- 1Department of Psychiatry and Narcology, Riga Stradins University, Riga, Latvia
- 2Department of Public Health and Epidemiology, Riga Stradins University, Riga, Latvia
- 3Department of Psychiatry, University of California, San Diego, San Diego, CA, United States
- 4Department of Cardiology, University Clinic of Paul Stradins, Riga, Latvia
Background: Depression and anxiety have been recognized as independent risk factors for both the development and prognosis of cardiovascular (CV) diseases (CVD). The Systematic Coronary Risk Evaluation (SCORE) function measures the 10-year risk of a fatal CVD and is a crucial tool for guiding CV patient management. This study is the first in Latvia to investigate the association of depression and anxiety with the 10-year CV mortality risk in a primary care population.
Methods: This cross-sectional study was conducted at 24 primary care facilities. During a 1-week period in 2015, all consecutive adult patients were invited to complete a nine-item Patient Health Questionnaire (PHQ-9) and a seven-item Generalized Anxiety Disorder scale (GAD-7) followed by sociodemographic questionnaire and physical measurements. The diagnostic Mini International Neuropsychiatric Interview (M.I.N.I.) was administered by telephone in the period of 2 weeks after the first contact at the primary care facility. A hierarchical multivariate analysis was performed.
Results: The study population consisted of 1,569 subjects. Depressive symptoms (PHQ-9 ≥10) were associated with a 1.57 (95% confidence interval (CI): 1.06–2.33) times higher odds of a very high CV mortality risk (SCORE ≥10%), but current anxiety disorder (M.I.N.I.) reduced the CV mortality risk with an odds ratio of 0.58 (95% CI: 0.38–0.90).
Conclusions: Our findings suggest that individuals with SCORE ≥10% should be screened and treated for depression to potentially delay the development and improve the prognosis of CVD. Anxiety could possibly have a protective influence on CV prognosis.
Introduction
Depression and cardiovascular (CV) diseases (CVD) are the two most common non-communicable diseases causing disability and mortality worldwide (1, 2). In Latvia, the mortality rate from CVD is among the highest in the European Union (EU) and was responsible for 57% of all deaths in 2015 (3, 4). The standard premature mortality from CVD is three times higher in Latvia than in the EU (5).
During the last two decades there is a growing interest in non-conventional cardiovascular risk factors such as psychosocial factors. The seminal INTERHEART study, which considered 15,152 myocardial infarction (MI) cases from 52 countries, showed that nine risk factors were responsible for 90% of the population attributable risk (PAR) and that psychosocial factors (including anxiety and depression) alone were responsible for 32.5% of it, suggesting that they were as important as smoking (PAR, 35.7%) and even more relevant than hypertension (PAR, 17.9%) and diabetes mellitus (PAR, 9.9%) as risk factors for CVD (6). Depression and anxiety have been established as independent risk factors for both the onset of and the prognosis of CVD (7, 8), although the contribution of anxiety as an etiological risk factor is contradictory (9, 10).
Depressive and anxiety disorders are the most frequent mental conditions in patients suffering from CVD and are highly comorbid (11, 12). Between 15 and 20% of CV patients meet the diagnostic criteria for major depressive disorder (MDD), and an even larger proportion (40–65%) indicate subsyndromal levels of depressive symptoms (13, 14). The prevalence of elevated symptoms of anxiety in CV patients has been reported to be approximately 30% (12, 14). Data on the relationship between depression, anxiety and CVD from the Baltic region are limited and controversial (15–17).
The American Heart Association (AHA) has taken a lead role in highlighting the importance of depression in CV patients by recommending routine screening of all cardiac patients in 2008 (18, 19). However, a recent systematic review by Thombs et al. (20) found no evidence that this strategy improves depression or cardiac outcomes (20). Furthermore, in patients with already diagnosed coronary artery disease (CAD), mental health interventions for MDD showed moderate efficacy for reducing cardiac events, but remained controversial in the ability to reduce total mortality (7, 21). This finding underscores the importance of primary prevention of CVD and the need to identify the target population who would most benefit from depression and anxiety screening.
The Systematic Coronary Risk Evaluation (SCORE) function measures the 10-year risk of a fatal CVD. The SCORE charts have been elaborated to rapidly calculate CV mortality risk with sufficient accuracy in both high- and low-risk European populations. Since 1994, the SCORE has been widely advocated by the joint recommendations from the European Association of Preventive Cardiology, European Society of Cardiology, European Atherosclerosis Society and European Society of Hypertension (7, 22). There is also an electronic version of the SCORE risk charts that is even easier to use in daily clinical practice (23).
This project aimed to be the first study to examine the association of anxiety and depression with the 10-year CV mortality risk in a primary care population of Latvia. This research addresses a relevant gap in the body of knowledge concerning Latvian, Baltic and East European populations. The study findings have implications for medical education, policy, and program development in these countries.
Materials and Methods
The current research was performed in 2015 as a part of the National Research Program BIOMEDICINE (2014–2017) to estimate the frequency of most common psychiatric disorders in primary care population of Latvia. The study approached patients of 24 primary care facilities across the country (8 in rural and 16 in urban regions). This research was carried out in the two most widely spoken languages in Latvia (Latvian and Russian).
Ethics
This study was authorized by the Ethics Committee of the Riga Stradins University, Riga, Latvia (No. 8/18.06.2015.). All subjects were included in the study only after signing written informed consent. The research was conducted accordingly with the Declaration of Helsinki and its subsequent amendments.
Subjects and Procedures
The inclusion criteria were as follows: all consecutive treatment-seeking patients attending primary care facility, persons who were 18 years of age or older, and subjects who had provided their informed consent. The exclusion criteria were as follows: persons who declined to be enrolled in this research project, persons who were younger than 18 years of age, and persons who presented with an urgent health complaints requiring immediate intervention.
During 1 week period in 2015, all consecutive adult persons who corresponded to the inclusion criteria were approached to complete the Patient Health Questionnaire (PHQ-9) for screening of depressive symptoms and the Generalized Anxiety Disorder questionnaire (GAD-7) for screening of anxiety symptoms in Latvian or Russian (language as preferred by participant), followed by a structured interview on sociodemographic characteristics and measurements of weight, height, waist circumference, total cholesterol, and blood pressure. The diagnostic Mini International Neuropsychiatric Interview (M.I.N.I.) was administered by telephone in the period of 2 weeks after the first contact at the primary care facility by specially trained interviewers (psychiatrists). SCORE was calculated for each individual patient using the electronic version of the high risk chart developed and supported by the European Society of Cardiology (23). Information about the prescription of cardiovascular and psychotropic medications from the last 3 months were acquired using medical records.
Assessment Tools and Measures
The Patient Health Questionnaire-9 is a nine-item self-reported depression screening tool based on the diagnostic criteria for MDD according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) (24). Recent meta-analysis by Meader and colleagues that aimed to define the most effective tool for detection of MDD in persons with chronic somatic diseases showed that among other widely used screening instruments the PHQ-9 revealed good diagnostic accuracy. A score of 10 or higher on the PHQ-9 had a sensitivity of 84% and a specificity of 88% for detecting MDD (25). Both Latvian and Russian versions of the PHQ-9 for Latvia were validated as part of the National Research Project BIOMEDICINE (2014–2017) (26).
The 7-item Generalized Anxiety Disorder scale is a self-rating screening tool for anxiety symptoms (27). The GAD-7 has been established as a reliable tool for detection of most common anxiety disorders. A cut-off score of 10 points and higher has a sensitivity of 89% and a specificity of 82% for generalized anxiety disorder (GAD). It is moderately good at screening panic disorder (PD) (sensitivity-74%, specificity-81%), social anxiety disorder (sensitivity-72%, specificity-80%), and post-traumatic stress disorder (PTSD) (sensitivity-66%, specificity-81%) (28).
The M.I.N.I. is a structured diagnostic interview for most common mental disorders in accordance with the DSM-IV and the 10th version of the International Classification of Diseases (29). The M.I.N.I. has been previously translated for use in Latvian and Russian languages by authorship holders. The M.I.N.I. authorship holder prof. David Sheehan provided written permission to use this scale in our study.
The SCORE system measures the 10-year risk of a fatal CV event (e.g., stroke, myocardial infarction or aneurysm of the aorta). The SCORE risk assessment is derived using data from 12 European cohort studies with 205,178 participants covering a wide geographic spread of countries at different levels of CV risk. The SCORE charts have been elaborated to calculate risk in both high- and low-risk European populations. The reported predictive values representing areas under receiver operating characteristic curves for SCORE have ranged from 0.71 to 0.84 (22). Total CV risk estimation using SCORE is a crucial tool for supporting clinicians during the optimization of individual CV risk reduction in apparently healthy individuals. This risk estimation is based on the following risk factors: gender, age, smoking, systolic blood pressure, and total cholesterol. The threshold for very high risk is defined as a calculated SCORE ≥10%, and it was used as a cut-off score in our study (7, 23).
The sociodemographic questionnaire included questions about demographics (age, sex, ethnicity, marital status, education), CV risk factors, history of CVD, diabetes mellitus and psychiatric disorders, use of CV and psychotropic medications. The section on CV risk factors included questions about family history of premature CVD in first-degree relatives (<55 years in men and <65 years in women), physical activity (number of moderate exercise sessions of at least 30 min per week), smoking habits (smoking status, number of cigarettes), alcohol use, and consumption of fresh vegetables, fruits and fish.
Statistical Analysis
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) version 20.0 (IBM SPSS Corp.). Statistical significance was considered as p < 0.05. Differences of the study sample between comparative SCORE groups were detected using Chi-Square test or Fisher's exact test.
To examine associations of depression and anxiety with the SCORE function, we conducted an univariate and stepwise multivariate analysis (using binary logistic regression) according to the conceptual hierarchical framework model (30), in which possible confounding variables were distributed into 3 groups: proximal (positive family history, number of cigarettes, diabetes, use of antihypertensive, cholesterol lowering medications), intermediate (body mass index/waist circumference, depression and/or anxiety, sedentary lifestyle, consumption of fresh vegetables and fruits, consumption of fish, alcohol use) and distal factors (education, employment status, marital status, place of residence). Factors that were used in the calculation of the SCORE function (gender, age, blood pressure, total cholesterol, smoking status) were excluded from the list of independent variables in the regression analysis.
As current depressive episode according to the M.I.N.I. and anxiety symptoms detected by the GAD-7 did not show statistically significant results in the univariate analysis, these measures were not included in the final regression model. To gain more statistical power, we combined all anxiety disorders according to the M.I.N.I. into one current anxiety variable for the final analysis, including GAD, PD, PTSD, and agoraphobia. Previous research has demonstrated that these anxiety disorders contribute to the risk of developing CVD and a worse prognosis of CVD (7, 31).
Results
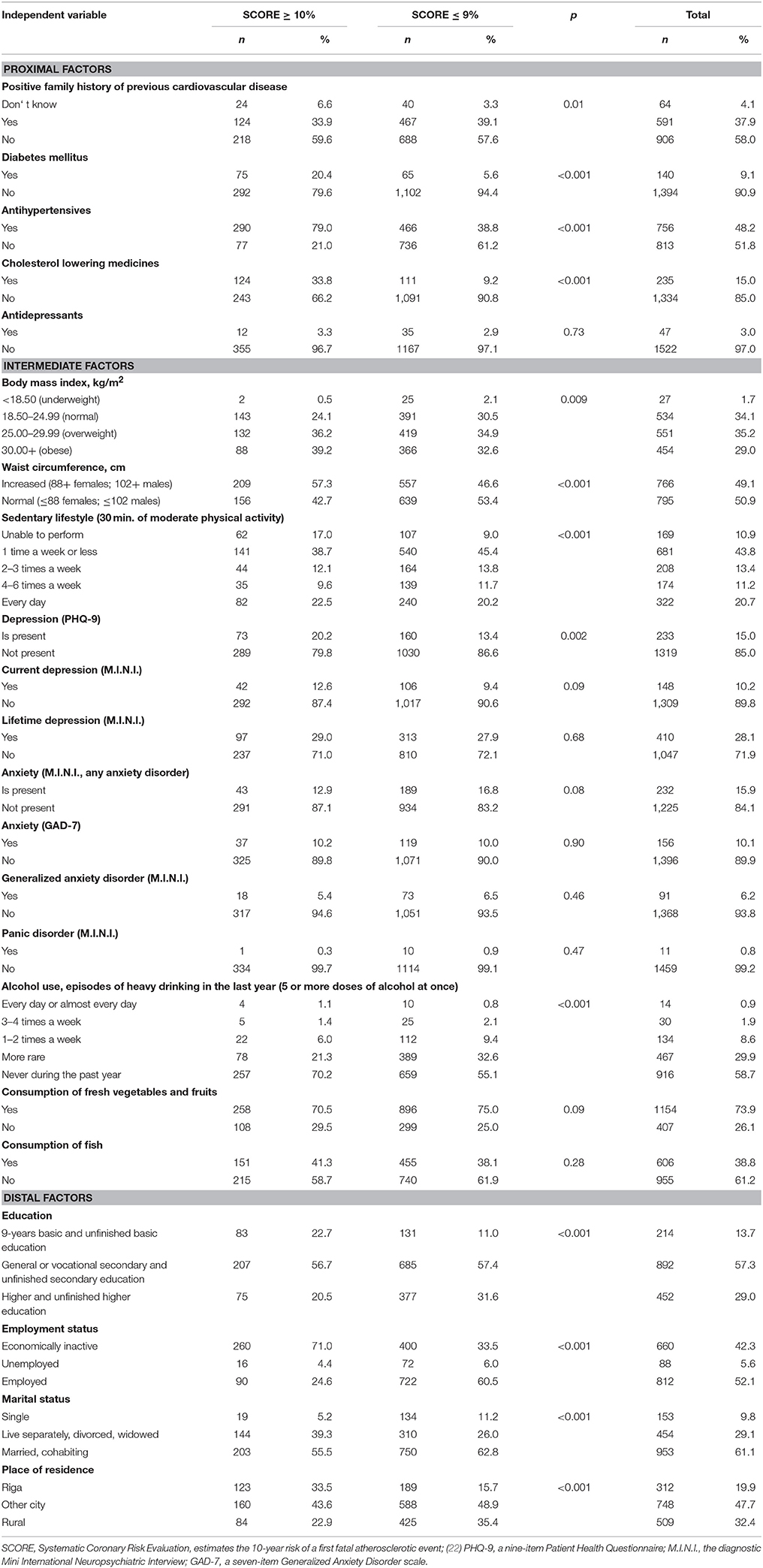
From 1,756 approached subjects 152 declined to participate in this study. The mean response rate was 91.3%, it varied between 86.3 and 93.7% across 24 primary care facilities all over the country. Those who declined did not significantly differ in the basic sociodemographic characteristics from the study sample. In total, 1,604 patients were approached to complete the PHQ-9 and the GAD-7 questionnaires, which were completed by 1,585 of participants. Among those who completed both questionnaires, the SCORE measure was calculated for 1,569 subjects (69.0% women), who were included in the final analysis. Of the eligible study subjects, 23.4% (n = 367) showed a very high 10-year CV mortality risk according to the SCORE (≥10%). Clinical symptoms of depression (PHQ-9 ≥10) were present in 15.0% (n = 233) of individuals. According to the M.I.N.I., 10.2% (n = 148) had current and 28.1% (n = 410) had a lifetime depressive episode. Clinically relevant anxiety symptoms (GAD-7 ≥10) were detected in 10.1% (n = 156) of individuals. According to the M.I.N.I., 15.9% (n = 232) had a current anxiety disorder. A complete description of the sample is shown in Table 1.
In the final multivariate analysis model (Table 2), a very high risk of CV mortality was significantly associated with three proximal factors: presence of diabetes, use of antihypertensive and cholesterol lowering medicines. Among distal factors, three variables increased the risk of CV mortality: lower education level, inactive economic status or unemployment, and urban place of residence.
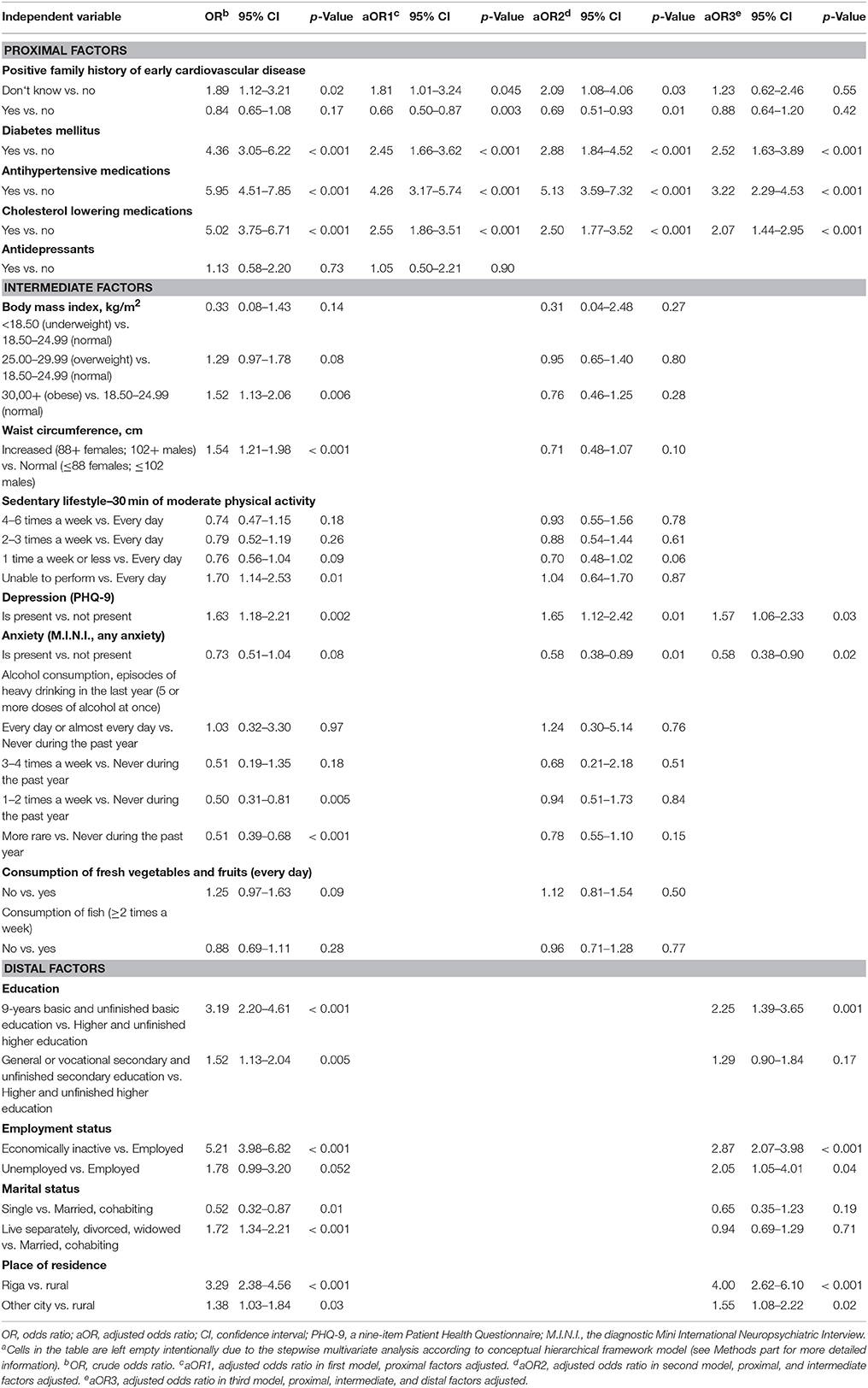
Table 2. Factors associated with a very high risk of cardiovascular mortality in univariate and hierarchical multivariate analysesa.
The only intermediate factors that remained significantly associated with a SCORE ≥10% after adjustment for socio-economic and traditional CV risk factors were depression (according to the PHQ-9) and anxiety (according to the M.I.N.I.). Subjects with clinical symptoms of depression had a 1.57 (p = 0.03) times higher odds of very high CV risk. Interestingly, current anxiety disorder showed a preventive effect on CV mortality. Subjects with diagnosed anxiety disorder had a 0.58 lower odds (p = 0.02) of having a SCORE ≥10%.
Discussion
This is the first study in Latvia to explore the relationship between depression, anxiety and the 10-year risk of a first fatal atherosclerotic event in primary care population based on the SCORE system. The most relevant findings were that patients with clinical symptoms of depression (PHQ-9 ≥10) demonstrated a 1.57 times higher odds of a very high 10-year CV risk as measured by the SCORE function, but current anxiety disorder (M.I.N.I.) reduced the risk of CV mortality with an OR of 0.58. These findings remained statistically significant even after adjusting for multiple socio-demographic and traditional CV risk factors.
A global overview of the literature from approximately 50 prognostic studies on the link between depression and CVD from the last 25 years concluded that clinically relevant depressive symptoms are associated with a 1.6 to 2.2-fold higher risk of adverse outcomes (31, 32); however, prior studies in the Baltic nations have been contradictory. A prospective cohort study of primary care population (n = 1,115) in Lithuania examined the association of the metabolic syndrome, current major depressive episode, lifetime major depressive episode, and GAD with 10-year CV mortality (33). Butnoriene et al. (33) found that lifetime major depressive episode was associated with an elevated risk of CV mortality in women (HR = 1.86; p = 0.019) adjusted for conventional CV risk factors. In men, neither current MDE nor lifetime MDE were associated with mortality. Another study from Lithuania by Burokiene et al. (15) showed a more modest but statistically significant association of CV morbidity and clinically relevant depressive symptoms (OR = 1.18; p = 0.001). Surprisingly, a cross-sectional study involving 1,094 patients from 23 family practices across Estonia did not indicate higher co-morbidity of CVD in depressed patients when compared to non-depressed patients (16). Our findings about the association of depression with CV mortality are in line with prior studies identifying depression as an independent risk factor for CV morbidity and mortality.
Although many studies have examined the association of depression with separate traditional CV risk factors, including arterial hypertension, hypercholesterolemia, diabetes and obesity, we found only one publication that used the SCORE system (34). Koponen et al. (34) reported that clinically relevant depressive symptoms were associated with a 2.9-fold higher (95% CI 1.4–5.7) 10-year CV mortality risk in men and a 1.4-fold higher (95% CI 1.1–4.2) risk in women using the SCORE function. Despite similar objectives, there were several significant differences in the methodology of this study. In the study by Koponen et al. (34) a “high/very high” risk for CV mortality was defined as a SCORE ≥3%. We chose a SCORE ≥10% as a threshold for very high risk of CV mortality in accordance with the European Guidelines on cardiovascular disease prevention in clinical practice (2016) (7). We also used additional confounding factors such as place of residence and anxiety, which appeared to have a significant impact on the SCORE results.
In contrast to depression, the relationship between anxiety and CVD is less clear. Meta-analysis by Roest et al. (35) summarizing 20 studies with 249,846 participants found that anxious persons were at an increased risk for incident CAD (HR = 1.26; p < 0.0001) and CV mortality (HR = 1.48; p = 0.003), independent of sociodemographic characteristics, traditional and lifestyle CV risk factors (35). However, the meta-analytic assessment on the link between anxiety and CAD was not controlled for depression, which is very frequent comorbid condition with anxiety. Since the publication of that review in 2010, more recent studies have suggested that anxiety may act as a protective factor in certain instances (9, 10). The most recent meta-analysis (2016) also included studies focusing on stroke and peripheral vascular disease, summarizing 37 studies with 1,565,699 participants (36). Batelaan and colleagues found that clinically relevant anxiety symptoms were associated with a 1.52 times higher risk of incident CV morbidity (95% CI 1.36–1.71). Although the data on the prognostic influence of anxiety are complex and even controversial, most publications support the association of anxiety with CV mortality, but they do so to a lesser extent compared with depression. In addition, a few studies have been performed in the Baltic region, but none have examined the association of anxiety with the SCORE function. Butnoriene et al. (33) showed that current GAD predicted greater CV mortality in women (HR = 1.86–1.99; p ≤ 0.025), but not in men. A small study (n = 64) from Estonia also reported differences between young male and female post-MI patients, indicating that females suffered a higher level of cognitive worry and were less able to relax in the prodromal period of MI (37).
One of the most unexpected findings of our study was that current anxiety disorder (M.I.N.I.) was associated with a reduced CV mortality risk, suggesting a possible protective influence. This result is in agreement with the findings of Meyer et al. (9), which showed that elevated symptoms of anxiety were associated with beneficial effects on survival in individuals with stable CV conditions (HR = 0.70; p = 0.031) comparing to individuals after acute MI with reduced systolic left ventricular function (HR = 1.32; p = 0.011) (9). Therefore, it has been hypothesized that prognostic influence of anxiety might be modulated through CVD severity (degree of left ventricular dysfunction).
The use of a structured diagnostic interview for the detection of anxiety disorders, a nationally representative primary care convenience sample including persons with a wide range of ages, and a hierarchical multivariate analysis including control for conventional CV, socioeconomic risk factors, anxiety and place of residence are important strengths of this study.
There are several limitations to the results of current study. First, because of the cross-sectional setting of this study, we could not draw definite conclusions about the causality of the identified relationships between clinically relevant depressive symptoms or anxiety disorders and cardiovascular mortality risk. Second, the PHQ-9 with a cut-off score of 10 points and higher has been accepted as a reliable instrument for detection of MDD in chronic physical diseases (25). However, the PHQ-9 is a screening tool and not a diagnostic criterion for MDD, which can result in false positive cases. Third, we combined all anxiety disorders according to the M.I.N.I., including GAD, PD, agoraphobia, and PTSD, in the current anxiety variable of the final analysis to gain more statistical power. Although these diagnoses share the common basic symptoms of anxiety and neurobiological mechanisms (38, 39), we were unable to clarify whether our findings were attributable to all included anxiety disorders.
Conclusions
We found a statistically significant association between depression (PHQ-9 ≥10) and a very high risk of CV mortality. In contrast to our expectations, current anxiety disorder (M.I.N.I.) was found to be negatively associated with CV mortality risk (SCORE ≥10%), which suggests that anxiety could potentially have a protective influence on CV prognosis. The findings of this study suggest that individuals with the SCORE ≥10% could benefit from screening and treatment of depression to potentially delay the development and improve the prognosis of CVD. Further research is needed to investigate the influence of anxiety on CV mortality risk in Latvian population.
Author Contributions
ER and JV created the design of this study. ER coordinated the study. DZ consulted about mental health aspects and IM consulted about cardiovascular aspects of the study design and statistical analysis. JV and RI participated in the data collection. AK performed the analyses. RI wrote the first draft of the manuscript. All authors participated in the writing and revision of the successive drafts of the manuscript. All authors read and approved the final manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors acknowledge the National Research Program BIOMEDICINE (2014–2017) for funding this study. Ministry of Education and Sciences, Republic of Latvia.
References
1. Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet (2016) 388:1459–544. doi: 10.1016/s0140-6736(16)31012-1
2. World Health Organisation: Depression. (2017) (Accessed April 30, 2017). Available online at: http://www.who.int/mediacentre/factsheets/fs369/en/
3. The Statistical Yearbook of Health Care in Latvia. (2015) (Accessed April 14, 2017). Available online at: https://www.spkc.gov.lv/en/statistics
4. The Potential Years of Life Lost. The Centre for Disease Prevention and Control of Latvia (2015) (April February 5, 2017). Available online at: https://www.spkc.gov.lv/en/statistics
5. The Causes of Death-Diseases of the Circulatory System. (2013) (Accessed February 8, 2017). Available online at: http://ec.europa.eu/eurostat/statistics-explained/index.php/Causes_of_death_statistics
6. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet (2004) 364:937–52. doi: 10.1016/s0140-6736(04)17018-9
7. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Atherosclerosis (2016) 252:207–74. doi: 10.1016/j.atherosclerosis.2016.05.037
8. Lichtman JH, Froelicher ES, Blumenthal JA, Carney RM, Doering LV, Frasure-Smith N, et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation (2014) 129:1350–69. doi: 10.1161/cir.0000000000000019
9. Meyer T, Buss U, Herrmann-Lingen C. Role of cardiac disease severity in the predictive value of anxiety for all-cause mortality. Psychosom. Med. (2010) 72:9–15. doi: 10.1097/PSY.0b013e3181c64fc0
10. Meyer T, Hussein S, Lange HW, Herrmann-Lingen C. Anxiety is associated with a reduction in both mortality and major adverse cardiovascular events five years after coronary stenting. Eur J Prev Cardiol. (2015) 22:75–82. doi: 10.1177/2047487313505244
11. Goodwin RD, Davidson KW, Keyes K. Mental disorders and cardiovascular disease among adults in the United States. J Psychiat. Res. (2009) 43:239–46. doi: 10.1016/j.jpsychires.2008.05.006
12. Pajak A, Jankowski P, Kotseva K, Heidrich J, de Smedt D, De Bacquer D. Depression, anxiety, and risk factor control in patients after hospitalization for coronary heart disease: the EUROASPIRE III Study. Eur J Prevent Cardiol. (2013) 20:331–40. doi: 10.1177/2047487312441724
13. Thombs BD, Bass EB, Ford DE, Stewart KJ, Tsilidis KK, Patel U, et al. Prevalence of depression in survivors of acute myocardial infarction. J Gen Int Med. (2006) 21:30–8. doi: 10.1111/j.1525-1497.2005.00269.x
14. Pogosova N, Kotseva K, De Bacquer D, von Känel R, De Smedt D, Bruthans J, et al. Psychosocial risk factors in relation to other cardiovascular risk factors in coronary heart disease: Results from the EUROASPIRE IV survey. A registry from the European Society of Cardiology. Eur J Prevent. Cardiol. (2017) 24:1371–80. doi: 10.1177/2047487317711334
15. Burokiene N, Karčiauskaite D, Kasiulevičius V, Kučinskas V, Kučinskiene ZA. Manifestation of anxiety and depression and their association with cardiovascular diseases in the Lithuanian population. Acta Med Litu. (2014) 21:123–30. doi: 10.6001/actamedica.v21i3.2996
16. Suija K, Kalda R, Maaroos HI. Patients with depressive disorder, their co-morbidity, visiting rate and disability in relation to self-evaluation of physical and mental health: a cross-sectional study in family practice. BMC Family Pract. (2009) 10:38. doi: 10.1186/1471-2296-10-38
17. Ivanovs R, Kivite A, Ziedonis D, Mintale I, Vrublevska J, Rancans E. Association of depression and anxiety with cardiovascular co-morbidity in a primary care population in Latvia: a cross-sectional study. BMC Pub Health (2018) 18:328. doi: 10.1186/s12889-018-5238-7
18. Lichtman JH, Bigger JT Jr, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lesperance F, et al. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation (2008) 118:1768–75. doi: 10.1161/circulationaha.108.190769
19. Huffman JC, Celano CM. Depression in cardiovascular disease: from awareness to action. Trends Cardiov Med. (2015) 25:623–4. doi: 10.1016/j.tcm.2015.02.007
20. Thombs BD, Roseman M, Coyne JC, de Jonge P, Delisle VC, Arthurs E, et al. Does evidence support the American Heart Association's recommendation to screen patients for depression in cardiovascular care? An updated systematic review. PLoS ONE (2013) 8:e52654. doi: 10.1371/journal.pone.0052654
21. Rutledge T, Redwine LS, Linke SE, Mills PJ. A meta-analysis of mental health treatments and cardiac rehabilitation for improving clinical outcomes and depression among patients with coronary heart disease. Psychosomat Med. (2013) 75:335–49. doi: 10.1097/PSY.0b013e318291d798
22. Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. (2003) 24:987–1003. doi: 10.1016/S0195-668X(03)00114-3
23. The HeartScore. The European Society of Cardiology (2012) (Accessed February 11, 2017). Available online at: http://www.heartscore.org/en_GB/
24. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Int Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
25. Meader N, Mitchell AJ, Chew-Graham C, Goldberg D, Rizzo M, Bird V, et al. Case identification of depression in patients with chronic physical health problems: a diagnostic accuracy meta-analysis of 113 studies. Br J Gen Pract. (2011) 61:e808–20. doi: 10.3399/bjgp11X613151
26. Vrublevska J, Trapencieris M, Rancans E. Adaptation and validation of the Patient Health Questionnaire-9 to evaluate major depression in a primary care sample in Latvia. Nord J Psychiat. (2017) 72:112–8. doi: 10.1080/08039488.2017.1397191
27. Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Archiv Int Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
28. Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Int Med. (2007) 146:317–25. doi: 10.7326/003-4819-146-5-200703060-00004
29. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry (1998) 59(Suppl. 20):22–33.
30. Victora CG, Huttly SR, Fuchs SC, Olinto MT. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. Int J Epidemiol. (1997) 26:224–7.
31. Pogosova N, Saner H, Pedersen SS, Cupples ME, McGee H, Hofer S, et al. Psychosocial aspects in cardiac rehabilitation: From theory to practice. A position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation of the European Society of Cardiology. Eur J Prev Cardiol. (2015) 22:1290–306. doi: 10.1177/2047487314543075
32. Frasure-Smith N, Lesperance F. Depression and cardiac risk: present status and future directions. Heart (2010) 96:173–6. doi: 10.1136/hrt.2009.186957
33. Butnoriene J, Bunevicius A, Saudargiene A, Nemeroff CB, Norkus A, Ciceniene V, et al. Metabolic syndrome, major depression, generalized anxiety disorder, and ten-year all-cause and cardiovascular mortality in middle aged and elderly patients. Int J Cardiol. (2015) 190:360–6. doi: 10.1016/j.ijcard.2015.04.122
34. Koponen H, Jokelainen J, Keinanen-Kiukaanniemi S, Vanhala M. Depressive symptoms and 10-year risk for cardiovascular morbidity and mortality. World J Biol Psychiatry (2010) 11:834–9. doi: 10.3109/15622975.2010.486842
35. Roest AM, Martens EJ, de Jonge P, Denollet J. Anxiety and risk of incident coronary heart disease: a meta-analysis. J Am Coll Cardiol. (2010) 56:38–46. doi: 10.1016/j.jacc.2010.03.034
36. Batelaan NM, Seldenrijk A, Bot M, van Balkom AJ, Penninx BW. Anxiety and new onset of cardiovascular disease: critical review and meta-analysis. Br J Psychiatry (2016) 208:223–31. doi: 10.1192/bjp.bp.114.156554
37. Uuskula M. Psychological differences between young male and female survivors of myocardial infarction. Psychother Psychosom. (1996) 65:327–30.
38. Bandelow B, Baldwin D, Abelli M, Altamura C, Dell'Osso B, Domschke K, et al. Biological markers for anxiety disorders, OCD and PTSD - a consensus statement. Part I: neuroimaging and genetics. World J Biol Psychiatry (2016) 17:321–65. doi: 10.1080/15622975.2016.1181783
39. Bandelow B, Baldwin D, Abelli M, Bolea-Alamanac B, Bourin M, Chamberlain SR, et al. Biological markers for anxiety disorders, OCD and PTSD: a consensus statement. Part II: neurochemistry, neurophysiology and neurocognition. World J Biol Psychiatry (2017) 18:162–214. doi: 10.1080/15622975.2016.1190867
Keywords: depressive symptoms, depression, anxiety, anxiety disorders, 10-year cardiovascular mortality risk, SCORE, Latvia
Citation: Ivanovs R, Kivite A, Ziedonis D, Mintale I, Vrublevska J and Rancans E (2018) Association of Depression and Anxiety With the 10-Year Risk of Cardiovascular Mortality in a Primary Care Population of Latvia Using the SCORE System. Front. Psychiatry 9:276. doi: 10.3389/fpsyt.2018.00276
Received: 01 April 2018; Accepted: 07 June 2018;
Published: 26 June 2018.
Edited by:
Jutta Lindert, University of Applied Sciences Emden Leer, GermanyReviewed by:
Peter Lepping, Bangor University, United KingdomAndreas Hoell, Zentralinstitut für Seelische Gesundheit (ZI), Germany
Copyright © 2018 Ivanovs, Kivite, Ziedonis, Mintale, Vrublevska and Rancans. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rolands Ivanovs, rolands.ivanovs@gmail.com
 Rolands Ivanovs
Rolands Ivanovs Anda Kivite2
Anda Kivite2 Elmars Rancans
Elmars Rancans