- 1Section of Neuroscience and Clinical Pharmacology, Department of Biomedical Sciences, University of Cagliari, Monserrato, Italy
- 2Section on Clinical Psychoneuroendocrinology and Neuropsychopharmacology, National Institute on Alcohol Abuse and Alcoholism Division of Intramural Clinical and Basic Research and National Institute on Drug Abuse Intramural Research Program, National Institutes of Health, Bethesda, MD, United States
- 3Medication Development Program, National Institute on Drug Abuse Intramural Research Program, National Institutes of Health, Baltimore, MD, United States
- 4Center for Alcohol and Addiction Studies, Brown University, Providence, RI, United States
A limited number of medications are approved to treat Alcohol Use Disorder (AUD). Furthermore, the magnitude of their therapeutic effect is relatively modest, suggesting the potential for subtypes of patients who respond to a specific medication. The use of these medications is also limited in clinical practice by a series of contraindications such as medical comorbidities and/or concurrent use of other medications. In recent years, animal and human studies have been conducted to evaluate the efficacy of baclofen, a GABAB receptor agonist approved for clinical use as a muscle relaxant, in the treatment of AUD. However, these studies have yielded contrasting results. Despite this discrepancy, baclofen is often used off-label to treat AUD, especially in some European countries and Australia. Recently, several factors have been considered to try to shed light on the potential reasons and mechanisms underlying the inconsistent results obtained until now. The presence of a psychiatric comorbidity may be amongst the abovementioned factors playing a role in explaining different responses to baclofen treatment in terms of alcohol drinking outcomes. Therefore, the aim here was to conduct a narrative review of the scientific literature related to the use of baclofen in AUD, both in patients with and without concomitant psychiatric disorders. All clinical studies (randomized and controlled, open-label, retrospective, human laboratory studies, and case reports) were analyzed and discussed, bearing in mind other potential factors that may have influenced baclofen response, including dose administered, severity of AUD, use of other psychosocial therapies, and the presence of physical disorders. This review indicates that the most frequent psychiatric comorbidities in patients affected by AUD undergoing baclofen treatment are anxiety and mood disorders. Unfortunately, no definitive conclusions can be drawn due to the lack of specific analyses on whether baclofen efficacy is different in AUD patients with comorbid psychiatric disorders vs. those without. Therefore, it will be critical that psychiatric comorbidities are considered in the planning of future studies and in the analysis of the data, with the ultimate goal of understanding whether subtypes of AUD patients may respond best to baclofen.
Introduction
AUD and Need for Other Medications
Alcohol Use Disorder (AUD) is a severe and complex mental disorder mainly characterized by excessive alcohol consumption and the inability to control it (1). Despite being one of the leading causes of morbidity and mortality worldwide (2, 3), only a limited number of medications are available to help AUD patients achieve abstinence or reduce their alcohol consumption (4, 5). In most countries (e.g., Europe, North America, Australia, parts of Asia, and Africa), these medications include disulfiram, naltrexone, and/or acamprosate (6, 7). Recently, nalmefene was also approved in Europe (6). Unfortunately, only a very small number of AUD patients receive these medications. In the US, <10% of people with AUD receive any type of alcohol treatment (8) and fewer than 4% receive a medication as an intervention or treatment (9).
Possible reasons for the underutilization of medications for AUD include a lack of knowledge, by both patients and physicians, and the misperceptions that medications do not work or that AUD should not be treated with a medication (6). However, certain characteristics of AUD medications also contribute to discouraging physicians from prescribing them. Globally, the magnitude of the therapeutic effects of AUD medications is relatively modest (4), and patient response may differ to a specific drug (10, 11). AUD medications are also contraindicated in patients with some medical comorbidities (4, 5, 12, 13). For instance, naltrexone and disulfiram are contraindicated amongst patients with clinically-relevant liver diseases; on the other hand, acamprosate is contraindicated in patients with kidney failure. Furthermore, disulfiram should not be used in patients who are not capable of understanding the risks of consuming alcohol while they are taking disulfiram. In clinical practice, these conditions are frequent and contribute to a further reduction in the available treatment choices for AUD patients. Another frequent condition in clinical practice is the presence of comorbid mental disorders such as substance use disorder, mood disorder, and/or anxiety disorder, especially among patients with more severe AUD (14). The use of medications for AUD among these latter patients is even lower than among AUD patients without other comorbid mental disorders, because of the concern of medication-alcohol interactions (15). For all these reasons, the identification of new, safe, and effective medications is a critical priority in the field of AUD treatment (16–18).
Baclofen and AUD
Baclofen is a GABAB receptor agonist approved for clinical use as a muscle relaxant. In recent years, animal and human studies conducted to evaluate the efficacy of baclofen in the treatment of AUD have yielded contrasting results (19). Despite this discrepancy, baclofen is often used to treat AUD, especially in European countries and Australia, as a consequence of the wide off-label prescription of the drug by general practitioners (20). Recently, several factors have been considered and analyzed to shed light on the potential reasons and mechanisms underlying the inconsistent treatment results obtained until now. It has been suggested that the presence of a psychiatric comorbidity may be amongst the abovementioned factors playing a role in explaining different responses to baclofen treatment, in terms of alcohol drinking outcomes. Preclinical and clinical findings clearly indicate a key role of the GABAB receptor in depression and anxiety disorders (21, 22). Some studies found that baclofen reduces anxiety levels in AUD patients (23–25). Conversely, other studies did not find significant effects of baclofen on anxiety levels in AUD patients (26), or they found that patients without comorbid mental disorders achieved better results compared to patients with comorbid mental disorders (27–29). Therefore, the aim of the present paper was to conduct a narrative review of the scientific literature related to the clinical use of baclofen in AUD to achieve abstinence or reduce alcohol consumption, both in patients with and without concomitant psychiatric disorders. All clinical studies (randomized and controlled, open-label, retrospective, test-tube lab research, and case reports) were summarized and discussed, bearing in mind other potential factors that may have influenced baclofen response, e.g., baclofen dose, severity of AUD, use of other psychosocial therapies, and the presence of medical comorbidities.
Methodology
Data were obtained for the narrative mini-review by searching the published medical literature in Medline (PubMed) up to May 2018. There were no language restrictions; the search was limited to humans. The search terms used included alcoholism or AUD or alcohol dependence AND baclofen.
Review of the Scientific Literature Related to the Use of Baclofen in AUD Both in Patients With and Without Concomitant Psychiatric Disorders
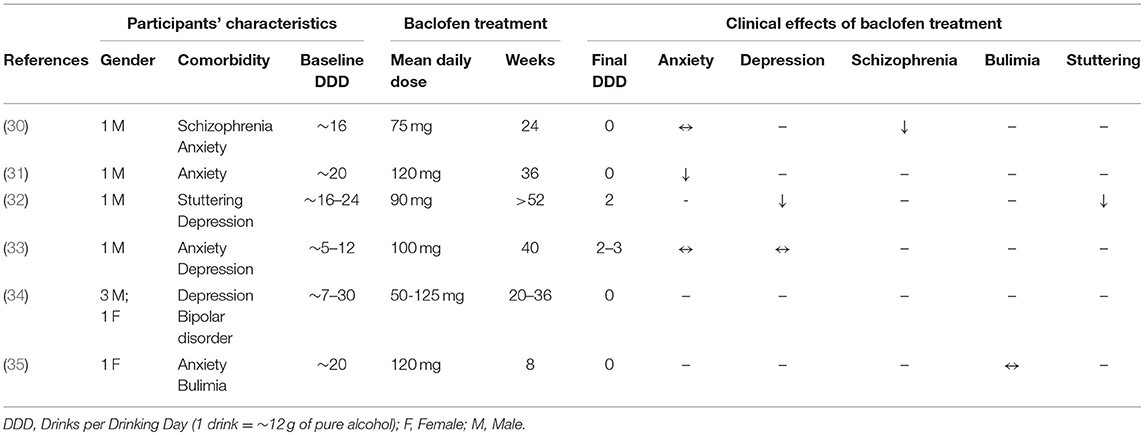
Case Reports
A few case reports describe the results obtained by the use of baclofen in AUD patients [see Table 1; (30–35)]. All these patients suffered from severe AUD, as shown by their high level of alcohol consumption at baseline, the lack of a response to other previous treatments for AUD, and the presence of one or more comorbid psychiatric disorders, such as anxiety, mood disorder, schizophrenia, and bulimia. Patients received daily doses of baclofen, ranging from 50 to 120 mg, and were followed for a timeframe ranging from 8 to 52 weeks. In all these patients, baclofen administration led to alcohol abstinence or to a marked reduction in alcohol consumption. On the other hand, possible effects of baclofen on the severity of the other mental disorders were not reported by most of the studies and, when reported, the results were contrasting.
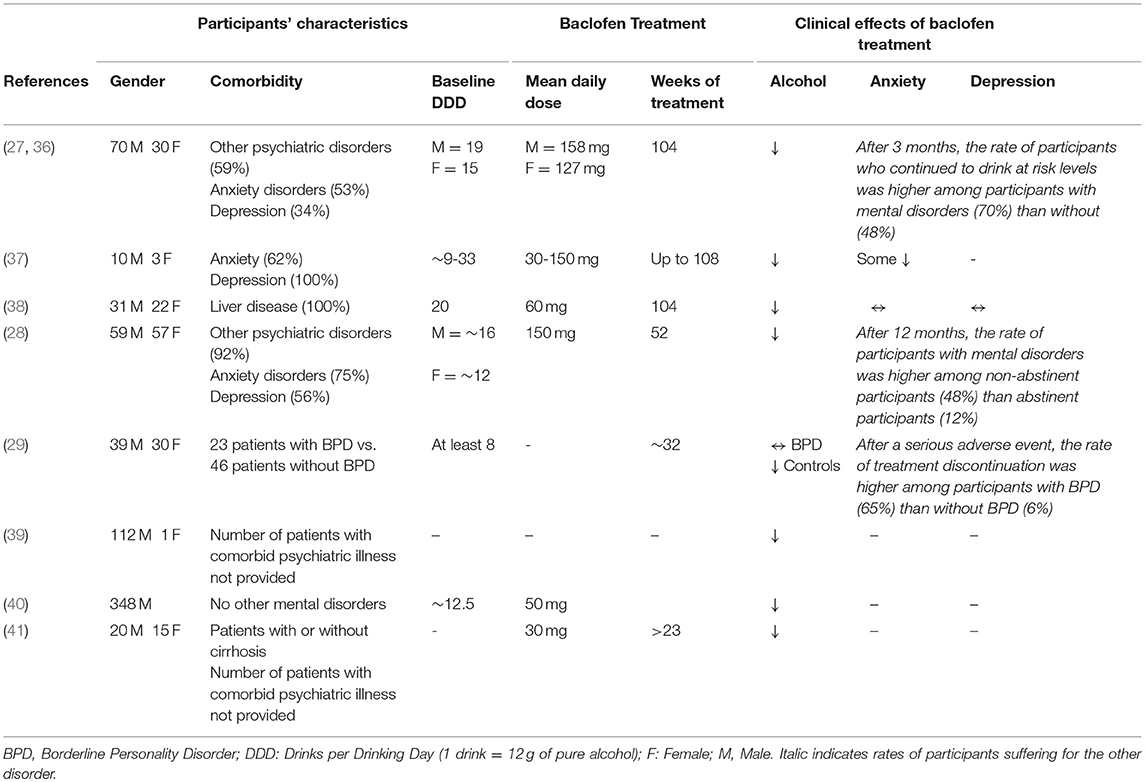
Retrospective Studies
A series of retrospective studies evaluated the efficacy of baclofen among large samples of AUD patients [see Table 2; (27–29, 36–41)]. These patients showed high baseline levels of alcohol consumption, were not responders to previous pharmacological treatments, and suffered from other mental or physical disorders. The majority of these patients suffered mainly from anxiety and depression (27, 36, 37), whereas two studies were conducted in AUD patients with clinically-significant liver disease (38, 41). The daily doses of baclofen ranged from 30 to ~150 mg. One study observed that the average dose received by female patients was lower than the one received by males (27). Three studies found that patients without comorbid mental disorders achieved better results compared to patients with comorbid mental disorders [anxiety, depression, and/or borderline personality disorder; 27–29]]. Another study did not find a significant effect of baclofen on either anxiety or depression, which were evaluated using self-reported rating scales (38).
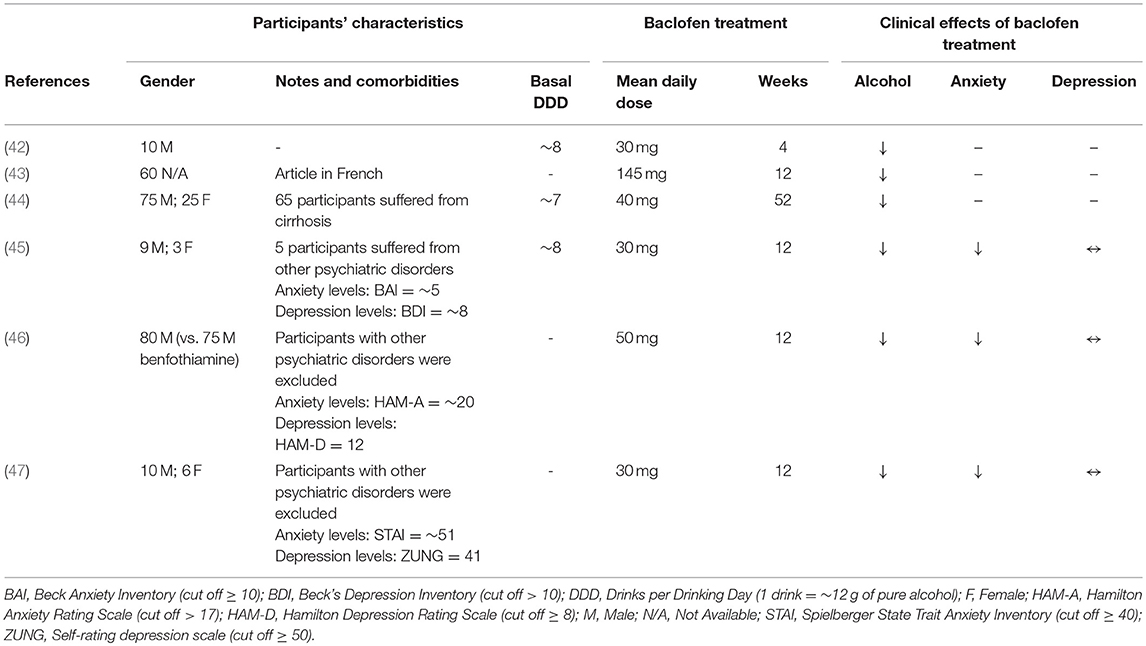
Open Studies
Table 3 shows open studies in which baclofen was administered to help AUD patients to achieve abstinence or reduce alcohol consumption [see Table 3; (42–47)]. Among these studies, only three provided information on comorbid mental disorders (45–47): in one study (45), five out of twelve participants suffered from mental disorders other than AUD; in the other two studies, patients with severe mental disorders, other than AUD, were excluded (46, 47). In all studies, participants received daily doses of baclofen ranging from 30 to 145 mg and were monitored from 4 to 52 weeks. All these studies reported that baclofen reduced alcohol consumption. Among the studies in which the anxiety and depression levels of participants were evaluated, baclofen administration reduced anxiety but not depression levels (45–47).
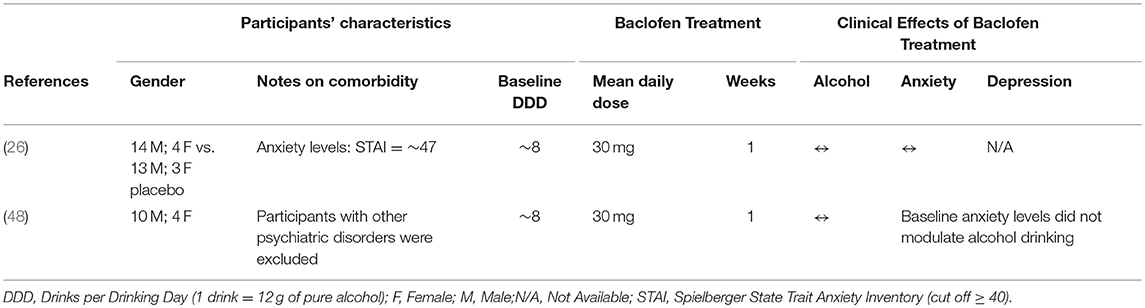
Human Laboratory Studies
Two laboratory studies investigated the effects of baclofen in non-treatment seeking AUD participants [see Table 4; (26, 48)]. In both studies, participants received 30 mg/day baclofen for approximately a week. In one study, participants with recent (past 6 months) mental disorders, other than AUD, were excluded (48). In the other one, participants had high anxiety levels (see Table 4), but only a few participants had a formal diagnosis, based on DSM-IV, of current anxiety disorders (5 out of 34) or current mood disorder (1 out of 34) (26). One study found that baclofen reduced alcohol self-administration but not cue-elicited craving; furthermore, baseline anxiety levels did not modulate alcohol drinking (48). The other one did not report significant effects of baclofen on either alcohol consumption, cue-elicited craving, or anxiety levels (26). In both studies, baclofen amplified the subjective effects of alcohol, which was suggested as a potential biobehavioral mechanism of how baclofen may affect alcohol drinking (26, 48).
Randomized Double-Blind Placebo-Controlled Trials
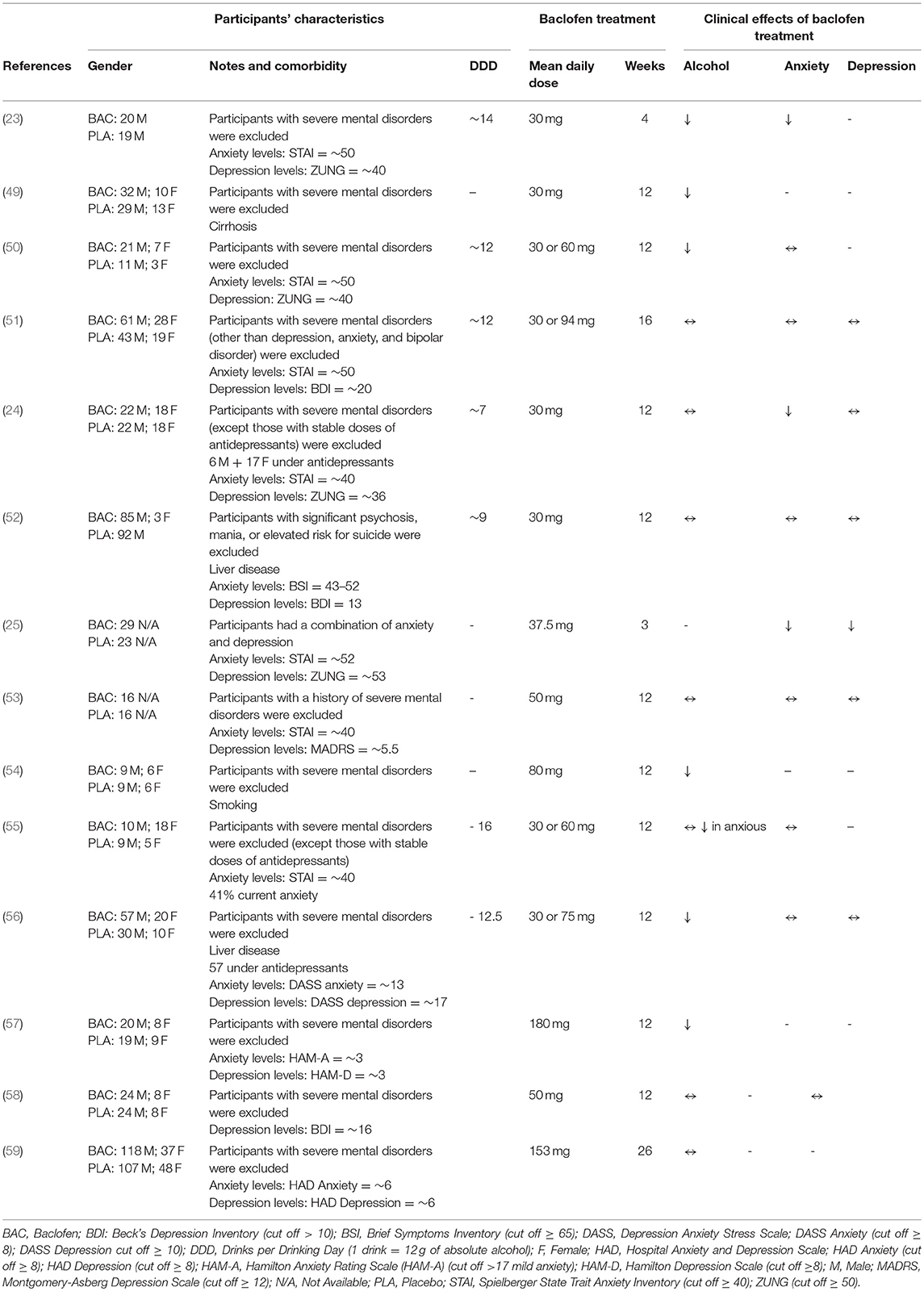
The findings of the randomized, double-blind placebo-controlled trials of baclofen in the treatment of AUD are outlined in Table 5 (23–25, 49–59). All the studies excluded participants with severe mental disorders other than AUD but, in some studies, participants who received stable doses of antidepressants (24, 55, 56) or participants affected by depression, anxiety, and/or bipolar disorder (51) were allowed to participate. Participants received daily doses of baclofen ranging from 30 to 180 mg for a timeframe ranging from 3 to 26 weeks. All the studies, except two (49, 54), reported the mean values of anxiety and/or depression levels. Most studies used self-reported rating scales such as STAI (Spielberger State Trait Anxiety Inventory) for anxiety and BDI (Beck's Depression Inventory) or ZUNG for depression. Only a few studies used interviewer-rated scales such as HAM-A (Hamilton Anxiety Rating Scale) for anxiety and HAM-D (Hamilton Depression Rating Scale) or MADRS (Montgomery-Asberg Depression Scale) for depression.
In two studies, participants had high baseline anxiety levels (23, 50), in two other studies high baseline depression levels (52, 58), and in three studies both high baseline anxiety and depression levels (25, 51, 56). Baclofen administration induced contrasting results regarding alcohol consumption. It reduced alcohol consumption in some studies (23, 49, 50, 54, 55, 57), but not in others (24, 51–53, 55, 58, 59). One study suggested a relationship between comorbid anxiety and treatment response to baclofen (55). In this study, baclofen administration reduced alcohol consumption in anxious patients, but did not induce significant modifications in other participants. However, this relationship was not observed in other studies. Baclofen reduced alcohol consumption in studies in which participants had high (23, 50, 56) or low (57) baseline anxiety levels. On the other hand, baclofen failed to modify alcohol consumption in other studies in which participants had high (51) or low (59) baseline anxiety levels. No study provided the results obtained specifically in participants affected by other mental disorders.
Discussion
The presence of another mental disorder, such as anxiety and depression, other than AUD represents a frequent and complex clinical phenomenon (1, 14, 60). The pharmacological treatment of AUD patients affected by comorbid mental disorders represents a significant challenge (61, 62). AUD and a second mental disorder may occur independently, or one of the two disorders may have influenced the development of the other one (1, 63). For instance, an anxious patient may develop AUD as consequence of the excessive alcohol consumption to self-medicate anxiety. On the other hand, AUD patients frequently develop temporary alcohol-induced depressive and/or anxiety symptoms during intoxication and/or withdrawal (63). Accordingly, physicians need to establish if AUD patients with a comorbid mental disorder require a pharmacological treatment for both the conditions (e.g., if both the conditions are severe and long lasting) or not (e.g., if co-occurrent symptoms are alcohol-induced and tend to resolve without treatment within 3–4 weeks) (63).
According to preclinical studies, GABAB receptors modulate anxiety and depression-related behaviors (21), and baclofen may induce better results among AUD patients affected by anxiety and/or mood disorders through a reduction of the severity of these disorders. The present narrative mini-review was aimed at investigating the role of psychiatric comorbidity in explaining potential different responses to baclofen treatment among AUD patients. The results show that the majority of AUD patients treated with baclofen and described by the case reports, as well as the observational and retrospective studies, suffered from anxiety and/or mood disorders. This finding agrees with data of large epidemiological studies (14, 60). However, the results of the present review also show that, despite these disorders being common among AUD patients, patients with severe mental disorders (including severe anxiety and mood disorders) were excluded by the randomized, controlled, trials (RCTs) conducted to evaluate the efficacy of baclofen to treat AUD. Therefore, these results do not allow us o evaluate whether baclofen efficacy is different in AUD patients with comorbid psychiatric disorders compared to those without. One RCT found that baclofen administration reduced alcohol consumption in anxious patients, but not in patients with low levels of anxiety (55). However, in this study, baclofen administration did not significantly reduce anxiety levels. A recent meta-analysis also found no difference between baclofen and placebo in reducing both depression and anxiety levels among AUD patients (64). The results of the present review may be useful to better understand these results. Indeed, both these studies (55, 64) evaluated the efficacy of baclofen in modifying the severity of anxiety or depression among AUD patients not affected by severe mental disorders. In addition, the RCTs used different scales to measure the severity of anxiety and/or depression, such as self-reported rating scales (e.g., STAI, BDI, and ZUNG) and interviewer-rated scales (e.g., HAM-A, HAM-D, and MADRS). The exclusion of patients with severe mental disorders, and the variability in the scales adopted, prevents current meta-analyses to evaluate potential differences in baclofen efficacy in reducing the severity of the comorbid mental disorders. To reduce the variability, the interviewer-rated scales should be used rather than self-reported rating scales (65, 66). Accordingly, it is desirable that future RCTs investigate the efficacy of baclofen in AUD patients affected by other mental disorders, using interviewer-rated scales to establish the effects on the severity of anxiety and/or depression.
Conclusions
There is a critical need to develop novel medications for AUD. In addition, the new diagnostic criteria of AUD in the DSM-5 may increase the prevalence of new cases of this mental disorder, compared to the criteria provided by the DSM-IV (67), therefore the importance of developing new effective treatments is even greater. The GABAB receptor represents a promising pharmacological target, a concept that has been supported by a plethora of animal studies. Medication development for CNS indications is challenging and, indeed, the translation of findings from animal models to humans is one of the most difficult steps in this field. The presence of both positive and negative RCTs is not uncommon in the AUD literature. The medication development field, at large, and the results of recent meta-analyses show baclofen is not exempt from this pattern (65, 68, 69). Inconsistencies across studies may be due to several factors, which may include (but are not limited to) differences at several levels, e.g., (a) medication-related differences like baclofen doses, medication adherence, interactions with other concomitant medications, or pharmacokinetics; (b) patient-related differences like gender, severity of AUD, tolerance to baclofen's effects, psychiatric comorbidities, or medical comorbidities; and (c) geographic- and site-related differences like specific patient-provider interactions, or amount and type of behavioral interventions provided in addition to the medication. These factors are likely to explain not only why RCTs have yielded different results, but also why analyses focused on one specific factor (e.g., baclofen dose, patients with anxiety comorbidity) have also generated conflicting results. Despite the lack of consistent evidence of efficacy, baclofen is frequently used off-label to treat AUD, especially in some European countries and Australia (70). It is preferable that future prospective studies and meta-analytical efforts try to look at the interactions of all these factors as they relate to the medication, patient, and site, in order to identify which are, if any, the best variables that may predict the patient's phenotype that is most likely to benefit from the treatment with baclofen. Finally, it is important to keep in mind that, while baclofen represents the prototypic agonist of the GABAB receptor, very promising rodent data suggest the GABAB positive allosteric modulators may represent a better pharmacological approach (19). Therefore, future efforts should also focus on profiling these compounds from a toxicology and safety standpoint, in order to bring them to the clinical setting and test their safety and potential efficacy in humans.
Author Contributions
RA led the literature search and drafted the manuscript. LL provided substantial contributions to the intellectual content of the manuscript. Both authors approved the final version of the manuscript.
Funding
RA is supported by the University of Cagliari intramural funding FIR 2017. LL is supported by the National Institutes of Health (NIH) intramural funding ZIA-AA000218, Section on Clinical Psychoneuroendocrinology and Neuropsychopharmacology, jointly supported by the Division of Intramural Clinical and Biological Research of the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and the Intramural Research Program of the National Institute on Drug Abuse (NIDA). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the funders, which had no role in the development of this article.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorder (DSM-5). Washington, DC: American Psychiatric Association (2013).
2. Forouzanfar MH, Afshin A, Alexander LT, Anderson HR, Bhutta ZA, Biryukov S, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet (2016) 388:1659–724. doi: 10.1016/S0140-6736(16)31679-8
3. Kassebaum NJ, Arora M, Barber RM, Bhutta ZA, Brown J, Carter A, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet (2016) 388:1603–58. doi: 10.1016/S0140-6736(16)31460-X
4. Soyka M, Kranzler HR, Hesselbrock V, Kasper S, Mutschler J, Möller HJ. WFSBP task force on treatment guidelines for substance use disorders. guidelines for biological treatment of substance use and related disorders, part 1: alcoholism, first revision. World J Biol Psychiatry (2017) 18:86–119. doi: 10.1080/15622975.2016.1246752
5. Reus VI, Fochtmann LJ, Bukstein O, Eyler AE, Hilty DM, Horvitz-Lennon M, et al. The american psychiatric association practice guideline for the pharmacological treatment of patients with alcohol use disorder. Am J Psychiatry (2018) 175:86–90. doi: 10.1176/appi.ajp.2017.1750101
6. Goh ET, Morgan MY. Review article: pharmacotherapy for alcohol dependence - the why, the what and the wherefore. Aliment Pharmacol Ther. (2017) 45:865–82. doi: 10.1111/apt.13965
7. Soyka M, Müller CA. Pharmacotherapy of alcoholism - an update on approved and off-label medications. Expert Opin Pharmacother. (2017) 18:1187–99. doi: 10.1080/14656566.2017.1349098
8. Center for Behavioral Health Statistics and Quality. 2016 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration (2017).
9. Mark TL, Kassed CA, Vandivort-Warren R, Levit KR, Kranzler HR. Alcohol and opioid dependence medications: prescription trends, overall and by physician specialty. Drug Alcohol Depend. (2009) 99:345–9. doi: 10.1016/j.drugalcdep.2008.07.018
10. Leggio L, Kenna GA, Fenton M, Bonenfant E, Swift RM. Typologies of alcohol dependence. From Jellinek to genetics and beyond. Neuropsychol Rev. (2009) 19:115–29. doi: 10.1007/s11065-008-9080-z
11. Jones JD, Comer SD, Kranzler HR. The pharmacogenetics of alcohol use disorder. Alcohol Clin Exp Res. (2015) 39:391–402. doi: 10.1111/acer.12643
12. Antonelli M, Ferrulli A, Sestito L, Vassallo GA, Tarli C, Mosoni C, et al. Alcohol addiction–the safety of available approved treatment options. Expert Opin Drug Saf. (2018) 17:169–77. doi: 10.1080/14740338.2018.1404025
13. Sinclair JM, Chambers SE, Shiles CJ, Baldwin DS. Safety and tolerability of pharmacological treatment of alcohol dependence: comprehensive review of evidence. Drug Saf. (2016) 39:627–45. doi: 10.1007/s40264-016-0416-y
14. Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, et al. Epidemiology of DSM-5 alcohol use disorder: results ffrom the national epidemiologic survey on alcohol and related conditions III. JAMA Psychiatry (2015) 72:757–66. doi: 10.1001/jamapsychiatry.2015.0584
15. Pettinati HM, O'Brien CP, Dundon WD. Current status of co-occurring mood and substance use disorders: a new therapeutic target. Am J Psychiatry (2013) 170:23–30. doi: 10.1176/appi.ajp.2012.12010112
16. Litten RZ, Falk DE, Ryan ML, Fertig JB. Discovery, development, and adoption of medications to treat alcohol use disorder: goals for the phases of medications development. Alcohol Clin Exp Res. (2016) 40:1368–79. doi: 10.1111/acer.13093
17. Litten RZ, Falk DE, Ryan ML, Fertig J, Leggio L. Advances in pharmacotherapy development: human clinical studies. In: Handbook of Experimental Pharmacology. Berlin, Heidelberg: Springer (2017).
18. Lyon J. More treatments on deck for alcohol use disorder. JAMA (2017) 317:2267–9. doi: 10.1001/jama.2017.4760
19. Agabio R, Leite-Morris K, Addolorato G, Colombo G. Targeting the GABAB receptor for the treatment of alcohol use disorder. In: Colombo G editors. GABAB Receptor. Basel: Springer International Publishing Switzerland (2016).
20. Rolland B, Bordet R, Cottencin O. Alcohol-dependence: the current French craze for baclofen. Addiction (2012) 107:848–9. doi: 10.1111/j.1360-0443.2011.03752.x
21. Felice D, O'Leary OF, Cryan JF. Targeting the GABAB receptor for the treatment of depression and anxiety disorders. In: Colombo G. editors. GABAB Receptor. Basel: Springer International Publishing Switzerland (2016).
22. Jacobson LH, Vlachou S, Slattery DA, Li X, Cryan JF. The gamma-aminobutyric acid b receptor in depression and reward. Biol Psychiatry (2018) 83:963–76. doi: 10.1016/j.biopsych.2018.02.006
23. Addolorato G, Caputo F, Capristo E, Domenicali M, Bernardi M, Janiri L, et al. Baclofen efficacy in reducing alcohol craving and intake: a preliminary double- blind randomized controlled study. Alcohol Alcohol (2002) 37:504–8. doi: 10.1093/alcalc/37.5.504
24. Garbutt JC, Kampov-Polevoy AB, Gallop R, Kalka-Juhl L, Flannery BA. Efficacy and safety of baclofen for alcohol dependence: a randomized, double-blind, placebo-controlled trial. Alcohol Clin Exp Res. (2010) 34:1849–57. doi: 10.1111/j.1530-0277.2010.01273.x
25. Krupitsky EM, Burakov AM, Ivanov VB, Krandashova GF, Lapin IP, Grinenko A, et al. Baclofen administration for the treatment of affective disorders in alcoholic patients. Drug Alcohol Depend (1993) 33:157–63. doi: 10.1016/0376-8716(93)90057-W
26. Farokhnia M, Schwandt ML, Lee MR, Bollinger JW, Farinelli LA, Amodio JP, et al. Biobehavioral effects of baclofen in anxious alcohol-dependent individuals: a randomized, double-blind, placebo-controlled, laboratory study. Transl Psychiatry (2017) 7:e1108. doi: 10.1038/tp.2017.71
27. de Beaurepaire R. Suppression of alcohol dependence using baclofen: a 2-year observational study of 100 patients. Front Psychiatry (2012) 3:103. doi: 10.3389/fpsyt.2012.00103
28. Rigal L, Alexandre-Dubroeucq C, de Beaurepaire R, Le Jeunne C, Jaury P. Abstinence and “low-risk” consumption 1 year after the Initiation of high-dose baclofen: a retrospective study among “high-risk” drinkers. Alcohol Alcohol (2012) 47:439–42. doi: 10.1093/alcalc/ags028
29. Rolland B, Valin T, Langlois C, Auffret M, Gautier S, Deheul S, et al. Safety and drinking outcomes among patients with comorbid alcohol dependence and borderline personality disorder treated with high-dose baclofen: a comparative cohort study. Int Clin Psychopharmacol. (2015) 30:49–53. doi: 10.1097/YIC.0000000000000054
30. Agabio R, Marras P, Addolorato G, Carpiniello B, Gessa GL. Baclofen suppresses alcohol intake and craving for alcohol in a schizophrenic alcohol-dependent patient: a case report. J Clin Psychopharmacol. (2007) 27:319–20. doi: 10.1097/01.jcp.0000270079.84758.fe
31. Ameisen O. Complete and prolonged suppression of symptoms and consequences of alcohol-dependence using high-dose baclofen: a self-case report of a physician. Alcohol Alcohol. (2005) 40:147–50. doi: 10.1093/alcalc/agh130
32. Beraha E, Bodewits P, van den Brink W, Wiers R. Speaking fluently with baclofen? BMJ Case Rep. (2017). doi: 10.1136/bcr-2016-218714
33. Bucknam W. Suppression of symptoms of alcohol dependence and craving using high-dose baclofen. Alcohol Alcohol. (2007) 42:158–60. doi: 10.1093/alcalc/agl091
34. Pastor A, Jones DM, Currie J. High-dose baclofen for treatment-resistant alcohol dependence. J Clin Psychopharmacol. (2012) 32:266–8. doi: 10.1097/JCP.0b013e31824929b2
35. Weibel S, Lalanne L, Riegert M, Bertschy G. Efficacy of high-dose baclofen for alcohol use disorder and comorbid bulimia: a case report. J Dual Diagn. (2015) 11:203–4. doi: 10.1080/15504263.2015.1104483
36. de Beaurepaire R. The use of very high doses of baclofen in the treatment of alcohol dependence: a case series. Front Psychiatry (2014) 5:143. doi: 10.3389/fpsyt.2014.00143
37. Dore GM, Lo K, Juckes L, Bezyan S, Latt N. Clinical experience with baclofen in the management of alcohol-dependent patients with psychiatric comorbidity: a selected case series. Alcohol Alcohol. (2011) 46:714–20. doi: 10.1093/alcalc/agr131
38. Heydtmann M, Macdonald B, Lewsey J, Masson N, Cunningham L, Irnazarow A, et al. Tailored dose baclofen in patients with alcoholic liver disease: a case series with 2-year follow-up of hospitalisation. Addict Res Theor. (2015) 23:510–7. doi: 10.3109/16066359.2015.1040003
39. Rozatkar AR, Kapoor A, Sidana A, Chavan BS. Clinical experience of baclofen in alcohol dependence: a chart review. Ind Psychiatry J. (2016) 25:11–6. doi: 10.4103/0972-6748.196043
40. Shukla L, Shukla T, Bokka S, Kandasamy A, Benegal V, Murthy P, et al. Correlates of baclofen effectiveness in alcohol dependence. Indian J Psychol Med. (2015) 37:370–3. doi: 10.4103/0253-7176.162913
41. Yamini D, Lee SH, Avanesyan A, Walter M, Runyon B. Utilization of baclofen in maintenance of alcohol abstinence in patients with alcohol dependence and alcoholic hepatitis with or without cirrhosis. Alcohol Alcohol. (2014) 49:453–6. doi: 10.1093/alcalc/agu028
42. Addolorato G, Caputo F, Capristo E, Colombo G, Gessa GL, Gasbarrini G. Ability of baclofen in reducing alcohol craving and intake: II–Preliminary clinical evidence. Alcohol Clin Exp Res. (2000) 24:67–71. doi: 10.1111/j.1530-0277.2000.tb04555.x
43. Ameisen O, de Beaurepaire R. Suppression of alcohol dependence and alcohol consumption with high-dose baclofen: an open trial [Suppression de la dépendance à l'alcool et de la consommation d'alcool par le baclofène à haute dose: un essai en ouvert]. Ann Méd-Psychol. (2010) 168:159–62. [In French]. doi: 10.1016/j.amp.2009.12.008
44. Barrault C, Lison H, Roudot-Thoraval F, Garioud A, Costentin C, Béhar V, et al. One year of baclofen in 100 patients with or without cirrhosis: a French real-life experience. Eur J Gastroenterol Hepatol. (2017) 29:1155–60. doi: 10.1097/MEG.0000000000000922
45. Flannery BA, Garbutt JC, Cody MW, Renn W, Grace K, Osborne M, et al. Baclofen for alcohol dependence: a preliminary open-label study. Alcohol Clin Exp Res. (2004) 28:1517–23. doi: 10.1097/01.ALC.0000141640.48924.14
46. Gupta M, Verma P, Rastogi R, Arora S, Elwadhi D. Randomized open-label trial of baclofen for relapse prevention in alcohol dependence. Am J Drug Alcohol Abuse (2017) 43:324–31. doi: 10.1080/00952990.2016.1240797
47. Leggio L, Ferrulli A, Cardone S, Miceli A, Kenna GA, Gasbarrini G, et al. Renin and aldosterone but not the natriuretic peptide correlate with obsessive craving in medium-term abstinent alcohol-dependent patients: a longitudinal study. Alcohol (2008) 42:375–81. doi: 10.1016/j.alcohol.2008.03.128
48. Leggio L, Zywiak WH, McGeary JE, Edwards S, Fricchione SR, Shoaff JR, et al. A human laboratory pilot study with baclofen in alcoholic individuals. Pharmacol Biochem Behav. (2013) 103:784–91. doi: 10.1016/j.pbb.2012.11.013
49. Addolorato G, Leggio L, Ferrulli A, Cardone S, Vonghia L, Mirijello A, et al. Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet (2007) 370:1915–22. doi: 10.1016/S0140-6736(07)61814-5
50. Addolorato G, Leggio L, Ferrulli A, Cardone S, Bedogni G, Caputo F, et al. Baclofen Study Group. Dose-response effect of baclofen in reducing daily alcohol intake in alcohol dependence: secondary analysis of a randomized, double-blind, placebo-controlled trial. Alcohol Alcohol. (2011) 46:312–7. doi: 10.1093/alcalc/agr017
51. Beraha EM, Salemink E, Goudriaan AE, Bakker A, de Jong D, Smits N, et al. Efficacy and safety of high-dose baclofen for the treatment of alcohol dependence: a multicentre, randomised, double-blind controlled trial. Eur Neuropsychopharmacol. (2016) 26:1950–9. doi: 10.1016/j.euroneuro.2016.10.006
52. Hauser P, Fuller B, Ho SB, Thuras P, Kern S, Dieperink E. The safety and efficacy of baclofen to reduce alcohol use in veterans with chronic hepatitis C: a randomized controlled trial. Addiction (2017) 112:1173–83. doi: 10.1111/add.13787
53. Krupitsky EM, Rybakova KV, Kiselev AS, Alexeeva YV, Berntsev VA, Chekhlaty EI, et al. Double blind placebo controlled randomized pilot clinical trial of baclofen (Baclosan(R)) for alcohol dependence. Zh Nevrol Psikhiatr Im S S Korsakova (2015) 115:53–62. doi: 10.17116/jnevro20151156153-62
54. Leggio L, Zywiak WH, Edwards SM, Tidey JW, Swift RM, Kenna GA. A preliminary double-blind, placebo-controlled randomized study of baclofen effects in alcoholic smokers. Psychopharmacology (Berl) (2015) 232:233–43. doi: 10.1007/s00213-014-3652-9
55. Morley KC, Baillie A, Leung S, Addolorato G, Leggio L, Haber PS. Baclofen for the treatment of alcohol dependence and possible role of comorbid anxiety. Alcohol Alcohol. (2014) 49:654–60. doi: 10.1093/alcalc/agu062
56. Morley KC, Baillie A, Fraser I, Furneaux-Bate A, Dore G, Roberts M, et al. Baclofen in the treatment of alcohol dependence with or without liver disease: multisite, randomised, double-blind, placebo-controlled trial. Br J Psychiatry (2018) 212:362–9. doi: 10.1192/bjp.2018.13
57. Müller CA, Geisel O, Pelz P, Higl V, Krüger J, Stickel A, et al. High-dose baclofen for the treatment of alcohol dependence (BACLAD study): a randomized, placebo-controlled trial. Eur Psychopharmacol. (2015) 25:1167–77. doi: 10.1016/j.euroneuro.2015.04.002
58. Ponizovsky AM, Rosca P, Aronovich E, Weizman A, Grinshpoon A. Baclofen as add-on to standard psychosocial treatment for alcohol dependence: a randomized, double-blind, placebo-controlled trial with 1year follow-up. J Subst Abuse Treat. (2015) 52:24–30. doi: 10.1016/j.jsat.2014.11.007
59. Reynaud M, Aubin HJ, Trinquet F, Zakine B, Dano C, Dematteis M, et al. A randomized, placebo-controlled study of high-dose baclofen in alcohol-dependent patients-the ALPADIR study. Alcohol Alcohol. (2017) 52:439–46. doi: 10.1093/alcalc/agx030
60. Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry (2007) 64:830–42. doi: 10.1001/archpsyc.64.7.830
61. Agabio R, Trogu E, Pani PP. Antidepressants for the treatment of people with co-occurring depression and alcohol dependence. Cochrane Database Syst Rev. (2018) 4:CD008581. doi: 10.1002/14651858.CD008581.pub2
62. Ipser JC, Wilson D, Akindipe TO, Sager C, Stein DJ. Pharmacotherapy for anxiety and comorbid alcohol use disorders. Cochrane Database Syst Rev. (2015) 1:CD007505. doi: 10.1002/14651858.CD007505.pub2
63. Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction (2006) 101(Suppl 1):76–88. doi: 10.1111/j.1360-0443.2006.01592.x
64. Rose AK, Jones A. Baclofen: its effectiveness in reducing harmful drinking, craving, and negative mood. A meta-analysis. Addiction (2018) 113:1396–406. doi: 10.1111/add.14191
65. Altman E, Gilmore C, Peterson J, Andriukaitis S. Psychiatric rating scales in diagnostic assessment and clinical treatment. Psychiatr Med. (1991) 9:189–211.
66. Möller HJ. Rating depressed patients: observer- vs self-assessment. Eur Psychiatry (2000) 15:160–72. doi: 10.1016/S0924-9338(00)00229-7
67. Bartoli F, Carrà G, Crocamo C, Clerici M. From DSM-IV to DSM-5 alcohol use disorder: an overview of epidemiological data. Addict Behav. (2015) 41:46–50. doi: 10.1016/j.addbeh.2014.09.029
68. Bschor T, Henssler J, Müller M, Baethge C. Baclofen for alcohol use disorder-a systematic meta-analysis. Acta Psychiatr Scand. (2018). doi: 10.1111/acps.12905. [Epub ahead of print].
Keywords: GABAB, baclofen, alcohol use disorder, mental health disorders, anxiety, mood disorders
Citation: Agabio R and Leggio L (2018) Baclofen in the Treatment of Patients With Alcohol Use Disorder and Other Mental Health Disorders. Front. Psychiatry 9:464. doi: 10.3389/fpsyt.2018.00464
Received: 13 July 2018; Accepted: 06 September 2018;
Published: 28 September 2018.
Edited by:
Alain Dervaux, Centre Hospitalier Universitaire (CHU) de Amiens, FranceReviewed by:
Kirsten Morley, University of Sydney, AustraliaGiuseppe Carrà, Università degli Studi di Milano Bicocca, Italy
Copyright © 2018 Agabio and Leggio. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Roberta Agabio, YWdhYmlvQHVuaWNhLml0">e-mailYWdhYmlvQHVuaWNhLml0
 Roberta Agabio
Roberta Agabio Lorenzo Leggio
Lorenzo Leggio