- 1National Addiction Management Service, Institute of Mental Health, Singapore, Singapore
- 2Family Medicine and Primary Care, Lee Kong Chian School of Medicine, Nanyang Technological University Singapore, Singapore, Singapore
- 3National Psychiatry Residency Program, National Healthcare Group, Singapore, Singapore
- 4Department of Developmental Psychiatry, Institute of Mental Health, Singapore, Singapore
Background: Opiates, cannabis, and stimulants are highly abused and are prevalent disorders. Psychological interventions are crucial given that they help individuals maintain abstinence following a lapse or relapse into substance use. The dual-process theory has posited that while the repeated use of a substance leads to increased automatic processing and increased automatic tendencies to approach substance-specific cues, in addition to the inhibition of other normal cognitive processes. Prior reviews are limited, as they failed to include trials involving participants with these prevalent addictive disorders or have not reviewed the published literature extensively.
Objectives: The primary aim of this review is to synthesize the evidence for cognitive biases in opioid use, cannabis use, and stimulant use disorders. The secondary aim of the review is to determine if cognitive bias could be consistently detected using the different methods. Lastly, this review will narratively synthesize the evidence of possible associations between cognitive biases and other addiction-related outcomes.
Methods: A search was conducted from November 2017 to January 2018 on PubMed, MEDLINE, Embase, PsycINFO, Science Direct, Cochrane Central, and Scopus. Articles were included if participants had a primary diagnosis of opioid use, cannabis use, or stimulant use disorder. The selection process of the articles was in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines. A qualitative synthesis was undertaken.
Results: A total of 38 studies were identified. The main finding is the evidence that cognitive biases are present in the 38 studies identified, except for a single study on opioid use and stimulant use disorders. Cognitive biases were reported despite a variety of different methods being utilized. Synthesis of secondary outcome was not feasible, due to the varied outcomes reported.
Conclusions: Cognitive biases have been consistently observed in opioid use, cannabis use, and stimulant use disorders, despite a range of assessment tools being utilized in the assessment for these biases.
Introduction
Attention bias in substance use disorder refers to the preferential allocation of attention to substance-related stimuli (1), while approach biases refer to the automatic action tendencies to reach out for substance-related cues (1). Thus, this implies that for an individual with a substance use disorder, substance-related cues can grab the individual's attention (2). Previously theories such as classical conditioning or incentive-sensitisation theories, have provided explanations as to how these cognitive biases develop (2). More recently, the dual-process theory has posited that whilst the repeated usage of a substance leads to increased automatic processing and increased automatic tendencies to approach substance-specific cues, in addition, other normal cognitive processes are affected (3). The cognitive control process, which normally serves to inhibit this automatic behavior, is itself inhibited (3). This coupled with the increased dopamine in the cortico-striatal circuit, results in individuals having increased attention and automatic tendencies toward substances, precipitating a relapse. Cox et al. (4) highlighted the need for specific interventions to modify these automatic unconscious processes. Whilst the Stroop task has been routinely used for the assessment of cognitive biases, several other paradigms have been used to retrain attentional or approach tendencies, such as the visual probe or the approach/avoidance task (4, 5). The visual probe task, when used as a cognitive retraining intervention instead of an assessment intervention, involves pairing probes with a neutral stimulus 100% of the time, to retrain attentional biases away from substance cues (4). When the approach/avoidance task is used as a retraining tool, it involves the presentation of substance-related cues in the push-away format and neutral cues in a pull-closer format (5). To date, there has been some initial research conducted on substance use disorders, both in determining whether cognitive biases are present for specific addictive disorders and in the evaluation of the effectiveness of bias modification (6, 7).
Several reviews have examined the presence of cognitive biases in addictive disorders as well as the effectiveness of bias modification. Cristea et al. (1) undertook the first meta-analysis examining the effectiveness of bias modification for substance use disorders. Even though the authors included in their review search terminologies for a variety of addictive disorders, they only managed to identify and include studies that included participants with alcohol or tobacco use disorders. This review reported that bias modification for both cognitive biases was moderately effective, with an effect size of 0.60 (Hedge G) (1). Notably, the review found no association between the reduction in biases and other outcomes such as cravings. One of the major limitations of the review (1) was that it included participants who had either alcohol or tobacco disorders, with no studies being included that focused on other substances of abuse. High risk of biases was identified in the studies include, which might have affected the results synthesis. Whilst Cristea et al. (1) did not, in their meta-analytical review found any association between cravings and attentional biases, their findings are not unexpected. Field et al. (8) in their previous review sought to determine the relationship between cravings and attentional biases. From the 68 studies that they have included, they reported the presence of a weak relationship between attentional biases and cravings (r = 0.19). Field et al. (8) have reported there being a larger association between attentional biases and illicit substances and caffeine, as compared to alcohol and tobacco. Christiansen et al. (9) attempted in their review to determine if there was an association between cognitive biases and relapse, and their study included participants with alcohol, tobacco, cocaine, and cannabis disorders. It was reported in the review that the assessment of cognitive biases did not predict relapse and that attentional bias modification did not reduce the future risk of relapse. Whilst the review by Christiansen et al. (9) included participants with a range of addictive disorders, the time frame was not specified, nor the inclusion and the exclusion criteria used in the selection of the articles. In addition, the database search was limited to that of PubMed, Scopus, and prior published reviews. Hence, there is a possibility that other relevant citations were missed and reduced the quality of the evidence synthesis.
The fact that the reviews to date are limited to certain substance disorders matters. The recent report released by the United Nations Office on Drugs and Crime (UNDOC) stated that in 2015, 29.5 million individuals had a substance use disorder (10), with an estimated 28 million healthy years of life lost due to drug use (10). Substances like cannabis, opioids, amphetamines, and prescription opioids are widely abused. In 2015, it was estimated that there were 183 million cannabis users, 35 million opioid users, and 37 million amphetamine and prescription stimulant users (10). For the management of substance use disorders, there are limited pharmacological options. Symptomatic medications, such as benzodiazepines or antipsychotics, are routinely prescribed for patients to control acute intoxication symptoms following cannabis or stimulant use. There remain no medications that are approved to help individuals maintain abstinence following cannabis or stimulant use. Psychological interventions can help individuals maintain abstinence following a lapse or relapse (11). Psychological interventions routinely used include cognitive behavioral therapy, contingency management, and more recently mindfulness-based relapse prevention (11). A prior review provided evidence that cognitive behavioral therapy is effective for substance use disorders, with an effect size of 0.45 (Cohen D) (12). However, despite this effectiveness of cognitive behavioral therapy, 40–50% of individuals still relapse within a year of successful treatment and another 70% of individuals relapse within 3 years (13). The high relapse rate following a moderately successful intervention suggests that it has not adequately addressed all the issues leading to a lapse or relapse. Cognitive behavioral therapy mainly addresses the cognitive control issues and fails to address the unconscious processes responsible for relapse. Consequently, further studies have been conducted evaluating the effectiveness of cognitive bias modification for individuals with different types of substance use disorders.
Given the limitations of previous reviews and the recent review by (14), together with recent studies that have evaluated cognitive biases in substance disorders that are highly prevalent (opioid, cannabis, and stimulant use disorders), there is a need for a systematic review to synthesize the information from these studies. The primary aim of this review is to synthesize the evidence for cognitive biases in the following substance use disorders: opioid use, cannabis use, and stimulant use disorders. If biases are consistently present, this will help to guide future research involving bias modification. The secondary aim of the review is to determine if cognitive bias could be consistently detected using the different methods. Lastly, this review will narratively synthesize the evidence of possible associations between cognitive biases and other addiction-related outcomes.
Methods
A search was conducted, on the following databases (PubMed, MEDLINE, Embase, PsycINFO, Science Direct, and Scopus), from inception through to January 2018. The following search terminologies were used: (“attention bias” OR “approach bias” OR “avoidance bias” OR “cognitive bias”) AND (“addiction” OR “substance” OR “drug” OR “abuse” OR “dependence” OR “Opiates” OR “Heroin” OR “Cannabis” OR “Marijuana” OR “Stimulants” OR “Amphetamines” OR “Cocaine”).
Inclusion and Exclusion Criteria
Only articles that were written in English language were included. Articles were included if participants had a primary diagnosis of opioid use, cannabis use, or stimulant use disorder. Articles were excluded if participants had other psychiatric disorders as a primary disorder, or if the study involved a pharmacological intervention in which medications were used to examine their effects on cognitive biases. All types of study design were included.
Selection of Articles
Two authors (MZ and JY) independently selected the relevant articles. Articles were initially screened based on their titles and abstracts. Articles that were shortlisted were then further evaluated against the inclusion and exclusion criteria. If the reviewers disagreed, this was resolved through a discussion with another author (GS.). The selection of the articles for inclusion was in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Guidelines.
Statistical Analysis
The following data were systematically extracted from each of the identified articles and recorded on a standardized electronic data collation form: (a) authors and study year, (b) study design and methodology (study design, sample size, types of sample, country, demographics of sample, diagnosis of participants, methods in which diagnosis was established), (c) cognitive biases assessment and modification methods, (d) outcomes of interest (presence of attention or approach biases, effectiveness of biases modification, other secondary outcomes reported such as craving scores or addiction outcomes).
As the reported outcome measures were heterogeneous, a meta-analytical synthesis was not feasible. The secondary outcomes reported varied by the studies, and even if there were similar outcomes reported, very often, a quantitative approach (meta-analysis) was not feasible as no effect size or statistics were reported. Hence, a qualitative synthesis was undertaken instead. As both randomized and non-randomized studies were included, there remains no single risk of bias tool that could be applied across all the studies for quality assessment. Hence, quality assessment was not performed.
Results
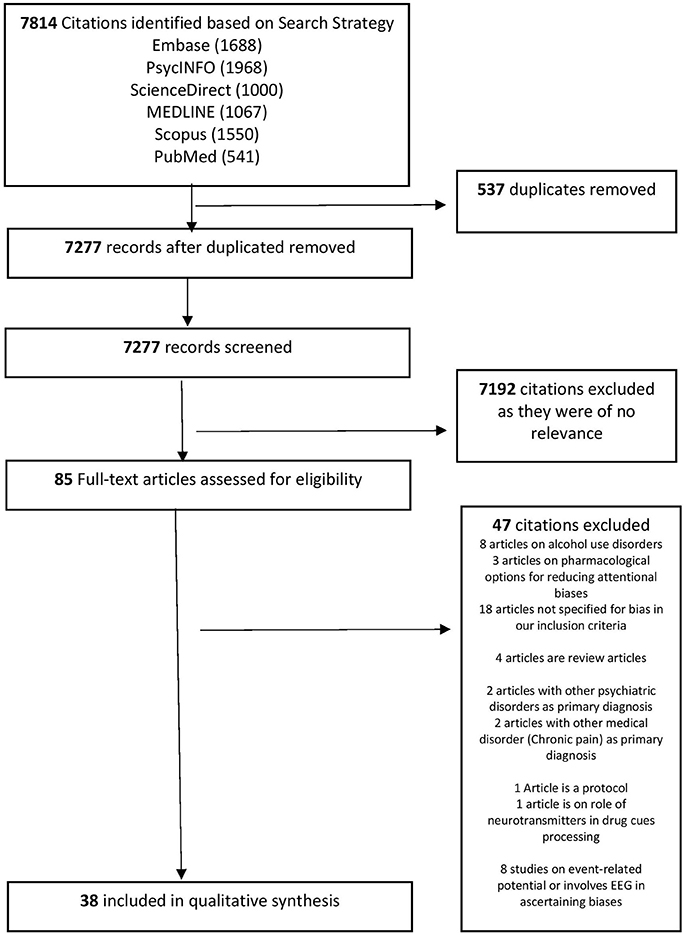
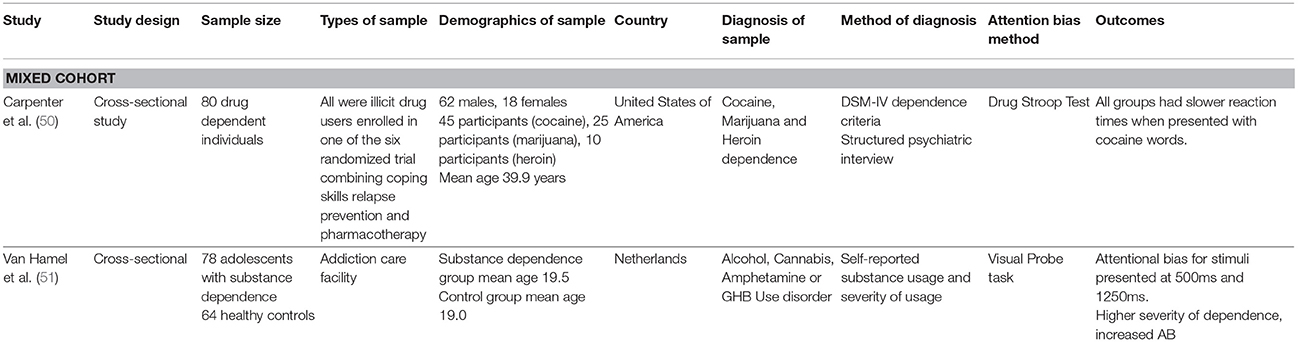
Based on our search strategy, a cumulative total of 7,814 citations were extracted from Embase, PsycINFO, Science Direct, Scopus, MEDLINE, and PubMed. Five hundred and thirty-seven duplicated articles were removed, leaving 7,277 citations. On further screening, 7,192 citations were removed as they were of not relevant. Eighty-five full-text articles were downloaded and evaluated against the inclusion and exclusion criteria. Forty-seven citations were excluded for reasons documented in Figure 1. Thirty-eight articles were selected for this qualitative synthesis. Figure 1 provides an overview of the selection process of the articles for the current review. Tables 1–4 provide an overview of the core characteristics of the included studies (n = 38).
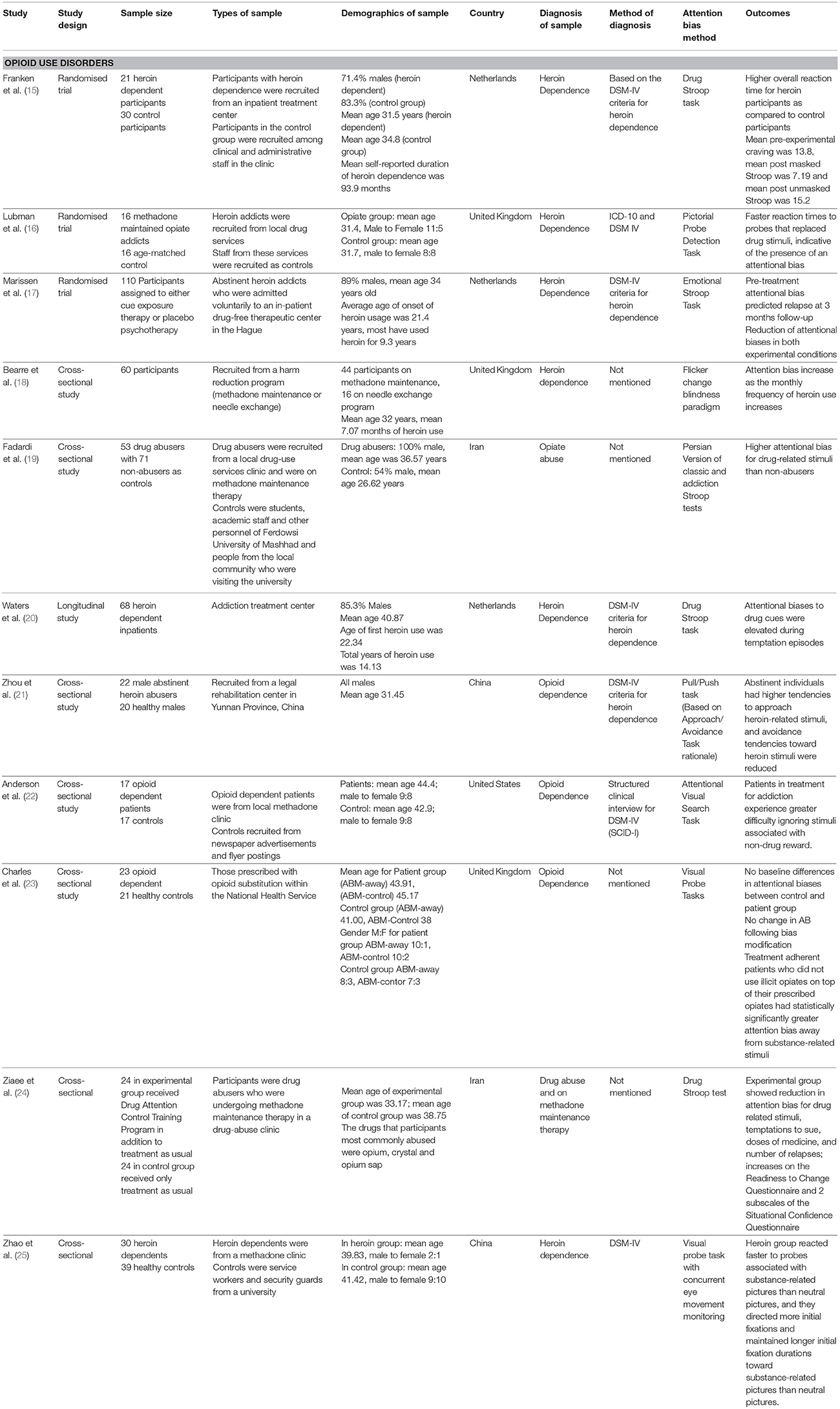
Eleven articles involved participants with opioid use disorder, 16 articles involved participants with cocaine use disorder, nine articles involved participants with cannabis use disorder, and two articles involved samples of participants with different disorders (i.e., drug-dependent participants with either cocaine, cannabis, or opiate dependence; or participants with alcohol, cannabis, amphetamine, or GHB use disorders). Out of the 11 articles involving participants with opioid use disorder, three were randomized trials, seven were cross-sectional studies and one was a longitudinal study. Out of the 16 articles involving participants with cocaine use disorder, three were randomized trials, 11 were cross-sectional studies, one a pilot study and one a case-controlled study. Out of the nine articles involving participants with cannabis use disorder, two were case-control studies and seven were cross-sectional studies.
Characteristics of 11 Studies for Opioid Use Disorders
Three studies [Franken et al. (15), Marissen et al. (17), and Zhou et al. (21)], recruited participants in an inpatient treatment facility. The remaining studies (n = 8) recruited participants who were outpatients or who had attended a harm reduction program. Six studies [Bearre et al. (18), Fadardi et al. (19), Anderson et al. (22), Charles et al. (23), Ziaee (24), and Zhao et al. (25)] included participants who were receiving methadone substitution-based treatment. Apart from the study by Ziaee et al. (24), which failed to provide information about the gender ratios of the recruited cohort of individuals, all studies had predominantly male participants, and the mean age was between 30 and 45 years. Most of the included studies were conducted in Europe (n = 6), with the remaining studies conducted in the United States (n = 1), Iran (n = 2), and China (n = 2). The diagnosis of opioid use disorders was ascertained by means of the Diagnostic and Statistical Manual (DSM) criteria for almost all of the studies. Only four studies [those of Bearre et al. (18), Fadardi et al. (19), Charles et al.(23), and Ziaee et al. (24)] failed to report how the diagnosis was ascertained. In the assessment of attention biases, the Stroop task was used in five studies; the visual probe task in two studies and the remaining studies used the visual probe task with concurrent eye tracking (n = 1), approach and avoidance task (n = 1), attentional visual search (n = 1), and flicker change blindness paradigm (n = 1).
Primary and Secondary Outcomes Reported in the 11 Studies for Opioid Use Disorders
Ten of the eleven reported the presence of biases in their sampled participants, except in Charles et al. (23) reported no baseline attentional differences between the healthy controls and opioid-dependent participants. Studies that assessed attention bias using the Stroop task reported an higher overall reaction time (15) among abusers, or enhanced attentional biases for drug-related stimuli especially among abusers (19) and that attentional biases to drug-related cues were heightened when abusers had temptation episodes (20). Studies that assessed attention bias using the visual probe task reported that the reaction time for abusers was faster when they had probes that replaced drug-related stimuli. The only study that paired the visual probe task with concurrent eye tracking (25) demonstrated that abusers not only have faster reaction time to drug-related probes, but also more initial fixations and maintained fixations on drug-related probes or images. For the approach and avoidance task, Zhou et al. (21) reported that former users of opioids have a greater tendency to approach heroin-related stimuli and a reduced tendency to avoid or push away these stimuli. The study using the flicker change blindness paradigm reported an association between the attention biases and the monthly frequency of heroin use. The study assessing attentional bias using attentional visual search showed that attention biases were present and that the presence of attentional biases would cause abusers to have heightened attention for other non-drug-related reward probes.
Four of the included studies reported other secondary outcomes following attention bias assessment and modification and provided evidence for the potential effectiveness of bias modification. Franken et al. (15) reported a reduction in the mean craving scores following masked Stroop intervention. The study by Ziaee et al. (24) found bias modification was associated with a reduction in several outcome parameters, including temptations to use, doses of medication, and number of relapses. Marissen et al. (17) reported findings similar to those of Ziaee et al. (24) concerning relapse, as Marissen et al. (17) found that baseline attentional biases could predict relapse at three months' follow-up. With regard to the effectiveness of the interventions, Marissen et al. (17) reported a reduction in attentional biases amongst individuals who received either cue exposure therapy or placebo psychotherapy. In contrast to the reductions in attentional biases were demonstrated by Marissen et al. (17) and Charles et al. (22) did not find any changes in attentional biases following their intervention.
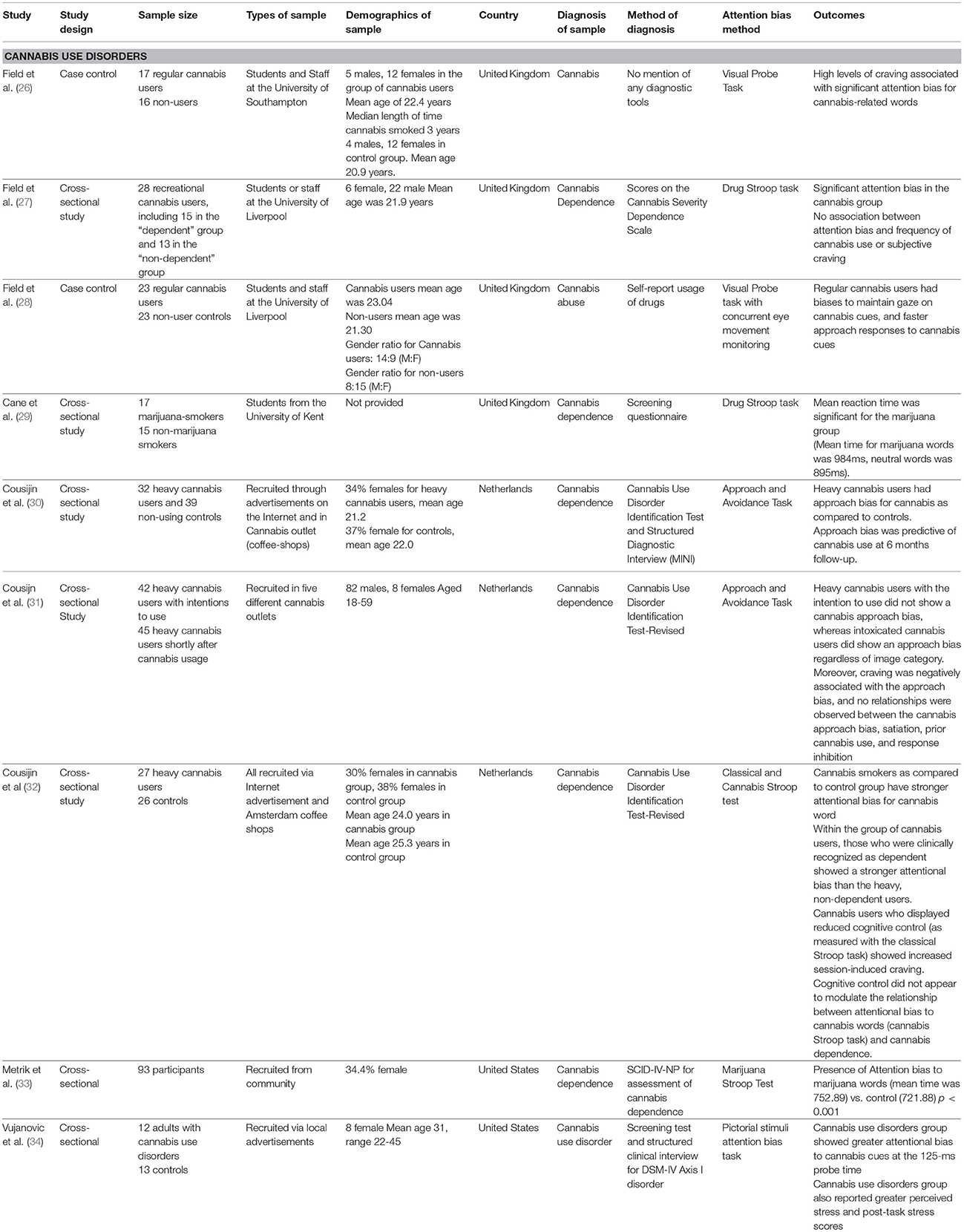
Characteristics of 9 Studies for Cannabis Use Disorders
Four studies [Field et al. (26–28) and Cane e al. (29)] recruited students; the remainder (n = 5) recruited through advertisements or from cannabis outlets. No study recruited participants who were part of inpatient treatment or rehabilitation facility. The majority of the sampled participants were males. The mean age in years across all of the studies ranged from 20 to the early 30s. Seven of the studies were conducted in Europe, and the remaining two studies were conducted in the United States. There was heterogeneity in the method of ascertaining the diagnosis, with one study Field et al. (28) basing their diagnosis on self-reported information, four studies [Field et al., (27), Cane et al., (29), and Cousijin et al. (31, 32)] on questionnaires, and the remainder (Cousijin et al. (30), Metrik et al. (33), and Vujanovic et al. (34)] on structured interviews. In the assessment of biases, the Stroop task was used in four of the studies, and the remainder of the studies used the visual probe task (n = 1), or the visual probe task with concurrent eye tracking (n = 1), or the pictorial attention bias task (n = 1), or the approach and avoidance task (n = 2).
Primary and Secondary Outcomes Reported in 9 Studies for Cannabis Use Disorders
All of the studies provided evidence for the presence of biases. For study that assessed attention bias using the Stroop task, it was reported that the mean reaction times for cannabis or marijuana stimuli were longer as compared to neutral stimuli (29). Stroop-based testing also helped in the differentiation of users who used varying amounts of cannabis (32), as it was reported that those who were clinically dependent had had a stronger attentional bias as compared to those who were non-dependent. The visual probe task and the visual probe task coupled with concurrent eye tracking provided both direct and indirect evidence of the presence of attention bias, as regular cannabis users exhibited biases in maintaining gaze on cannabis cues and increased reaction times for cannabis cues (28). Like that of the visual probe task, the pictorial stimuli attention bias task also reported the presence of attentional biases among cannabis users and these biases were most prominent when the probe was presented for 125 ms (which is shorter than the normal duration of 500 ms). For the studies that used the approach and avoidance task, one study reported the presence of an approach bias amongst heavy users (individuals who used cannabis on 10 or more days per month), whereas the other study did not report the presence of an approach bias in heavy users but found an approach bias for cannabis cues only amongst those users who were intoxicated at the time of testing.
There is mixed evidence for the association between attention bias and cravings. Field et al. (26) reported that the high levels of cravings were associated with attentional biases but in a later study, Field et al. (27) reported observing no association between attention biases and cravings. Cousijin et al. (31) also reported the lack of an association between approach biases and cravings. One study Cousijin et al. (30) reported approach bias to be a predictor of relapse.
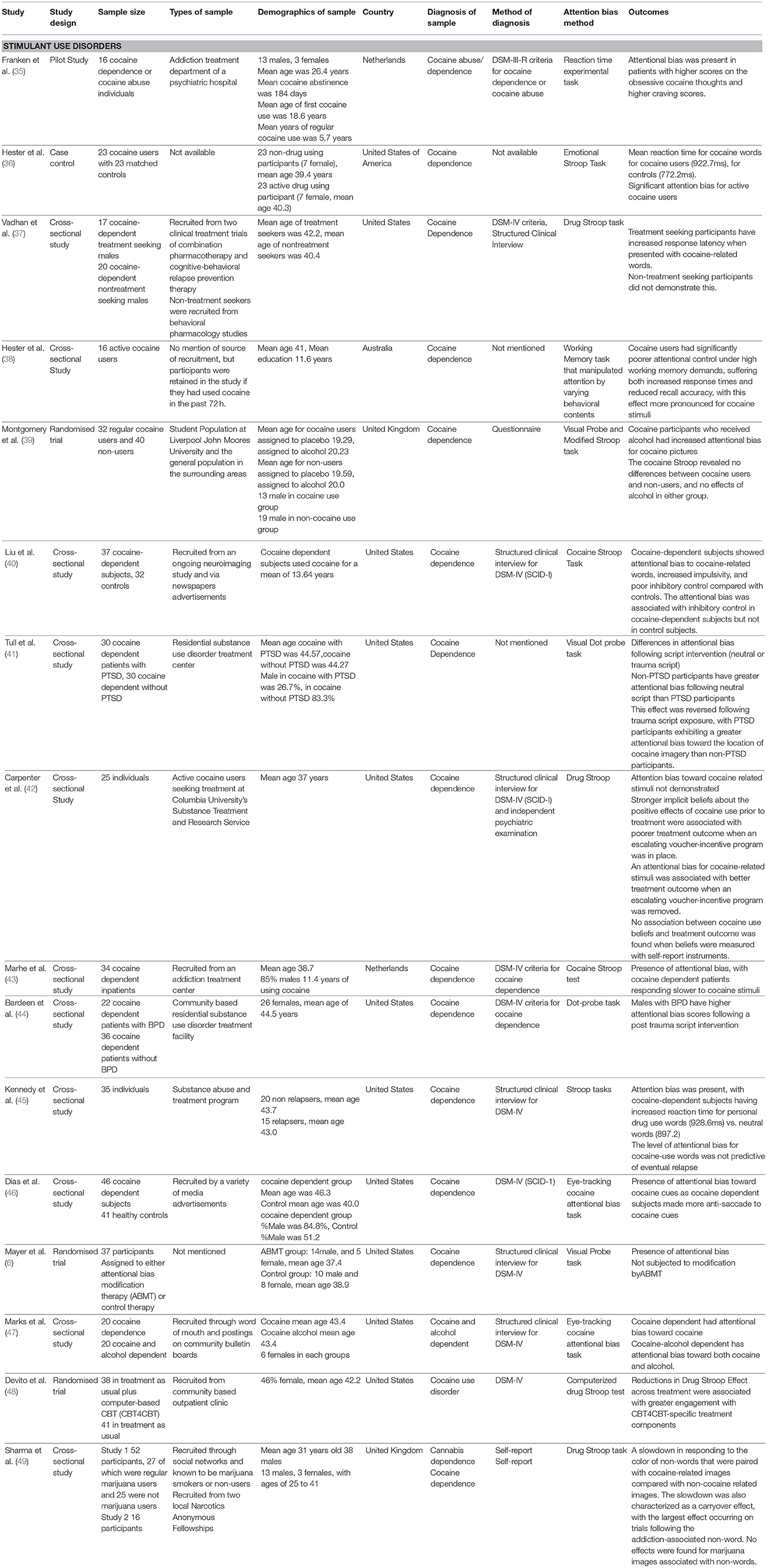
Characteristics of the 16 Studies for Stimulant Use Disorders
Eight studies [Franken et al. (35); Vadhan et al. (37), Tull et al. (41), Carpenter et al. (42), Marhe et al. (43), Bardeen et al. (44), Kennedy et al. (45), and Devito et al. (48)] recruited a clinical or treatment-seeking cohort of participants, one study Montgomery et al. (39) recruited a student sample, and five studies [Hester and Garavan (38); Liu et al. (40), Dias et al. (46), Marks et al. (47), and Sharma et al. (49)] recruited a cohort of participants from the community. There was a predominance of males in those samples that reported a gender ratio. The mean age across the studies varied within the range of 20–45 years, with a single study Montgomery et al. (39) including an adolescent cohort (mean age 19 years old). Twelve of the included studies were conducted in the United States, four studies in Europe, and one study in Australia. The diagnosis of stimulant use disorder, most studies (12 out of 17 studies) used the diagnostic criteria, two studies used a questionnaire or self-report, respectively, and the remainder of the studies did not provide any information as to how the diagnosis was ascertained. Eight studies utilized Stroop testing, one study used a reaction time experimental task, one study used a working memory task, four studies used the visual probe task, and two studies used the visual probe task with eye-tracking.
Primary and Secondary Outcomes Reported in Studies for Stimulant Use Disorders
All of the included studies reported the presence of biases except Carpenter et al. (42), which failed to demonstrate an attention bias in their sample of cocaine users. Two studies reported the severity of the underlying dependency to affect the resultant biases [Franken et al. (35) and Van Hamel et al. (51)]. Studies that assessed attention bias using the visual probe with eye-tracking to assess for attentional bias demonstrated that the cocaine-using cohort exhibited gaze preferences toward cocaine stimuli.
Concerning secondary outcomes, Franken et al. (35) reported that attentional bias was elevated in patients who had higher levels of cravings. Liu et al. (40) observed that attentional bias amongst cocaine users was associated with heightened impulsivity and poorer inhibitory control. Marks et al. (47) reported that there appears to be generalization of attentional bias for cocaine stimuli to that of alcohol stimuli. Mayer et al. (6) reported that there was no effectiveness of attention bias modification in reducing cocaine-related attentional biases.
Outcomes Reported in Studies With a Heterogeneous Sample
Two studies [Carpenter et al. (42) and Van Hamel et al. (51)] studied group with differing diagnosis. The studies included drug-dependent participants with either cocaine, cannabis or opiate dependence; or participants with alcohol, cannabis, amphetamines, or GHB use disorders. Both the Stroop test and the visual probe task were used in the assessment of attentional biases, and both trials demonstrated the presence of attentional biases.
Discussion
This is perhaps the first review that synthesizes the evidence of cognitive biases in opiate, cannabis and stimulant use disorders. The main finding is the evidence that cognitive biases are present in the 38 studies identified, except for a single study on opioid use and stimulant use disorders. There were differences in the participants recruited for each disorder, with opioid use disorder studies recruiting mainly treatment-seeking individuals, who were either abstinent or maintained on opiate substitution therapy. The bias assessment methods used included the Stroop task, visual probe, eye movement tracking, approach and avoidance task, attentional visual search, and flicker change blindness paradigm. The findings for the secondary outcomes were narratively reported, but not synthesized due to their high heterogeneity.
Our main finding is the evidence that cognitive biases are present in opiate use, cannabis use, and stimulant use disorders. This finding is novel as there have not been any prior reviews of cannabis use disorders. In their meta-analysis, Cristea et al. (1) attempted to search for randomized trials for these substance disorders, but eventually only included trials that evaluated participants with alcohol or tobacco use disorders. Given this, the paper by Eberl et al. (5) only provided evidence that cognitive biases were present and could be subjected to modification among participants with either alcohol or tobacco use disorders. A review by Christiansen et al. (9) included participants with opiate use disorders (17, 42, 43) and participants with cocaine use disorders (17, 42, 43, 45, 52). Whilst the work by Field and Cox (2) provided evidence for the presence of cognitive biases in opiate and cocaine use disorders, the evidence synthesis was from a limited number of studies, given that the primary objective of the review was to ascertain the association between cognitive bias and relapse. In their critical review, Leeman et al. (53) provided evidence for the presence of attentional biases in cocaine use disorders. This review was limited only to the assessment of cocaine studies as the authors reported that prior studies have reported that individuals with cocaine use disorders have particularly robust cognitive biases and that, given the lack of effective treatment approaches, novel approaches such as bias modification need to be considered (53). It is clear that the current review addressed several gaps in the prior reviews, by synthesizing the evidence for cognitive biases in three highly prevalent substance use disorders (opioid, cannabis, and stimulant use disorders) through evaluating studies with different study designs. None of the prior reviews synthesized evidence for the presence of attentional biases for individuals with cannabis use disorders. Evidence synthesis for this is of particular importance, given that cannabis use has been increasingly globally (34), and an estimated 10% of regular cannabis users do eventually develop dependence. Also, apart from the risk of developing an addictive disorder, cannabis use has been associated with heightened risk for the development of other psychiatric disorders, such as psychosis, cognitive impairment, and potentially also amotivational syndrome. Thus, the identification of the presence of cognitive bias in individuals with cannabis use disorders signifies that there remains a need for interventions to deal with these unconscious processes. Also, cognitive bias assessment could also help in the differentiation of individuals who are clinically dependent on cannabis and those who are using cannabis recreationally, as it has been demonstrated that individuals who are clinically dependent have stronger attentional biases. Whilst our synthesized results demonstrate the presence of cognitive biases in all three addictive disorders, it should be noted that there were two outlier studies (23, 42). One of the studies (23) attributed this finding to the fact that the presentation of the opioid-related stimuli might have appeared to be novel to the control sample.
Our synthesis of the published literature demonstrated the presence of biases in individuals who receive opiate substitution therapy (16). The presence of biases among individuals maintained on opiate substitution therapy implies that whilst pharmacological interventions might help in the stabilization of the lifestyle and minimisation of harms associated with illicit usage, it does not have any effect on factors that could still predispose individuals to a lapse or relapse (14). Drug-related stimuli have been proposed to be “cognitive intermediates” prior to a lapse or relapse, given that such salient stimuli activate unconscious processes, leading to one having increased attention, but also leaves the individual with fewer resources available to apply learned coping strategies. Hence, there is clearly a need for cognitive bias modification to be considered for individuals with addictive disorders. There has been increased recognition of this need, as evident by the protocol proposed by Heitman et al. (54), in which they attempt to investigate both the effectiveness and cost-effectiveness of an online Internet-based cognitive bias modification method that is delivered in addition to treatment as usual for individuals with alcohol or cannabis use disorders. Whilst there has been a prior study (55) that has evaluated combined cognitive bias modification and cognitive behavioral therapy, there remains, to our knowledge, no published studies or protocol for a similar study for substance use disorders. A consideration of the integration of both modalities of therapy is crucial, given that cognitive behavioral therapies typically target the top-down or reflective conscious decision-making processes, whilst bias modification could target the bottom-up or unconscious processes that are responsible for lapse and relapse occurrences.
The fact that cognitive biases could be detected by different tools negates the previous concerns raised about the reliability of the assessment tools. Biases were reported to be present despite there being a varied range of assessment tools that were utilized. The combination of indirect and direct measures used in the ascertainment of cognitive biases helped improve the evidence base, supporting the presence of these biases in all three disorders. Across all three disorders, a combination of both indirect and direct measures was used in the ascertainment of cognitive biases. Indirect measures, as aforementioned, refer to assessment tools such as the Stroop task or the visual probe task. In these indirect measures, participants are required to either name the color in which neutral and drug-related words are printed or respond to probes that replace either neutral or salient stimuli (53). Reaction time is measured and used as a surrogate in the determination of attentional biases. Direct measures provide better evidence of cognitive biases, given that eye movements in response to neutral or drug cures are used in the ascertainment of cognitive biases (12). Ataya et al. (56) previously investigated the internal reliability of the Stroop task and the visual probe task in the assessment of attention biases and reported that the modified Stroop task was more reliable as compared to the visual probe task, as it is a simpler task and is less likely to influence the reaction time that is being measured. Field and Christiansen (57) reported that the eye-movement measurement of cognitive bias does help to further mitigate against the concerns about reliability. Given that a variety of conventional indirect measures and direct measures were used for all the different disorders, we believe that this helps to better the quality of our synthesized evidence of the presence of cognitive biases in these disorders.
Notably, there was a single study Montgomery et al. (39) that has utilized different methods of cognitive bias assessment in the same group of participants. Interestingly, the authors reported that there was an increase in attentional biases following the administration of the visual probe task. However, participants' response did not differ when the modified Stroop task was used. Montgomery et al. (39) explained the differences in their results by highlighting that the visual-probe task might be better in measuring visuospatial attention. The Stroop task might not be as sensitive in the measurement of visuospatial attention but is better in assessing for response inhibition and other cognitive processes. Whilst we have previously discussed the advantages of having both direct and indirect measures in the assessment of biases, the results arising from Montgomery et al. 's (39) study has other implications if only indirect measures are to be used. This might be in the context of web or mobile-delivery of cognitive bias modification intervention. As such, it is of importance for researchers to carefully consider which assessment tool might be most appropriate, depending on the stimulus that they present to participants, given that the visual probe task is better able to measure visuospatial attention, and the Stroop task better for response inhibition. Also, while the Stroop task has been found to be more reliable, the results arising from Montgomery et al.'s (39) study also highlights the need for researchers to consider other aspects of the intervention, that might affect whether the task is capable of detecting biases.
This review has several strengths. A comprehensive search through the literature identified studies for the highly prevalent addictive disorders. No other reviews have synthesized the existing evidence for biases and cannabis use disorders. There are however limitations. The inclusion of a mixture of study designs, including both randomized and non-randomized studies affects the quality of the evidence, given that non-randomized studies have the risk of confounding and other biases. We were unable to perform a risk of bias assessment, due to the diversity of study designs and there remains no single tool that could assess risk of bias across different study designs. Whilst we search for studies involving participants with stimulant use disorders, the studies included involved participants who were primarily using cocaine. It will be beneficial if studies involving participants who were using amphetamines be conducted and incorporate into future synthesis, particularly as there is an increasing global trend of amphetamine abuse and dependence. We are also limited to a qualitative synthesis of the data extracted from each of the studies pertaining to attentional biases. Most of the studies included focus on the assessment of attentional biases in substance-using individuals, so evidence synthesis for the effectiveness of attentional or approach bias modification could not be undertaken. Secondary outcome measures had great heterogeneity, so we were unable to identify a common dataset for the synthesis.
Conclusions
Cognitive biases have been consistently observed in opioid use, cannabis use, and stimulant use disorders, despite a range of assessment tools being utilized in the assessment for these biases. The presence of attentional and approach bias signifies the importance of bias modification interventions. There remains a need for future research to explore the presence of attentional biases in other stimulant use disorders, such as amphetamine use disorders. It is also of importance for future research to evaluate the efficacy of bias modification for these highly prevalent disorders and to determine if reduction of these biases is associated with improvements in other addiction outcomes.
Data Availability
All available data have been included in the manuscript.
Author Contributions
MZ, DF, and HS conceptualized and planned the current review. MZ and JY were involved in the literature search, extraction, and selection of the articles for inclusion in the current review. MZ wrote the initial draft of the manuscript and TW helped in the amendments of the initial draft. All authors were involved in the subsequent revisions and preparations of the manuscript prior to submission.
Funding
MZ is supported by a grant under the Singapore Ministry of Health's National Medical Research Council (Grant number NMRC/Fellowship/0048/2017) for Ph.D. training. The funding source was not involved in any part of this project.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Cristea IA, Kok RN, Cuijpers P. The effectiveness of cognitive bias modification interventions for substance addictions: a meta-analysis. PLoS ONE (2016) 11:e0162226. doi: 10.1371/journal.pone.0162226
2. Field M, Cox WM. Attentional bias in addictive behaviors: a review of its development, causes, and consequences. Drug Alcohol Depend. (2008) 97:1–20. doi: 10.1016/j.drugalcdep.2008.03.030
3. Field M, Marhe R, Franken IH. The clinical relevance of attentional bias in substance use disorders. CNS Spectr. (2014) 19:225–30. doi: 10.1017/S1092852913000321
4. Cox WM, Fadardi JS, Intriligator JM, Klinger E. Attentional bias modification for addictive behaviors: clinical implications. CNS Spectr. (2014) 19:215–24. doi: 10.1017/S1092852914000091
5. Eberl C, Wiers RW, Pawelczack S, Rinck M, Becker ES, Lindenmeyer J. Implementation of approach bias re-training in alcoholism-how many sessions are needed? Alcohol Clin Exp Res. (2014) 38:587–94. doi: 10.1111/acer.12281
6. Mayer AR, Wilcox CE, Dodd AB, Klimaj SD, Dekonenko CJ, Claus ED, et al. The efficacy of attention bias modification therapy in cocaine use disorders. Am J Drug Alcohol Abuse (2016) 42:459–68. doi: 10.3109/00952990.2016.1151523
7. Wiers CE, Ludwig VU, Gladwin TE, Park SQ, Heinz A, Wiers RW, et al. Effects of cognitive bias modification training on neural signatures of alcohol approach tendencies in male alcohol-dependent patients. Addict Biol. (2015) 20:990–9. doi: 10.1111/adb.12221
8. Field M, Munafo MR, Franken IH. A meta-analytic investigation of the relationship between attentional bias and subjective craving in substance abuse. Psycho Bull. (2009) 135:589–607. doi: 10.1037/a0015843
9. Christiansen P, Schoenmakers TM, Field M. Less than meets the eye: reappraising the clinical relevance of attentional bias in addiction. Addict Behav. (2015) 44:43–50. doi: 10.1016/j.addbeh.2014.10.005
10. United Nations Office on Drugs and Crime. Exexcutive Summary: Conclusions and Policy Implications. Available online at: https://www.unodc.org/unodc/en/scientists/world-drug-report-2017—executive-summary-conclusions-and-policy-implications.html (Accessed April 12th 2018).
11. European Monitoring Centre for Drugs and Drug Addiction. Perspectives on Drugs: The Role of Psychosocial Interventions in Drug Treatment. Available online at: http://www.emcdda.europa.eu/publications/topics/pods/psychosocial-interventions_en (Accessed April 12th 2018).
12. McHugh RK, Hearon BA, Otto MW. Cognitive behavioral therapy for substance use disorders. Psychiatr Clin North Am. (2010) 33:511–25. doi: 10.1016/j.psc.2010.04.012
13. Cutler RB, Fishbain DA. Are alcoholism treatments effective? The project MATCH data. BMC Public Health (2005) 5:75. doi: 10.1186/1471-2458-5-75
14. Zhang M, Ying J, Wing T, Song G, Fung DSS, Smith H. A systematic review of attention biases in opioid, cannabis, stimulant use disorders. Int J Environ Res Public Health. (2018) 15.
15. Franken IH, Kroon LY, Wiers RW, Jansen A. Selective cognitive processing of drug cues in heroin dependence. J Psychopharmacol. (2000) 14:395–400. doi: 10.1177/026988110001400408
16. Lubman DI, Peters LA, Mogg K, Bradley BP, Deakin JF. Attentional bias for drug cues in opiate dependence. Psychol Med. (2000) 30:169–75. doi: 10.1017/S0033291799001269
17. Marissen MA, Franken IH, Waters AJ, Blanken P, van den Brink W, Hendriks VM. Attentional bias predicts heroin relapse following treatment. Addiction (2006) 101:1306–12. doi: 10.1111/j.1360-0443.2006.01498.x
18. Bearre L, Sturt P, Bruce G, Jones BT. Heroin-related attentional bias and monthly frequency of heroin use are positively associated in attenders of a harm reduction service. Addict Behav. (2007) 32:784–92. doi: 10.1016/j.addbeh.2006.06.019
19. Fadardi JS, Ziaee SS. A comparative study of drug-related attentional bias: evidence from Iran. Exp Clin Psychopharmacol. (2010) 18:539–45. doi: 10.1037/a0021559
20. Waters AJ, Marhe R, Franken IH. Attentional bias to drug cues is elevated before and during temptations to use heroin and cocaine. Psychopharmacology (2012) 219:909–21. doi: 10.1007/s00213-011-2424-z
21. Zhou Y, Li X, Zhang M, Zhang F, Zhu C, Shen M. Behavioural approach tendencies to heroin-related stimuli in abstinent heroin abusers. Psychopharmacology (2012) 221:171–6. doi: 10.1007/s00213-011-2557-0
22. Anderson BA, Faulkner ML, Rilee JJ, Yantis S, Marvel CL. Attentional bias for nondrug reward is magnified in addiction. Exp Clin Psychopharmacol. (2013) 21:499–506. doi: 10.1037/a0034575
23. Charles M, Wellington CE, Mokrysz C, Freeman TP, O'Ryan D, Curran HV. Attentional bias and treatment adherence in substitute-prescribed opiate users. Addict Behav. (2015) 46:100–5. doi: 10.1016/j.addbeh.2015.03.017
24. Ziaee SS, Fadardi JS, Cox WM, Yazdi SA. Effects of attention control training on drug abusers' attentional bias and treatment outcome. J Consult Clin Psychol. (2016) 84:861–73. doi: 10.1037/a0040290
25. Zhao H, Yang B, Zhu Q, Zhang G, Xiao Y, Guo X, et al. Eye movement evidence of attentional bias for substance-related cues in heroin dependents on methadone maintenance therapy. Subst Use Misuse (2017) 52:527–34. doi: 10.1080/10826084.2016.1264967
26. Field M, Mogg K, Bradley BP. Cognitive bias and drug craving in recreational cannabis users. Drug Alcohol Depend. (2004) 74:105–11. doi: 10.1016/j.drugalcdep.2003.12.005
27. Field M. Cannabis ‘dependence’ and attentional bias for cannabis-related words. Behav Pharmacol. (2005) 16:473–6. doi: 10.1097/00008877-200509000-00021
28. Field M, Eastwood B, Bradley BP, Mogg K. Selective processing of cannabis cues in regular cannabis users. Drug Alcohol Depend. (2006) 85:75–82. doi: 10.1016/j.drugalcdep.2006.03.018
29. Cane JE, Sharma D, Albery IP. The addiction Stroop task: examining the fast and slow effects of smoking and marijuana-related cues. J Psychopharmacol. (2009) 23:510–9. doi: 10.1177/0269881108091253
30. Cousijn J, Goudriaan AE, Wiers RW. Reaching out towards cannabis: approach-bias in heavy cannabis users predicts changes in cannabis use. Addiction (2011) 106:1667–74. doi: 10.1111/j.1360-0443.2011.03475.x
31. Cousijn J, Snoek RW, Wiers RW. Cannabis intoxication inhibits avoidance action tendencies: a field study in the Amsterdam coffee shops. Psychopharmacology (2013) 229:167–76. doi: 10.1007/s00213-013-3097-6
32. Cousijn J, Watson P, Koenders L, Vingerhoets WA, Goudriaan AE, Wiers RW. Cannabis dependence, cognitive control and attentional bias for cannabis words. Addict Behav. (2013) 38:2825–32. doi: 10.1016/j.addbeh.2013.08.011
33. Metrik J, Aston ER, Kahler CW, Rohsenow DJ, McGeary JE, Knopik VS, et al. Cue-elicited increases in incentive salience for marijuana: craving, demand, and attentional bias. Drug Alcohol Depend. (2016) 167:82–8. doi: 10.1016/j.drugalcdep.2016.07.027
34. Vujanovic AA, Wardle MC, Liu S, Dias NR, Lane SD. Attentional bias in adults with cannabis use disorders. J Addict Dis. (2016) 35:144–53. doi: 10.1080/10550887.2015.1116354
35. Franken IH, Kroon LY, Hendriks VM. Influence of individual differences in craving and obsessive cocaine thoughts on attentional processes in cocaine abuse patients. Addict Behav. (2000) 25:99–102. doi: 10.1016/S0306-4603(98)00112-9
36. Hester R, Dixon V, Garavan H. A consistent attentional bias for drug-related material in active cocaine users across word and picture versions of the emotional Stroop task. Drug Alcohol Depend. (2006) 81:251–7. doi: 10.1016/j.drugalcdep.2005.07.002
37. Vadhan NP, Carpenter KM, Copersino ML, Hart CL, Foltin RW, Nunes EV. Attentional bias towards cocaine-related stimuli: relationship to treatment-seeking for cocaine dependence. Am J Drug Alcohol Abuse (2007) 33:727–36. doi: 10.1080/00952990701523722
38. Hester R, Garavan H. Neural mechanisms underlying drug-related cue distraction in active cocaine users. Pharmacol Biochem Behav. (2009) 93:270–7. doi: 10.1016/j.pbb.2008.12.009
39. Montgomery C, Field M, Atkinson AM, Cole JC, Goudie AJ, Sumnall HR. Effects of alcohol preload on attentional bias towards cocaine-related cues. Psychopharmacology (2010) 210:365–75. doi: 10.1007/s00213-010-1830-y
40. Liu S, Lane SD, Schmitz JM, Waters AJ, Cunningham KA, Moeller FG. Relationship between attentional bias to cocaine-related stimuli and impulsivity in cocaine-dependent subjects. Am J Drug Alcohol Abuse (2011) 37:117–22. doi: 10.3109/00952990.2010.543204
41. Tull MT, McDermott MJ, Gratz KL, Coffey SF, Lejuez CW. Cocaine-related attentional bias following trauma cue exposure among cocaine dependent in-patients with and without post-traumatic stress disorder. Addiction (2011) 106:1810–8. doi: 10.1111/j.1360-0443.2011.03508.x
42. Carpenter KM, Martinez D, Vadhan NP, Barnes-Holmes D, Nunes EV. Measures of attentional bias and relational responding are associated with behavioral treatment outcome for cocaine dependence. Am J Drug Alcohol Abuse (2012) 38:146–54. doi: 10.3109/00952990.2011.643986
43. Marhe R, Luijten M, van de Wetering BJ, Smits M, Franken IH. Individual differences in anterior cingulate activation associated with attentional bias predict cocaine use after treatment. Neuropsychopharmacology (2013) 38:1085–93. doi: 10.1038/npp.2013.7
44. Bardeen JR, Dixon-Gordon KL, Tull MT, Lyons JA, Gratz KL. An investigation of the relationship between borderline personality disorder and cocaine-related attentional bias following trauma cue exposure: the moderating role of gender. Compr Psychiatry (2014) 55:113–22. doi: 10.1016/j.comppsych.2013.08.011
45. Kennedy AP, Gross RE, Ely T, Drexler KP, Kilts CD. Clinical correlates of attentional bias to drug cues associated with cocaine dependence. Am J Addict. (2014) 23:478–84. doi: 10.1111/j.1521-0391.2014.12134.x
46. Dias NR, Schmitz JM, Rathnayaka N, Red SD, Sereno AB, Moeller FG, et al. Anti-saccade error rates as a measure of attentional bias in cocaine dependent subjects. Behav Brain Res. (2015) 292:493–9. doi: 10.1016/j.bbr.2015.07.006
47. Marks KR, Pike E, Stoops WW, Rush CR. Alcohol administration increases cocaine craving but not cocaine cue attentional bias. Alcohol Clin Exp Res. (2015) 39:1823–31. doi: 10.1111/acer.12824
48. DeVito EE, Kiluk BD, Nich C, Mouratidis M, Carroll KM. Drug stroop: mechanisms of response to computerized cognitive behavioral therapy for cocaine dependence in a randomized clinical trial. Drug Alcohol Depend. (2017) 183:162–8. doi: 10.1016/j.drugalcdep.2017.10.022
49. Sharma D, Money S. Carryover effects to addiction-associated stimuli in a group of marijuana and cocaine users. J Psychopharmacol. (2010) 24:1309–16. doi: 10.1177/0269881109350079
50. Carpenter KM, Schreiber E, Church S, McDowell D. Drug Stroop performance: relationships with primary substance of use and treatment outcome in a drug-dependent outpatient sample. Addict Behav. (2006) 31:174–81.
51. van Hemel-Ruiter ME, Wiers RW, Brook FG, de Jong PJ. Attentional bias and executive control in treatment-seeking substance-dependent adolescents: a cross-sectional and follow-up study. Drug Alcohol Depend. (2016) 159:133–41. doi: 10.1016/j.drugalcdep.2015.12.005
52. Mitchell MR, Balodis IM, Devito EE, Lacadie CM, Yeston J, Scheinost D, et al. A preliminary investigation ofStroop-related intrinsic connectivity in cocaine dependence: Associations with treatment outcomes Am J Drug Alcohol Abuse. (2013) 39:392–402.
53. Leeman RF, Robinson CD, Waters AJ, Sofuoglu M. A critical review of the literature on attentional bias in cocaine use disorder and suggestions for future research. Exp Clin Psychopharmacol. (2014) 22:469–83. doi: 10.1037/a0037806
54. Heitmann J, van Hemel-Ruiter ME, Vermeulen KM, Ostafin BD, MacLeod C, Wiers RW, et al. Internet-based attentional bias modification training as add-on to regular treatment in alcohol and cannabis dependent outpatients: a study protocol of a randomized control trial. BMC Psychiatry (2017) 17:193. doi: 10.1186/s12888-017-1359-2
55. de Hullu E, Sportel BE, Nauta MH, de Jong PJ. Cognitive bias modification and CBT as early interventions for adolescent social and test anxiety: two-year follow-up of a randomized controlled trial. J Behav Ther Exp Psychiatry (2017) 55:81–9. doi: 10.1016/j.jbtep.2016.11.011
56. Ataya AF, Adams S, Mullings E, Cooper RM, Attwood AS, Munafo MR. Internal reliability of measures of substance-related cognitive bias. Drug Alcohol Depend. (2012) 121:148–51. doi: 10.1016/j.drugalcdep.2011.08.023
Keywords: attention bias, approach bias, cognitive bias, substance use, addiction
Citation: Zhang MWB, Ying J, Wing T, Song G, Fung DSS and Smith HE (2018) Cognitive Biases in Cannabis, Opioid, and Stimulant Disorders: A Systematic Review. Front. Psychiatry 9:376. doi: 10.3389/fpsyt.2018.00376
Received: 13 April 2018; Accepted: 26 July 2018;
Published: 15 August 2018.
Edited by:
Alain Dervaux, Centre Hospitalier Universitaire (CHU) de Amiens, FranceReviewed by:
Domenico De Berardis, Azienda Usl Teramo, ItalyRobert F. Leeman, University of Florida, United States
Copyright © 2018 Zhang, Ying, Wing, Song, Fung and Smith. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Melvyn W. B. Zhang, bWVsdnluX3diX3poYW5nQGltaC5jb20uc2c=
 Melvyn W. B. Zhang
Melvyn W. B. Zhang Jiangbo Ying3
Jiangbo Ying3 Helen E. Smith
Helen E. Smith