- 1Department of Clinical Epidemiology, Translational Medical Center, National Center of Neurology and Psychiatry, Kodaira, Japan
- 2Department of Neuropsychiatry, Hirosaki University School of Medicine, Hirosaki, Japan
Decisional capacity to consent is an emerging ethical and legal concept, and is closely related to self-determination of patients facing important medical decisions or research participations. Recently, the MacArthur Competence Assessment Tool (MacCAT), a semi-structured interview consisting of four dimensions (Understanding, Appreciation, Reasoning, and Expression of a Choice), was developed to assess the decisional capacity. Decision-making capacity in a group of patients with schizophrenia, as measured by the MacCAT, has been shown to be impaired in comparison with healthy control people. However, this does not necessarily mean the presence of impaired decisional capacity in all cases. Considering the real-world practice of obtaining informed consent from patients with schizophrenia, it is important to evaluate the relationship between psychopathological features and decisional capacity of the illness. Negative symptoms of schizophrenia have been demonstrated to be related to the ability to understand information relevant to the decision, reason rationally, and appreciate a situation and its consequences. On the other hand, positive symptoms, such as delusions and hallucinations have been an inconsistent correlate of poor capacity. Furthermore, some studies indicate that impairment of cognitive function, a core symptom of schizophrenia, could be more largely associated with decisional capacity than positive and negative symptoms. Therefore, it is reasonable to assume cognitive enhancement would enlarge the capacity to consent and promote autonomy in medical treatment and research participation in patients with schizophrenia. Further studies are warranted to elucidate this and related issues.
Introduction
Competence to consent for individuals with psychiatric symptoms or impaired cognitive functioning has become central to the debate on the informed consent in clinical care and research settings. Clinicians and researchers bear the responsibilities to protect two aspects of human rights; the right of competent patients to make choices about their medical care and the right of incompetent patients to be protected from the potential harm of their decisions (1). However, in real-world clinical settings, some patients with capacity were detained in hospital by law, or other patients with incapacity were admitted to hospital on a voluntary basis (2). In terms of clinical research, some patients with incapacity might have participated in clinical trials with their own consent.
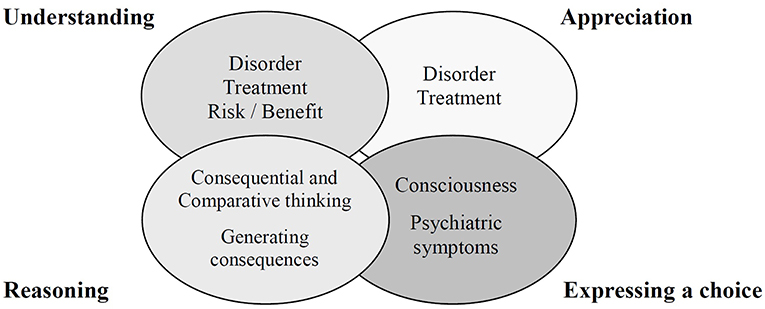
Although several decision-making tasks specifically assess decisional capacities (3, 4), the medical/psychiatric literature has commonly cited the following abilities as relevant to capacity for informed consent: (1) understanding information relevant to treatment decision making; (2) appreciating the personal significance of treatment information, especially concerning one's own illness and the probable consequences of one's treatment options; (3) reasoning with relevant information to engage in a logical process of weighting treatment options; and (4) expressing a choice (5). These are also the key elements of the MacArthur Competence Assessment Tool (MacCAT) (6) (Figure 1), which has been widely used for competence assessment (7). However, the MacCAT is not clearly designed to provide a total score for the assessment of decision-making capacity. Furthermore, the abilities assessed in the MacCAT do not necessarily equate to the abilities relevant to the assessment of decision-making capacity in many jurisdictions.
Schizophrenia is a severe mental disorder that generally appears in late adolescence or early adulthood. Epidemiological data indicates that prevalence of schizophrenia is approximately 1% in the worldwide population. Symptoms of schizophrenia are clinically divided into three main categories of positive symptoms (delusions, disordered thoughts, and hallucinations), negative symptoms (restricted affect and drive), and impairments in cognitive function (8, 9). When schizophrenia was first identified by Kraepelin, he noted the fundamental role of cognitive impairment in this disorder, and called this dementia praecox (10). Although patients with schizophrenia are more likely to lack the competence to consent than control groups (6, 11), the diagnosis of schizophrenia cannot be equated with decisional incapacity (12). Many researchers have investigated the associations of competence to consent with positive and negative symptoms of schizophrenia (13–15). Although poor capacity has correlated with negative symptoms more consistently than positive symptoms, high levels of positive symptoms, including disorganization, may affect competence to consent. Furthermore, recent empirical data suggest that neurocognitive functioning could explain a larger proportion of the variance in competence to consent than positive and negative symptoms of schizophrenia (14, 16, 17).
Therefore, the aim of this narrative review is to elucidate (1) the relationships between cognitive function and competence to consent, and (2) the interventions to compensate the decision-making capacity in patients with schizophrenia.
Cognitive Measures of Multiple Domains and Competence to Consent
Several studies investigated the association of competence to consent and cognitive measures such as the Mini-Mental State Examination (MMSE) (15, 17–19) and the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) (13, 16). On the whole, poor understanding subscales of MacCAT have been a more consistent correlate of poor cognitive functioning than have other subscales. However, all of above mentioned studies employed MacCAT-Clinical Research (MacCAT-CR) for assessing participants' decision-making abilities for clinical research. So, the potential range of understanding subscales being at least three times those of the other subscales might affect inconsistent results of other subscales.
A longitudinal assessment for capacity, in terms of understanding, was conducted among participants in the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia study (20). Over 18 months treatment, poorer baseline neurocognitive composite scores consisting of processing speed, verbal memory, vigilance, reasoning, and working memory, predicted falling below the critical decision-making capacity threshold. In the same analysis, lower baseline scores of understanding subscale also were associated with falling below the threshold during follow-up period.
Cognitive Measures of Each Domain and Competence to Consent
Verbal communication plays an important role in informed consent (21). Two studies demonstrated the relationship between understanding subscales and verbal cognitive functioning based on the Wechsler Adult Intelligence Scale (WAIS)-Revised (WAIS-R) (22, 23). In addition, other studies showed that appreciation and reasoning subscales are associated with verbal comprehension composed of vocabulary, similarities, and information subtests from the WAIS–Third Edition (WAIS-III) (17, 24). Although previous studies indicated that verbal abilities may predict competence to consent, the relationship between specific dimensions of decisional capacity and individual verbal ability areas is still obscure.
Memory is a complex process, consisting of registration, storage, retainment, and retrieval of information (25). Previous studies from US revealed that the RBANS memory index had significant relationships to understanding, appreciation (13) and reasoning subscales (16). Another study from Hong Kong indicated an association of understanding subscales with immediate and delayed logical memory from the Wechsler Memory Scale (WMS) (5). Furthermore, some studies implicated that memory also underlies an aspect of learning outcome (17, 24). Palmer et al. showed the relationship of learning composite scores with three subscales of MacCAT (understanding, appreciation, and reasoning) (24). They also demonstrated that auditory and visual learning abilities could affect the competence to consent (17).
Working memory is a complex and multifaced construct to store and simultaneously manipulate a limited amount of information during short intervals. This capacity facilitates further cognitive processing, such as response selection relevant for a specific context. Working memory comprises two short-term information storage systems, the visuospatial network for visual material and the phonologic loop for verbal-acoustic material (25). In the CATIE schizophrenia trial (14), this cognitive domain was assessed by a computerized test of visuospatial working memory and letter number sequencing test of auditory working memory. Specifically, working memory performance showed considerable bivariate relationships with the understanding, appreciation, and reasoning subscale scores from the MacCAT-CR. Furthermore, similar results were reported in other studies employing the letter number sequencing test (5) and WAIS-III (17). A previous study indicated an association between language comprehension and working memory for sentences (26). Impairment of working memory in patients with schizophrenia might be consequent upon verbal comprehension deficits.
Information processing represents a cognitive process of taking information and encoding it to be understood and recalled when appropriately cued. Processing speed is the rapidity by which information processing occurs (25). Several studies showed bivariate correlation between processing speed composite scores and understanding, appreciation, and reasoning subscales of MacCAT (14, 17, 24), but only the relationship between processing speed composite scores and understanding subscales was replicated in a multiple regression model (14). In patients with schizophrenia, processing speed performance is strongly associated with global cognitive deficits (27). Thus, processing speed may contribute to the relationship between competence to consent and general cognitive performance.
Executive function involves the simultaneous use of information rather than the basic cognitive process, and governs goal-directed behaviors or adaptive responses to complex or novel situations. Generally, executive function is characterized by several complex mental abilities, including unique skills used for expansion, modulation, and implementation of goal-directed activities (25). This domain of cognitive function has been thought to rely on frontal lobe functions (28). A positive correlation has been reported between performance on the Frontal Assessment Battery and total scores of the MacCAT (29) in chronic schizophrenia patients. Specifically, scores on the understanding subscale were most consistently correlated with executive function (5, 24).
Cognitive underpinnings underlying the limited decisional capacity in psychiatric patients remain to be explored (30). One intriguing study (31) showed that performance on a metacognition test was more closely related to decisional capacity compared to executive function. Metacognition focuses on the level of self-confidence of patients in comparison with actual performance, and predicts performance on the MacCAT-T (31).
Interventions to Compensate the Decision-Making Capacity
Although antipsychotic medication may improve decisional capacities (32, 33), clinicians and researchers should improve the informed consent process to maximize the decision-making capacities of patients with schizophrenia. Providing information repeatedly and discussing presented information with participants may strengthen the competence to consent (16, 34). Furthermore, consent procedures via multimedia may facilitate the understanding to decide on complex or high-risk protocols (35). Naughton et al. conducted a small uncontrolled study to evaluate the effect of metacognitive training (MCT) to improve a person's awareness of cognitive biases and thinking styles on decision-making capacities (36). MCT was found to elicit improvement in understanding and reasoning, but not appreciation abilities of patients. Furthermore, cognitive remediation may improve competence to consent (37), providing ethically adequate care, as well as clinical improvement.
Limitations
Several limitations of this review should be acknowledged. The principal limitation is the relatively small sample sizes in most studies, mentioned here, on the relationship between cognitive function and competence to consent in patients of schizophrenia. Secondly, for ethical and legal reasons, only subjects who consented to participate in studies were included. Even among individuals who consented to participate, 10% were too agitated to complete the entire assessments (6), suggesting that generalization of previous findings should be considered with caution. Thirdly, the MacCAT does not have a specific cutoff to dichotomize competence vs. incompetence. This may obscure the associations between cognitive functions and decisional capacities (38). Finally, the MacCAT, which is based on not only medical literature but also existing case law and statutes, does not assess the emotional aspect of decisional capacities. Further studies investigating the relationship between cognitive function and decisional capacities, including both comprehensive emotional and legal aspects, are needed.
Conclusions
Neurocognitive functioning may explain competence to consent more accurately than positive and negative symptoms. Previous results have not indicated differential relationships between specific cognitive ability areas and decision-making capacity. Interventions with multimedia procedure, MCT, etc. likely enhance competence to consent. Cognitive remediation might provide ethically adequate care as well as clinical improvement. Clinicians and researchers are responsible for maximizing decision-making capacities of patients in the informed consent process. Further studies are warranted to elucidate competence to consent and related issues.
Author Contributions
NS, NY-F, and TS were involved in the study concept, interpretation of manuscript, critical revision of manuscript for intellectual content, literature review, and drafting of the manuscript.
Funding
Funding for this study was provided by a Grant-in-Aid for Scientific Research (C) (17K10347). The Ministry of Education, Culture, Sports, Science and Technology, Japan.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This research was well supported by staffs of Translational Medical Center.
References
1. Grisso T, Appelbaum P. Assessing Competence to Consent to Treatment. A Guide for Physicians and Other Health Professionals. New York, NY: Oxford University Press (1998).
2. Owen GS, Szmukler G, Richardson G, David AS, Hayward P, Rucker J, et al. Mental capacity and psychiatric in-patients: implications for the new mental health law in England and Wales. Br J Psychiatry. (2009). 195:257–63. doi: 10.1192/bjp.bp.108.059782.
3. Toplak ME, Sorge GB, Benoit A, West RF, Stanovich KE. Decision-making and cognitive abilities: a review of associations between Iowa Gambling Task performance, executive functions, and intelligence. Clin Psychol Rev. (2010). 30:562–81. doi: 10.1016/j.cpr.2010.04.002.
4. Manes F, Torralva T, Ibáñez A, Roca M, Bekinschtein T, Gleichgerrcht E. Decision-making in frontotemporal dementia: clinical, theoretical and legal implications. Dement Geriatr Cogn Disord. (2011). 32:11–7. doi: 10.1159/000329912
5. Wong JG, Cheung EP, Chen EY. Decision-making capacity of inpatients with schizophrenia in Hong Kong. J Nerv Ment Dis. (2005). 193:316–22. doi: 10.1097/01.nmd.0000161685.54077.e4
6. Grisso T, Appelbaum PS, Hill-Fotouhi C. The MacCAT-T: a clinical tool to assess patients' capacities to make treatment decisions. Psychiatr Serv. (1997). 48:1415–9. doi: 10.1176/ps.48.11.1415
7. Wang SB, Wang YY, Ungvari GS, Ng CH, Wu RR, Wang J, et al. The MacArthur competence assessment tools for assessing decision-making capacity in schizophrenia: a meta-analysis. Schizophr Res. (2017). 183:56–63. doi: 10.1016/j.schres.2016.11.020
10. McGlashan TH. Eugen Bleuler: centennial anniversary of his 1911 publication of Dementia Praecox or the group of schizophrenias. Schizophr Bull. (2011). 37:1101–3. doi: 10.1093/schbul/sbr130
11. Jeste DV, Depp CA, Palmer BW. Magnitude of impairment in decisional capacity in people with schizophrenia compared to normal subjects: an overview. Schizophr Bull. (2006). 32:121–8. doi: 10.1093/schbul/sbj001
12. Okai D, Owen G, McGuire H, Singh S, Churchill R, Hotopf M. Mental capacity in psychiatric patients: Systematic review. Br J Psychiatry. (2007). 191:291–7. doi: 10.1192/bjp.bp.106.035162
13. Moser DJ, Schultz SK, Arndt S, Benjamin ML, Fleming FW, Brems CS, et al. Capacity to provide informed consent for participation in schizophrenia and HIV research. Am J Psychiatry. (2002). 159:1201–7. doi: 10.1176/appi.ajp.159.7.1201
14. Stroup S, Appelbaum P, Swartz M, Patel M, Davis S, Jeste D, et al. Decision-making capacity for research participation among individuals in the CATIE schizophrenia trial. Schizophr Res. (2005). 80:1–8. doi: 10.1016/j.schres.2005.08.007
15. Lan TH, Wu BJ, Chen HK, Liao HY, Lee SM, Sun HJ. Validation of chinese version of the MacArthur competence assessment tool for clinical research (MacCAT-CR) in patients with schizophrenia spectrum disorders. Psychiatry Res. (2013). 210:634–40. doi: 10.1016/j.psychres.2013.07.002
16. Carpenter WT Jr, Gold JM, Lahti AC, Queern CA, Conley RR, Bartko JJ, et al. Decisional capacity for informed consent in schizophrenia research. Arch Gen Psychiatry. (2000). 57:533–8. doi: 10.1001/archpsyc.57.6.533
17. Palmer BW, Dunn LB, Appelbaum PS, Jeste DV. Correlates of treatment-related decision-making capacity among middle-aged and older patients with schizophrenia. Arch Gen Psychiatry. (2004). 61:230–6. doi: 10.1001/archpsyc.61.3.230
18. Palmer BW, Dunn LB, Appelbaum PS, Mudaliar S, Thal L, Henry R, et al. Assessment of capacity to consent to research among older persons with schizophrenia, Alzheimer disease, or diabetes mellitus: comparison of a 3-item questionnaire with a comprehensive standardized capacity instrument. Arch Gen Psychiatry. (2005). 62:726–33. doi: 10.1001/archpsyc.62.7.726
19. Wu BJ, Liao HY, Chen HK, Lan TH. Psychopathology, psychopharmacological properties, decision-making capacity to consent to clinical research and the willingness to participate among long-term hospitalized patients with schizophrenia. Psychiatry Res. (2016). 237:323–30. doi: 10.1016/j.psychres.2016.01.020
20. Stroup TS, Appelbaum PS, Gu H, Hays S, Swartz MS, Keefe RS, et al. Longitudinal consent-related abilities among research participants with schizophrenia: results from the CATIE study. Schizophr Res. (2011). 130:47–52. doi: 10.1016/j.schres.2011.04.012.
21. Merz JF, Druzdzel MJ, Mazur DJ. Verbal expressions of probability in informed consent litigation. Med Decis Making. (1991). 11:273–81. doi: 10.1177/0272989X9101100405
22. Grisso T, Appelbaum PS. The MacArthur treatment competence study. III: abilities of patients to consent to psychiatric and medical treatments. Law Hum Behav. (1995). 19:149–74.
23. Kovnick JA, Appelbaum PS, Hoge SK, Leadbetter RA. Competence to consent to research among long-stay inpatients with chronic schizophrenia. Psychiatr Serv. (2003). 54:1247–52. doi: 10.1176/appi.ps.54.9.1247
24. Palmer BW, Jeste DV. Relationship of individual cognitive abilities to specific components of decisional capacity among middle-aged and older patients with schizophrenia. Schizophr Bull. (2006). 32:98–106. doi: 10.1093/schbul/sbj002
25. Kar SK, Jain M. Current understandings about cognition and the neurobiological correlates in schizophrenia. J Neurosci Rural Pract. (2016). 7:412–8. doi: 10.4103/0976-3147.176185
26. Condray R, Steinhauer SR, van Kammen DP, Kasparek A. Working memory capacity predicts language comprehension in schizophrenic patients. Schizophr Res. (1996). 20:1–13. doi: 10.1016/0920-9964(95)00061-5
27. Keefe RS, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L. The brief assessment of cognition in schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res. (2004). 68:283–97. doi: 10.1016/j.schres.2003.09.011
28. Eisenberg DP, Berman KF. Executive function, neural circuitry, and genetic mechanisms in schizophrenia. Neuropsychopharmacology. (2010). 35:258–77. doi: 10.1038/npp.2009.111
29. Linder M, Lev-Ari L, Kurs R, Melamed Y. Evaluation of the capacity of inpatients with chronic schizophrenia to provide informed consent for participation in clinical trials; use of the Hebrew version of the MacArthur competence assessment tool for clinical research (MacCAT-CR). Isr Med Assoc J. (2012). 14:470–4.
30. Palmer BW, Savla GN. The association of specific neuropsychological deficits with capacity to consent to research or treatment. J Int Neuropsychol Soc. (2007). 13:1047–59. doi: 10.1017/S1355617707071299
31. Koren D, Poyurovsky M, Seidman LJ, Goldsmith M, Wenger S, Klein EM. The neuropsychological basis of competence to consent in first-episode schizophrenia: a pilot metacognitive study. Biol Psychiatry. (2005). 57:609–16. doi: 10.1016/j.biopsych.2004.11.029
32. Dornan J, Kennedy M, Garland J, Rutledge E, Kennedy HG. Functional mental capacity, treatment as usual and time: magnitude of change in secure hospital patients with major mental illness. BMC Res Notes. (2015). 8:566. doi: 10.1186/s13104-015-1547-4
33. Owen GS, Ster IC, David AS, Szmukler G, Hayward P, Richardson G, Hotopf M. Regaining mental capacity for treatment decisions following psychiatric admission: a clinico-ethical study. Psychol Med. (2011). 41:119–28. doi: 10.1017/S0033291710000383
34. Palmer BW, Nayak GV, Dunn LB, Appelbaum PS, Jeste DV. Treatment-related decision-making capacity in middle-aged and older patients with psychosis: a preliminary study using the MacCAT-T and HCAT. Am J Geriatr Psychiatry. (2002). 10:207–11. doi: 10.1097/00019442-200203000-00012
35. Jeste DV, Palmer BW, Golshan S, Eyler LT, Dunn LB, Meeks T, et al. Multimedia consent for research in people with schizophrenia and normal subjects: a randomized controlled trial. Schizophr Bull. (2009). 35:719–29. doi: 10.1093/schbul/sbm148
36. Naughton M, Nulty A, Abidin Z, Davoren M, O'Dwyer S, Kennedy HG. Effects of group metacognitive training (MCT) on mental capacity and functioning in patients with psychosis in a secure forensic psychiatric hospital: a prospective-cohort waiting list controlled study. BMC Res Notes. (2012). 5:302. doi: 10.1186/1756-0500-5-302
37. Vingerhoets WA, Bloemen OJ, Bakker G, van Amelsvoort TA. Pharmacological interventions for the MATRICS cognitive domains in schizophrenia: what's the evidence? Front Psychiatry. (2013). 4:157. doi: 10.3389/fpsyt.2013.00157
38. Dunn LB, Palmer BW, Appelbaum PS, Saks ER, Aarons GA, Jeste DV. Prevalence and correlates of adequate performance on a measure of abilities related to decisional capacity: differences among three standards for the MacCAT-CR in patients with schizophrenia. Schizophr Res. (2007). 89:110–8. doi: 10.1016/j.schres.2006.08.005
Keywords: competence to consent, cognitive function, schizophrenia, MacArthur Competence Assessment Tools, decisional capacity
Citation: Sugawara N, Yasui-Furukori N and Sumiyoshi T (2019) Competence to Consent and Its Relationship With Cognitive Function in Patients With Schizophrenia. Front. Psychiatry 10:195. doi: 10.3389/fpsyt.2019.00195
Received: 30 November 2017; Accepted: 18 March 2019;
Published: 12 April 2019.
Edited by:
Renzo Bianchi, University of Neuchâtel, SwitzerlandReviewed by:
Julio Eduardo Armijo, Diego Portales University, ChileChristopher James Ryan, University of Sydney, Australia
Copyright © 2019 Sugawara, Yasui-Furukori and Sumiyoshi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Norio Sugawara, bnNuZ2FAbmNucC5nby5qcA==
 Norio Sugawara
Norio Sugawara Norio Yasui-Furukori2
Norio Yasui-Furukori2 Tomiki Sumiyoshi
Tomiki Sumiyoshi