- 1Department of Occupational Health Practice and Management, Institute of Industrial Ecological Sciences, University of Occupational and Environmental Health, Kitakyushu, Japan
- 2Data Science Center for Occupational Health, University of Occupational and Environmental Health, Kitakyushu, Japan
- 3Department of Public Health, Kitasato University School of Medicine, Sagamihara, Japan
- 4Department of Preventive Medicine and Community Health, School of Medicine, University of Occupational and Environmental Health, Kitakyushu, Japan
Objective: The aim of this study was to examine how attention-deficit hyperactivity disorder (ADHD) symptoms play an interaction effect on the association between psychosocial work environments and health (psychological distress/work engagement) among workers.
Methods: This is a cross-sectional study of 2,693 employees at a pharmaceutical company using a self-administered questionnaire evaluating ADHD symptoms (Adult ADHD Self-Report Scale Screener), psychosocial work environments (job demands, job control and social support), and health outcomes (psychological distress; K6, and work engagement; Utrecht Work Engagement Scale). Multiple regression analyses were applied to assess the interaction between ADHD symptoms and psychosocial work environments on health outcomes.
Results: The prevalence of workers with ADHD symptoms was 5.9% (n = 159). Significant interaction effects of ADHD symptoms × job control and ADHD symptoms × social support were observed (β = −0.067, p < 0.01 and β = −0.052, p < 0.01, respectively) on psychological distress after adjustment of age, sex, occupation and education. The interaction effect of ADHD symptoms × each psychosocial work environment was not observed on work engagement.
Conclusions: Job control and social support were more influential factors that were related to psychological distress in accordance with ADHD symptoms. This study also found no difference of the interaction between psychosocial work environments and ADHD symptoms on work engagement. To the best of our knowledge, this study was first to clarify the effect of ADHD symptoms on the association between psychosocial work environments and health outcomes (psychological distress/work engagement). These findings can aid employers how to arrange better work environments for workers with ADHD symptoms.
Introduction
Attention-deficit hyperactivity disorder (ADHD) is a neuropsychiatric disorder characterized by inattention, excessive motor activity, and impulsivity. ADHD starts in childhood and can persist into adolescence and adulthood (1, 2). Adults with ADHD experience difficulties in social interactions and are more likely to suffer from depression and social anxiety disorder (2). Workers with ADHD tend to show work impairment and reduced productivity (e.g., absenteeism and presenteeism) (3). Furthermore, adults with ADHD are at increased risk of accidents, trauma, and workplace injuries (4).
Individuals with ADHD are common in the workplace. An estimated 1.9–4.2% of workers are reported to have adult ADHD in the United States, and an average of 3.5% was found among workers in 10 countries (i.e., Belgium, Colombia, France, Germany, Italy, Lebanon, Mexico, the Netherlands, Spain, and the United States) (5–7). Moreover, it is known that ADHD symptoms exist on a continuum, and therefore there are people with subthreshold ADHD. Similar to adults with ADHD, those with subthreshold ADHD are also at risk of adverse outcomes (8, 9). It is likely that some workers with mental disorders have undiagnosed ADHD or subthreshold ADHD (10, 11), and these individuals with ADHD symptoms may be at a higher risk for developing a mental health disorder.
The mental health of workers is associated with the psychosocial work environments. The past study indicated that unfavorable psychosocial work environments, such as high job demands, low job control and low social support are associated with psychological distress of workers (12). It was known that high job demands and low job control are prospective risk factors for common mental disorders (12, 13). Psychosocial work environments affect not only poor health, but also positive aspects of health such as work engagement. Work engagement is of strong interest to employers because lower work engagement leads to greater loss of productivity (14). High job control and high social support are intrinsically and/or extrinsically motivating and therefore taken as the primary drivers of work engagement (15–18). Adults with ADHD symptoms such as hyperactivity-impulsivity and inattention (1) tend to experience problems with working memory, planning, and anticipation (19, 20). These deficits are closely linked to the ability to function at work (21–23). The past qualitative study suggested that coping with workload is a key point for employed women with ADHD to success in employment (24). This suggests that psychosocial work environments are more important key factors to fit to work for workers with ADHD symptoms. To the best of our knowledge, however, it is not clear what role ADHD symptoms would play in the relationships between psychosocial work environments and negative/positive well-being as the health outcome.
The purpose of this study was to investigate how ADHD symptoms modify the relationship psychosocial work environments and negative/positive aspects of mental health (psychological distress/work engagement) for workers.
We have two hypotheses.
Hypothesis 1. ADHD symptoms enhance the association between low job control and psychological distress.
Workers with ADHD symptoms have the difficulty to follow the instructions of others (25), and then job control might be more important factor to fit to work among workers with ADHD symptoms.
Hypothesis 2. ADHD symptoms enhance the association between high job control and work engagement.
Adults with ADHD tend to be resilient and creative, to have foresight, and to generate ideas (26). Workers with ADHD often have the entrepreneurship and professionalism (27). ADHD may offer performance advantages in entrepreneurial environments or in professions where rapid decision making or creativity is required (26–28). Job control is high in these professions. That is why the association between high job control and work engagement may be stronger among workers with ADHD symptoms.
In addition to two hypotheses, we conducted the exploratory analyses to investigate how ADHD symptoms modify the relationship other psychosocial work environments (job demands and social support) and health for workers.
Methods
Participants
We distributed self-administered questionnaires to employees of a pharmaceutical company. Participation was voluntary. Company health care staff sent an email in September 2016 to all employees (n = 4,738; male = 3,361, female = 1,377) to inform them about the study and encourage them to complete the questionnaire. The questionnaire included psychosocial work environments, psychological distress, work engagement, and the Adult ADHD Self-Report Scale short version (ASRS screener) (29). Only the researchers had access to results of the questionnaire (the company staff did not).
The research protocol was approved by the Ethics Committee of Medical Research, University of Occupational and Environmental Health, Japan.
Measures
ADHD
The short-form ASRS Screener is available in many languages and comprises a checklist of six questions about ADHD symptoms based on the diagnostic criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (30). Respondents rate the frequency with which individual ADHD symptoms have occurred over the past 6 months using a five-point Likert scale (0 = never, 1 = rarely, 2 = sometimes, 3 = often, and 4 = very often). Response scores are equally weighted and summed to generate a total score ranging from 0 to 24, with higher scores indicating an increased risk of ADHD. Cronbach's alpha coefficient was 0.61 for this sample. To screen for ADHD, dichotomous responses to each of the six questions were counted; respondents who made a positive response in 4 or more questions were considered to have a positive screening (29), and were placed in the workers with ADHD symptoms. To examine the interaction between the severity of ADHD symptoms and psychosocial work environments, total ASRS score was used.
Psychosocial Work Environments
We used the Brief Job Stress Questionnaire (BJSQ) to measure job stressors (31). The BJSQ is a standardized instrument used to assess social and psychological characteristics of jobs based on the job stress model developed by the group of researchers from the US National Institute for Occupational Safety and Health (NIOSH) (31). We assessed three work components in the BJSQ: job demands (six items), job control (three items), and social support at the workplace (six items). There are four response options to each question, ranging from strongly agree to strongly disagree.
Job demands include qualitative job overload (three items) and quantitative job overload (three items). Total possible score ranges from 6 to 24. Job control consists of three items, and the total possible score for job control ranges from 3 to 12. Social support at the workplace includes supervisor support (three items) and coworker support (three items), with total possible scores ranging from 6 to 24. Cronbach's alpha coefficient of job demands, job controls, and social support were 0.79, 0.83, and 0.88, respectively.
Outcome: Psychological Distress
Psychological distress was measured using the Japanese version of the K6 scale, which has demonstrated acceptable internal consistency, reliability, and validity (32). The K6 scale comprises six items measuring psychological distress level on a five-point scale ranging from 0 (none of the time) to 4 (all of the time) (total score range: 0–24). Cronbach's alpha coefficient for this sample was 0.89.
Outcome: Work Engagement
Work engagement was assessed using the nine-item Japanese version of the Utrecht Work Engagement Scale (UWES-9) (33). The UWES-9 was developed in order to measure the characteristics of vigor, dedication, and absorption. Items are rated on a seven-point response scale, from 0 (never) to 6 (always), resulting in a total score ranging from 0 to 54. The Japanese translation of the UWES-9 has demonstrated acceptable internal consistency reliability, as well as factor and construct validity (34). Cronbach's alpha coefficient for this sample was 0.95.
Demographic Characteristics
The questionnaire also measured the following demographic characteristics: sex, age, education, and occupation. Age was used as a continuous variable. Education was categorized into four groups (less than 12 years, 12–14 years, 16–18 years, and more than 18 years). Occupation was categorized into six groups based on the categories established in the International Standard Classification of Occupation: supervisory, clerical, blue collar, sales, research, and technical. Dummy variables were created using the clerical category as a reference.
Statistical Analysis
We calculated means and standard deviations, or proportion of the demographic characteristics of participants. To assess for interaction between the severity of ADHD symptoms and psychosocial work environments, we conducted multiple regression analyses using ASRS totals as continuous variables among all participants. Prior to testing, the total ASRS, job demands, job control, and social support scores were mean-centered. ASRS scores, job demands × ASRS, job control × ASRS, and social support × ASRS were included as independent variables. Psychological distress and work engagement were used as dependent variables. We first conducted a crude model (Model 1), then adjusted for age and sex to generate a second model (Model 2). Psychosocial work environments differ depending on occupation, and health outcomes differ depending on socioeconomic status such as education. To confirm the consistency of results, we created additional models adjusted for occupation (Model 3), and education (Model 4). When significant interaction effects of psychosocial work environments × ASRS were observed, we conducted post-hoc simple slope analyses at one standard deviation above/below the mean score of ASRS scores. In a series of analyses, R2, adjusted R2, and ΔR2 were calculated in each step to assess model fit. In addition, residual analyses were conducted to estimate the amount of autocorrelation in the residuals using the Durbin-Watson statistic (ranging from 0 to 4.0 and a value of 2.0 means that there is no autocorrelation). The level of significance was 0.05. Statistical analyses were performed using IBM SPSS Statistics for Windows, Version 24 (IBM Corporation, Armonk, NY).
Results
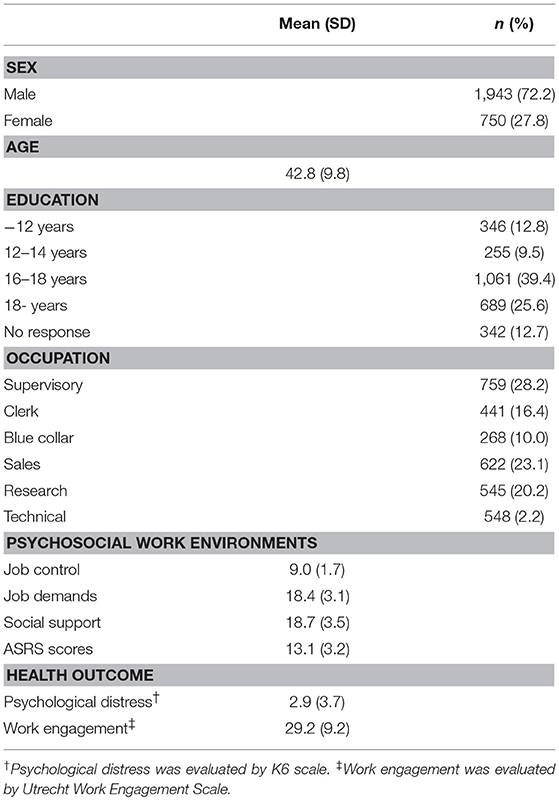
The respondents were 2,791 workers out of all employees (response rate = 59.8%). The proportion of women and mean age of respondents and all employees were 28.1%, 42.7 and 29.1%, 42.5, respectively. After excluding cases with missing data, 2,693 cases were analyzed as complete cases. In this sample, the prevalence of workers with ADHD symptoms was 5.9% (n = 159). Table 1 shows the demographic characteristics (sex, age, education, and occupation) and the means and standard deviations of psychosocial work environments, ASRS, and health outcomes (psychological distress and work engagement) scores of participants in this study.
Table 2 shows the main effects and interaction effects of psychosocial work environments and ADHD symptoms on psychological distress among all participants. After adjusting for demographic characteristics (Model 4), a significant interaction effect of job control × ASRS (ADHD symptoms) on psychological distress was observed (β = −0.067, p < 0.01), as well as a significant interaction effect of social support × ASRS on psychological distress (β = −0.052, p < 0.01). However, no significant interaction of job demands × ASRS on psychological distress was seen. Because we observed significant interactions of job control × ASRS, and social support × ASRS, we conducted post-hoc simple slope analyses at one standard deviation above/below the mean ASRS score. The post-hoc simple slope analyses showed that the simple slopes of job control and social support were greater at higher levels of ASRS compared to the lower levels of ASRS.
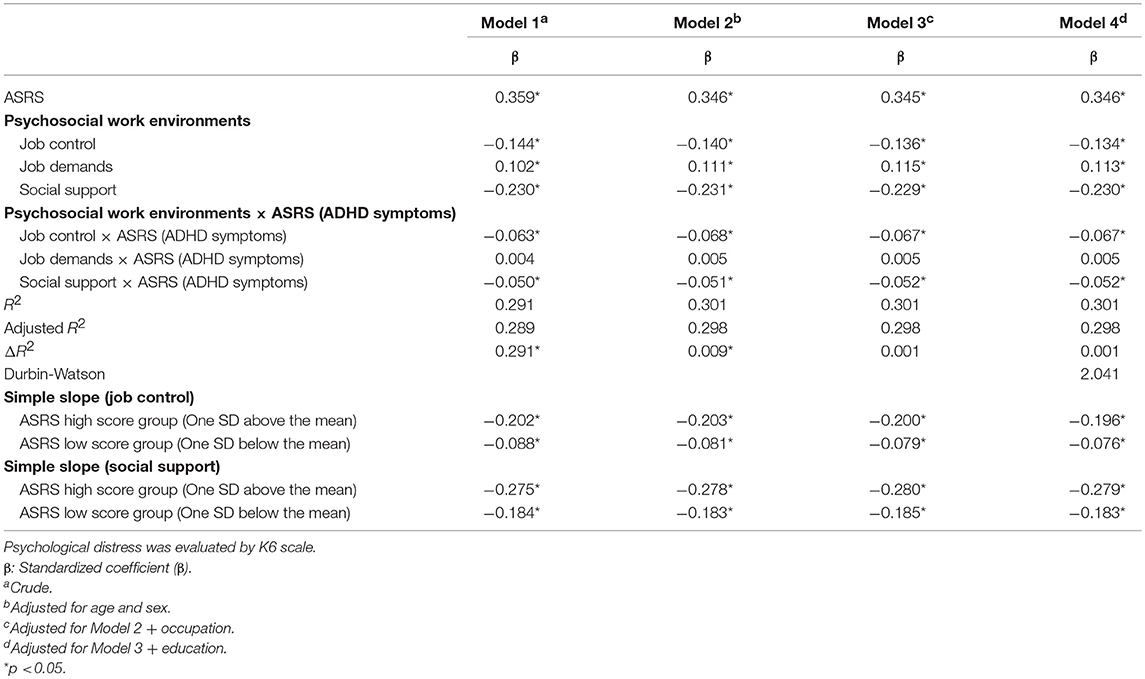
Table 2. Main effects and interaction effects of ASRS and job control, job demands, and social support on K6 values, and the simple slope of ASRS according to level of job control and social support on psychological distress (K6) among all participants.
Table 3 shows the main and interaction effects of psychosocial work environments and ADHD symptoms on work engagement among all participants. The interaction effects of psychosocial work environments × ASRS on work engagement were not significant.
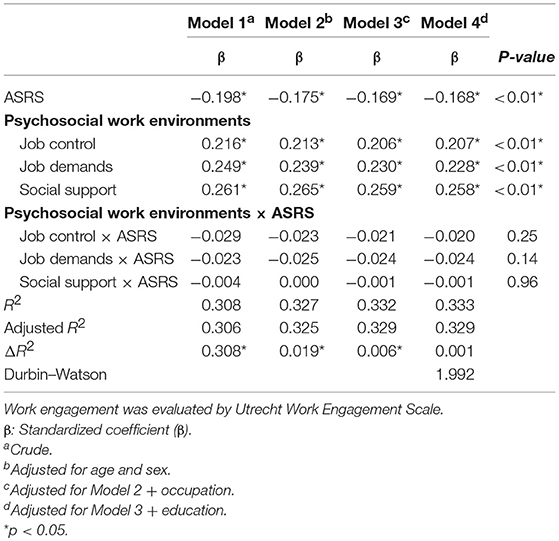
Table 3. Main effects and interaction effects of ASRS and job control, job demands, and social support on work engagement among all participants.
For residual analyses, the Durbin-Watson statistic ranged from 1.988 to 2.041 (i.e., very near to the optimum of 2.0), which indicated there was almost no autocorrelation in the residuals (see Tables 2, 3).
Discussion
This study demonstrated that there was a significant interaction effect of job control × ADHD symptoms and social support × ADHD symptoms on psychological distress. This study also found there was no interaction effect of psychosocial work environments × ADHD symptoms on work engagement.
Psychosocial Work Environments and Psychological Distress
Multiple regression analysis showed an interaction effect of job control × ASRS severity on psychological distress. Greater job control was associated with lower psychological distress, and ADHD symptoms strengthened the association. These findings suggest that greater levels of job control are important to maintain mental health for workers with ADHD symptoms. However, past studies have shown that in workers with Autism Spectrum Disorder (ASD), greater job control is associated with poor health quality (35). ADHD and ASD are frequently comorbid, however the results of the past study may not apply to workers with an ADHD tendency who have comorbid ASD. Further research is needed to clarify the differences in psychosocial factors between individuals with ADHD and ASD and those with ADHD alone.
Multiple regression analysis showed no interaction effect of job demands × ASRS severity on psychological distress. Workers with ADHD often have the entrepreneurship and professionalism (27). These characteristics are fit to work with broad discretion, while these characteristics spontaneously encourage to concentrate on a task and then these way of working often lead to excessive workload. High job demands lead to poor health of workers with ADHD symptoms as is the case with workers without ADHD, and supervisors and occupational health staff pay attention to such circumstances. We observed that multiple regression analysis showed a significant interaction effect of social support × ADHD symptoms on psychological distress. Lack of social support might enhance the difficulty in work especially among workers with ADHD symptoms. These observations may support the importance of care by supervisors and occupational health staff for workers with ADHD.
Psychosocial Work Environments and Work Engagement
We found that there was no significant interaction effect of job demands × ADHD symptoms and job control × ADHD symptoms on work engagement. Workers who interpret high job demands and high job control as a challenge may show improved work engagement. Although motivational themes identified by individuals with ADHD symptoms are similar to those identified by workers without ADHD symptoms, past research has shown that the details of the motivational factors differ, and that individuals with ADHD symptoms do not prefer predictable and familiar tasks (36). It may be necessary to devise strategies such as providing them with novel and diverse tasks. Further research is needed to reveal how psychosocial work environments are associated with work engagement for workers with ADHD symptoms.
Multiple regression analysis also did not show a significant interaction effect of social support × ADHD symptoms on work engagement. Bozionelos reported that incremental feedback on individual tasks resulted in greater improvements in work efficiency in workers with ADHD than in those without ADHD (28). It is difficult to explain this inconsistency, and we have to probe deeply how to perceive the support from supervisors or co-workers among workers with ADHD symptoms.
Generalization of This Study Sample
The prevalence of workers with ADHD symptoms in this study was 5.6%, a slightly higher than the prevalence rate by structured interview [3.5% (5) and 4.2% (6)]. The past study reported that the prevalence rate by a self-administrated questionnaire cover a wide range [1.9% (7) and 6.0% (8)], while the participation rate of the former study was substantially low (35–38%) (7). The prevalence rate by a self-administrated questionnaire tend to be higher than that by structured interview, therefore the prevalence rate of workers with ADHD in this study was rarely difference in the past studies. Between the prevalence rate of men and women, there was no difference in this study. This finding contradicts some past reports, which showed that men had a higher prevalence rate of ADHD as diagnosed by structured interview (5, 6). In this study, we used a self-administrated questionnaire to identify ADHD symptoms. Women tend to internalize problems to a greater degree than men, which may lead to overestimation of ADHD and produce a high prevalence rate of ADHD among women when self-administered questionnaires are used. In similar studies using self-administered questionnaires, the prevalence rate of ADHD is either not different between males and females, or higher in females (7, 8).
The mental health status of workers with ADHD symptoms was poorer than that of workers without ADHD symptoms, which supports past findings (37). Among workers with ADHD symptoms, 7.9% of individuals scored higher than 13 points on the K6, which was the cut-off point for severe mental illness (38), compared with only 1.8% of individuals among workers without ADHD symptoms. This suggests that individuals with ADHD symptoms require medical treatment, and that occupational health staff needs to assist these individuals in obtaining psychiatric help.
Several limitations of our study warrant mention. First, all participants were from a single pharmaceutical company, and work engagement levels were higher than among other Japanese workers (39). This may be because the company emphasizes employee health and a pleasant working environment. Therefore, there may be limitations on the generalization of the study findings. Second, we did not collect information about marital status, whereas past studies using the K6 score or work engagement as a dependent variable adjusted for marital status. Third, this was a cross-sectional study that used a self-administered questionnaire, and no causal relationships between the variables can therefore be inferred. Further research is necessary to clarify the nature of these associations.
Despite these limitations, this study is to our knowledge the first to investigate the role of ADHD symptoms on the relationship between psychosocial work environments and negative/positive health. This work may serve as a basis for future discussion of the preferred psychosocial work environments for workers with ADHD symptoms.
Author Contributions
MN, TN, and KM conceived and coordinated the project. MN, TN, and AI completed the analysis. MN and TN drafted the initial manuscript. MN, TN, AI, KM, and SM revised the manuscript, and commented on drafts of the report.
Funding
This study was funded by the Collabo-Health Study Group and Shionogi & CO., LTD. The funder had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing (2013).
2. Thapar A, Cooper M. Attention deficit hyperactivity disorder. Lancet. (2016) 387:1240–50. doi: 10.1016/S0140-6736(15)00238-X
3. Küpper T, Haavik J, Drexler H, Ramos-Quiroga JA, Wermelskirchen D, Prutz C, et al. The negative impact of attention-deficit/hyperactivity disorder on occupational health in adults and adolescents. Int Arch Occup Environ Health. (2012) 85:837–47. doi: 10.1007/s00420-012-0794-0
4. Breslin FC, Pole JD. Work injury risk among young people with learning disabilities and attention-deficit/hyperactivity disorder in Canada. Am J Public Health. (2009) 99:1423–30. doi: 10.2105/AJPH.2008.140855
5. de Graaf R, Kessler RC, Fayyad J, ten Have M, Alonso J, Angermeyer M, et al. The prevalence and effects of adult attention-deficit/hyperactivity disorder (ADHD) on the performance of workers: results from the WHO World Mental Health Survey Initiative. Occup Environ Med. (2008) 65:835–42. doi: 10.1136/oem.2007.038448
6. Kessler RC, Adler L, Ames M, Barkley RA, Birnbaum H, Greenberg P, et al. The prevalence and effects of adult attention deficit/hyperactivity disorder on work performance in a nationally representative sample of workers. J Occup Environ Med. (2005) 47:565–72. doi: 10.1097/01.jom.0000166863.33541.39
7. Kessler RC, Lane M, Stang PE, Van Brunt DL. The prevalence and workplace costs of adult attention deficit hyperactivity disorder in a large manufacturing firm. Psychol Med. (2009) 39:137–47. doi: 10.1017/S0033291708003309
8. Das D, Cherbuin N, Butterworth P, Anstey KJ, Easteal S. A population-based study of attention deficit/hyperactivity disorder symptoms and associated impairment in middle-aged adults. PLoS ONE. (2012) 7:e31500. doi: 10.1371/journal.pone.0031500
9. Faraone SV, Biederman J. Can attention-deficit/hyperactivity disorder onset occur in adulthood? JAMA Psychiatry. (2016) 73:655–6. doi: 10.1001/jamapsychiatry.2016.0400
10. Able SL, Johnston JA, Adler LA, Swindle RW. Functional and psychosocial impairment in adults with undiagnosed ADHD. Psychol Med. (2007) 37:97–107. doi: 10.1017/S0033291706008713
11. Norén Selinus E, Molero Y, Lichtenstein P, Anckarsäter H, Lundström S, Bottai M, et al. Subthreshold and threshold attention deficit hyperactivity disorder symptoms in childhood: psychosocial outcomes in adolescence in boys and girls. Acta Psychiatr Scand. (2016) 134:533–45. doi: 10.1111/acps.12655
12. Stansfeld S, Candy B. Psychosocial work environment and mental health—a meta-analytic review. Scand J Work Environ Health. (2006) 32:443–62. doi: 10.5271/sjweh.1050
13. Nieuwenhuijsen K, Bruinvels D, Frings-Dresen M. Psychosocial work environment and stress-related disorders, a systematic review. Occup Med. (2010) 60:277–86. doi: 10.1093/occmed/kqq081
14. Bakker AB, Demerouti E. Towards a model of work engagement. Career Dev Int. (2008)13:209–23. doi: 10.1108/13620430810870476
15. Bakker AB, Demerouti E. The Job Demands-Resources model: state of the art. J Manag Psychol. (2007) 22:309–28.
16. Bakker AB, Demerouti E, Sanz-Vergel AI. Burnout and work engagement: the JD–R approach. Ann Rev Organ Psychol Organ Behav. (2014) 1:389–411. doi: 10.1146/annurev-orgpsych-031413-091235
17. Demerouti E, Bakker AB, De Jonge J, Janssen PP, Schaufeli WB. Burnout and engagement at work as a function of demands and control. Scand J Work Environ Health. (2001) 27:279–86. doi: 10.5271/sjweh.615
18. Van den Broeck A, Elst TV, Baillien E, Sercu M, Schouteden M, De Witte H, et al. Job Demands, Job Resources, burnout, work engagement, and their relationships: an analysis across sectors. J Occup Environ Med. (2017) 59:369–76. doi: 10.1097/JOM.0000000000000964
19. Young S. Spatial working memory and strategy formation in adults diagnosed with attention deficit hyperactivity disorder. Personal Individ Differ. (2006) 41:653–61. doi: 10.1016/j.paid.2006.03.005
20. Young S. Planning ability in adults diagnosed with attention-deficit/hyperactivity disorder: a deficit in planning ability. Neuropsychology. (2007) 21:581–9. doi: 10.1037/0894-4105.21.5.581
21. Young S, Toone B, Tyson C. Comorbidity and psychosocial profile of adults with attention deficit hyperactivity disorder. Personal Individ Differ. (2003) 35: 743–55. doi: 10.1016/S0191-8869(02)00267-2
22. Young S, Gudjonsson GH. Growing out of ADHD: the relationship between functioning and symptoms. J Atten Disord. (2008) 12:162–9. doi: 10.1177/1087054707299598
23. Gupta R, Kar BR, Srinivasan N. Cognitive-motivational deficits in ADHD: development of a classification system. Child Neuropsychol. (2011) 17:67–81. doi: 10.1080/09297049.2010.524152
24. Schreuer N, Dorot R. Experiences of employed women with attention deficit hyperactive disorder: a phenomenological study. Work. (2017) 56:429–41. doi: 10.3233/WOR-172509
26. White HA, Shah P. Creative style and achievement in adults with attention-deficit/hyperactivity disorder. Pers Individ Diff. (2011) 50:673–7. doi: 10.1016/j.paid.2005.11.007
27. Verheul I, Rietdijk W, Block J, Franken I, Larsson H, Thurik R. The association between attention-deficit/hyperactivity (ADHD) symptoms and self-employment. Eur J Epidemiol. (2016) 31:793–801. doi: 10.1007/s10654-016-0159-1
28. Bozionelos N, Bozionelos G. Attention deficit/hyperactivity disorder at work: Does it impact job performance? Acad Manage Pers. (2013) 27:0107. doi: 10.5465/amp.2013.0107
29. Kessler RC, Adler LA, Gruber MJ, Sarawate CA, Spencer T, Van Brunt DL. Validity of the World Health Organization Adult ADHD Self-Report Scale (ASRS) Screener in a representative sample of health plan members. Int J Methods Psychiatr Res. (2007) 16:52–65. doi: 10.1002/mpr.208
30. Takeda T, Tsuji Y, Kurita H. Psychometric properties of the Japanese version of the Adult Attention-deficit hyperactivity disorder (ADHD) Self-Report Scale (ASRS-J) and its short scale in accordance with DSM-5 diagnostic criteria. Res Dev Disabil. (2017) 63:59–66. doi: 10.1016/j.ridd.2017.02.011
31. Shimomitsu T, Haratani T, Nakamura K, Kawakami N, Hayashi T, Hiro H, et al. Final Development of the Brief Job Stress Questionnaire mainly Used for Assessment of the Individuals. The Ministry of Labor Sponsored Grant for the Prevention of Work-Related Illness. Kato M, editor. FY 1999 report. Tokyo: Tokyo Medical University (in Japanese) (2000). p. 126–64.
32. Furukawa TA, Kawakami N, Saitoh M, Ono Y, Nakane Y, Nakamura Y, et al. The performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int J Methods Psychiatr Res. (2008) 17:152–8. doi: 10.1002/mpr.257
33. Schaufeli WB, Bakker AB, Salanova M. The measurement of work engagement with a short questionnaire: a cross-national study. Educ Psychol Meas. (2006) 66:701–16. doi: 10.1177/0013164405282471
34. Shimazu A, Schaufeli WB, Kosugi S, Suzuki A, Nashiwa H, Kato A, et al. Work engagement in Japan: validation of the Japanese version of the Utrecht Work Engagement Scale. Appl Psychol. (2008) 57:510–23. doi: 10.1111/j.1464-0597.2008.00333.x
35. Hayakawa N, Okada T, Nomura K, Tsukada T, Nakamura M. Is high job control a risk factor for poor quality of life in workers with high autism spectrum tendencies? A cross-sectional survey at a factory in Japan. J Occup Health. (2015) 57:419–26. doi: 10.1539/joh.14-0231-OA
36. Fayyad J, Sampson NA, Hwang I, Adamowski T, Aguilar-Gaxiola S, Al-Hamzawi A, et al. The descriptive epidemiology of DSM-IV Adult ADHD in the World Health Organization World Mental Health Surveys. Atten Defic Hyperact Disord. (2017) 9:47–65. doi: 10.1007/s12402-016-0208-3
37. Prochaska JJ, Sung HY, Max W, Shi Y, Ong M. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int J Methods Psychiatr Res. (2012) 21:88–97. doi: 10.1002/mpr.1349
38. Burton WN, Chen CY, Li X, Schultz AB. The Association of Employee engagement at work with health risks and presenteeism. J Occup Environ Med. (2017) 59:988–92. doi: 10.1097/JOM.0000000000001108
Keywords: ADHD, job demands, job control, social support, psychological distress, work engagement
Citation: Nagata M, Nagata T, Inoue A, Mori K and Matsuda S (2019) Effect Modification by Attention Deficit Hyperactivity Disorder (ADHD) Symptoms on the Association of Psychosocial Work Environments With Psychological Distress and Work Engagement. Front. Psychiatry 10:166. doi: 10.3389/fpsyt.2019.00166
Received: 22 June 2018; Accepted: 06 March 2019;
Published: 27 March 2019.
Edited by:
Meichun Mohler-Kuo, University of Applied Sciences and Arts of Western Switzerland, SwitzerlandReviewed by:
Lawrence T. Lam, University of Technology Sydney, AustraliaMiryoung Lee, University of Texas Health Science Center, United States
Copyright © 2019 Nagata, Nagata, Inoue, Mori and Matsuda. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Masako Nagata, bS1uYWdhdGFAbWVkLnVvZWgtdS5hYy5qcA==
 Masako Nagata
Masako Nagata Tomohisa Nagata1
Tomohisa Nagata1 Akiomi Inoue
Akiomi Inoue