- 1Key Laboratory of Mental Health, Ministry of Health (Peking University), National Clinical Research Center for Mental Disorders (Peking University Sixth Hospital), Peking University Sixth Hospital and Peking University Institute of Mental Health, Beijing, China
- 2Beijing Hui-Long-Guan Hospital, Peking University, Beijing, China
- 3Mood Disorders Center, Beijing Anding Hospital, Capital Medical University, Beijing, China
- 4Division of Mood Disorders, Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 5Shanghai Tongji Hospital, Tongji University Medical School, Shanghai, China
- 6Division of Mood Disorders, Shenzhen Mental Health Centre, Shenzhen, China
- 7The First Hospital of Harbin Medical University, Harbin, China
- 8Hangzhou Seventh People's Hospital, Hangzhou, China
- 9West China Hospital, Sichuan University, Chengdu, China
- 10The Affiliated Brain Hospital, Nanjing Medical University, Nanjing, China
- 11Mental Health Institute, The Second Xiangya Hospital, Central South University, Changsha, China
- 12The Second Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, China
- 13The Third Affiliated Hospital of Sun Yat-Sen University, Guangzhou, China
Objective: To analyze the factors associated with recent suicide attempts including socio-demographic and clinical characteristics in major depressive disorder (MDD) patients in China.
Methods: The data were from a nationwide sample from 13 major psychiatric hospitals or the psychiatric units of general hospitals in China, from September 1, 2010 to February 28, 2011. Melancholic features and suicide attempts in the past month were defined according to the melancholic feature module and the suicide module of the Mini International Neuropsychiatric Interview (MINI). Socio-demographic and clinical characteristics were compared between MDD patients with and without recent suicide attempts. Further analyses regarding the factors associated with recent suicide attempts in MDD patients were performed via multivariate logistic regression analysis.
Results: Among 1,172 MDD patients, 57 (4.9%) were reported to have made a suicide attempt in the past month. Compared to the MDD patients without recent suicide attempt, significantly higher percentage of patients in the recent suicide attempters group had previous suicide attempts (χ2 = 171.861, p < 0.001) and depressive episodes with melancholic features (χ2 = 22.837, p < 0.001). Logistic regression analysis indicated that previous suicide attempts (OR = 20.81, 95% CI: 11.12–38.94, p < 0.001) and depressive episodes with melancholic features (OR = 4.43, 95% CI: 2.09–9.43, p < 0.001) were independently associated with recent suicide attempts in MDD patients.
Limitations: Cross-sectional design, retrospective recall of suicide attempt data.
Conclusion: Recent suicide attempts are associated with melancholic features and previous suicide attempts in MDD patients in China. These data may help clinicians to identify MDD patients at high risk of suicide attempt behavior.
Introduction
Suicide is a serious public health problem that has received increasing attention worldwide (1, 2). According to a WHO report, an estimated 7,88,000 people died from suicide in the year 2015 globally, and the age-standardized suicide rate was 10.7 per 1,00,000 persons (3). In China, the suicide rate was 8.5 per 1,00,000 persons (3).
A national case-control psychological autopsy study conducted in China showed that mental disorders are present in up to 63% of people who died by suicide (4). The most common mental illness among the individuals who died by suicide was major depressive disorder (MDD) (4). A Swedish epidemiological study showed that depression is associated with a 20-fold increased risk of suicide (5). There is compelling evidence, however, that adequate prevention and management of suicidal behavior among MDD patients is beneficial to reduce suicide rates (6). A previous suicide attempt is the strongest risk factor for subsequent suicide attempt and death (7–9). Identifying the factors associated with suicide attempts is important for early identification efforts and can lead to reduction in the incidence of suicide.
Previous studies in Western countries reported risk factors for suicide attempts in MDD patients. They include family history of psychiatric disorders (10), adverse life events such as unemployment and divorce (11), comorbidity with anxiety disorders (12), early age at onset (13, 14), more frequent depressive episodes (14) and higher number of admissions (14). Because of different socio-cultural and economic contexts between the Western countries and China, these findings may not necessarily apply to the Chinese population (15).
There has been limited study of the risk factors for attempted suicide in MDD patients in China. A case-control study of 215 suicide attempters with MDD showed that hopelessness, negative life-events and family history of suicide were risk factors for attempted suicide (16). The small sample size and single study site limit the generalizability of the findings. Another study of 6,008 Han Chinese women diagnosed with recurrent MDD showed that more depressive symptoms, stressful life events, positive family history of MDD, a greater number of episodes, significant melancholic symptoms, and earlier age of onset were risk factors for suicide (17). However, this study was limited to female MDD patients, so it does not necessarily pertain to both genders.
The Diagnostic Assessment Service for People with Bipolar Disorder in China (DASP) is the first nationwide, multicenter and large sample study conducted in patients with major affective disorders in China. A previous study using this data analyzed factors associated with suicide risk in MDD patients including social-demographic and clinical features (18). The following risk factors were identified: male gender, unemployment, more frequent depressive episodes, depressive episodes with suicidal ideation, and attempts, depressive episodes with psychotic symptoms, and no current antidepressant use. Previous suicide attempts has been identified as one of the best predictor of eventual suicide death (19). A 5-year follow-up study showed that 16–34% of subjects attempted suicide again within 1 or 2 years after their first attempt (20). In order to find risk factors associated with recent a suicide attempt, therefore, we re-analyzed the data of the DASP project. The goal was to see if we could identify a group of patients with high risk of suicide attempt behaviors for whom it would be appropriate to provide more aggressive clinical management and effective suicide prevention measures.
Methods
Study Participants and Settings
The data were obtained from DASP (21–23), which was initiated by the Chinese Society of Psychiatry and conducted in 13 major psychiatric hospitals or the psychiatric units of general hospitals from September 1, 2010 to February 28, 2011. In- and outpatients who received treatment and met the following criteria were enrolled: (i) aged 16–65 years old; (ii) DSM-IV or ICD-10 diagnosis of MDD based on a review of medical records; (iii) understood the purpose of the study and provided written informed consent. Exclusion criteria were as follows: (i) a history of or ongoing severe somatic diseases, such as severe cardio-cerebral vascular diseases, respiratory diseases, liver diseases, kidney diseases, or malignant tumors; (ii) depressive disorders secondary to a general medical or neurological condition; (iii) a previous diagnosis of bipolar disorder; (iv) treatment with electroconvulsive therapy in the past month. The study protocol was approved by the Ethics Committees of all participating centers.
Instrument and Assessment Procedures
Patients with MDD who were receiving treatment in the participating hospitals/units were consecutively referred by their treating psychiatrists to the research team to be screened for eligibility. Patients fulfilling the study entry criteria were invited to participate in the study (22). The patients' basic socio-demographic and clinical characteristics were collected with a questionnaire designed for the study. The items of questionnaire included gender, marital status, employment status, education level, frequent depressive episodes, symptom characteristics of depressive episodes, major depressive episodes following obvious causes (such as postpartum); seasonal depressive episodes; family history of psychiatric disorders; age, age at onset, number of lifetime depressive episodes, number of admissions, receiving antidepressants treatment and other medicines. Frequent depressive episodes were defined as more than 4 depressive episodes in the previous year (24). Assessment of symptom characteristics of depressive episodes including atypical depressive features (increased appetite, increased sleep, and weight gain), psychotic symptoms, anxiety symptoms, or disorder and seasonal depressive episodes was completed by a clinical interview and was supplemented by a review of patients' medical records.
Prior to the study, all 13 raters (qualified psychiatrists) of research team were trained in the use of the Chinese version of the Mini International Neuropsychiatric Interview (MINI), Version 5.0 (25, 26) in 20 patients treated for MDD. The kappa values were greater than 0.85. After providing written consent following a full explanation about the study, patients met a rater for a confirmatory diagnostic interview of MDD based on DSM-IV criteria using the MINI supplemented by a review of medical records and, whenever possible, an interview of relatives.
Recent Suicide Attempts and Previous Suicide Attempts
Recent suicide attempts were assessed by one of the questions in the suicidal module of MINI (21). “Did you attempt suicide within the past month?” If the question was answered “yes,” the patient was classified as a recent suicide attempter. Previous suicide attempts were also assessed by one of the questions in MINI (21). “In your lifetime (the past month was not included), did you ever make a suicide attempt? The responses of patients were recorded.
Melancholic Features
Melancholic features were defined using the melancholic features module of MINI, which is in accordance with the DSM-IV criteria (27). The criteria include loss of pleasure in all, or almost all activities and/or lack of reactivity to usually pleasurable stimuli, plus three (or more) features of the following: distinct quality of depressed mood, depression regularly worse in the morning, early morning awakening (at least 2 h before usual awakening), marked psychomotor retardation or agitation, significant anorexia or weight loss, and excessive or inappropriate guilt.
Statistical Analysis
The data were analyzed using SPSS, version 20.0 (SPSS Inc., Chicago, IL, USA). Group differences between the recent suicide attempters and a non-suicide attempters control group were measured using independent-sample t-tests or Mann-Whitney U-tests for continuous data and chi-square tests for categorical data. Multiple logistic regression analysis was performed to identify the factors associated with recent suicide attempt in MDD patients. The variables with a univariate p-value < 0.05 and possible clinical variables related to suicide such as age, gender, depressive episodes with psychotic symptoms, and depressive episodes with anxiety symptoms or disorder were included in the multiple logistic regression analysis. The level of significance was set at 0.05 (two-tailed).
Results
Patients
The total number of screened patients was 1,757. Of these patients, 270 patients refused or failed to complete the interview, 306 patients were excluded because of meeting DSM-IV criteria for bipolar disorder based on the MINI, and 9 patients were lacking information on the suicidal module of the MINI. Ultimately, 1,172 patients were included in the present study, and 57 (4.9%) of the subjects had a suicide attempt during the past month.
Basic Socio-Demographic and Clinical Features
Table 1 shows the comparison of the socio-demographic and clinical characteristics between recent suicide attempters and the non-suicide attempters group. Compared to the MDD patients without recent suicide attempt, significantly higher percentage of patients in the recent suicide attempters group had previous suicide attempts (χ2 = 171.861, p < 0.001) and depressive episodes with melancholic features (χ2 = 22.837, p < 0.001).
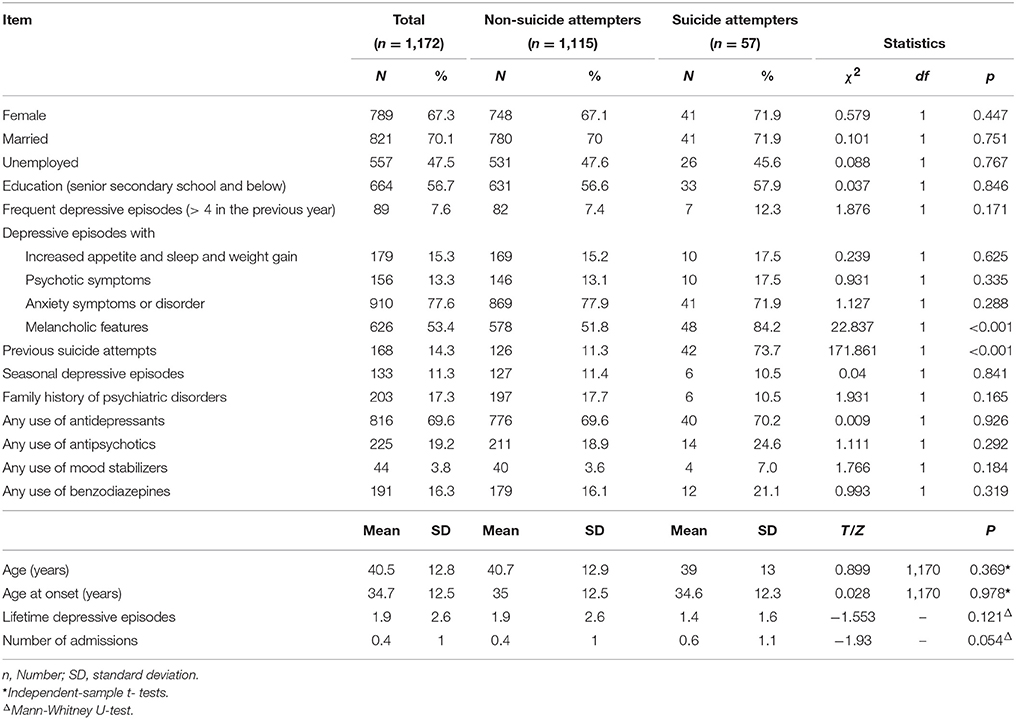
Table 1. Comparison of the basic demographic and clinical variables between recent suicide attempters and non-recent suicide attempters diagnosed with MDD.
Correlates of Recent Suicide Attempts
Candidate variables including previous suicide attempts and depressive episodes with melancholic features with a p-value < 0.05 on univariate analysis and clinical relevant variables including age, gender, depressive episodes with psychotic symptoms, depressive episodes with anxiety symptoms, or disorder were entered into multivariable model. Multiple logistic regression analysis with the forward stepwise method also showed that previous suicide attempts (OR = 20.81, 95% CI: 11.12–38.94, p < 0.001) and depressive episodes with melancholic features (OR = 4.43, 95% CI: 2.09–9.43, p < 0.001) were the risk factors for recent suicide attempts in MDD patients (Table 2).
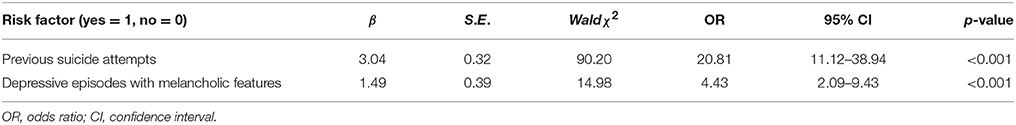
Table 2. Multiple logistic regression analysis of the risk factors for recent suicide attempts in MDD patients.
Discussion
Among 1,172 treatment-seeking outpatients and inpatients with MDD, 4.9% of the subjects had suicide attempt behavior in the past month. The patients with recent suicide attempt behaviors were more likely to have melancholic features and previous suicide attempts.
In the present study, 14.3% of the patients with MDD had previous suicide attempts. Previous Western studies had suggested the important effect of previous suicide attempts for future suicides (8). Among the previous suicide attempters in this study, 25% of them made a suicide attempt during the investigated time. Therefore, patients with previous suicide attempts should be carefully monitored. It is necessary to provide them with additional support and services by clinicians and other care providers.
Previous studies also have proposed that melancholic features may be associated with past suicide attempts and the probability of future attempts (28, 29). A more recent study in six Asian countries showed that the suicidal risk in MDD patients with melancholic features is 1.79 times higher than in subjects without melancholic features (30). Another study that investigated Chinese women with MDD also showed that melancholia is associated with suicide attempts (17). Consistent with these studies, we also found that melancholic features is a risk factor for suicide attempt in the investigated patients. Numerous studies have documented that melancholic depression is associated with poorer treatment response, more severe cognitive impairment, greater severity of illness, and higher suicide risk than MDD patients without melancholic features (30–34). These help explain the high suicide attempt rate in MDD patients with melancholic features.
Several studies showed that psychotic symptoms increased the risk of suicide in MDD patients (35, 36). One 4-year follow up study conducted in Finland found that psychotic symptoms increased the risk of completed suicide after a serious suicide attempt by 3.32 fold compared with patients without psychotic features (37). However, others have not confirmed this finding (38). A systematic review showed that psychotic symptoms increase the risk of suicide attempts during an acute episode of MDD, but they have little effect on attempted suicide after the acute episode is remitted (39). Psychosis was not identified as an independent risk factor for recent suicide attempts in the present study. This may be because many subjects were not in an acute episode at the time of evaluation.
Most previous studies conducted in Western countries reported that women make more suicide attempts but more males die due to their suicide attempts (13, 40). In China the pattern was different: more women than men make suicide attempts and complete suicides (41). This was the case according to data before the year 2000. However, no gender difference was found after the year 2000 in China (42). In the investigated group, women constituted about 75 percent of recent suicide attempters. However, no association was found between suicide attempts and gender.
There are several limitations in the present study. First, the DASP was a cross-sectional survey in which most of the data were retrospectively collected. Therefore, recall bias might have affected the accuracy of the data. Second, the cross-sectional nature of the study could not establish a causal relationship between the demographic and clinical features and the suicide attempts. A prospective study should be carried to evaluate risk factors of suicide in patients diagnosed with MDD. Third, the severity of depression in patients with MDD was not evaluated. Perroud et al. found that MDD patients with suicide attempts were more severely ill than subjects who had not attempted suicide (43). The Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study also found that subjects with prior suicide attempts had greater current severity of medical illness than non-attempters in MDD patients (13). However, a 10-year longitudinal study did not find an association between severity of depression symptoms and future suicide attempt (12). Fourth, as the investigation of suicide variables was not a primary aim of the DASP project, other potential risk factors for suicide attempts including misuse of alcohol and drugs (10) and co-morbid personality disorders (12, 44, 45) were not recorded. The present study, however, has a multi-center design and a large sample size and therefore may reflect the real world of clinical practice with MDD patients in China.
In conclusion, two clinical features were found to be related to recent suicide attempt in MDD patients in our study. Focusing on these clinical characteristics may help clinicians to identify the patients with high-risk of suicidal behavior and implement effective preventive interventions to reduce suicide.
Author Contributions
Y-AS and T-MS designed research. F-DY, GW, Y-RF, ZL, H-CY, JH, Z-YC, YH, JS, X-PW, H-CL, and J-BZ performed research and collected data. L-MX and LC analyzed data. L-MX, Y-AS, and T-MS wrote the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The study was initiated by the Chinese Society of Psychiatry with support from AstraZeneca China. AstraZeneca China had no role in the study design or the generation or interpretation of the results. The authors are grateful to all the clinicians who helped to organize the study in each study site. The analysis and submission of the manuscript were partially supported by the Capital Foundation of Medicine Research and Development (2016-1-4111) and the Natural Science Foundation of China (grant numbers:81630031).
References
1. Fond G, Guillaume S, Jaussent I, Beziat S, Macgregor A, Bernard P, et al. Prevalence and smoking behavior characteristics of nonselected smokers with childhood and/or adult self-reported ADHD symptoms in a smoking-cessation program: a cross-sectional study. J Atten Disord. (2015) 19:293–300. doi: 10.1177/1087054713497396
2. Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet (2007) 369:1302–13. doi: 10.1016/S0140-6736(07)60368-7
3. World Health Organization. Global Health Observatory Data. (2017). Available online at: http://www.who.int/gho/mental_health/suicide_rates/en/
4. Phillips MR, Yang G, Zhang Y, Wang L, Ji H, Zhou M. Risk factors for suicide in China: a national case-control psychological autopsy study. Lancet (2002) 360:1728–36. doi: 10.1016/S0140-6736(02)11681-
5. Osby U, Brandt L, Correia N, Ekbom A, Sparen P. Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry (2001) 58:844–50. doi: 10.1001/archpsyc.58.9.844
6. Isometsa ET, Henriksson MM, Aro HM, Heikkinen ME, Kuoppasalmi KI, Lonnqvist JK. Suicide in major depression. Am J Psychiatry (1994) 151:530–6. doi: 10.1176/ajp.151.4.530
7. Suominen K, Isometsa E, Suokas J, Haukka J, Achte K, Lonnqvist J. Completed suicide after a suicide attempt: a 37-year follow-up study. Am J Psychiatry (2004) 161:562–3. doi: 10.1176/appi.ajp.161.3.562
8. Sokero TP, Melartin TK, Rytsala HJ, Leskela US, Lestela-Mielonen PS, Isometsa ET. Prospective study of risk factors for attempted suicide among patients with DSM-IV major depressive disorder. Br J Psychiatry (2005) 186:314–8. doi: 10.1192/bjp.186.4.314
9. Suokas J, Suominen K, Isometsa E, Ostamo A, Lonnqvist J. Long-term risk factors for suicide mortality after attempted suicide–findings of a 14-year follow-up study. Acta Psychiatr Scand (2001) 104:117–21. doi: 10.1034/j.1600-0447.2001.00243.x
10. Hawton K, Casanas ICC, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. (2013) 147:17–28. doi: 10.1016/j.jad.2013.01.004
11. Choo C, Diederich J, Song I, Ho R. Cluster analysis reveals risk factors for repeated suicide attempts in a multi-ethnic Asian population. Asian J Psychiatr (2014) 8:38–42. doi: 10.1016/j.ajp.2013.10.001
12. May AM, Klonsky ED, Klein DN. Predicting future suicide attempts among depressed suicide ideators: a 10-year longitudinal study. J Psychiatr Res. (2012) 46:946–52. doi: 10.1016/j.jpsychires.2012.04.009
13. Claassen CA, Trivedi MH, Rush AJ, Husain MM, Zisook S, Young E, et al. Clinical differences among depressed patients with and without a history of suicide attempts: findings from the STAR*D trial. J Affect Disord. (2007) 97:77–84. doi: 10.1016/j.jad.2006.05.026
14. Azorin JM, Kaladjian A, Besnier N, Adida M, Hantouche E, Lancrenon S, et al. Suicidal behaviour in a French Cohort of major depressive patients: characteristics of attempters and nonattempters. J Affect Disord. (2010) 123:87–94. doi: 10.1016/j.jad.2009.09.004
15. Cao XL, Zhong BL, Xiang YT, Ungvari GS, Lai KY, Chiu HF, et al. Prevalence of suicidal ideation and suicide attempts in the general population of China: A meta-analysis. Int J Psychiatry Med. (2015) 49:296–308. doi: 10.1177/0091217415589306
16. Zhang YQ, Yuan GZ, Li GL, Yao JJ, Cheng DH, Chu X, et al. A case-control study on the risk factors for attempted suicide in patients with major depression. Chin J Epidemiol. (2007) 28:131–5.
17. Zhu Y, Zhang H, Shi S, Gao J, Li Y, Tao M, et al. Suicidal risk factors of recurrent major depression in Han Chinese women. PLoS ONE (2013) 8:e80030. doi: 10.1371/journal.pone.0080030
18. Chen L, Liu YH, Zheng QW, Xiang YT, Chen DF, Duan YP, et al. Risk factors to suicidal attempt in major depressive disorder patients. Chin J Psychiatry (2013) 46:339–43.
19. Goldstein RB, Black DW, Nasrallah A, Winokur G. The prediction of suicide. Sensitivity, specificity, and predictive value of a multivariate model applied to suicide among 1906 patients with affective disorders. Arch Gen Psychiatry (1991) 48:418–22.
20. Scoliers G, Portzky G, van Heeringen K, Audenaert K. Sociodemographic and psychopathological risk factors for repetition of attempted suicide: a 5-year follow-up study. Arch Suicide Res. (2009) 13:201–13. doi: 10.1080/13811110902835130
21. Chen L, Liu YH, Zheng QW, Xiang YT, Duan YP, Yang FD, et al. Suicide risk in major affective disorder: results from a national survey in China. J Affect Disord. (2014) 155:174–9. doi: 10.1016/j.jad.2013.10.046
22. Xiang YT, Zhang L, Wang G, Hu C, Ungvari GS, Dickerson FB, et al. Sociodemographic and clinical features of bipolar disorder patients misdiagnosed with major depressive disorder in China. Bipolar Disord. (2013) 15:199–205. doi: 10.1111/bdi.12052
23. Xin LM, Chen L, Ji ZP, Zhang SY, Wang J, Liu YH, et al. Risk factors for anxiety in major depressive disorder patients. Clin Psychopharmacol Neurosci. (2015) 13:263–8. doi: 10.9758/cpn.2015.13.3.263
24. Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv. (2001) 52:51–5. doi: 10.1176/appi.ps.52.1.51
25. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry (1998) 59 (Suppl 20):22–33.
26. Si T, Shu L, Dang WM, Su YA, Chen JX, Dong WT, et al. Evaluation of the reliability and validity of chinese version of the Mini International Neuropsychiatric Interview in patients with mental disorders (in Chinese). Chin Ment Health J. (2009) 23:493–503.
27. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourthed. Washington, DC: American Psychiatric Association Press (1994).
28. Agargun MY, Besiroglu L, Cilli AS, Gulec M, Aydin A, Inci R, et al. Nightmares, suicide attempts, and melancholic features in patients with unipolar major depression. J Affect Disord. (2007) 98:267–70. doi: 10.1016/j.jad.2006.08.005
29. Grunebaum MF, Galfalvy HC, Oquendo MA, Burke AK, Mann JJ. Melancholia and the probability and lethality of suicide attempts. Br J Psychiatry (2004) 184:534–5. doi: 10.1192/bjp.184.6.534
30. Jeon HJ, Peng D, Chua HC, Srisurapanont M, Fava M, Bae JN, et al. Melancholic features and hostility are associated with suicidality risk in Asian patients with major depressive disorder. J Affect Disord. (2013) 148:368–74. doi: 10.1016/j.jad.2013.01.001
31. McGrath PJ, Khan AY, Trivedi MH, Stewart JW, Morris DW, Wisniewski SR, et al. Response to a selective serotonin reuptake inhibitor (citalopram) in major depressive disorder with melancholic features: a STAR*D report. J Clin Psychiatry (2008) 69:1847–55. doi: 10.4088/JCP.v69n1201
32. Caldieraro MA, Baeza FL, Pinheiro DO, Ribeiro MR, Parker G, Fleck MP. Clinical differences between melancholic and nonmelancholic depression as defined by the CORE system. Compr Psychiatry (2013) 54:11–5. doi: 10.1016/j.comppsych.2012.05.012
33. Roca M, Monzon S, Vives M, Lopez-Navarro E, Garcia-Toro M, Vicens C, et al. Cognitive function after clinical remission in patients with melancholic and non-melancholic depression: a 6 month follow-up study. J Affect Disord. (2015) 171:85–92. doi: 10.1016/j.jad.2014.09.018
34. Withall A, Harris LM, Cumming SR. A longitudinal study of cognitive function in melancholic and non-melancholic subtypes of major depressive disorder. J Affect Disord. (2010) 123:150–7. doi: 10.1016/j.jad.2009.07.012
35. Park MH, Kim TS, Yim HW, Jeong SH, Lee C, Lee CU, et al. Clinical characteristics of depressed patients with a history of suicide attempts: results from the CRESCEND study in South Korea. J Nerv Ment Dis. (2010) 198:748–54. doi: 10.1097/NMD.0b013e3181f4aeac
36. Roose SP, Glassman AH, Walsh BT, Woodring S, Vital-Herne J. Depression, delusions, and suicide. Am J Psychiatry (1983) 140:1159–62. doi: 10.1176/ajp.140.9.1159
37. Suominen K, Haukka J, Valtonen HM, Lonnqvist J. Outcome of patients with major depressive disorder after serious suicide attempt. J Clin Psychiatry (2009) 70:1372–8. doi: 10.4088/JCP.09m05110blu
38. Leadholm AK, Rothschild AJ, Nielsen J, Bech P, Ostergaard SD. Risk factors for suicide among 34,671 patients with psychotic and non-psychotic severe depression. J Affect Disord. (2014) 156:119–25. doi: 10.1016/j.jad.2013.12.003
39. Zalpuri I, Rothschild AJ. Does psychosis increase the risk of suicide in patients with major depression? A systematic review. J Affect Disord. (2016) 198:23–31. doi: 10.1016/j.jad.2016.03.035
40. Yang SJ, Stewart R, Kang HJ, Kim SY, Bae KY, Kim JM, et al. Response to antidepressants in major depressive disorder with melancholic features: the CRESCEND study. J Affect Disord. (2013) 144:42–50. doi: 10.1016/j.jad.2012.06.004
41. Phillips MR, Li X, Zhang Y. Suicide rates in China, 1995-99. Lancet (2002) 359:835–40. doi: 10.1016/S0140-6736(02)07954-0
42. Li Y, Li Y, Cao J. Factors associated with suicidal behaviors in mainland China: a meta-analysis. BMC Public Health (2012) 12:524. doi: 10.1186/1471-2458-12-524
43. Perroud N, Uher R, Hauser J, Rietschel M, Henigsberg N, Placentino A, et al. History of suicide attempts among patients with depression in the GENDEP project. J Affect Disord. (2010) 123:131–7. doi: 10.1016/j.jad.2009.09.001
44. Jylha P, Rosenstrom T, Mantere O, Suominen K, Melartin T, Vuorilehto M, et al. Personality disorders and suicide attempts in unipolar and bipolar mood disorders. J Affect Disord. (2016) 190:632–9. doi: 10.1016/j.jad.2015.11.006
Keywords: suicide attempt, major depressive disorder, risk factor, melancholic features, China
Citation: Xin L-M, Chen L, Su Y-A, Yang F-D, Wang G, Fang Y-R, Lu Z, Yang H-C, Hu J, Chen Z-Y, Huang Y, Sun J, Wang X-P, Li H-C, Zhang J-B and Si T-M (2018) Risk Factors for Recent Suicide Attempts in Major Depressive Disorder Patients in China: Results From a National Study. Front. Psychiatry 9:300. doi: 10.3389/fpsyt.2018.00300
Received: 30 November 2017; Accepted: 15 June 2018;
Published: 03 July 2018.
Edited by:
Zoe Fisher, Abertawe Bro Morgannwg University Health Board, United KingdomReviewed by:
Mirko Manchia, Università degli Studi di Cagliari, ItalyYuping Ning, Southern Medical University, Guangdong, China; The Affiliated Brain Hospital of Guangzhou Medical University (Guangzhou Huiai Hospital), China
Copyright © 2018 Xin, Chen, Su, Yang, Wang, Fang, Lu, Yang, Hu, Chen, Huang, Sun, Wang, Li, Zhang and Si. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yun-Ai Su, c3V5dW5haUAxNjMuY29t
Tian-Mei Si, c2kudGlhbi1tZWlAMTYzLmNvbQ==
 Li-Min Xin
Li-Min Xin Lin Chen
Lin Chen Yun-Ai Su
Yun-Ai Su Fu-De Yang2
Fu-De Yang2 Tian-Mei Si
Tian-Mei Si