- 1Department of Pediatrics, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States
- 2Department of Gastroenterology and Hepatology, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States
- 3Department of Pediatric Surgery, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States
Torsion of an accessory spleen is an exceedingly rare cause of abdominal pain in pediatric patients. The diagnosis is frequently challenging as presentation is variable and diagnostic imaging can be aspecific. The current case describes an unusual presentation of a torted accessory spleen in a 5-year-old girl with biliary atresia splenic malformation syndrome who initially presented with non-specific abdominal symptoms and fever. The diagnosis was made following fine-needle aspiration of a suspected intraabdominal abscess. The case highlights the diagnostic challenge of accessory splenic torsion and stresses the importance of its inclusion on the differential diagnosis of pediatric patients, especially those with known splenic or laterality abnormalities, presenting with both acute and sub-acute abdominal symptoms.
Background
Accessory spleens or splenules represent a congenital focus of normal splenic tissue separate from the spleen. They are typically asymptomatic and observed in ~10–30% of patients at autopsy (1, 2). Rarely, accessory spleens become symptomatic following torsion of their vascular pedicle, which compromises blood flow to the organ, leading to a potentially wide spectrum of clinical presentations. Cases may present with a variety of non-specific symptoms (e.g., vague abdominal pain, nausea, vomiting, and fever), recurrent abdominal pain, or with an acute abdomen (3). Diagnosis is typically made in the operating room as diagnostic imaging is often times unrevealing. Definitive treatment is almost always splenectomy (4, 5). Herein, the authors describe an unusual presentation of a torted splenule in a 5-year-old patient with biliary atresia splenic malformation syndrome (BASM).
Case Presentation
A 5-year-old girl was admitted with a 1-day history of generalized malaise, right upper quadrant abdominal pain, vomiting, and fever. Her medical history is significant for mosaic terminal 18q deletion, bronchomalacia, and BASM (with known situs inversus, polysplenia, and malrotation) status post hepatoportoenterostomy with resulting chronic liver fibrosis.
She was initially well appearing with a benign abdominal examination and normal vital signs. Laboratory evaluation including basic metabolic panel, complete blood count with differential, prothrombin time/international normalized ratio, and hepatic function panel were reassuring. Blood cultures were obtained and piperacillin/tazobactam was initiated secondary to concern for possible cholangitis. Metronidazole was added after stool pathogen panel returned positive for the giardia antigen. Interestingly, abdominal x-ray, obtained around time of admission, showed significant colonic stool burden, and a continuous polyethylene glycol infusion via nasogastric tube was run for 24 h with good effect in terms of stool output and relief of abdominal pain.
On day 3 of admission, despite broad spectrum antibiotics and negative blood cultures, the patient continued to be febrile and developed marked abdominal distension. Abdominal ultrasound was obtained and demonstrated perihepatic and lower abdominal ascites. Right-sided spleen was visualized with normal parenchymal echotexture. Ultrasound guided paracentesis was performed, with fluid analysis revealing 3,724 total nucleated cells with 71% neutrophils. Peritoneal fluid culture did not speciate an organism, however, at the time, this was believed to be due to antibiotic sterilization. A presumptive diagnosis of spontaneous bacterial peritonitis was made, and after consultation with Infectious Diseases, intravenous ceftriaxone was initiated for better empiric coverage of encapsulated organisms.
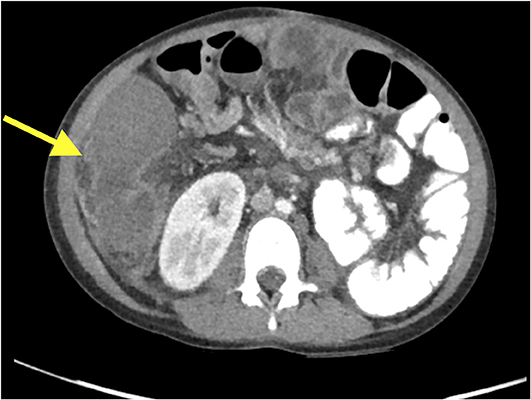
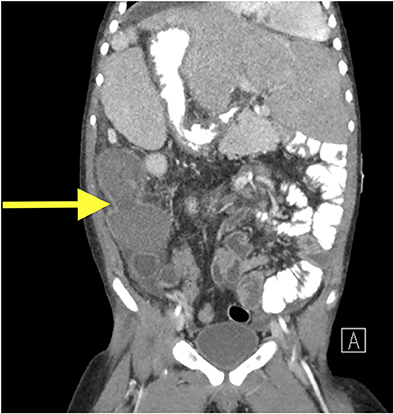
Despite greater than 48 h of appropriate antibiotics, the patient continued to be intermittently febrile and complain of significant abdominal discomfort and distension. Subsequent abdominal computed tomography (CT) showed a large, rim enhancing fluid collection in the right upper abdomen concerning for abscess (see Figures 1, 2). After consultation with Pediatric Surgery, the patient was taken to Interventional Radiology for abscess drainage. Upon attempted fluid aspiration, soft tissue was obtained. Pathological evaluation revealed the tissue to be consistent with a splenic infarction (see Figure 3). Given the location and appearance of the tissue, a diagnosis of accessory splenic torsion was made.
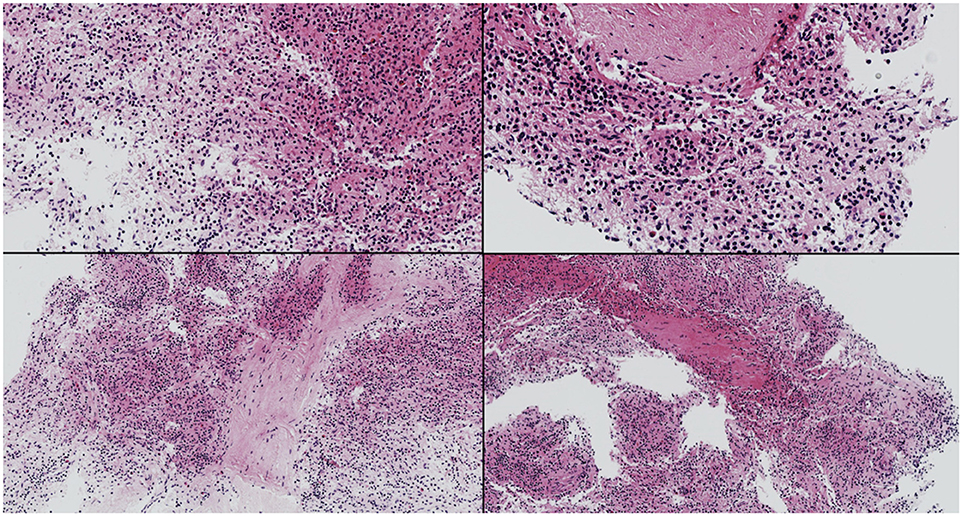
Figure 3. Fragments of splenic tissue with patchy hemorrhagic necrosis consistent with splenic infarction.
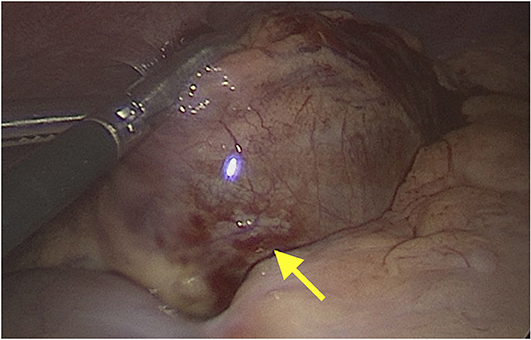
The initial treatment approach included conservative management with antibiotics, nasogastric tube feedings and pain control based on the desire to avoid surgical intervention in a patient with a complex medical and surgical history, as well as the noted resolution of splenic infarction without surgery (6). However, due to persistent fevers and uncontrolled abdominal pain, the patient ultimately underwent removal of the infarcted splenule via laparoscopic assisted excision (see Figure 4). Surgery was well-tolerated, and histological examination confirmed the diagnosis of accessory splenic torsion. Post-operative course was uneventful, and the patient was discharged from the hospital on post-operative day 8.
Discussion
The human spleen is derived from proliferating mesenchyme overlying the dorsal pancreatic endoderm between the tiers of the dorsal mesogastrium during the fifth week of embryogenesis (1). Between weeks 7 and 8 the rotation of the stomach causes the left mesogastrium surface to fuse with the peritoneum above the left kidney. An accessory spleen is formed when mesenchymal remnants fail to fuse with the main splenic mass and deposit along the path of splenic development (1). They are exclusively found on the left side of the abdomen, however in the case of situs inversus (as seen in the current case), right sided accessory spleens are observed (5).
Accessory spleens are a frequently observed congenital anomaly occurring in ~10–30% of patients on postmortem studies (1, 2). Of those with accessory spleens only 14% have more than one (7). Accessory spleens are almost always asymptomatic. Complications, such as torsion and infarction, are extremely rare. To the authors knowledge, only 19 pediatric cases of accessory splenic torsion, including the current case, have been described in the English literature (2–6, 8–18). This is the second reported case of an accessory splenic torsion occurring in a child with known situs inversus and the only documented case in a patient with BASM (5).
Biliary atresia describes a progressive, idiopathic, fibro-obliterative disease of the extrahepatic biliary tree and is the most common indication for liver transplantation in pediatric patients. Biliary atresia often presents in isolation; however, the condition can present in combination with congenital malformations. In the setting of known splenic abnormalities the condition is referred to as BASM. BASM occurs in ~10–15% of patients with biliary atresia (19, 20). In addition to splenic malformations (e.g., polysplenia or asplenia), situs inversus, malrotation, interrupted inferior vena cava, and cardiac anomalies are characteristic of the condition. Retrospective data suggests that patients with BASM have poorer outcomes than children with biliary atresia without other anomalies or malformations (21). These differences appear to be related to the higher risk of developing hepatorenal syndrome as well as various cardiac and intrabdominal complications. There are no known risk factors for developing an accessory splenic torsion, however it remains possible that pediatric patients with known splenic and intrabdominal abnormalities could be predisposed to this rare complication.
Diagnosis of a torted accessory spleen can be challenging, and separating the findings from possible cholangitis, gastroenteritis, bacterial peritonitis, abdominal abscess, and constipation in the above case proved difficult. Maintaining a high index of suspicion, especially in a patient with known splenic anomalies, is paramount as results of diagnostic imaging may be non-specific or unavailable in the emergency setting. As seen in Figures 1, 2, CT appearance of an accessory splenic torsion may mimic a drainable abdominal fluid collection or abscess (8). Ultrasonography with Doppler and magnetic resonance imaging may allow for further characterization of a possible torted splenule, however even with modern imaging modalities the diagnosis is often uncertain.
Almost all reported pediatric cases of accessory splenic torsion are diagnosed at time of surgery (4, 5, 9, 11, 13, 14, 16–18). Once confirmed, management is typically operative, however conservative management has proven successful (6). Scire et al. (6) report a 10-year-old male patient diagnosed with accessory splenic torsion after presenting to the emergency room with acute abdominal pain. He was treated with analgesics and antibiotics and had spontaneous symptom resolution (e.g., abdominal pain) within 1 week. Subsequent ultrasound imaging revealed progressive reduction in the dimensions of the accessory spleen at 3-month, 6-month, and 1-year follow-ups. Unfortunately, despite a similar approach, conservative management in the current case proved unsuccessful and surgical intervention was ultimately required.
Conclusion
Accessory splenic torsion is a rare pediatric entity and should remain on the differential for pediatric patients presenting with both acute and non-specific abdomen pain, especially in the setting of known splenic malformations and/or other laterality defects. Once confirmed, conservative management could be considered, but operative management is most common.
Data Availability Statement
All datasets analyzed for this study are included in the manuscript.
Ethics Statement
Signed informed consent was obtained from the patient's mother for publication of this case report and any potentially identifying information has been removed.
Author Contributions
DS, NF, RF, PC, and JF conceptualized, drafted, reviewed, and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable to all aspects of the work.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Alexander Katz, MD for his assistance in providing and interpreting the histology presented in this report.
Abbreviations
BASM, Biliary atresia splenic malformation syndrome.
References
1. Yildiz AE, Ariyurek MO, Karcaaltincaba M. Splenic anomalies of shape, size, and location: pictorial essay. Sci World J. (2013) 2013:321810. doi: 10.1155/2013/321810
2. Valls C, Mones L, Guma A, Lopez-Calonge E. Torsion of a wandering accessory spleen: CT findings. Abdomin Imaging. (1998) 23:194–5. doi: 10.1007/s002619900321
3. Impellizzeri P, Montalto AS, Borruto FA, Antonuccio P, Scalfari G, Arena F, et al. Accessory spleen torsion: rare cause of acute abdomen in children and review of literature. J Pediatr Surg. (2009) 44:e15–8. doi: 10.1016/j.jpedsurg.2009.06.029
4. Ren C, Liu Y, Cao R, Zhao T, Chen D, Yao L, et al. Colonic obstruction caused by accessory spleen torsion: a rare case report and literature review. Medicine. (2017) 96:e8116. doi: 10.1097/MD.0000000000008116
5. Ishibashi H, Oshio T, Sogami T, Nii A, Mori H, Shimada M. Torsion of an accessory spleen with situs inversus in a child. J Med Invest. (2012) 59:220–3. doi: 10.2152/jmi.59.220
6. Scire G, Zampieri N, El-Dalati G, Camoglio FS. Conservative management of accessory spleen torsion in children. Minerva Pediatr. (2013) 65:453–6.
8. Trinci M, Ianniello S, Galluzzo M, Giangregorio C, Palliola R, Briganti V, et al. A rare case of accessory spleen torsion in a child diagnosed by ultrasound (US) and contrast-enhanced ultrasound (CEUS). J Ultrasound. (2019) 22:99–102. doi: 10.1007/s40477-019-00359-4
9. Yousef Y, Cameron BH, Maizlin ZV, Boutross-Tadross O. Laparoscopic excision of infarcted accessory spleen. J Laparoendosc Adv Surg Techn Part A. (2010) 20:301–3. doi: 10.1089/lap.2009.0286
10. Mendi R, Abramson LP, Pillai SB, Rigsby CK. Evolution of the CT imaging findings of accessory spleen infarction. Pediatr Radiol. (2006) 36:1319–22. doi: 10.1007/s00247-006-0323-y
11. Gardikis S, Pitiakoudis M, Sigalas I, Theocharous E, Simopoulos C. Infarction of an accessory spleen presenting as acute abdomen in a neonate. Eur J Pediatr Surg. (2005) 15:203–5. doi: 10.1055/s-2005-837605
12. Perez Fontan FJ, Soler R, Santos M, Facio I. Accessory spleen torsion: US, CT and MR findings. Eur Radiol. (2001) 11:509–12. doi: 10.1007/s003300000547
13. Seo T, Ito T, Watanabe Y, Umeda T. Torsion of an accessory spleen presenting as an acute abdomen with an inflammatory mass. US, CT, and MRI findings. Pediatr Radiol. (1994) 24:532–34. doi: 10.1007/BF02015022
14. Nutman J, Mimouni M, Zer M, Grunebaum M, Varsano I. Accessory spleen as a cause of an abdominal mass. Z Kinderchirurgie. (1982) 37:71–2.
15. Onuigbo WI, Ojukwu JO, Eze WC. Infarction of accessory spleen. J Pediatr Surg. (1978) 13:129–30.
16. Broker FH, Khettry J, Filler RM, Treves S. Splenic torsion and accessory spleen: a scintigraphic demonstration. J Pediatr Surg. (1975) 10:913–5.
17. Babcock TL, Coker DD, Haynes JL, Conklin HB. Infarction of an accessory spleen causing an acute abdomen. Am J Surg. (1974) 127:336–7.
18. Settle E. The surgical importance of accessory spleens: with report of two cases. Am J Surg. (1940) 50:22–6.
19. Davenport M, Tizzard SA, Underhill J, Mieli-Vergani G, Portmann B, Hadzic N. The biliary atresia splenic malformation syndrome: a 28-year single-center retrospective study. J Pediatr. (2006) 149:393–400.
20. Shneider BL, Brown MB, Haber B, Whitington PF, Schwarz K, Squires R, et al. A multicenter study of the outcome of biliary atresia in the United States, 1997 to 2000. J Pediatr. (2006) 148:467–74. doi: 10.1016/j.jpeds.2005.12.054
Keywords: accessory spleen, torsion, biliary atresia splenic malformation syndrome (BASM), abdominal pain, congenital anomaly
Citation: Simon DA, Fleishman NR, Choi P, Fraser JD and Fischer RT (2020) Torsion of an Accessory Spleen in a Child With Biliary Atresia Splenic Malformation Syndrome. Front. Pediatr. 8:220. doi: 10.3389/fped.2020.00220
Received: 22 October 2019; Accepted: 14 April 2020;
Published: 04 May 2020.
Edited by:
Arjan Te Pas, Leiden University, NetherlandsReviewed by:
Jonathan M. Wells, Canterbury District Health Board, New ZealandAndrew S. Day, University of Otago, New Zealand
Copyright © 2020 Simon, Fleishman, Choi, Fraser and Fischer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: David A. Simon, ZGFzaW1vbiYjeDAwMDQwO2NtaC5lZHU=
 David A. Simon
David A. Simon Nathan R. Fleishman2
Nathan R. Fleishman2 Jason D. Fraser
Jason D. Fraser Ryan T. Fischer
Ryan T. Fischer