- 1Brain and Mental Health Research Hub, Monash Institute of Cognitive and Clinical Neurosciences, School of Psychological Sciences, Monash University, Melbourne, VIC, Australia
- 2School of Psychology and Illawarra Health and Medical Research Institute, University of Wollongong, Wollongong, NSW, Australia
- 3The Australian Centre for Cannabinoid Clinical and Research Excellence, New Lambton Heights, NSW, Australia
Substance use disorder is characterized by repeated use of a substance, leading to clinically significant distress, making it a serious public health concern. The endocannabinoid system plays an important role in common neurobiological processes underlying substance use disorder, in particular by mediating the rewarding and motivational effects of substances and substance-related cues. In turn, a number of cannabinoid drugs (e.g., rimonabant, nabiximols) have been suggested for potential pharmacological treatment for substance dependence. Recently, cannabidiol (CBD), a non-psychoactive phytocannabinoid found in the cannabis plant, has also been proposed as a potentially effective treatment for the management of substance use disorder. Animal and human studies suggest that these cannabinoids have the potential to reduce craving and relapse in abstinent substance users, by impairing reconsolidation of drug-reward memory, salience of drug cues, and inhibiting the reward-facilitating effect of drugs. Such functions likely arise through the targeting of the endocannabinoid and serotonergic systems, although the exact mechanism is yet to be elucidated. This article seeks to review the role of the endocannabinoid system in substance use disorder and the proposed pharmacological action supporting cannabinoid drugs' therapeutic potential in addictions, with a focus on CBD. Subsequently, this article will evaluate the underlying evidence for CBD as a potential treatment for substance use disorder, across a range of substances including nicotine, alcohol, psychostimulants, opioids, and cannabis. While early research supports CBD's promise, further investigation and validation of CBD's efficacy, across preclinical and clinical trials will be necessary.
Introduction
Substance use disorder (SUD) is a global problem, with over 30 million individuals estimated to have an SUD (1). Within the United States alone, SUD-related expenditure (e.g., treatment and productivity cost) exceeded 23 billion USD per year (2), presenting a worrisome issue. Treatment to date has had minimal success, with a high likelihood of relapse (3). There is also no reliably established pharmacotherapy for SUDs, such as cannabis, and stimulant use disorder; and current pharmacotherapies (e.g., opiate substitution with methadone; naltrexone for alcohol use disorder; nicotine replacement) have limited efficacy in relapse prevention (4, 5). SUD has been conceptualized as a maladaptive and relapsing cycle of intoxication, binging, withdrawal and craving that results in excessive substance use despite adverse consequences (6). Recent models implicate major brain circuits involved in reward saliency, motivation, and memory/learned associations in maintaining addiction (7). Critically, these circuits may largely be modulated by the endocannabinoid system (ECS), presenting a promising pharmaceutical avenue for treating SUDs.
The Endocannabinoid System
The ECS consists of cannabinoid receptors (e.g., CB1R, CB2R), the endogenous ligands that bind to these cannabinoid receptors [e.g., anandamide and 2-arachidonoylglycerol (2-AG)], and enzymes for their biosynthesis and degradation [e.g., fatty acid amide hydrolase (FAAH) and monoacylglyrecol lipase (MAGL)] (8). Over the past decade, primary interest has focused on CB1Rs, for their purported role across a range of physiological functions, including directing the psychoactive effect of delta9-tetrahydrocannabinol (THC), a phytocannabinoid present in cannabis (8, 9). CB1Rs are one of the most common G-protein-coupled receptors in the central nervous system, preferentially residing on presynaptic neurons across diverse regions including the neocortex, striatum, and hippocampus (10, 11). Their widespread distribution allows them to guide a host of functions ranging from cognition, memory, mood, appetite, and sensory responses (8). Endocannabinoids themselves function as neuromodulators that are released by post-synaptic neurons, and bind to the presynaptic CB1Rs to moderate the release of neurotransmitters, such as gamma-aminobutyric-acid (GABA), glutamate, and dopamine (DA) (10, 12, 13). While the specific CB1R function depends on the cell population and region in which they reside, their role in retrograde signaling permits them to regulate signaling activity across cognitive, emotive, and sensory functions, lending therapeutic capacity (14).
ECS Role in Reward Signaling
Of the functions that the ECS is involved in, of critical interest, is its influence on the brain reward circuitry, particularly in response to substances of abuse. The rewarding effect of substances of abuse is thought to be primarily mediated by the mesolimbic DA pathway, originating from dopaminergic cell bodies in ventral midbrain [ventral tegmental area (VTA)], carrying reward-related information to the ventral striatum [nucleus accumbens (NAc)] (15). The acute reinforcing effect of addictive substances is thought to be due to their direct or indirect activation of DA neurons along this pathway (16). The VTA-NAc pathway as such plays a key function in reward assessment, anticipation, and valuation, making it a critical component underlying substance use and addiction (17).
DA activity is intrinsically tied to cannabinoid activity. CB1Rs are particularly densely located across the striatal regions that mediate reward function (i.e., NAc and VTA) (18), and their regulatory role on the VTA-NAc pathway may be crucial in modulating overall reward tone (19, 20). Rodent studies have demonstrated that THC increases neuronal firing rates in the VTA (21), likely through local disinhibition of DA-ergic neurons, by binding to CB1Rs present on glutamatergic and/or GABAergic neurons (although it is prudent to note that THC's capacity to potentiate DAergic release differs between rodents and humans) (15, 20, 22, 23). Similarly, other substances of abuse (e.g., opioids, cocaine) have also been demonstrated to potentiate dopaminergic activity via the ECS (24, 25). For example, alcohol is found to have a downstream potentiation effect on the ECS in rats (26), such as an increase in endogenous cannabinoid (anandamide and 2-AG) levels (27, 28) and downregulation of CB1R expression (29). Alcohol-induced DAergic release is furthermore dependent on the presence of CB1Rs (30). Nicotine activates DA neurons in the VTA either directly through stimulation of nicotinic cholinergic receptors or indirectly through glutaminergic nerve terminals that are modulated by the ECS (31). Meanwhile opioid receptors are often co-located with CB1Rs in the striatum (32), and may be modulated by and interact with CB1R activity reciprocally (33, 34). Only psychostimulants are suggested to act directly on DAergic axon terminals in the NAc, potentially avoiding upstream endocannabinoid involvement in the VTA (35).
CB1R's role in the motivational and reinforcing effects of rewards has been demonstrated in animal models with CB1R agonists. For example, acute exposure to CB1R agonists (e.g., THC; CP 55,940; WIN 55,212-2; HU 210) augments NAc DA transmission (36), lowers the brain-reward threshold (17), induces conditioned place preference (CPP) (37), and establishes persistent self-administration of substances of abuse, including cannabis and alcohol (17, 38). Meanwhile, CB1R antagonists (e.g., rimonabant) have been shown to attenuate reinforcing effects of these substances, blocking the increase of DA release in the NAc (37, 39). While substances of abuse, such as alcohol, stimulants, nicotine and opioids have differing upstream mechanisms of action (14, 40), the evidence suggest the downstream involvement of the ECS in their reward mechanism.
In summary, the ECS, by direct CB1R activity, modulates and is modulated by mesolimbic DA activity (41). While the action of individual substances may differ, they share a common effect of precipitating DAergic activity from the VTA neurons (42), with this DA-ergic activity mediated by the ECS (14). It is thus thought that the disruption of endocannabinoid signaling may prove effective in treating SUDs (41). Nevertheless, it is necessary to note that this is a simplistic understanding, given the potential involvement of non-DA-ergic neurons in the VTA, and additional neuronal circuits including those involving glutamatergic and opioids, that are yet to be fully elucidated (39, 43).
ECS Role in Substance Use Disorder (SUD)
Besides the ECS role in reward, it is necessary to acknowledge that substance reward and reinforcement are different from substance dependence. Where the former explain initial substance use, and are suggested to be related to increased DA in striatal and limbic (NAc and amygdala) regions (44, 45); the latter reflects further compulsive substance intake, loss of control, and persistent intake despite the substance's adverse effects and tolerance to its pleasurable responses (44, 46, 47).
Several lines of thought suggest SUD to be a learned habit (48, 49) mediated by persistent changes in striatal function (e.g., synaptic plasticity occurring during learning) (50). Substances of abuse are thought to influence long-lasting plastic changes across corticostriatal circuits, through repeated perturbation of DA activity, thus making it difficult for addicts to cease their substance use, and enhancing risk of relapse (48, 50–52). In this role, CB1Rs present across the corticostriatal circuits, such as the PFC and striatum, mediate synaptic transmission, in their capacity as neuromodulators (35, 53). Evidence demonstrates the necessity of cannabinoid signaling on CB1Rs to induce long-lasting synaptic plasticity, such as long-term depression (LTD) of glutamatergic release across the dorsal and ventral striatum (19, 54). Such functional changes, particularly across the striatal structures responsible for the rewarding and motivational effects of substances of abuse, are not only necessary in providing reward salience, but also in establishing compulsive substance use habit (39, 55). The ECS thus represents a necessary contributor toward cellular adaptations in the transition from recreational substance use to a use disorder (50, 56).
A further function of ECS-mediated synaptic plasticity may be to facilitate emotional learning and memory processes, which promote increased emotional response to substance-related cues (57). The limbic system, in particular the amygdala and hippocampus, by supporting the formation of associative memory, promotes positive and negative reinforcement of rewards including those of substances of abuse (58). Indeed, animal models demonstrate memory performance to not only be dependent on emotional processes, but may be modulated by augmentation of ECS signaling (59–62). Phytocannabinoids, such as THC and CBD for example have been found to modulate brain activity level across limbic regions during emotional processing tasks (63, 64). Endocannabinoids may further induce long-term changes in synaptic strength across the hippocampus, mediating associative memory formation (65–67). Literature investigating cannabinoid agonists and antagonists on SUD solidifies the role of the ECS in emotional learning and memory processes. CB1R agonists and antagonists have respectively been demonstrated to facilitate and attenuate memory extinction in various fear and reward conditioning paradigms in animal models [see (57) for review]. Within the context of SUD, cannabinoid modulation of emotional memory may have implications for extinction, consolidation, and reinstatement of substance-related memory (68). These processes are primarily assessed through place conditioning paradigms, such as CPP. CB1R antagonism by rimonabant for example, has been demonstrated to disrupt the reconsolidation and facilitate the extinction of CPP to substances of abuse, such as methamphetamine and cocaine, potentially via disrupting reward-associated memory (69, 70). Nevertheless, evidence on SUD behavior is mixed and potentially dependent on type and dose of cannabinoids (70, 71).
The ECS's role in reward signaling and learning may as such shape addictive behavior in SUD. The following section details evidence of CB1R's involvement in SUD as demonstrated by cannabinoid agonism and antagonism in animal models.
Agonism of CB1R
CB1R agonism (either studied with the synthetic cannabinoid agonist WIN 55-212,2 or contrasted against CB1R knockout mice) has been shown to facilitate alcohol self-administration, CPP, and binge-like behavior in animals (38, 72–74). WIN 55,212-2 has also been found to increase motivation to self-administer nicotine, and facilitate cue-induced reinstatement in rats (75). Similar results are found in the heroin literature, with THC-induced CB1R agonism increasing substance self-administration in rats (76, 77).
Agonist substitution with CB1R agonists may have potential for treatment of cannabis use disorder by reducing withdrawal symptoms and the reinforcing effect of cannabis (78). Dronabinol—a stereoisomer of THC, and Nabilone—a synthetic analog of THC, originally intended for nausea and weight loss (55), have both been shown to have efficacy for cannabis withdrawal (79, 80). However, Dronabinol and Nabilone may not prevent cannabis use or relapse (78). It is likely that while these substances are efficacious in attenuating withdrawal symptoms by acting as a “proxy-substances,” they do not directly normalize substance use-related circuits and behavior.
Antagonism of CB1R
CB1R antagonism has originally been assumed to be a promising target for SUD treatment. SR141716, known as rimonabant, an inverse agonist of CB1R, has been extensively investigated in SUD for its antagonist effect on drug seeking and relapse behavior in both animal and human models.
Animal studies have shown rimonabant as effective in reducing self-administration of alcohol (81, 82), nicotine (83, 84), and heroin (85). Antagonism of CB1R by rimonabant, reduces alcohol-induced sensitization and reinstatement of nicotine-seeking in rats (83, 84, 86). When investigating the efficacy of CB1R antagonists on stimulant use however, the literature is mixed. While rimonabant's CB1R antagonism has been shown to block CPP and attenuate cue- and substance-induced relapse to psychostimulants, such as cocaine and methamphetamines (87–89), evidence pertaining to self-administration is inconsistent (90–92).
Human studies have also been conducted investigating the efficacy of rimonabant in cannabis, nicotine, and alcohol use. Cannabis and nicotine use have both shown sensitivity to rimonabant antagonism. Rimonabant attenuated the acute physiological effects of cannabis including subjective level of intoxication (93, 94), and clinical trials demonstrate rimonabant to be effective in increasing smoking cessation (95). However, the efficacy of rimonabant for alcohol cessation has been less promising. In a 12-weeks clinical trial of relapse rate in recently detoxified alcohol-dependant patients, rimonabant only had a modest effect (that did not reach significance) compared to placebo (96). Rimonabant also had no effect on alcohol consumption for non-treatment seeking heavy alcohol drinkers (97).
Despite promising findings of rimonabant against substance use and relapse, it has been found to produce significant negative psychiatric effects including depression, anxiety, and an elevated suicide rate, preventing it from being a viable treatment option (98). Nevertheless, the evidence indicates CB1R antagonism to have robust effects on some SUDs, highlighting a potential target for SUD treatment. One such candidate drug that antagonizes CB1R, and is increasingly being investigated as a therapeutic option for SUD, is cannabidiol (CBD).
Cannabidiol (CBD)
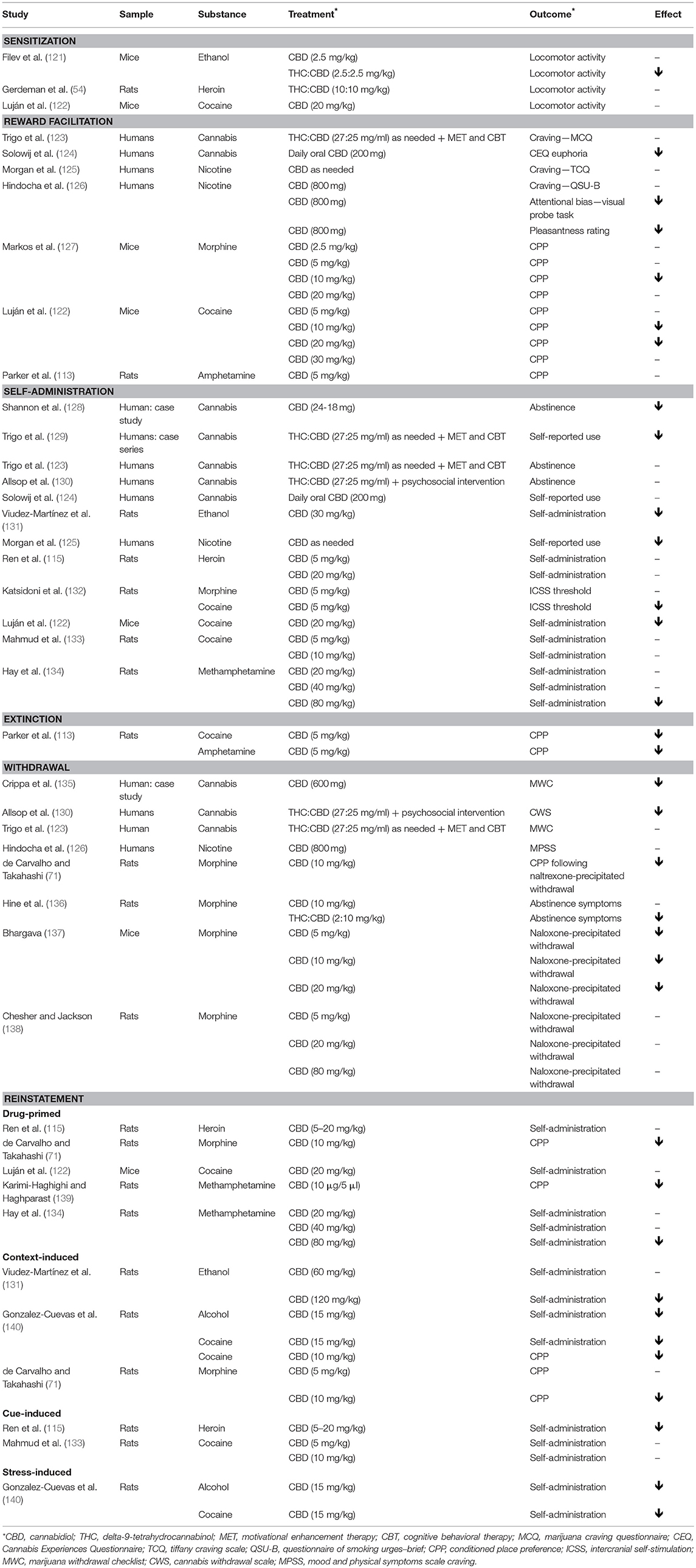
CBD is a phytocannabinoid found in cannabis that has recently emerged as a promising treatment for SUDs (99, 100). CBD is non-rewarding, and acts on a number of receptor systems including the opioid (101), serotonergic (102, 103), and cannabinoid (22) systems. Within the cannabinoid system, it is a non-competitive antagonist of CB1R with a low affinity for CB1Rs' primary ligand site (104, 105), instead acting through negative allosteric modulation (105, 106). CBD is found to inhibit endocannabinoid signaling in a dose-dependent manner, likely by binding to CB1Rs' allosteric site and altering the potency of other primary ligands (e.g., endocannabinoids, THC) (106, 107). Its ability to modulate overall ECS tone despite lacking intrinsic efficacy (105) meant that it may decrease CB1R activity without CB1 inverse agonist-related side effects, such as those produced by rimonabant (108, 109). Indeed, CBD has a good safety profile, with generally mild side effects in animal preclinical studies or human studies (110, 111). This, coupled by the limited abuse liability of CBD (112, 113), makes it a good therapeutic candidate. Systemically administered CBD has also been demonstrated to regulate mesolimbic DA activity (114), and potentially attenuate substance-induced dysregulation of the mesolimbic circuitry (115, 116), suggesting its utility against SUDs. Though its efficacy may be dependent on a range of factors including the sequence of administration (i.e., whether CBD is administered in conjunction with, prior to, or post substance-use), and dose ratio (117). A number of papers are urging for the investigation of CBD as a therapeutic option for SUD of multiple substances including stimulants (118), opioids (119, 120), and nicotine use disorder (31). The following section details evidence of CBD treatments for cannabis, alcohol, nicotine, opioid, and stimulants. Table 1 further lists this evidence by SUD constructs.
Cannabis
Pharmacological approaches to treating cannabis dependence via agonist replacement (i.e., Dronabinol and Nabilone) have limited efficacy (141). CBD itself has been trialed in rats, and found to be effective in ameliorating conditioned place aversion (CPA) produced by THC injection, but did not alter CPP (142). In human case studies, CBD has also been found to reduce self-reported cannabis use to non-use in a dependent male (128), and to reduced cannabis withdrawal in another (135), although the latter case study did find the subject to have relapsed after a 6-months follow up (135). CBD may have potential in reducing euphoria associated with cannabis use, despite not directly reducing cannabis use (124). However, investigative efforts with pure CBD have been limited. Instead most studies have focused on nabiximols—an oromucosal spray containing 2.7 mg of THC and 2.5 mg of CBD—for cannabis dependence (143).
A number of human case studies suggest nabiximols to be efficacious, in combination with behavioral therapy, in reducing cannabis use and withdrawal symptoms (129). However, case study evidence should be taken cautiously. Further case-control studies indicate nabiximols to be effective in reducing withdrawal, but not cannabis use (123, 130, 144). Nor did it improve abstinence rate (123). It was noted that while therapeutics may assist in short-term withdrawal, it is unlikely that ongoing abstinence can be achieved without psychosocial or clinical support (145). Additionally, the THC component of nabiximols causes the drug to have abuse potential and should not be used lightly (146).
Alcohol
In animal studies, CBD was effective in reducing ethanol self-administration, and at high enough concentration (120 mg/kg but not 60 mg/kg) attenuated ethanol relapse (131). Further animal studies show CBD (at 15 mg/kg) to effectively reduce cue and stress induced reinstatement of ethanol administration, up to 138 days post-CBD treatment (140). However, one study found CBD alone to be ineffective in attenuating ethanol sensitization, which is suggested to be the first step in drug-associated plasticity (121). Comparatively, pure THC and a 1:1 ratio of THC:CBD was found to be more efficacious in reducing ethanol sensitization. In a human trial of 10-weeks of daily CBD administration in cannabis users, no changes in alcohol or tobacco use was observed either, although the study sample was not dependent on alcohol (124).
Tobacco
In a placebo controlled study of 24 smokers, those who received a CBD inhaler significantly reduced the number of smoked cigarettes relative to the placebo group, despite no reported difference in craving between groups (125). In another study, oral CBD reduced the salience of cigarette cues, after overnight abstinence in smokers, relative to placebo, but did not reduce craving or withdrawal (126).
Opioids
Initial studies on the efficacy of cannabinoids in alleviating morphine withdrawal and abstinence symptoms occurred 40 years ago, with rodent models suggesting that CBD alone has low efficacy in alleviating signs of abstinence in rats, but CBD in combination with THC (5:1 ratio) did so significantly (136). THC itself was demonstrated to be more effective than CBD in inhibiting morphine abstinence syndrome in mice (137, 138). Nevertheless, more recent studies demonstrate that treatment with CBD blocked the reward-facilitating effect of morphine (132), reduced morphine CPP and CPA, and prevented drug and stress-induced reinstatement of CPP (71, 127). CBD was also found to have some efficacy in heroin studies in rats. While it did not specifically alter maintenance of self-administration, nor did it aid extinction of self-administration, it did attenuate cue-induced (but not drug-primed) self-administration following 14 days of abstinence, with CBD's effect lasting up to 2 weeks post-administration (115).
Stimulants
Evidence of CBD efficacy for stimulant use is mixed. Neither CBD, nor a 1:1 ratio of THC:CBD reversed the cocaine sensitization effect (although rimonabant did) (54, 122). Some studies suggest that acute CBD administration does not block the reward-facilitating effect of cocaine (132), reduce cocaine self-administration, or attenuate cue-induced cocaine seeking in rats (133). However, others did find CBD to disrupt acquisition of cocaine self-administration and CPP (122), and impair drug-primed reinstatement of CPP for methamphetamine (139). Further studies on relapse are similarly mixed with one demonstrating CBD's ability to attenuate reconsolidation of CPP (1 week post-CPP acquisition) for cocaine in mice (71), and effectively reduce cue and stress-induced reinstatement of cocaine seeking up to 48 days post-CBD treatment (140), whilst another suggested no effect of CBD on drug-primed reinstatement post-extinction (122). Dose dependency may explain contradictory findings, as Hay et al. (134) demonstrated that 80 mg/kg (and not less) of CBD was needed to significantly reduce motivation to self-administer methamphetamine and reinstatement post-extinction. While evidence for CBD use for stimulant addiction in animals is weak, a longitudinal observational study of 122 participants did find cocaine users who self-report using cannabis to control their cocaine use, to have reduced their cocaine use over a 3 years period (147). Nevertheless, street cannabis generally has low amounts of CBD (148) and findings cannot be extrapolated to CBD's therapeutic efficacy.
The relatively weaker evidence of CBD in disrupting the reward-facilitating effect and self-administration of substances of abuse, despite its comparative efficacy in CPP reinstatement paradigms, may reflect its role in attenuating reward-related memory, without altering the rewarding properties of substances per se. Evidence of CBD's role in regulating emotional memory is supported by studies of other conditions, such as anxiety and PTSD-related fear memory [see (47) and (141) for a more extensive review of cannabinoid's role in emotional memory processing across other paradigms]. However, evidence of CBD's role in the consolidation and extinction of substance-related memory in humans is yet limited.
Summary and Future Directions
CBD shows some promise in alleviating negative withdrawal effects and reducing motivation to self-administer or reinstatement of drug use in animals. However, evidence on its efficacy is limited and mixed. CBD alone may not be sufficiently effective in maintaining long-term abstinence without ongoing support and behavioral therapy, as evidenced by its lack of efficacy over treatments, such as cognitive behavioral therapy and motivational enhancement therapy (123, 129). A combination of pharmacotherapy and behavioral therapy may increase treatment potency and adherence (149), and CBD may be better suited as an adjunct treatment to primary behavioral or psychosocial therapy (124).
There is also much that is unknown about how CBD may be targeting and alleviating SUD-related effects. Recent evidence suggests that within the mesolimbic system, CBD also influences the serotonergic system, as an agonist of the serotonin 1A (5-HT1A) receptor (102, 103), which in addition to contributing to reduction in stress and anxiety (150), may be responsible for (i) blunting the reward-facilitating effect of substances of abuse (e.g., morphine in rats) (132); and (ii) modulating the formation of associative emotional memory related to substances of abuse (151). A number of studies have suggested the potential of selective serotonin reuptake inhibitors and other antidepressants in reducing substance (e.g., alcohol and nicotine) use via alleviating mood symptoms (152). CBD's capacity to alleviate stress, anxiety, and depressive symptoms may be mediating its treatment effect on SUDs (124, 153, 154). Indeed, CBD has been found to have therapeutic potential in alleviating affective and cognitive processing disturbances that may be induced by chronic substance (e.g., cannabis) use (63, 64, 155), proving potential utility in moderating the deleterious course of impairment, particularly in adolescent initiates of substance use (156). Additionally, other receptor and enzyme functions targeted by CBD, such as cannabinoid CB2Rs, non-cannabinoid transient receptor potential vanilloid type-1 (TRPV1) and type-2 (TRPV2) receptors, and ECS' catabolic enzymes FAAH and MAGL, should also be investigated for their role in the ECS and SUD (157–161).
In sum, some early research supports CBD's promise as pharmacotherapy against SUD. However, further investigation into CBD's mechanism of action, and validation of its efficacy, across preclinical and clinical trials will be necessary.
Author Contributions
YC wrote the core sections of the manuscript with the assistance of EC. NS and MY provided intellectual input and edits.
Funding
YC is supported by the Monash Postdoctoral Bridging Fellowship; NS is supported by the National Health and Medical Research Council (NHMRC) Centre of Research Excellence Grant (APP1135054). MY is supported by a National Health and Medical Research Council (NHMRC) of Australia Fellowship (APP1117188) and the David Winston Turner Endowment Fund.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. United Nations Office on Drugs and Crime. World Drug Report 2017. United Nations Publication, Sales No. E.17.XI.6 (2017).
2. Institute for Health Metrics and Evaluation. Global Burden of Disease Data. Available online at: www.healthdata.org
3. McLellan AT, Lewis DC, O'Brien CP, Kleber HD. Drug dependence, a chronic medical illness. JAMA (2000) 284:1689. doi: 10.1001/jama.284.13.1689
4. Pashaei T, Shojaeizadeh D, Rahimi Foroushani A, Ghazitabatabae M, Moeeni M, Rajati F, et al. Effectiveness of relapse prevention cognitive-behavioral model in opioid-dependent patients participating in the methadone maintenance treatment in Iran. Iran J Public Health (2013) 42:896–902.
5. Dermody SS, Wardell JD, Stoner SA, Hendershot CS. Predictors of daily adherence to naltrexone for alcohol use disorder treatment during a mobile health intervention. Ann Behav Med. (2018) 52:787–97. doi: 10.1093/abm/kax053
6. Goldstein RZ, Volkow ND. Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat Rev Neurosci. (2011) 12:652–69. doi: 10.1038/nrn3119
7. Volkow ND, Fowler JS, Wang G-J. The addicted brain: insights from imaging studies. J Clin Invest. (2003) 111:1444–51. doi: 10.1172/JCI18533
8. SvíŽenská I, Dubový P, Šulcová A. Cannabinoid receptors 1 and 2 (CB1 and CB2), their distribution, ligands and functional involvement in nervous system structures–a short review. Pharmacol Biochem Behav. (2008) 90:501–11. doi: 10.1016/j.pbb.2008.05.010
9. Gaoni Y, Mechoulam R. Isolation, structure, and partial synthesis of an active constituent of hashish. J Am Chem Soc. (1964) 86:1646–7. doi: 10.1021/ja01062a046
10. Di Marzo V, Bifulco M, De Petrocellis L. The endocannabinoid system and its therapeutic exploitation. Nat Rev Drug Discov. (2004) 3:771–84. doi: 10.1038/nrd1495
11. Herkenham M, Lynn AB, Little MD, Johnson MR, Melvin LS, de Costa BR, et al. Cannabinoid receptor localization in brain. Proc Natl Acad Sci USA. (1990) 87:1932–6. doi: 10.1073/pnas.87.5.1932
12. Terry GE, Liow J, Zoghbi SS, Hirvonen J, Farris AG, Lerner A, et al. Quantitation of cannabinoid CB1 receptors in healthy human brain using positron emission tomography and an inverse agonist radioligand. Neuroimage (2009) 48:362–70. doi: 10.1016/j.neuroimage.2009.06.059
13. McAllister SD, Glass M. CB1 and CB2 receptor-mediated signalling: a focus on endocannabinoids. Prostaglandins Leukot Essent Fat Acids (2002) 66:161–71. doi: 10.1054/plef.2001.0344
14. Lupica CR, Riegel AC. Endocannabinoid release from midbrain dopamine neurons: a potential substrate for cannabinoid receptor antagonist treatment of addiction. Neuropharmacology (2005) 48:1105–16. doi: 10.1016/j.neuropharm.2005.03.016
15. Gardner EL. Addictive potential of cannabinoids: the underlying neurobiology. Chem Phys Lipids (2002) 121:267–90. doi: 10.1016/S0009-3084(02)00162-7
16. Volkow ND, Wang G-J, Fowler JS, Logan J, Schlyer D, Hitzemann R, et al. Imaging endogenous dopamine competition with [11C]raclopride in the human brain. Synapse (1994) 16:255–62. doi: 10.1002/syn.890160402
17. Gardner EL. Endocannabinoid signaling system and brain reward: emphasis on dopamine. Pharmacol Biochem Behav. (2005) 81:263–84. doi: 10.1016/j.pbb.2005.01.032
18. Glass M, Dragunow M, Faull RL. Cannabinoid receptors in the human brain: a detailed anatomical and quantitative autoradiographic study in the fetal, neonatal and adult human brain. Neuroscience (1997) 77:299–318. doi: 10.1016/S0306-4522(96)00428-9
19. Robbe D, Kopf M, Remaury A, Bockaert J, Manzoni OJ. Endogenous cannabinoids mediate long-term synaptic depression in the nucleus accumbens. Proc Natl Acad Sci USA. (2002) 99:8384–8. doi: 10.1073/pnas.122149199
20. Riegel AC, Lupica CR. Independent presynaptic and postsynaptic mechanisms regulate endocannabinoid signaling at multiple synapses in the ventral tegmental area. J Neurosci. (2004) 24:11070–8. doi: 10.1523/JNEUROSCI.3695-04.2004
21. Cheer JF, Marsden CA., Kendall DA., Mason R. Lack of response suppression follows repeated ventral tegmental cannabinoid administration: an in vitro electrophysiological study. Neuroscience (2000) 99:661–7. doi: 10.1016/S0306-4522(00)00241-4
22. Pertwee RG. The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: delta9-tetrahydrocannabinol, cannabidiol and delta9-tetrahydrocannabivarin. Br J Pharmacol. (2008) 153:199–215. doi: 10.1038/sj.bjp.0707442
23. Bossong MG, Mehta MA, Berckel BNM Van Howes OD, S Kahn RS, Stokes PRA. Further human evidence for striatal dopamine release induced by administration of Δ9-tetrahydrocannabinol (THC): selectivity to limbic striatum. Psychopharmacology (Berl). (2015) 232:2723–9. doi: 10.1007/s00213-015-3915-0
24. Mascia MS, Obinu MC, Ledent C, Parmentier M, Böhme GA, Imperato A, et al. Lack of morphine-induced dopamine release in the nucleus accumbens of cannabinoid CB1receptor knockout mice. Eur J Pharmacol. (1999) 383:99–100.
25. Wang H, Treadway T, Covey DP, Cheer JF, Lupica CR. Cocaine-induced endocannabinoid mobilization in the ventral tegmental area. Cell Rep. (2015) 12:1997–2008. doi: 10.1016/j.celrep.2015.08.041
26. Serrano A, Rivera P, Pavon FJ, Decara J, Suárez J, Rodriguez de Fonseca F, et al. Differential effects of single versus repeated alcohol withdrawal on the expression of endocannabinoid system-related genes in the rat amygdala. Alcohol Clin Exp Res. (2012) 36:984–94. doi: 10.1111/j.1530-0277.2011.01686.x
27. Basavarajappa BS, Saito M, Cooper TB, Hungund BL. Stimulation of cannabinoid receptor agonist 2-arachidonylglycerol by chronic ethanol and its modulation by specific neuromodulators in cerebellar granule neurons. Biochim Biophys Acta (2000) 1535:78–86. doi: 10.1016/S0925-4439(00)00085-5
28. Basavarajappa BS, Saito M, Cooper TB, Hungund BL. Chronic ethanol inhibits the anandamide transport and increases extracellular anandamide levels in cerebellar granule neurons. Eur J Pharmacol. (2003) 466:73–83. doi: 10.1016/S0014-2999(03)01557-7
29. Ortiz S, Oliva JM, Pérez-Rial S, Palomo T, Manzanares J. Chronic ethanol consumption regulates cannabinoid CB1 receptor gene expression in selected regions of rat brain. Alcohol Alcohol. (2004) 39:88–92. doi: 10.1093/alcalc/agh036
30. Hungund BL, Szakall I, Adam A, Basavarajappa BS, Vadasz C. Cannabinoid CB1 receptor knockout mice exhibit markedly reduced voluntary alcohol consumption and lack alcohol-induced dopamine release in the nucleus accumbens. J Neurochem. (2003) 84:698–704. doi: 10.1046/j.1471-4159.2003.01576.x
31. Gamaleddin IH, Trigo JM, Gueye AB, Zvonok A, Makriyannis A, Goldberg SR, et al. Role of the endogenous cannabinoid system in nicotine addiction: novel insights. Front Psychiatry (2015) 6:1–12. doi: 10.3389/fpsyt.2015.00041
32. Pickel VM, Chan J, Kash TL, Rodríguez JJ, Mackie K. Compartment-specific localization of cannabinoid 1 (CB1) and μ-opioid receptors in rat nucleus accumbens. Neuroscience (2004) 127:101–12. doi: 10.1016/j.neuroscience.2004.05.015
33. Rios C, Gomes I, Devi LA. μ opioid and CB1 cannabinoid receptor interactions: reciprocal inhibition of receptor signaling and neuritogenesis. Br J Pharmacol. (2009) 148:387–95. doi: 10.1038/sj.bjp.0706757
34. Corchero J, Fuentes JA, Manzanares J. Chronic treatment with CP-55,940 regulates corticotropin releasing factor and proopiomelanocortin gene expression in the hypothalamus and pituitary gland of the rat. Life Sci. (1999) 64:905–11. doi: 10.1016/S0024-3205(99)00016-8
35. Maldonado R, Valverde O, Berrendero F. Involvement of the endocannabinoid system in drug addiction. Trends Neurosci. (2006) 29:225–32. doi: 10.1016/j.tins.2006.01.008
36. French ED. Δ9-Tetrahydrocannabinol excites rat VTA dopamine neurons through activation of cannabinoid CB1 but not opioid receptors. Neurosci Lett. (1997) 226:159–62. doi: 10.1016/S0304-3940(97)00278-4
37. Braida D, Iosuè S, Pegorini S, Sala M. Δ9-Tetrahydrocannabinol-induced conditioned place preference and intracerebroventricular self-administration in rats. Eur J Pharmacol. (2004) 506:63–9. doi: 10.1016/j.ejphar.2004.10.043
38. Linsenbardt DN, Boehm SL. Agonism of the endocannabinoid system modulates binge-like alcohol intake in male C57BL/6J mice: involvement of the posterior ventral tegmental area. Neuroscience (2009) 164:424–34. doi: 10.1016/j.neuroscience.2009.08.007
39. Lupica CR, Riegel AC, Hoffman AF. Marijuana and cannabinoid regulation of brain reward circuits. Br J Pharmacol. (2004) 143:227–34. doi: 10.1038/sj.bjp.0705931
40. González S, Fernández-Ruiz J, Sparpaglione V, Parolaro D, Ramos JA. Chronic exposure to morphine, cocaine or ethanol in rats produced different effects in brain cannabinoid CB1 receptor binding and mRNA levels. Drug Alcohol Depend. (2002) 66:77–84. doi: 10.1016/S0376-8716(01)00186-7
41. Solinas M, Yasar S, Goldberg SR. Endocannabinoid system involvement in brain reward processes related to drug abuse. Pharmacol Res. (2007) 56:393–405. doi: 10.1016/j.phrs.2007.09.005
42. Di Chiara G, Imperato A. Drugs abused by humans preferentially increase synaptic dopamine concentration in the mesolimbic system of freely moving rats. Proc Natl Acad Sci USA. (1988) 85:5274–8. doi: 10.1073/pnas.85.14.5274
43. Melis M, Pstis M, Perra S, Muntoni AL, Pillolla G, Gessa GL. Endocannabinoids mediate presynaptic inhibition of glutamatergic transmission in rat ventral tegmental area dopamine neurons through activation of CB1 receptors. J Neurosci. (2004) 24:53–62. doi: 10.1523/JNEUROSCI.4503-03.2004
44. Volkow ND, Fowler JS. Addiction, a disease of compulsion and drive: involvement of the orbitofrontal cortex. Cereb Cortex (2000) 10:318–25. doi: 10.1093/cercor/10.3.318
45. Pontieri FE, Tanda G, Orzi F, Di Chiara G. Effects of nicotine on the nucleus accumbens and similarity to those of addictive drugs. Nature (1996) 382:255–7. doi: 10.1038/382255a0
46. Koob GF, Bloom FE. Cellular and molecular mechanisms of drug dependence. Science (1988) 242:715–23. doi: 10.1126/science.2903550
47. Fischman MW, Schuster CR, Javaid J, Hatano Y, Davis J. Acute tolerance development to the cardiovascular and subjective effects of cocaine. J Pharmacol Exp Ther. (1985) 235:677–82.
48. Hyman SE, Malenka RC. Addiction and the brain: the neurobiology of compulsion and its persistence. Nat Rev Neurosci. (2001) 2:695–703. doi: 10.1038/35094560
49. Robinson TE, Berridge KC. The psychology and neurobiology of addiction: an incentive-sensitization view. Addiction (2000) 95 Suppl. 2:S91–117. doi: 10.1046/j.1360-0443.95.8s2.19.x
50. Gerdeman GL, Partridge JG, Lupica CR, Lovinger DM. It could be habit forming: drugs of abuse and striatal synaptic plasticity. Trends Neurosci. (2003) 26:184–92. doi: 10.1016/S0166-2236(03)00065-1
51. Waelti P, Dickinson A, Schultz W. Dopamine responses comply with basic assumptions of formal learning theory. Nature (2001) 412:43–8. doi: 10.1038/35083500
52. Berridge KC, Robinson TE. What is the role of dopamine in reward: hedonic impact, reward learning, or incentive salience? Brain Res Rev. (1998) 28:309–69. doi: 10.1016/S0165-0173(98)00019-8
53. De Vries TJ, Schoffelmeer ANM. Cannabinoid CB1 receptors control conditioned drug seeking. Trends Pharmacol Sci. (2005) 26:420–6. doi: 10.1016/j.tips.2005.06.002
54. Gerdeman GL, Schechter JB, French ED. Context-specific reversal of cocaine sensitization by the CB1 cannabinoid receptor antagonist rimonabant. Neuropsychopharmacology (2008) 33:2747–59. doi: 10.1038/sj.npp.1301648
55. Sloan ME, Gowin JL, Ramchandani VA, Hurd YL, Le Foll B. The endocannabinoid system as a target for addiction treatment: trials and tribulations. Neuropharmacology (2017) 124:73–83. doi: 10.1016/j.neuropharm.2017.05.031
56. Hoffman AF, Riegel AC, Lupica CR. Functional localization of cannabinoid receptors and endogenous cannabinoid production in distinct neuron populations of the hippocampus. Eur J Neurosci. (2003) 18:524–34. doi: 10.1046/j.1460-9568.2003.02773.x
57. Stern CAJ, Carvalho CR de, Bertoglio LJ, Takahashi RN. Effects of cannabinoid drugs on aversive or rewarding drug-associated memory extinction and reconsolidation. Neuroscience (2018) 370:62–80. doi: 10.1016/j.neuroscience.2017.07.018
58. Parsons LH, Hurd YL. Endocannabinoid signalling in reward and addiction. Nat Rev Neurosci. (2015) 16:579–94. doi: 10.1038/nrn4004
59. Brancato A, Cavallaro A, Lavanco G, Plescia F, Cannizzaro C. Reward-related limbic memory and stimulation of the cannabinoid system: an upgrade in value attribution? J Psychopharmacol. (2018) 32:204–14. doi: 10.1177/0269881117725683
60. Brancato A, Lavanco G, Cavallaro A, Plescia F, Cannizzaro C. The use of the emotional-object recognition as an assay to assess learning and memory associated to an aversive stimulus in rodents. J Neurosci Methods (2016) 274:106–15. doi: 10.1016/j.jneumeth.2016.09.010
61. Campolongo P, Ratano P, Manduca A, Scattoni ML, Palmery M, Trezza V, et al. The endocannabinoid transport inhibitor AM404 differentially modulates recognition memory in rats depending on environmental aversiveness. Front Behav Neurosci. (2012) 6:1–10. doi: 10.3389/fnbeh.2012.00011
62. Draycott B, Loureiro M, Ahmad T, Tan H, Zunder J, Laviolette SR. Cannabinoid transmission in the prefrontal cortex bi-phasically controls emotional memory formation via functional interactions with the ventral tegmental area. J Neurosci. (2014) 34:13096–109. doi: 10.1523/JNEUROSCI.1297-14.2014
63. Fusar-Poli P, Crippa JA, Bhattacharyya S, Bogwardt SJ, Allen P, Martin-Santos R, et al. Distinct effects of D9-tetrahydrocannabinol and cannabidiol on neural activation during emotional processing. Arch Gen Psychiatry (2009) 66:95–105. doi: 10.1001/archgenpsychiatry.2008.519
64. Bhattacharyya S, Morrison PD, Fusar-Poli P, Martin-Santos R, Borgwardt S, Winton-Brown T, et al. Opposite effects of Δ-9-tetrahydrocannabinol and cannabidiol on human brain function and psychopathology. Neuropsychopharmacology (2010) 35:764–74. doi: 10.1038/npp.2009.184
65. Heifets BD, Castillo PE. Endocannabinoid signaling and long-term synaptic plasticity. Annu Rev Physiol. (2009) 71:283–306. doi: 10.1146/annurev.physiol.010908.163149
66. Hyman SE, Malenka RC, Nestler EJ. Neural mechanisms of addiction: the role of reward-related learning and memory. Annu Rev Neurosci. (2006) 29:565–98. doi: 10.1146/annurev.neuro.29.051605.113009
67. Chambers RA. Impulsivity, dual diagnosis, and the structure of motivated behavior in addiction. Behav Brain Sci. (2008) 31:443–4. doi: 10.1017/S0140525X08004792
68. Lee JLC, Bertoglio LJ, Guimarães FS, Stevenson CW. Cannabidiol regulation of emotion and emotional memory processing: relevance for treating anxiety-related and substance abuse disorders. Br J Pharmacol. (2017) 174:3242–56. doi: 10.1111/bph.13724
69. Yu L, Wang X, Zhao M, Liu Y, Li Y, Li F, et al. Effects of cannabinoid CB1 receptor antagonist rimonabant in consolidation and reconsolidation of methamphetamine reward memory in mice. Psychopharmacology (Berl). (2009) 204:203–11. doi: 10.1007/s00213-008-1450-y
70. Hu SS, Liu Y, Yu L. Medial prefrontal cannabinoid CB 1 receptors modulate consolidation and extinction of cocaine-associated memory in mice. Psychopharmacology (Berl). (2015) 232:1803–15. doi: 10.1007/s00213-014-3812-y
71. de Carvalho CR, Takahashi RN. Cannabidiol disrupts the reconsolidation of contextual drug-associated memories in Wistar rats. Addict Biol. (2017) 22:742–51. doi: 10.1111/adb.12366
72. Colombo G, Serra S, Brunetti G, Gomez R, Melis S, Vacca G, et al. Stimulation of voluntary ethanol intake by cannabinoid receptor agonists in ethanol-preferring sP rats. Psychopharmacology (Berl). (2002) 159:181–7. doi: 10.1007/s002130100887
73. Thanos PK, Dimitrakakis ES, Rice O, Gifford A, Volkow ND. Ethanol self-administration and ethanol conditioned place preference are reduced in mice lacking cannabinoid CB1 receptors. Behav Brain Res. (2005) 164:206–13. doi: 10.1016/j.bbr.2005.06.021
74. Houchi H, Babovic D, Pierrefiche O, Ledent C, Daoust M, Naassila M. CB1 receptor knockout mice display reduced ethanol-induced conditioned place preference and increased striatal dopamine D2 receptors. Neuropsychopharmacology (2005) 30:339–49. doi: 10.1038/sj.npp.1300568
75. Gamaleddin I, Wertheim C, Zhu AZX, Coen KM, Vemuri K, Makryannis A, et al. Cannabinoid receptor stimulation increases motivation for nicotine and nicotine seeking. Addict Biol. (2012) 17:47–61. doi: 10.1111/j.1369-1600.2011.00314.x
76. Solinas M, Panlilio LV, Goldberg SR. Exposure to Δ-9-tetrahydrocannabinol (THC) increases subsequent heroin taking but not heroin's reinforcing efficacy: a self-administration study in rats. Neuropsychopharmacology (2004) 29:1301–11. doi: 10.1038/sj.npp.1300431
77. Solinas M, Panlilio LV, Tanda G, Makriyannis A, Matthews SA, Goldberg SR. Cannabinoid agonists but not inhibitors of endogenous cannabinoid transport or metabolism enhance the reinforcing efficacy of heroin in rats. Neuropsychopharmacology (2005) 30:2046–57. doi: 10.1038/sj.npp.1300754
78. Levin FR, Mariani JJ, Brooks DJ, Pavlicova M, Cheng W, Nunes EV. Dronabinol for the treatment of cannabis dependence: A randomized, double-blind, placebo-controlled trial. Drug Alcohol Depend. (2011) 116:142–50. doi: 10.1016/j.drugalcdep.2010.12.010
79. Vandrey R, Stitzer ML, Mintzer MZ, Huestis MA, Murray JA, Lee D. The dose effects of short-term dronabinol (oral THC) maintenance in daily cannabis users. Drug Alcohol Depend. (2013) 128:64–70. doi: 10.1016/j.drugalcdep.2012.08.001
80. Herrmann ES, Cooper ZD, Bedi G, Ramesh D, Reed SC, Comer SD, et al. Effects of zolpidem alone and in combination with nabilone on cannabis withdrawal and a laboratory model of relapse in cannabis users. Psychopharmacology (Berl). (2016) 233:2469–78. doi: 10.1007/s00213-016-4298-6
81. Maccioni P, Colombo G, Carai MA. Blockade of the cannabinoid CB1 receptor and alcohol dependence: preclinical evidence and preliminary clinical data. CNS Neurol Disord Drug Targets (2010) 9:55–9. doi: 10.2174/187152710790966623
82. Arnone M, Maruani J, Chaperon F, Thiébot MH, Poncelet M, Soubrié P, et al. Selective inhibition of sucrose and ethanol intake by SR 141716, an antagonist of central cannabinoid (CB1) receptors. Psychopharmacology (Berl). (1997) 132:104–6.
83. Diergaarde L, de Vries W, Raasø H, Schoffelmeer ANM, De Vries TJ. Contextual renewal of nicotine seeking in rats and its suppression by the cannabinoid-1 receptor antagonist Rimonabant (SR141716A). Neuropharmacology (2008) 55:712–6. doi: 10.1016/j.neuropharm.2008.06.003
84. Cohen C, Perrault G, Griebel G, Soubrié P. Nicotine-associated cues maintain nicotine-seeking behavior in rats several weeks after nicotine withdrawal: reversal by the cannabinoid (CB1) receptor antagonist, rimonabant (SR141716). Neuropsychopharmacology (2005) 30:145–55. doi: 10.1038/sj.npp.1300541
85. De Vries TJ, Homberg JR, Binnekade R, Raasø H, Schoffelmeer ANM. Cannabinoid modulation of the reinforcing and motivational properties of heroin and heroin-associated cues in rats. Psychopharmacology (Berl). (2003) 168:164–9. doi: 10.1007/s00213-003-1422-1
86. Cohen C, Perrault G, Voltz C, Steinberg R, Soubrié P. SR141716, a central cannabinoid (CB1) receptor antagonist, blocks the motivational and dopamine-releasing effects of nicotine in rats. Behav Pharmacol. (2002) 13:451–63. doi: 10.1097/00008877-200209000-00018
87. Braida D, Iosuè S, Pegorini S, Sala M. 3,4 Methylenedioxymethamphetamine-induced conditioned place preference (CPP) is mediated by endocannabinoid system. Pharmacol Res. (2005) 51:177–82. doi: 10.1016/j.phrs.2004.07.009
88. Chaperon F, Soubrié P, Puech AJ, Thiébot MH. Involvement of central cannabinoid (CB1) receptors in the establishment of place conditioning in rats. Psychopharmacology (Berl). (1998) 135:324–32.
89. De Vries TJ, Shaham Y, Homberg JR, Crombag H, Schuurman K, Dieben J, et al. A cannabinoid mechanism in relapse to cocaine seeking. Nat Med. (2001) 7:1151–4. doi: 10.1038/nm1001-1151
90. Cossu G, Ledent C, Fattore L, Imperato A, Böhme GA, Parmentier M, et al. Cannabinoid CB1 receptor knockout mice fail to self-administer morphine but not other drugs of abuse. Behav Brain Res. (2001) 118:61–5. doi: 10.1016/S0166-4328(00)00311-9
91. Caillé S, Parsons LH. Cannabinoid modulation of opiate reinforcement through the ventral striatopallidal pathway. Neuropsychopharmacology (2006) 31:804–13. doi: 10.1038/sj.npp.1300848
92. Soria G, Mendizábal V, Touriño C, Robledo P, Ledent C, Parmentier M, et al. Lack of CBI cannabinoid receptor impairs cocaine self-administration. Neuropsychopharmacology (2005) 30:1670–80. doi: 10.1038/sj.npp.1300707
93. Huestis MA, Boyd SJ, Heishman SJ, Preston KL, Bonnet D, Le Fur G, et al. Single and multiple doses of rimonabant antagonize acute effects of smoked cannabis in male cannabis users. Psychopharmacology (Berl). (2007) 194:505–15. doi: 10.1007/s00213-007-0861-5
94. Gorelick DA, Heishman SJ, Preston KL, Nelson RA, Moolchan ET, Huestis MA. The cannabinoid CB1 receptor antagonist rimonabant attenuates the hypotensive effect of smoked marijuana in male smokers. Am Heart J. (2006) 151:1–5. doi: 10.1016/j.ahj.2005.11.006
95. Cahill K, Ussher MH. Cannabinoid type 1 receptor antagonists for smoking cessation. Cochrane Database Syst Rev. (2011) 2017:1–26. doi: 10.1002/14651858.CD005353.pub4
96. Soyka M, Koller G, Schmidt P, Lesch OM, Leweke M, Fehr C, et al. Cannabinoid receptor 1 blocker rimonabant (SR 141716) for treatment of alcohol dependence: results from a placebo-controlled, double-blind trial. J Clin Psychopharmacol. (2008) 28:317–24. doi: 10.1097/JCP.0b013e318172b8bc
97. Cohen RA, Harezlak J, Schifitto G, Hana G, Clark U, Gongvatana A, et al. Effects of nadir CD4 count and duration of human immunodeficiency virus infection on brain volumes in the highly active antiretroviral therapy era. J Neurovirol. (2010) 16:25–32. doi: 10.3109/13550280903552420
98. Christensen R, Kristensen PK, Bartels EM, Bliddal H, Astrup A. Efficacy and safety of the weight-loss drug rimonabant: a meta-analysis of randomised trials. Lancet (2007) 370:1706–13. doi: 10.1016/S0140-6736(07)61721-8
99. Pertwee RG. Cannabinoid pharmacology: the first 66 years. Br J Pharmacol. (2006) 147:S163–71. doi: 10.1038/sj.bjp.0706406
100. Santos RG dos, Hallak JEC, Zuardi AW, Crippa JA de S. Cannabidiol for the treatment of drug use disorders. In: V. P. Preedy, Editor. Handbook of Cannabis and Related Pathologies, London: Elsevier Inc. (2017). p. 939–46.
101. Kathmann M, Flau K, Redmer A, Tränkle C, Schlicker E. Cannabidiol is an allosteric modulator at mu- and delta-opioid receptors. Arch Pharmacol. (2006) 372:354–61. doi: 10.1007/s00210-006-0033-x
102. Russo EB, Burnett A, Hall B, Parker KK. Agonistic properties of cannabidiol at 5-HT1a receptors. Neurochem Res. (2005) 30:1037–43. doi: 10.1007/s11064-005-6978-1
103. Campos AC, Guimarães FS. Involvement of 5HT1A receptors in the anxiolytic-like effects of cannabidiol injected into the dorsolateral periaqueductal gray of rats. Psychopharmacology (Berl). (2008) 199:223–30. doi: 10.1007/s00213-008-1168-x
104. Thomas A, Baillie GL, Phillips AM, Razdan RK, Ross RA, Pertwee RG. Cannabidiol displays unexpectedly high potency as an antagonist of CB1 and CB2 receptor agonists in vitro. Br J Pharmacol. (2007) 150:613–23. doi: 10.1038/sj.bjp.0707133
105. Laprairie RB, Bagher AM, Kelly MEM, Denovan-Wright EM. Cannabidiol is a negative allosteric modulator of the cannabinoid CB 1 receptor. Br J Pharmacol. (2015) 172:4790–805. doi: 10.1111/bph.13250
106. Tham M, Yilmaz O, Alaverdashvili M, Kelly MEM, Denovan-wright EM, Laprairie RB. Allosteric and orthosteric pharmacology of cannabidiol and cannabidiol-dimethylheptyl at the type 1 and type 2 cannabinoid receptors. Br J Pharmacol. (2018). doi: 10.1111/bph.14440. [Epub ahead of print].
107. Straiker A, Dvorakova M, Zimmowitch A, Mackie K. Cannabidiol inhibits endocannabinoid signaling in autaptic hippocampal neurons. Mol Pharmacol. (2018) 94:743–8. doi: 10.1124/mol.118.111864
108. Bergamaschi MM, Queiroz RHC, Zuardi AW, Crippa JAS. Safety and side effects of cannabidiol, a Cannabis sativa constituent. Curr Drug Saf. (2011) 6:237–49. doi: 10.2174/157488611798280924
109. Rohleder C, Müller JK, Lange B, Leweke FM. Cannabidiol as a potential new type of an antipsychotic. A critical review of the evidence. Front Pharmacol. (2016) 7:422. doi: 10.3389/fphar.2016.00422
110. Iffland K, Grotenhermen F. An update on safety and side effects of cannabidiol: a review of clinical data and relevant animal studies. Cannabis Cannabinoid Res. (2017) 2:139–54. doi: 10.1089/can.2016.0034
111. Taylor L, Gidal B, Blakey G, Tayo B, Morrison G. A phase I, randomized, double-blind, placebo-controlled, single ascending dose, multiple dose, and food effect trial of the safety, tolerability and pharmacokinetics of highly purified cannabidiol in healthy subjects. CNS Drugs (2018) 32:1053–67. doi: 10.1007/s40263-018-0578-5
112. Babalonis S, Haney M, Malcolm RJ, Lofwall MR, Votaw VR, Sparenborg S, et al. Oral cannabidiol does not produce a signal for abuse liability in frequent marijuana smokers. Drug Alcohol Depend. (2017) 172:9–13. doi: 10.1016/j.drugalcdep.2016.11.030
113. Parker LA, Burton P, Sorge RE, Yakiwchuk C, Mechoulam R. Effect of low doses of Δ9-tetrahydrocannabinol and cannabidiol on the extinction of cocaine-induced and amphetamine-induced conditioned place preference learning in rats. Psychopharmacology (Berl). (2004) 175:360–6. doi: 10.1007/s00213-004-1825-7
114. Murillo-Rodríguez E, Palomero-Rivero M, Millán-Aldaco D, Mechoulam R, Drucker-Colín R. Effects on sleep and dopamine levels of microdialysis perfusion of cannabidiol into the lateral hypothalamus of rats. Life Sci. (2011) 88:504–11. doi: 10.1016/j.lfs.2011.01.013
115. Ren Y, Whittard J, Higuera-Matas A, Morris CV, Hurd YL. Cannabidiol, a nonpsychotropic component of cannabis, inhibits cue-induced heroin seeking and normalizes discrete mesolimbic neuronal disturbances. J Neurosci. (2009) 29:14764–9. doi: 10.1523/JNEUROSCI.4291-09.2009
116. Renard J, Loureiro M, Rosen LG, Zunder J, de Oliveira C, Schmid S, et al. Cannabidiol counteracts amphetamine-induced neuronal and behavioral sensitization of the mesolimbic dopamine pathway through a novel mTOR/p70S6 kinase signaling pathway. J Neurosci. (2016) 36:5160–9. doi: 10.1523/JNEUROSCI.3387-15.2016
117. Zuardi AW, Hallak JEC, Crippa JAS. Interaction between cannabidiol (CBD) and Δ9-tetrahydrocannabinol (THC): influence of administration interval and dose ratio between the cannabinoids. Psychopharmacology (Berl). (2012) 219:247–9. doi: 10.1007/s00213-011-2495-x
118. Fischer B, Kuganesan S, Gallassi A, Malcher-Lopes R, van den Brink W, Wood E. Addressing the stimulant treatment gap: a call to investigate the therapeutic benefits potential of cannabinoids for crack-cocaine use. Int J Drug Policy (2015) 26:1177–82. doi: 10.1016/j.drugpo.2015.09.005
119. Hurd YL, Yoon M, Manini AF, Hernandez S, Olmedo R, Ostman M, et al. Early phase in the development of cannabidiol as a treatment for addiction: opioid relapse takes initial center stage. Neurotherapeutics (2015) 12:807–15. doi: 10.1007/s13311-015-0373-7
120. Hurd YL. Cannabidiol: swinging the marijuana pendulum from ‘weed’ to medication to treat the opioid epidemic. Trends Neurosci. (2017) 40:124–7. doi: 10.1016/j.tins.2016.12.006
121. Filev R, Engelke DS, Da Silveira DX, Mello LE, Santos-Junior JG. THC inhibits the expression of ethanol-induced locomotor sensitization in mice. Alcohol (2017) 65:31–5. doi: 10.1016/j.alcohol.2017.06.004
122. Luján MÁ, Castro-Zavala A, Alegre-Zurano L, Valverde O. Repeated Cannabidiol treatment reduces cocaine intake and modulates neural proliferation and CB1R expression in the mouse hippocampus. Neuropharmacology (2018) 143:163–75. doi: 10.1016/j.neuropharm.2018.09.043
123. Trigo JM, Soliman A, Quilty LC, Fischer B, Selby P, Barnes AJ, et al. Nabiximols combined with motivational enhancement/cognitive behavioral therapy for the treatment of cannabis dependence: a pilot randomized clinical trial. PLoS ONE (2018) 13:e0190768. doi: 10.1371/journal.pone.0190768
124. Solowij N, Broyd SJ, Beale C, Prick J-A, Greenwood L, van Hell H, et al. Therapeutic effects of prolonged cannabidiol treatment on psychological symptoms and cognitive function in regular cannabis users: a pragmatic open-label clinical trial. Cannabis Cannabinoid Res. (2018) 3:21–34. doi: 10.1089/can.2017.0043
125. Morgan CJA, Das RK, Joye A, Curran HV, Kamboj SK. Cannabidiol reduces cigarette consumption in tobacco smokers: preliminary findings. Addict Behav. (2013) 38:2433–6. doi: 10.1016/j.addbeh.2013.03.011
126. Hindocha C, Freeman TP, Grabski M, Stroud JB, Crudgington H, Davies AC, et al. Cannabidiol reverses attentional bias to cigarette cues in a human experimental model of tobacco withdrawal. Addiction (2018) 113:1696–705. doi: 10.1111/add.14243
127. Markos JR, Harris HM, Gul W, Elsohly MA, Sufka KJ. Effects of cannabidiol on morphine conditioned place preference in mice. Planta Med. (2018) 84:221–4. doi: 10.1055/s-0043-117838
128. Shannon S, Opila-lehman J. Cannabidiol oil for decreasing addictive use of marijuana: a case report. Integr Med. (2015) 14:31–5.
129. Trigo JM, Soliman A, Staios G, Quilty L, Fischer B, George TP, et al. Sativex associated with behavioral-relapse prevention strategy as treatment for cannabis dependence: a case series. J Addict Med. (2016) 10:274–9. doi: 10.1097/ADM.0000000000000229
130. Allsop DJ, Copeland J, Lintzeris N, Dunlop AJ, Montebello M, Sadler C, et al. Nabiximols as an agonist replacement therapy during cannabis withdrawal: a randomized clinical trial. JAMA Psychiatry (2014) 71:281–91. doi: 10.1001/jamapsychiatry.2013.3947
131. Viudez-Martínez A, García-Gutiérrez MS, Navarrón CM, Morales-Calero MI, Navarrete F, Torres-Suárez AI, et al. Cannabidiol reduces ethanol consumption, motivation and relapse in mice. Addict Biol. (2018) 23:154–64. doi: 10.1111/adb.12495
132. Katsidoni V, Anagnostou I, Panagis G. Cannabidiol inhibits the reward-facilitating effect of morphine: involvement of 5-HT 1A receptors in the dorsal raphe nucleus. Addict Biol. (2013) 18:286–96. doi: 10.1111/j.1369-1600.2012.00483.x
133. Mahmud A, Gallant S, Sedki F, D'Cunha T, Shalev U. Effects of an acute cannabidiol treatment on cocaine self-administration and cue-induced cocaine seeking in male rats. J Psychopharmacol. (2017) 31:96–104. doi: 10.1177/0269881116667706
134. Hay GL, Baracz SJ, Everett NA, Roberts J, Costa PA, Arnold JC, et al. Cannabidiol treatment reduces the motivation to self-administer methamphetamine and methamphetamine-primed relapse in rats. J Psychopharmacol. (2018) 32:1369–78. doi: 10.1177/0269881118799954
135. Crippa JAS, Hallak JEC, Machado-de-Sousa JP, Queiroz RHC, Bergamaschi M, Chagas MHN, et al. Cannabidiol for the treatment of cannabis withdrawal syndrome: a case report. J Clin Pharm Ther. (2013) 38:162–4. doi: 10.1111/jcpt.12018
136. Hine B, Torrelio M, Gershon S. Interactions between cannabidiol and Δ9-THC during abstinence in morphine-dependent rats. Life Sci. (1975) 17:851–8. doi: 10.1016/0024-3205(75)90435-X
137. Bhargava HN. Effect of some cannabinoids on naloxone-precipitated abstinence in morphine-dependent mice. Psychopharmacology (Berl). (1976) 49:267–70. doi: 10.1007/BF00426828
138. Chesher GB, Jackson DM. The quasi-morphine withdrawal syndrome: effect of cannabinol, cannabidiol and tetrahydrocannabinol. Pharmacol Biochem Behav. (1985) 23:13–5. doi: 10.1016/0091-3057(85)90122-4
139. Karimi-Haghighi S, Haghparast A. Cannabidiol inhibits priming-induced reinstatement of methamphetamine in REM sleep deprived rats. Prog Neuro-Psychopharmacology Biol Psychiatry (2018) 82:307–13. doi: 10.1016/j.pnpbp.2017.08.022
140. Gonzalez-Cuevas G, Martin-Fardon R, Kerr TM, Stouffer DG, Parsons LH, Hammell DC, et al. Unique treatment potential of cannabidiol for the prevention of relapse to drug use: preclinical proof of principle. Neuropsychopharmacology (2018) 43:2036–45. doi: 10.1038/s41386-018-0050-8
141. Budney AJ, Vandrey RG, Stanger C. Pharmacological and psychosocial interventions for cannabis use disorders. Rev Bras Psiquiatr. (2010) 32:46–55. doi: 10.1590/S1516-44462010000500008
142. Vann RE, Gamage TF, Warner JA, Marshall EM, Taylor NL, Martin BR, et al. Divergent effects of cannabidiol on the discriminative stimulus and place conditioning effects of Δ9-tetrahydrocannabinol. Drug Alcohol Depend. (2008) 94:191–8. doi: 10.1016/j.drugalcdep.2007.11.017
143. Robson P. Abuse potential and psychoactive effects of δ-9-tetrahydrocannabinol and cannabidiol oromucosal spray (Sativex), a new cannabinoid medicine. Expert Opin Drug Saf. (2011) 10:675–85. doi: 10.1517/14740338.2011.575778
144. Trigo JM, Lagzdins D, Rehm J, Selby P, Gamaleddin I, Fischer B, et al. Effects of fixed or self-titrated dosages of Sativex on cannabis withdrawal and cravings. Drug Alcohol Depend. (2016) 161:298–306. doi: 10.1016/j.drugalcdep.2016.02.020
145. Allsop DJ, Lintzeris N, Copeland J, Dunlop A, McGregor IS. Cannabinoid replacement therapy (CRT): Nabiximols (Sativex) as a novel treatment for cannabis withdrawal. Clin Pharmacol Ther. (2015) 97:571–4. doi: 10.1002/cpt.109
146. Schoedel KA, Chen N, Hilliard A, White L, Stott C, Russo E, et al. A randomized, double-blind, placebo-controlled, crossover study to evaluate the subjective abuse potential and cognitive effects of nabiximols oromucosal spray in subjects with a history of recreational cannabis use. Hum Psychopharmacol Clin Exp. (2011) 26:224–36. doi: 10.1002/hup.1196
147. Socías ME, Kerr T, Wood E, Dong H, Lake S, Hayashi K, et al. Intentional cannabis use to reduce crack cocaine use in a Canadian setting: a longitudinal analysis. Addict Behav. (2017) 72:138–43. doi: 10.1016/j.addbeh.2017.04.006
148. Swift W, Wong A, Li KM, Arnold JC, McGregor IS. Analysis of cannabis seizures in NSW, Australia: cannabis potency and cannabinoid profile. PLoS ONE (2013) 8:e0070052. doi: 10.1371/journal.pone.0070052
149. Carroll KM, Onken LS. Behavioral therapies for drug abuse. Am J Psychiatry (2005) 162:1452–60. doi: 10.1176/appi.ajp.162.8.1452
150. Fusar-Poli P, Allen P, Bhattacharyya S, Crippa JA, Mechelli A, Borgwardt S, et al. Modulation of effective connectivity during emotional processing by delta-9-tetrahydrocannabinol and cannabidiol. Int J Neuropsychopharmacol. (2010) 13:421–32. doi: 10.1017/S1461145709990617
151. Norris C, Loureiro M, Kramar C, Zunder J, Renard J, Rushlow W, et al. Cannabidiol modulates fear memory formation through interactions with serotonergic transmission in the mesolimbic system. Neuropsychopharmacology (2016) 41:2839–50. doi: 10.1038/npp.2016.93
152. Torrens M, Fonseca F, Mateu G, Farré M. Efficacy of antidepressants in substance use disorders with and without comorbid depression: a systematic review and meta-analysis. Drug Alcohol Depend. (2005) 78:1–22. doi: 10.1016/j.drugalcdep.2004.09.004
153. Zlebnik NE, Cheer JF. Beyond the CB1 receptor: is cannabidiol the answer for disorders of motivation? Annu Rev Neurosci. (2016) 39:1–17. doi: 10.1146/annurev-neuro-070815-014038
154. Crippa JA, Guimarães FS, Campos AC, Zuardi AW. Translational Investigation of the therapeutic potential of cannabidiol (CBD): toward a new age. Front Immunol. (2018) 9:2009. doi: 10.3389/fimmu.2018.02009
155. Gruber SA, Rogowska J, Yurgelun-Todd DA. Altered affective response in marijuana smokers: an FMRI study. Drug Alcohol Depend. (2009) 105:139–53. doi: 10.1016/j.drugalcdep.2009.06.019
156. Trezza V, Campolongo P, Manduca A, Morena M, Palmery M, Vanderschuren LJMJ, et al. Altering endocannabinoid neurotransmission at critical developmental ages: impact on rodent emotionality and cognitive performance. Front Behav Neurosci. (2012) 6:2. doi: 10.3389/fnbeh.2012.00002
157. De Petrocellis L, Ligresti A, Moriello AS, Allarà M, Bisogno T, Petrosino S, et al. Effects of cannabinoids and cannabinoid-enriched Cannabis extracts on TRP channels and endocannabinoid metabolic enzymes. Br J Pharmacol. (2011) 163:1479–94. doi: 10.1111/j.1476-5381.2010.01166.x
158. Adamczyk P, Miszkiel J, McCreary AC, Filip M, Papp M, Przegalinski E. The effects of cannabinoid CB1, CB2 and vanilloid TRPV1 receptor antagonists on cocaine addictive behavior in rats. Brain Res. (2012) 1444:45–54. doi: 10.1016/j.brainres.2012.01.030
159. Trigo JM, Le Foll B. Inhibition of monoacylglycerol lipase (MAGL) enhances cue-induced reinstatement of nicotine-seeking behavior in mice. Psychopharmacology (Berl). (2016) 233:1815–22. doi: 10.1007/s00213-015-4117-5
160. Forget B, Guranda M, Gamaleddin I, Goldberg SR, Le Foll B. Attenuation of cue-induced reinstatement of nicotine seeking by URB597 through cannabinoid CB1 receptor in rats. Psychopharmacology (Berl). (2016) 233:1823–8. doi: 10.1007/s00213-016-4232-y
Keywords: endocannabinoid system, ECS, substance use disorder, treatment efficacy, cannabidiol, CBD, addiction
Citation: Chye Y, Christensen E, Solowij N and Yücel M (2019) The Endocannabinoid System and Cannabidiol's Promise for the Treatment of Substance Use Disorder. Front. Psychiatry 10:63. doi: 10.3389/fpsyt.2019.00063
Received: 30 November 2018; Accepted: 28 January 2019;
Published: 19 February 2019.
Edited by:
Alexander Mario Baldacchino, University of St Andrews, United KingdomReviewed by:
Carla Cannizzaro, Università degli Studi di Palermo, ItalyAviv M. Weinstein, Ariel University, Israel
Copyright © 2019 Chye, Christensen, Solowij and Yücel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yann Chye, eWFubnlpbmcuY2h5ZUBtb25hc2guZWR1
 Yann Chye
Yann Chye Erynn Christensen
Erynn Christensen Nadia Solowij
Nadia Solowij Murat Yücel
Murat Yücel