
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pharmacol. , 08 May 2020
Sec. Ethnopharmacology
Volume 11 - 2020 | https://doi.org/10.3389/fphar.2020.00670
 Wei-Te Huang1†
Wei-Te Huang1† Hao-Hsiu Hung1†
Hao-Hsiu Hung1† Yi-Wei Kao2,3
Yi-Wei Kao2,3 Shi-Chen Ou1
Shi-Chen Ou1 Yu-Chuan Lin1
Yu-Chuan Lin1 Wei-Zen Cheng1
Wei-Zen Cheng1 Zi-Rong Yen4
Zi-Rong Yen4 Jian Li2
Jian Li2 Mingchih Chen2
Mingchih Chen2 Ben-Chang Shia3,5,6*
Ben-Chang Shia3,5,6* Sheng-Teng Huang1,7,8,9,10,11*
Sheng-Teng Huang1,7,8,9,10,11*Background and Purpose: Pattern differentiation is a critical element of the prescription process for Traditional Chinese Medicine (TCM) practitioners. Application of advanced machine learning techniques will enhance the effectiveness of TCM in clinical practice. The aim of this study is to explore the relationships between clinical features and TCM patterns in breast cancer patients.
Methods: The dataset of breast cancer patients receiving TCM treatment was recruited from a single medical center. We utilized a neural network model to standardize terminologies and address TCM pattern differentiation in breast cancer cases. Cluster analysis was applied to classify the clinical features in the breast cancer patient dataset. To evaluate the performance of the proposed method, we further compared the TCM patterns to therapeutic principles of Chinese herbal medication in Taiwan.
Results: A total of 2,738 breast cancer cases were recruited and standardized. They were divided into 5 groups according to clinical features via cluster analysis. The pattern differentiation model revealed that liver-gallbladder dampness-heat was the primary TCM pattern identified in patients. The main therapeutic goals of the top 10 Chinese herbal medicines prescribed for breast cancer patients were to clear heat, drain dampness, and detoxify. These results demonstrated that the neural network successfully identified patterns from a dataset similar to the prescriptions of TCM clinical practitioners.
Conclusion: This is the first study using machine-learning methodology to standardize and analyze TCM electronic medical records. The patterns revealed by the analyses were highly correlated with the therapeutic principles of TCM practitioners. Machine learning technology could assist TCM practitioners to comprehensively differentiate patterns and identify effective Chinese herbal medicine treatments in clinical practice.
Breast cancer is the most common cancer affecting the female population globally. As an adjunct for cancer treatments, complementary and alternative medicine (CAM) is an increasingly popular option sought by patients with breast cancer (Crocetti et al., 1998; Balneaves et al., 2006; Boon et al., 2007). Meanwhile, Traditional Chinese Medicine (TCM) is an important component of CAM, and is currently widely used by breast cancer patients in the ethnic Chinese population (Chen et al., 2008). Many patients seek TCM to resolve side effects including nausea and vomiting, fatigue, paresthesia, chronic pain, constipation, and anorexia which may result from standard Western medicine cancer treatments (Chung et al., 2016).
Despite the increased popularity of TCM, modernization in the field of TCM remains gradual (Ling and Xu, 2013). One particular limitation lies in the fact that the diagnostic and therapeutic systems of TCM depend heavily on the notion of pattern differentiation. The TCM pattern is a diagnostic summary of each individual based on four diagnostic methods: observation, listening, questioning, and pulse detection (World Health Organization. Regional Office for the Western, 2007). Until recently, inefficient data extraction methods have limited the development of automated TCM pattern differentiation. Furthermore, the combinational and highly individualized nature of TCM prescriptions in clinical practice create challenges for researchers to successfully execute randomized control trials to verify TCM theories.
In recent decades, access to electronic medical records (EMR) and advanced machine-learning techniques have enabled the development of computational methods to enhance the field of TCM. More specifically, researchers can now automate the data mining process through natural language processing and information extraction methods. A previous study has demonstrated a framework of automatic diagnosis of TCM by analyzing raw free-text clinical records (Wang et al., 2012).
Artificial neural networks (ANN) are non-linear models that have shown to be useful in elucidating the relationship between the input and output signals of a complex system (Zhang et al., 2018). In this study, we utilized DeepMedic software which incorporated TCM pattern data with ANN to differentiate the TCM patterns identified in individual breast cancer patients. A series of methods including cluster analysis were applied to analyze a dataset of EMR. The cluster analysis was also applied to evaluate the relationships between clinical features, referred to as symptoms and signs in TCM clinical practice, to distinguish TCM pattern differentiation. To evaluate the performance of the TCM pattern differentiation system developed for our study, we further compared the TCM patterns identified in each cluster subgroup with the top ten Chinese herbal prescriptions for Taiwanese breast cancer patients (Huang et al., 2017).
The aim of this study was to apply neural network analysis and cluster analysis to reveal patterns from an EMR dataset and to compare them with the prescriptions of TCM clinical practitioners for the treatment of patients with breast cancer in Taiwan.
The EMR of breast cancer patients (ICD-9 174.0–174.9) having received TCM treatment between January 01, 2003 and June 15, 2018 were collected from the China Medical University Hospital (CMUH) database. The diagnoses were based on the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). This study was approved by the Research Ethics Committee of China Medical University and Hospital, Taichung, Taiwan (CMUH107-REC2-023). All of the datasets analyzed were decoded so that the review board waived the requirement to sign informed consent from patients.
In this study, we used the DeepMedic software to standardize the terminologies of TCM, and to summarize the most likely TCM pattern in each case. The standardization process aimed to unify the polysemous or synonymous vocabulary used in the TCM diagnostic system to facilitate the neural network analysis. The standardization process was accomplished by modifying symptom vocabulary to match the thesaurus within the DeepMedic software, which contains over 20,000 symptom terminologies. Respective standard nomenclatures were applied in the standardization process of syndrome elements, TCM patterns, and treatment modalities. The DeepMedic software can convert TCM patterns into several codes, and label the standard TCM terminologies. For each case being analyzed as input, the specific TCM pattern was identified by determining the higher-weighted code of symptoms and signs. A forward and backward propagation of the neural network, consisting of several hidden layers, was used to calculate the weightings of each code. The weighting of each pattern was based on different symptoms and signs, calculated by using the well-known heuristic equation, Term-Frequency-Inverse Document Frequency (TF-IDF), with some modifications.
TF = (the frequencies of symptom A in code B/code)
The efficacies, as well as the details of related methods, have been demonstrated in our previous study (Lin et al., 2019). The website accessing the demo version of DeepMedic software can be found at: http://bigdata-demo.deepmedic.cn/.
In statistical methodologies, the purpose of cluster analysis is to group the classification objects according to the characteristics of the particular dataset. Study objects classified to the same group have similar characteristics, while those classified to different groups indicate that there are considerable differences in the characteristics. We used K-means cluster to divide data into groups, and the number of clusters was determined by using the smallest total within the sum of squares.
Each variable in the dataset of this study was recorded by binary classification of “yes/no”. Additionally, more even variables are more effective at finding similarity between each cluster. Therefore, we calculated the mean and standard deviation from all variables according to the concept of coefficient of variation. The KPI obtained from dividing the standard deviation by the mean is used for selecting variables. The statistical formula is shown below. The higher value of this statistic represents more even variables. In order to find the optimal KPI, we limited the capture frequency of the variable to more than 5%. Starting from the minimum KPI, we increased the interval by 0.01 to find the best one.
If there were no statistically significant differences and greater than 5% frequency of a variable among clusters, this variable would be determined as a primary feature (PF). Additionally, symptoms that had significant differences in frequency but similar rankings, where the difference between the highest and the lowest ranking was not more than 10 and all frequencies of this variable in each cluster were more than 5% among clusters, were considered the primary features of breast cancer cases, since these symptoms had similar importance in each cluster. When the cluster analytical result of KPI has the most number of primary features, it will be defined as the best KPI.
A symptom is defined as a subjective experience of a disease or physical ailment reported by a patient, while a sign is defined as any abnormal indication of disease that is identified by TCM practitioners (Dodd et al., 2001). Pulse and tongue inspections are the primary diagnostic methods applied by TCM practitioners to collect the data of clinical signs. Despite the correlation between symptoms and signs, the data collection methodologies are different; therefore, we separately collected and analyzed data of symptoms and three types of signs for subsequent TCM pattern differentiation.
Clinical signs including tongue appearance, tongue coating, and pulse were analyzed individually due to variables. The symptoms and signs were ranked according to the frequency of concurrent events. To make the high-ranking symptom and sign variables more representative, we excluded variables with a frequency of less than 5%, and the remaining variables were regarded as secondary features (SF) in each cluster.
From the previous analysis, we obtained the PF and SF of each cluster in the cluster analysis with the best KPI. Each SF had different chances in the cluster due to differing frequencies. In order to analyze various possibilities, we disassembled the SF in a cluster and combined them into “Sx_n”. Where “x” was the number of a cluster, and “n” was the top number of symptoms of the SF. For example, S1_5 represented the top five symptoms of the SF in cluster 1 and its frequency was judged by the fifth symptom. Finally, these were combined with the PF as “P + Sx_n”. DeepMedic software was applied to objectively analyze the general TCM pattern of all combinations. We counted the number of various types of patterns and weighted each pattern with the frequency of the last symptom in each combination to calculate the percentage of this pattern occurring in the cluster. The percentage of a pattern equal to the average frequency of a pattern was divided by the sum of average frequency of all patterns. The statistical formula is shown below.
TCM herbs were classified into several categories based on their usage. To prove that the study objects are compatible with the clinical prescriptions, we analyzed the top 10 single herbs and formulas prescribed by clinical TCM practitioners in Taiwan (Huang et al., 2017). To compare the usage in frequency and dose of each herb and formula, we ranked these medications according to the value obtained by the number of person-days multiplied by average daily dose.
Overall, the architecture (see Figure 1) of this study is primarily composed of five steps, as shown below.
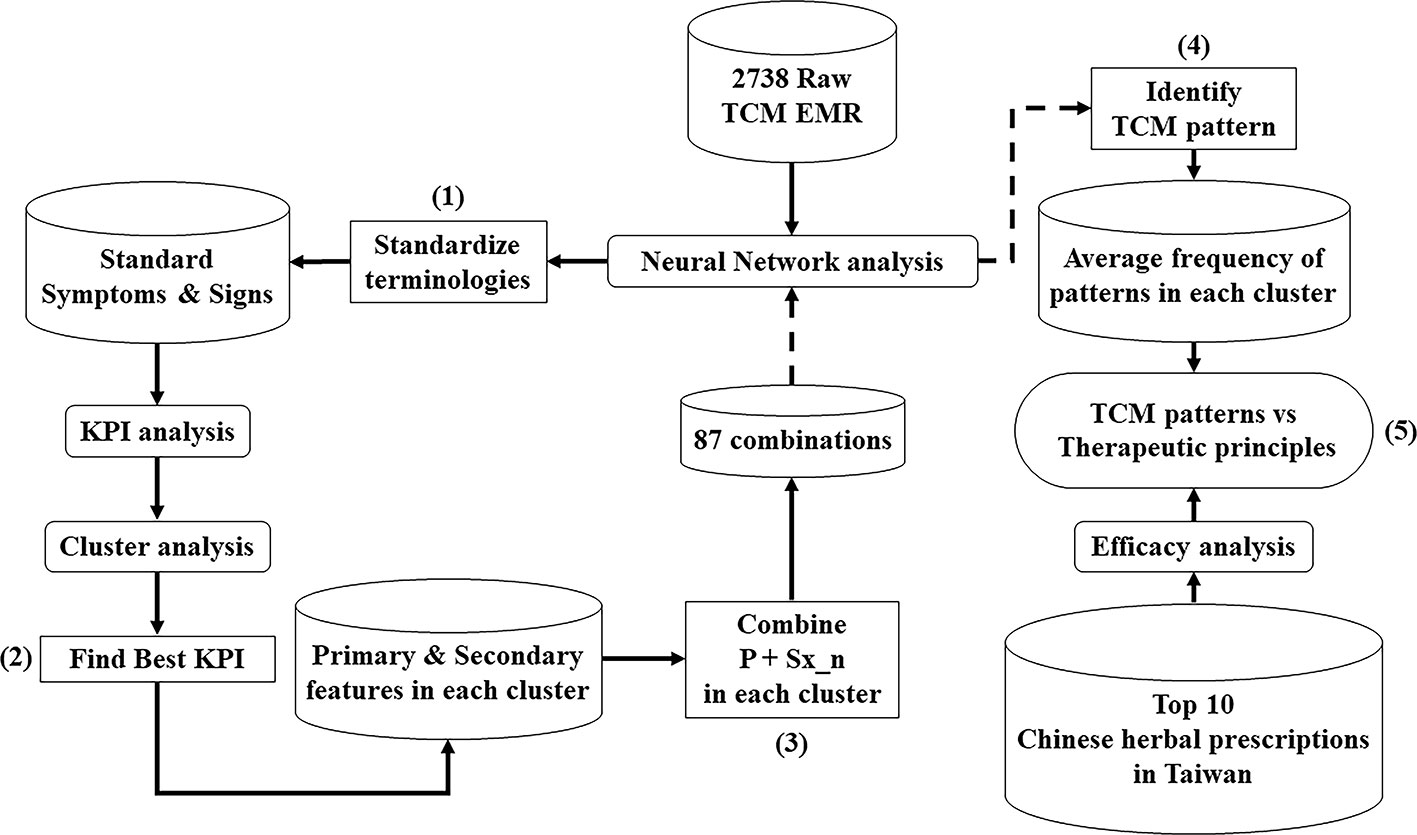
Figure 1 The analytical architecture of TCM EMR in the patients with breast cancer. The workflow (1) ~ (5) describes the process of multiple analyses to classify TCM clinical features and patterns of breast cancer patients, compared with therapeutic principles of Chinese herbal prescriptions by TCM practitioners in Taiwan.
1. Standardize the terminologies of TCM.
2. Find the best KPI to indicate that cluster analytical result has the most number of primary features.
3. Combine primary features and secondary features into different arrangements in each cluster.
4. Identify TCM patterns of each combination in each cluster through machine-learning confirmation.
5. Compare the similarity between TCM patterns in each cluster and the therapeutic principles of Top 10 Chinese herbal prescriptions in Taiwan.
We selected only the initial visit records of individual patients, and excluded the remaining follow-up records, which contained incomplete data. All of these records must have included patient's gender, age, and details concerning symptoms and signs. A total of 78,917 breast cancer patients' records were recruited, including 2,913 complete initial visit records, of which 2,738 cases contained records of the specific herbs and formulas prescribed. The flowchart of our data acquisition is shown in Figure 2.
In the 2,738 analyzable records, the top twenty symptoms in frequency included “insomnia”, “dry mouth”, “lack of strength”, “dizziness”, “loss of appetite”, “abdominal distention”, “profuse dreaming”, “bitter taste of mouth”, “lumbago”, “back pain”, “afraid of cold”, “loose stool”, “headache”, “nausea”, “absence of thirst”, “cough”, “acid regurgitation”, “soreness”, “nocturia”, and “dry eyes”. The top five tongue appearances included “pale red tongue”, “red tongue”, “teeth-marked tongue”, “dark red tongue”, and “dry tongue”. The top five tongue coatings included “white coating”, “thin coating”, “thin white tongue”, “slimy coating”, and “thick coating”. The top five pulses included “string-like pulse”, “slippery pulse”, “fine pulse”, “weak pulse”, and “sunken pulse”. The ranking and frequency of each symptom and sign are listed in Table 1.
The declining slope of total within the sum of squares moderated when the data was divided into five groups, indicating that it was an acceptable number of groups for the analysis of breast cancer patient records (Supplementary Figure 1).
The minimum KPI for this study of breast cancer patients was 0.231, and the best one was 0.252045. The frequency ranking differences of tongue appearances, tongue coatings, and pulses in each cluster were evaluated. According to the proportion between symptoms and signs, if the difference of an individual tongue appearance or pulse was no more than 3 among clusters, or individual coating was no more than 5 among clusters, it would be considered a PF.
The PF of breast cancer patients included insomnia, dry mouth, lack of strength, dizziness, loss of appetite, bitter taste of mouth, abdominal distention, headache, loose stool, nausea, slippery pulse, and rapid pulse. The number of cases and SF in each cluster subgroup are listed in Table 2.
There were 87 combinations of PF and SF. The analysis of these feature combinations is demonstrated in Supplementary Table 1. Liver-gallbladder dampness-heat (LGDH) was the TCM pattern identified as PF. The main TCM pattern and its percentage in each cluster subgroup are demonstrated in Table 3 and Figure 3. LGDH was the main TCM pattern (43%) among all feature combinations, followed by the patterns of depressed liver qi transforming into fire (DLTF) (20%) and retained dampness-toxin (RDT) (12%).
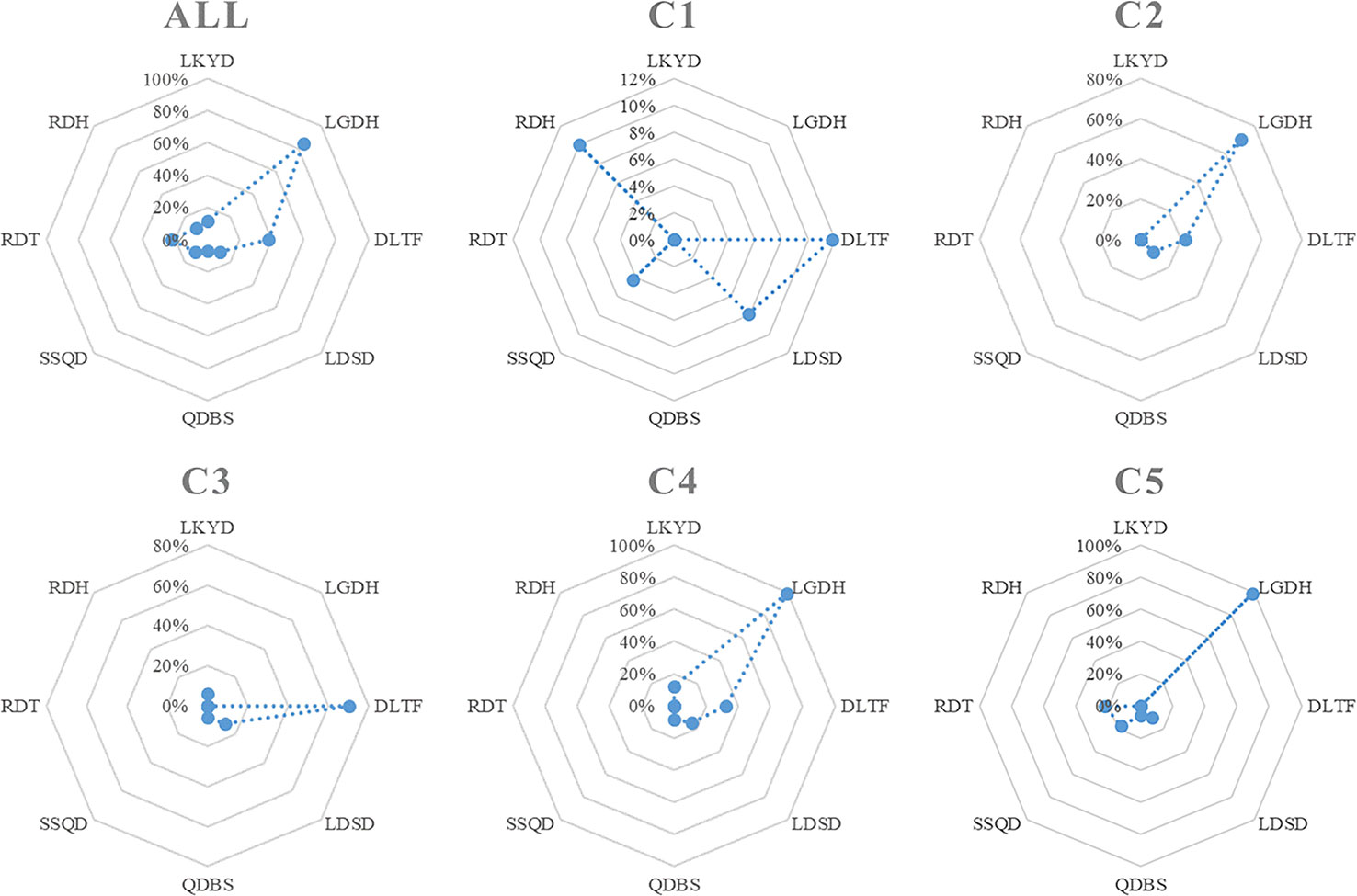
Figure 3 The TCM pattern distribution in each cluster subgroup. LKYD, Liver-kidney yin deficiency; LGDH, Liver-gallbladder dampness-heat; DLTF, Depressed liver qi transforming into fire; LDSD, Liver depression and spleen deficiency; QDBS, Qi deficiency with blood stasis; SSQD, Spleen-stomach qi deficiency; RDT, Retained dampness-toxin; RDH, Retained dampness-heat.
In cluster 1, DLTF was the main TCM pattern (35%), followed by retained dampness-heat (RDH) (30%), and liver depression and spleen deficiency (LDSD) (23%). LGDH was the main TCM pattern (70%) in cluster 2, followed by DLTF (22%). DLTF was the main TCM pattern (74%) in cluster 3, followed by LDSD (13%). In cluster 4, LGDH was still the main TCM pattern (59%), followed by DLTF (19%), and LDSD (9%). LGDH accounted for the main TCM pattern (64%) in cluster 5, followed by RDT (15%), and spleen-stomach qi deficiency (SSQD) (11%). For detailed definition of each pattern from WHO (World Health Organization. Regional Office for the Western, 2007), please refer to Supplementary Table 2.
As shown in Tables 4 and 5, the top 10 of Chinese herbal prescriptions in breast cancer patients included those that could clear heat, drain dampness and detoxify (29%), harmonize the liver and spleen (19%), tonify qi (18%), nourish the heart to tranquilize (15%), activate blood and resolve stasis (12%), tonify yin (4%), clear heat and resolve phlegm (2%), and offensive purgative (1%). The components of each formula were summarized in Supplementary Table 3.
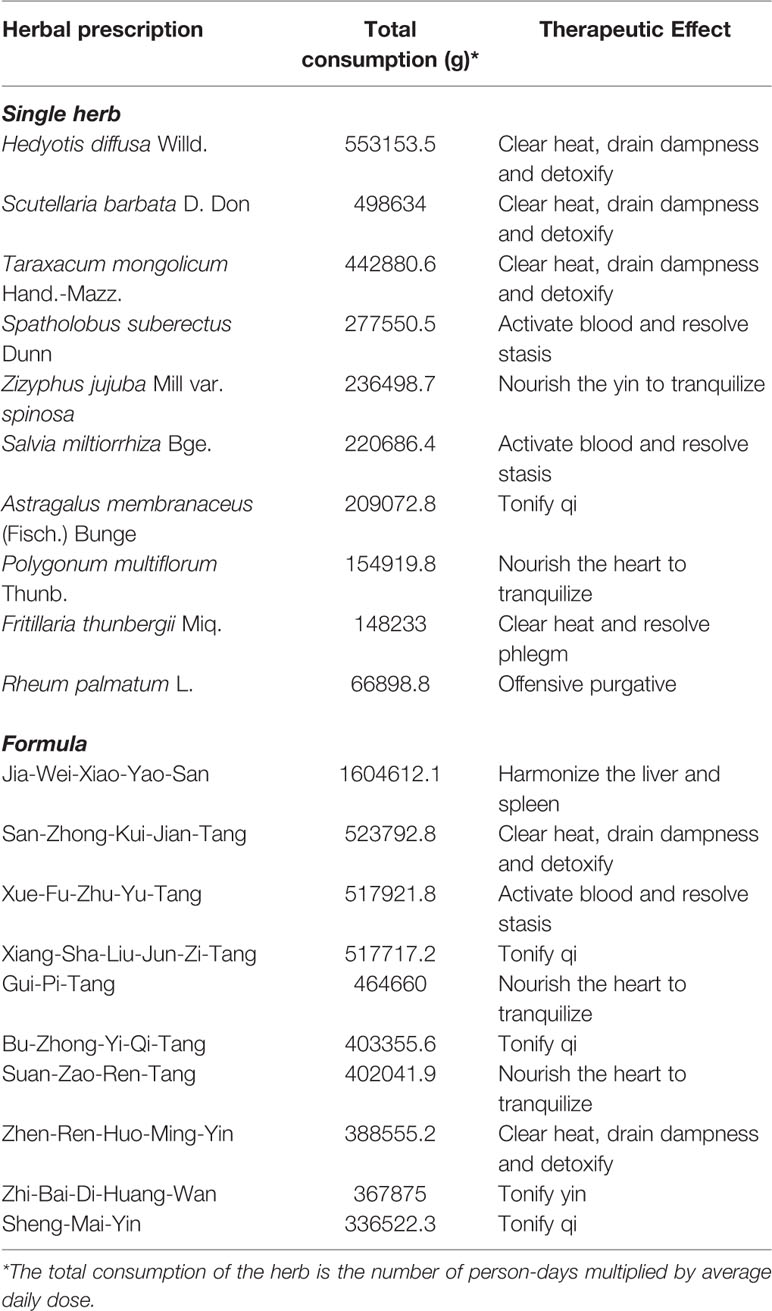
Table 4 The top 10 of Chinese herbal prescription including single herbs and formulae in breast cancer patients in Taiwan.
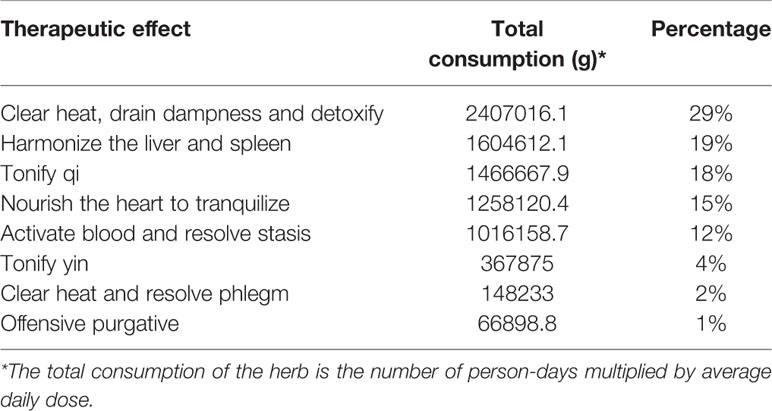
Table 5 The therapeutic effects of the commonly used Chinese herbs in breast cancer patients in Taiwan.
TCM combined with western medical treatment is widely used among breast cancer patients. Previous studies have revealed lower 5-year recurrence and metastasis rate, and decreased incidence of chronic hepatitis while receiving radiotherapy and/or chemotherapy, in breast cancer patients with the combination use of TCM (Liu et al., 2008; Huang et al., 2017). Some Chinese medicinal herbs have demonstrated effects in controlling the progression, increasing the susceptibility to radiotherapy and chemotherapy, elevating immunity, and decreasing the toxicities or side effects of cancer therapies (Yin et al., 2013). Based on the potential therapeutic effects of TCM, we explored the relationships between clinical features and TCM patterns in breast cancer patients via the applications of machine learning techniques. TCM clinical records were gathered in this study for text analysis.
Text analysis is a subfield of natural language processing (NLP). In the past, the lack of a widely adopted and consistently implemented medical terminology limited the use of machine-learning in medical research, especially in the field of TCM. In this study, we used the DeepMedic software to analyze unstructured electronic TCM clinical records. The software standardized and integrated key TCM terminology via the application of an NLP system and neural network. A total of 2,738 breast cancer records were standardized and divided into 5 subgroups via cluster analysis according to the frequency of clinical features reported in each case. Since patterns were not directly observable, the TCM patterns were differentiated via DeepMedic software by analyzing the PF and SF in each cluster subgroup.
As shown in Table 3 and Figure 3, LGDH was the main TCM pattern (43%) identified in breast cancer patients, which was compatible with the analysis of PF. According to the TCM patterns including LGDH, DLTF, and RDH, the liver is the main disease location of breast cancer, while dampness and heat were the main pathological mechanisms. According to TCM theory, the liver is related to the nerve-endocrine-immune network, it is responsible for the regulation of emotion, the promotion of digestion and absorption, and the maintenance of qi and blood circulation via the nerves and endocrine (Liu et al., 2017). In TCM theory, “fire” is the advanced status of “heat” in severity, while “toxin” indicates faster transmission of heat and worsening condition. Since heat and fire will damage the yin, and the depressed liver qi will impair the function of the spleen, some patients exhibit both yin and spleen qi deficiencies. Qi deficiency with blood stasis (QDBS) was also one of the SF identified in breast cancer patients, since qi deficiency will result in stagnated blood circulation. As exhibited in Table 3 and Figure 3, the frequency of the LGDH and DLTF patterns had great impact on these cluster subgroups. The presence of some minor TCM patterns also helped to distinguish these five subgroups.
Cluster 1
The percentage the DLTF pattern (35%) was similar to that of the RDH pattern (30%). Additionally, the percentage of the LDSD (23%) and SSQD (13%) patterns were higher than those of other cluster subgroups. This indicates that there was no dominant TCM pattern in cluster 1.
Cluster 2
The percentages and frequencies of the TCM patterns in cluster 2 were similar to the overall cases. Compared with other patterns, the LGDH pattern was higher (70%). The secondary pattern in cluster 2 was DLTF.
Cluster 3
The percentage of the DLTF pattern was higher (74%) than in other subgroups. Patterns related with heat were the leading patterns in cluster 3. Unlike other clusters, there was no pattern related with dampness in cluster 3. Due to depressed liver qi and heat, some patients demonstrated patterns of spleen qi deficiency (13%), blood stasis (6%), and liver kidney yin deficiency (LKYD) (6%).
Cluster 4
LGDH was the dominant pattern in cluster 4, according to its high percentage (59%) and frequency (99%), followed by the DLTF pattern. Some patients demonstrated the LDSD and QDBS patterns, similar to cluster 3.
Cluster 5
LGDH was the primary pattern identified in cluster 5, with a high percentage (64%) and frequency (99%). RDT was the secondary pattern (22%) in cluster 5. Based on TCM theory, this indicates that more than one fifth of patients have a higher degree of severity and the disease develops at a faster rate.
Overall, LGDH was the leading pattern in clusters 2, 4, and 5. Meanwhile, DLTF was the secondary pattern in clusters 2 and 4, but the leading pattern in cluster 3. RDT was the secondary pattern in cluster 5. As for the patterns of spleen stomach deficiency and of blood stasis, higher frequencies were noted in clusters 4 and 5. Of note, there was no leading pattern identified in cluster 1, indicating no clear TCM pattern based on the analysis. More clinical data and information regarding clinical features are required in the TCM pattern analysis of this cluster subgroup. Clinical TCM practitioners need to exercise vigilance when treating such patients as those included in cluster 1, as these patients demonstrate no clear direction for Chinese medical treatment. As shown in Supplementary Table 1, the cluster analysis revealed that LGDH was the primary pattern exhibited by breast cancer patients in Taiwan.
According to the DeepMedic software analysis, the liver was the main viscera associated with breast cancer patients, followed by gallbladder, spleen, stomach, and kidney. Dampness, heat, and qi stagnation were the major etiologies associated with breast cancer, followed by yin deficiency, qi deficiency, and blood stasis. As shown in Table 5, the main therapeutic goal of TCM practitioners in Taiwan for treatment of breast cancer patients was to clear heat, drain dampness, and detoxify, consistent with the patterns of LGDH, DLTF, RDT, and RDH. This result corresponds with a previous study by Zhang et al, which reported that heat-clearing and detoxifying herbs are commonly prescribed in TCM formulas for the treatment of cancer (Zhang et al., 2017). The therapeutic principle of harmonizing the liver and spleen is consistent with LDSD. The therapeutic principle of tonifying qi is consistent with the patterns of LDSD, SSQD, and QDBS. The principle of activating blood and resolving stasis is consistent with the pattern of QDBS. The principle of tonifying yin is consistent with the pattern of LKYD. The pattern of clearing heat and resolving phlegm is consistent with the patterns of RDT and RDH. Collectively, the therapeutic principles of these Chinese herbal medications are suitable with the needs of breast cancer patients based on their TCM patterns.
Bias in the TCM pattern differentiation indeed exists, as it is difficult to adjust the weight based on the frequency of each clinical feature in the DeepMedic software. Moreover, selective bias may be present due to the retrieved clinical cases in this study being from a single medical center. Owing to a limited number of clinical cases, it is difficult to elucidate the TCM patterns in the different stages of breast cancer. Further study is necessary to evaluate whether different TCM patterns are related to the progression of tumor growth or to the side effects of different therapeutic modalities.
This is the first study to apply a machine-learning model to standardize EMR terminology and analyze TCM patterns in breast cancer patients. With the application of neural network and cluster analyses, five primary TCM patterns were identified based on the clinical symptoms and signs reported in breast cancer patients. The therapeutic principles and prescriptions by TCM clinical practitioners focus on treating dampness, heat, and qi stagnation as the major pathologies in patients with breast cancer. In conclusion, machine learning technology could assist TCM practitioners to comprehensively differentiate patterns and identify effective Chinese herbal medicine treatments in clinical practice.
The datasets generated for this study are available on request to the corresponding authors.
This study was approved by the Research Ethics Committee of China Medical University and Hospital, Taichung, Taiwan (CMUH107-REC2-023). All of the datasets analyzed were decoded so that the review board waived the requirement to sign informed consent from patients.
W-TH and H-HH equally wrote the draft and interpreted the data. W-TH, Y-WK, S-CO, H-HH, Y-CL, and Z-RY collected and assembled the data. W-TH and Y-WK analyzed the data. JL and MC provided methodological support and rectified all of analyzed data. B-CS and S-TH designed and conceived the study, and edited the manuscript. All of the authors approved the final manuscript.
This work was supported and funded by the Ministry of Science and Technology of Taiwan (MOST 108-2320-B-039-022), Health and Welfare Surcharge of Tobacco Products, China Medical University Hospital Cancer Research Center of Excellence (MOHW108-TDU-B-212-124024), China Medical University Hospital (DMR-108-007, DMR-108-009, DMR-108-044 and CRS-108-001), An-Nan Hospital, China Medical University (ANHRF-108-06 and ANHRF-108-08) and the Chinese Medicine Research Center, China Medical University, under the Higher Education Sprout Project, Ministry of Education (CMRC-CHM-1) in Taiwan.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We thank DeepMedic, Inc. (Taipei, Taiwan) for sharing the software of DeepMedic for data analysis and extensive comments. The authors would like to thank James Waddell of Concise Language Services for the critical reading and revision of our manuscript.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2020.00670/full#supplementary-material
AF, Average frequency; ANN, Artificial neural networks; AP, Amount of people; CAM, Complementary and Alternative Medicine; CMUH, Chinese Medical University Hospital; DLTF, Depressed liver qi transforming into fire; EMR, Electronic medical records; ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; KPI, Key Performance Indicators; LDSD, Liver depression and spleen deficiency; LGDH, Liver-gallbladder dampness-heat; LKYD, Liver-kidney yin deficiency; NLP, Natural language processing; PF, Primary features; QDBS, Qi deficiency with blood stasis; RDH, Retained dampness-heat; RDT, Retained dampness-toxin; SF, Secondary features; SSQD, Spleen-stomach qi deficiency; TCM, Traditional Chinese medicine; TF-IDF, Term-Frequency-Inverse Document Frequency.
Balneaves, L. G., Bottorff, J. L., Hislop, T. G., Herbert, C. (2006). Levels of commitment: exploring complementary therapy use by women with breast cancer. J. Altern. Complement Med. 12 (5), 459–466. doi: 10.1089/acm.2006.12.459
Boon, H. S., Olatunde, F., Zick, S. M. (2007). Trends in complementary/alternative medicine use by breast cancer survivors: comparing survey data from 1998 and 2005. BMC Womens Health 7 (4). doi: 10.1186/1472-6874-7-4
Chen, Z., Gu, K., Zheng, Y., Zheng, W., Lu, W., Shu, X. O. (2008). The use of complementary and alternative medicine among Chinese women with breast cancer. J. Altern. Complement Med. 14 (8), 1049–1055. doi: 10.1089/acm.2008.0039
Chung, V. C., Wu, X., Lu, P., Hui, E. P., Zhang, Y., Zhang, A. L., et al. (2016). Chinese Herbal Medicine for Symptom Management in Cancer Palliative Care: Systematic Review And Meta-analysis. Med. (Baltimore) 95 (7), e2793. doi: 10.1097/MD.0000000000002793
Crocetti, E., Crotti, N., Feltrin, A., Ponton, P., Geddes, M., Buiatti, E. (1998). The use of complementary therapies by breast cancer patients attending conventional treatment. Eur. J. Cancer 34 (3), 324–328. doi: 10.1016/s0959-8049(97)10043-0
Dodd, M., Janson, S., Facione, N., Faucett, J., Froelicher, E. S., Humphreys, J., et al. (2001). Advancing the science of symptom management. J. Adv. Nurs. 33 (5), 668–676. doi: 10.1046/j.1365-2648.2001.01697.x
Huang, K. C., Yen, H. R., Chiang, J. H., Su, Y. C., Sun, M. F., Chang, H. H., et al. (2017). Chinese Herbal Medicine as an Adjunctive Therapy Ameliorated the Incidence of Chronic Hepatitis in Patients with Breast Cancer: A Nationwide Population-Based Cohort Study. Evid. Based Complement Alternat. Med. 2017, 1052976. doi: 10.1155/2017/1052976
Lin, Y. C., Huang, W. T., Ou, S. C., Hung, H. H., Cheng, W. Z., Lin, S. S., et al. (2019). Neural network analysis of Chinese herbal medicine prescriptions for patients with colorectal cancer. Complement Ther. Med. 42, 279–285. doi: 10.1016/j.ctim.2018.12.001
Ling, S., Xu, J. W. (2013). Model organisms and traditional chinese medicine syndrome models. Evid. Based Complement Alternat. Med. 2013, 761987. doi: 10.1155/2013/761987
Liu, S., Zhao, J., Liu, J., Sun, Z. -P., Hua, Y. -Q., Lu, D. -M., et al. (2008). Effects of Ru'ai Shuhou Recipe on 5-year recurrence rate after mastectomy in breast cancer. J. Chin. Integr. Med. 6 (10), 1000–1004. doi: 10.3736/jcim20081003
Liu, Z. W., Shu, J., Tu, J. Y., Zhang, C. H., Hong, J. (2017). Liver in the Chinese and Western Medicine. Integr. Med. Int. 4 (1-2), 39–45. doi: 10.1159/000466694
Wang, Y., Yu, Z., Jiang, Y., Liu, Y., Chen, L., Liu, Y. (2012). A framework and its empirical study of automatic diagnosis of traditional Chinese medicine utilizing raw free-text clinical records. J. BioMed. Inform 45 (2), 210–223. doi: 10.1016/j.jbi.2011.10.010
World Health Organization. Regional Office for the Western, P. (2007). WHO international standard terminologies on traditional medicine in the Western Pacific Region: (Manila : WHO Regional Office for the Western Pacific).
Yin, S. Y., Wei, W. C., Jian, F. Y., Yang, N. S., Therapeutic Applications of Herbal Medicines for Cancer Patients. (2013). Evid. Based Complement. Alternat. Med. 2013, 302426. doi: 10.1155/2013/302426
Zhang, Y., Liang, Y., He, C. (2017). Anticancer activities and mechanisms of heat-clearing and detoxicating traditional Chinese herbal medicine. Chin. Med. 12 (20). doi: 10.1186/s13020-017-0140-2
Keywords: traditional Chinese medicine, electronic medical records, breast cancer, neural network analysis, cluster analysis, pattern differentiation
Citation: Huang W-T, Hung H-H, Kao Y-W, Ou S-C, Lin Y-C, Cheng W-Z, Yen Z-R, Li J, Chen M, Shia B-C and Huang S-T (2020) Application of Neural Network and Cluster Analyses to Differentiate TCM Patterns in Patients With Breast Cancer. Front. Pharmacol. 11:670. doi: 10.3389/fphar.2020.00670
Received: 26 January 2020; Accepted: 23 April 2020;
Published: 08 May 2020.
Edited by:
Min Ye, Peking University, ChinaCopyright © 2020 Huang, Hung, Kao, Ou, Lin, Cheng, Yen, Li, Chen, Shia and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ben-Chang Shia, c3RhdDEwMDFAdG11LmVkdS50dw==; Sheng-Teng Huang, c2hlbmcudGVuZ0B5YWhvby5jb20=; ZDk4Mjk0QG1haWwuY211aC5vcmcudHc=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.