- 1Department of Child and Adolescent Psychiatry, Medical University of Vienna, Vienna, Austria
- 2Department for Ethics and Law in Medicine, Medical University of Vienna, Vienna, Austria
- 3Department of Pediatrics and Adolescent Medicine, Medical University of Vienna, Vienna, Austria
- 4Department of Psychiatry and Department for Ethics and Law in Medicine, Medical University of Vienna, Vienna, Austria
Background: Psychological sequels to criminal violence can be long lasting and severe. They are in many countries not sufficiently considered in court cases as an important circumstance that could be used to assess the severity of the crime, also guiding redress, compensation, and rehabilitation of the victim, and—in children—child custody considerations. So far, the focus of forensic assessment has often been limited to diagnostic categories, especially “posttraumatic stress disorder” (PTSD), a diagnosis that presently is subjected to rapidly changing definitions both in and between diagnostic systems. Other indicators such as quality of life (QoL) might be of equal importance as compared to clinical or research diagnostic categories to understand and evaluate the impact of a crime and the amount of help needed and, in the legal context, redress to be asked. Symptoms might differ depending on the crime encountered.
Objective and Methods: QoL and general symptom patterns including a PTSD diagnosis were assessed in a group of 10- to 17-year-old minors with (n = 33) and without (n = 49) PTSD diagnosis who all had experienced sexual abuse, physical abuse, death of a parent, or their parents’ divorce, using standardized diagnostic instruments.
Results: PTSD patients reported a significantly lower QoL than non-PTSD controls. Reported symptom patterns with potential impact on life, such as intrusive thoughts, differed between the victims of different crime types, with the highest rates of both intrusive symptoms and combined symptom profile in victims of sexual abuse. Data indicate that the changes between older and present criteria and between DSM and recently published ICD 11 might help identify different groups and symptom profiles.
Conclusion: Specific trauma-related symptom profiles integrating the type of crime encountered and its individual impact on QoL may help improve future forensic assessment and guide compensation and rehabilitation plans. Carefully designed studies are now needed to further explore the use and forensic usability of complex indicators and the impact of violence in different forensic settings.
Introduction
The International Classification of Diseases (ICD-10) defines trauma as “a stressful event or situation (either short- or long-lasting) of an exceptionally threatening or catastrophic nature, which is likely to cause pervasive distress in almost anyone” (1). Trauma in childhood and adolescence often occurs within the family (2) and may include physical, sexual, and emotional abuse; neglect; being separated from parents; as well as witnessing inter-parental violence (3). These traumatic events have a high recurrence, which in its own right may lead to complex traumatization (4, 5) and to the development of posttraumatic stress disorders (PTSDs) in children and adolescents, with lifetime prevalence rates ranging as high as 9% for 13- to 15-year-old adolescents (6).
PTSD constitutes a complex and heterogeneous syndrome that has been shown to encompass up to 79,794 different symptom constellations that meet the criteria for PTSD (7). During the past decades, however, the symptom clusters that were regarded as indicative of PTSD diagnoses in the American Psychiatric Associations DSM model (8, 9) underwent significant changes that were to a similar degree parallel to those seen in the World Health Organization’s International Classification of Diseases, with again marked differences between DSM 5 and ICD-11. This constitutes a challenge also in the effort to provide reliable standards in forensic assessment (10)—an issue to be discussed later in this article. The fact that, in a further step, issues like functioning and quality of life (QoL) must also be considered in diagnostic assessment has gradually been implemented into both of these major diagnostic systems, and partly achieved by integrating the WHO Assessment Schedule.
The fact that, in a further step, resulting issues like functioning and QoL must also be considered in diagnostic assessment has been slowly implemented into both systems and has partly been achieved by integrating the WHO Disability Assessment Schedule 2 (11). The importance of individual symptom profiles, especially of the actual individual QoL that results from symptoms or in the framework of a diagnosis, has so far been neglected and not covered by most studies.
Literature suggests that apart from the severity, extent, and frequency of trauma exposure (12), the probability of developing PTSD may also significantly depend on the type of traumatic event (13–18). Prior studies (6) found that sexual abuse, rape, childhood neglect, physical abuse, as well as attempted suicide had the highest associations with PTSD and subclinical PTSD when compared to other trauma types such as death of a family member, threat of violence, or serious accidents. Among trauma types, sexual abuse seems to be an especially strong and consistent risk factor for the development of PTSD symptoms (19–22).
In addition to the development of PTSD, the type of trauma may also affect other mental health problems or disorders such as depression, withdrawal behavior, anxiety disorders, suicidal attempts, aggression, antisocial behavior, delinquency, peer problems, or substance abuse (14, 15, 17, 21, 23–29).
Apart from personally experiencing a trauma, witnessing a traumatic event may have similarly deleterious repercussions. McCloskey and Walker (14) reported that children who witnessed the death or illness of a significant other were at the greatest risk of developing PTSD, followed by experiencing recurrent domestic abuse as well violent crime. Similarly, Melhem et al. (15) found that children, whose parents died of suicide, an accidental death, or a sudden natural death, showed higher rates of depression and PTSD than non-bereaved controls. In sum, however, studies comparing those two types of traumata—self-experienced vs. witnessed—with regard to their effect on PTSD symptomatology and other mental health problems are still scarce.
Lastly, a traumatic experience may not only lead to specific psychopathological symptoms, but also have a more general impact on the person’s social ties, friendship, and interests and, thus, may affect the patients’ overall QoL. Past studies (30) substantiate this assumption, showing that posttraumatic stress is significantly linked to a reduction of QoL in children and adolescents. Also, prior findings highlight the negative long-term effects childhood traumata can have on physical, psychological, and social QoL in adulthood (31, 32). Only one study has, however, thus far examined this relationship and found that neglect and sexual abuse were associated with reduced mental health-related QoL, whereas psychological and physical abuse caused a reduction in both mental and physical health-related QoL (33).
To date, research has mainly focused on differences in psychopathology, and especially on the prevalence of clinical symptoms or diagnosis, but not on their specific impact on life in connection with the experience encountered by the victim. Thus, the current study aimed to explore whether 1) experiencing different kinds of traumatic events and 2) fulfilling or not the criteria for a PTSD diagnosis have an impact on symptoms profile and QoL, which should also be considered in civil and criminal court.
Method
The current study was carried out in a group of consecutive patients at the Trauma and Forensics outpatient clinic at the Department of Child and Adolescence Psychiatry at the Medical University of Vienna. Following a detailed briefing, all parents signed an informed consent form agreeing to the voluntary participation of their children. Minors aged 14 and above also signed informed consent. Accordingly, children and adolescents were provided with written informed consent forms stating that withdrawal would not affect their treatment and that all communications would be anonymous. The local institutional review board approved the study in its current form. All participants were interviewed by expert interviewers (trained psychologists with a long-standing expertise in psychotraumatology). Parents were interviewed separately. The study was approved by the Ethics Committee of the Medical University of Vienna (EK-number: 476/2004).
Participants
In total, 82 patients (46 female, 36 male) between 10 years 7 months and 17 years 11 months (M = 13.6; SD = 2.348) completed the required questionnaires. All patients had experienced or witnessed a traumatic event, either sexual abuse (n = 19), physical abuse (n = 19), loss of a close family member (n = 19), or the divorce of their parents (n = 25). Patients were assessed a month post-trauma at the earliest and not later than 2–3 months after the last traumatic experience. Patients without sufficient language skills or with other psychiatric diagnosis prior to the traumatic event were excluded from the study.
Trauma types covered a range of multiple specific traumatic experiences: 1) Sexual assaults comprised anal/vaginal rape, brutal insertion of fingers or objects, simultaneous abuse by different perpetrators, oral sex, forced masturbation, kissing, and touching (including anal/vaginal area or penis). 2) Physical abuse was defined here as beating in the face or head, knocking unconscious, pulling hairs until bleeding, beating leading to injury, cold/hot showering, and kicks against the body. 3) The loss of a family member included the death of a sibling, mother, or father after an accident, terminal disease, homicide, suicide, or a family member who went missing. 4) The category divorce, in turn, was defined as the divorce of biological parents including legal action, separation from one parent or both parents for an undefined longer period, or the child being a witness of emotional violence between parents or being treated as a property in the conflict situation.
Measures
ICD-10- and DSM-IV TR-based instruments were used given that these were the only available ones, validated in German, at the time the study was carried out.
PTSD symptomatology. The revised form of the Impact of Event Scale-Revised (IES-R) (34) was used to assess subjective distress caused by traumatic events. The 22-item self-report measure was completed by the participating children and adolescents. It examines symptoms of intrusive thoughts (criterion B), avoidance (criterion C), and hyperarousal (criterion D). The IES-R is a valid and reliable screening instrument for PTSD and has previously been used in several studies investigating PTSD symptomatology (35–37). The IES-R shows a good overall reliability (α = 0.93; scales α range from 0.83 to 0.89). In addition, a routine screening checklist for PTSD symptoms developed locally for everyday clinical documentation independent from the research project was given to the participants as they were also offered treatment in our outpatient department.
General symptomatology. The school-age assessment forms of the Child Behavior Checklist (CBCL 6–18) (38) are based on DSM-IV categories and represent an empirically based screening of the following psychopathological dimensions: (39) socially withdrawn, (40) somatic complaints, (41) anxious/depressed, (42) social problems, (43) thought problems, (44) attention problems, as well as (45) rule-breaking behavior and (46) aggressive behavior. The CBCL 6–18 was completed by children’s biological mothers (n = 57), biological fathers (n = 17), stepmothers (n = 2), and a grandmother (n = 1). Five parents did not complete this questionnaire.
The German version of the Structured Clinical Interview for DSM-IV (SCID) PTSD and Major Depression section (47) was administered by trained psychologists to diagnose PTSD and differentiate PTSD and depression or acute stress reactions in children and adolescents.
Quality of life. The Inventory for the Assessment of Quality of Life in Children and Adolescents (ILK) (48) is a disorder-nonspecific screening instrument that assesses QoL in children with and without mental disorders on the following items: school, family, peer contacts, interests, and free time, as well as stress through assessment and therapy and stress through the mental disorder or, somatic disease, as well as an overall rating of the patients’ QoL. The ILK shows an adequate overall reliability of α = 0.62 in the current study. It has been widely used in a number of studies with different clinical populations and has been shown to be to be a useful and reliable instrument (39–46).
Results
ANOVAs were computed to analyze differences between trauma types regarding PTSD symptomatology, behavioral symptomatology, and QoL. Statistical analyses were carried out using SPSS 20 (IBM) and considering an alpha error of 5% in all calculations. Below, the results are presented according to the abovementioned research questions.
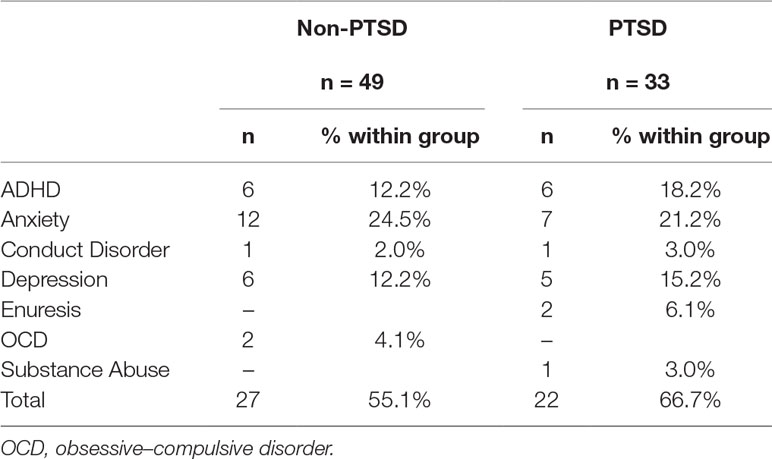
Post-assessment, 33 patients were diagnosed with PTSD (ICD-10-Code F43.1), whereas 49 patients did not fulfill the criteria for a PTSD diagnosis. Table 1 shows the frequency of comorbid disorders in PTSD and non-PTSD children after traumatic events.
PTSD Symptomatology
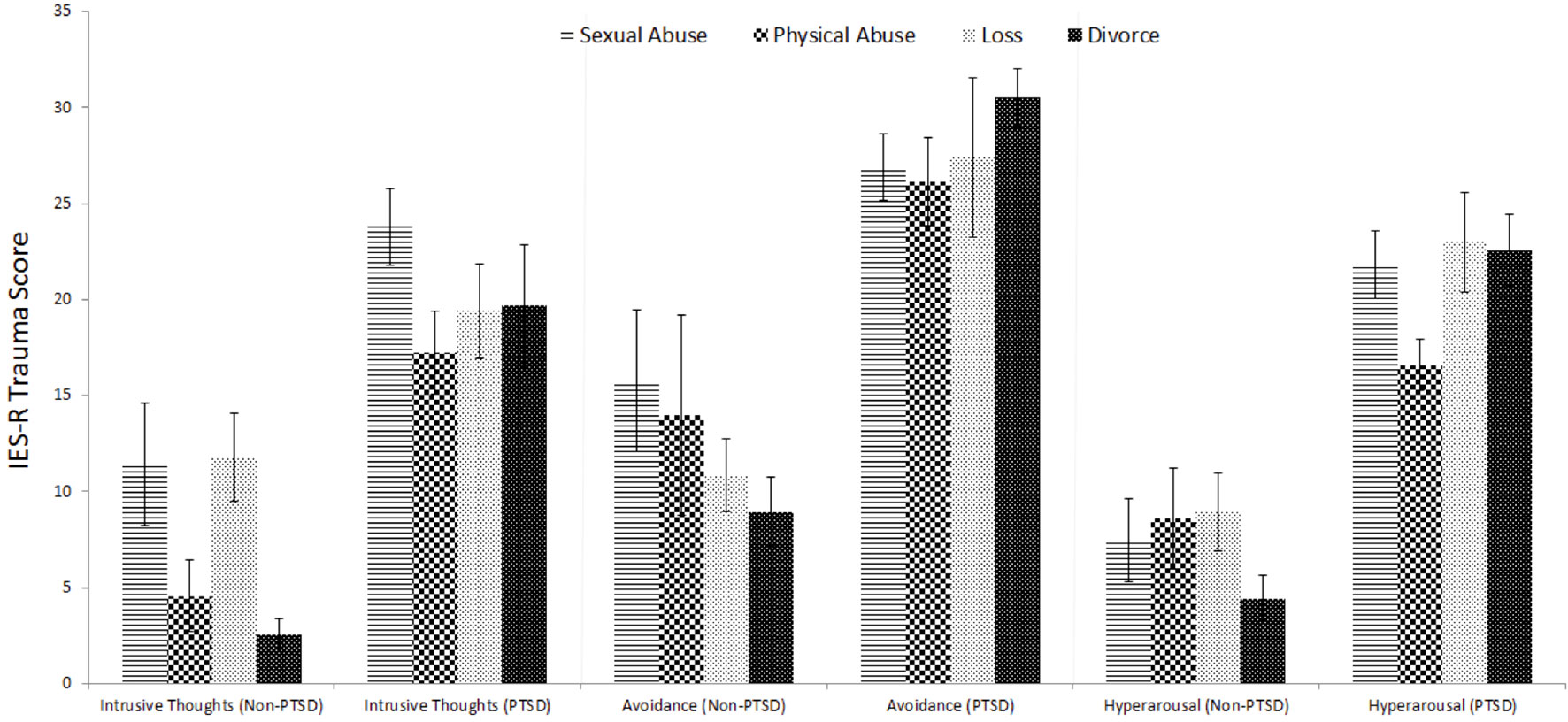
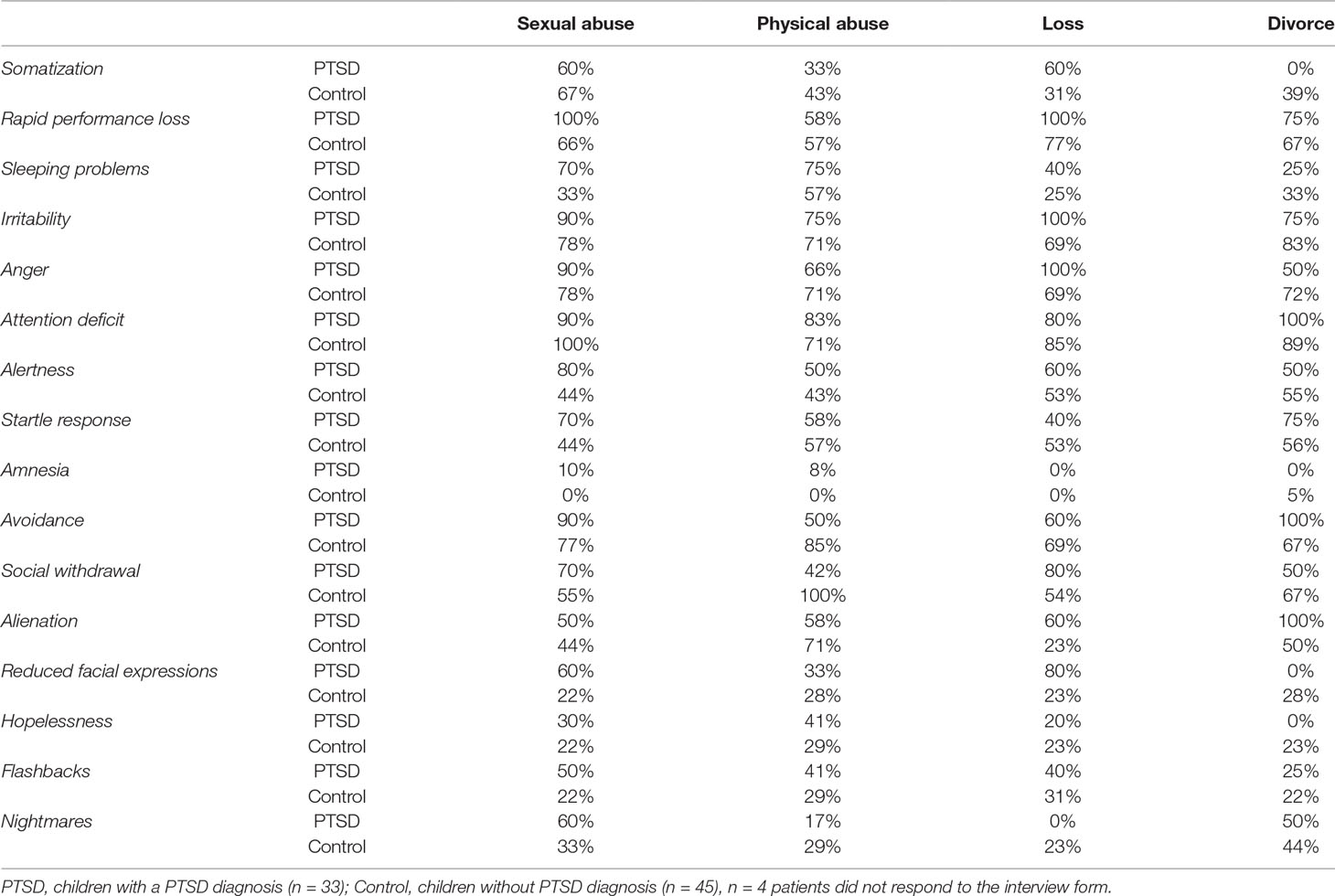
Figure 1 shows differences between the four trauma-type groups in means and the standard error of the mean for the key PTSD symptoms intrusive thoughts, avoidance, and hyperarousal. More specifically, the two-factor ANOVA with Bonferroni post hoc tests indicated a significant main effect of trauma type for intrusive thoughts (F3,74 = 4.260; p = 0.008; par. η² = 0.147) with children reporting significantly less intrusive thoughts after their parents’ divorce than those children who experienced sexual abuse (p < 0.001), physical abuse (p = 0.035), or loss of a significant other (p = 0.006). Additionally, there was a significant difference between children with PTSD and without PTSD (F1,74 = 56.421; p < 0.001; par. η² = 0.433) regarding intrusive thoughts or flashbacks. With regard to avoidance, there was no significant difference between the four traumatic events (F3,74 = 0.214; p = 0.887; par. η² = 0.009), but there was a significantly relevant difference between children with and without PTSD (F1,74 = 57.192; p < 0.001; par. η² = 0.436). Similarly, no difference in hyperarousal was found between the trauma types (F3,74 = 1.547; p = 0.210; par. η² = 0.059), but again a significant main effect emerged for PTSD diagnosis (F1,74 = 104.287; p < 0.001; par. η² = 0.585). Table 2 shows the descriptive results of the symptom screening using an interview form.
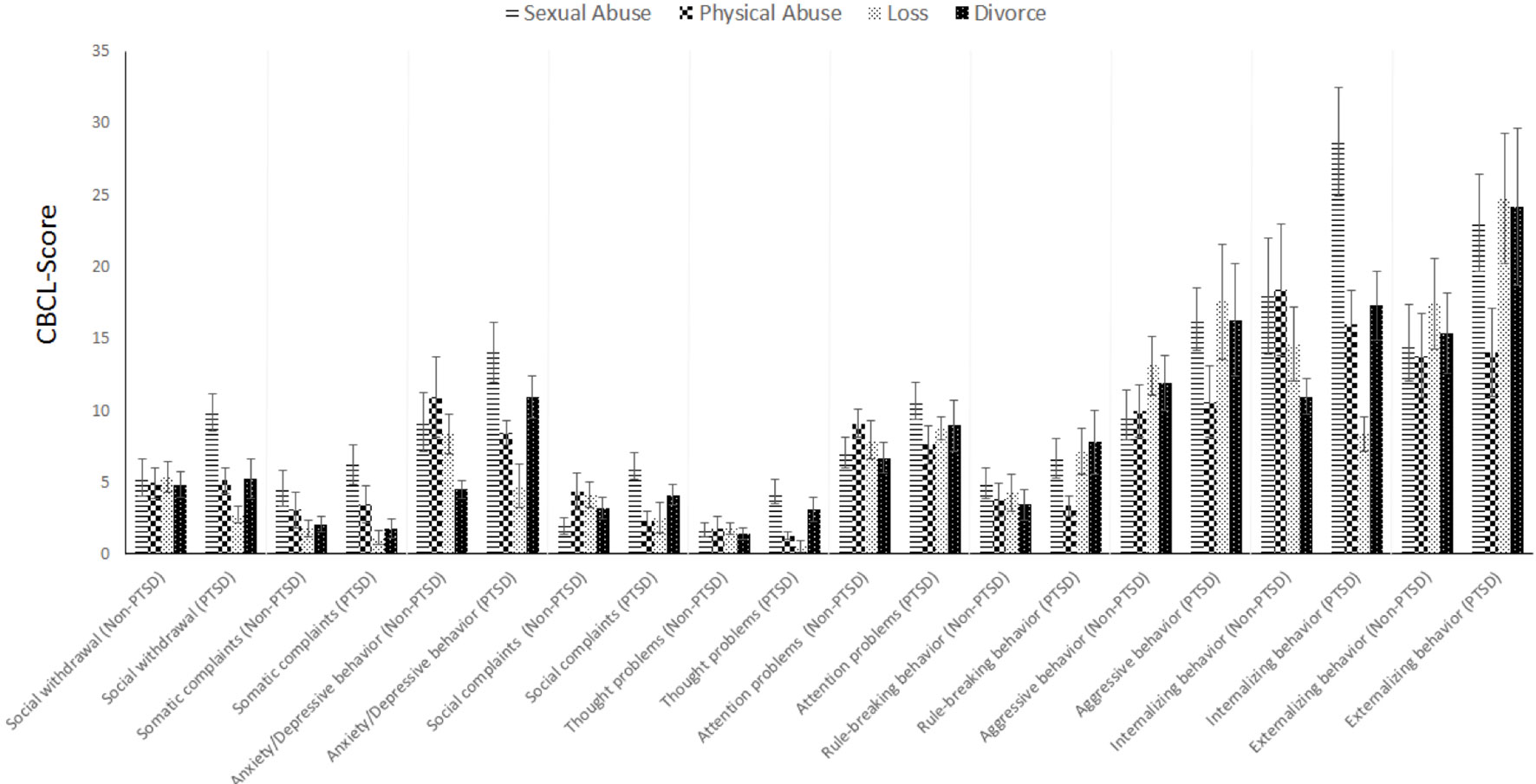
Behavioral Symptomatology
According to the CBCL scores of n = 78 parents (of children with PTSD diagnosis, n = 33; without a PTSD diagnosis, n = 49), a statistically relevant difference between the four types of traumatic events was found for social withdrawal (F3,68 = 3.261; p = 0.027; par. η² = 0.126). After Bonferroni correction, results indicated a significant difference in social withdrawal between children after sexual trauma and children after loss or divorce (p < 0.05). With an alpha error increase to 10%, differences between these two subgroups and children after physical abuse also became significant. Furthermore, an interaction effect of types of traumatic events and the groups of children with or without PTSD was found (F3,68 = 3.005; p = 0.036; par. η² = 0.117), indicating that, in particular, children with PTSD after sexual abuse show the highest levels of social withdrawal.
With regard to somatic complaints, children whose parents were divorced reported less complaints than children who experienced sexual abuse (F3,68 = 5.342; p = 0.002; par. η² = 0.191). Also, there was a significant main effect of trauma type regarding anxious and depressive behaviors (F3,68 = 3.670; p = 0.016; par. η² = 0.139); corresponding Bonferroni analyses revealed a difference between children after sexual abuse and children after the loss of a family member (p = 0.032) and those who experienced the divorce of their parents (p = 0.002).
Regarding thought problems, again a significant effect was found for the type of traumatic event (F3,68 = 3.670; p = 0.017; par. η² = 0.138). Bonferroni analyses indicated group differences between sexually abused and physically abused children (p = 0.027) as well as children who experienced loss (0.026), but not those with divorced parents (p = 1.000). A significant interaction effect showed that children with PTSD particularly tended to have more thought problems after sexual trauma or divorce (F3,68 = 4.419; p = 0.007; par. η² = 0.163).
Finally, differences between children with and without PTSD were found regarding rule-breaking behavior (F3,68 = 4.827; p = 0.031; par. η² = 0.066) and aggressive behavior (F3,68 = 4.916; p = 0.020; par. η² = 0.067), showing that children with a PTSD diagnosis tend to show more oppositional behavior than children who experienced a traumatic event but were not diagnosed with PTSD. Interestingly, there were no significant differences for social complaints or attention problems, either between children with and without PTSD or between the four trauma types. For an overview over general symptomatology, see Figure 2.
QoL
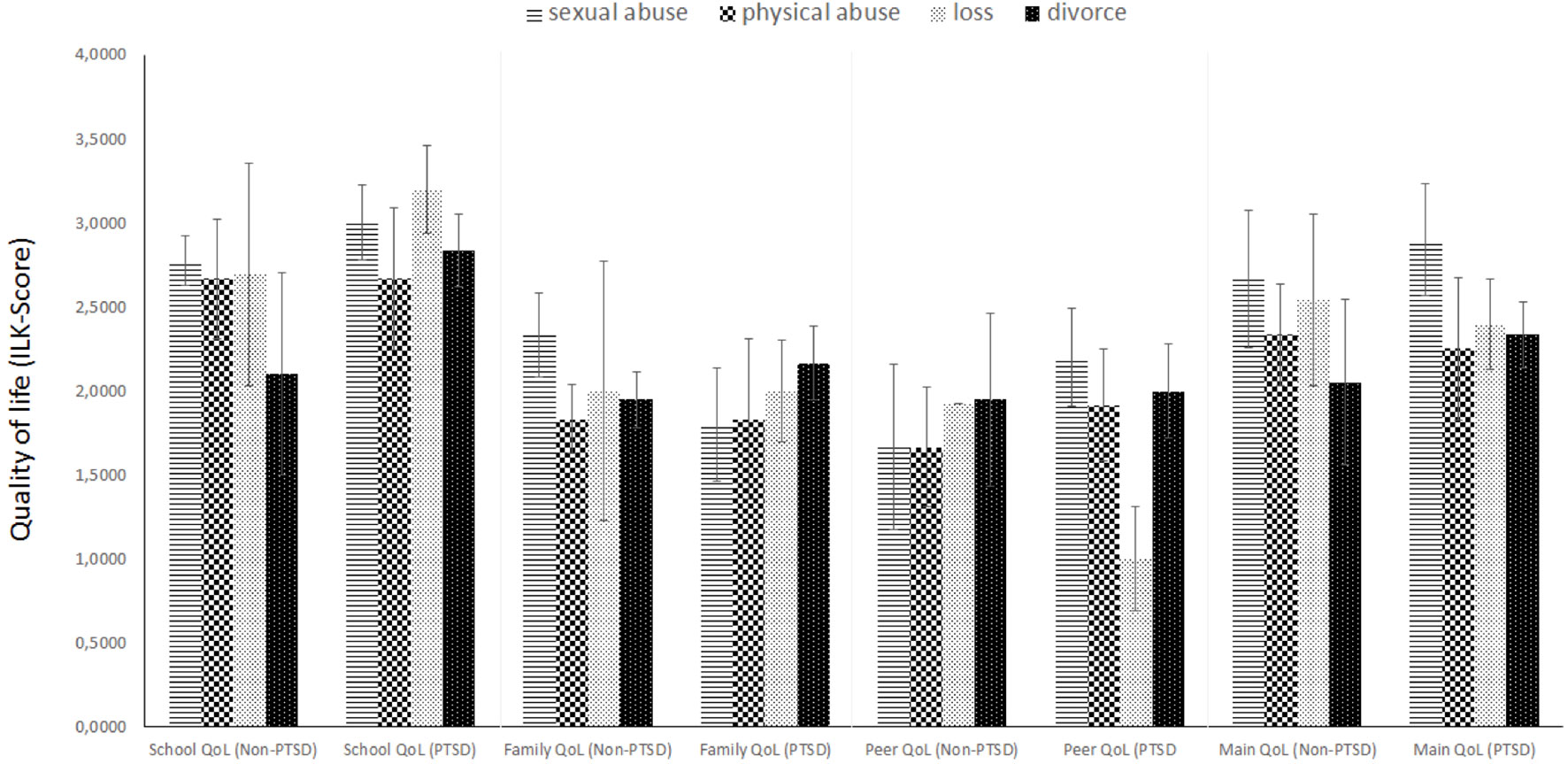
There was no difference in children’s QoL between the four different types of traumatic events; however, children with and without a PTSD diagnosis reported a significantly different QoL. Children with PTSD especially rated stressors related to the mental disorder as significantly higher than their non-PTSD diagnosed peers (F3,68 = 4.092; p = 0.047; par. η² = 0.054); in contrast, there were no group differences regarding stressors related to assessment or therapy. Moreover, children with PTSD described significantly more problems with their mental health (F3,72 = 9.698; p = 0.003; par. η² = 0.119). As shown in Figure 3, no group differences (either for trauma type or for PTSD diagnosis) were found regarding school, family, peer contacts, and main QoL assessment.
Discussion
The main objective of the study was to assess whether children and adolescents respond by different symptom patterns to four types of traumatic events and to assess QoL in both samples of PTSD and non-PTSD children and adolescents.
PTSD Symptomatology
First of all, the three DSM-IV symptom clusters discriminated well between the PTSD and non-PTSD groups, with PTSD subjects showing significantly more intrusive thoughts (criterion B), avoidance (criterion C), and hyperarousal (criterion D). When comparing the four trauma types, no group differences were found except for intrusion. Children and adolescents who experienced sexual abuse reported substantially more intrusive symptoms than children with a history of other traumatic experience regardless of whether those subjects were subsequently diagnosed with PTSD or not. Generally, the experience of sexual abuse showed the most consistent negative effects on most relevant symptom scales. For instance, sexual abuse victims reported most somatic complaints, most anxious and depressive symptoms, as well as thought problems, and they showed strongest social withdrawal when compared to the other groups. Additionally, children who were both diagnosed with PTSD and had a history of sexual assault were at double jeopardy of developing thought problems and being socially withdrawn. These results are generally in line with prior studies (19–21, 22, 49) and once again emphasize the particularly deleterious effects of sexual abuse on a child’s mental health.
In particular, the significantly heightened level of intrusive thoughts and thought problems in sexual abuse victims is a consistent finding across past studies (50).
PTSD Criteria in DSM 5
The current study was, as noted earlier, based on the DSM-IV criteria for PTSD as no appropriate, validated German DSM 5 assessment tools existed at the time of the study’s realization. Yet, in comparison to the DSM-IV, the DSM 5 (9) released in 2013 now entails 20 instead of 17 symptoms and four instead of the initial three symptom clusters. The avoidance criterion C was separated into two clusters, avoidance (criterion C) and negative alterations in cognitions and mood (criterion D).
First studies (51, 52) involving children aged 7–11 years reveal differences in PTSD diagnosis and low agreement between the two diagnostic systems. Also, the DSM 5 had low endorsement rates and identified fewer children than the three-cluster model in DSM-IV; in particular, the cognitions/mood and the avoidance clusters were found to preclude many children (51). The authors conclude that the nature of these clusters, and especially their emphasis on sophisticated cognition processes and internalization, may be inappropriate for preadolescent children. Similarly, the best model fit for children and adolescents was found for the three-cluster PTSD model proposed by ICD-11 (52) as opposed to the four-cluster model of the DSM 5 (53). Future studies should, thus, make a conscious effort to incorporate a developmental perspective that is sensitive to age-specific cognitive and emotional maturation processes (54). Given furthermore the trauma type specific symptom clusters found in this study, it is possible that symptom severity and presentation may vary as a function of not only age but also trauma type. Additional research is needed to further debunk these associations and shed more light onto the complex associations between type of trauma, age, and symptom presentation.
Crime Type-Related Symptom Patterns and QoL
When disentangling the differential effects of specific trauma types, very distinct symptom profiles for four trauma types can be found. Sexual abuse predominantly evokes internalizing symptoms such as social withdrawal and social problems as well as anxiety and depression. Also, children with a history of sexual abuse report more somatic complaints when compared to those who experienced a divorce or the loss of a parent. Depression and anxiety, in turn, are elevated especially in children who witnessed a divorce and subsequently develop PTSD symptoms. Finally, the afflicted tend to more frequently show oppositional or aggressive behavior, which may also result in delinquency.
The profiles found here correspond partly with results from other studies; yet, comparisons are difficult because, to our knowledge, no study has thus far directly compared the four trauma types considered here. Similar studies, however, found victims of sexual abuse to report above average overall PTSD cluster symptoms (avoidance, intrusion, and hyperarousal) but also to show more depressive and internalizing symptoms than victims of physical abuse (55). These specific symptom profiles may be used to inform forensic assessment as well as customized treatment for PTSD patients with different histories of traumatic experiences. For instance, the most afflicted group of sexual abuse victims may especially profit from high-frequency trauma-focused cognitive behavioral therapy with an emphasis on trauma narrative, cognitive coping, and trauma processing skills with a focus not only on PTSD symptoms but also on comorbid mental health problems (56).
Finally, results concerning QoL indicate that, while all four groups reported an equally low QoL, a PTSD diagnosis seems to adversely affect overall QoL. The significant difference in self-reported stressors relating to the mental disorder as well as mental health problems between PTSD patients and non-PTSD patients suggests a strong effect of PTSD symptoms alone on QoL. Comorbid disorders may be partialled out as both groups showed comparable comorbidities. Hence, children and adolescents are at a heightened risk of suffering from multiple drawbacks in many areas of life, a result that is in line with prior research (30).
Limitations of This Study and Considerations for Future Research
Our study was built solely on a sample of help-seeking, clinical clients. Future studies should also use healthy controls as a basis for further debunking the etiology of PTSD in children and adolescents (14). Additionally, gender could be taken up as a possible risk factor of PTSD symptom development (18). In the current study, gender was equally distributed across the groups; however, no conclusions can be drawn regarding the differential effect of trauma type on gender or gender-specific differences in symptom profiles. Also, we could not include further specific trauma features besides type of violence encountered such as frequency. This will undoubtedly pose a challenge for future research, especially when attempting to control for the confounding influence of multiple stressors often encountered in families with low socioeconomic status and a history of violence. At the same time, however, the choice to use the non-PTSD group of children and adolescents as controls helped to control for the influence of a traumatic experience, since all participants had a history of trauma. Also, it allowed for direct comparisons and for partialling out the mediating effect of comorbid disorders on QoL or on associated mental health problems.
Conclusion
We succeeded in showing that there is a distinct impact of trauma type on overall psychopathology with sexual abuse entailing the most debilitating consequences including, in particular, QoL for the affected individual. Also, PTSD symptoms in themselves have a wide-ranging effect on multiple areas of life, significantly diminishing the overall QoL of patients, indicating that the development of this disorder might be the most important predictor of low QoL. In assessment, care should be taken not to limit assessment of PTSD symptoms and presence or absence of clinical diagnosis, as well as to evaluate individual symptom patterns and their impact on QoL to better elucidate the specific impact of violent crimes and abuse.
A special challenge in different settings of forensic assessment will also be set by the marked differences between criteria using the different APA and WHO systems and their recent revisions that are based on highly diverse symptom clusters and different categorical models. This must be discussed when considering evaluation practices and standards. QoL or social functioning indicators and a better understanding of individual symptom profiles and their impact on everyday life might be a better means to understand impact and consequent needs for courts dealing with violence and abuse.
Further studies exploring the use of the different diagnostic systems, daily functioning, and QoL would be desirable.
Author Contributions
SV-K was the lead researcher and coordinator of the study. MK-P contributed as the main legal and victimology expert. AF, KS, and BH have assisted in the development of the project, contacted patients, and collected and inserted the data. OK contributed to data analysis. TW contributed in supervision, writing, data analysis, and final submission.
Funding
This study has been performed by means of the “Bürgermeister-Fonds” of the city of Vienna (Number: 2421).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. World Health Organization. The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Geneva: World Health Organization (1992). p. 147.
2. Kapella O, Baierl A, Rille-Pfeiffer C, Geserick C, Schmidt E, Schröttle M. Gewalt in der Familie und im nahen sozialen Umfeld: Österreichische Prävalenzstudie zur Gewalt an Frauen und Männern. Wien: Österreichisches Institut für Familienforschung an der Universität Wien (2011).
3. Riedesser P, Resch F, Adam H, Herpertz-Dahlmann B, Resch F, Schulte-Markwort M, et al. Entwicklungspsychotraumatologie. In: Herpertz-Dahlmann B, Resch F, Schulte-Markwort M, Warnke A, editors. Entwicklungspsychiatrie. Biopsychologische Grundlagen und die Entwicklung psychischer Störungen. Schattauer-Verlag (2008). p. 243–52.
4. Kolassa IT, Ertl V, Eckart C, Kolassa S, Onyut LP, Elbert T. Spontaneous remission from PTSD depends on the number of traumatic event types experienced. Psychol Trauma Theor Res Pract Policy (2010) 2(3):169–74. doi: 10.1037/a0019362
5. Terr LC. Childhood traumas: an outline and overview. Am J Psychiatry (1991) 148:10–20. doi: 10.1176/ajp.148.1.10
6. Elklit A. Victimization and PTSD in a Danish national youth probability sample. J Am Acad Child Adolesc Psychiatry (2002) 41(2):174–81. doi: 10.1097/00004583-200202000-00011
7. Galatzer-Levy IR, Bryant RA. 636,120 ways to have posttraumatic stress disorder. Perspect Psychol Sci (2013) 8:651–62. doi: 10.1177/1745691613504115
8. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association (2000).
9. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association (2013). doi: 10.1176/appi.books.9780890425596
10. Wenzel T, Frewer A, Mirzaei S. The DSM 5 and the Istanbul protocol: diagnosis of psychological sequels of torture. Torture (2015) 25(1):51–61. doi: 10.7146/torture.v25i1.109508
11. Üstün TB, Kostanjsek N, Chatterji S, Rehm J. Measuring health and disability: Manual for WHO Disability Assessment Schedule (WHODAS 2.0). Geneva: World Health Organization (2010).
12. Fairbank JA. The epidemiology of trauma and trauma related disorders in children and youth. PTSD Res Q (2008) 19(1):1–7. doi: 10.1037/e459392008-001
13. Collin-Vézina D, Coleman K, Milne L, Sell J, Daigneault I. Trauma experiences, maltreatment-related impairments, and resilience among child welfare youth in residential care. Int J Mental Health Addict (2011) 9(5):577–89. doi: 10.1007/s11469-011-9323-8
14. McCloskey LA, Walker M. Posttraumatic stress in children exposed to family violence and single-event trauma. J Am Acad Child Adolesc Psychiatry (2000) 39(1):108–15. doi: 10.1097/00004583-200001000-00023
15. Melhem NM, Walker M, Moritz G, Brent DA. Antecedents and sequelae of sudden parental death in offspring and surviving caregivers. Arch Pediatr Adolesc Med (2008) 162(5):403–10. doi: 10.1001/archpedi.162.5.403
16. Pine DS, Cohen JA. Trauma in children and adolescents: risk and treatment of psychiatric sequelae. Biol Psychiatry (2002) 51(7):519–31. doi: 10.1016/S0006-3223(01)01352-X
17. Silva RR, Alpert M, Munoz DM, Singh S, Matzner F, Dummit S. Stress and vulnerability to posttraumatic stress disorder in children and adolescents. Am J Psychiatry (2000) 157(8):1229–35. doi: 10.1176/appi.ajp.157.8.1229
18. Trickey D, Siddaway AP, Meiser-Stedman R, Serpell L, Field AP. meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clin Psychol Rev (2012) 32(2):122–38. doi: 10.1016/j.cpr.2011.12.001
19. Ackerman PT, Newton JE, McPherson WB, Jones JG, Dykman RA. Prevalence of post traumatic stress disorder and other psychiatric diagnoses in three groups of abused children (sexual, physical, and both). Child Abuse Neglect (1998) 22(8):759–74. doi: 10.1016/S0145-2134(98)00062-3
20. Bal S, Oost PV, Bourdeaudhuij ID, Crombez G. Avoidant coping as a mediator between self-reported sexual abuse and stress-related symptoms in adolescents. Child Abuse Neglect (2003) 27:883–97. doi: 10.1016/S0145-2134(03)00137-6
21. Fergusson DM, Boden JM, Horwood LJ. Exposure to childhood sexual and physical abuse and adjustment in early adulthood. Child Abuse Neglect (2008) 32(6):607–19. doi: 10.1016/j.chiabu.2006.12.018
22. Kelley LP, Weathers FW, Devitt-Murphy ME, Eakin DE, Flood AM. A comparison of PTSD symptom patterns in three types of civilian trauma. J Traumatic Stress (2009) 22(3):227–35. doi: 10.1002/jts.20406
23. Anthonysamy A, Zimmer-Gembeck MJ. Peer status and behaviors of maltreated children and their classmates in the early years of school. Child Abuse Neglect (2007) 31(9):971–91. doi: 10.1016/j.chiabu.2007.04.004
24. DePrince AP, Weinzierl KM, Combs MD. Executive function performance and trauma exposure in a community sample of children. Child Abuse Neglect (2009) 33(6):353–61. doi: 10.1016/j.chiabu.2008.08.002
25. Johnson J, Maxwell A, Galea S. The epidemiology of posttraumatic stress disorder. Psychiatr Ann (2009) 39(6):326–34. doi: 10.3928/00485713-20090514-01
26. Kitzmann KM, Gaylord NK, Holt AR, Kenny ED. Child witnesses to domestic violence: A meta-analytic review. J Consulting Clin Psychol (2003) 71(2):339–52. doi: 10.1037/0022-006X.71.2.339
27. Mersky JP, Reynolds AJ. Child maltreatment and violent delinquency: Disentangling main effects and subgroup effects. Child Maltreat (2007) 12(3):246–58. doi: 10.1177/1077559507301842
28. Prasad MR, Kramer LA, Ewing-Cobbs L. Cognitive and neuroimaging findings in physically abused preschoolers. Arch Dis Childhood (2005) 90(1):82–5. doi: 10.1136/adc.2003.045583
29. Putnam FW. Ten-year research update review: Child sexual abuse. J Am Acad Child Adolesc Psychiatry (2003) 42(3):269–78. doi: 10.1097/00004583-200303000-00006
30. Alisic E, Van der Schoot TA, van Ginkel JR, Kleber RJ. Looking beyond posttraumatic stress disorder in children: Posttraumatic stress reactions, posttraumatic growth, and quality of life in a general population sample. J Clin Psychiatry (2008) 69(9):1455–61. doi: 10.4088/JCP.v69n0913
31. Amir M, Lev-Wiesel R. (2003) Time does not heal all wounds: Quality of life and psychological distress of people who survived the Holocaust as children 55 years later. J Traumatic Stress (2003) 16(3):295–9. doi: 10.1023/A:1023756326443
32. Goenjian AK, Roussos A, Steinberg AM, Sotiropouloud C, Walling D, Kakaki M, et al. Longitudinal study of PTSD, depression, and quality of life among adolescents after the Parnitha earthquake. J Affective Disord (2013) 133(3):509–15. doi: 10.1016/j.jad.2011.04.053
33. Afifi TO, Enns MW, Cox BJ, de Graaf R, Have M, Sareen J. Child abuse and health-related quality of life in adulthood. J Nerv Mental Dis (2007) 195(10):797–804. doi: 10.1097/NMD.0b013e3181567fdd
34. Maercker A, Schützwohl M. Erfassung von psychischen Belastungsfolgen: Die Impact of Event Skala-revidierte Version (IES-R) [Assessment of post-traumatic stress reactions: The Impact of Event Scale-Revised (IES-R)]. Diagnostica (1998) 44(3):130–41. doi: 10.1037/t55092-000
35. Coker AL, Weston R, Creson DL, Justice B, Blakeney P. PTSD symptoms among men and women survivors of intimate partner violence: The role of risk and protective factors. Violence Vict (2005) 20(6):625–43. doi: 10.1891/0886-6708.20.6.625
36. Griffing S, Lewis CS, Chu M, Sage RE, Madry L, Primm BJ. Exposure to interpersonal violence as a predictor of PTSD symptomatology in domestic violence survivors. J Interpers Violence (2006) 21(7):936–54. doi: 10.1177/0886260506288938
37. Tsujiuchi T, Yamaguchi M, Masuda K, Tsuchida M, Inomata T, Kumano H, et al. High prevalence of post-traumatic stress symptoms in relation to social factors in affected population one year after the Fukushima nuclear disaster. PLOS One (2016) 11(3):e0151807. doi: 10.1371/journal.pone.0151807
38. Achenbach TM, Ruffle TM. The child behavior checklist and related forms of assessing behavioural/emotional problems and competencies. Pediatr Rev (2000) 21(8):365–271. doi: 10.1542/pir.21-8-265
39. Mattejat F, Simon B, Konig U, Quaschner K, Barchewitz C, Felbel D, et al. Quality of life of children and adolescents with psychiatric disorders. Results of the 1st multicenter study with an inventory to assess the quality of life in children and adolescents. Z Kinder Jugendpsychiatr Psychother (2003) 31(4):293–303. doi: 10.1024/1422-4917.31.4.293
40. Goessler UR, Bugert P, Bieback K, Huber K, Fleischer LI, Hormann K, et al. Differential modulation of integrin expression in chondrocytes during expansion for tissue engineering. In Vivo (2005) 19(3):501–7.
41. Fleischhaker C, Munz M, Bohme R, Sixt B, Schulz E. [Dialectical Behaviour Therapy for adolescents (DBT-A)—A pilot study on the therapy of suicidal, parasuicidal, and self-injurious behaviour in female patients with a borderline disorder]. Z Kinder Jugendpsychiatr Psychother (2006) 34(1):15–25. quiz 6-7. doi: 10.1024/1422-4917.34.1.15
42. Kiss E, Baji I, Mayer L, Skulteti D, Benak I, Vetro A. Validity and psychometric properties of a quality of life questionnaire in a Hungarian child and adolescent population. Psychiatr Hung (2007) 22(1):33–42.
43. Kiss E, Kapornai K, Baji I, Mayer L, Vetro A. Assessing quality of life: Mother–child agreement in depressed and non-depressed Hungarian. Eur Child Adolesc Psychiatry (2009) 18(5):265–73. doi: 10.1007/s00787-008-0727-3
44. Remschmidt H, Mattejat F. The quality of life of children and adolescents with ADHD undergoing outpatient psychiatric treatment: Simple disorders of activity and attention and hyperkinetic conduct disorders in comparison with each other and with other diagnostic groups. Atten Defic Hyperact Disord (2010) 2(4):161–70. doi: 10.1007/s12402-010-0036-9
45. Kamp-Becker I, Schroder J, Muehlan H, Remschmidt H, Becker K, Bachmann CJ. Health-related quality of life in children and adolescents with autism spectrum disorder. Z Kinder Jugendpsychiatr Psychother (2011) 39(2):123–31. doi: 10.1024/1422-4917/a000098
46. Balazs J, Miklosi M, Toro KT, Nagy-Varga D. Reading disability and quality of life based on both self- and parent-reports: importance of gender differences. Front Psychol (2016) 7:1942. doi: 10.3389/fpsyg.2016.01942
47. Wittchen HU, Wunderlich U, Gruschwitz S, Zaudig M. SKID-I. Strukturiertes Klinisches Interview für DSM-IV. Achse I: Psychische Störungen. Interviewheft und Beurteilungsheft. Eine deutschsprachige, erweiterte Bearbeitung der amerikanischen Originalversion des SKID I. Göttingen: Hogrefe (1997)
48. Mattejat F, Simon B, König U, Quaschner K, Barchewitz C, Felbel D, et al. Lebensqualität bei psychisch kranken Kindern und Jugendlichen: Ergebnisse der ersten multizentrischen Studie mit dem Inventar zur Erfassung der Lebensqualität bei Kindern und Jugendlichen (ILK). Zeitschrift für Kinder-und Jugendpsychiatrie und Psychotherapie (2003) 31(4):293–303. doi: 10.1024/1422-4917.31.4.293
49. Giaconia RM, Reinherz HZ, Silverman AB, Pakiz B, Frost AK, Cohen E. Traumas and posttraumatic stress disorder in a community population of older adolescents. J Am Acad Child Adolesc Psychiatry (1995) 34(10):1369–80. doi: 10.1097/00004583-199510000-00023
50. Dalenberg CJ, Brand BL, Gleaves DH, Dorahy MJ, Loewenstein RJ, Cardena E, et al. Evaluation of the evidence for the trauma and fantasy models of dissociation. Psychol Bull (2012) 138(3):550–88. doi: 10.1037/a0027447
51. Danzi BA, La Greca AM. DSM IV, DSM 5, and ICD 11: Identifying children with posttraumatic stress disorder after disasters. J Child Psychol Psychiatry (2016) 57(12):1444–52. doi: 10.1111/jcpp.12631
52. La Greca AM, Danzi BA, Chan SF. DSM-5 and ICD-11 as competing models of PTSD in preadolescent children exposed to a natural disaster: assessing validity and co-occurring symptomatology. Eur J Psychotraumatol (2017) 8(1). doi: 10.1080/20008198.2017.1310591
53. World Health Organization. ICD 11—Beta draft. Retrieved from: https://icd.who.int/dev11/l-m/en [16.11.2017].(2017)
54. Sachser C, Berliner L, Holt T, Jensen T, Jungbluth NJ, Risch EC, et al. Comparing the dimensional structure and diagnostic algorithms between DSM-5 and ICD-11 PTSD in children and adolescents. Eur Child Adolesc Psychiatry (2017) 27(2):1–10. doi: 10.1007/s00787-017-1032-9
55. Pynoos RS, Steinberg AM, Layne CM, Briggs EC, Ostrowski SA, Fairbank JA. DSM5 PTSD diagnostic criteria for children and adolescents: A developmental perspective and recommendations. J Traumatic Stress (2009) 22:391–8. doi: 10.1002/jts.20450
Keywords: forensic assessment, quality of life, posttraumatic stress disorder, children, adolescents, type of trauma
Citation: Voelkl-Kernstock S, Kletecka-Pulker M, Felnhofer A, Kothgassner OD, Skala K, Hansmann B and Wenzel T (2019) Psychopathology and Quality of Life in Traumatized or Victimized Underage Individuals as Factors for Forensic Multilevel Assessment—A Pilot Investigation. Front. Psychiatry 10:684. doi: 10.3389/fpsyt.2019.00684
Received: 13 September 2018; Accepted: 23 August 2019;
Published: 18 September 2019.
Edited by:
Thomas Nilsson, University of Gothenburg, SwedenReviewed by:
Peter Andiné, University of Gothenburg, SwedenIoanna Giannopoulou, National and Kapodistrian University of Athens, Greece
Copyright © 2019 Voelkl-Kernstock, Kletecka-Pulker, Felnhofer, Kothgassner, Skala, Hansmann and Wenzel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sabine Voelkl-Kernstock, c2FiaW5lLnZvZWxrbC1rZXJuc3RvY2tAbWVkdW5pd2llbi5hYy5hdA==
 Sabine Voelkl-Kernstock
Sabine Voelkl-Kernstock Maria Kletecka-Pulker
Maria Kletecka-Pulker Anna Felnhofer
Anna Felnhofer Oswald David Kothgassner
Oswald David Kothgassner Katrin Skala1
Katrin Skala1 Thomas Wenzel
Thomas Wenzel