- 1Center for Health Outcomes and Policy Research, School of Nursing, University of Pennsylvania, Philadelphia, PA, United States
- 2College of Nursing and Health Innovation, University of Texas at Arlington, Arlington, TX, United States
- 3Department of Economics, Dartmouth College, Hanover, NH, United States
- 4School of Nursing, University of Pennsylvania, Philadelphia, PA, United States
- 5School of Nursing, University of Kansas, Kansas City, KS, United States
- 6College of Nursing, University of Michigan, Ann Arbor, MI, United States
- 7Department of Health Policy and Administration, The Pennsylvania State University, University Park, PA, United States
Background: The satisfaction of parents of infants in neonatal intensive care is important to parent-infant bonding and parents' ability to care for their baby, including after discharge. Given the principal caregiver role of nurses in this setting, parent satisfaction is influenced by high quality nursing care. Nursing care that is required but missed, such as counseling and support, might influence parent satisfaction. How missed nursing care relates to parent satisfaction is unknown.
Objective: To describe the satisfaction of parents of infants in neonatal intensive care and to determine how satisfaction relates to missed nursing care in a sample of USA nursing units.
Methods: The design was cross-sectional and correlational. Thirty neonatal intensive care units that participate in the National Database of Nursing Quality Indicators were recruited. To maximize sample variation in missed care, the highest and lowest quartile hospitals on missed nursing care, measured by nurse survey, were eligible. Ten parents of infants who were to be discharged were recruited from each site to complete a survey. Parent satisfaction was measured by the EMPATHIC-38 instrument, comprising five subscales: information, care and treatment, organization, parental participation, and professional attitude, and a total satisfaction score. Multivariate regression models were estimated.
Results: Parent satisfaction was high (5.70 out of 6.00). The prevalence of missed care was 25 and 51% for low and high missed care units, respectively, and 40% for all units. On average, nurses missed 1.06 care activities; in the low and high missed care units the averages were 0.46 and 1.32. Over 10% of nurses missed activities that involved the parent, e.g., teaching, helping breastfeeding mothers, and preparing families for discharge. One standard deviation decrease in missed care activities at the unit level was associated with a 0.08-point increase in parent satisfaction with care and treatment (p = 0.01).
Conclusion: Parents in USA neonatal intensive care units are highly satisfied. Neonatal intensive care nurses routinely miss care. Parent satisfaction with care and treatment is related to missed nursing care. Nursing care that is missed relates primarily to the care of the baby by the parents, which could have long term health and developmental consequences.
Introduction
Many parents of a critically ill infants are fully responsible for the infant's care upon discharge from the neonatal intensive care unit (NICU). During the infant's stay, the principal healthcare provider is the registered nurse. Effective nursing care, including communication with, and guidance and education of parents, can improve the parents' confidence and ability to care for their child at home. Therefore, communication is an integral part of family-centered care (1). When a nurse misses care, essential elements of nursing care like communication with parents does not take place. Missed nursing care occurs when required nursing care is omitted or delayed in response to multiple demands or inadequate resources (2). Missed nursing care in the NICU has not been linked to parent satisfaction. The purpose of this study was to determine the associations between missed nursing care and NICU parent satisfaction.
Background and Significance
Nursing and NICU Parent Satisfaction
Family-centered care in the NICU is regarded as a core strategy to improve the outcomes of critically ill infants because it acknowledges and addresses the key role of parents in the infant's health, both during inpatient care and following discharge (3). A core element of family-centered care is effective communication by nurses with parents (3). Nurse communication has been linked to NICU parent satisfaction (4–6).
When a nurse misses care related to the parent it may affect parent satisfaction. Nurses play a critical role in communicating with parents, providing education about the care of their preterm baby, and initiating breastfeeding support. Depending on the quality of nursing care of parents, including emotional support, teaching, counseling, and discharge preparation, parents may suffer emotional distress, have difficulty bonding with their infant, and be ill prepared to care for their baby after discharge.
Evidence from an integrative review of parent satisfaction with NICU care suggests that parent satisfaction with their overall NICU care experience has been high, with lower proportions of dissatisfaction across several countries, including the Unites States, the United Kingdom, Australia, Canada, South Africa, Israel, and the Netherlands (4). Communication has been found to be a consistent correlate of parent satisfaction in the NICU across parent satisfaction studies (4–6). Greater parental involvement in care is associated with better outcomes. For example, in a quasi-experimental study in a Chinese NICU, a parental educational intervention that encouraged active involvement in care for at least 4 h a day resulted in significantly better infant outcomes, including a higher breastfeeding rate and a lower readmission rate (7).
Missed Nursing Care
Over the past decade, researchers have examined missed nursing care as an indicator of the quality of nursing care. Two systematic reviews have documented the predictors and consequences of missed nursing care in various inpatient settings (8, 9). In adult populations, missed nursing care has been linked to patient satisfaction, adverse events, mortality, and readmission (10–14). Evidence about missed nursing care in NICUs is consistent with findings from adult settings and has been growing. NICU missed care literature can be described using three major categories: system factors that related to missed care, consequences of missed care, and missed care disparities across settings.
System factors, including work environments, nurse workloads, and infant acuity, have been shown to predict missed nursing care. In a sample of 5,862 NICU staff nurses reporting about 303 USA NICUs, nurses with higher workloads, poorer work environments, and higher acuity patients had higher odds of missed care (15). In nine Quebec NICUs, missed care was less frequent in better work environments (16). Data from 230 USA certified neonatal nurses suggested that system factors, such as unit census, contribute to missed care (17). In one USA NICU, at an academic medical center, caring for three or more infants was associated with 2.5 higher odds of missed nursing care, and subjective nurse workload ratings were associated with a 34% increase in the odds of missing a care activity during a shift (18).
Consequences for infant outcomes and parent satisfaction could result from missed care in the NICU. One study in a USA medical center linked delayed feeding (a type of missed care) of NICU infants to time required to achieve full oral feedings and length of stay (19). Nurses who worked in seven Quebec NICUs reported that missed discharge teaching was inversely associated with nurse-ratings of parent-infant readiness for discharge, and that missed parental support, teaching, and infant comfort care was associated with ratings of poorer pain control (20).
Disparities among populations exposed to missed care in the NICU is also a concern. For example, data from 134 USA NICUs suggested that nurses in NICUs with a larger proportion of Black infants, compared to all other infants, were assigned more patients on average and missed almost 50% more nursing care (21).
Study Contribution and Purpose
Missed nursing care is a modifiable characteristic of care settings. There no evidence yet on whether missed nursing care influences NICU parent satisfaction. Furthermore, multisite evidence from the USA about NICU parent satisfaction is not available. Our study, therefore, contributes by describing NICU parent satisfaction in a large USA NICU sample examining whether missed nursing care relates to variation in parent satisfaction. Multisite USA evidence will be valuable to practitioners internationally for comparison with the USA parent experience. Correlational evidence linking missed nursing care to parent satisfaction is a step toward identifying points of intervention to improve parent satisfaction. Our research may inform nurse managers about the dimensions of parent satisfaction and the relationship between missed care and parent satisfaction, so managers and staff can become aware of missed care and consider addressing it.
The purpose of this study was to describe the satisfaction of parents of infants in neonatal intensive care and to determine how satisfaction relates to missed nursing care in a sample of nursing units in the USA.
Methods
Design and Setting
The design was cross-sectional and correlational. The setting was the NICU.
Data Sources
Missed care was measured from a survey of registered nurses (RN) conducted in 2018 for the National Database of Nursing Quality Indicators® (NDNQI®), which is a voluntary program that collects data about nursing-sensitive indicators to improve patient care quality in hospitals (22). Parent satisfaction was measured from a survey of parents of NICU infants. American Hospital Association (AHA) Annual Survey data were utilized to measure hospital characteristics and the number of NICU beds. The NICU level was classified as reported to the NDNQI by the participating hospital.
NICU and Parent Samples
The target population included USA NICU nurses and parents. NICU inclusion criteria were having 2017 NDNQI RN survey data and falling in the top or bottom quartile on frequency of missed nursing care, as reported by staff nurse respondents and aggregated to the unit level. The top and bottom quartiles of the distribution were selected to achieve maximum variation in missed nursing care. The parent inclusion criteria were being the parent of a NICU infant being discharged to go home within the next 24 h. Exclusion criteria were if the infant died or was transferred to another NICU. An incentive of 25 US$ cash or gift card, depending on the institution's IRB requirements, was given to parents who completed the survey. In addition, because the parent survey was conducted in 2018, all NDNQI NICUs with 2018 nurse survey data, including the sample NICUs, were combined into a NDNQI 2018 NICU cohort to provide descriptive statistics for comparison with the sample that participated in the parent satisfaction study.
Procedures
NICU Screening, Recruitment, and Preparation for Data Collection
We screened 271 NICUs with 2017 NDNQI NICU nurse survey data and selected 160 (80 sites were selected from the top and bottom quartiles to achieve a minimum sample of 24). The basis for selecting 160 was the expected volunteer and completion rates from previous NDNQI projects: (30% volunteer rate; 55% of volunteers complete data collection) (160 × 0.3 = 48; 48 × 0.55 = 26, which is close to but >24). After five were omitted for multiple units in the same hospital and other reasons, 155 were invited to participate. Recruitment began in February 2018 for a project start date of July 2018. Hospital incentives for participating included 250 US$ payable to the nursing unit, free continuing education for registered nurses about NICU nursing systems research, and a 1-year subscription to American Nurse Today.
Each NICU assigned an on-site project coordinator affiliated with the hospital to facilitate data collection. Project coordinators were responsible for recruiting parents. When a NICU infant was expected to be discharged in the next 24 h, the nurse manager contacted the project coordinator. The project coordinator approached parents about the study and performed the informed consent process. The project coordinator maintained a record of eligible and recruited parents to calculate participation rate. Project coordinators documented cases in which parents either refused to participate or were missed. Typically, a parent was missed if an infant was discharged before the project coordinator could recruit the parent. To promote consistent data collection practices across sites, webinars were held on recruitment and data collection procedures.
Institutional Review Board (IRB) approval was obtained from the University of Pennsylvania for our protocol. Each NICU obtained IRB approval through reliance on the IRB at the University of Pennsylvania, by having the project coordinator join the research team as site principal investigator or obtaining separate IRB approval through their institution. Depending on the timing of IRB approval, data collection occurred on a rolling basis from July 2018 to February 2019.
Measures/Instruments
Demographic Questions
These included items about race/ethnicity, age range, level of completed education, and parent status (i.e., mother, father, both, guardian) of the respondent. Whether the infant weighed <1,500 g at birth was also included to capture very low birthweight status. Parents were asked the length of the infant's stay (in days), and on a typical day, how many hours the parent spent on the NICU.
EMPATHIC-38
A 38-item modified tool to measure parent satisfaction based on the original EMPowerment of PArents in THe Intensive Care 30 questionnaire (EMPATHIC-30) (23) was utilized. The EMPATHIC-30 was developed in the Netherlands to measure the satisfaction of parents of hospitalized children (23). The EMPATHIC-30 was shortened from the 65-item EMPATHIC and has demonstrated reliability and validity, while retaining essential content, and taking less time to complete (23). It encompasses the care by nurses and physicians as well as organization and cleanliness. A sample item is, “the nurses took action immediately when our child's condition worsened.” The research team, in consultation with the EMPATHIC developer (Latour), selected 6 items from the EMPATHIC-N, a 57-item parent satisfaction questionnaire which was developed for the NICU setting (24), to increase the content about the nurse's role. To increase the accuracy of item-level measurement, we separated the terms nurses and doctors into two items resulting in an addition of eight items rather than six. The eight items were included in the same domains as the EMPATHIC-N; the two instruments have consistent domains. The five EMPATHIC-38 domains are information (five items), care and treatment (12 items), organization (five items), parental participation (eight items), and professional attitude (eight items). Items were on a 1–6 Likert-type scale, with response options ranging from “certainly no” (1) to “certainly yes” (6), with a “not applicable” option. An overall score is calculated as the mean of all items.
Some of the original survey language in Dutch English was modified for USA English speakers for understandability, with Latour's approval. For our Spanish speaking USA population, we adapted a Spain Spanish version (25) to Latin American Spanish. The Latin American Spanish version was back translated by two independent reviewers who were fluent in English and Latin American Spanish until there were no discrepancies, indicating its accuracy. The psychometric properties of both adaptations were evaluated and found to be satisfactory, as will be detailed in a concurrent manuscript. Internal consistency reliability in the current sample was satisfactory, exceeding 0.70 for four of the EMPATHIC-38 domains. The fifth domain, Organization, had an alpha of 0.60. Concurrent validity was supported in significant positive correlations between the overall score and several indicators of parent satisfaction.
Missed Care
Missed care was measured by self-report, the most common method found in a recent systematic review that included 42 quantitative reports (26). The selected measure is a standard in the field (14, 26), comprising 12 care activities considered fundamental to the science and practice of nursing, such as patient surveillance. This set was augmented by four items designed for this study to address NICU outcomes of breastmilk feeding and hospital-acquired infection: breastfeeding support, timely feedings, hand hygiene, and central line maintenance/care. The NDNQI added “ambulation or range of motion” based on clinical rationale and consistency with similar missed care measures. The total number of missed care items was 17.
The NDNQI survey item we used to measure missed care asks, “On the most recent shift you worked, which of the following nursing activities were necessary but left undone because of time constraints?” Respondents are asked to check all that apply. Variables were created from the missed care responses: (1) a set of binary variables indicating whether any or no care was missed and whether each activity was missed and (2) a frequency variable for the number of missed nursing activities. The 30 sample units were classified as having high or low missed care based on their location in the top or bottom half of the missed care frequency distribution in 2018.
Data Analysis
Parent data from NICUs were linked by AHA ID to NDNQI nurse survey data and AHA hospital characteristics. Hospital and NICU characteristics for three groups were compared: the 30 recruited NICUs, all NDNQI NICUs with nurse survey data from 2018, and hospitals with a NICU from the AHA survey. Parent and infant characteristics for high missed care units, low missed care units, and all 2018 NDNQI NICUs were described. The average number of missed care items and the percent of nurses who missed at least one care activity was compared across high, low, and all 2018 NDNQI NICUs. The distribution of the prevalence of each missed care activity across all 2018 NDNQI NICUs. The correlation of the average number of care activities missed and parent satisfaction with care and treatment was calculated.
Mixed effects multi-level regression models were estimated for the effect of missed care frequency on each parent satisfaction domain and total parent satisfaction. For regression models, missed nursing care was calculated as the standardized average number of missed care activates at the unit level. Results were interpreted as the effect of a one standard deviation (SD) change in missed nursing care. Parent characteristics (i.e., Hispanic ethnicity, race, age, level of education) and an infant characteristic (i.e., low birth weight) were controlled for in all regression models. Regression model calculations were clustered at the unit level. The alpha level for significance was set at 0.05.
Results
Sample Characteristics
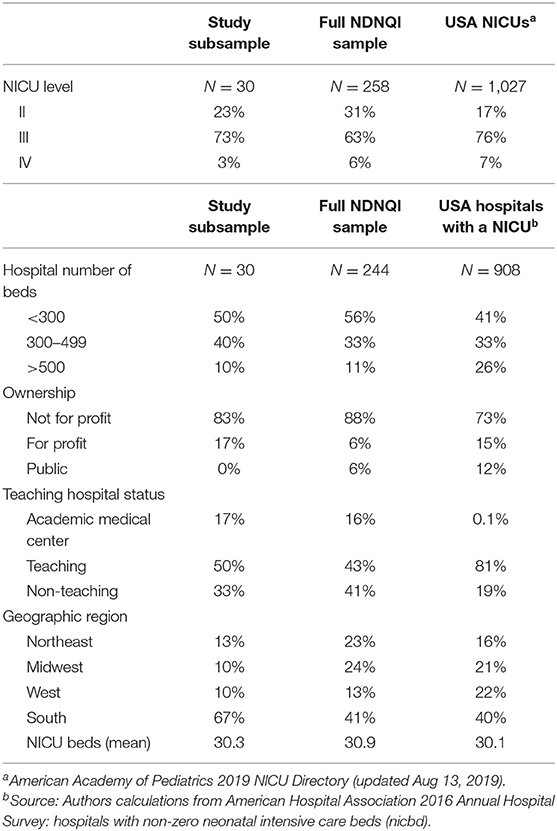
Forty NICUs volunteered (26% volunteer rate) and 30 participated (75% completion rate). The 30 NICUs comprised 15 low and 15 high missed care units from the top and bottom quartiles. The typical sample NICU was level III newborn care, and was in a non-profit, teaching hospital in the South with fewer than 500 beds (Table 1).
Although characteristics of both the full NDNQI sample and the population of USA hospitals with a NICU are presented in Table 1, we emphasize the comparison between our sample and the USA population to which we would expect to generalize our findings. Newborn care nursing units in the USA are classified into four levels, in which Level I is normal newborns and levels II through IV reflect increasing complexity of care. Our sample proportions of levels II, III, and IV were 23, 73, and 3%, quite similar to the national distribution of 17, 76, and 7%, respectively (Table 1). On most hospital characteristics, including size, teaching status, ownership, and number of NICU beds, our sample distribution was similar to that of the USA population. Our sample's hospitals were disproportionately located in the South (67 vs. 40% nationally). The average number of NICU beds in our sample was 30.3. For the NDNQI and national samples, the average number of NICU beds was about 30 (Table 1).
There were 300 parents surveyed: 10 from each NICU. Most respondents (73%) were mothers (Table 2). The typical NICU parent was non-Hispanic, White, between 25 and 34 years of age, and had at least a high school education; however, there was a range parents represented from different races, age groups, and education categories. Regarding race, most parents were White (59%), or Black or African American (21%). While about half the parents were 25–34 years old, about one fifth each were 18–24 years old or 35–44 years old. For highest level of education completed, about half had a high school degree or GED, two fifths had associate, bachelor's or higher degrees, and 8% had trade/vocational training. These characteristics did not differ across the low and high missed care unit sub-samples.
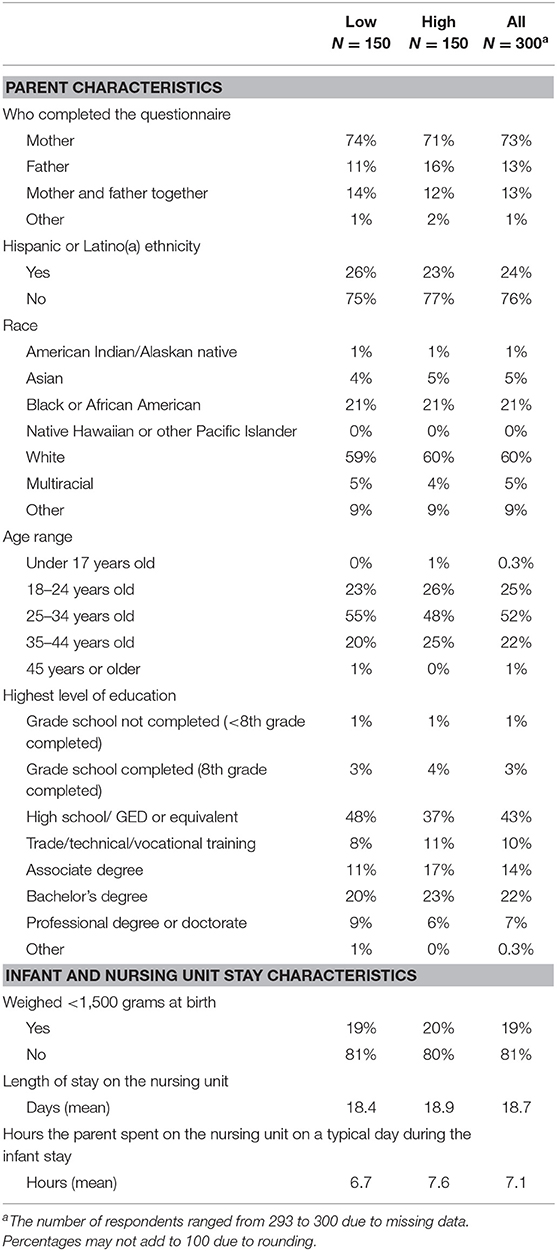
Table 2. Parent and infant characteristics in all 30 units and in units classified as low and high frequency of missed nursing care (N = 300 parents).
Most parents (81%) did not have a VLBW infant. The most common length of NICU stay for infants was 3 or 4 days (range = 1.5–266). Parents spent about 7 h a day on the unit, with parents in high missed care units spending one half-hour more on average than parents from low missed care units.
Missed Care Description
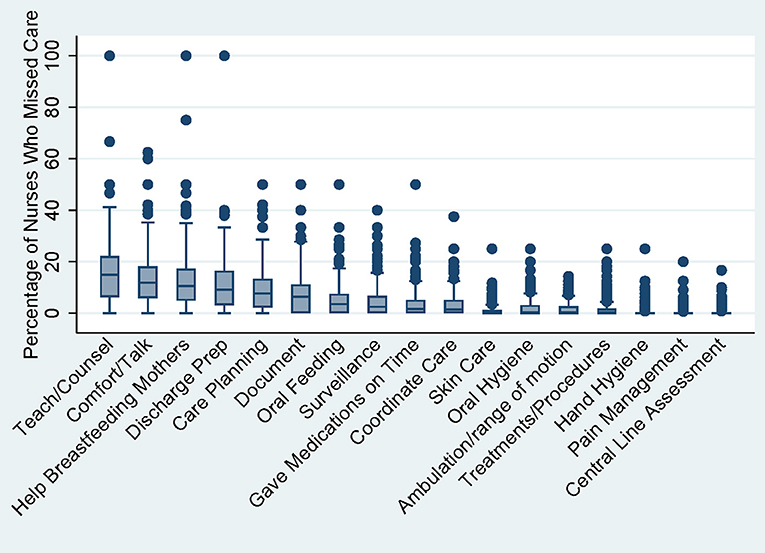
There were 258 NDNQI NICUs with nurse survey data in 2018 for comparison with our sample. Across these 258 units, the mean percentage of nurses who missed any care was 37% and the mean frequency of missed care items was 0.95 out of 17. The median percentage of nurses who missed care (i.e., prevalence) was highest for the following four care activities: teaching and counseling patients and families (15%), comfort and talk with patients (12%), help and counsel breastfeeding mothers (11%), and prepare patients and families for discharge (9%) (Figure 1). Prevalence was lowest (0%) for oral care, skin care, ambulation, treatment and procedures, hand hygiene, pain management, and central line assessment (Figure 1).
Table 3 displays means and standard deviations for the three missed care variables in low and high missed care units compared to all 258 NICUs surveyed in 2018. The average number of missed care activities (theoretical range from 1 to 17) was 0.46 for low missed care units, 0.95 for all units, and 1.32 for high missed care units. The percentage of nurses who missed at least one care activity was 25% for low missed care units, 38% for all units, and 51% in high missed care units. The units with higher missed care activities tended, on average, to have 2–5 times higher missed care on most items except for central line assessment and care (Table 3).
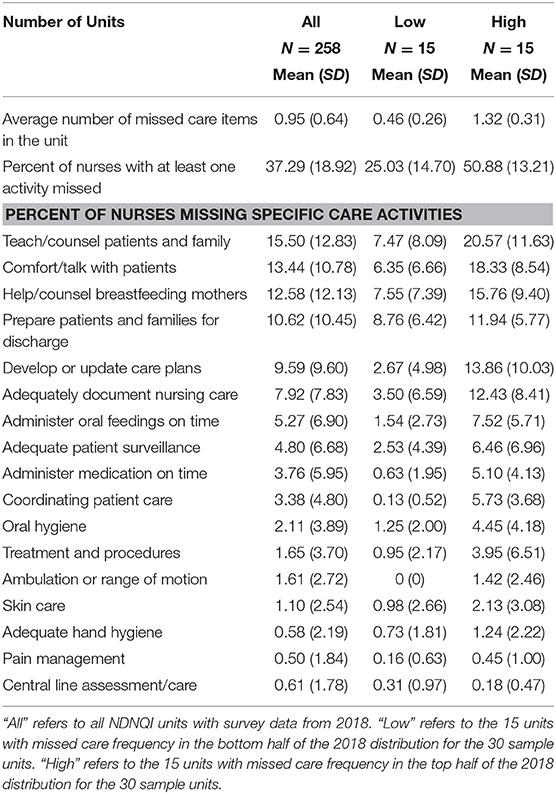
Table 3. Distribution of missed nursing care across 2018 NDNQI nursing units: low, all, and high missed care (unit-level).
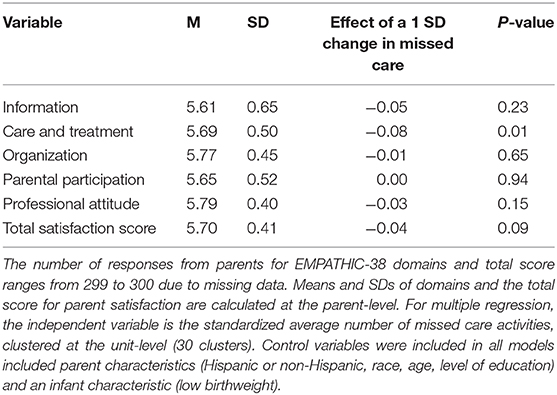
Parent Satisfaction Description
The average parent rating for total parent satisfaction was high at 5.70 (SD = 0.41) (theoretical range from 1 to 6). Of the five domains of the EMPATHIC-38 scale, parent satisfaction for our sample ranged from 5.61 (information domain) to 5.79 (professional attitude). There was little variation between mean scores and standard deviations for all EMPATHIC-38 subscales and the total satisfaction score (Table 4).
Relationship Between Missed Care and Parent Satisfaction
The average number of missed care activities was negatively correlated with the care and treatment domain of parent satisfaction (r = −0.43, p = 0.02) as it does in our Figure 2 graph. In linear regression models that controlled for parent and infant characteristics, a one standard deviation decrease in the standardized average number of missed care activities at the unit level was associated with a 0.08-point increase in parent satisfaction for the care and treatment domain of EMPATHIC-38 (b = −0.08, p = 0.01; Table 4). The association of missed care with the other domains of parent satisfaction (i.e., information, organization, parental participation, professional attitude) and the total parent satisfaction score was smaller in magnitude and not statistically significant (Table 4).
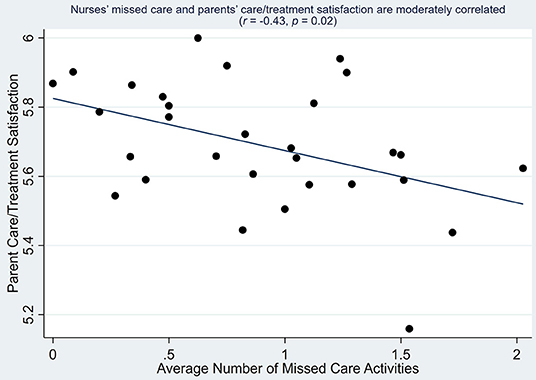
Figure 2. Correlation between parent satisfaction with care and treatment and average number of missed care activities (unit-level).
Discussion
Based on the key role that nurses play in caring for both the infant and its parents, we theorized that parental satisfaction would relate to nursing care. So, when nurses missed care, we expected it to affect the parent's experiences. In fact, our study of 945 staff nurses and 300 parents in 30 USA NICUs showed that at units where more nursing care was missed, parents reported less satisfaction with care and treatment. To our knowledge, no other research has established a relationship between missed care and parent satisfaction, demonstrating a novel contribution of this paper.
Parent satisfaction matters because the parents' experiences during the infant's hospitalization lay the foundation for their parental role. Therefore, the significance of NICU parent satisfaction cannot be overstated. Nurses are a critical part of nurturing the parent-infant dyad. The NICU is a nurse intensive setting, where typically, one nurse cares for two infants (27). Our findings imply that the centrality of nursing to this high intensity population is important for all health care providers in this setting as well as hospital administrators to recognize. The parent/newborn dyad is unique among inpatient populations, even as compared to other intensive pediatric settings, because of this critical stage of human development. The types of care that are missed most frequently relate to the parents' role. These include teaching and counseling, comforting and talking, breastfeeding support, and discharge preparation. Breastmilk is vital to the newborn development, particularly for critically ill infants, and yet the challenges of providing breastmilk to this infant group are considerable.
The care activities missed most frequently in our study, i.e., teaching and counseling, comforting and talking, breastfeeding support, and discharge preparation, require good communication practices with the parent. Our finding that frequently missed care related to communication influences parent satisfaction is consistent with other studies that link communication and parent satisfaction in the NICU (4–6).
The care and treatment domain of the EMPATHIC-38 comprises 12 items. Two items refer to the team working closely together and attending to the prevention and treatment of pain in the child. The remaining items comprise five distinct statements asked about nurses and doctors separately, yielding ten items. These five statements refer to discharge preparation, comfort, emotional support, and acting immediately if the child's condition worsened. The high degree of congruence in content between what nurses miss most frequently and the items in the care and treatment domain indicates that parents may have awareness of missed care and it influences their satisfaction.
Parents of NICU infants in our sample were highly satisfied. This finding is consistent with NICU parent satisfaction reported across other samples globally in the NICU (24, 28) and pediatric intensive care unit (PICU) (25). For example, in a Dutch sample from which the EMPATHIC-N was derived, values ranged from 5.22 to 5.57 in a cohort of 59 parents used for confirmatory analysis (24). In that sample, the highest scores were given for Professional Attitude and the lowest scores for Information (24). Mean scores for individual items of the Italian EMPATHIC-N in an Italian sample ranged from 4.3 to 5.9 (28). In a Brazilian sample of parents, the most frequently reported satisfaction rating was between 4 and 5 for items of the EMPATHIC-N (29). In Spain, parents rated their satisfaction in the PICU as high; above 5 for most items of the EMPATHIC-30 (25).
Missed nursing care was common in our sample. Thirty-eight percent of nurses missed care on their previous shift. The average frequency of activities missed was 0.95. These statistics are similar to those reported from two earlier large samples. Compared to a sample of 2016 NDNQI NICUs with nurse survey data, the 2018 prevalence and frequency were higher: in 2016 the prevalence was 36% and the frequency was 0.88 activities (15). In a sample of 134 NICUs from four large USA states from 2006, the prevalence was 44% and the frequency was 1.23 activities (21).
Over ten percent of nurses missed activities that involve the parents, i.e., teach/counsel patients and family, comfort/talk with patients, help/counsel breastfeeding mothers, and prepare patients and families for discharge. These four activities have the most direct impact on family-centered care, as compared to physical elements of care such as skin care or treatments and procedures. These results are consistent with evidence from province-wide samples of Quebec NICUs in 2007–2008, and in 2014, which showed that the most frequently missed activities were discharge planning, parental support and teaching, and comfort care (16, 20).
In this study we measured parent satisfaction within 24 h up to expected discharge. This timing was consistent with that of previous studies, which surveyed NICU parents prior to discharge (25, 30), or on the day of discharge and up to 3 days after discharge (28). In other parent satisfaction studies, Latour et al. surveyed parents 2–3 weeks after discharge of a child from the PICU (23, 31) and 3–4 weeks after discharge of infants from the NICU (24). If satisfaction was measured later for NICU parents, e.g., 1 week after discharge, it might differ from the viewpoint at discharge. A later assessment would incorporate the parent's perspective after the parent has had time to be at home to care for the infant—and see if they felt they were adequately prepared (through nursing teaching, counseling, and education) to care for their infant at home after discharge. Future research in larger samples should be conducted to provide additional evidence about how missed nursing care relates to parent satisfaction.
Limitations
The NICU sampling frame was NDNQI hospitals, which due to participation in a voluntary benchmarking database for quality of care, may not represent USA NICUs. The NICU sample was recruited based on high and low reported missed care values. The results do not necessarily represent all NICUs. The missed care data were unit-level aggregates and did not apply directly to the parent/infant dyads represented in our sample. As parent surveys were conducted at discharge in the hospital, parent data did not reflect satisfaction after the parents took the baby home. The geographic distribution of sample hospitals was disproportionally Southern, but all geographic regions were represented.
Conclusion
Parents in USA neonatal intensive care units are highly satisfied at the point of discharge. Neonatal intensive care nurses routinely miss required care activities. Parent satisfaction with care and treatment is significantly related to the frequency of missed nursing care. The care activities that nurses miss relate primarily to the care of the baby by the parents once discharged, which could have long term health and developmental consequences.
Data Availability Statement
The nurse survey data underlying the study are not available to the public as the project does not meet the National Institutes of Health minimum budget requiring data sharing. The nurse survey data are restricted due to a data use agreement with Press Ganey, Inc. The parent survey data may be available from the corresponding author. The National Database of Nursing Quality Indicators® (NDNQI®) data were supplied by Press Ganey Associates, Inc. Press Ganey Associates, Inc. specifically disclaims responsibility for any analyses, interpretations, or conclusions.
Author Contributions
EL, JR, and DS: study concept and design. EL, EC, and JS: data acquisition. EL, JS, JR, DS, EC, and LH: data analysis and interpretation. EL, JS, DS, JR, BK, and LH: manuscript preparation. All authors reviewed and edited the final manuscript.
Funding
This project was supported by grant number R01HS024918 from the Agency for Healthcare Research and Quality. JS was supported by the National Institutes of Health, National Institute of Nursing Research (Grant Number: T32NR007104, Aiken, PI) during parent satisfaction data collection for this project.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Ding X, Zhu L, Zhang R, Wang L, Wang TT, Latour JM. Effects of family-centred care interventions on preterm infants and parents in neonatal intensive care units: a systematic review and meta-analysis of randomised controlled trials. Aust Crit Care. (2019) 32:63–75. doi: 10.1016/j.aucc.2018.10.007
2. Kalisch BJ, Landstrom GL, Hinshaw AS. Missed nursing care: a concept analysis. J Adv Nurs. (2009) 65:1509–17. doi: 10.1111/j.1365-2648.2009.05027.x
3. Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. (2017) 45:103–28. doi: 10.1097/CCM.0000000000002169
4. Butt ML, McGrath JM, Samra HA, Gupta R. An integrative review of parent satisfaction with care provided in the neonatal intensive care unit. J Obstet Gynecol Neonatal Nurs. (2013) 42:105–20. doi: 10.1111/1552-6909.12002
5. Wigert H, Blom MD, Bry K. Parents' experiences of communication with neonatal intensive-care unit staff: an interview study. BMC Pediatr. (2014) 14:1–8. doi: 10.1186/s12887-014-0304-5
6. Sankar V, Batra P, Saroha M, Sadiza J. Parental satisfaction in the traditional system of neonatal intensive care unit services in a public sector hospital in North India. South Afr J Child Health. (2017) 11:54–7. doi: 10.7196/SAJCH.2017.v11i1.1253
7. Lv B, Gao XR, Sun J, Li TT, Liu ZY, Zhu LH, et al. Family-centered care improves clinical outcomes of very-low-birth-weight infants: a quasi-experimental study. Front Pediatr. (2019) 7:138. doi: 10.3389/fped.2019.00138
8. Papastavrou E, Andreou P, Efstathiou G. Rationing of nursing care and nurse-patient outcomes: a systematic review of quantitative studies. Int J Health Plann Manage. (2014) 29:3–25. doi: 10.1002/hpm.2160
9. Recio-Saucedo A, Dall'Ora C, Maruotti A, Ball J, Briggs J, Meredith P, et al. What impact does nursing care left undone have on patient outcomes? Review of the literature. J Clin Nurs. (2018) 27:2248–59. doi: 10.1111/jocn.14058
10. Schubert M, Glass TR, Clarke SP, Aiken LH, Schaffert-Witvliet B, Sloane DM, et al. Rationing of nursing care and its relationship to patient outcomes: the Swiss extension of the international hospital outcomes study. Int J Qual Health Care. (2008) 20:227–37. doi: 10.1093/intqhc/mzn017
11. Schubert M, Clarke SP, Aiken LH, de Geest S. Associations between rationing of nursing care and inpatient mortality in Swiss hospitals. Int J Qual Health Care. (2012) 2012:3. doi: 10.1093/intqhc/mzs009
12. Kalisch BJ, Xie B, Dabney BW. Patient-reported missed nursing care correlated with adverse events. Am J Med Qual. (2013) 29:415–22. doi: 10.1177/1062860613501715
13. Brooks Carthon JM. The quality of hospital work environments and missed nursing care are linked to heart failure readmissions: a cross sectional study of US hospitals. BMJ Qual Saf. (2015) 24:255–63. doi: 10.1136/bmjqs-2014-003346
14. Lake ET, Germack HD, Viscardi MK. Missed nursing care is linked to patient satisfaction: a cross-sectional study of US hospitals. BMJ Qual Saf. (2016) 25:535–43. doi: 10.1136/bmjqs-2015-003961
15. Lake ET, Staiger DO, Cramer E, Hatfield LA, Smith JG, Kalisch BJ, et al. Association of patient acuity and missed nursing care in U.S. neonatal intensive care units. Med Care Res Rev. (2018). doi: 10.1177/1077558718806743. [Epub ahead of print].
16. Rochefort CM, Clarke SP. Nurses' work environments, care rationing, job outcomes, and quality of care on neonatal units. J Adv Nurs. (2010) 66:2213–24. doi: 10.1111/j.1365-2648.2010.05376.x
17. Tubbs-Cooley HL, Pickler RH, Younger JB, Mark BA. A descriptive study of nurse-reported missed care in neonatal intensive care units. J Adv Nurs. (2015) 71:813–24. doi: 10.1111/jan.12578
18. Tubbs-Cooley HL, Mara CA, Carle AC, Mark BA, Pickler RH. Association of nurse workload with missed nursing care in the neonatal intensive care unit. JAMA Pediatr. (2019) 173:44–51. doi: 10.1001/jamapediatrics.2018.3619
19. Tubbs-Cooley HL, Pickler RH, Meinzen-Derr JK. Missed oral feeding opportunities and preterm infants' time to achieve full oral feedings and neonatal intensive care unit discharge. Am J Perinatol. (2015) 32:1–8. doi: 10.1055/s-0034-1372426
20. Rochefort CM, Rathwell BA, Clarke SP. Rationing of nursing care interventions and its association with nurse-reported outcomes in the neonatal intensive care unit: a cross-sectional survey. BMC Nurs. (2016) 15:46. doi: 10.1186/s12912-016-0169-z
21. Lake ET, Staiger D, Edwards EM, Smith JG, Rogowski JA. Nursing care disparities in neonatal intensive care units. Health Serv Res. (2018) 53(Suppl. 1):3007–26. doi: 10.1111/1475-6773.12762
22. Montalvo I. The national database of nursing quality indicators® (NDNQI®). Online J. Issues Nurs. (2007) 12. doi: 10.3912/OJIN.Vol12No03Man02
23. Latour JM, Duivenvoorden HJ, Tibboel D, Hazelzet JA. The shortened EMpowerment of PArents in THe Intensive Care 30 questionnaire adequately measured parent satisfaction in pediatric intensive care units. J Clin Epidemiol. (2013) 66:1045–50. doi: 10.1016/j.jclinepi.2013.02.010
24. Latour JM, Duivenvoorden HJ, Hazelzet JA, van Goudoever JB. Development and validation of a neonatal intensive care parent satisfaction instrument. Pediatr Crit Care Med. (2012) 13:554–9. doi: 10.1097/PCC.0b013e318238b80a
25. Pilar Orive FJ, Basabe Lozano J, Lopez Zuniga A, Lopez Fernandez YM, Escudero Argaluza J, Latour JM. [Spanish translation and validation of the EMPATHIC-30 questionnaire to measure parental satisfaction in intensive care units]. An Pediatr. (2018) 89:50–7. doi: 10.1016/j.anpede.2017.08.006
26. Jones TL, Hamilton P, Murry N. Unfinished nursing care, missed care, and implicitly rationed care: State of the science review. Int J Nurs Stud. (2015) 52:1121–37. doi: 10.1016/j.ijnurstu.2015.02.012
27. Rogowski JA, Staiger DO, Patrick TE, Horbar JD, Kenny MJ, Lake ET. Nurse staffing in neonatal intensive care units in the United States. Res Nurs Health. (2015) 38:333–41. doi: 10.1002/nur.21674
28. Dall'Oglio I, Fiori M, Tiozzo E, Mascolo R, Portanova A, Gawronski O, et al. Neonatal intensive care parent satisfaction: a multicenter study translating and validating the Italian EMPATHIC-N questionnaire. Ital J Pediatr. (2018) 44:5. doi: 10.1186/s13052-017-0439-8
29. Gomez DB, Vidal SA, Lima LC. Brazilian adaptation and validation of the Empowerment of Parents in the Intensive Care-Neonatology (EMPATHIC-N) questionnaire. J Pediatr. (2017) 93:156–64. doi: 10.1016/j.jped.2016.06.007
30. Papamichael E, Ioannou M, Talias MA. EMPATHIC-N in a Greek-Cypriot sample: confirming its factorial structure. BMC Health Serv Res. (2018) 18:968. doi: 10.1186/s12913-018-3793-3
Keywords: parent satisfaction, missed nursing care, neonatal intensive care unit, infant, patient satisfaction, nurses, hospitals
Citation: Lake ET, Smith JG, Staiger DO, Hatfield LA, Cramer E, Kalisch BJ and Rogowski JA (2020) Parent Satisfaction With Care and Treatment Relates to Missed Nursing Care in Neonatal Intensive Care Units. Front. Pediatr. 8:74. doi: 10.3389/fped.2020.00074
Received: 20 December 2019; Accepted: 14 February 2020;
Published: 18 March 2020.
Edited by:
Jos M. Latour, University of Plymouth, United KingdomReviewed by:
Carole Ann Kenner, The College of New Jersey, United StatesMats Eriksson, Örebro University, Sweden
Copyright © 2020 Lake, Smith, Staiger, Hatfield, Cramer, Kalisch and Rogowski. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eileen T. Lake, ZWxha2VAbnVyc2luZy51cGVubi5lZHU=
 Eileen T. Lake
Eileen T. Lake Jessica G. Smith
Jessica G. Smith Douglas O. Staiger3
Douglas O. Staiger3