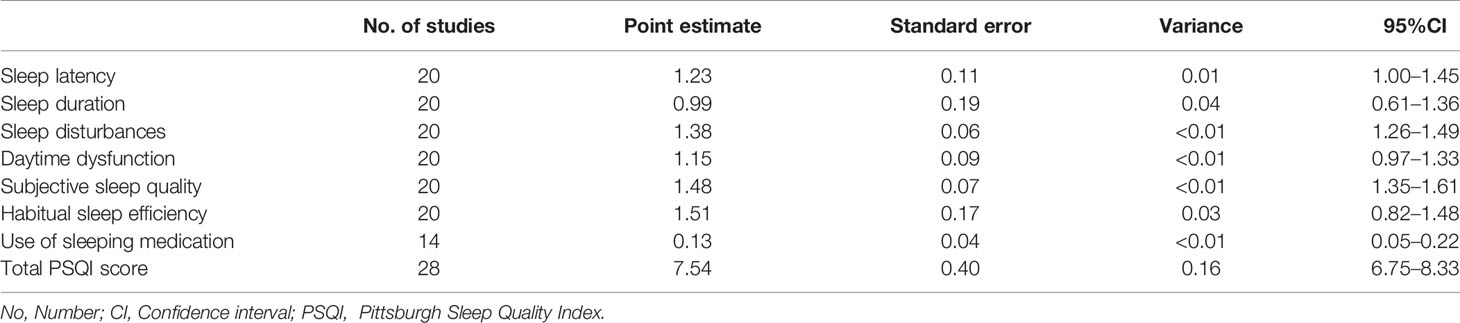
The Pooled PSQI Global and Component Score
Based on the 28 studies with available data on total PSQI score and the 20 studies with PSQI component scores, the pooled PSQI total score was 7.54 ± 0.40 (95% CI of mean score: 6.75–8.33), while the average component scores of PSQI varied from 0.13 ± 0.04 (95% CI of mean score: 0.05–0.22) for use of sleeping medication to 1.51 ± 0.17 (95% CI of mean score: 0.82–1.48) for habitual sleep efficiency (Table 2).
Subgroup and Meta-regression Analyses
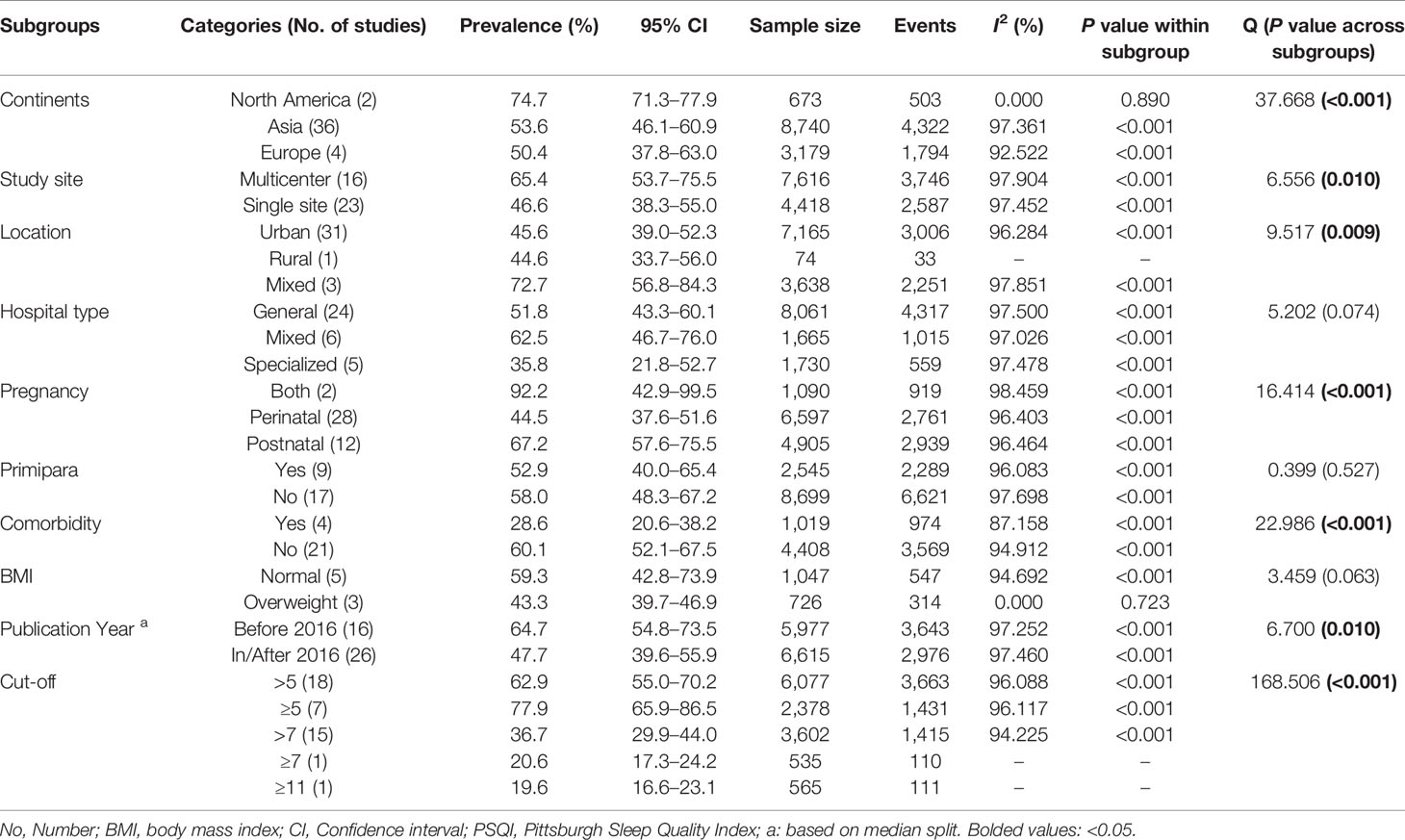
The results of subgroup analyses are presented in Table 3. Postnatal women reported higher poor sleep prevalence than perinatal women (67.2% and 44.5%, respectively, P < 0.001). People in North America reported the highest prevalence of poor sleep quality (74.7%), followed by Asia (53.6%) and Europe (50.4%, P < 0.001). Studies using multicenter design showed significantly higher prevalence than those using a single site design (65.4% and 46.6%, respectively, P = 0.01). Individuals with physical comorbidities reported lower prevalence of poor sleep quality than those without (28.6% and 60.1%, respectively, P < 0.001). In addition, studies published before the year of 2016 reported significantly higher prevalence of poor sleep than those published in/after 2016 (64.7% and 47.7%, respectively, P = 0.01). Studies using lower cut-off values (i.e., ≥5) reported higher prevalence than those using high cut-offs (i.e., ≥11). Meta-regression analyses revealed that the prevalence of poor sleep quality was negatively associated with survey year (Slope = -0.079, P < 0.001), but positively associated with maternal age (Slope = 0.005, P < 0.001) and quality assessment score (Slope = 0.051, P < 0.001) (Supplementary Figures 1–3).
Study Quality Assessment, Sensitivity Analyses, and Publication Bias
The quality assessment scores ranged from 4 to 6 (Supplementary Table 1). Most (81%) of the studies did not utilize random or consecutive sampling method, and around half (52%) did not report response rate, or the response rate was less than 70%. Sensitivity analysis did not find individual studies that could significantly change the overall primary results. The funnel plot and Begg's tests (P = 0.06) did not find publication bias (Supplementary Figure 4).
Discussion
To our best knowledge, this was the first meta-analysis to examine the prevalence of poor sleep quality in perinatal and postpartum women and investigate its associated factors. The pooled prevalence (54.2%, 95% CI: 47.9–60.5%) of this meta-analysis was similar to the findings in pregnant women (45.7%, 95% CI: 36.5–55.2%) (1), but was higher than nonpregnant populations using the same sleep assessment tool, such as college students (24.1%, 95% CI: 21.0–27.5%) (82) and older adults (35.9%, 95% CI: 30.6–41.2%) (83).
Compared to nonpregnant women, those in perinatal and postpartum period are more likely to experience acute partial sleep deprivation and chronic sleep disruption, especially during labor and the first few days after giving birth (84). Commonly reported contributing factors of poor sleep quality included level of progesterone (37), physical discomforts (85), the infant's sleep–wake patterns, and the feeding practices (86).
Subgroup analyses revealed that the prevalence of poor sleep quality was higher in postnatal (67.2%, 95% CI: 57.6–75.5%) than in perinatal women (44.5%, 95% CI: 37.6–51.6%), which confirmed some (47), but not all studies (87–89). For instance, one longitudinal study using the PSQI found that 71% of women reported poor sleep in prenatal assessment and the figure increased to 77% during postpartum period (47). However, another longitudinal study found that women's sleep quality decreased progressively from their second to third trimester, but gradually improved during postnatal period (87). Studies using actigraphy and PSG also showed that even though mothers' nighttime sleep deteriorates progressively throughout pregnancy and becomes poorest on the night before delivery, an improving trend further into the postpartum period was found (88, 89). Different study characteristics, socioeconomic contexts, and measurement tools could partly contribute to the different findings between studies.
As expected, use of lower PSQI cutoff values was associated with higher prevalence of poor sleep quality. The pooled PSQI total score in this meta-analysis was 7.54 ± 0.40 (95% CI of mean score: 6.75–8.33), which is consistent with the average PSQI score of 6.97 (95% CI of mean score: 5.30–6.85) throughout pregnancy reported previously (1). The lowest PSQI component score was 0.13 ± 0.04 (95% CI of mean score: 0.05–0.22) in the domain of “use of sleeping medication.” It is possible that pregnant and postnatal women worry about the impact of medication side effects or potential risk on their infants; therefore, they are reluctant to receive medication treatment for sleep disturbances.
Studies conducted in America and those involving multicenter and mixed locations (rural and urban) tended to report higher prevalence of poor sleep quality. This could be partly attributed to the uneven number of studies across different subgroups; for example, only two studies were conducted in America, and only three studies included participants from both urban and rural areas. Women with physical comorbidities reported lower prevalence of poor sleep than those without. It is possible that while women with comorbidities were treated for their physical complaints, they received additional care/help for their sleep problems. Meta-regression analyses revealed a decreasing trend of poor sleep quality over time. With the increased attention on sleep in the past year, women in perinatal and postnatal period could have an easier access to sleep clinics and relevant health services.
In this meta-analysis, older maternal age was associated with higher prevalence of poor sleep quality, which is consistent with most earlier findings (83, 90). Traditionally, older women tended to have heavier domestic duties and care burden, and are more likely to experience physical discomforts and slower recovery from delivery (85, 91), all of which could increase the likelihood of poor sleep quality. However, Sedov et al. (1) suggested that in pregnant women, only gestational age, but not maternal age, was related to poor sleep quality.
Several limitations should be acknowledged in this meta-analysis. First, substantial heterogeneity, which is unavoidable in epidemiological studies (92, 93), still remained although subgroup and sensitivity analyses were performed. Second, some variables that may affect sleep quality, such as depression, economic status, marital status, and interpersonal relationship difficulties, were not investigated due to insufficient data in included studies. Third, the number of studies was relatively small in some subgroups. Finally, those with severe sleep problems, such as RLS and OSA, were not included in this meta-analysis. Sleep quality should be meta-analyzed separately in these populations.
Conclusions
In conclusion, this meta-analysis showed that poor sleep quality is common in perinatal and postnatal women. Given the negative impact of poor sleep quality on health outcomes and well-being, regular screening for poor sleep quality would be beneficial to improve sleep quality in this population.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation, to any qualified researcher.
Author Contributions
Study design: YY, YTX. Data collection, analysis, and interpretation: YY, WL, TJM, LZ. Drafting of the manuscript: YY, YTX. Critical revision of the manuscript: BH, GU. Approval of the final version for publication: all co-authors.
Funding
The study was supported by the National Science and Technology Major Project for investigational new drug (2018ZX09201-014), the Beijing Municipal Science & Technology Commission (No. Z181100001518005), and the University of Macau (MYRG2019-00066-FHS).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.00161/full#supplementary-material
Abbreviations
CBTI, Cognitive behavioral therapy for insomnia; PRISMA, Preferred reporting items for systematic reviews and meta-analyses; PSG, Polysomnography; PSQI, Pittsburgh sleep quality index.
References
1. Sedov ID, Cameron EE, Madigan S, Tomfohr-Madsen LM. Sleep quality during pregnancy: A meta-analysis. Sleep Med Rev (2018) 38:168–76. doi: 10.1016/j.smrv.2017.06.005
2. Fernandez-Alonso AM, Trabalon-Pastor M, Chedraui P, Perez-Lopez FR. Factors related to insomnia and sleepiness in the late third trimester of pregnancy. Arch Gynecol Obstet (2012) 286:55–61. doi: 10.1007/s00404-012-2248-z
3. Mindell JA, Cook RA, Nikolovski J. Sleep patterns and sleep disturbances across pregnancy. Sleep Med (2015) 16:483–8. doi: 10.1016/j.sleep.2014.12.006
4. Ko SH, Chen CH, Wang HH, Su YT. Postpartum women's sleep quality and its predictors in Taiwan. J Nurs Scholarship Off Publ Sigma Theta Tau Int Honor Soc Nurs (2014) 46:74–81. doi: 10.1111/jnu.12053
5. MedicineNet. Medical Definition of Perinatal (2019). https://www.medicinenet.com/script/main/art.asp?articlekey=7898>(accessed 5th June 2019)
6. Tomfohr LM, Buliga E, Letourneau NL, Campbell TS, Giesbrecht GF. Trajectories of Sleep Quality and Associations with Mood during the Perinatal Period. Sleep (2015) 38:1237–45. doi: 10.5665/sleep.4900
8. Rychnovsky J, Hunter LP. The relationship between sleep characteristics and fatigue in healthy postpartum women. Womens Health Issues (2009) 19:38–44. doi: 10.1016/j.whi.2008.07.015
9. Nishihara K, Horiuchi S, Eto H, Uchida S. Comparisons of sleep patterns between mothers in post-partum from 9 to 12 weeks and non-pregnant women. Psychiat Clin Neuros (2001) 55:227–8. doi: 10.1046/j.1440-1819.2001.00835.x
10. Matsumoto K, Shinkoda H, Kang MJ, Seo YJ. Longitudinal study of mothers' sleep-wake behaviors and circadian time patterns from late pregnancy to postpartum - Monitoring of wrist actigraphy and sleep logs. Biol Rhythm Res (2003) 34:265–78. doi: 10.1076/brhm.34.3.265.18812
11. Rawtaer I, Mahendran R, Chan HY, Lei F, Kua EH. A nonpharmacological approach to improve sleep quality in older adults. Asia-Pac Psychiat (2018) 10:e12301 doi: 10.1111/appy.12301.
12. Bhatta N, Assanangkornchai S. Patterns of domestic violence against women during pregnancy and the postpartum period in Kathmandu, Nepal. Asia-Pac Psychiat (2019) 11:e12342. doi: 10.1111/appy.12342.
13. Mindell JA, Jacobson BJ. Sleep disturbances during pregnancy. J Obstet Gynecol Neonatal Nurs (2000) 29:590–7. doi: 10.1111/j.1552-6909.2000.tb02072.x
14. Wen SY, Ko YL, Jou HJ, Chien LY. Sleep quality at 3 months postpartum considering maternal age: a comparative study. Women birth J Aust Coll Midwives (2018) 31:e367–73. doi: 10.1016/j.wombi.2018.02.004
15. Panvatvanich S, Lolekha P. Restless Legs Syndrome in Pregnant Thai Women: Prevalence, Predictive Factors, and Natural Course. J Clin Neurol (2019) 15:97–101. doi: 10.3988/jcn.2019.15.1.97
16. Bayer JK, Hiscock H, Hampton A, Wake M. Sleep problems in young infants and maternal mental and physical health. J Paediatr Child Health (2007) 43:66–73. doi: 10.1111/j.1440-1754.2007.01005.x
17. Hung CH, Lin CJ, Stocker J, Yu CY. Predictors of postpartum stress. J Clin Nurs (2011) 20:666–74. doi: 10.1111/j.1365-2702.2010.03555.x
18. Yamazaki A. Family synchronizers: Predictors of sleep-wake rhythm for Japanese first-time mothers. Sleep Biol Rhythms (2007) 5:218–25. doi: 10.1111/j.1479-8425.2007.00274.x
19. Lee KA, Zaffke ME, McEnany G. Parity and sleep patterns during and after pregnancy. Obstet Gynecol (2000) 95:14–8. doi: 10.1097/00006250-200001000-00003
20. Lee SY, Lee KA. Early postpartum sleep and fatigue for mothers after cesarean delivery compared with vaginal delivery: an exploratory study. J Perinat Neonatal Nurs (2007) 21:109–13. doi: 10.1097/01.JPN.0000270627.73993.b0
21. Moller-Olsen C, Friedman SH, Prakash C, North A. Clinical characteristics of maternal mental health service users treated with mood stabilizing or antipsychotic medication. Asia-Pac Psychiat (2018) 10:e12304. doi: 10.1111/appy.12304.
22. Naghi I, Keypour F, Ahari SB, Tavalai SA, Khak M. Sleep disturbance in late pregnancy and type and duration of labour. J Obstet Gynaecol (2011) 31:489–91. doi: 10.3109/01443615.2011.579196
23. Okun ML, Schetter CD, Glynn LM. Poor Sleep Quality is Associated with Preterm Birth. Sleep (2011) 34:1493–8. doi: 10.5665/sleep.1384
24. Gelaye B, Barrios YV, Zhong QY, Rondon MB, Borba CPC, Sanchez S E, et al. Association of poor subjective sleep quality with suicidal ideation among pregnant Peruvian women. Gen Hosp Psychiat (2015) 37:441–7. doi: 10.1016/j.genhosppsych.2015.04.014
25. Krystal AD, Edinger JD. Measuring sleep quality. Sleep Med (2008) 9(Suppl 1):S10–17. doi: 10.1016/S1389-9457(08)70011-X
26. Becker NB, Jesus SN, Joao K, Viseu JN, Martins RIS. Depression and sleep quality in older adults: a meta-analysis. Psychol Health Med (2017) 22:889–95. doi: 10.1080/13548506.2016.1274042
27. Zheng B, Li M, Wang KL, Lv J. Analysis of the reliability and validity of the Chinese version of Pittsburgh sleep quality index among medical college students. Beijing Da Xue Xue Bao Yi Xue Ban (2016) 48:424–8.
28. Doi Y, Minowa M, Uchiyama M, Okawa M, Kim K, Shibui K, et al. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res (2000) 97:165–72. doi: 10.1016/s0165-1781(00)00232-8
29. Sohn SI, Kim DH, Lee MY, Cho YW. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath (2012) 16:803–12. doi: 10.1007/s11325-011-0579-9
30. Blais FC, Gendron L, Mimeault V, Morin CM. [Evaluation of insomnia: validity of 3 questionnaires]. Encephale (1997) 23:447–53.
31. Seidi PAM, Mohammadi H, Khazaie H, Abas NQ, Jaff D. Psychometric properties of the Kurdish version of Pittsburgh Sleep Quality Index. Sleep Med (2019) 63:75–81. doi: 10.1016/j.sleep.2019.04.022
32. Bertolazi AN, Fagondes SC, Hoff LS, Dartora EG, Miozzo IC, de Barba ME, et al. Validation of the Brazilian Portuguese version of the Pittsburgh Sleep Quality Index. Sleep Med (2011) 12:70–5. doi: 10.1016/j.sleep.2010.04.020
33. Popevic MB, Milovanovic APS, Milovanovic S, Nagorni-Obradovic L, Nesic D, Velaga M. Reliability and Validity of the Pittsburgh Sleep Quality Index-Serbian Translation. Eval Health Prof (2018) 41:67–81. doi: 10.1177/0163278716678906
34. Takacs J, Bodizs R, Ujma PP, Horvath K, Rajna P, Harmat L, et al. Reliability and validity of the Hungarian version of the Pittsburgh Sleep Quality Index (PSQI-HUN): comparing psychiatric patients with control subjects. Sleep Breath (2016) 20:1045–51. doi: 10.1007/s11325-016-1347-7
35. Farrahi Moghaddam J, Nakhaee N, Sheibani V, Garrusi B, Amirkafi A. Reliability and validity of the Persian version of the Pittsburgh Sleep Quality Index (PSQI-P). Sleep Breath (2012) 16:79–82. doi: 10.1007/s11325-010-0478-5
36. Hedman C, Pohjasvaara T, Tolonen U, Suhonen-Malm AS, Myllyla VV. Effects of pregnancy on mothers' sleep. Sleep Med (2002) 3:37–42. doi: 10.1016/S1389-9457(01)00130-7
37. Lee KA. Alterations in sleep during pregnancy and postpartum: a review of 30 years of research. Sleep Med Rev (1998) 2:231–42. doi: 10.1016/S1087-0792(98)90010-7
38. Zhou H, Li W, Ren Y. Poor sleep quality of third trimester exacerbates the risk of experiencing postnatal depression. Psychol Health Med (2018) 25(2):229–38. doi: 10.1080/13548506.2018.1549738
39. Murphey C, Carter P, Price LR, Champion JD, Nichols F. Psychological Distress in Healthy Low-Risk First-Time Mothers during the Postpartum Period: An Exploratory Study. Nurs. Res Pract (2017) 12:1–12. doi: 10.1155/2017/8415083
40. Parker G, Beresford B, Clarke S, Gridley K, Pitman R, Spiers G, et al. Technical report for SCIE research review on the prevalence and incidence of parental mental health problems and the detection, screening and reporting of parental mental health problems. University of York: Social Policy Research Unit (2008).
41. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med (2002) 21:1539–58. doi: 10.1002/sim.1186
42. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis. United Kingdom: Wiley (2009), 107–17.
43. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
44. Astuti Y, Rachmawati IN, Rahma H. The Correlation Between Infant Temperament and Sleep Quality of Postpartum Mother in Primary Health Care Prambanan and Jogonalan Klaten Indonesia. Adv Sci Lett (2017) 23:12571–4. doi: 10.1166/asl.2017.10819
45. Cui Y. The relationship between depressive symptoms and sleep quality during pregnancy (in Chinese). China Health Care Nutr (2017) 27:307–8.
46. Dorheim SK, Bondevik GT, Eberhard-Gran M, Bjorvatn B. Sleep and depression in postpartum women: a population-based study. Sleep (2009) 32:847–55. doi: 10.1093/sleep/32.7.847
47. Francis B, Klebanoff M, Oza-Frank R. Racial discrimination and perinatal sleep quality. Sleep Health (2017) 3:300–5. doi: 10.1016/j.sleh.2017.05.012
48. Fu L. Study on maternal sleep status after childbirth and its correlation with infant growth and development (in Chinese). Master thesis, Central South University: University Press (2012).
49. Gao X, Yang FL. Investigation and analysis of the influence of education level on sleep quality of pregnant women in late pregnancy (in Chinese). J Aerospace Med (2012) 23:1008–10.
50. Gunduz S, Kosger H, Aldemir S, Akcal B, Tevrizci H, Hizli D. Sleep deprivation in the last trimester of pregnancy and inadequate vitamin D: Is there a relationship? J Chin Med Assoc : JCMA (2016) 79:34–8. doi: 10.1016/j.jcma.2015.06.017
51. Hairston IS, Solnik-Menilo T, Deviri D, Handelzalts JE. Maternal depressed mood moderates the impact of infant sleep on mother–infant bonding. Arch Women's Ment Health (2016) 19:1029–39. doi: 10.1007/s00737-016-0652-2
52. Han Y, Zheng LY, Huang R. Canonical correlation analysis of sleep quality and quality of life in pregnant women (in Chinese). Maternal Child Health Care China (2015) 30:4533–5.
53. Huang CM, Carter PA, Guo JL. A comparison of sleep and daytime sleepiness in depressed and non-depressed mothers during the early postpartum period. J Nurs Res : JNR (2004) 12:287–96. doi: 10.1097/01.JNR.0000387513.75114.bb
54. Hung HM, Tsai PS, Ko SH, Chen CH. Patterns and predictors of sleep quality in Taiwanese pregnant women. MCN. Am J Maternal Child Nurs (2013) 38:95–101. doi: 10.1097/NMC.0b013e3182659345
55. Iranpour S, Kheirabadi GR, Esmaillzadeh A, Heidari-Beni M, Maracy MR. Association between sleep quality and postpartum depression. J Res Med Sci Off J Isfahan Univ Med Sci (2016) 21:110. doi: 10.4103/1735-1995.193500
56. Ko H, Shin J, Kim MY, Kim YH, Lee J, Kil KC. Sleep disturbances in Korean pregnant and postpartum women. J Psychosom Obstetrics Gynecol (2012) 33:85–90. doi: 10.3109/0167482X.2012.658465
57. Ko Y-L, Lin P-C, Chen S-C. Stress, sleep quality and unplanned Caesarean section in pregnant women. Int J Nurs Pract (2015) 21:454–61. doi: 10.1111/ijn.12267
58. Li Z, Wang NR. Study on the relationship between maternal sleep quality and physical growth of infants in a certain urban area (in Chinese). Guide China Med (2018) 16:1–4.
59. Li P, Zhang Y, Feng Y. Correlation between sleep quality and postpartum depression status (in Chinese). Maternal Child Health Care China (2016) 31:1369–72.
60. Luo T, Hua J, Li Y. Correlation between depressive symptoms and sleep quality in late pregnancy (in Chinese). Maternal Child Health Care China (2016) 31:2157–9.
61. Sut HK, Asci O, Topac N. Sleep Quality and Health-Related Quality of Life in Pregnancy. J Perinat Neonatal Nurs (2016) 34:302–9. doi: 10.1097/jpn.0000000000000181
62. Tobback E, Behaeghel K, Hanoulle I, Delesie L, Loccufier A, Van Holsbeeck A. Comparison of subjective sleep and fatigue in breast- and bottle-feeding mothers. Midwifery (2017) 47:22–7. doi: 10.1016/j.midw.2017.01.009
63. Tian Y, Tuo MH, Ma RM. Correlation between depression and sleep quality in pregnant women in late pregnancy (in Chinese). Chin J Dis Control Prev (2018) 22:630–4.
64. Tsai SY, Kuo LT, Lai YH, Lee CN. Factors associated with sleep quality in pregnant women: a prospective observational study. Nurs Res (2011) 60:405–12. doi: 10.1097/NNR.0b013e3182346249
65. Tsai SY, Lee CN, Wu WW, Landis CA. Sleep hygiene and sleep quality of third-trimester pregnant women. Res Nurs Health (2016) 39:57–65. doi: 10.1002/nur.21705
66. Volkovich E, Tikotzky L, Manber R. Objective and subjective sleep during pregnancy: links with depressive and anxiety symptoms. Arch Womens Ment Health (2016) 19:173–81. doi: 10.1007/s00737-015-0554-8
67. Wang G, Deng Y, Jiang Y, Lin Q, Dong S, Song Y, et al. Trajectories of sleep quality from late pregnancy to 36 months postpartum and association with maternal mood disturbances: a longitudinal and prospective cohort study. Sleep (2018) 41(12):1–10. doi: 10.1093/sleep/zsy179
68. Wang H. Investigation and Analysis of Sleeping Status of Pregnant Women in Hospital during Hospitalization and Nursing Countermeasures (in Chinese). Chin J Woman Child Health Res (2017) 28:227–8.
69. Wang W, Xu JA, Yuan XR. Relationship between personality characteristics and coping styles of pregnant women and sleep quality (in Chinese). Guangdong Med J (2017) 38:3505–8.
70. Wang Y. Analysis of sleep disorders and emotional status in pregnant women at the end of pregnancy (in Chinese). Modern Med Health (2010) 26:1993–95.
71. Wu X. Correlation between sleep quality and adverse emotions in pregnant women in third trimester (in Chinese). J Bethune Military Med Coll (2017) 15:745–6.
72. Wu P, Fu DX, Liu YM. Investigation on factors affecting sleep quality of pregnant women in late pregnancy in Chongqing (in Chinese). Maternal Child Health Care China (2017) 32:2001–3.
73. Yang Y, Mao J, Ye Z, Zeng X, Zhao H, Liu Y. Determinants of sleep quality among pregnant women in China: a cross-sectional survey. J Waternal-Fetal Neonatal Med Off J Eur Assoc Perinatal Med Fed Asia Oceania Perinatal Societies Int Soc Perinatal Obstet (2018) 31:2980–5. doi: 10.1080/14767058.2017.1359831
74. Yang J, Min LH, Liu XJ. Investigation on sleep quality during maternal hospitalization (in Chinese). Chin Nurs Res (2006) 20:213–4.
75. Zhang W, Chen J, Wang LM. Related factors of sleep disorders in pregnant women in late pregnancy and the effect of nursing intervention (in Chinese). Chin Nurs Res (2008) 28:2570–2.
76. Zhang Y. The relationship between depressive symptoms and sleep quality during pregnancy (in Chinese). World Latest Med Inf (2018) 18:67–71.
77. Zhang L, Huang YJ, Xu T. Sleep quality and influencing factors in women in the third trimester (in Chinese). J Maternal Child Health Care China (2011) 26:4710–3.
78. Zhao L, Xiao H, Zou F. Study on the current status of female fatigue and related factors in 6 weeks postpartum (in Chinese). J Chin J Pract Nurs (2018) 34:2133–7.
79. Zhao M, Le Y, Yu QM. Analysis on the status quo and influencing factors of sleep quality of pregnant women in Shihezi City (in Chinese). J Guangdong Med J (2017) 38:3005–10.
80. Zheng R. Correlation between sleep quality and sleepiness, fatigue, anxiety and depression in pregnant women (in Chinese). Master thesis, Central South University: University Press (2011).
81. Zhu L, Wang GH, Jiang YR. Study on sleep status and related factors of women in the third trimester (in Chinese). J Chin J Woman Child Health Res (2018) 29:22–6.
82. Li L, Wang YY, Wang SB, Zhang L, Li L, Xu DD. Prevalence of sleep disturbances in Chinese university students: a comprehensive meta-analysis. J Sleep Res (2018) 27:e12648. doi: 10.1111/jsr.12648
83. Lu L, Wang SB, Rao W, Zhang Q, Ungvari GS, Ng CH, et al. The Prevalence of Sleep Disturbances and Sleep Quality in Older Chinese Adults: A Comprehensive Meta-Analysis. Behav Sleep Med (2018), 17(6):683–97. doi: 10.1080/15402002.2018.1469492
84. Bei B, Coo S, Trinder J. Sleep and Mood During Pregnancy and the Postpartum Period. Sleep Med Clin (2015) 10:25–33. doi: 10.1016/j.jsmc.2014.11.011
85. Kamysheva E, Skouteris H, Wertheim EH, Paxton SJ, Milgrom J. A prospective investigation of the relationships among sleep quality, physical symptoms, and depressive symptoms during pregnancy. J Affect Disord (2010) 123:317–20. doi: 10.1016/j.jad.2009.09.015
86. Dennis CL, Ross L. Relationships among infant sleep patterns, maternal fatigue, and development of depressive symptomatology. Birth (2005) 32:187–93. doi: 10.1111/j.0730-7659.2005.00368.x
87. Jomeen J, Martin CR. The impact of choice of maternity care on psychological health outcomes for women during pregnancy and the postnatal period. J Eval Clin Pract (2008) 14:391–8. doi: 10.1111/j.1365-2753.2007.00878.x
88. Beebe KR, Lee KA. Sleep disturbance in late pregnancy and early labor. J Perinat Neonatal Nurs (2007) 21:103–8. doi: 10.1097/01.JPN.0000270626.66369.26
89. Kang MJ, Matsumoto K, Shinkoda H, Mishima M, Seo YJ. Longitudinal study for sleep-wake behaviours of mothers from pre-partum to post-partum using actigraph and sleep logs. Psychiatry Clin Neurosci (2002) 56:251–2. doi: 10.1046/j.1440-1819.2002.00992.x
90. Alessi C, Vitiello MV. Insomnia (primary) in older people. BMJ Clin Evid (2011) 2011:93. doi: 10.14260/jemds/2015/2302
91. Hellstrom A, Hagell P, Fagerstrom C, Willman A. Measurement properties of the Minimal Insomnia Symptom Scale (MISS) in an elderly population in Sweden. BMC Geriatr (2010) 10:84. doi: 10.1186/1471-2318-10-84
92. Mata DA, Ramos MA, Bansal N, Khan R, Guille C, Di Angelantonio E. Prevalence of Depression and Depressive Symptoms Among Resident Physicians A Systematic Review and Meta-analysis. Jama-J Am Med Assoc (2015) 314:2373–83. doi: 10.1001/jama.2015.15845
Keywords: sleep quality, perinatal, postnatal, women, meta-analysis
Citation: Yang Y, Li W, Ma T-J, Zhang L, Hall BJ, Ungvari GS and Xiang Y-T (2020) Prevalence of Poor Sleep Quality in Perinatal and Postnatal Women: A Comprehensive Meta-Analysis of Observational Studies. Front. Psychiatry 11:161. doi: 10.3389/fpsyt.2020.00161
Received: 08 November 2019; Accepted: 20 February 2020;
Published: 13 March 2020.
Edited by:
Hruda N. Mallick, All India Institute of Medical Sciences, IndiaReviewed by:
Axel Steiger, Ludwig Maximilian University of Munich, GermanyLourdes DelRosso, University of Washington, United States
Copyright © 2020 Yang, Li, Ma, Zhang, Hall, Ungvari and Xiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu-Tao Xiang, eHl1dGx5QGdtYWlsLmNvbQ==
†These authors have contributed equally to this work
 Yuan Yang
Yuan Yang Wen Li1,2†
Wen Li1,2† Ling Zhang
Ling Zhang