- 1Department of Gastroenterology, Wenzhou Central Hospital, Wenzhou, China
- 2School of Sports Science, Wenzhou Medical University, Wenzhou, China
- 3Sports Hospital Affiliated With Zhejiang College of Sports, Zhejiang College of Sports, Hangzhou, China
Purpose: This systematic review and meta-analysis was designed to evaluate the effects of acupuncture intervention on alleviating delayed onset of muscle soreness (DOMS) after intense exercise.
Method: Randomized controlled trials (RCTs) were searched from online databases including Medline (PubMed), Cochrane Library, Web of Science, Embase, PsycINFO, China Knowledge Resource Integrated Database (CNKI), and Wanfang (Chinese) up to April 2019. Data points were extracted from the eligible RCTs at the time points of 24, 48, and 72 h post strenuous exercise-induced DOMS. The outcomes of muscle soreness rating (MSR), creatine kinase (CK), and maximal isometric force (MIF) were pooled into the meta-analysis to assess the acupuncture intervention on DOMS.
Results: Six eligible RCTs were included in the meta-analysis, and the results showed that acupuncture intervention significantly decreased MSR [standardized mean difference (SMD) −0.49, 95%CI −0.73 to −0.24, P < 0.001, I2 = 34%] and the serum level of CK (SMD −0.91, 95%CI −1.27 to −0.56, P < 0.001, I2 = 30%), accompanied with the improvement of the muscle strength (MIF) (SMD 0.54, 95%CI 0.16 to 0.93, P = 0.006, I2 = 51%) after intense exercise. At the same time, the findings also revealed that acupuncture intervention had a long-lasting effect and tended to accumulate the effect size and that it had the most efficacy on alleviating DOMS at the time point of 72 h post exercise.
Conclusion: The current evidence indicates that acupuncture intervention after intense exercise could be effective for alleviating DOMS and improving muscle recovery. The long-lasting effect of acupuncture intervention on DOMS started from 24 h and would reach a peak on the time point of 72 h post exercise.
Introduction
It is well-established that delayed-onset muscle soreness (DOMS) will occur in both amateur and professional athletes who experience a high intensity of exercise (Lewis et al., 2012). DOMS is mainly caused by exhaustive or unaccustomed muscle work, especially of eccentric contractions (Bleakley et al., 2012; Lewis et al., 2012).
DOMS commonly occurs within the initial 24 h after strenuous or extreme exercises and reaches a peak between 24 and 72 h (Howatson and van Someren, 2008; Lewis et al., 2012), and it is frequently associated with muscle swelling and weakness and loss of motion range, leading to negative interference with daily activities and athletic performance or even increased risk of injuries (Cheung et al., 2003; Lavender and Nosaka, 2006; Kargarfard et al., 2016; De Marchi et al., 2017). Studies showed that the primary mechanical damage of muscle fibers during strenuous eccentric contractions or repetitive muscle work, accompanied with subsequent inflammation, caused DOMS (Proske and Morgan, 2001; Yu et al., 2002; Peake et al., 2005; Kanda et al., 2013; Kawamura et al., 2018). Zimmermann et al. (2012) found that exercise-induced DOMS activated widespread brain areas by fMRI, which also produces pain experience.
Numerous physiotherapeutic interventions such as cold-water immersion, massage, vibration, stretching, acupuncture, and electrotherapy were used to avoid or alleviate DOMS (Weerapong et al., 2005; Howatson et al., 2009; Bleakley et al., 2012; Costello et al., 2012; Hill et al., 2014; Jeon et al., 2015; Guo et al., 2017). As one of the traditional Chinese medicines, acupuncture has been proven effective in various musculoskeletal disorders including muscle soreness; thus, acupuncture therapy has been widely performed to improve the recovery of muscle-related injury and DOMS (Hubscher et al., 2008; Wand et al., 2013; Law et al., 2015). In traditional Chinese medicine theory, needling or acupuncture could activate the meridian and create a “de-qi” sensation, which accelerated the recovery of the symptoms of exercise-induced DOMS (Chang et al., 2019). In addition, the impact of acupuncture on extra segmental and central neuromodulation through local axon reflexes also explained the curative effect of acupuncture in Western countries (Chon and Lee, 2013). However, based on the up-to-date evidence, there is no consensus about acupuncture treatment on relieving DOMS and improving muscle recovery after intense exercise. Hubscher et al. (2008) discovered that needle acupuncture reduced muscle pain and increased muscle strength after exercise-induced DOMS, whereas other studies showed that acupuncture had no significant effect on improving the symptoms of DOMS (Barlas et al., 2000; Fleckenstein et al., 2016). Different types of acupuncture, such as using a laser or not, and different acupuncture points may result in inconsistent outcomes (Itoh et al., 2011; Fleckenstein et al., 2016).
O'Connor and Hurley (2003) systematic review investigated the effectiveness of many physiotherapy interventions (including acupuncture) on DOMS and found no evidence to support that acupuncture helped reduce DOMS, but there were only two trials included in the review. Recently, another systematic review based on more randomized controlled trial (RCTs) (which were not pooled into a meta-analysis) indicated that the therapeutic effect of acupuncture analgesia in DOMS is conflicting (Ko and Clarkson, 2019). Therefore, this systematic review and meta-analysis aimed to update the current evidence to evaluate the effects of acupuncture intervention on reducing DOMS and improving muscle performance after strenuous exercise.
Methods
The current systematic review and meta-analysis was conducted according to the Cochrane guidelines (Higgins et al., 2019).
Search Strategy
An electronic literature search for the relevant research articles which were published from January 1980 to May 2019 with no language restriction was conducted on the following online databases: Medline (PubMed), Cochrane Library, Web of Science, Embase, PsycINFO, China Knowledge Resource Integrated Database (CNKI), and Wanfang (Chinese). The keywords for searching are acupuncture, exercise, muscle pain, DOMS, and RCTs, and the details of the search strategy were provided in the Supplementary Data (S1).
Inclusion and Exclusion Criteria
Trials were included according to the following criteria: (a) only the studies were designed as RCTs; (b) participants should be healthy regardless of nationality; (c) the acupuncture intervention should be used after exercise for the recovery of the symptoms of DOMS; (d) the acupuncture intervention should be compared to control intervention (no intervention or placebo) regardless of any types of acupuncture; and (e) outcomes should cover muscle pain or soreness rating or maximal isometric force (MIF) or the serum creatine kinase (CK) level.
Trials were excluded according to the following criteria: (a) the data of mean and SD are inaccessible from the articles or the corresponding authors, and (b) the acupuncture intervention was used before exercise.
Trial Selection
The titles and abstracts of all the selected articles were reviewed by two reviewers (Huang CH and Wang ZP) independently for an initial scan, and then the full contents of the articles were carefully checked to assess whether the articles satisfied the inclusion criteria or not. In case of disagreement with trial selection, the two reviewers discussed with each other or consulted another reviewer (Chen X).
Quality Assessment
According to the Cochrane Collaboration recommendation (Higgins et al., 2019), all the included RCTs should be assessed with seven main risks of bias, including random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other biases. Two reviewers (Huang CH and Wang ZP) independently evaluated all the selected trials with three grades of biases (high or low or unclear), which were labeled by the Cochrane Collaboration tool (Revman Version 5.3, The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, 2014). Any disagreement was settled by discussion or a consultation with another reviewer (Chen X).
Then the GRADE scores of the pooled meta-analyses were evaluated according to the Cochrane guidelines (Higgins et al., 2019).
Data Extraction
All the data points were extracted by two reviewers (Huang CH and Wang ZP) independently from the eligible included trials, including study characteristics (the first author and publication year), participant characteristics (age and gender, groups, and number of participants), intervention descriptions, outcomes, and measurement time points. Then we extracted every trail's mean and SD for meta-analysis.
Statistical Analysis
Review Manager software (Revman Version 5.3, The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, 2014) was used to perform the meta-analysis. Standardized mean difference (SMD) was used to analyze the data points as the trials used different exercises to induce different muscle DOMS models and the scales for muscle soreness also vary between trials; P < 0.05 was considered to be a significant difference. The I2 statistic was used to evaluate the heterogeneity of the effects, and the I2 < 25, < 75, and > 25%, and ≥75% were considered as low, moderate, and high heterogeneity, respectively (Higgins et al., 2003). Meta-analysis was conducted when there are two or more outcomes from the trials by the random-effects model. Subgroups were performed to analyze the effectiveness of acupuncture on DOMS at different time points of 24, 48, and 72 h post strenuous exercise.
As the included articles are <9, funnel plot asymmetry was not used to evaluate the publication bias. Sensitivity analysis was used to assess the stability of results by removing each data point one by one. If the outcome showed the data of the mean and standard error (SEM), the standard deviation (SD) would be calculated as SD = SE × (n = sample size).
Results
Search Results
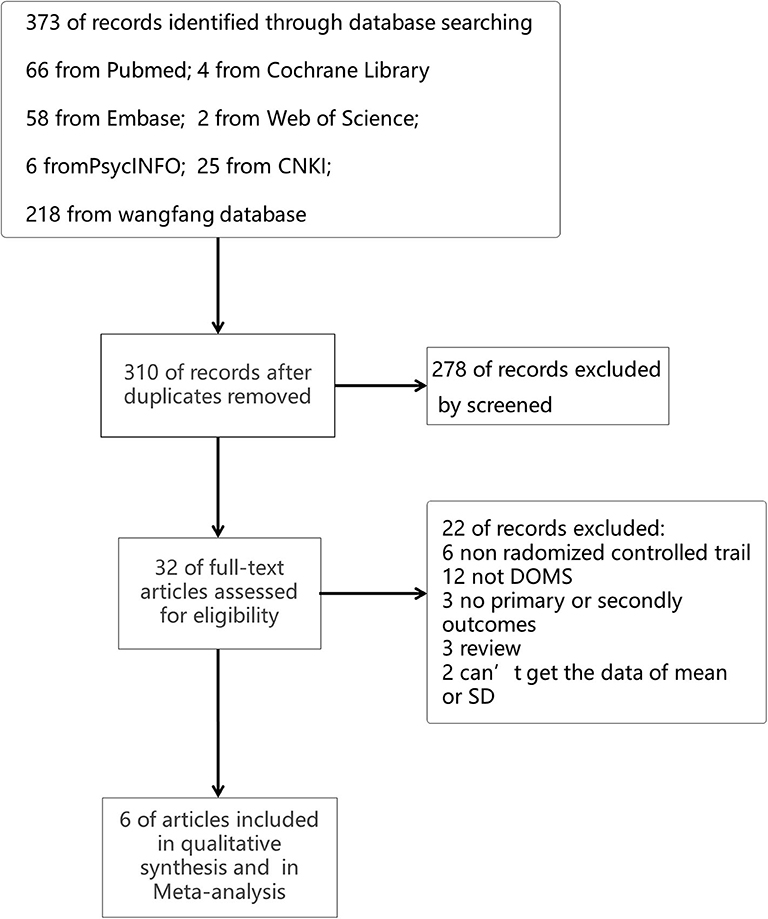
A total of 373 searching records were obtained from our initial online database search, and 32 potentially eligible trials were identified by reviewing the information of articles' titles and abstracts. After carefully reviewing the contents of all the 32 articles, six articles with 210 participants finally satisfied the inclusion criteria and were included in this meta-analysis. The process of identifying these trials from searching on databases is illustrated in Figure 1.
Description of Included Studies
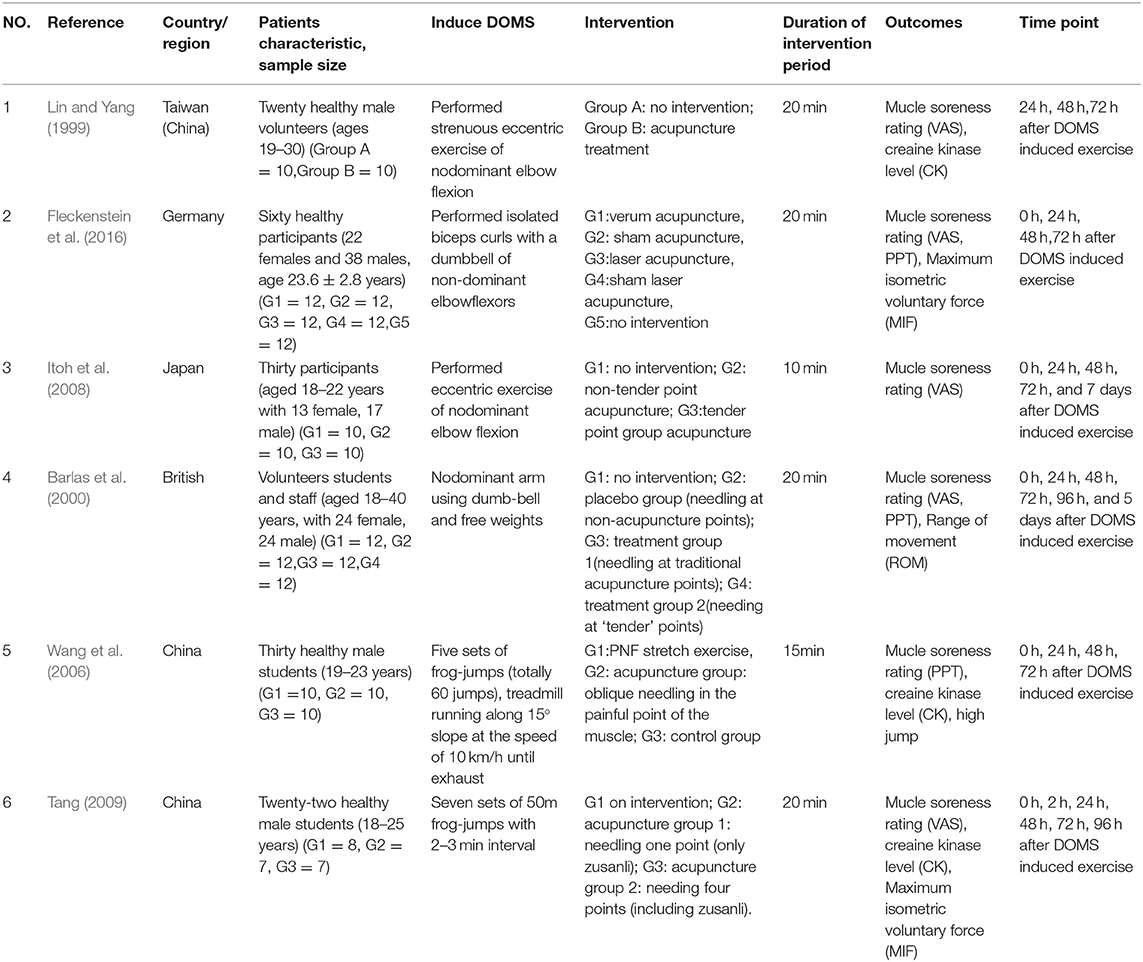
Six articles published from 1999 to 2016 were included in this meta-analysis (Lin and Yang, 1999; Barlas et al., 2000; Wang et al., 2006; Itoh et al., 2008; Tang, 2009; Fleckenstein et al., 2016), and the characteristics were shown in Table 1. Among these studies, four articles were published in English and two in Chinese. The publication countries were China (n = 3, 50%), Germany (n = 1, 16.7%), Japan (n = 1, 16.7%), and United Kingdom (n = 1, 16.7%). All participants included were healthy, aged from 18 to 40 years old with 151 males and 59 females.
Acupuncture and Control Intervention
All trials use the acupuncture intervention and needling acupuncture point (tender point or Ashi point), and one trial also added a third group using laser acupuncture. The duration of needles being retained in place ranged from 10 to 20 min. Half (three) trials twirled needles to manually provoke “de-qi” stimulation every 5 min.
All trials assigned no intervention (just sit for rest) for the control group. One trial added laser sham acupuncture group as the control for laser acupuncture.
Risk of Bias of Included Trials
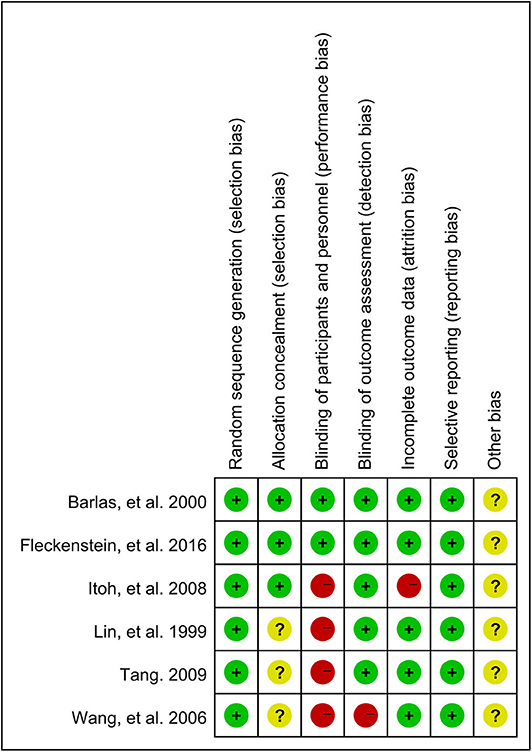
The risk of bias of the included trials was evaluated according to the recommendation by Higgins et al. (2011). All of the six articles used the randomization method, but only three of them reported the information about allocation concealment (50%). Only two studies (33.3%) used the blind method for participants as they set a group of placebo or sham acupuncture, which increased the risk of performance bias. Most of the trials (86.7%) masked their outcome assessors and showed the low risk of detection bias, as well as the low risk of attrition (86.7%) and reporting bias (100%). As funnel plot asymmetry was not applicable, publication bias was unclear. It was unclear whether the trials had other biases. The detail of the assessment of all the risks of bias was shown in Figure 2.
Effect of Acupuncture Intervention on Muscle Soreness Rating
As shown in Figure 3, 21 data points demonstrated that acupuncture intervention significantly alleviated muscle soreness rating (MSR) when compared with the control group (SMD −0.49, 95%CI −0.73 to −0.24, P < 0.001, I2 = 34%). Among these, the subgroups of 24 h (SMD −0.49, 95%CI −0.94 to −0.04, P = 0.03, I2 = 43%) and 72 h (SMD −0.63, 95%CI −0.97 to −0.29, P < 0.001, I2 = 0%) time points also showed that compared to that in the control group, MSR significantly decreased when the participants received acupuncture intervention. The subgroup of the 48 h time point illustrated no significant difference between acupuncture intervention and no intervention although acupuncture intervention showed a slight reduction trend of MSR (SMD −0.37, 95%CI −0.90 to 0.17, P = 0.18, I2 = 59%).
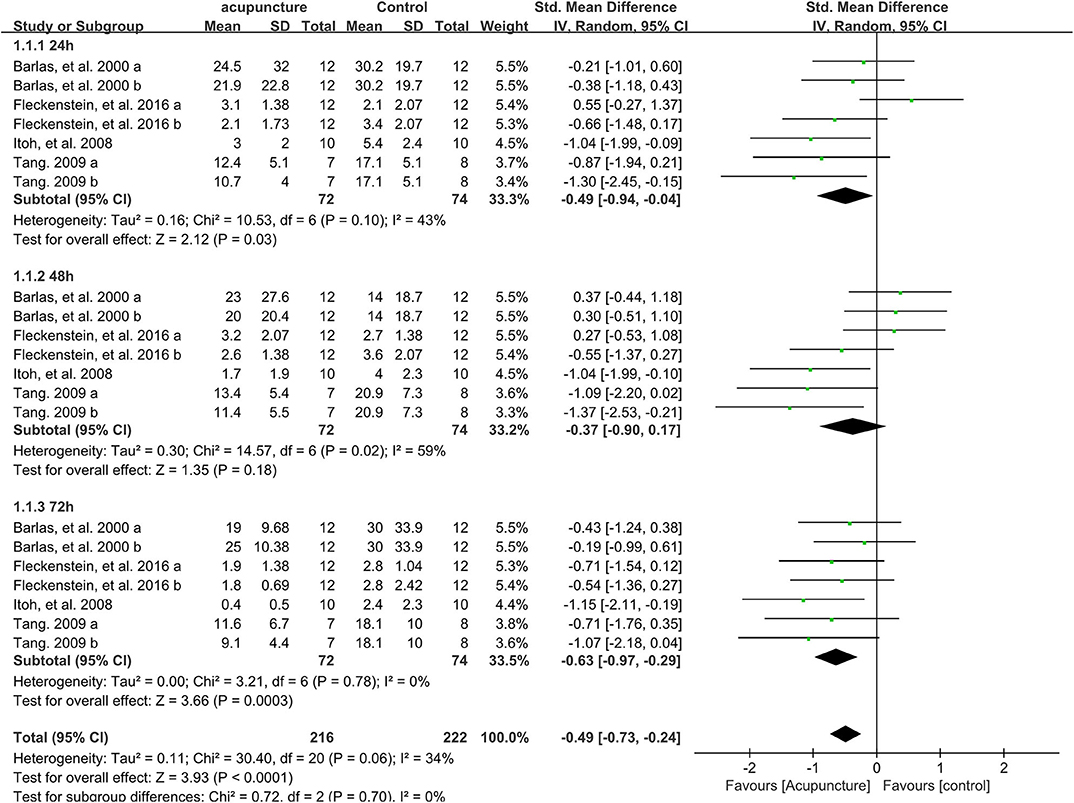
Figure 3. Meta-analysis of the effect of acupuncture intervention on MSR (divided three subgroups and the total effect). MSR, muscle soreness rating.
Sensitivity analysis of the MSR outcome revealed that the effect was stable when data points were removed one by one.
Effect of Acupuncture Intervention on the Pressure Pain Threshold
Eighteen data points compared the pressure pain threshold (PPT) between acupuncture and control groups after intense exercise; no significant difference was found in terms of the total effect based on the meta-analysis (SMD 0.08, 95%CI −0.27 to 0.43, P = 0.42, I2 = 66%) (Figure 4). Besides, all subgroups showed no significant difference on PPT after strenuous exercise whether the participants received the acupuncture intervention or not on the time points of 24 h (SMD 0.05, 95%CI −0.57 to 0.66, P = 0.88, I2 = 67%), 48 h (SMD −0.01, 95%CI −0.59 to 0.57, P = 0.97, I2 = 63%) or 72 h (SMD 0.21, 95%CI −0.53 to 0.94, P = 0.58, I2 = 76%) post exercise (Figure 4).
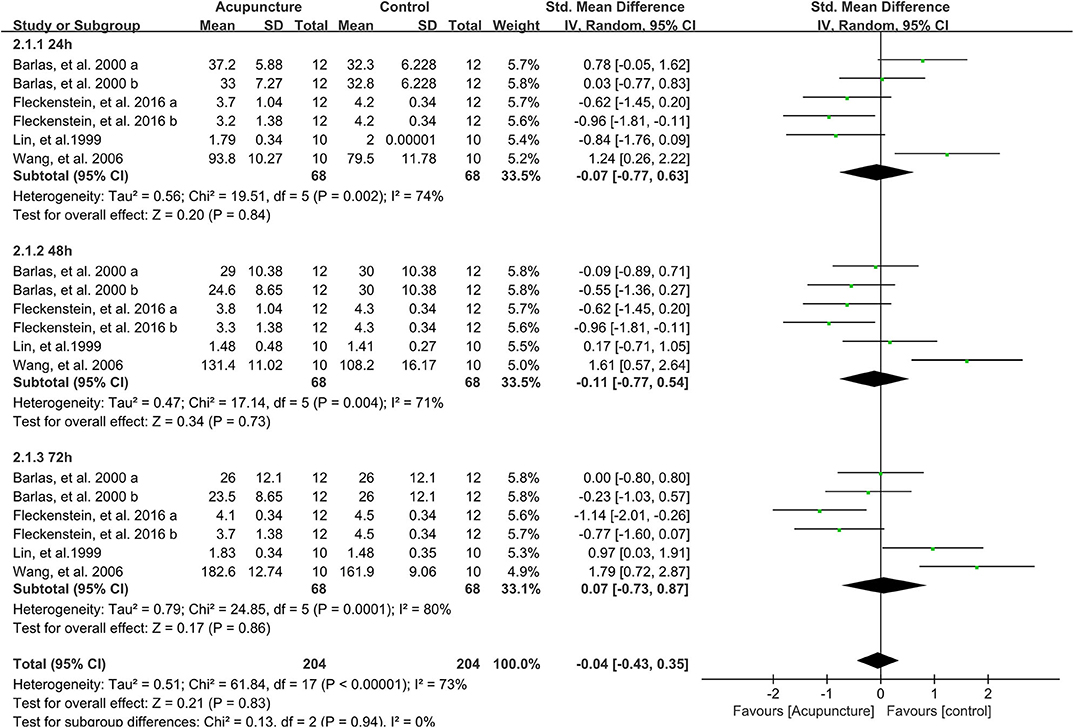
Figure 4. Meta-analysis of the effect of acupuncture intervention on PPT (divided into three subgroups and the total effect). PPT, pressure pain threshold.
Sensitivity analysis demonstrated that the results were stable when the data points were removed one by one.
Effect of Acupuncture Intervention on Serum Level of CK
As shown in Figure 5, four data points compared the effect of acupuncture intervention on the serum level of CK of the control group on the time points of 24, 48, and 72 h post strenuous exercise. The subgroup meta-analysis demonstrated that acupuncture intervention significantly decreased the serum level of CK on the time points of 24 h (SMD −0.99, 95%CI −1.83 to −0.16, P < 0.02, I2 = 61%), 48 h (SMD −0.92, 95%CI −1.45 to −0.38, P < 0.001, I2 = 10%), and 72 h (SMD −0.87, 95%CI −1.50 to −0.24, P < 0.007, I2 = 34%) after strenuous exercise. Consistent with the subgroup meta-analysis, the total effect of the 12 data points also revealed that acupuncture intervention could significantly decrease the serum level of CK after strenuous exercise (SMD −0.91, 95%CI −1.27 to −0.56, P < 0.001, I2 = 30%).
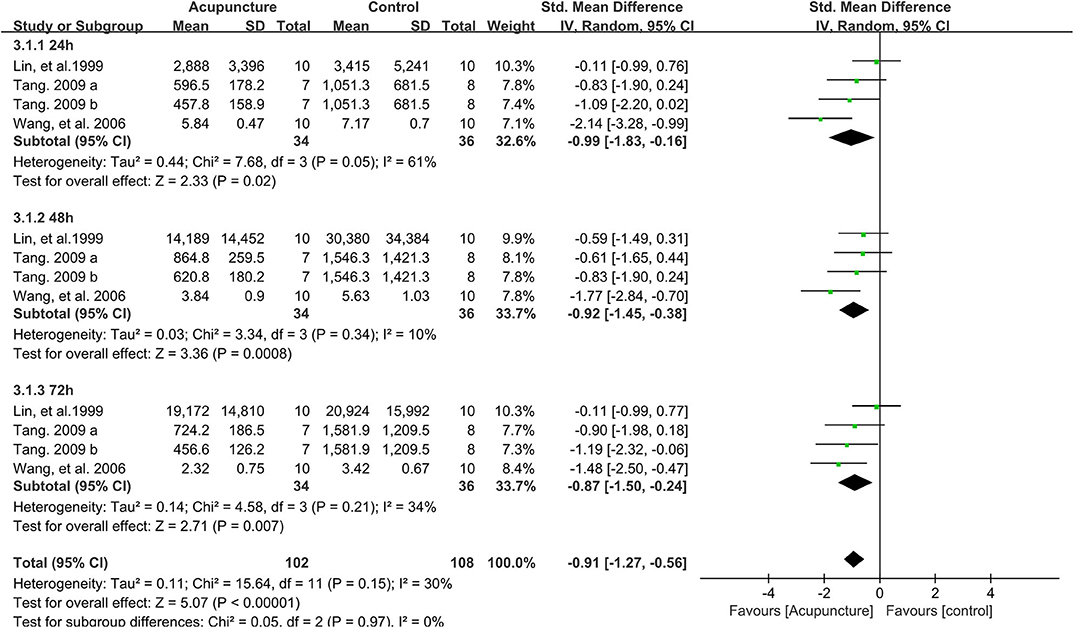
Figure 5. Meta-analysis of the effect of acupuncture intervention on the serum CK level (divided into three subgroups and the total effect). CK, creatine kinase.
Sensitivity analysis showed that the effect of acupuncture intervention on the serum level of CK was stable when the data points were removed one by one.
Effect of Acupuncture Intervention on the MIF
Four data points compared the performance of MIF between acupuncture and control groups on the time points of 24, 48, and 72 h after strenuous exercise. Based on subgroup meta-analysis, it was found that acupuncture intervention significantly improved the MIF performance only on the time point of 72 h (SMD 0.78, 95%CI −0.00 to 1.56, P = 0.05, I2 = 61%) post exercise, with a slight increase of MIF but no significant difference observed on the time points of 24 h (SMD 0.45, 95%CI −0.34 to 1.23, P = 0.26, I2 = 64%) or 48 h (SMD 0.42, 95%CI −0.18 to 1.02, P = 0.17, I2 = 40%) (Figure 6). However, the total effect of the 12 data points showed that acupuncture intervention significantly enhanced the MIF performance when compared to the control group (SMD 0.54, 95%CI 0.16 to 0.93, P = 0.006, I2 = 51%) (Figure 6).
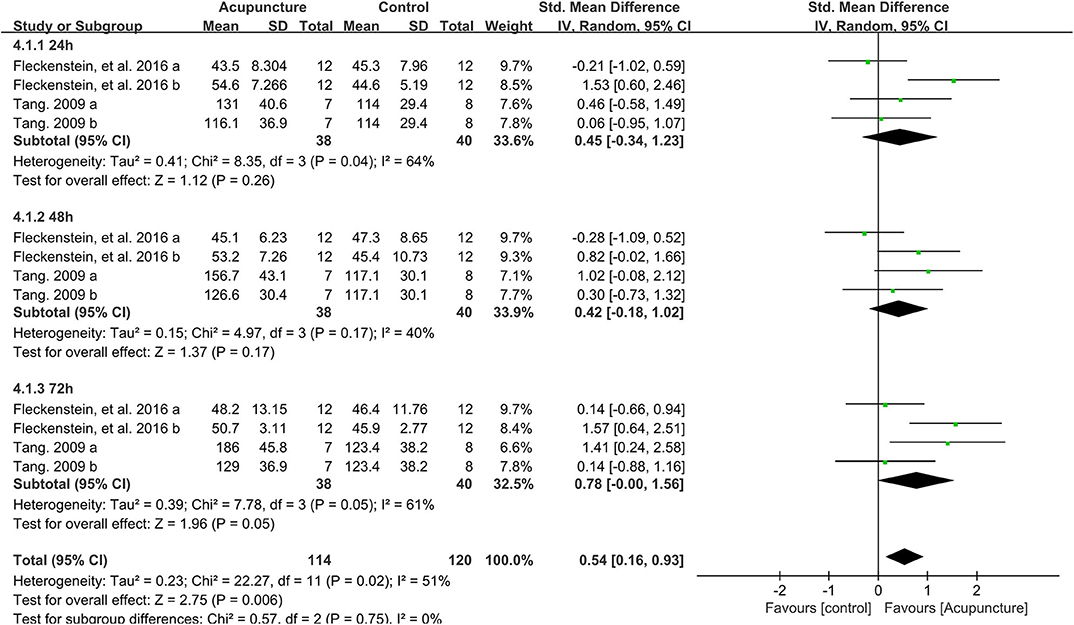
Figure 6. Meta-analysis of the effect of acupuncture intervention on MIF (divided into three subgroups and the total effect). MIF, maximal isometric force.
Sensitivity analysis revealed that the result of the total effect of acupuncture intervention on MIF was stable when the data points were removed one by one.
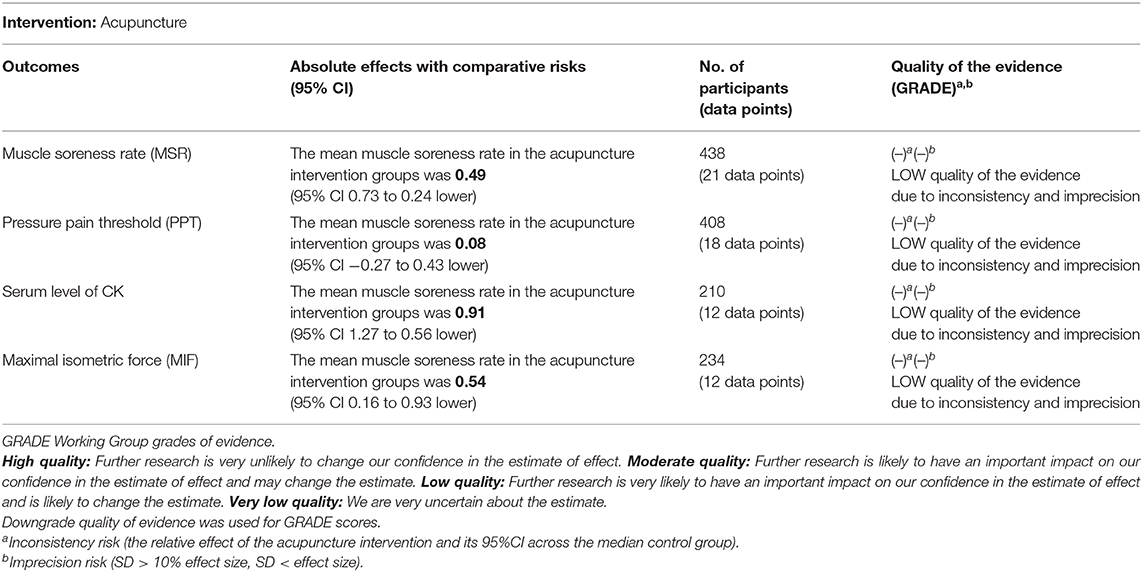
Result of GRADE Scores
The result of GRADE scores displayed that the qualities of evidence in the four outcomes of meta-analyses were low (Table 2). Inconsistency and imprecision were the main factors contributing to the low quality of evidence.
Adverse Events
All included trials did not state any adverse events.
Discussion
Exercise-induced muscle damage and soreness occur in both amateurs and professional athletes after strenuous exercise; thus, many studies have been focusing on reducing muscle soreness and increasing the recovery of muscle strength for the next event (Jakeman et al., 2010). In traditional Chinese medicine, massage, cupping, and acupuncture have been widely used in treating muscle pain and improving muscle recovery after exercise (Chen et al., 2016). Systematic reviews revealed that massage and cupping could be beneficial to muscle soreness and the performance of muscle strength after intense exercise (Guo et al., 2017; Bridgett et al., 2018). Animal studies suggested that acupuncture intervention helped to recover the reduction of perimysial junctional plate (PJP) number and the alteration of PJP domain homeostasis induced by eccentric training, leading to an increase of the muscle damage repair (Kong et al., 2017). Moreover, laser acupuncture also showed a beneficial effect as it reduced inflammation and myofascial pain in rats (Lorenzini et al., 2010). Nevertheless, there is still a lack of evidence to support these mechanisms in the human study, and the corresponding guidelines for medical practitioners remain elusive.
To address the conflicting results across various studies regarding the effect of acupuncture intervention on DOMS (Barlas et al., 2000; Hubscher et al., 2008; Fleckenstein et al., 2016), we have conducted this systematic review and meta-analysis to better understand the effectiveness of acupuncture intervention on DOMS and muscle strength recovery after exercise. The key findings demonstrated that participants receiving acupuncture intervention had experienced reduced muscle soreness after strenuous exercise. In addition, the results of a subgroup meta-analysis revealed that the beneficial effect of acupuncture intervention on alleviating muscle pain had more efficacy on the time points of 72 h (SMD −0.63) than 24 h (SMD −0.49) and 48 h post exercise, indicating that the effect of acupuncture on muscle pain tends to be long-lasting and accumulated peak at 72 h post intense exercise, which is consistent with Law et al. (2015) systematic review showing that laser acupuncture had a long-term effect on musculoskeletal pain. However, the results of PPT in this study show no significant difference between acupuncture therapy and the control group, indicating that the mechanisms of acupuncture therapy may vary in alleviating muscle pain and increasing PPT. Furthermore, the different types of acupuncture intervention may affect the effect size of PPT, because of the high heterogeneity of the PPT outcome and because the positive effects only come from two Chinese trials on the time point of 72 h post exercise (Lin and Yang, 1999; Wang et al., 2006).
It is now clear that the serum level of CK will increase rapidly and that muscle strength decreases when DOMS occurs because of the damage in the skeletal muscle and the subsequent inflammation after intense exercise (Clarkson and Sayers, 1999; Romagnoli et al., 2015; Muller et al., 2019). The current evidence showed that acupuncture intervention reduced the serum level of CK based on the total effect meta-analysis, as well as the subgroup effect on the time points of 24, 48, and 72 h post exercise-induced DOMS, indicating that acupuncture intervention could improve the recovery of muscle damage. This could be explained by the findings of Kong et al. (2017) and Wen et al. (2019) studies, which showed that acupuncture intervention could improve the recovery from muscle damage and inflammation. We also found that acupuncture intervention increased MIF after strenuous exercise when compared to the control intervention. Improved muscle damage recovery was thought to be one of the reasons that caused increased MIF, the reduction of muscle soreness might be another reason, and the benefit of acupuncture intervention on the reduction in serum inflammation mediators such as interleukin 6 (IL-6) and interleukin 8 (IL-8) may also contribute to muscle performance recovery (Li et al., 2015; Mo et al., 2017). Furthermore, the subgroup meta-analysis of the 72 h post exercise time point showed a significant increase of MIF, with no significant differences observed on the time points of 24 and 48 h after exercise. This result is consistent with the muscle soreness rating and the serum level of CK we have observed before, strengthening the evidence that acupuncture has a long-lasting effect on DOMS; the effect size accumulated peaked on the time point of 72 h post intense exercise.
Strengths and Limitations
The present study systematically reviewed the effect of acupuncture intervention on DOMS after strenuous exercise and pooled the RCTs into a meta-analysis, aiming to get a better understanding of the effect of acupuncture therapy on alleviating DOMS. Two reviewers searched and selected the trials independently, assessed the quality, extracted the data points, and pooled the trials into a meta-analysis according to the protocols and methodological schemes recommended, which strengthen the power of this meta-analysis. Different from Law et al. (2015) study, this study focused only on treating or preventing muscle pain induced by strenuous exercise (DOMS) but did not include other musculoskeletal disorders. The stability of the effects revealed by sensitivity analysis also strengthened the evidence that acupuncture intervention after exercise helps muscle recovery and alleviates DOMS. Moreover, based on the subgroup effect of different time points after intense exercise, this review discovered a long-lasting effect of acupuncture intervention on DOMS and revealed an accumulative effect.
However, there are some limitations in this present systematic review. First of all, the number of trials was relatively small; there are only eight articles that met the inclusion criteria, but we could not extract the mean and SD from two articles (Hubscher et al., 2008; Itoh et al., 2011) or by e-mailing the corresponding authors; thus, only six articles were pooled into the meta-analysis. More RCTs were needed for more evidence on assessing the effect of acupuncture on DOMS. Besides, the quality of the included articles is not high. Half trials did not detail any information on allocation concealment, and only two of them used sham acupuncture as a binding method for participants, which increased selection and performance bias. Selected trials contain varied acupuncture methods (dry needling or laser acupuncture) and acupuncture points (one point, four points, or just Ashi points), leading to the high heterogeneity. However, Chang et al. (2019) showed no significant difference between laser acupuncture and acupuncture intervention on DOMS, and the stability of total effects by sensitivity analyses also supports pooling the data points into a meta-analysis. Furthermore, the inconsistency and imprecision of the pooled meta-analyses also downgraded the quality of evidence in the results of the GRADE score. Finally, the publication bias could not be assessed by funnel plot asymmetry because the total included articles are <9.
Conclusion
The current evidence suggests that acupuncture intervention alleviates DOMS and improves muscle recovery as well as performance after strenuous exercise. To date, no adverse events have been recorded. This meta-analysis also demonstrated that the long-lasting effect of acupuncture intervention on DOMS started from 24 h and would reach a peak on the time point of 72 h post exercise. These findings may support the potential use of acupuncture intervention for sports or exercise practice. Nonetheless, we should be cautious when using the conclusion because of the outlined limitations in this systematic review.
Data Availability Statement
All datasets generated for this study are included in the article/Supplementary Material.
Author Contributions
XC and RZ designed this systematic review and supervised the whole program. CH and ZW reviewed all the trials and extracted the information and the data points. SH searched the articles from all the online databases. XX analyzed the data and prepared the figures and the table. CH and XC wrote the paper. All the authors reviewed and approved the manuscript.
Funding
This work was supported by Wenzhou public welfare science and technology plan project (Grant No. S20180028) and the Wenzhou Medical University Scientific Research Foundation for Talented Scholars (Grant No. QTJ19033).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank Dr. Heng Qiu for the English re-editing of this systematic review.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2020.00666/full#supplementary-material
References
Barlas, P., Robinson, J., Allen, J., and Baxter, G. D. (2000). Lack of effect of acupuncture upon signs and symptoms of delayed onset muscle soreness. Clin. Physiol. 20, 449–456. doi: 10.1046/j.1365-2281.2000.00280.x
Bleakley, C., McDonough, S., Gardner, E., Baxter, G. D., Hopkins, J. T., and Davison, G. W. (2012). Cold-water immersion (cryotherapy) for preventing and treating muscle soreness after exercise. Cochrane Database Syst. Rev. CD008262. doi: 10.1002/14651858.CD008262.pub2
Bridgett, R., Klose, P., Duffield, R., Mydock, S., and Lauche, R. (2018). Effects of cupping therapy in amateur and professional athletes: systematic review of randomized controlled trials. J. Altern. Complement. Med. 24, 208–219. doi: 10.1089/acm.2017.0191
Chang, W. D., Wu, J. H., Chang, N. J., Lee, C. L., and Chen, S. (2019). Effects of laser acupuncture on delayed onset muscle soreness of the biceps brachii muscle: a randomized controlled trial. Evid. Based Complement. Alternat. Med. 2019:6568976. doi: 10.1155/2019/6568976
Chen, D., Yang, G., Wang, F., and Qi, W. (2016). [Motion acupuncture for therapeutic target]. Zhongguo Zhen Jiu 36, 1177–1180. doi: 10.13703/j.0255-2930.2016.11.019
Cheung, K., Hume, P., and Maxwell, L. (2003). Delayed onset muscle soreness : treatment strategies and performance factors. Sports Med. 33, 145–164. doi: 10.2165/00007256-200333020-00005
Chon, T. Y., and Lee, M. C. (2013). Acupuncture. Mayo Clin. Proc. 88, 1141–1146. doi: 10.1016/j.mayocp.2013.06.009
Clarkson, P. M., and Sayers, S. P. (1999). Etiology of exercise-induced muscle damage. Can. J. Appl. Physiol. 24, 234–248. doi: 10.1139/h99-020
Costello, J. T., Algar, L. A., and Donnelly, A. E. (2012). Effects of whole-body cryotherapy (-110 degrees C) on proprioception and indices of muscle damage. Scand. J. Med. Sci. Sports 22, 190–198. doi: 10.1111/j.1600-0838.2011.01292.x
De Marchi, T., Schmitt, V. M., Danubia da Silva Fabro, C., da Silva, L. L., Sene, J., Tairova, O., et al. (2017). Phototherapy for improvement of performance and exercise recovery: comparison of 3 commercially available devices. J. Athl. Train. 52, 429–438. doi: 10.4085/1062-6050-52.2.09
Fleckenstein, J., Niederer, D., Auerbach, K., Bernhorster, M., Hubscher, M., Vogt, L., et al. (2016). No effect of acupuncture in the relief of delayed-onset muscle soreness: results of a randomized controlled trial. Clin. J. Sport Med. 26, 471–477. doi: 10.1097/JSM.0000000000000259
Guo, J., Li, L., Gong, Y., Zhu, R., Xu, J., Zou, J., et al. (2017). Massage alleviates delayed onset muscle soreness after strenuous exercise: a systematic review and meta-analysis. Front. Physiol. 8:747. doi: 10.3389/fphys.2017.00747
Higgins, J. P., Altman, D. G., Gotzsche, P. C., Juni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343:d5928. doi: 10.1136/bmj.d5928
Higgins, J. P., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., et al. (2019). (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (Updated July 2019). Cochrane. Available online at: www.training.cochrane.org/handbook
Higgins, J. P., Thompson, S. G., Deeks, J. J., and Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ 327, 557–560. doi: 10.1136/bmj.327.7414.557
Hill, J., Howatson, G., van Someren, K., Leeder, J., and Pedlar, C. (2014). Compression garments and recovery from exercise-induced muscle damage: a meta-analysis. Br. J. Sports Med. 48, 1340–1346. doi: 10.1136/bjsports-2013-092456
Howatson, G., Goodall, S., and van Someren, K. A. (2009). The influence of cold water immersions on adaptation following a single bout of damaging exercise. Eur. J. Appl. Physiol. 105, 615–621. doi: 10.1007/s00421-008-0941-1
Howatson, G., and van Someren, K. A. (2008). The prevention and treatment of exercise-induced muscle damage. Sports Med. 38, 483–503. doi: 10.2165/00007256-200838060-00004
Hubscher, M., Vogt, L., Bernhorster, M., Rosenhagen, A., and Banzer, W. (2008). Effects of acupuncture on symptoms and muscle function in delayed-onset muscle soreness. J. Altern. Complement. Med. 14, 1011–1016. doi: 10.1089/acm.2008.0173
Itoh, K., Minakawa, Y., and Kitakoji, H. (2011). Effect of acupuncture depth on muscle pain. Chin. Med. 6:24. doi: 10.1186/1749-8546-6-24
Itoh, K., Ochi, H., and Kitakoji, H. (2008). Effects of tender point acupuncture on delayed onset muscle soreness (DOMS)–a pragmatic trial. Chin. Med. 3:14. doi: 10.1186/1749-8546-3-14
Jakeman, J. R., Byrne, C., and Eston, R. G. (2010). Lower limb compression garment improves recovery from exercise-induced muscle damage in young, active females. Eur. J. Appl. Physiol. 109, 1137–1144. doi: 10.1007/s00421-010-1464-0
Jeon, H. S., Kang, S. Y., Park, J. H., and Lee, H. S. (2015). Effects of pulsed electromagnetic field therapy on delayed-onset muscle soreness in biceps brachii. Phys. Ther. Sport 16, 34–39. doi: 10.1016/j.ptsp.2014.02.006
Kanda, K., Sugama, K., Hayashida, H., Sakuma, J., Kawakami, Y., Miura, S., et al. (2013). Eccentric exercise-induced delayed-onset muscle soreness and changes in markers of muscle damage and inflammation. Exerc. Immunol. Rev 19, 72–85.
Kargarfard, M., Lam, E. T., Shariat, A., Shaw, I., Shaw, B. S., and Tamrin, S. B. (2016). Efficacy of massage on muscle soreness, perceived recovery, physiological restoration and physical performance in male bodybuilders. J. Sports Sci. 34, 959–965. doi: 10.1080/02640414.2015.1081264
Kawamura, T., Suzuki, K., Takahashi, M., Tomari, M., Hara, R., Gando, Y., et al. (2018). Involvement of neutrophil dynamics and function in exercise-induced muscle damage and delayed-onset muscle soreness: effect of hydrogen bath. Antioxidants (Basel) 7:127. doi: 10.3390/antiox7100127
Ko, G. W. Y., and Clarkson, C. (2019). The effectiveness of acupuncture for pain reduction in delayed-onset muscle soreness: a systematic review. Acupunct. Med. 38, 63–74. doi: 10.1177/0964528419887978
Kong, M., Zhang, X., Ye, M. L., and Zhang, X. L. (2017). Changes of perimysial junctional plates induced by excessive eccentric training and the effects of acupuncture intervention. Sheng Li Xue Bao 69, 17–32. doi: 10.13294/j.aps.2016.0104
Lavender, A. P., and Nosaka, K. (2006). Changes in fluctuation of isometric force following eccentric and concentric exercise of the elbow flexors. Eur. J. Appl. Physiol. 96, 235–240. doi: 10.1007/s00421-005-0069-5
Law, D., McDonough, S., Bleakley, C., Baxter, G. D., and Tumilty, S. (2015). Laser acupuncture for treating musculoskeletal pain: a systematic review with meta-analysis. J. Acupunct. Meridian Stud. 8, 2–16. doi: 10.1016/j.jams.2014.06.015
Lewis, P. B., Ruby, D., and Bush-Joseph, C. A. (2012). Muscle soreness and delayed-onset muscle soreness. Clin. Sports Med. 31, 255–262. doi: 10.1016/j.csm.2011.09.009
Li, J., Li, J., Chen, R., and Cai, G. (2015). Targeting NF-kappaBeta and TNF-alpha activation by electroacupuncture to suppress collagen-induced rheumatoid arthritis in model rats. Altern. Ther. Health Med. 21, 26–34.
Lin, J. G., and Yang, S. H. (1999). Effects of acupuncture on exercise-induced muscle soreness and serum creatine kinase activity. Am. J. Chin. Med. 27, 299–305. doi: 10.1142/S0192415X99000343
Lorenzini, L., Giuliani, A., Giardino, L., and Calza, L. (2010). Laser acupuncture for acute inflammatory, visceral and neuropathic pain relief: an experimental study in the laboratory rat. Res. Vet. Sci. 88, 159–165. doi: 10.1016/j.rvsc.2009.06.001
Mo, Y., Chen, S., Yang, L., Huang, L., Jin, D., Yu, Z., et al. (2017). The effect of transcutaneous electrical acupoint stimulation on inflammatory response in patients undergoing limb ischemia-reperfusion. Mediators Inflamm. 2017:8369737. doi: 10.1155/2017/8369737
Muller, E., Proller, P., Ferreira-Briza, F., Aglas, L., and Stoggl, T. (2019). Effectiveness of grounded sleeping on recovery after intensive eccentric muscle loading. Front. Physiol. 10:35. doi: 10.3389/fphys.2019.00035
O'Connor, R., and Hurley, D. A. (2003). The effectiveness of physiotherapeutic interventions in the management of delayed onset muscle soreness: a systematic review. Physical Therapy Rev. 8, 177–195. doi: 10.1179/108331903225003181
Peake, J., Nosaka, K., and Suzuki, K. (2005). Characterization of inflammatory responses to eccentric exercise in humans. Exerc. Immunol. Rev. 11, 64–85.
Proske, U., and Morgan, D. L. (2001). Muscle damage from eccentric exercise: mechanism, mechanical signs, adaptation and clinical applications. J. Physiol. 537, 333–345. doi: 10.1111/j.1469-7793.2001.00333.x
Romagnoli, M., Sanchis-Gomar, F., Alis, R., Risso-Ballester, J., Bosio, A., Graziani, R. L., et al. (2015). Changes in muscle damage, inflammation, and fatigue-related parameters in young elite soccer players after a match. J. Sports Med. Phys. Fitness. 56, 1198–1205.
Tang, H. (2009). The study of the curative effect of different acupuncture schemes on delayed onset muscle soreness (Master Degree Thesis), Capital University of Physical Education and Sports, Beijing, China.
Wand, B. M., Abbaszadeh, S., Smith, A. J., Catley, M. J., and Moseley, G. L. (2013). Acupuncture applied as a sensory discrimination training tool decreases movement-related pain in patients with chronic low back pain more than acupuncture alone: a randomised cross-over experiment. Br. J. Sports Med. 47, 1085–1089. doi: 10.1136/bjsports-2013-092949
Wang, X. D., Zhang, B. G., and Wang, A. L. (2006). Proprioceptive Neuromuscular Facilitation Stretching Versus Puncturing Ashi Point for Delayed-Onset Muscle Soreness in Triceps Surae. Liaoning: Zhongguo Linchuang Kangfu, 14–17.
Weerapong, P., Hume, P. A., and Kolt, G. S. (2005). The mechanisms of massage and effects on performance, muscle recovery and injury prevention. Sports Med. 35, 235–256. doi: 10.2165/00007256-200535030-00004
Wen, G. J., Liu, H., Chen, J., Zhang, S. F., Li, Y. K., and Zhou, S. G. (2019). Effect of warm acupuncture on pathological morphology and pain-induced inflammatory mediators in rats with myofascial pain trigger. Zhongguo Gu Shang 32, 260–264. doi: 10.3969/j.issn.1003-0034.2019.03.013
Yu, J. G., Malm, C., and Thornell, L. E. (2002). Eccentric contractions leading to DOMS do not cause loss of desmin nor fibre necrosis in human muscle. Histochem. Cell Biol. 118, 29–34. doi: 10.1007/s00418-002-0423-1
Keywords: acupuncture, exercise, delayed-onset muscle soreness (DOMS), systematic review, meta-analysis
Citation: Huang C, Wang Z, Xu X, Hu S, Zhu R and Chen X (2020) Does Acupuncture Benefit Delayed-Onset Muscle Soreness After Strenuous Exercise? A Systematic Review and Meta-Analysis. Front. Physiol. 11:666. doi: 10.3389/fphys.2020.00666
Received: 18 August 2019; Accepted: 25 May 2020;
Published: 17 July 2020.
Edited by:
Thomas Leonhard Stöggl, University of Salzburg, AustriaReviewed by:
Matthew J. Barnes, Massey University, New ZealandKatsuhiko Suzuki, Waseda University, Japan
Copyright © 2020 Huang, Wang, Xu, Hu, Zhu and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xi Chen, Y2hlbmFiMDA0JiN4MDAwNDA7MTI2LmNvbQ==; Rong Zhu, emh1cm9uZyYjeDAwMDQwO3dtdS5lZHUuY24=
†These authors have contributed equally to this work
 Chunwei Huang1,2†
Chunwei Huang1,2† Shuangshuang Hu
Shuangshuang Hu Rong Zhu
Rong Zhu Xi Chen
Xi Chen