- 1Department of Anesthesiology, Fuwai Hospital, National Center of Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
- 2Department of Information, Fuwai Hospital, National Center of Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
- 3Center for Pediatric Cardiac Surgery, Fuwai Hospital, National Center of Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
- 4Department of Anesthesiology, Chongqing Hospital of Traditional Chinese Medicine, Chongqing, China
Background: Prolonged pleural effusion (PPE) contributes to adverse outcomes after total cavopulmonary connection (TCPC) completion. We aimed to identify risk factors for PPE following TCPC surgery.
Methods: We studied a retrospective cohort of 525 who undergoing TCPC surgery from 2010 to 2019. We defined PPE as the duration of pleural effusion exceeding 14 days. Logistic regression was applied to identify risk factors for PPE and Cox regression was used to identify risk factors for predicting the duration of pleural effusion. The impacts of PPE on the short-term outcomes were evaluated.
Results: The rate of PPE was 27.4% in our study and independent risk factors for PPE included: young age, no fenestration, low postoperative total protein, prolonged mechanical ventilation and chylothorax. These predictors were also achieved in the Cox regression for predicting the duration of pleural effusion. The applicability of the model was acceptable in different subgroups, which derived from the total cohort. Patients with PPE were associated with more renal replacement treatment, longer length of ICU and hospital stay, more hospitalization costs and a higher rate of in-hospital mortality.
Conclusions: PPE in our study occurs at a relatively lower rate than that reported in previous studies and patients with PPE was associated with higher rate of in-hospital mortality when compared to patients without PPE. Young age, no fenestration, low postoperative total protein, prolonged mechanical ventilation, and chylothorax were identified as independent risk factors to predict PPE. A preventive strategy that targets the identified risk factors to reduce the incidence of PPE following TCPC surgery could be beneficial for in-hospital outcomes, and the model needs further validation before its application.
Introduction
Total cavopulmonary connection (TCPC) is one of the most frequently performed procedures in children with complex congenital heart disease. Currently, there are about 22,000 and 50,000 cases of functionally univentricular heart disease in Europe and the US, respectively (1). The early and late mortality after TCPC surgery was about 2.9 and 3.4% (2, 3). Although significant advances in surgical techniques had been made in the past years, numerous challenges remain to care for these patients. Following TCPC surgery, various short-term morbidities may occur, such as prolonged pleural effusion (PPE), arrhythmias, acute kidney injury, etc., which are associated with adverse in-hospital and long-term outcomes.
Following cardiac surgery, pleural effusion is a common complication with potential impact on outcomes. In previous studies, pleural effusion has been shown a notable risk factor for prolonged ICU stay and long-term morbidities (4, 5), and PPE also independently increases the risk of early and late deaths (6, 7). Despite several risk factors for PPE were reported in the current literature, including cardiopulmonary bypass longer than 120 min, heterotaxy, no fenestration, increased pulmonary artery pressure, pulmonary atresia, low preoperative peripheral oxygen saturation, and postoperative infection (8–11). However, the studies did not include early postoperative biomarkers, which represent functions of main organs after the surgery, and the injuries of the main organs might influence the duration of pleural effusion. In addition, the studies might not be applicable to a Chinese setting, in which the age at operation is older than that in the developed countries.
To address the current knowledge gap, we aim to identify risk factors for PPE and to investigate the consequences of PPE following TCPC surgery.
Materials and Methods
Study Population
From July 2010 to May 2019, patients who received TCPC completion under cardiopulmonary bypass (CPB) at Fuwai Hospital were, respectively analyzed. Patients who died within 14 days after the surgery were excluded. The study was approved by the Research Ethics Board of Fuwai Hospital and all data were retrieved from electronic medical records.
Definition of Outcome Variables
PPE was defined as the postoperative duration of pleural effusion exceeding 14 days.
Data Collection and Variable Definition
All possible predicting variables were included on the basis of clinical judgment, literature review and availability in our hospital. The preoperative baseline data were collected: age at operation, weight, gender, body surface area, peripheral oxygen saturation (SpO2) inhaling air when admission to the hospital, preoperative pulmonary artery pressure, prior Glenn, prior B-T shunt, heterotaxy syndrome diagnosis, original anatomy and ventricle morphology. The following pre- and postoperative blood laboratory parameters were collected: count of white blood cell, neutrophil, lymphocyte, monocyte and platelet, levels of hemoglobin, prothrombin time, total protein, albumin, alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase, total bilirubin, serum creatinine, isoenzyme of creatine kinase-MB, lactate dehydrogenase and high-sensitivity C-reactive protein. The following preoperative echocardiography variables were collected: main ventricle ejection fraction, main ventricle end-diastolic diameter z-score, atrioventricular valve regurgitation and Nakata index. Intraoperative variables which reflected the status during the surgery included senior surgeons who performed TCPC procedure over 10 cases per year averagely, preoperative SpO2 inhaling 100% oxygen after intubation, CPB time, aortic cross-clamp time, creation of fenestration, internal tunnel procedure, concomitant atrioventricular valve surgery, minimal temperature during CPB, maximum vasoactive-Inotropic score (VIS) during surgery, postoperative SpO2 inhaling 50-60% oxygen after surgery and intraoperative fluid balance. The following postoperative variables were also collected: maximal lactic acid within 6 h after surgery, cumulative fluid balance within 72 h after surgery and postoperative pulmonary artery pressure when admission to ICU.
The preoperative variables were measured at the closest time before surgery and postoperative variables were the first measurements when admitted to the ICU. The diagnosis of chylothorax was reached by high concentration of triglycerides (110 mg/dL or > serum triglycerides) and lymphocytes (80% of cells) in the pleural effusion at the postoperative day 5–7. Renal replacement treatment included peritoneal dialysis and blood filtration.
Fluid balance (mL/kg) was calculated: Fluid balance = [(amount of crystalloids + colloids + packed red cell + plasma + platelets + enteral nutrition) – (blood loss + urine output + gastrointestinal losses + drain losses + dialysis or ultrafiltrate)]/weight. Z-scores indexed to body surface area were applied when calculating left ventricular end-diastolic diameter z-score. Estimated glomerular filtration rate (eGFR) was computed: eGFR = 0.413*height (cm) / serum creatinine (SCr) level (mg/dL) (12). VIS was calculated: dopamine (μg/kg/min) + dobutamine (μg/kg/min) + 10 * milrinone (μg/kg/min) + 50 * levosimendan (μg/kg/min) + 100 * epinephrine (μg/kg/min) + 100 * norepinephrine (μg/kg/min) + 10,000 * vasopressin (U/kg/min) (13).
Perioperative Management
Patients before TCPC were administrated with normal diet. CPB with or without aortic cross-clamping was chosen if necessary and ultrafiltration was used in all patients after CPB. All patients received extracardiac TCPC surgery and the conduit size was selected according the age and weight at the operation. All patients were admitted to the ICU after TCPC surgery. The biochemical testing for chylothorax was routinely examined in our hospital on postoperative day 5–7. The decision of chest tube removal was made if the drainage of pleural effusion <2 mL/kg/day/tube. Conventional anticoagulant therapy was started at night on the same day as the operation depending on coagulation function. In patients without chylothorax, low-fat diet was given after TCPC until chest tube removal; in those with chylothorax, low-fat diet was given until 6 weeks after discharge from hospital. Other managements were based on the routine practice of Fuwai Hospital.
Statistical Analysis
Missing data were imputed using the R package “missForest” with random forest algorithm. Distributions of the recorded data, imputed data, and mixed data were compared to assess the impact of the imputation process on the original data. Logistic regression using backward elimination method was applied to identify the predictors for PPE and Cox regression with backward elimination method was used for predicting the duration of pleural effusion. Variables with p ≤ 0.15 in univariate analysis were put into multivariate logistic and Cox models, and multicollinearity was evaluated before the variables were put into the multivariate logistic or Cox analysis. Ordinal logistic regression was applied to examine the relationship between different groups of pleural effusion duration (<14, 14–21, >21 days) and postoperative outcomes. Six subgroups were used to identify the application ability of the PPE model in different population. The calibration and discrimination ability of the model were assessed by calibration curve, Hosmer-Lemeshow goodness-of-fit test (HL test) and receiver operating characteristic curve (ROC). P ≤ 0.05 was deemed statistically significant. All analyses were performed in R software (version 3.6.0).
Results
Missing Data
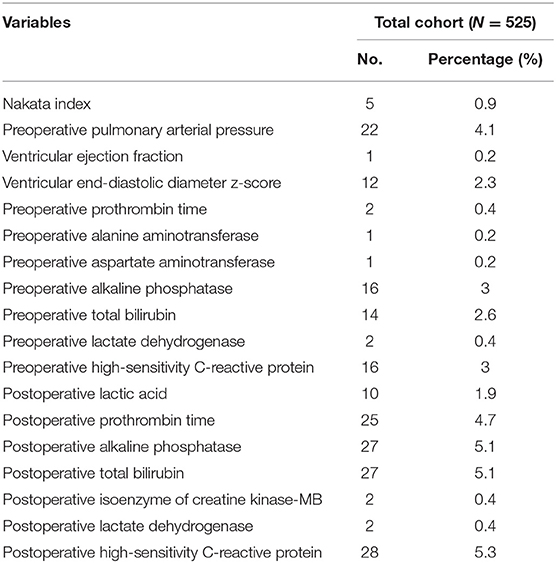
There were no significant differences among the distributions of the recorded data, imputed data and mixed data. The rate of missing data in this study ranged from 0.2% to 5.3%. In total 429 out of 525 records (82%) were complete cases. Among the 5 variables included in the logistic model, no variables had missing values (Table 1).
Characteristics of the Study Population
A total of 531 patients received TCPC surgery from July 2010 to May 2019 at our hospital. Six patients died within 14 days after the surgery and were excluded. A total of 525 patients finally included in the study.
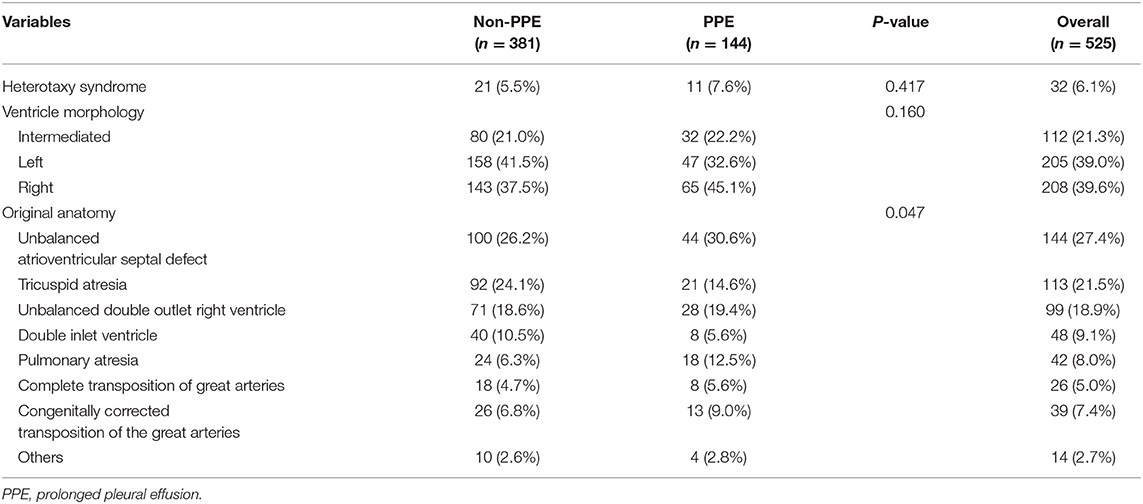
The median and quartile of the age in the total cohort were 6 (4.2, 11) years old. Among 525 patients, 6.1% patients had the diagnosis of heterotaxy syndrome, the percentages of right ventricle morphology and left ventricle morphology were 39.6 and 39%, respectively, the diagnosis of unbalanced atrioventricular septal defect, tricuspid atresia and unbalanced double outlet right ventricle account for 67.8% of the disease, 62.7% patients had the history of prior Glenn, 45.1% patients created a fenestration and 10.1% patents performed a concomitant atrioventricular valve surgery. All patients received CPB and 66.7% patients underwent aortic cross-clamping. The CPB and aortic cross-clamp time were 128 ± 67 min and 27.6 ± 46 min, respectively. The perioperative characteristics of the study patients with p < 0.15 in univariate analysis are displayed in Table 2 and the anatomy characteristics of the study patients are shown in Table 3.
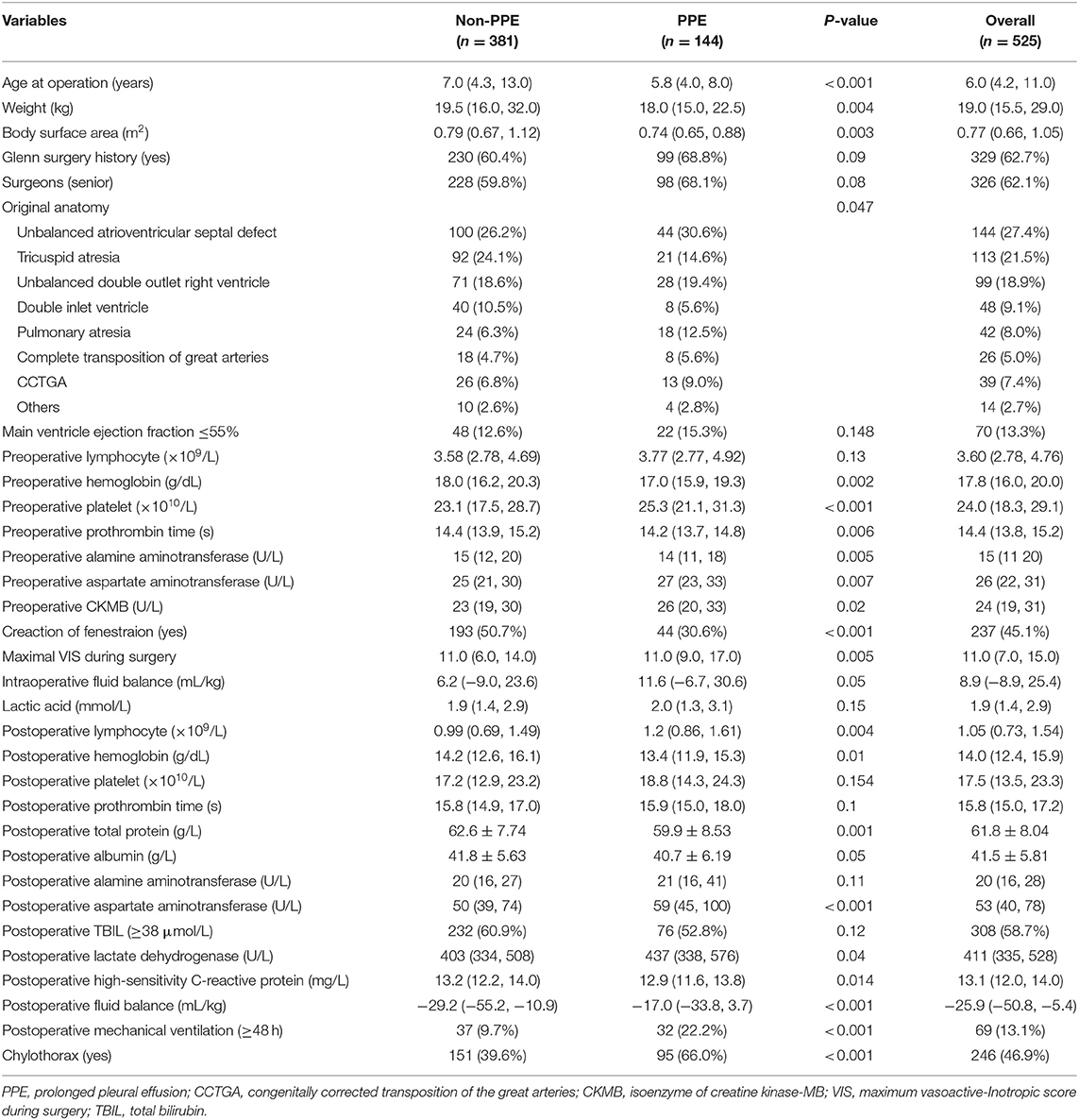
Table 2. The perioperative characteristics of the study patients with p < 0.15 in univariate analysis.
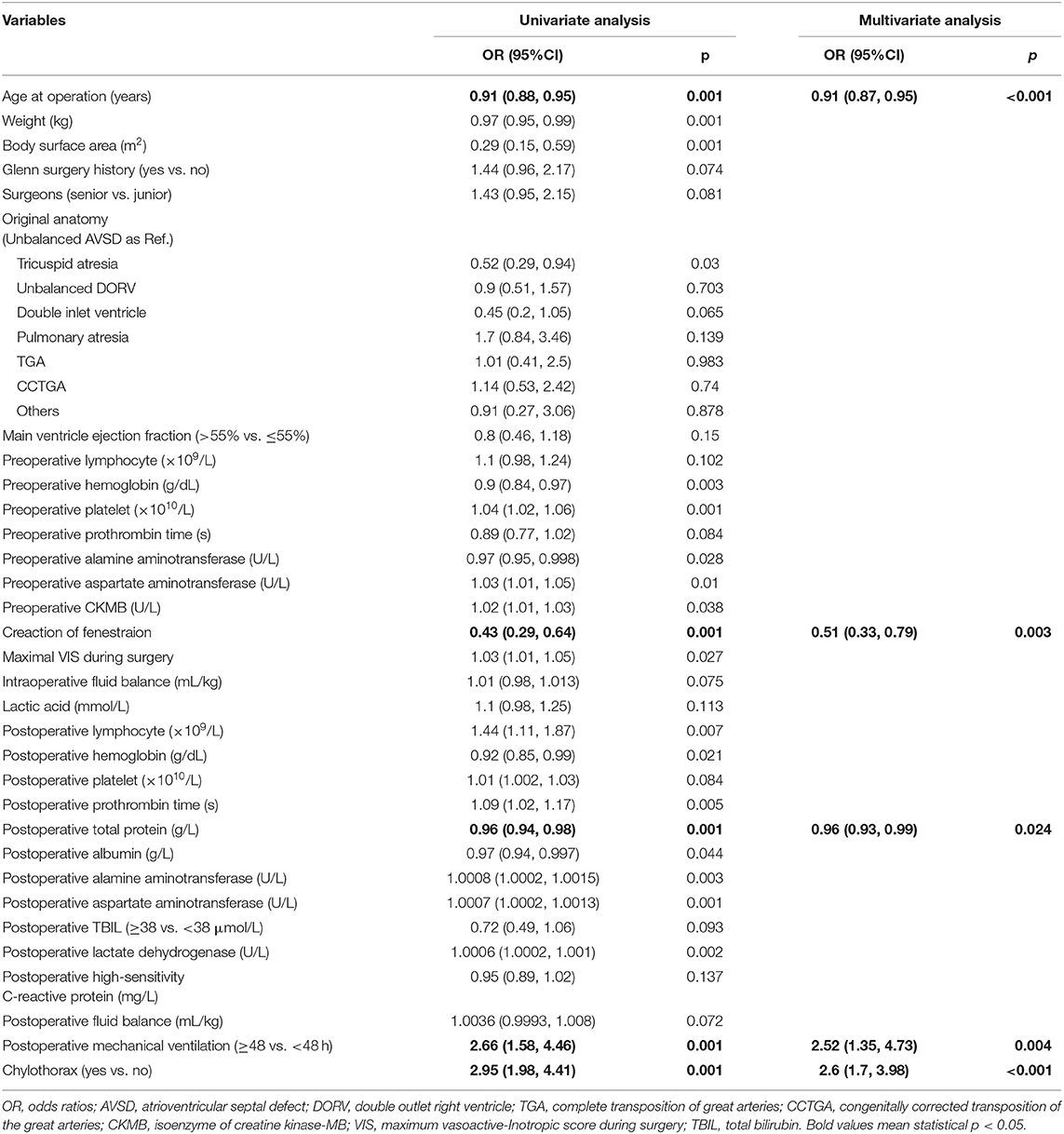
Logistic Regression for Predicting the PPE
Among the 64 variables, 32 variables had p ≤ 0.15 in the univariate logistic analysis and the five variables were the independent predictors in the multivariate logistic analysis. The five independent risk factors were young age at operation, no fenestration, low postoperative total protein level, prolonged mechanical ventilation and chylothorax. The odd ratios of the logistic analysis are shown in Table 4.
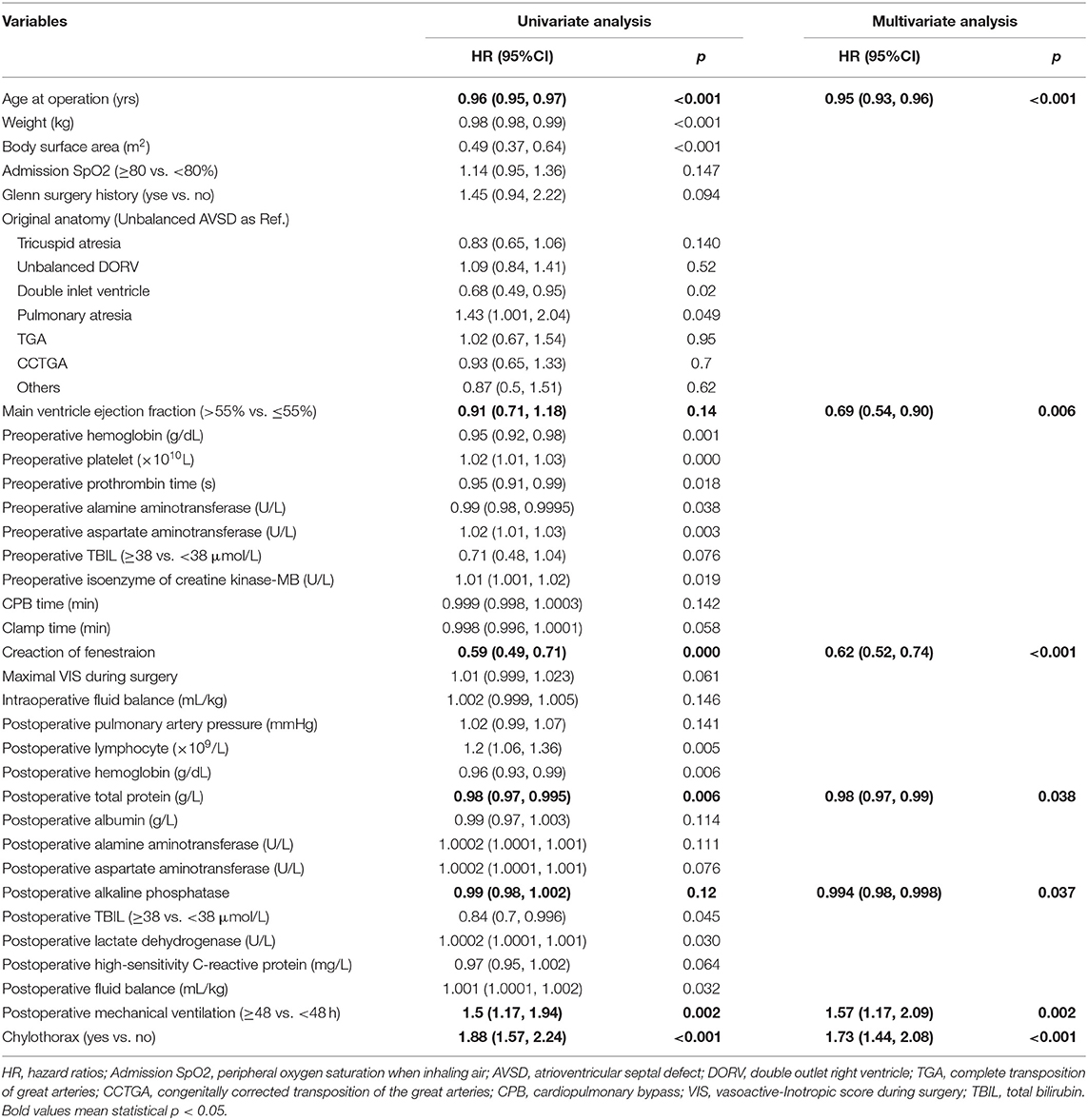
Cox Regression for Predicting the Duration of Pleural Effusion
Thirty-three variables with p ≤ 0.15 in the univariate Cox regression were entered into the multivariate Cox regression and seven variables were identified as independent factors for predicting the duration of pleural effusion. The seven independent predictors included age at operation, main ventricle ejection fraction, creation of fenestration, postoperative levels of total protein and alkaline phosphatase, postoperative mechanical ventilation and chylothorax. The hazard ratios of the logistic analysis are shown in Table 5.
Performance of the PPE Model in the Total Cohort and Different Subgroups
The area under ROC curve (AUC) and p-value of HL test in the total cohort was 0.75 (0.70, 0.80) and 0.99, respectively. The strongest discrimination ability was achieved in subgroup patients with left ventricle morphology with AUC of 0.77 (0.70, 0.85). The moderate discrimination ability (AUC ≥ 0.7) were also achieved in other 4 subgroups, which included patients with Glenn history, patients whose age between 2 and 4 years, patients diagnosed with right ventricle morphology and patients receiving the operation after 2017. However, poor discrimination (AUC <0.7) were achieved in subgroup patients with heterotaxy syndrome. Good fitness (HL test p > 0.05) were found in all six subgroups. The calibration and ROC curves are shown in Figure 1.
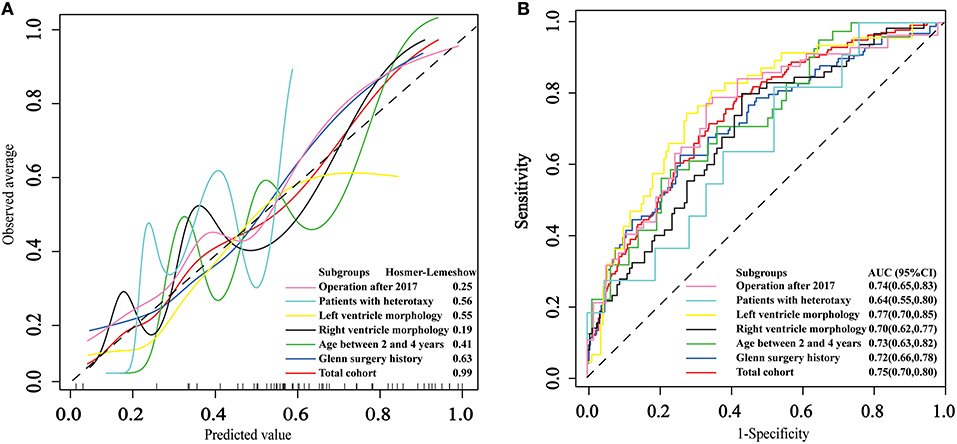
Figure 1. The application and performance of the model in the total cohort and 6 subgroups. (A) Calibration curves of the logistic model. (B) Receiver operating characteristic curves for prolonged pleural effusion.
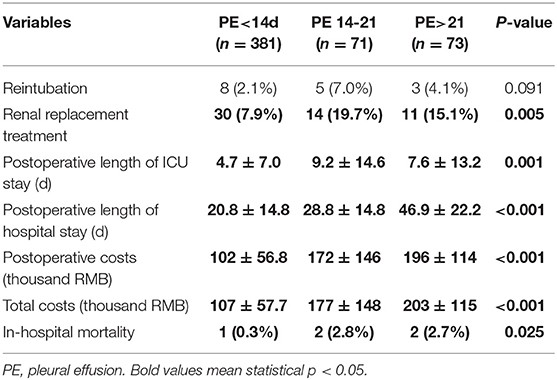
Postoperative Short Term Outcomes
The in-hospital mortality was 2.1% (11/533). The rate of PPE was 27.4% in this study and PPE was associated with in-hospital mortality. Compared to patients without PPE, patients with PPE were associated with longer length of ICU and hospital stay, higher rates of renal replacement treatment and increased hospitalization costs (Table 6).
Discussions
In our study, we identified 27.4% of all 525 patients as having PPE following TCPC surgery and the independent factors for PPE were age at operation, creation of fenestration, postoperative total protein level, postoperative mechanical ventilation and chylothorax. These predictors were also independent factors for predicting the duration of pleural effusion in Cox regression. The length of hospital stay increased by 18 days and the hospitalization costs increased by 61.7 thousand RMB in patients with PPE after TCPC surgery. Our findings help to stratify high-risk patients and strategies that target the identified risk factors might improve the in-hospital outcomes.
The application of the PPE logistic model to six subgroups were evaluated, because the characteristics of the total cohort were different from those in developed countries, such as age, prior Glenn, the ratio of right ventricle morphology to left ventricle morphology, etc. (2, 3, 11), one of the reasons was that the relatively poorer economic status in our country could lead to the consequences that patients come to the hospital later and receive surgery at a bigger age. In our study, the model had good fitness in the total cohort and six subgroups, and its discrimination ability in the total cohort and subgroups was acceptable. Therefore, the model derived from this study was applicable to not only the Chinese population but also the subgroups, which may be similar to those in other countries.
Different definition for PPE leads to different incidence of PPE. Previous studies had empirically predefined the cutoff value for prolonged duration of pleural effusion as 14 days and the incidence of the PPE was 34.2% (10), which was relatively higher than that in our study (27.4%). However, there is still no consensus on the definition of PPE. In this study, we performed both logistic and Cox regression analysis to free from the adverse effects of dichotomy definition on the results.
No fenestration was an independent factor in our study. Creation of fenestration was recommended as an effective procedure during TCPC operation (14) because fenestration can benefit patients from increased preload of the systemic ventricle if pulmonary blood flow is limited and helps to reduce pulmonary artery pressure if a pulmonary hypertensive crisis occurs. The presence of fenestration was nearly 45.1% in our patients, with a higher rate in more recent years. Our findings were consistent with the study from Zou et al., which found that the creation of fenestration can lower the risk of PPE (9). Overall, fenestration should be performed in patients with high risk for PPE because of its reduction in morbidities and mortality following TCPC surgery (15).
It is noteworthy that a shorter duration of mechanical ventilation predicts lower risk of PPE in our study. Previous studies suggested that early extubation including extubation in operation room is a safe and effective practice following TCPC surgery (16). Furthermore, recent studies demonstrated that prolonged mechanical ventilation after TCPC surgery was associated with adverse in-hospital outcomes, and that early extubation could produce clinical benefits in these patients, such as shorter length of ICU and hospital stay (17, 18). Our data added further evidence to support this opinion by showing that prolonged mechanical ventilation could heighten the risk of PPE and extend length of hospital stay in patients after TCPC surgery. One of the possible explanations behind this finding is that a rise in intra-thoracic pressure and central venous pressure, which is produced by mechanical ventilation, could lead to a decline in lymphatic drainage and reabsorption of pleural fluid (19). In addition, patients with prolonged mechanical ventilation usually require more fluid intake, which might aggravate the PPE. Therefore, maintaining an optimal duration of mechanical ventilation should be one of the prioritized goals in the perioperative management of patients following TCPC surgery.
In our study, young age was an independent risk factor for PPE, which was consistent with the results from Fedderly's study (20). This could be explained by the possible reason that young children are easier to suffer from injuries because the surgery on young children is much more complex than that in adults.
Our findings provide references for both clinical management and future research on complication following TCPC surgery. Our study suggested that optimizing the patents' selection, creation of fenestration in high-risk patients, improving postoperative total protein levels, avoiding prolonged mechanical ventilation and positively dealing with chylothorax can help to lower the risk of PPE in patients after TCPC surgery, shorten length of ICU and hospital stay, and reduce unnecessary hospitalization costs.
Limitations
There are several limitations in this study. Firstly, this study had a retrospective design. Although a large number of variables were put into the multivariate model to control for the confounders, certain unknown heterogeneities could exist and a patient selection bias may be present due to the non-random design of this study. In addition, the causal association between duration of mechanical ventilation and PPE can not be achieved in this retrospective study. Secondly, perioperative management strategies were to some extent determined by the subjective judgment of the anesthesiologists and the routine practice standards of Fuwai Hospital, so the conclusions drawn from this study could be subject to changes due to the growing experiences of doctors and the modifications of management standards of our hospital. Thirdly, the discrimination power of the model is not strong (AUC < 0.8). Maybe the model did not include other important variables, such as the complexity of the surgery process, which can not be exactly measured, and some catheter parameters like cardiac output, pulmonary vascular resistance, which was measured in some patients in our hospital. Our study could not demonstrate the exact relationship between postoperative infection and PPE. Fourthly, external validation of the model is warranted before its use in clinical practice. Lastly, the lack of data on long-term mortality could limit this study.
Conclusions
The incidence of PPE in our study was relatively lower than that suggested by previous study and compared to patients without PPE, patients with PPE were associated with a higher incidence of in-hospital mortality. We identified young age, no fenestration, low postoperative total protein, prolonged mechanical ventilation, and chylothorax as independent risk factors to predict PPE. A preventive strategy that targets these factors might reduce the incidence of PPE and shorten length of ICU and hospital stay, and reduce unnecessary hospitalization costs.
Data Availability Statement
The datasets generated for this study will not be made publicly available Because of data protection policy in our hospital.
Ethics Statement
This retrospective study was approved by the Institutional Review Boards of Fuwai Hospital, and informed consent was waived because of its retrospective nature.
Author Contributions
All authors contributed extensively to the work presented in this paper. FY, YJ, and SL proposed the idea of this investigation. QL, WZ, LZ, HW, YLi, and XW were responsible for the collection of data and material. QL helped with the statistical analysis and wrote the manuscript. FY, YJ, ZS, and YLiu helped to revise the manuscript. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
For supports in retrieving the data, we thank Weinan Chen from the Department of Information, Fuwai Hospital, National Center of Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, 100037, China.
References
1. van der Ven JPG, van den Bosch E, Bogers AJCC, Helbing WA. State of the art of the Fontan strategy for treatment of univentricular heart disease. F1000Research. (2018) 7:935. doi: 10.12688/f1000research.13792.1
2. Akintoye E, Veldtman GR, Miranda WR, Connolly HM, Egbe AC. Optimum age for performing Fontan operation in patients with univentricular heart. Congenit Heart Dis. (2018) 14:138–9. doi: 10.1111/chd.12690
3. Kverneland LS, Kramer P, Ovroutski S. Five decades of the Fontan operation: a systematic review of international reports on outcomes after univentricular palliation. Congenit Heart Dis. (2018) 13:181–93. doi: 10.1111/chd.12570
4. Allen KY, Downing TE, Glatz AC, Rogers LS, Ravishankar C, Rychik J, et al. Effect of Fontan-associated morbidities on survival with intact Fontan circulation. Am J Cardiol. (2017) 119:1866–71. doi: 10.1016/j.amjcard.2017.03.004
5. Ono M, Burri M, Balling G, Beran E, Cleuziou J, Pabst von Ohain J, et al. Predicted clinical factors associated with the intensive care unit length of stay after total cavopulmonary connection. J Thorac Cardiovasc Surg. (2019) 157:2005–13. doi: 10.1016/j.jtcvs.2018.10.144
6. Downing TE, Allen KY, Glatz AC, Rogers LS, Ravishankar C, Rychik J, et al. Long-term survival after the Fontan operation: twenty years of experience at a single center. J Thorac Cardiovasc Surg. (2017) 154:243–53. doi: 10.1016/j.jtcvs.2017.01.056
7. Pundi KN, Johnson JN, Dearani JA, Pundi KN, Li Z, Hinck CA, et al. 40-year follow-up after the Fontan operation. J Am Coll Cardiol. (2015) 66:1700–10. doi: 10.1016/j.jacc.2015.07.065
8. Ovroutski S, Sohn C, Barikbin P, Miera O, Alexi-Meskishvili V, Hübler M, et al. Analysis of the risk factors for early failure after extracardiac Fontan operation. Ann Thorac Surg. (2013) 95:1409–16. doi: 10.1016/j.athoracsur.2012.12.042
9. Zou M, Wang Y, Cui H, Ma L, Yang S, Xia Y, et al. Outcomes of total cavopulmonary connection for single ventricle palliation. J Thorac Dis. (2016) 8:43–51. doi: 10.3978/j.issn.2072-1439.2016.01.41
10. Lo Rito M, Al-Radi OO, Saedi A, Kotani Y, Ben Sivarajan V, Russell JL, et al. Chylothorax and pleural effusion in contemporary extracardiac fenestrated Fontan completion. J Thorac Cardiovasc Surg. (2018) 155:2069–77. doi: 10.1016/j.jtcvs.2017.11.046
11. Fu S, Feng ZC, Dietmar S. Factors influencing pleural effusion after Fontan operation: an analysis with 95 patients. Chin Med Sci J. (2010) 25:38–43. doi: 10.1016/S1001-9294(10)60018-1
12. Zheng K, Gong M, Qin Y, Song H, Shi X, Wu Y, et al. Validation of glomerular filtration rate-estimating equations in Chinese children. PLos ONE. (2017) 12:e180565. doi: 10.1371/journal.pone.0180565
13. Zhang C, Luo Q, Li Y, Wu X, Hao Z, Li S, et al. Predictors of short-term outcomes following repair of anomalous origin of the left coronary artery from the pulmonary artery in chinese children: a case-control study. J Cardiothorac Vasc Anesth. (2018) 32:2644–51. doi: 10.1053/j.jvca.2018.04.008
14. Saiki H, Kuwata S, Iwamoto Y, Ishido H, Taketazu M, Masutani S, et al. Fenestration in the Fontan circulation as a strategy for chronic cardioprotection. Heart. (2019) 105:1266–72. doi: 10.1136/heartjnl-2018-314183
15. Lemler MS, Scott WA, Leonard SR, Stromberg D, Ramaciotti C. Fenestration improves clinical outcome of the Fontan procedure. Circulation. (2002) 105:207–12. doi: 10.1161/hc0202.102237
16. Kintrup S, Malec E, Kiski D, Schmidt C, Brünen A, Kleinerüschkamp F, et al. Extubation in the operating room after Fontan procedure: does it make a difference. Pediatr Cardiol. (2019) 40:468–76. doi: 10.1007/s00246-018-1986-5
17. Ono M, Georgiev S, Burri M, Mayr B, Cleuziou J, Strbad M, et al. Early extubation improves outcome following extracardiac total cavopulmonary connection. Interact Cardiovasc Thorac Surg. (2019) 29:85–92. doi: 10.1093/icvts/ivz010
18. Pike NA, Okuhara CA, Toyama J, Gross BP, Wells WJ, Starnes VA. Reduced pleural drainage, length of stay, and readmissions using a modified Fontan management protocol. J Thorac Cardiovasc Surg. (2015) 150:481–7. doi: 10.1016/j.jtcvs.2015.06.042
19. Talwar S, Das A, Khadgawat R, Sahu MK, Choudhary SK, Airan B. A prospective study of risk factors associated with persistent pleural effusion after total cavopulmonary connection with special reference to serum cortisol level. Indian J Thorac Cardiovasc Surg. (2018) 34:345–54. doi: 10.1007/s12055-017-0617-8
Keywords: prolonged pleural effusion, congenital heart disease, total cavopulmonary connection, fenestration, chylothorax
Citation: Luo Q, Zhao W, Su Z, Liu Y, Jia Y, Zhang L, Wang H, Li Y, Wu X, Li S and Yan F (2019) Risk Factors for Prolonged Pleural Effusion Following Total Cavopulmonary Connection Surgery: 9 Years' Experience at Fuwai Hospital. Front. Pediatr. 7:456. doi: 10.3389/fped.2019.00456
Received: 31 August 2019; Accepted: 21 October 2019;
Published: 07 November 2019.
Edited by:
Andreas Schwingshackl, University of California, Los Angeles, United StatesReviewed by:
Vijay Srinivasan, Children's Hospital of Philadelphia, United StatesWeiguang Yang, School of Medicine, Stanford University, United States
Copyright © 2019 Luo, Zhao, Su, Liu, Jia, Zhang, Wang, Li, Wu, Li and Yan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fuxia Yan, eWFuZnV4aWEmI3gwMDA0MDtzaW5hLmNvbQ==
 Qipeng Luo1
Qipeng Luo1 Zhanhao Su
Zhanhao Su Yiwei Liu
Yiwei Liu Yuan Jia
Yuan Jia Fuxia Yan
Fuxia Yan