
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 25 October 2018
Sec. Forensic Psychiatry
Volume 9 - 2018 | https://doi.org/10.3389/fpsyt.2018.00534
This article is part of the Research Topic Caring for Those Who are Neglected and Forgotten: Psychiatry in Prison Environments View all 20 articles
 Sebastian Schildbach*
Sebastian Schildbach* Carola Schildbach
Carola SchildbachIn 1939, the Penrose hypothesis suggested that the number of psychiatric hospital beds was inversely related to the size of prison populations. Central to a causal interpretation of the Penrose hypothesis is the idea that a small proportion of any population requires institutional mental care. Several studies re-examining longitudinal and cross-sectional data found that a fall in available psychiatric hospital beds occurred over the same period as a rise in prisoner numbers. The observed inverse relationship was mostly interpreted as being the consequence of a lack of compassion for the disadvantaged in society, while other studies concluded that the correlation was spurious and determined by confounders. In Germany, Austria, and Switzerland, lawbreakers who are unwilling or unable to pay a fine for committing a petty crime such can face compensation imprisonment. Every tenth German detainee serves compensation imprisonment with an average incarceration time of 2–3 months. We analyzed the social-economic backgrounds and the levels of mental disorders in four populations of compensation prisoners, consisting of 100 participants each, in the German capital Berlin in 1999, 2004, 2010, and 2017. Largely, the compensation prisoners were homeless, single, and unemployed, exhibited a high degree of substance abuse and showed an extraordinary high prevalence of mental disorders. Unfortunately, as the average stay in prison is short, there are no decisive concepts for social rehabilitation after imprisonment. In addition to a lack of resocialization, potential job loss, and social stigmatization, the newly acquired subcultural contacts facilitate reoffending. This study aims to give an overview of the medical, sociologic, and psychopathologic examinations on compensation prisoners. By analyzing trends in the prevalence of mental disorders, we will discuss the medical appropriateness and sociologic sense of compensation imprisonment with respect to the Penrose hypothesis. Thereby, we aim at shedding light on the question whether compensation imprisonment is an indispensable tool for law enforcement or if it is a punishment of the poor or mentally ill, which further deteriorates their unfavorable socio-economic situation. Finally, we will propose measures to reduce the number of reoffenders and to enable the compensation detainees to reintegrate successfully into society.
In 1939, the English scientist Lionel Penrose found an inverse correlation between the size of psychiatric inpatient clinics and the number of detainees based on cross-sectional data from diverse European countries (1). His assumption that the number of psychiatric hospital beds was inversely related to the size of prison populations was later termed the “Penrose hypothesis.” A common expression summarizing Penrose's findings is “transinstitutionalization,” which refers to a process where mentally ill individuals, who are discharged from, or no longer admitted to, mental hospitals, are frequently found in prisons (2–4).
Even 80 years after its formulation, the Penrose hypothesis has neither been rejected nor confirmed. Despite repeated observations of transinstitutionalization, and an increase of the numbers of imprisoners, it is still unclear whether there is an association between capacities in psychiatric clinics and prison sizes (5).
In 2004, a meta-analysis on data from 158 countries found the opposite relationship compared to Penrose, namely that in low-and-middle-income countries, prison, and psychiatric populations were positively correlated (6). However, similar to the preceding study by Penrose, this meta-analysis used cross-sectional data.
Longitudinal data on treatment histories of U.S. prisoners revealed that the decrease in the number of psychiatric hospital beds accounted only for a small proportion of the expanding prison populations between 1968 and 1978 (7). Longitudinal data from Europe indicated that psychiatric care might have reached a phase of transinstitutionalization (8, 9), in which the numbers of mental health care beds might further decline, and that at the same time, capacities in prisons might extend (10). Still, none of these studies provided undisputable evidence for a direct correlation between decreasing capacities of mental health care institutions beds and increasing prison populations (11, 12). Another study suggested that both the numbers of mental health care beds and the numbers of detainees might be influenced by economic factors (13). However, none of the published studies have thus far sufficiently disproved Penrose's direct inverse association theory (14).
A recent longitudinal study found that since 1990, capacities of mental health care institutions were considerably cut down in South America, while prison populations boosted despite a strong economic growth (15). The observed developments appear to support the Penrose hypothesis, because the numbers of psychiatric beds decreased more substantially when and where the number of imprisoners increased (15). Comparable conclusions of a decline of mental health care beds and a simultaneous rise in numbers of detainees were documented in Ireland and Norway (16, 17).
In Germany, Austria, and Switzerland, the penalty system includes a certain type of punishment termed “compensation imprisonment.” If a convicted person refuses to pay the fine for a crime, he or she must go to jail instead for a short period. This compensation imprisonment is regulated under section 43 of the German Penal Code and is conceived to ensure the effectiveness of the penalty system (18, 19). The proportion of compensation prisoners amounts for ~10% of all inmates in Germany (20). For nearly two decades, the meaningfulness of compensation imprisonment has been discussed (21–23). Because of the fact that the mean period of imprisonment is short, there are no meaningful approaches for social rehabilitation after imprisonment. As a consequence of this lack of resocialization, the detainees have to face potential job loss and social stigmatization, and the newly achieved contacts with other criminals facilitate reoffending (24).
In our previous longitudinal study from 1999 to 2017 on the prevalence of mental diseases in compensation prisoners, we found that 72.75% of these special clientele suffered from alcohol-induced mental and behavioral disorders, 45.5% suffered from mental and behavioral disorders due to use of illegal drugs, 35% exhibited phobic anxiety disorders, and 26.25% showed signs of depressive disorders (25). In addition, somatoform disorders and dysthymia were found at frequencies between 10 and 20% (25).
Therefore, our hypothesis is that compensation imprisonment is a punishment of the poor and mentally ill. With respect to the Penrose hypothesis, we suggest that the proposed process of transinstitutionalization can most likely be observed in compensation prisoners, as these detainees would most likely benefit from a mental health care treatment, while they are put into prison instead. Thereby, compensation imprisonment increases inequality and poverty among people at the edge of society.
The process of data acquisition and diagnosis of mental disorders was described before (25). In total, four study populations of randomly selected compensation prisoners were collected in the years 1999 (26), 2004 (27), 2010 and 2017 (25). As all study participants were diagnosed with the same diagnostic system DIA-X, the data were pooled for inferring the prevalence of diverse mental disorders in compensation prisoners.
For diagnosing psychiatric disorders, the long form of the computer-aided expert system DIA-X was used (28). DIA-X supports the user reliably and efficiently with the diagnosis of about 100 mental disorders according to ICD-10 (International Classification of Diseases) and DSM-IV (Diagnostic and Statistical Manual of Mental Disorders) (29). The long version of DIA-X is a standardized interview for measuring mental disorders in the last 12 months. The modular structure and the possibilities of branching ensure that despite the standardization only the symptom constellation important for the respective subject is placed in the center of the interview. DIA-X was applied as computer version. For the DIA-X standardized interview, the interrater agreement was reported to range between 97 and 100% for the most common mental disorders, and the interrater kappa was reported to range between 0.67 (somatization disorder) and 0.99 (agoraphobia) (28).
Additionally, selected social and demographic characteristics basic data were collected. Each session lasted between 90 and 120 min, on average 105 min (25).
In order to compare compensation prisoners with general prisoners and with the general population in terms of the prevalence of the diverse mental disorders, a literature search was performed to assess the prevalence rates of the mental illnesses. For mental diseases in general prisoners, the following articles were consulted: (30–34).
The prevalence of mental diseases in the general population were extracted from Angst (35), Martin (36), Bloomfield et al. (37), Hilderink et al. (38), Patra and Sarkar (39), Qian et al. (40), Grant et al. (41), Chang et al. (42), Vandeleur et al. (43), and Leutgeb et al. (44).
In order to assess the percentage of compensation prisoners in all detainees and to be able to determine a temporal trend, we used data from the German Federal Statistical Office. The Federal Statistical Office publishes at regular intervals the stock of prisoners in the German prisons with respect to their regional placement and with respect to the form of imprisonment on the deadlines March 31, August 31, and November 30 of each year. For this study, the total number of inmates and the number of compensation prisoners were taken from the collections on November 30 each year starting from 2009 to 2017 (45, 46).
A simple linear regression analysis was used for modeling the relationship between the percentage of compensation prisoners on all prisoners (dependent variable) and the time in years since 2009 (independent variable).
Table 1 gives an overview of the prevalence of various mental illnesses among prisoners and the general population. Furthermore, a distinction was made between detainees in general and compensation prisoners.
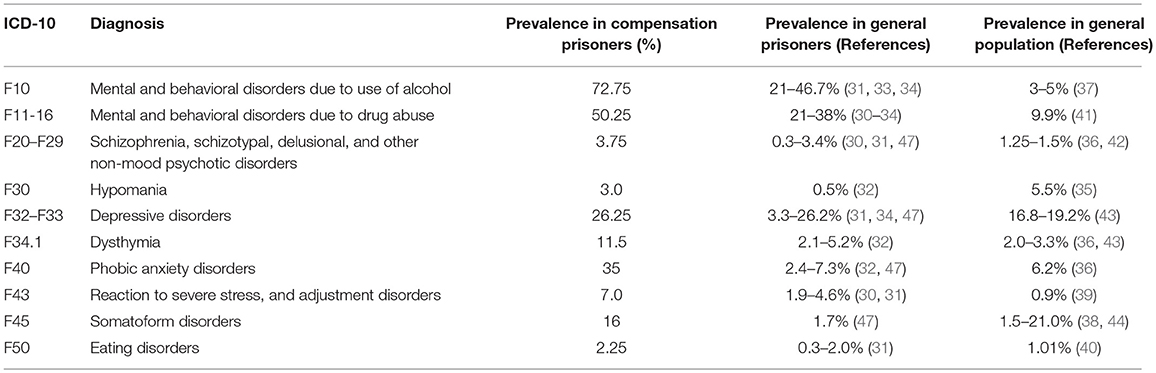
Table 1. Overview of the average prevalence of mental disorders compensation prisoners, general prisoners and in the general population.
The first striking feature of this statistic is that the prevalence of mental illness due to the use of alcohol among compensation prisoners was 72.75%, while prisoners in general exhibited prevalence rates of 21–47%. In the normal population, the prevalence of alcohol-related mental illnesses was only around 3–5%. Compensation prisoners were therefore three times as likely to suffer from alcohol-related mental illness as average prisoners were and 10–20 times as likely to be troubled by alcohol-related mental illness as the average population.
Mental illness caused by substance abuse was found to have a prevalence of 50.25% among compensation prisoners, while its prevalence varied between 21 and 38% among general inmates and lay at only 10% in the general population.
In hypomania and depressive disorders, there were no deviations in the prevalence in compensation prisoners. Dysthymia affected 11.5% of compensation prisoners but only 2.1–5.2% of average prisoners and 2.0–3.3% of the norm population. With regard to dysthymia, the prevalence of compensation prisoners was thus threefold higher than that of the average population.
Phobic anxiety disorders were detected in 35% of compensation prisoners, but the prevalence in the normal population was only 6.2%. The difference in adjustment disorders was particularly pronounced: with a prevalence of 7% for compensation prisoners and 1.9–4.6% for general detainees and only 0.9% for the norm population, the presence of adjustment disorders among compensation inmates exceeded the norm many times over.
Another eye-catching finding was that 16% of compensation inmates were diagnosed with somatoform disorders, while only 1.7% of other inmates and only 1.5–21.0% of the general population suffered from somatoform disorders.
On average, about 1% of the population suffers from eating disorders, with women being significantly more affected than men are. In prisons, on average, 0.3% of men and 2.0% of women suffered from eating disorders. Therefore, it was conspicuous that our study population of compensation prisoners, which consisted exclusively of men, had an eating disorder rate of 2.25%.
Table 2 presents the development of the numbers of all detainees and of compensation detainees in Germany from 2009 to 2017. The number of inmates in Germany has declined considerably in recent years. From the beginning of available records in 2003 until 2009, the number of inmates exceeded 70,000 every yearly cut-off date (45). The number of inmates was below 70,000 for the first time in 2010 (45), and since then the numbers have been decreasing constantly (46). On the other hand, the numbers of compensation prisoners remained constant or increased steadily since 2009, both in absolute terms and in percentage terms.
To sum up, the number of compensation prisoners in Germany, who were in jail by the end of November in each year, increased nationwide from 3,868 detainees in 2009 to 4,580 detainees in 2017, with a simultaneous decrease in the total number of prisoners. While 5.5% of all inmates were compensation prisoners in 2009, in 2017 the amount of compensation prisoners increased to 7.1% of all prisoners. More concretely, this finding in relative terms meant that the total number of detainees decreased by 9.1% from 2009 to 2017, while the number of compensation prisoners increased by 18.4% between 2009 and 2017.
A simple linear regression analysis with the time in years as independent factor and the percentage of compensation prisoners on all prisoners as dependent variable explained a large amount of variance in the data (R2 = 0.871). Every year, the proportion of compensation prisoners on all prisoners increased by 0.253%, and the association was highly significant (p < 0.001).
Convicts who cannot pay the fine for committing a petty crime like fare evasion have to serve compensation imprisonment. The risk of compensation imprisonment is therefore many times greater for poor people than for financially well-off people.
The comparison of the prevalence of mental disease in compensation prisoners with population samples from general prisons and from the general population yielded a clear result: compensation prisoners are many more times more prone to suffer from mental diseases induced by alcohol and drug abuse than the normal population. Even in comparison with population samples from worldwide prisons, the prevalence of alcohol-and drug-abuse related disorders was extraordinarily high. Our finding that 72.75% of compensation prisoners suffered from mental and behavioral disorders due to use of alcohol is in line with the findings of Konrad and Opitz-Welke, who reported that 77% of their study population consisting of compensation and investigation prisoners were diagnosed with alcohol abuse (48)
In addition, dysthymia, phobic anxiety disorders, adjustment disorders, somatoform disorders, and eating disorders occurred at frequencies wide above the standard levels. The exceptionally high prevalence of adjustment disorders could reflect immediate negative reactions to incarceration (49).
One explanation for this observation could be an interaction between being poor and being mentally ill. Indeed, several studies could demonstrate that people who live in poverty appear to be at higher risk for mental illnesses (50–52). However, the association between poverty and mental disorders is complex and bidirectional. On the one hand, besides genetics, adverse life events or substance abuse, poverty can be a main factor causing mental illness. On the other hand, mental illness may lead people down a road to poverty, because of disability, stigma or the need to spend extra money on health care (50, 51). Lund and colleagues suggest that poverty more often leads to depression while disorders like schizophrenia more often lead to poverty (50, 51).
Therefore, the conversion of the monetary fine for committing a petty crime into imprisonment primarily affects the socially marginalized, the poor, and the mentally ill. Consequently, compensation imprisonment may constitute the backbone of the sanction system, but it seems dysfunctional to our subjects.
The longitudinal analysis of prisoner numbers in Germany yielded a clear trend: while the number of people in jail is constantly decreasing, the number of compensation prisoners is constantly increasing. As social-demographic study on compensation prisoners demonstrated that these people were mainly homeless, unemployed, and had hardly any sustaining family background (25). The finding that compensation prisoners suffered from a wide spectrum of mental disorders, which exceeded the standard population by a magnitude, underscored the hypothesis that these people are in fact victims of a transinstitutionalization process.
If prisons in fact could be a substitute for mental health care clinics, then the question arises to what these facilities could offer to the many inmates with serious mental disorders. One modality that jails offer is structure, which is implemented in the form of a protected setting and of employees who can hold back improper and destructive behavior, and conceive a personalized psychiatric treatment regime. However, for those people with serious mental disorders and who serve compensation imprisonment, this structured setting is not sufficient, as their stay in prison is generally very short and standard treatment plans are not being carried out for reasons of time. For this clientele, psychiatric inpatient treatment and drug and alcohol withdrawal would be preferable to incarceration into a prison.
It is broadly accepted that numerous people with genuine psychological problems, who have been criminalized, could be dealt with effectively in the community, if there were sufficient and available treatment facilities (53). However, in Eastern Germany, after the political change, the number of general psychiatric beds fell by 61% and the prisoners' rate dropped by 77%, so that within a few years the rates between East and West Germany converged. In both parts of Germany, capacities were built up in the execution of sentences, assisted living and rehabilitation facilities. In West Germany, the number of psychiatric beds fell by 40% between 1989 and 2003 (54). However, at the same time, forensic psychiatric bed numbers increased in most countries, especially in East Germany (12). Consistent with the Penrose hypothesis, it seemed that the extensive decline in general mental health care beds might have partly been compensated by a rise in forensic mental health care beds. Although the reduction of general psychiatric beds may not have caused a growth of prison populations, available data do not allow excluding a possible transinstitutionalization of people with mental disorders from psychiatric hospitals to prisons (12).
Lamentably, the deficient treatment of mentally challenged people during compensation imprisonment and the inadequate number of clinic beds (acute, intermediate, and long term) for the individuals who require them are some of the realities of transinstitutionalization that have set the stage for criminalization (55).
The Penrose hypothesis has been a valuable reference point for investigations into the intricate relationship between the mental health care system and the legal enforcement system for more nearly 80 years (53). Our results do not prove that validity of the Penrose hypothesis, but in the special setting of compensation imprisonment, our observations support the idea of a transinstitutionalization process. This transinstitutionalization process could possibly lead to an unintentional stigmatization of socially marginalized, poor and mentally ill persons as criminals (56, 57).
However, it is important to emphasize that within the context of this study, the Penrose hypothesis was used as an analogy and that our results were purely descriptive. Therefore, our implications and conclusions are of speculative nature and cannot be confirmed by the descriptive data.
One limitation of the study is that was not possible to diagnose personality orders with the diagnostic system DIA-X. However, antisocial, borderline, and paranoid personality disorders were associated strongly with substance-use disorders (58–60). Therefore, determining the prevalence of personality disorders would provide interesting insights into the mental health of this particular study population, which has an extremely high rate of substance abuse. The diagnosis of personality disorders could be a relevant factor especially for compensation prisoners minimize recidivism among those in legally supervised treatment (61).
Another limitation of using the diagnostic system DIA-X is constituted by a potential underestimation of more chronic forms of schizophrenia that are dominated by negative symptoms in compensation prisoners.
Finally, we cannot validate whether the reduction of mental health care beds in Germany concerned mostly chronic diseases like schizophrenia or mental disabilities, as there are no statistical reports on this issue. However, this information would be a prerequisite in order to prove that substance abusers were especially affected by the reduction of psychiatric hospital beds.
The German law already offers an alternative to compensation imprisonment, which is community service. People sentenced to serve compensation imprisonment can apply for serving voluntary community work instead (19). This seems very meaningful, as imprisonment would further deteriorate their precarious financial and social situation and would further impair their fragile state of mental health. If these people are put to jail and released again without support, they will find themselves in a vicious circle without the hope of ever escaping their compromising situation.
Given that a large proportion of the compensation prisoners suffered from mental illness, we believe that it is advisable to first psychologically diagnose anyone convicted of compensation imprisonment. This could be achieved with the DIA-X diagnostic system, for example. Then a therapy should take place accompanying the voluntary work, which should deal with the respective problems of the individual. For serious mental illness, a transfer to a psychiatric hospital would be worth considering. In any case, nothing should be left unturned to integrate the convict into a functioning social environment.
Our studies add weight to claims that compensation imprisonment leads to an ethically questionable and clinically inappropriate transinstitutionalization and further criminalization of poor or mentally ill people from the edge of society into prisons, which are poorly set up to treat and support them. Policymakers should therefore consider the current limits of compensation imprisonment.
In January 2016, a comprehensive research proposal was submitted to the criminal services of the penal institutions in Berlin and to the social services of the penal institution Plötzensee, which were both approved in February 2016. In addition, the prison management of the penal institution Plötzensee approved the study in April 2016. Finally, the Berlin Commissioner for Data Protection issued a clearance certificate in May 2016.
CS conducted the literature search, collected and evaluated the data, performed the statistical analyses, and supported SS with writing the article wrote the article. SS conceived and prepared the study, wrote the research proposal, communicated with the authorities, recruited the patients, organized the data collection, and wrote the article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Penrose LS. Mental disease and crime: outline of a comparative study of European statistics. Br J Med Psychol. (1939) 18:1–15. doi: 10.1111/j.2044-8341.1939.tb00704.x
2. Palermo GB. Transinstitutionalization and an overburdened judicial system. Med Law (1998) 17:77–82.
3. Slovenko R. The transinstitutionalization of the mentally ill. Ohio North Univ Law Rev. (2003) 29:641–60.
4. Prins SJ. Does transinstitutionalization explain the overrepresentation of people with serious mental illnesses in the criminal justice system? Commun Ment Health J. (2011) 47:716–22. doi: 10.1007/s10597-011-9420-y
5. Tsai AC, Venkataramani AS. A more robust test of the penrose hypothesis. JAMA Psychiatry (2015) 72:735–6. doi: 10.1001/jamapsychiatry.2015.0212
6. Large MM, Nielssen O. The Penrose hypothesis in 2004: patient and prisoner numbers are positively correlated in low-and-middle income countries but are unrelated in high-income countries. Psychol Psychother. (2009) 82:113–9. doi: 10.1348/147608308X320099
7. Severson ME. The impact of a state hospital closure on local jails: the Kansas experience. Commun Ment Health J. (2000) 36:571–87. doi: 10.1023/A:1001982118380
8. Priebe S, Turner T. Reinstitutionalisation in mental health care. BMJ (2003) 326:175. doi: 10.1136/bmj.326.7382.175
9. Topor A, Andersson G, Bulow P, Stefansson CG, Denhov A. After the Asylum? N Instit Landsc Commun Ment Health J. (2016) 52:731–7. doi: 10.1007/s10597-015-9928-7
10. Priebe S, Badesconyi A, Fioritti A, Hansson L, Kilian R, Torres-Gonzales F, et al. Reinstitutionalisation in mental health care: comparison of data on service provision from six European countries. BMJ (2005) 330:123–6. doi: 10.1136/bmj.38296.611215.AE
11. Priebe S, Frottier P, Gaddini A, Kilian R, Lauber C, Martinez-Leal R, et al. Mental health care institutions in nine European countries, 2002 to 2006. Psychiatr Serv. (2008) 59:570–3. doi: 10.1176/ps.2008.59.5.570
12. Mundt AP, Franciskovic T, Gurovich I, Heinz A, Ignatyev Y, Ismayilov F, et al. Changes in the provision of institutionalized mental health care in post-communist countries. PLoS ONE (2012) 7:e38490. doi: 10.1371/journal.pone.0038490
13. Ceccherini-Nelli A, Priebe S. Economic factors and psychiatric hospital beds – an analysis of historical trends. Int J Soc Econ. (2007) 34:788–810. doi: 10.1108/03068290710826396
14. Toynbee M. The Penrose hypothesis in the 21st century: revisiting the asylum. Evid Based Ment Health (2015) 18:76. doi: 10.1136/eb-2015-102115
15. Mundt AP, Chow WS, Arduino M, Barrionuevo H, Fritsch R, Girala N, et al. Psychiatric hospital beds and prison populations in South America since 1990: does the Penrose hypothesis apply? JAMA Psychiatry (2015) 72:112–8. doi: 10.1001/jamapsychiatry.2014.2433
16. Kelly BD. Penrose's Law in Ireland: an ecological analysis of psychiatric inpatients and prisoners. Ir Med J. (2007) 100:373–4.
17. Hartvig P, Kjelsberg E. Penrose's law revisited: the relationship between mental institution beds, prison population and crime rate. Nord J Psychiatry (2009) 63:51–6. doi: 10.1080/08039480802298697
18. Strafgesetzbuch GB St. § 43 Ersatzfreiheitsstrafe. (1997) Available online at: https://www.gesetze-im-internet.de/stgb/43.html (Accessed October 2, 2017).
19. Albrecht H-J. Commentary on §§40-43 [Kommentar zu §§40-43]. In: Kindhäuser, U, Neumann, U, Paeffgen H-U. editors. NOMOS Commentary: Criminal Code [NOMOS Kommentar: Strafgesetzbuch]. Baden-Baden: Nomos Verlagsgesellschaft (2013). p. 1723–56.
20. Villmow B. Short imprisonment, compensation imprisonment and charitable work [Kurze Freiheitsstrafe, Ersatzfreiheitsstrafe und gemeinnützige Arbeit]. In: Albrecht H-J. editor. International Perspectives in Criminology and Criminal Law. Commemorative publication for Günther Kaiser's 70th birthday [Internationale Perspektiven in Kriminologie und Strafrecht. Festschrift für Günther Kaiser zum 70. Geburtstag]. Berlin: Duncker & Humbold Verlag (1999). p. 1708.
21. Dünkel F. The German Prison System in the International Comparison [Der Deutsche Strafvollzug im Internationalen Vergleich] (2003). Available online at: http://www.thomasfeltes.de/beijing/Strafvollzug%20BRD.pdf (Accessed October 3, 2017).
22. Matt E. Detention and no alternative? On the situation of compensation prisoners on the example of Bremen [Haft und keine Alternative? Zur Situation von Ersatzfreiheitsstrafen-Verbüßern am Beispiel von Bremen]. Monatssch Kriminol. (2005) 88:339–50.
23. Bögelein N, Ernst A, Neubacher F. How can the avoidance of substitutional penalties succeed? On the life situation of the convicted and the cooperation of state and non-governmental organizations. [Wie kann die Vermeidung von Ersatzfreiheitsstrafen gelingen? Zur Lebenssituation der Verurteilten und zur Zusammenarbeit staatlicher und nichtstaatlicher Organisationen.]. Bewährungshilfe (2014) 61:282–94.
24. Dolde G. Enforcement of compensation imprisonment - a significant proportion in short-term execution [Vollzug von Ersatzfreiheitsstrafen - ein wesentlicher Anteil im Kurzstrafenvollzug]. Zeitschrift für Strafvollzug und Straffälligenhilfe (1999) 48:330–5.
25. Schildbach S, Schildbach C. Prevalence of psychiatric disorders in detainees serving imprisonment as an alternative punishment for failure to pay penalty fees: a longitudinal study. Int J Law Psychiatry (2018) 58:105–9. doi: 10.1016/j.ijlp.2018.03.006
26. Dubielczyk R. Prevalence of Mental Disorders in Compensation Prisoners [Prävalenz psychischer Störungen bei Ersatzfreiheitsstrafern]. Dissertation. Freie Universität Berlin, Berlin (2002).
27. Müller-Foti G, Robertz FJ, Schildbach S, Wickenhäuser R. Punishing the disoriented? Medical and criminological implications of incarcerating patients with mental disorders for failing to pay a fine. Int J Prisoner Health (2007) 3:87–97. doi: 10.1080/17449200701321365
28. Wittchen HU, Perkonigg A. DIA-X: Diagnostic Expert System for Mental Disorders [DIA-X: Diagnostisches Expertensystem für PSYCHISCHE STÖRUNGEN] Göttingen: Hogrefe Verlag (1997).
29. Hasin D, Hatzenbuehler ML, Keyes K, Ogburn E. Substance use disorders: diagnostic and statistical manual of mental disorders, fourth edition (DSM-IV) and international classification of diseases, tenth edition (ICD-10). Addiction (2006) 101(Suppl. 1):59–75. doi: 10.1111/j.1360-0443.2006.01584.x
30. Gunn J, Maden A, Swinton M. Treatment needs of prisoners with psychiatric disorders. BMJ (1991) 303:338–41.
31. Watzke S, Ullrich S, Marneros A. Gender- and violence-related prevalence of mental disorders in prisoners. Eur Arch Psychiatry Clin Neurosci. (2006) 256:414–21. doi: 10.1007/s00406-006-0656-4
32. Andreoli SB, Dos Santos MM, Quintana MI, Ribeiro WS, Blay SL, Taborda JG, et al. Prevalence of mental disorders among prisoners in the state of Sao Paulo, Brazil. PLoS ONE (2014) 9:e88836. doi: 10.1371/journal.pone.0088836
33. Fazel S, Yoon IA, Hayes AJ. Substance use disorders in prisoners: an updated systematic review and meta-regression analysis in recently incarcerated men and women. Addiction (2017) 112:1725–39. doi: 10.1111/add.13877
34. Yi Y, Turney K, Wildeman C. Mental health among jail and prison inmates. Am J Mens Health (2017) 11:900–9. doi: 10.1177/1557988316681339
35. Angst J. The emerging epidemiology of hypomania and bipolar II disorder. J Affect Disord. (1998) 50:143–51. doi: 10.1016/S0165-0327(98)00142-6
36. Martin P. The epidemiology of anxiety disorders: a review. Dialog Clin Neurosci. (2003) 5:281–98.
37. Bloomfield K, Kraus L, Soyka M. Alcohol consumption and alcohol-related disorders [Alkoholkonsum und alkoholbezogene Störungen]. Gesundheitsberichterstattung des Bundes (2008) 40:3–30. doi: 10.1024/2008.07.05
38. Hilderink PH, Collard R, Rosmalen JG, Oude Voshaar RC. Prevalence of somatoform disorders and medically unexplained symptoms in old age populations in comparison with younger age groups: a systematic review. Ageing Res Rev. (2013) 12:151–6. doi: 10.1016/j.arr.2012.04.004
39. Patra BN, Sarkar S. Adjustment disorder: current diagnostic status. Indian J Psychol Med. (2013) 35:4–9. doi: 10.4103/0253-7176.112193
40. Qian J, Hu Q, Wan Y, Li T, Wu M, Ren Z, et al. Prevalence of eating disorders in the general population: a systematic review. Shanghai Arch Psychiatry (2013) 25:212–23. doi: 10.3969/j.issn.1002-0829.2013.04.003
41. Grant BF, Saha TD, Ruan WJ, Goldstein RB, Chou SP, Jung J, et al. Epidemiology of DSM-5 drug use disorder: results from the national epidemiologic survey on alcohol and related conditions-III. JAMA Psychiatry (2016) 73:39–47. doi: 10.1001/jamapsychiatry.2015.2132
42. Chang WC, Wong CSM, Chen EYH, Lam LCW, Chan WC, Ng RMK, et al. Lifetime prevalence and correlates of schizophrenia-spectrum, affective, and other non-affective psychotic disorders in the chinese adult population. Schizophr Bull. (2017) 43:1280–90. doi: 10.1093/schbul/sbx056
43. Vandeleur CL, Fassassi S, Castelao E, Glaus J, Strippoli MF, Lasserre AM, et al. Prevalence and correlates of DSM-5 major depressive and related disorders in the community. Psychiatry Res. (2017) 250:50–8. doi: 10.1016/j.psychres.2017.01.060
44. Leutgeb R, Berger S, Szecsenyi J, Laux G. Patients with somatoform disorders: more frequent attendance and higher utilization in primary Out-of-Hours care? PLoS ONE (2018) 13:e0202546. doi: 10.1371/journal.pone.0202546
45. Statistisches Bundesamt SB. Number of Prisoners in German Prisons from 2003 - 2013 [Bestand der Gefangenen und Verwahrten in den Deutschen Justizvollzugsanstalten nach Ihrer Unterbringung auf Haftplätzen des Geschlossenen und Offenen Vollzugs jeweils zu den Stichtagen 31. März, 31. August und 30. November eines Jahres. Stichtag 31. März 2003 bis 30. November 2013]. (2014) Available online at: https://www.destatis.de/DE/Publikationen/Thematisch/Rechtspflege/StrafverfolgungVollzug/BestandGefangeneVerwahrte5243201139004.pdf?__blob=publicationFile (Accessed July 3, 2018).
46. Statistisches Bundesamt SB. Number of prisoners in German prisons from 2014 - 2017 [Bestand der Gefangenen und Verwahrten in den deutschen Justizvollzugsanstalten nach ihrer Unterbringung auf Haftplätzen des geschlossenen und offenen Vollzugs jeweils zu den Stichtagen 31. März, 31. August und 30. November eines Jahres. Stichtag 30. November 2017] (2018). Available online at: https://www.destatis.de/DE/Publikationen/Thematisch/Rechtspflege/StrafverfolgungVollzug/BestandGefangeneVerwahrtePDF_5243201.pdf?__blob=publicationFile (Accessed July 3, 2018).
47. Kumar V, Daria U. Psychiatric morbidity in prisoners. Indian J Psychiatry (2013) 55:366–70. doi: 10.4103/0019-5545.120562
48. Konrad N, Opitz-Welke A. Psychiatric problems in prison [Psychiatrische Probleme im Justizvollzug]. In: Dreßing H, Habermeyer E, editors. Psychiatric Assessment (Sixth Edition) [Psychiatrische Begutachtung (Sechste Ausgabe)]. München: Elsevier (2015). p. 351–62.
49. Kocalevent RD, Mierke A, Danzer G, Klapp BF. Adjustment disorders as a stress-related disorder: a longitudinal study of the associations among stress, resources, and mental health. PLoS ONE (2014) 9:e97303. doi: 10.1371/journal.pone.0097303
50. Lund C, Breen A, Flisher AJ, Kakuma R, Corrigall J, Joska JA, et al. Poverty and common mental disorders in low and middle income countries: a systematic review. Soc Sci Med. (2010) 71:517–28. doi: 10.1016/j.socscimed.2010.04.027
51. Lund C, De Silva M, Plagerson S, Cooper S, Chisholm D, Das J, et al. Poverty and mental disorders: breaking the cycle in low-income and middle-income countries. Lancet (2011) 378:1502–14. doi: 10.1016/S0140-6736(11)60754-X
52. Lepiece B, Reynaert C, Jacques D, Zdanowicz N. Poverty and mental health: what should we know as mental health professionals? Psychiatr Danub. (2015) 27(Suppl. 1):S92–6.
53. Lamb HR. Does deinstitutionalization cause criminalization? The penrose hypothesis. JAMA Psychiatry (2015) 72:105–6. doi: 10.1001/jamapsychiatry.2014.2444
54. Mir J, Priebe S, Mundt AP. Mentally ill people in East and West Germany: indicators of institutionalization since the political change [Psychisch Kranke in Ost- und Westdeutschland: Indikatoren der Institutionalisierung seit der politischen Wende]. Der Nervenarzt (2013) 84:844–50. doi: 10.1007/s00115-012-3657-8
55. Lamb HR, Bachrach LL. Some perspectives on deinstitutionalization. Psychiatr Serv. (2001) 52:1039–45. doi: 10.1176/appi.ps.52.8.1039
56. Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatisation of people with mental illnesses. Br J Psychiatry (2000) 177:4–7. doi: 10.1192/bjp.177.1.4
57. Sartorius N, Gaebel W, Cleveland HR, Stuart H, Akiyama T, Arboleda-Florez J, et al. WPA guidance on how to combat stigmatization of psychiatry and psychiatrists. World Psychiatry (2010) 9:131–44. doi: 10.1002/j.2051-5545.2010.tb00296.x
58. Kienast T, Stoffers J, Bermpohl F, Lieb K. Borderline personality disorder and comorbid addiction: epidemiology and treatment. Dtsch Arztebl Int. (2014) 111:280–6. doi: 10.3238/arztebl.2014.0280
59. Gillespie NA, Aggen SH, Neale MC, Knudsen GP, Krueger RF, South SC, et al. Associations between personality disorders and cannabis use and cannabis use disorder: a population-based twin study. Addiction (2018) 113:1488–98. doi: 10.1111/add.14209
60. Habersaat S, Ramain J, Mantzouranis G, Palix J, Boonman C, Fegert JM, et al. Substance-use disorders, personality traits, and sex differences in institutionalized adolescents. Am J Drug Alcohol Abuse (2018) 44:686–94. doi: 10.1080/00952990.2018.1491587
Keywords: compensation imprisonment, mental disorders, penrose hypothesis, transinstitutionalization, DIA-X
Citation: Schildbach S and Schildbach C (2018) Criminalization Through Transinstitutionalization: A Critical Review of the Penrose Hypothesis in the Context of Compensation Imprisonment. Front. Psychiatry 9:534. doi: 10.3389/fpsyt.2018.00534
Received: 06 July 2018; Accepted: 08 October 2018;
Published: 25 October 2018.
Edited by:
Norbert Konrad, Charité Universitätsmedizin Berlin, GermanyReviewed by:
Elmar Habermeyer, Psychiatrische Universitätsklinik Zürich, SwitzerlandCopyright © 2018 Schildbach and Schildbach. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sebastian Schildbach, cHJheGlzLnNlYmFzdGlhbi5zY2hpbGRiYWNoQGhpbi5jaA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.