- 1Department of Rehabilitation, School of International Medical Technology, Shanghai Sanda University, Shanghai, China
- 2Department of Rehabilitation, Shanghai General Hospital, Shanghai Jiao Tong University, Shanghai, China
- 3Department of Rehabilitation, Shanghai Fifth Rehabilitation Hospital, Shanghai, China
Background: There were limited studies on the effect of skin temperature and local blood flow using kinesio tape (KT) adhered to the skin in different taping methods. This study aimed to determine the short-term effect of KT and athletic tape (AT) on skin temperature in the lower back and explore the possible effect of different taping methods (Y-strip and fan-strip taping) on local microcirculation.
Materials and Methods: Twenty-six healthy participants completed the test-retest reliability measurement of the infrared thermography (IRT), intraclass correlation coefficient (ICC), and standard error of measurement (SEM) were calculated to evaluate the reliability. Then, 21 healthy participants received different taping condition randomly for 5 times, including Y-strip of kinesio taping (KY), fan-strip of kinesio taping (Kfan), Y-strip of athletic taping (AY), fan-strip of athletic taping (Afan), and no taping (NT). Above taping methods were applied to the participants’ erector spinae muscles on the same side. Skin temperature of range of interest (ROI) was measured in the taping area through IRT at pre taping and 10 min after taping. Additionally, participants completed self-perceived temperature evaluation for different taping methods through visual analog scaling. One-way repeated-measured analysis of variance was used to compare the temperature difference among different taping methods. Bonferroni test was used for post hoc analysis.
Results: There was a good test-retest reliability (ICC = 0.82, 95% CI = 0.60–0.92; SEM = 0.33; and MD = 0.91) of the IRT. Significant differences were observed in the short-term effect on skin temperature among all different taping methods (p = 0.012, F = 3.435, and ηp2 = 0.147), post hoc test showed a higher significantly skin temperature difference in Kfan taping compared to no taping (p = 0.026, 95% CI = 0.051–1.206); However, no significant differences were observed among self-perceived temperature (p = 0.055, F = 2.428, and ηp2 = 0.108).
Conclusion: This study showed that the fan-strip of KT increased significantly the skin temperature of the waist after taping for 10 min. The application of KT may modify the skin temperature of the human body and promote local microcirculation, although it remained unclear for the real application.
Introduction
Kinesio tape (KT) is an elastic adhesive skin tape, which has been reported to increase local blood and lymphatic flow, promote proprioceptive input, enhance muscle strength, suppress pain, improve stability, and improve range of motion (Ekiz et al., 2015; Stryker et al., 2016; Wozniak-Czekierda et al., 2017; Bischoff et al., 2018; Kasawara et al., 2018; Gulpinar et al., 2019). It differs from traditional athletic tape (AT) which is an inelastic adhesive skin tape that functions to provide fixed protection (Kase et al., 2003; De Ridder et al., 2015). In clinical application, KT is generally cut into I-strip, O-strip, X-strip, Y-strip, or fan-strip for different functions according to the characteristics of human body joint and muscle shapes. Among with them, I-strip, and O-strip were used commonly to provide stability for muscles and fascia according to the anatomical structures, X-strip was used to relieve pain owing to the effect of lifting skin, Y-strip, and fan-strip were used commonly to eliminate swelling and promote lymphatic circumfluence because of the tails (Kumbrink, 2012; Chen and Yu, 2017; Vercelli et al., 2017). However, the quantitative and reliable taping standard for reducing swelling has not been established in previous studies.
Currently, there was limited research exploring the effect of KT on local circulation and swelling relief (Kalron and Bar-Sela, 2013). Additionally, the related mechanism of KT reported in these studies are contradictory. Vercelli et al. (2017) reported that KT improved blood and lymphatic reflux through the formation of skin wrinkles which increased the gap between the skin and the underlying connective tissue, which is useful for the treatment of lymphedema, venous insufficiency, swelling, and superficial hematoma. However, another study reported that KT could promote lymphatic reflux and reduce swelling due to pressurized bandaging effect (Aguilar-Ferrandiz et al., 2014).
Numerous literatures have indicated that the local microcirculation was related closely with skin temperature (Tauchmannova et al., 1993; Ng, 2009; Gomes Moreira et al., 2017). Changes in blood flow reflected from vasoconstriction and vasodilation can result in fluctuations in skin temperature, and vice versa (Taylor et al., 1984; Pergola et al., 1993). More recently, studies have focused on the effect of KT in terms of skin temperature changes in order to seek the evidence of KT promoting circulation from the perspective of skin temperature. Slomka et al. (2018) reported that the skin temperature from infrared thermography (IRT) decreased immediately on removal and then increased significantly after I-strip taping continuously for 4 days. Similarly, Windisch et al. (2017) found that the skin temperature of the wound site in fan-strip group was higher significantly than in control group after the total knee replacement. However, inconsistent with above research, Yang and Lee (2018) indicated that the skin temperature decreased immediately after I-strip taping in the region of interest (ROI) through IRT. Therefore, there was of great contradictory in the research which explored the effect of KT on local skin temperature and related mechanism was required to be verified. In addition, although IRT was used to measure skin temperature in these studies, they did not report instrument-related test-retest reliability.
Infrared thermography which analyzes the changes and distribution of skin temperature by detecting infrared radiation emitted from the body, has been proved to be a safe, convenient, non-invasive, and painless detection method for body temperature. It plays an important role of detecting whether the surface temperature changes symmetrically (Jones et al., 2005). Therefore, it has been used widely in skin temperature changes before and after physical therapy interventions (Sefton et al., 2010; Holey et al., 2011; Roy et al., 2013; Magalhães et al., 2015).
Therefore, this study aimed to investigate the test-retest reliability of infrared thermal imaging measurement and the effect of different taping methods on local skin temperature through IRT. We hypothesized that the skin temperature would increase after fan-strip and Y strip of kinesio taping.
Materials and Methods
Participants
Considering a power of 0.80, a level of 0.05 in repeated measures analysis of variance, a minimum of 20 participants would be required. Finally, a total of 21 participants were recruited from local university. They were included if they: (1) Were healthy adult college students; (2) Had no history of spinal musculoskeletal (including sacroiliac) or neurosurgical injuries within the past 3 months; (3) Had not received medication in the past 3 months; (4) Had no knowledge of KT; and (5) Had intact skin over the back region and a bilateral skin temperature difference of <0.5°C prior to taping. Participants who were less than 18 years old, had a BMI > 24, had a tattoo or scar located on the back, had sustained a back injury 3 months prior to data collection, had lumbago symptoms or lumbar or sacroiliac joint lesions, were menstruating, had allergy to KT, and declined to provide a signed informed consent were excluded. The baseline characteristics of the participants are shown in Table 1.
All participants were instructed to read and sign the inform consent. This study was approved by the Ethics committee of Shanghai University of Sport. (no. 2018071).
Experimental Protocol
Laboratory Preparation
In an independent confined space of 18 square meters without any light and electronic or metal devices, an ultrafine fiber black cloth was used as a background for the whole room to absorb and reduce thermal infrared reflection. Only the researcher and participant were permitted to enter. The indoor temperature was adjusted to 24.5 ± 0.5°C, The indoor humidity was controlled at 40% (Sillero Quintana et al., 2015; Slomka et al., 2018). In addition, we also monitored the indoor atmospheric pressure and body temperature changes of the participants.
Participant Preparation
Participants were required to (1) refrain from any physical activity, cigarette smoking, drinking coffee, alcoholic beverages, or other stimulants for at least 24 h prior to the measurements; (2) avoid applying creams, gels, cosmetics, deodorants, or antiperspirants on the skin of the lower back region; (3) avoid direct sunlight, ultraviolet radiation, or thermal radiation prior to measurement; (4) avoid any treatment (including medication), any forms of massage, taking a shower, or bath before measurement; and (5) maintain their usual work, rest, and eating habits (Sillero Quintana et al., 2015).
Reliability Measurement
To investigate the reliability of IRT, a total of 28 participants were recruited to take part in the skin temperature measurement of the IRT, and finally 26 participants completed it. In the process, all participants received two temperature measurements without any intervention at the same time on day 1 and day 8, respectively. The location of measurement was consistent with ROI which was mentioned below. The inter-rater reliability was determined by correlation coefficient (ICC) to represent the relative measurement of reliability, and the standard error of measurement (SEM) of the two measurement of skin temperature was to represent the absolute measurement of reliability (Weir, 2005). The SEM and minimal difference (MD) calculation formula are as follows:
The SDd means the standard deviation of the difference in the two measurement of skin temperature.
Taping Procedures
Kinesio Tex Gold (5 cm × 5 m, United States; Matheus et al., 2017) and AT with the same specification were used in this study. Prior to taping, the taping area should be removed hair, and wiped with alcohol. Each participant then received five different taping conditions, including no taping (NT), Y-strip of Kinesio Taping (KY), fan-strip of Kinesio Taping (Kfan), Y-strip of Athletic Taping (AY), and fan-strip of Athletic Taping (Afan; Figure 1). The tape was applied by a KT-certified therapist who was not informed of the purpose of the experiment and the participants were unaware about the effect of taping. Owing to the repeated-measures design, incomplete counterbalanced method was used for the randomization of taping order. Two balanced Latin Square was constructed. In the first Latin Square, the first row followed the formula 1, 2, n, 3, n-1, 4, n-2…, where n was the serial number of tapping conditions. For subsequent rows, added one to the value corresponding to the previous line, returning to 1 after n. The second Latin Square was a mirror image of the first Latin Square (Supplementary Material 1). This randomization method ensured to pick out any carryover effects during the statistical analysis. A week of wash-out phase between each taping conditions was to limit any learning effect. For example, the participant received first random taping condition at Monday, then second random taping condition would be performed in next Monday, and so on. According to the proportional distribution law of KT tension, Y-strip is divided equally into two tails, and the fan-strip is divided equally into four tails (Yu et al., 2016). When applying the taping, the participants stood in an anatomical position, bending forward, kept their legs straight, touched the back of their feet with their middle finger to extend their lower back, the posterior superior iliac spine was used as the location to anchor the tape, and KT was extended up to the right L1–L5 erector spinal region. According to the KT user manual, the tension of tape was approximately 10–15% (Kase et al., 2003; Figure 1). Except from different cutting shapes, the length and coverage area of different taping methods are ensured to be consistent.
Figure 1. Different taping methods with Kinesio Tape and Athletic Tape. (a) Y-strip of kinesio taping; (b) Y-strip of athletic taping; (c) fan-strip of kinesio taping; and (d) fan-strip of athletic taping.
IRT Measurement
A Spectrum 9000 MB series digital infrared thermal imaging system (United Integrated Services Co, Ltd, New Taipei, Taiwan, China) was used for measurement and imaging. IASNET2 software was used for infrared measurement and analysis. The spectral sensitivity was 7–14 μm, the minimum analytical temperature difference was 0.05 ∼ 0.08°C, the accuracy of reading value was <0.3°C, the stability of reading value was <0.3°C, the accuracy of this system was 0.1°C, and the temperature measurement range was between 10°C and 40°C (Supplementary Material 2). Infrared sensors (IRSensor Type) were used for the microbolometer, the optimal resolution was 1024 × 768, and the skin emissivity assumption was 0.98.
Before measurement, participant was instructed to sit quietly, with their lower back exposed for 15 min to adapt to the room environment and achieve thermal balance (Fernández-Cuevas et al., 2015; Moreira et al., 2017). During measurement, participant stood with his/her back to the infrared thermal meter in the anatomical position, standing 1.5 meters in front of the infrared camera with arms and hands outstretched. The camera height was adjusted to be perpendicular to the ROI to avoid parallax. It has been reported that the skin blood flow would react and tend to be stable within 10 min after application of KT (Kase and Hashimoto, 1998). Therefore, the skin temperature change was measured at prior to taping (T0) and 10 min after taping (T1) through infrared thermal imaging. During the 10-min application, the participants stood with their back against the infrared thermal camera. Measurements were performed at the time of each taping between 10:00 am and 12:00 am.
Selection of ROI
Region of interest located at the site of erector spinae which not covered by taping, distanced vertically 5–6 cm away from axis of spine, and paralleled to the axis. In order to ensure that the ROI of each taping condition was consistent, since the width of tape were 5 cm, and Y-strip tape was cut equally into two tails with 2.5 cm width in each tail while fan-strip was cut equally into four tails with 1.25 cm width in each tail. The end point of the tail closest to the spine is about 1.5 cm vertically from the spine and the tails were taped in equal distribution. In this way, the width of the exposed skin area between the end point of each tail of Y-strip is about 3 cm, while the width of the exposed skin area between the end point of each tail of fan-strip is about 1 cm. Therefore, the exposed skin area ROI between the 2–3th end point of the fan-strip could coincide with the exposed skin area ROI between the two end points of the Y-strip, ROI of both were about 5–6 cm away from the axis of spine (Figure 2).
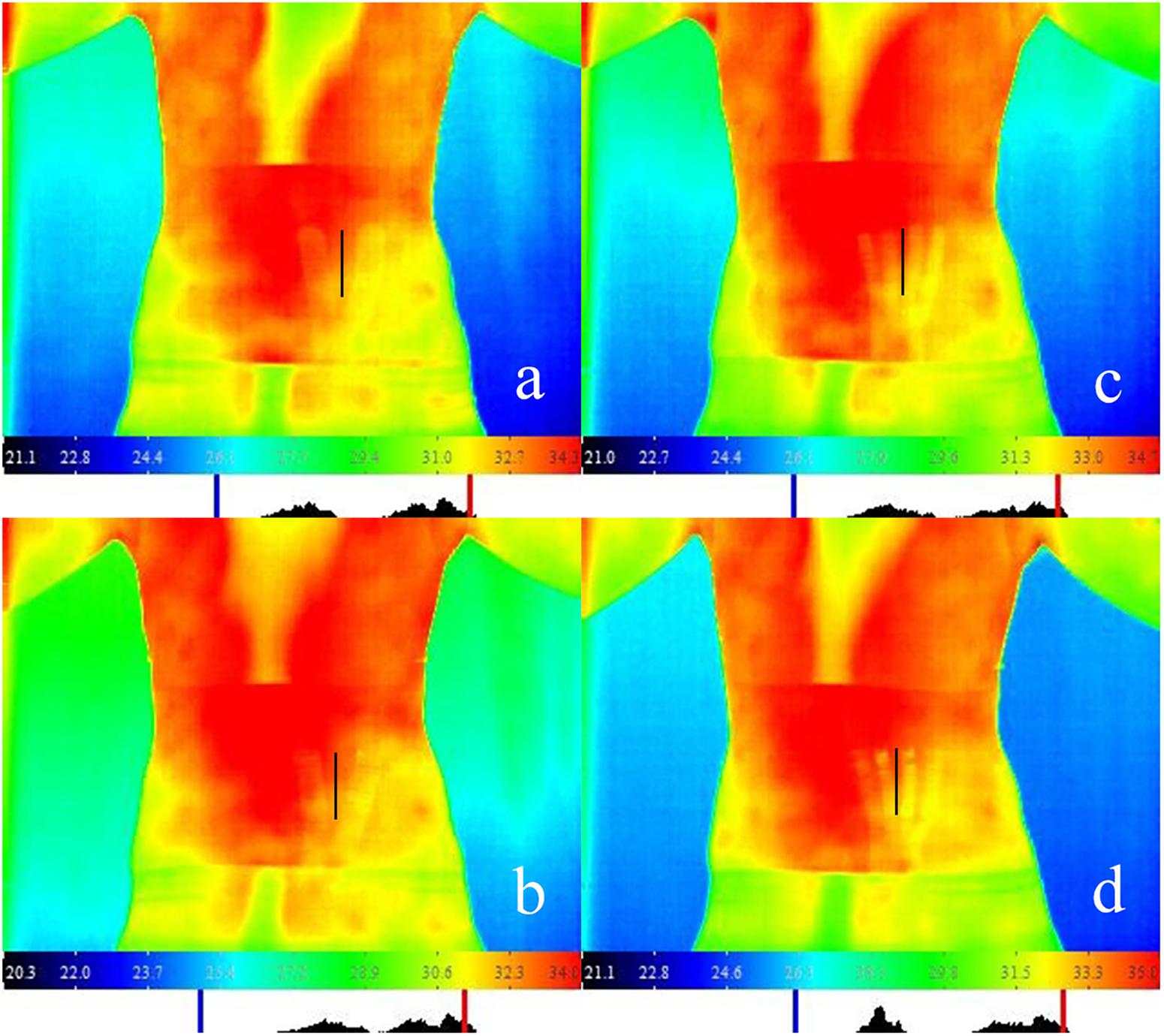
Figure 2. IRT measurement scenario for different taping methods with Kinesio Tape and Athletic Tape. (a) Y-strip of kinesio taping; (b) Y-strip of athletic taping; (c) fan-strip of kinesio taping; and (d) fan-strip of athletic taping. Note: In the infrared thermal image, the black line areas represent the region of interest (ROI).
Self-Perceived Temperature
Finally, participants were required to describe the degree of self-perceived temperature change of the waist after 10 min for various methods of taping, and complete the visual analog scaling. 5 points means “perceived temperature has no change,” 0 points means “significant decrease in self-perceived temperature,” and 10 points means “significant increase in self-perceived temperature.”
Statistical Analysis
The quantitative data conformed to normal distribution and was presented as mean ± standard deviation ( ± s). ICC was interpreted as follows: ICC values range > 0.9 excellent reliability, 0.75–0.9 good reliability, 0.5–0.75 moderate reliability, and <0.5 poor reliability. One-way repeated-measured analysis of variance was used to determine whether there was a significant difference among parameters of KY, Kfan, AY, Afan, and NT on the waist short-term skin temperature. Bonferroni test was used for post hoc analysis, the significance level was set at p < 0.05. Moreover, 95% confidence interval (CI) was determined, and the effect size was expressed as ηp2. Small effect with 0.01 ≤ ηp2 < 0.06, moderate effect with 0.06 ≤ ηp2 < 0.14, and large effect with ηp2 ≥ 0.14. All statistics were performed with IBM SPSS software (Version 19.0, Chicago, IL, United States).
Results
Table 2 shows the mean value and SDd of the test-retest data for skin temperature measurements in the ROI with the infrared thermal imaging system. The inter-rater agreement for skin temperature measurement in ROI was good (ICC = 0.82, 95% CI = 0.60–0.92; SEM = 0.33; and MD = 0.91). (Table 2).
There was no significant difference among the room temperature (p = 0.329, F = 1.152, and ηp2 = 0.054), humidity (p = 0.453, F = 0.837, and ηp2 = 0.040), and air pressure of the laboratory (p = 0.142, F = 2.060, and ηp2 = 0.093), and participants’ body temperature (p = 0.891, F = 0.143, and ηp2 = 0.007) for different taping methods (Table 3).
Significant differences were observed in the short-term effect on skin temperature for different taping methods (p = 0.012, F = 3.435, and ηp2 = 0.147); post hoc test showed a significantly higher skin temperature difference in Kfan taping compared to that of no taping (p = 0.026, 95% CI = 0.051–1.206). (Table 4 and Figure 3).

Table 4. Comparison of skin temperature and self-perceived temperature for different taping methods ( ± s).
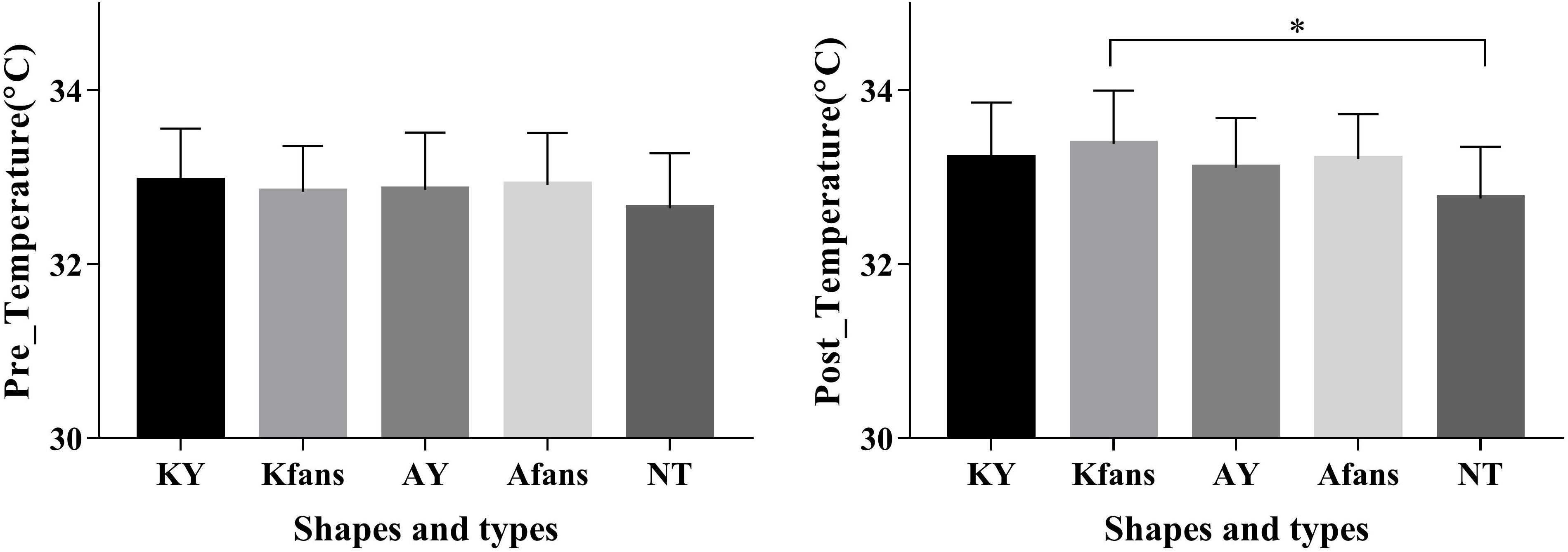
Figure 3. Comparison of skin temperature at post-taping for different taping methods ( ± s). Note: ∗Significant difference between groups, p < 0.05.
Additionally, the self-perceived temperature of Kfan is higher than other taping conditions, although there was no significant difference among different taping methods (p = 0.055, F = 2.428, and ηp2 = 0.108). (Table 4).
Discussion
To our knowledge, this was the first study to explore the effect of different taping methods on local skin temperature. Our measurement demonstrated that infrared thermal imaging system exhibit good test-retest agreement in skin temperature of healthy participants. In addition, our results showed that different taping methods could increase the local skin temperature significantly at the waist after taping for 10 min. The skin temperature of the fan-strip of KY was significantly higher than no taping condition, although it remained unclear for the real application.
Reliability Measurement
This study measured the reliability of the infrared thermal instrument and calculated ICC, SEM, and MD. Compared with ICC which is dimensionless, the SEM is interpretable in the units of variables to evaluate the reliability. The infrared thermal imaging system showed good test-retest agreement based on SEM (0.33°C) and ICC (0.82). As for the MD (0.91°C), this value means that only if the temperature difference between two measurements is greater than or equal to 0.91°C, the change is real at the 95% level (Weir, 2005). However, the MD exceeded the temperature differences that we observed in all the interventions, making the clinical application of KY questionable, despite a respectable SEM. Since our participants were healthy young adults, perhaps larger changes could be observed in the affected population.
Effect of Taping on Skin Temperature
This findings showed that fan-strip of KY had a significant effect on local skin temperature, which is consistent with previous studies. Slomka et al. (2018) reported that after taping for 4 days, the skin temperature decreased immediately on removal and then increased significantly. This result indicated that KT had a significant effect on local skin temperature changes. Similarly, Windisch et al. (2017) found the skin temperature at the wound site of KT group was higher significantly than control group and concluded that KT contributed to a reduction of swelling after total knee replacement. Conversely, Yang and Lee (2018) indicated that the skin temperature decreased immediately after taping in the ROI. However, they did not describe clearly the ROI of infrared measurement. The ROI temperature measured in our study was only the skin temperature around the tape and did not include skin covered by the tape. The coverage of the tape has an influence on measured skin temperature, which may be the main reason for differences in the results of our study. Skin temperature changes in the area covered by the tape were not reported considering that the tape covering might play a role in insulating the skin of the covered area. Therefore, only the temperature of the skin exposed between the tape and the tape coverage edge were reported in this study. It is suggested determining the emissivity of the tape to better interpret the skin temperature data under the coverage in future research.
The skin is the largest sensory organ of the human body and contains a large number of heat receptors, such as transient receptors and potential receptors (Romanovsky, 2014). Skin vessels activate vasodilation during local warming (Johnson et al., 2014), and animal studies have shown that the intrinsic contractility of lymphatic vessels and lymphatic vessel flow are affected due to temperature regulation (Solari et al., 2017). Our results showed that KT increased significantly local skin temperature in the short-term, with an average increase of 0.56°C in the fan-strip of KY, which created a temporary warming environment to these body parts. Local thermal stimulation has been reported to enhance endothelial cell secretion of nitric oxide (NO) and other substances, and NO participates in the induction of smooth muscle relaxation or vasodilation, thereby increasing local circulation flow (Kellogg et al., 2009).
Previous study showed that when the temperature difference between external and internal (test environment) was less than 5°C, thermal balance could be obtained within a 10-min adaptation period (Marins et al., 2014). Two other studies suggested that the minimum adaptation period should be 15 min (Fernández-Cuevas et al., 2015; Moreira et al., 2017). Therefore, we chose a 15-min adaptation period as the time interval before infrared thermal measurement to exclude the interference of temperature change factors.
Effect of Taping on Local Circulation
Several studies have confirmed the clinical effect of KT in improving local circulation (Aguilar-Ferrandiz et al., 2014; Vercelli et al., 2017; Windisch et al., 2017; Tantawy et al., 2019). In this study, when participants returned to an upright posture from bending forward, small folds of uniform density were formed in the taping area with KT. Kase et al. (2003) suggested that KT could increase the subcutaneous space, reduce the pressure of pain receptors in tissues, accelerate blood and lymph circulation, and ultimately reduce pain. In subcutaneous tissues, the capillary plexus is located approximately 0.3–0.7 mm below the skin surface, and the capillary network formed extends upward approximately between 0.04 mm and 0.08 mm beneath the skin (Swain and Grant, 1989). Yu et al. (2016) found that KT with natural tension applied to the skin would increase the subcutaneous gap by approximately 0.2 mm. This suggested that the folds produced by KT increased the circulatory space of the subcutaneous capillary network, thereby increasing its blood flow. Therefore, in this study, the application of KT may provide more subcutaneous space and acquire the potential to promote the flow of local microcirculation.
The mechanical load exerted by KT on the skin has been reported to produce extensive heterogeneous deformation (Alexander et al., 2008; Pamuk and Yucesoy, 2015), which forms a certain shear stress within the subcutaneous tissues and the extracellular matrix and between the continuity of connective tissue and muscle fibers (Berthier and Blaineau, 1997; Yucesoy et al., 2003; Huijing, 2009), and allowing the transmission of force between the myofascial membranes (Yucesoy and Huijing, 2007; Yucesoy, 2010). The increased shear stress in the blood vessel wall may increase mechanical stimulation of blood vessels, thereby inducing the secretion of NO, which has a strong vasodilator effect and an important role in increasing blood flow and promoting local microcirculation (Buga et al., 1991; Paniagua et al., 2001). It was reported that the increase in local blood flow has been reported to promote an increase in skin temperature (Tauchmannova et al., 1993; Ng, 2009; Gomes Moreira et al., 2017). That may be the underlying reason for the increase of skin temperature observed in our study.
Effect of Different Taping Methods on Skin Temperature
We found there was a short-term skin temperature increase using the fan-strip KT method, which was higher significantly than that of no taping. Yu et al. (2016) showed that the subcutaneous gap generated of KT was related to a recoiling force, and this recoiling force was not the same when using different methods of KT application. In this study, due to the proportional distribution of KT tension, we selected the strip of Y and fan taping which were used commonly in clinic. The fan-strip of KT skin temperature was higher significantly than the no taping in the short-term, which is consistent with Yu et al. (2016) findings showing that the recoiling force of the corresponding shape of the taping is approximately proportional to its area and distribution. Fan-strip of KT generates wider range of skin folds (subcutaneous gaps) and elastic recoil force on the skin. This may be one of the main reasons for temperature change in the skin near fan-strip KT.
Vercelli et al. (2017) applied the fan-strip of KT as a form of treatment for postoperative swelling and reported that KT did not change significantly the color intensity of the central area of taping but showed significant therapeutic effect at the edge of the KT, which suggested that the efficacy of KT may related to the formation of a pressure gradient between KT and adjacent area. Pamuk and Yucesoy (2015) used magnetic resonance imaging (MRI) analysis to evaluate local tissue deformation that occurred immediately after KT application and considered that KT promoted lymphatic drainage not only through lifting the skin but also through compressing the skin, which may depend on the pressure gradient in the tissue. The pressure gradient of KT generated from the skin is only distributed at the peripheral edges, and the pressure gradient of fan-strip KT was several multiples of no taping and Y-strip KT. Therefore, fan strip of KT was estimated theoretically to promote local blood flow more quickly and effectively, thereby changing the local skin temperature.
Effects of Two Different Fan-Strip Materials on Skin Temperature
Previous studies have shown that the skin surface temperature is closely related to subcutaneous perfusion and tissue metabolism and that skin infrared thermal radiation may reflect an increase or a decrease in local skin perfusion flow rates (Slomka et al., 2018). In this study, after using two different taping materials, we found the temperature difference at the waist in Kfan was significantly higher than that of no taping, but this was not observed with Afan. This phenomenon may have been due to the viscoelastic properties and thickness which similar to human skin. KT has good elastic properties and does not produce pressure on the deep tissues to restrict their movement (Hosp et al., 2018). Compared to KT, AT has poor viscoelasticity, and a weak pulling effect on skin; therefore, the subcutaneous gap and the thermal effect are less than that of KT.
In addition, we found that there was no significant difference for self-perceived temperature after taping for 10 min. This result indicated that the self-perceived temperature was not related to the materials and taping methods. However, there was an increase of self-perceived temperature, this may be due to the placebo effect which affected psychological expectations of participants.
Limitations
However, the limitations must be considered when interpreting the results. Firstly, we only observed temperature fluctuations at the waist after taping. As a core region of the human body, the temperature of the waist is relatively high with little fluctuation, while the temperature of the distal extremities may be more susceptible to external intervention (Hermanns et al., 2018). Secondly, it has been reported that skin temperature distribution is influenced by the subcutaneous fat of each body segment. (Neves et al., 2015; Salamunes et al., 2017), the lack of fatness measurement was a further limitation, which is important for skin temperature distribution. Additionally, all participants were healthy, whereas symptomatic patients may present with abnormal temperature distribution which may have more obvious response for taping. We neglected the reliability analysis in different taping interventions, which may affect the accuracy of the experimental results. Lastly, this study only observed the short-term effects of different taping methods on local skin temperature under static conditions, and dynamic and long-term effect were needed to be verified furtherly.
Future Research
Due to taping was used commonly in dynamic conditions during real complex environments, future research needs to involve the effects of different taping methods KT on skin temperature under a dynamic condition (e.g., during exercise; Trecroci et al., 2019). In addition, we also need to develop blinded, randomized controlled trials with greater sample size, extend the taping time, compare more types tapes such as spatial, or drift taping in order to explore time-effect relationship of different taping methods on the skin temperature combined with physiological mechanisms at the level of cell and blood.
Conclusion
This study indicated that the fan-strip of KY increased significantly the skin temperature of the waist after taping for 10 min among healthy adults. The application of KT may modify the skin temperature of the human body and promote local microcirculation, although it remained unclear for the real application.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of Shanghai University of Sport, ID 2018071. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
KL contributed to recruit the subjects, collect the data and writing the manuscript. ZD, LC, ZW, and SZhu contributed to recruit the subjects, and collect the data. QQ, WC, and SZha undertook statistical analysis. BY conceived of the study and interpreted the results.
Funding
This work was supported by the (Shanghai Science and Technology Committee #1) under Grant (number 16411955200); (Scientific Research program of Shanghai Disabled Persons’ Federation #2) under Grant (number K2016018); and (Scientific Research and Innovation Team Funding Plan of Shanghai Sanda University #3).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors are thankful for all the participants’ voluntary contribution during the completion of this study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2020.00488/full#supplementary-material
References
Aguilar-Ferrandiz, M. E., Castro-Sanchez, A. M., Mataran-Penarrocha, G. A., Guisado-Barrilao, R., Garcia-Rios, M. C., and Moreno-Lorenzo, C. (2014). A randomized controlled trial of a mixed Kinesio taping-compression technique on venous symptoms, pain, peripheral venous flow, clinical severity and overall health status in postmenopausal women with chronic venous insufficiency. Clin. Rehabil. 28, 69–81. doi: 10.1177/0269215512469120
Alexander, C. M., Mcmullan, M., and Harrison, P. J. (2008). What is the effect of taping along or across a muscle on motoneurone excitability? A study using Triceps Surae. Man. Ther. 13, 57–62. doi: 10.1016/j.math.2006.08.003
Berthier, C., and Blaineau, S. (1997). Supramolecular organization of the subsarcolemmal cytoskeleton of adult skeletal muscle fibers. A review. Biol Cell 89, 413–434. doi: 10.1016/s0248-4900(97)89313-6
Bischoff, L., Babisch, C., Babisch, J., Layher, F., Sander, K., Matziolis, G., et al. (2018). Effects on proprioception by Kinesio taping of the knee after anterior cruciate ligament rupture. Eur. J. Orthop. Surg. Traumatol. 28, 1157–1164. doi: 10.1007/s00590-018-2167-1
Buga, G. M., Gold, M. E., Fukuto, J. M., and Ignarro, L. J. (1991). Shear stress-induced release of nitric oxide from endothelial cells grown on beads. Hypertension 17, 187–193. doi: 10.1161/01.hyp.17.2.187
Chen, W., and Yu, B. (2017). Foundation and Practice Of Soft Tissue Taping Technique: Diagram Of Practical Diagnosis And Treatment Of Kinesio Taping. London: Shanghai Science and Technology Press.
De Ridder, R., Willems, T. M., Vanrenterghem, J., and Roosen, P. (2015). Effect of tape on dynamic postural stability in subjects with chronic ankle instability. Int. J. Sports Med. 36, 321–326. doi: 10.1055/s-0034-1385884
Ekiz, T., Aslan, M. D., and Ozgirgin, N. (2015). Effects of Kinesio Tape application to quadriceps muscles on isokinetic muscle strength, gait, and functional parameters in patients with stroke. J. Rehabil. Res. Dev. 52, 323–331. doi: 10.1682/jrrd.2014.10.0243
Fernández-Cuevas, I., Marins, J. C. B., Lastras, J. A., Carmona, P. M. G., Cano, S. P., García-Concepción, M., et al. (2015). Classification of factors influencing the use of infrared thermography in humans: a review. Infrared Phys. Technol. 71, 28–55.
Gomes Moreira, D., Andrade Fernandes, A. D., Sillero Quintana, M., Brito, C. J., Aparecida Doimo, L., and Bouzas Marins, J. C. (2017). Skin temperature of physically active elderly and young women measured using infrared thermography. J. Phys. Educ. Sport 17, 2531–2537.
Gulpinar, D., Tekeli Ozer, S., and Yesilyaprak, S. S. (2019). Effects of rigid and kinesio taping on shoulder rotation motions, posterior shoulder tightness, and posture in overhead athletes: a randomized controlled trial. J. Sport Rehabil. 28, 256–265. doi: 10.1123/jsr.2017-0047
Hermanns, H., Werdehausen, R., Hollmann, M. W., and Stevens, M. F. (2018). Assessment of skin temperature during regional anaesthesia-What the anaesthesiologist should know. Acta Anaesthesiol. Scand. 62, 1280–1289. doi: 10.1111/aas.13176
Holey, L. A., Dixon, J., and Selfe, J. (2011). An exploratory thermographic investigation of the effects of connective tissue massage on autonomic function. J. Manipulative Physiol. Ther. 34, 457–462. doi: 10.1016/j.jmpt.2011.05.012
Hosp, S., Csapo, R., Heinrich, D., Hasler, M., and Nachbauer, W. (2018). Does Kinesiology tape counter exercise-related impairments of balance in the elderly? Gait Posture 62, 167–172. doi: 10.1016/j.gaitpost.2018.03.022
Huijing, P. A. (2009). Epimuscular myofascial force transmission: a historical review and implications for new research. International society of biomechanics Muybridge award lecture, Taipei, 2007. J. Biomech. 42, 9–21. doi: 10.1016/j.jbiomech.2008.09.027
Johnson, J. M., Minson, C. T., and Kellogg, D. L. (2014). Cutaneous vasodilator and vasoconstrictor mechanisms in temperature regulation. Comprehens. Physiol. 4, 33–89. doi: 10.1002/cphy.c130015
Jones, M., Denson, A., and Williams, E. (2005). Assessing pregnancy status using digital infrared thermal imaging in Holstein heifers. J. Anim. Sci. 88, 40–41.
Kalron, A., and Bar-Sela, S. (2013). A systematic review of the effectiveness of Kinesio Taping–fact or fashion? Eur. J. Phys. Rehabil. Med. 49, 699–709.
Kasawara, K. T., Mapa, J. M. R., Ferreira, V., Added, M. A. N., Shiwa, S. R., Carvas, N., et al. (2018). Effects of Kinesio Taping on breast cancer-related lymphedema: a meta-analysis in clinical trials. Physiother. Theory Pract. 34, 337–345. doi: 10.1080/09593985.2017.1419522
Kase, K., and Hashimoto, T. (1998). Changes in the volume of the peripheral blood flow by using kinesio taping. Kinesio Taping Assoc. 82:1373. doi: 10.1016/j.apmr.2013.05.016
Kase, K., Wallis, J., and Kase, T. (2003). Clinical Therapeutic Applications of the Kinesio Taping Method. Tokyo: Ken I Kai Co Ltd.
Kellogg, D. L., Zhao, J. L., and Wu, Y. (2009). Roles of nitric oxide synthase isoforms in cutaneous vasodilation induced by local warming of the skin and whole body heat stress in humans. J. Appl. Physiol. 107, 1438–1444. doi: 10.1152/japplphysiol.00690.2009
Kumbrink, B. (2012). K Taping: An Illustrated Guide: Basics, Techniques, Indications. Berlin: Springer.
Magalhães, M. F., Dibai-Filho, A. V., de Oliveira Guirro, E. C., Girasol, C. E., de Oliveira, A. K., Dias, F. R. C., et al. (2015). Evolution of skin temperature after the application of compressive forces on tendon, muscle and myofascial trigger point. PLoS One 10:e0129034. doi: 10.1371/journal.pone.0129034
Marins, J. C. B., Moreira, D. G., Cano, S. P., Quintana, M. S., Soares, D. D., Fernandes, A. D. A., et al. (2014). Time required to stabilize thermographic images at rest. Infrared Phys. Technol. 65, 30–35.
Matheus, J. P., Zille, R. R., Gomide Matheus, L. B., Lemos, T. V., Carregaro, R. L., and Shimano, A. C. (2017). Comparison of the mechanical properties of therapeutic elastic tapes used in sports and clinical practice. Phys. Ther. Sport 24, 74–78. doi: 10.1016/j.ptsp.2016.08.014
Moreira, D. G., Costello, J. T., Brito, C. J., Adamczyk, J. G., Ammer, K., Bach, A. J. E., et al. (2017). Thermographic imaging in sports and exercise medicine: A Delphi study and consensus statement on the measurement of human skin temperature. J. Therm. Biol. 69, 155–162. doi: 10.1016/j.jtherbio.2017.07.006
Neves, E. B., Vilaca-Alves, J., Antunes, N., Felisberto, I. M., Rosa, C., and Reis, V. M. (2015). “Different responses of the skin temperature to physical exercise: Systematic review,” in Proceedings of the Conference Proceedings: Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Piscataway, NJ. doi: 10.1109/EMBC.2015.7318608
Ng, E. Y. K. (2009). A review of thermography as promising non-invasive detection modality for breast tumor. Int. J. Therm. Sci. 48, 849–859.
Pamuk, U., and Yucesoy, C. A. (2015). MRI analyses show that kinesio taping affects much more than just the targeted superficial tissues and causes heterogeneous deformations within the whole limb. J. Biomech. 48, 4262–4270. doi: 10.1016/j.jbiomech.2015.10.036
Paniagua, O. A., Bryant, M. B., and Panza, J. A. (2001). Role of endothelial nitric oxide in shear stress-induced vasodilation of human microvasculature: diminished activity in hypertensive and hypercholesterolemic patients. Circulation 103, 1752–1758. doi: 10.1161/01.cir.103.13.1752
Pergola, P. E., Kellogg, D. L. Jr., Johnson, J. M., Kosiba, W. A., and Solomon, D. E. (1993). Role of sympathetic nerves in the vascular effects of local temperature in human forearm skin. Am. J. Physiol. 265(3 Pt 2), H785–H792. doi: 10.1152/ajpheart.1993.265.3.H785
Romanovsky, A. A. (2014). Skin temperature: its role in thermoregulation. Acta Physiol. 210, 498–507. doi: 10.1111/apha.12231
Roy, R. A., Boucher, J. P., and Comtois, A. S. (2013). Comparison of paraspinal cutaneous temperature measurements between subjects with and without chronic low back pain. J. Manipulative Physiol. Ther. 36, 44–50. doi: 10.1016/j.jmpt.2012.12.002
Salamunes, A., Stadnik, A., and Neves, E. B. (2017). The effect of body fat percentage and body fat distribution on skin surface temperature with infrared thermography. J. Therm. Biol. 66, 1–9. doi: 10.1016/j.jtherbio.2017.03.006
Sefton, J. M., Yarar, C., Berry, J. W., and Pascoe, D. D. (2010). Therapeutic massage of the neck and shoulders produces changes in peripheral blood flow when assessed with dynamic infrared thermography. J. Alternat. Complem. Med. 16, 723–732. doi: 10.1089/acm.2009.0441
Sillero Quintana, M., Fernández Cuevas, I., Arnaiz-Lastras, J., and Marins, J. (2015). “TERMOINEF Group protocol for thermographic assessment in humans,” in Pre-Congress XIII EAT Congress. Available online at: https://www.researchgate.net/publication/281899883_TERMOINEF_Group_protocol_for_thermographic_assessment_in_humans
Slomka, B., Rongies, W., Ruszczuk, P., Sierdzinski, J., Saganowska, D., Zdunski, S., et al. (2018). Short-term effect of kinesiology taping on temperature distribution at the site of application. Res. Sports Med. 26, 365–380. doi: 10.1080/15438627.2018.1447468
Solari, E., Marcozzi, C., Negrini, D., and Moriondo, A. (2017). Temperature-dependent modulation of regional lymphatic contraction frequency and flow. Am. J. Physiol. Heart Circ. Physiol. 313, H879–H889. doi: 10.1152/ajpheart.00267.2017
Stryker, S. M., Di Trani, A. M., Swanik, C. B., Glutting, J. J., and Kaminski, T. W. (2016). Assessing performance, stability, and cleat comfort/support in collegiate club soccer players using prophylactic ankle taping and bracing. Res. Sports Med. 24, 39–53. doi: 10.1080/15438627.2015.1126274
Swain, I. D., and Grant, L. J. (1989). Methods of measuring skin blood flow. Phys. Med. Biol. 34, 151–175. doi: 10.1097/01.prs.0000148415.54546.ca
Tantawy, S. A., Abdelbasset, W. K., Nambi, G., and Kamel, D. M. (2019). Comparative study between the effects of kinesio taping and pressure garment on secondary upper extremity lymphedema and quality of life following mastectomy: a randomized controlled trial. Integr. Cancer Ther. 18:1534735419847276. doi: 10.1177/1534735419847276
Tauchmannova, H., Gabrhel, J., and Cibak, M. (1993). Thermographic findings in sports: their value in the prevention of soft tissue injuries. Thermol. Österr. 3, 91–95.
Taylor, W. F., Johnson, J. M., O’Leary, D. S., and Park, M. K. (1984). Modification of the cutaneous vascular response to exercise by local skin temperature. J. Appl. Physiol. 57, 1878–1884. doi: 10.1152/jappl.1984.57.6.1878
Trecroci, A., Formenti, D., Rossi, A., Esposito, F., and Alberti, G. (2019). Short-term delayed effects of kinesio taping on sprint cycling performance. J. Strength Cond. Res. 33, 1232–1236. doi: 10.1519/JSC.0000000000003125
Vercelli, S., Colombo, C., Tolosa, F., Moriondo, A., Bravini, E., Ferriero, G., et al. (2017). The effects of kinesio taping on the color intensity of superficial skin hematomas: a pilot study. Phys. Ther. Sport 23, 156–161. doi: 10.1016/j.ptsp.2016.06.005
Weir, J. P. (2005). Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J. Strength Cond. Res. 19, 231–240. doi: 10.1519/15184.1
Windisch, C., Brodt, S., Rohner, E., and Matziolis, G. (2017). Effects of Kinesio taping compared to arterio-venous impulse system on limb swelling and skin temperature after total knee arthroplasty. Int. Orthop. 41, 301–307. doi: 10.1007/s00264-016-3295-z
Wozniak-Czekierda, W., Wozniak, K., Hadamus, A., and Bialoszewski, D. (2017). Use of kinesiology taping in rehabilitation after knee arthroplasty: a randomised clinical study. Ortop. Traumatol. Rehabil. 19, 461–468. doi: 10.5604/01.3001.0010.5828
Yang, J.-M., and Lee, J.-H. (2018). Is kinesio taping to generate skin convolutions effective for increasing local blood circulation? Med. Sci. Monit. 24, 288–293. doi: 10.12659/msm.905708
Yu, B., Qi, Q., Chen, W., Wang, R., Zhou, W., and Li, K. (2016). Different application pattern of Kinesio taping on altering its retraction force and subcutaneous space of healthy adults. Chin. J. Rehabil. Med. 31, 296–300.
Yucesoy, C. A. (2010). Epimuscular myofascial force transmission implies novel principles for muscular mechanics. Exer. Sport Sci. Rev. 38, 128–134. doi: 10.1097/JES.0b013e3181e372ef
Yucesoy, C. A., and Huijing, P. A. (2007). Substantial effects of epimuscular myofascial force transmission on muscular mechanics have major implications on spastic muscle and remedial surgery. J. Electromyogr. Kinesiol. 17, 664–679. doi: 10.1016/j.jelekin.2007.02.008
Keywords: kinesio tape, skin temperature, infrared thermal imaging, taping shapes and materials, erector spinae
Citation: Liu K, Duan Z, Chen L, Wen Z, Zhu S, Qu Q, Chen W, Zhang S and Yu B (2020) Short-Term Effect of Different Taping Methods on Local Skin Temperature in Healthy Adults. Front. Physiol. 11:488. doi: 10.3389/fphys.2020.00488
Received: 03 February 2020; Accepted: 21 April 2020;
Published: 20 May 2020.
Edited by:
Taian Martins Vieira, Politecnico di Torino, ItalyReviewed by:
João Gustavo Claudino, University of São Paulo, BrazilAthos Trecroci, University of Milan, Italy
Copyright © 2020 Liu, Duan, Chen, Wen, Zhu, Qu, Chen, Zhang and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bo Yu, Ym95dWp0dUAxNjMuY29t
†These authors share first authorship
 Kun Liu
Kun Liu Zhouying Duan
Zhouying Duan Lihua Chen
Lihua Chen Zixing Wen
Zixing Wen Shengqun Zhu
Shengqun Zhu Qiang Qu
Qiang Qu Wenhua Chen
Wenhua Chen Shuxin Zhang
Shuxin Zhang Bo Yu
Bo Yu