- 1Stress and Affective Disorders Programme, University of São Paulo, São Paulo, Brazil
- 2School of Community and Health Studies, Centennial College, Toronto, ON, Canada
- 3Centre for Affective Disorders, Department Psychological Medicine, King's College London, London, United Kingdom
Numerous studies have researched the aggravating and maintainer effect of Early Life Stress in patients adults with psychiatric disorders. This study examined the relationship between depression and subtypes of early life stress among 81 psychiatric patients treated at the inpatient Day Hospital Unit of a University General Hospital. Psychiatric diagnosis was confirmed according to the MINI International Neuropsychiatric Interview (MINI). The Childhood Trauma Questionnaire (CTQ) was used for evaluating as retrospective assessment of the presence of ELS on these patients, and we also evaluated the severity of hopelessness with the Beck Hopelessness Scale (BHS). Our results suggested that the occurrence of depression in adulthood is related to situations of emotional abuse, sexual, and physical neglect during childhood. The analysis between depression and childhood emotional abuse was significant after a multiple logistic regression analysis OR (IC 95%): 4.4 (1.7–11.2), even accounting for gender adjusted OR [AOR] 4.0; (IC 1.5–10.5); psychiatry family history AOR 3.8 (1.4–10.5); previous suicide attempted AOR 3.7; (1.4–10.5) and Hopelessness AOR 3.2 (1.11–9.4). Thus, these findings demonstrate emotional abuse as a significant risk factor to be part of the mechanism involved in the pathogenesis of depression related to early life stress.
Introduction
Recent studies have examined the effect of stress in the early stages of development of the individual demonstrating that when stress occurs early, can lead to “biological scars” lifelong (1). The Early Life Stress (ELS) is a variety of traumatic experiences that can occur during childhood and adolescence, such as abuse, neglect, parental loss, divorce of parents, caregivers with psychiatric disorders, childhood disease involving prolonged hospitalizations, lack of primary care, abandonment, deprivation of food, and adequate shelter, lack of encouragement and support, as well as family violence (2, 3). Numerous studies have studied the aggravating effect and maintainer of the ELS in psychiatric disorders in adults. Recognized studies (4–7) evidence the future impact of various early trauma on mental health. In the systematic review we conducted (8) the data demonstrated that individual exposure to adversities in childhood and adolescence is predictive of psychiatric disorders in adulthood, such as depression and borderline personality disorder. In this same direction, other systematic review evaluated the association between subtypes of ELS with psychiatric disorders in adults, finding that physical abuse, sexual, and unspecified neglect are associated with mood disorder and anxiety disorders, while emotional abuse is associated with personality disorder and schizophrenia and that the physical neglect is related to personality disorders (9). In consonance, some studies (10–12) showed that emotional abuse is associated with depressive symptoms in adults. Furthermore, the literature indicates that it is quite common co-occurrence of abuse or neglect, it is difficult occurs in a single subtype of ELS, so that the incidence may range around 40–95% of the sample (13, 14). The study by Chartier et al. (15), shown that among psychiatric patients with ELS, 37% of them had reports of the occurrence of more than one subtype of ELS. The study of Felitti et al. (16) showed that individuals who have experienced situations of child adversity likely to have experienced more than one subtype ELS varies around approximately 80%. According to Hahm et al. (17), the co-occurrence of ELS subtypes is an essential measure of the severity of psychopathology, since in many studies was associated with increased severity of psychiatric symptoms. In this sense, given the importance of stress in the development of psychiatric disorders, recently the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), included among its ratings a specific category for the diagnosis of Trauma and Stressor-Related Disorders (18). Thus, researchers also point to the need to analyze how stress triggers interact with psychopathology, showing that stress increases the risk for depression, but leave the individual susceptible to the occurrence of different types of stress (10). According to Heim and Nemeroff (19) children exposed to traumatic experiences in early childhood have an increased risk of developing depression. The persistent sensitization of the circuits of the central nervous system, which are integrally involved in the regulation of tension and emotion, may represent the underlying biological substrates to increased vulnerability to subsequent stress, predisposing these individuals to develop a broad range of physical and mental disorders which are known to express or worsen in relation to acute stress. The intense stress starts to play a substantial adverse effect on a person's life, affecting not only the mental health but physical, cognition, and occupational performance in everyday activities. Another important consequence of ELS is related to the increase of suicide attempts in individuals with psychiatric disorders who suffered ELS. Several studies have suggested an association between ELS and increased suicidality in adulthood (7, 20–24). The study by Sfoggia et al. (25) it was shown that adults with a history of severe abuse and neglect had more suicide attempts than those who reported no ELS. Also, in the survey conducted by Brown et al. (26) relevant data found, in which victims of sexual abuse has eight times more likely to suicide. Our previous data (27), demonstrated that among the ELS subtypes, significant association was found only between the emotional abuse subtype and psychiatric diagnoses. Emotional abuse was positively associated with psychopathology in adults, particularly with depressive disorders. The patients with a history of emotional abuse had higher severity in depression, hopelessness, suicidal ideation, anxiety, and impulsivity. Thus, the present study aimed to analyze the relationship between depression and subtypes of ELS among patients with psychiatric disorders, mainly control the analysis of the association between emotional abuse and patients with depression treated at the inpatient Day Hospital Unit of a General University Hospital.
Methods
Study Sample and Design
The sample was composed of 81 adult psychiatric patients, treated at inpatient Day Hospital Unit of a General University Hospital. The inclusion criteria for this study were patients with psychiatric diagnosis confirmed according to Mini International Neuropsychiatric Interview (MINI) (28, 29), in the follow-up inpatient Day Hospital Unit, aged 18–65 years. We excluded patients with any significant physical illness in acute, mental disorders caused by a general medical condition or resulting from the direct physiological effect of a substance, substance-related disorders, mental retardation, and patients in an acute psychotic episode, cognitive deficits, and neurological progressive and degenerative diseases.
Procedure and Measures
The study was approved by the Research Ethics Committee of the General University Hospital, Faculty of Medicine of Ribeirao Preto, University of Sao Paulo. Participants were informed that the purpose of the study was to investigate the association between early life stress and psychiatric disorders in adult life. Later, written informed consent was obtained from all patients, and the questionnaires included in this study were applied.
Demographic and Clinical Data
Clinical and sociodemographic characteristics (age, gender, religious practice, family history of psychiatric disorder, suicide attempt, among others) were obtained through the administration of a sociodemographic questionnaire developed by researchers. We also evaluated the severity of hopelessness with the Beck Hopelessness Scale [BHS; (30)]. This is a self-report questionnaire with 20 true-false statements developed to assess the extent of positive and negative beliefs about the future. The version in Portuguese was translated and adapted by Cunha (31).
Psychiatric Diagnosis
The assessment of psychiatric diagnosis was conducted using Mini International Neuropsychiatric Interview [MINI; (28)], the version in Portuguese translated and adapted by Amorim (29). The MINI is a brief structured interview designed to assess criteria for the majority of psychiatric disorders classified in DSM-IV and ICD-10. There is a version called MINI PLUS, intended for assessment of the primary psychiatric diagnosis throughout life, in clinical and research psychiatry and systematically explores all the criteria for inclusion and exclusion and chronology (onset and duration of the disorder, number of episodes) (29). All subjects were interviewed by two senior psychiatrists (MFJ; CWB) trained and certified to the use of the standardized interviews. The interviewers had long-standing experience in the administration of standardized interviews. In the total sample, the distribution of psychiatric disorders was as follows: more than 75% had a diagnosis of mood disorders, prevailing depressive disorders (n = 44; 54%), followed by bipolar disorder (n = 17; 21%). The other diagnoses assessed were anxiety disorders (n = 10; 12.3%), eating disorders (n = 3; 4%), and others (n = 7; 8%). We did not include patients with diagnoses of substance use disorder in the sample because the Day Hospital Unit does not admit patients with this diagnosis.
Subtypes of Early Life Stress
The subtypes of ELS was assessed using the Childhood Trauma Questionnaire [CTQ; (32)]. The CTQ is a retrospective self-report questionnaire that investigates the history of abuse and neglect during childhood and can be applied to adolescents (from 12 years) and adults, where the responder assigns values of frequency to 28 sentences, graduate issues related to situations arising in childhood. The CTQ evaluates five subtypes of early life stress:
• Emotional abuse: verbal assaults on a child's sense of worth or well-being or any humiliating or demeaning behavior directed toward a child by an adult or older person;
• Physical abuse: bodily assaults on a child by an adult or older person that posed a risk of or resulted in injury;
• Sexual abuse: sexual contact or conduct between a child younger than 18 years of age and an adult or older person;
• Emotional neglect: the failure of caretakers to meet children's basic emotional and psychological needs, including love, belonging, nurturance, and support;
• Physical neglect: the failure of caretakers to provide for a child's basic physical needs, including food, shelter, clothing, safety, and healthcare (inadequate parental supervision was also included in this definition if it placed children's security in jeopardy) (3).
The items are rated on a Likert scale ranging from 1 (never) to 5 (very often). Furthermore, the scores range from 5 to 25 for each subtype of ELS. A cut-point for early life stress, and its subtypes (emotional, physical and sexual abuse, and emotional and physical neglect), was defined as when one of these experiences before the age of 18 reached a degree of at least moderate to severe, according to classification in the CTQ (3, 32–34). The version in Portuguese was translated and adapted by Grassi-Oliveira et al. (35).
Statistical Analysis
Logistic multiple regression analysis was conducted in Stata 9 statistical program to test the relationship between depression and emotional abuse when controlled by independent variables. Univariate analysis of depression was performed with each of the analyzed independent variables. We conducted the analysis of association between ELS and all psychiatric disorders. However, according to data presented in Table 2, there was no significant difference between the groups with and with- out ELS (χ2 = 8.44, df = 6.0, p = 0.188) in relation to the distribution of psychiatric diagnoses.
In addition, we performed a second statistical analysis, comparing ELS subtypes with psychiatric disorders. Thus, significant association was found only between the emotional abuse subtype and psychiatric diagnoses. Those with p < 0.30 or that are relevant in the literature to the Raw Model: Depression Disorder + Emotional Abuse and Model 2 = Raw Model + Gender; Model 3 = Model 2 + Familiar History of Mental Disorders; Model 4 = Model 3 + Suicide Attempt; and Model 5 = Model 4 + Hopelessness; were included in the multiple models using the stepwise forward strategy when the association between depression and emotional abuse in childhood was adjusted for all independent variables. Remained for analysis the variables with p < 0.20 or those that adjusted the dependent variables. We also used Chi-square for analysis of the occurrence of subtypes of ELS and the Student t-test for analysis of CTQ scores.
Results
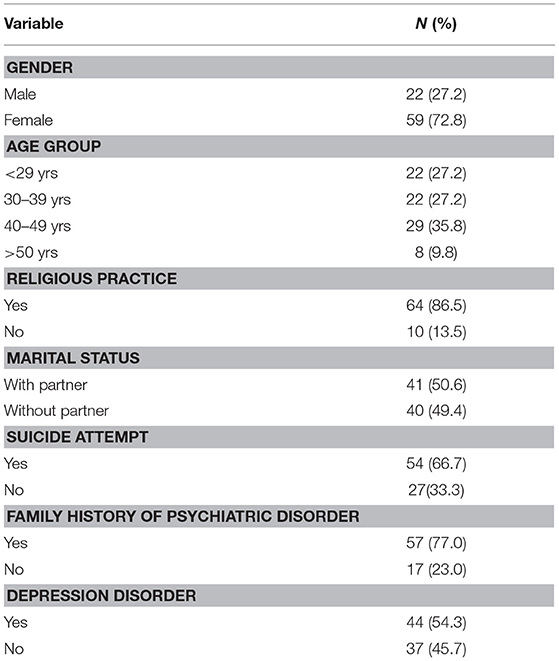
The participants were predominantly women (72.8%), under 40 years of age, reporting religious practice (86.5%) and with a family history of mental disorder (77.0%). Concerning, the psychiatric diagnosis, 54% of patients seen at the hospital had depression, followed by Bipolar disorder (21.0%). The other diagnoses assessed were: Anxiety Disorders (12.3%), Schizophrenia and Other Psychotic Disorders (6.2%), Eating Disorders (3.7%), Dissociative Disorders (1.2%), Impulse Control Disorders not elsewhere classified (1.2%). We do not include patients with diagnoses of Substance Use Disorder in the sample because the University Day Hospital does not include patients with this diagnosis. Further details can be found in Table 1.
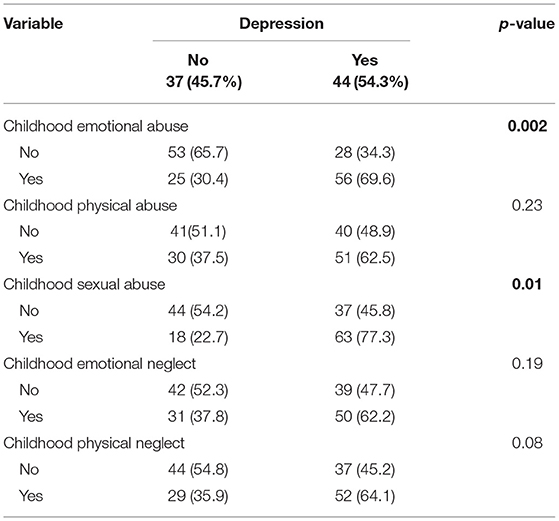
The data regarding the subtypes of early life stress are shown in Table 2. There has been a higher frequency of childhood emotional abuse among patients, while the sexual abuse had a lower occurrence, see in Table 3.
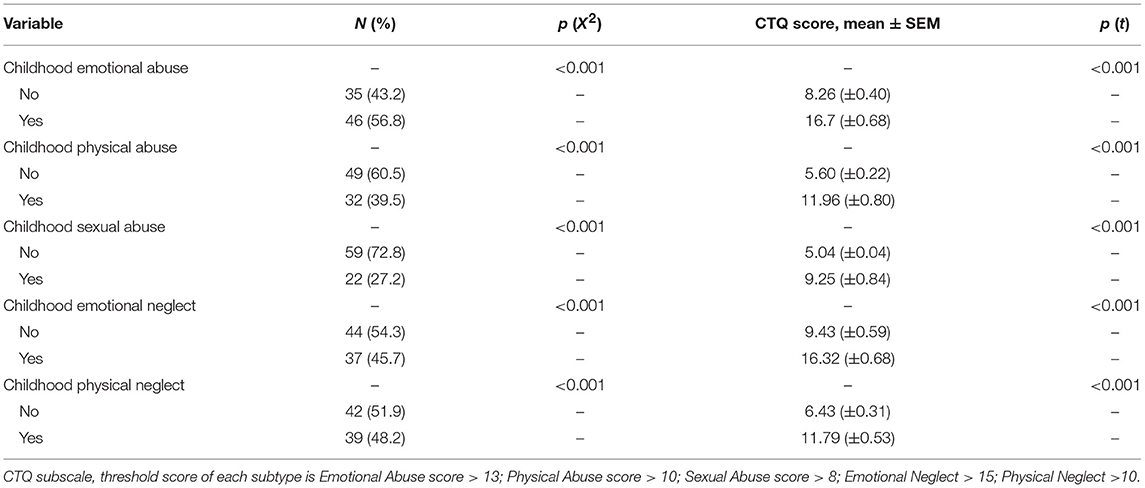
Table 2. Occurrence and CTQ scores of subtypes of early life stress among the whole sample (n = 81).
In this population, depression was associated with emotional abuse and sexual abuse, with considerable statistical significance. However, the relationship with physical neglect, demonstrated a trend (p = 0.08). These data indicate that the occurrence of depression in adulthood is related to situations of emotional abuse, sexual and physical neglect during childhood.
The analysis of the chances of occurrence of depression according to the epidemiological characteristics showed that women are more exposed compared with men. Moreover, it was also observed an increase of about four times the chance of depression among people who have suffered emotional or sexual abuse in childhood or who reported at least one suicide attempt throughout life. Patients with a high level of hopelessness also showed a higher chance of depression (Table 4).
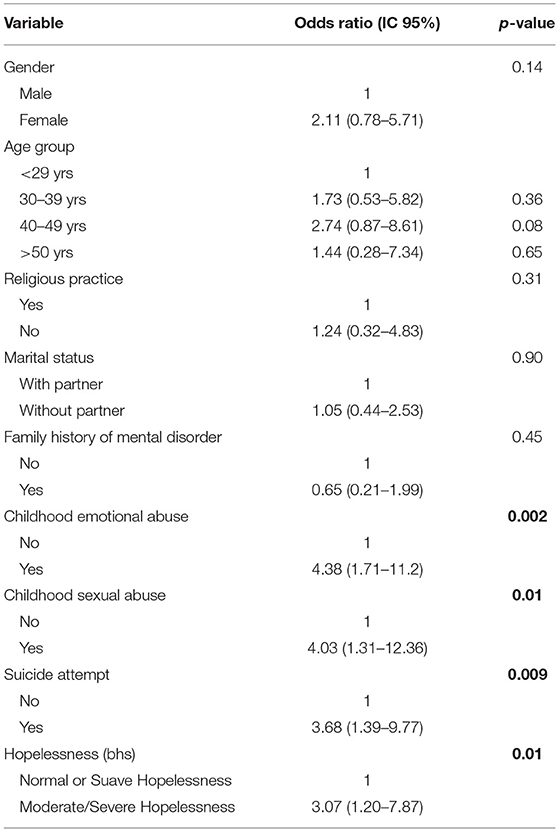
Table 4. Univariate logistic regression between depression and childhood emotional abuse among patients.
Patients with a history of childhood emotional abuse had a frequency of 4.38 higher of depression compared to those without such a history in the bivariate regression (Table 5). In the following models, with adjustments for demographic variables and health conditions, the magnitude of odds ratio decreased, although the adjusted odds ratio was still 3.23 times higher in the group exposed to emotional abuse during childhood (p-value 0.031). Multiple Logistic regression analysis between depression and childhood emotional abuse was significant after a multiple logistic regression analysis OR (IC 95%): 4.4 (1.7–11.2), even accounting for gender adjusted OR [AOR] 4.0, (1.5–10.5); psychiatry family history AOR 3.8 (1.4–10.5); previous suicide attempted AOR 3.7; (1.4–10.5) and Hopelessness AOR 3.2 (1.11–9.4).
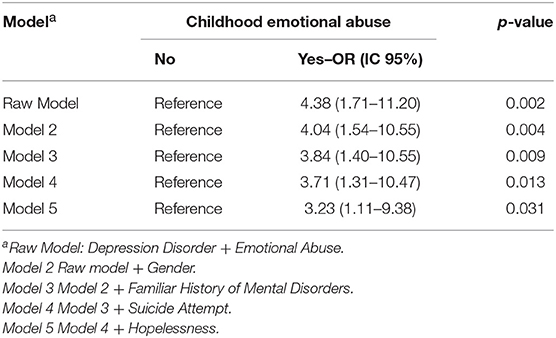
Table 5. Multiple Logistic regression analysis between depression and childhood emotional abuse among patients.
Discussion
Depression is one of the most common mental disorders, with estimates ranging around 16 % of the population at some point in life. The World Health Organization has recognized that it is one of the psychopathologies that lead to greater commitment and mental suffering, thus being considered a public health problem (36). For this reason, it is a necessary an identification of the etiological factors that could help to minimize the incidence of these conditions and also improve the development of more effective therapeutic approaches to minimize the harmful effects of such a psychopathological condition. The scientific literature has been pointing out that the early stressors in childhood, called early stress, are also closely linked to the onset of psychiatric disorders (4, 37). Among the early stress subtypes, emotional abuse has been studied in several studies, showing that the same appears to be associated with the development of depressive disorders in adulthood (10, 11, 38–40). The study conducted by Pinto et al. (41), with a Portuguese sample also demonstrated, from logistic regression and linear analysis that adversity in childhood and adolescence elucidate around 6% of depressive symptoms and increases the risk of suicide attempts around 1,818 times. In our study evidenced a percentage around 70% of depressive patients with emotional abuse and from the results of the regression analysis was found an odds ratio of 4.38 times of occurrence of depression in patients with emotional abuse in childhood, thus demonstrating the importance of this early stress subtype as a trigger to trigger the depressive disorder. Emotional abuse often becomes unnoticeable by the health and education professionals because of its invisibility and discretion; however, it is imperative to its recognition. Moreover, in our research, we found a predominance of depressive patients were female (72.8%) and from the multiple logistic regression analysis was shown that patients with emotional abuse in childhood and females have an odds ratio of occurrence 4.04 times in developing depression, thus corroborating evidence from the scientific literature. According to studies by Kessler et al. (42), Fleck et al. (43) there is a relationship of two depressed women to a man, from adolescence, prevalence this explained by multifactor, with emphasis neuroendocrine and biological agents. Hormonal changes at different stages of development of women, i.e., premenstrual period, pregnancy and perimenopausal period seem to offer explanations for the association between depression and females (44). Research conducted by Weissman and Klerman (45) pioneered this relationship is particularly important for other researchers to extend understanding of the etiology for the higher prevalence of depression in women compared to men. Furthermore, studies show that men tend to have coping strategies to externalized depression, such as alcohol and drug abuse, while women internalize the symptoms, expressing sadness from social isolation, crying, and emotional withdrawal, more symptoms characteristic of depressive symptomatology (46). Other studies show that adolescent girls have problems related to the sense of well-being, the performance of social roles, as well as physical and sexual abuse in childhood, while men are involved with the abuse of alcohol and drugs, being this behavior a trigger also for attempted suicide (47). Another result of high scientific evidence concerning the association between depression and family history of psychiatric disorder. In our survey, 77% of patients had a family history of psychiatric disorders, and from the regression analysis, patients with a history of emotional abuse, female and mental disorder family history have an odds ratio of 3.84 times more on developing depression. This result corroborates the findings in the literature since the risk of depression increases 2 to 3 times in first-degree relatives of individuals with major depression compared to healthy people (48). Levinson (49) emphasizes that an individual who has a first-degree relative with depression have a higher risk of developing the same disorder, therefore the prevalence of depression in children of depressed parents is 5–12% higher than in the general population. Besides the positive family history is indicative of poor prognosis in psychiatric treatment (24, 50).
In the meta-analysis of Sullivan et al. (51) has seen an odds ratio of 2.84 times in patients with a family history of depression, compared to individuals with no family history. Such genetic influence becomes more evident when analyzing the appearance period of the disease and the number of episodes, as family members of individuals with recurrent depression and early onset present 17.4% rate while the relatives of individuals with single episode late-onset depression and have rates of 3.4% (52). It is worth mentioning that genetic predisposition and interaction with the environment is an individual aspect, therefore will depend on the combination of genetics and environment for the person presenting or not depression (53). Consecrated studies and current also show a potential association between depression and suicide, and impulsive behavior and aggression are important clues in this association (54–57). The study of Isometsa et al. (58) showed that while half of the depressed who committed suicide were receiving psychiatric treatment, few were under proper treatment for depression at the time of suicide, deserving emphasis on male patients, which they receive less frequent diagnosis of depression, thereby receiving less treatment and those who were diagnosed adhere less. Kessler et al. (59) evaluated the ratio between major depression and suicidal ideation, planning, trial and suicidal gestures in the years 1990–1992, and this research repeated after a decade; the findings of this study remained similar, demonstrating the temporal stability of the association between depression and suicide. Our study is in accordance with scientific evidence (24), since more than 70% of the sample had a history of suicide attempt; besides from the statistical analysis it was shown that patients with emotional abuse in childhood, female, with a history of mental illness in the family and attempted suicide have an odds ratio of occurrence of 3.71 times to develop depression. Also, the cohort of 3,017 individuals conducted by Brezo et al. (60) found an odds ratio of 6.8 times between childhood sexual abuse and suicide. Another exciting point identified in this study was the association between depression and hopelessness. According to the theory of Aaron Beck, depression result from thoughts and distorted beliefs where there is a negative view of the future, generating great hopelessness about life itself. Also, the hopelessness is closely associated with suicidal ideation, and the incidence of suicide in depressed people is 15%. Leahy (61) points that stress is a primary source of distorted thoughts in depressed activation in this sense the cognitive restructuring process will work to prevent the presence of depressed mood, apathy, fatigue, and other physiological changes present in depression. In our study, it was clear that patients with emotional abuse in childhood, female, with a history of mental disorders and suicide attempts and hopelessness have the odds ratio of 3.23 times in developing depression. It is important to emphasize that our study presents a methodological limitation regarding the research of early stress with psychiatric disorders in adults, so it would be necessary to evaluate the stress of current life, so further research can help to broaden the understanding of past stress and present, favoring the understanding of depressive illness. Depression is a complex disease, and explained by the interaction of genotype including heredity, the lived-in childhood environment, which can be marked for possible traumas, temperament that gives the individual the ability to deal with the environment and the resilience of some individuals who may explain different response to the same stressful events.
Conclusions
Our results suggested that the occurrence of depression in adulthood is related to situations of emotional abuse, sexual and physical neglect during childhood. The relationship between depression and childhood emotional abuse in females with psychiatry family history and previous suicide attempted is significant. Thus, these findings contribute to better understanding the mechanism involved in the pathogenesis of depression related to childhood emotional abuse.
Author Contributions
MJ conceived and designed the study. CM-M, TP, and CB organized the database. MJ, CM-M, ST, and ER performed the statistical analysis and reviewed the literature. CM-M, ST, and CB dealt with psychometric evaluation. MJ, TP, and CM-M wrote the manuscript. MJ critically reviewed and finalized the paper. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This work was supported by Academy of Medical Sciences/Royal Society, UK funding to MJ. It also represents independent research part funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsely NHS Foundation Trust and King's College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Conflict of Interest Statement
MJ is Honorary Consultant at South London and Maudsley NHS Foundation Trust. MJ has within the last year received honoraria for speaking from GSK, Lundbeck and Pfizer.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Juruena MF. Early-life stress and HPA axis trigger recurrent adulthood depression. Epilepsy Behav. (2014) 38:148–59. doi: 10.1016/j.yebeh.2013.10.020
2. Zavaschi MLS, Satler F, Poester D, Vargas CF, Piazenski R, Rohde LAP, et al. Association between childhood loss trauma and depression in adulthood. Rev Bras Psiquiatr. (2002) 24:189–95. doi: 10.1590/S1516-44462002000400009
3. Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse Negl. (2003) 27:169–90. doi: 10.1016/S0145-2134(02)00541-0
4. Collishaw S, Pickles A, Messer J, Rutter M, Shearer C, Maughan B. Resilience to adult psychopathology following childhood maltreatment, evidence from a community sample. Child Abuse Negl. (2007) 31:211–29. doi: 10.1016/j.chiabu.2007.02.004
5. Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents. Am J Psychiatry (2003) 160:1453–60. doi: 10.1176/appi.ajp.160.8.1453
6. Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol Med. (1997) 27:1101–19. doi: 10.1017/S0033291797005588
7. Mullen PE, Martin JL, Anderson JC, Romans SE, Herbison GP. The long-term impact of the physical, emotional, and sexual abuse of children, a community study. Child Abuse Negl. (1996) 20:7–21. doi: 10.1016/0145-2134(95)00112-3
8. Martins CMS, Tofoli SM, Baes CVW, Juruena MF. Analysis of the occurrence of early life stress in adult psychiatric patients, a systematic review. Psychol Neurosci. (2011) 4:219–27. doi: 10.3922/j.psns.2011.2.007
9. Carr CP, Martins CMS, Stingel AM, Lemgruber VB, Juruena MF. The role of early life stress in adult psychiatric disorders. A sistematic review according to childhood trauma subtypes. J Nerv Mental Dis. (2013) 201:1007–20. doi: 10.1097/NMD.0000000000000049
10. Wingenfeld K, Schaffrath C, Rulkoetter N, Mensebach C, Schlosser N, Beblo T, et al. Associations of childhood trauma, trauma in adulthood and previous-year stress with psychopathology in patients with major depression and borderline personality disorder. J Child Abuse Negl. (2011) 35:647–54. doi: 10.1016/j.chiabu.2011.04.003
11. Gibb BE, Chelminski I, Zimmerman M. Childhood emotional, physical, and sexual abuse, and diagnoses of depressive and anxiety disorders in adult psychiatric outpatients. Depression Anxiety (2007) 24:256–63. doi: 10.1002/da.20238
12. Gibb BE, Butler AC, Beck JS. Childhood abuse, depression, and anxiety in adult psychiatric outpatients. Depression Anxiety (2003) 17:226–8. doi: 10.1002/da.10111
13. Berzenski SR, Yates TM. Classes and consequences of multiple maltreatment, a person centered analysis. Child Maltreat. (2011) 16:250–61. doi: 10.1177/1077559511428353
14. Higgins DJ, McCabe MP. Multi-type maltreatment and the long-term adjustment of adults. Child Abuse Rev. (2000) 9:6–18. doi: 10.1002/(SICI)1099-0852(200001/02)9:1<6::AID-CAR579>3.0.CO;2-W
15. Chartier MJ, Walker JR, Naimark B. Separate and cumulative effects of adverse childhood experiences inpredicting adult health and health care utilization. Child Abuse Negl. (2010) 34:454–64. doi: 10.1016/j.chiabu.2009.09.020
16. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V. Relationship of childhood abuse and household dysfunctions to many of the leading causes of death in adults, The adverse childhood study. Am J Prev Med. (1998) 14:245–58. doi: 10.1016/S0749-3797(98)00017-8
17. Hahm HC, Lee Y, Ozonoff A, Van Wert MJ. The impact of multiple types of child adolescence to young adulthood. J Youth Adolesc. (2010) 39:528–40. doi: 10.1007/s10964-009-9490-0
18. Martins CMS, Juruena MF. Trauma-and stressor-related disorders. Medicina (2017) 50(Suppl. 1):37–50. doi: 10.11606/issn.2176-7262.v50isupl1.p37-50
19. Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders, preclinical and clinical studies. Biol Psychiatry (2001) 49:1023–39. doi: 10.1016/S0006-3223(01)01157-X
20. Briere J, Kaltman S, Green BL. Accumulated childhood trauma and symptom complexity. J Traumatic Stress (2008) 21:223–6. doi: 10.1002/jts.20317
21. Ford JD, Wasser T, Connor DF. Identifying and determining the symptom severity associated with polyvictimization among psychiatrically impaired children in the outpatient setting. Child Maltreat. (2011) 16:216–26. doi: 10.1177/1077559511406109
22. Sesar K, Zivcic-Becirevic I, Sesar D. Multi-type maltreatment in childhood and psychological adjustment in adolescence, questionnaire study among adolescents in western Herzegovina Canton. Croat Med J. (2008) 49:243–526. doi: 10.3325/cmj.2008.2.243
23. Arrata CM, Langhinrichsen-Rohling J, Bowers D, O'Brien N. Differential correlates of multitype maltreatment among urban youth. J Child Abuse Negl. (2007) 31:393–415. doi: 10.1016/j.chiabu.2006.09.006
24. Tunnard C, Rane LJ, Wooderson SC, Markopoulou K, Poon L, Fekadu A, et al. The impact of childhood adversity on suicidality and clinical course in treatment-resistant depression. J Affect Disord. (2014) 152:122–30. doi: 10.1016/j.jad.2013.06.037
25. Sfoggia A, Pacheco MA, Grassi-Oliveira R. History of childhood abuse and neglect and suicidal behavior at hospital admission. Crisis (2008) 29:154–8. doi: 10.1027/0227-5910.29.3.154
26. Brown J, Cohen P, Johnson JG, Smailes EM. Childhood abuse and neglect, specificity of effects on adolescent and young adult depression and suicidality. J Am Acad Child Adolesc Psychiatry (1999) 38:1490–6. doi: 10.1097/00004583-199912000-00009
27. Martins CM, Baes C, Tofoli S, Juruena MF. Emotional abuse in childhood is differential factor for the development of depression in adults. J Nerv Mental Dis. (2014) 202:774–82. doi: 10.1097/NMD.0000000000000202
28. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini International Neuropsychiatric Interview (MINI), the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry (1998) 59:22–33.
29. Amorim P. Mini International Neuropsychiatric Interview (MINI), validação de entrevista breve para diagnóstico de transtornos mentais. Rev Bras Psiquiatr. (2000) 22:106–15. doi: 10.1590/S1516-44462000000300003
30. Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism, the hopelessness scale. J Consult Clin Psychol. (1974) 42:861–5. doi: 10.1037/h0037562
32. Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry (1994) 151:1132–6. doi: 10.1176/ajp.151.8.1132
33. Carpenter LL, Carvalho JP, Tyrka AR, Wier LM, Mello AF, Mello MF, et al. Decreased adrenocorticotropic hormone and cortisol responses to stress in healthy adults reporting significant childhood maltreatment. Biol Psychiatry (2007) 62:1080–7. doi: 10.1016/j.biopsych.2007.05.002
34. Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the childhood trauma questionnaire in an adolescent psychiatric population. J Am Acad Child Adolesc Psychiatry (1997) 36:340–8. doi: 10.1097/00004583-199703000-00012
35. Grassi-Oliveira RG, Stein LM, Pezzi JC. Tradução e validação de conteúdo da versão em português do Childhood Trauma Questionnaire. Rev Saúde Públ. (2006) 40:249–55. doi: 10.1590/S0034-89102006000200010
36. WHO. Depression and Other Common Mental Disorders. Global Health Estimates. WHO reference number (2017).
37. McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychopathology in the national comorbidity survey reapplication (NCS-R) III, associations with functional impairment related to DSM-IV disorders. Psychol Med. (2010) 40:847–59. doi: 10.1017/S0033291709991115
38. Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long-term health consequences of child physical abuse, emotional abuse, and neglect, a systematic review and meta-analysis. PLoS Med. (2012) 9:1001349. doi: 10.1371/journal.pmed.1001349
39. Seok J, Lee K, Kim W, Lee S, Kang E, Ham B, et al. Impact of early-life stress and resilience on patients with major depressive disorder. Yonsei Med J. (2012) 53:1093–8. doi: 10.3349/ymj.2012.53.6.1093
40. Shapero BG, Black SK, Liu RT, Klugman J, Bender RE, Abramson LY, et al. Stressful life events and depression symptoms, the effect of childhood emotional abuse on stress reactivity. J Clin Psychol. (2013) 70:1–15. doi: 10.1002/jclp.22011
41. Pinto VCP, Alvez JFC, Maia AC. Adversity in childhood predicts depressive symptoms and suicide attempts in adult Portuguese women. Estudos de Psicologia (2015) 32:617–25. doi: 10.1590/0103-166X2015000400005
42. Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, et al. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med. (2005) 16:2515–23. doi: 10.1056/NEJMsa043266
43. Fleck MP, Berlim MT, Lafer B, Sougey EB, Del Porto JA, Brasil MA, et al. Review of the guidelines of the Brazilian Medical Association for the treatment of depression. Braz J Psychiatry (2009) 31(Suppl. 1):S7–17. doi: 10.1590/S1516-44462009000500003
44. Baptista T, Reyes D, Hernández L. Antipsychotic drugs and reproductive hormones: relationship to body weight regulation. Pharmacol Biochem Behav. (1999) 62:409–17.
45. Weissman MM, Klerman GL. Sex diferences and the epidemiology of depression. Arch Gen Psychiatry (1977) 34:98–111.
46. Windle MA. Longitudinal study of stress buffering for adolescente problem behaviors. Dev Mental Psychol. (1992) 522–530. doi: 10.1037/0012-1649.28.3.522
47. Smith DK, Saldana L. Trauma delinquency and substance use: co-occurring problems for adolescent girls in the juvenile justice system. J Child Adolesc Subst Abuse (2013) 22:450–65. doi: 10.1080/1067828X.2013.788895
48. Klerman GL, Weissman MM. Increasing rates of depression. JAMA (1989) 261:229–35. doi: 10.1001/jama.1989.03420150079041
49. Levinson DF. The genetics of depression: a review. Biological Psychiatry (2006) 60:84–92. doi: 10.1016/j.biopsych.2005.08.024
50. Nierenberg AA, Trivedi MH, Fava M, Biggs MM, Shores-Wilson K, Wisniewski SR, et al. Family history of mood disorder and characteristics of major depressive disorder, a STAR*D (sequenced treatment alternatives to relieve depression) study. J Psychiatr Res. (2007) 41:214–21. doi: 10.1016/j.jpsychires.2006.02.005
51. Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression, review and meta-analysis. Am J Psychiatry (2000) 157:1552–62. doi: 10.1176/appi.ajp.157.10.1552
52. Bland RC, Newman SC, Orn H. Recurrent and non-recurrent depression. A family study. Arch Gener Psychiatry (1986) 43:1085–9. doi: 10.1001/archpsyc.1986.01800110071009
53. Menezes IC, Baes CV, Lacchini R, Juruena MF. Genetic biomarkers for differential diagnosis of major depressive disorder and bipolar disorder, a critical and systematic review. Behav Brain Res. (2018) 57–358:29–38. doi: 10.1016/j.bbr.2018.01.008
54. McGirr A, Renaud J, Seguin M, Alda M, Benkelfat C, Lesage A, et al. An examination of DSM-IV depressive symptoms and risk for suicide completion in major depressive disorder, a psychological autopsy study. J Affect Disord. (2007) 97:203–9. doi: 10.1016/j.jad.2006.06.016
55. Dumais A, Lesage AD, Alda M, Rouleau G, Dumont M, Chawky N, et al. Risk factors for suicide completion in major depression, a case-control study of impulsive and aggressive behaviors in men. Am J Psychiatry (2005) 162:2116–24. doi: 10.1176/appi.ajp.162.11.2116
56. Brent DA, Oquendo M, Birmaher B, Greenhill L, Kolko D, Stanley B, et al. Familial transmission of mood disorders, convergence and divergence with transmission of suicidal behavior. J Am Acad Child Adolesc Psychiatry (2004) 43:1259–66. doi: 10.1097/01.chi.0000135619.38392.78
57. Turecki G. Dissecting the suicide phenotype: the role of impulsive-aggressive behaviours. J Psychiatry Neurosci. (2005) 30:398–408.
58. Isometsa ET, Henriksson MM, Aro HM, Heikkinen ME, Kuoppasalmi KI, Lonnqvist JK. Suicide in major depression. Am J Psychiatry (1994) 151:530–6. doi: 10.1176/ajp.151.4.530
59. Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures and attempts in the United States, 1990-1992 to 2001-2003. JAMA (2005) 293:2487–95. doi: 10.1001/jama.293.20.2487
60. Brezo J, Paris J, Barker ED, Tremblay R, Vitaro F, Zoccolillo M, et al. Natural history of suicidal behaviors in a population-based sample of young adults. Psychol Med. (2007) 37:1563–74. doi: 10.1017/S003329170700058X
Keywords: early life stress, subtypes of early life stress, depressive disorder, emotional abuse, neglect, childhood trauma
Citation: Martins-Monteverde CMS, Baes CVW, Reisdorfer E, Padovan T, Tofoli SMdC and Juruena MF (2019) Relationship Between Depression and Subtypes of Early Life Stress in Adult Psychiatric Patients. Front. Psychiatry 10:19. doi: 10.3389/fpsyt.2019.00019
Received: 04 September 2018; Accepted: 11 January 2019;
Published: 05 February 2019.
Edited by:
Diogo Telles-Correia, Universidade de Lisboa, PortugalReviewed by:
Liang Gong, Southeast University, ChinaAlexandre Paim Diaz, Federal University of Santa Catarina, Brazil
Copyright © 2019 Martins-Monteverde, Baes, Reisdorfer, Padovan, Tofoli and Juruena. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mario Francisco Juruena, bWFyaW8uanVydWVuYUBrY2wuYWMudWs=
 Camila Maria Severi Martins-Monteverde
Camila Maria Severi Martins-Monteverde Cristiane Von Werne Baes
Cristiane Von Werne Baes Emilene Reisdorfer2
Emilene Reisdorfer2 Mario Francisco Juruena
Mario Francisco Juruena