
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CLINICAL TRIAL article
Front. Pediatr. , 01 March 2019
Sec. Neonatology
Volume 7 - 2019 | https://doi.org/10.3389/fped.2019.00040
 Meryl Vedrenne-Cloquet1,2*
Meryl Vedrenne-Cloquet1,2* Sophie Breinig3
Sophie Breinig3 Agnes Dechartres4
Agnes Dechartres4 Camille Jung5
Camille Jung5 Sylvain Renolleau2
Sylvain Renolleau2 Laetitia Marchand-Martin6
Laetitia Marchand-Martin6 Xavier Durrmeyer1,7
Xavier Durrmeyer1,7Purpose: This study aimed to describe cerebral Near InfraRed Spectroscopy (NIRS) profiles during neonatal intubation using two different premedication regimens.
Methods: Neonates requiring non-emergency intubation were enrolled in an ancillary study, conducted in two French Neonatal Intensive Care Units participating in a larger on-going multicenter, double blind, randomized, controlled trial. Patients were randomly assigned to the “atropine-propofol” (Prop) group or the “atropine-atracurium-sufentanil” (SufTrac) group. Regional cerebral oxygen saturation (rScO2), pulse oxymetry (SpO2), mean arterial blood pressure (MABP), and transcutaneous partial pressure of carbon dioxide (TcPCO2) were collected at 9 predefined time points from 1 min before to 60 min after the first drug injection. The two primary outcomes were a decrease in rScO2 value >20% from baseline and a decrease in fractional cerebral tissue oxygen extraction (FTOE) value >10% from baseline, at any time point. Secondary outcomes included physiological parameters changes over time and correlations between mean arterial blood pressure, and FTOE at different time points. Descriptive results were obtained and exploratory statistical analyses were performed for 24 included patients.
Results: rScO2 decreased in 5/11 (46%) infants from the Prop group and 10/13 (77%) from the SufTrac group (p = 0.11); FTOE decreased in 10/11 (91%) infants from the Prop group, and 12/13 (92%) from the SufTrac group (p = 0.90). rScO2 values decreased over time in both groups, whereas FTOE's pattern appeared more stable. SpO2 and transcutaneous TcPCO2 seemed more preserved in the Prop group while MABP seemed more preserved in the SufTrac group. No important correlation was observed between MABP and FTOE (r = 0.08 to 0.12 across the time points).
Conclusion: Our results suggest a frequent decrease in cerebral oxygenation without obvious impairment in cerebral autoregulation during neonatal intubation with premedication. This study confirms the feasibility and the informative value of cerebral NIRS monitoring in this setting.
Clinical Trial Registration: www.ClinicalTrials.gov, identifier NCT02700893.
Premedication is recommended before a (semi)-elective neonatal intubation (1) because awake intubation is painful and increases intracranial pressure (2). However, awake intubation remains common in some Neonatal Intensive Care Units (NICU) (3, 4), partly because of the fear of adverse drug reactions (4). The combination of a short-acting opioid with a muscle-blocker is among recommended regimens for premedication prior to neonatal intubation (1, 5) but can lead to thoracic rigidity and hypoxemia in very preterm infants (6). Propofol is a short-acting anesthetic that preserves spontaneous ventilation (7, 8) but can cause systemic hypotension (8, 9).
Low systemic blood flow is associated with brain damage in premature neonates (10, 11) since their cerebral autoregulation (CAR) is frequently impaired (12, 13). However, systemic hypotension, defined as a mean arterial blood pressure (MABP) (in mmHg) lower than gestational age (in weeks) (14), is poorly associated with low systemic blood flow (15). A multimodal evaluation has been proposed to assess cerebral hemodynamics and oxygenation beyond blood pressure monitoring (16), using Near Infra Red Spectroscopy (NIRS) (17). This technology offers a non-invasive monitoring of peripheral microcirculation, reflecting the adequacy between oxygen delivery and consumption in situ (18). Cerebral NIRS is easily achieved in neonates, allowing measurements of cerebral oxygen saturation (rScO2) without serious adverse effects (19), and has been found a useful tool during laryngoscopy (20–23).
This study aimed to describe cerebral oxygenation assessed by NIRS during neonatal intubation with 2 different premedication regimens: atropine-propofol or atropine-atracurium-sufentanil.
We conducted a prospective observational ancillary study strictly following the design and methods of a previously published multicenter, double-blind, randomized, controlled trial with parallel groups (24). The only particularity of this ancillary study was to collect cerebral NIRS values during the patients' participation in the study. This ancillary study was conducted in two of the 6 participating centers that had previous experience and available equipment for NIRS monitoring. This ancillary study was conceived in September 2015, after the main trial's interruption in August 2014. This ancillary study started in March 2016 when the main trial was resumed (see Supplement) (24). The ancillary study and the main trial were simultaneously prematurely interrupted in August 2016 for expired study kits and unavailability of additional funding (24).
Briefly, in this trial, neonates hospitalized in the NICU requiring a non-emergency endotracheal intubation were randomly assigned 1:1 to the “atropine-propofol” (Prop) group or the “atropine-atracurium-sufentanil” (SufTrac) group using a fixed block size of 4, and stratification by center and weight (≤ or > 1,000 g). The premedication and intubation procedures have already been reported elsewhere (24) and are detailed and illustrated in the Supplemental Figure 1. A double-dummy approach was used with intralipids as a placebo for propofol and normal saline as a placebo for atracurium and sufentanil so that treatments appeared identical (Supplemental Figure 1). Parents, physicians and, nurses were unaware of treatment allocation. The primary outcome of the main trial was prolonged desaturation.
All patients included in the main trial in the two centers between March and August 2016, were eligible for the ancillary study. Inclusion criteria were exactly similar to those of the main study and included: corrected age at the time of inclusion of < 45 weeks (in order to recruit exclusively neonates defined as infants with a maximal postnatal age of 28 days after full-term birth, which corresponds to 45 weeks of corrected age) and indication for non-emergency intubation. Exclusion criteria were exactly similar to those of the main study and included: sedatives or anesthetics administration in the previous 24 h, hemodynamic failure (MABP less than corrected gestational age and/or capillary refill time exceeding 3 s), upper airway malformation, life-threatening situation, previous inclusion in this, or in another trial, any contraindication to any study drug. In this ancillary study the only additional exclusion criteria was the presence of skin lesions on the forehead that precluded the use of NIRS sensors.
Data related to NIRS cerebral profiles were collected during the procedure using a 2-wavelength (730–810 nm) cerebral oxymeter (monitor INVOS 5100C®, Covidien, Medtronics, USA) to record rScO2. A transducer (neonatal sensor OXYALERT, Covidien, Medtronics, USA) was placed on the left fronto-parietal side of the patient's head. Pulse oxymetry (SpO2) acquired with an oximetry sensor placed on the right hand (LNOP® Neo-Pt L or Newborn, Masimo INC., Irvine, CA), transcutaneous partial pressure of carbon dioxide (TcPCO2), non-invasive blood pressure, and heart rate (HR) were also collected (24). Data were collected 1 min before the first drug injection, at the first drug injection, and at 3, 6, 9, 12, 15, 30, 45, and 60 min after it. To assess the balance between oxygen delivery and consumption, the Fractional cerebral Tissue Oxygen Extraction (FTOE) was calculated from rScO2 and pulse oxymetry (SpO2) as this ratio: FTOE = [SpO2-rScO2]/SpO2 (25, 26) for all time points.
The two predefined primary outcomes were a cerebral desaturation, defined as a decrease in rScO2 value > 20% from baseline (27, 28), and an impaired cerebral oxygen extraction, defined as a decrease in FTOE value > 10% from baseline, at any time point after the first injection. No consensual threshold exists to define a significant decrease in FTOE, so we arbitrarily set this threshold at 10% since a previous study considered a 5% decrease “small and probably clinically irrelevant” (29).
Secondary outcomes included changes over time for HR, MABP, SpO2, TcPCO2, rScO2, and FTOE in both groups. As a surrogate for CAR, we studied the correlation between MABP and FTOE at different predefined time points (1 min before and 6 min, and 15 min after the first injection), considering that the frequent occurrence of systemic desaturation during intubation (24) would preclude the interpretation of correlations between MABP and rSCO2 (17, 23).
This ancillary study was designed to provide observational data. No hypothesis was formulated. Thus, we did not conduct a formal sample size calculation for this ancillary exploratory study.
Results are summarized as medians and IQR for quantitative variables, and numbers and percentages for qualitative variables. We took into account the limited sample size and the obvious imbalance in some characteristics between groups. Therefore, baseline characteristics were compared between treatment groups, using Mann-Whitney and Fisher's exact tests or continuous and categorical variables, respectively, in spite for current recommendations concerning randomized trials (30) Due to the small sample size, we performed exploratory comparative tests using Fisher's exact tests for the primary outcomes. A p < 0.05 was considered statistically significant.
To analyze the link between MABP and FTOE, a Pearson correlation coefficient was calculated at predefined time-points (1 min before and 6 min and 15 min after the first injection).
No imputation of missing data was performed. Data were analyzed using SAS® 9.4.
Between 1 March 2016 and 31 August 2016, 27 infants were included in the main study in the two centers participating in the ancillary study (flow chart presented in Figure 1). Three patients allocated to the Prop group were excluded because NIRS measurements could not be performed. Data were collected and analyzed in 24 patients: 11 in the Prop group and 13 in the SufTrac group.
Clinical characteristics of patients from each group are provided in Table 1. Despite randomization, gestational age, and weight at inclusion were lower in the SufTrac group than in the Prop group. Baseline physiological and NIRS parameters were comparable (Table 1). In the SufTrac group, 12/13 patients received non-invasive ventilation before intubation. In the Prop group, 6/11 patients received non-invasive ventilation before intubation, and 4/11 patients were spontaneously breathing room air before intubation. These four patients were intubated in order to perform planned surgery under general anesthesia. One patient in each group was receiving invasive ventilation before the procedure and underwent endotracheal tube change.
Patients in the Prop group received more often additional treatment as planned in the protocol (7/11, 64%) than patients in the SufTrac group (2/13, 15%). In the Prop group, among the 7 patients who received 6 syringes, 4 received an additional open-label treatment: 2 received atracurium and sufentanil, one received propofol and atracurium, and one received propofol alone. The median [IQR] cumulated propofol dose in this group was 3.0 [2.5–3.5] mg/kg. In the SufTrac group, no infant required open label treatment.
A cerebral desaturation occurred in 5/11 patients (46%) from the Prop group and in 10/13 patients (77%) from the SufTrac group (p = 0.11). A decrease in FTOE occurred in 10/11 patients (91%) from the Prop group and in 12/13 patients (92%) from the SufTrac group (p = 0.90).
Figure 2 shows the mean rScO2, FTOE, SpO2, MABP, TCpCO2, and HR values over time in each group. rScO2 decreased in both groups at 6, 9, and 12 min after the first injection, with subsequent return to baseline and a graphically deeper decrease in the SufTrac group (Figure 2A). Mean SpO2 decreased at 6, 9, 12, and 15 min after the first injection, with subsequent return to values > 90% after 30 min and a graphically deeper decrease in the SufTrac group (Figure 2C). Mean MABP decreased in the Prop group, and initially increased then returned to baseline in the SufTrac group (Figure 2D). TcPCO2 remained stable in the Prop group and increased in the SufTrac group (Figure 2E). Heart rate increased in both groups (Figure 2F). Although a 10% decrease in FTOE at any time point was frequent in both groups, the mean FTOE pattern over time remained relatively stable during monitoring with remarkably superimposable curves in both groups (Figure 2B).
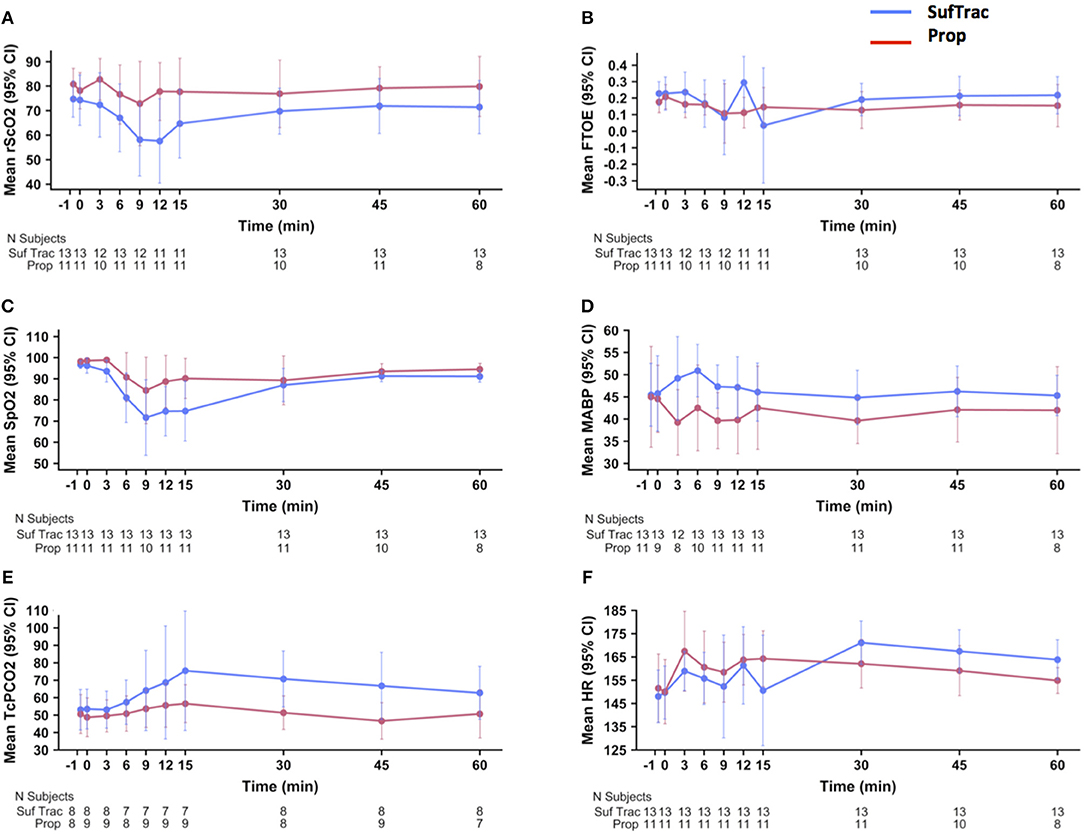
Figure 2. Physiological parameters and cerebral oxygenation changes overtime. These graphs illustrate the mean values (points) and 95% CI (error bars) on the Y axis for rScO2 (A), FTOE (B), SpO2 (C), MABP (D), TcPCO2 (E), and HR (F) over time. The x-axis indicates the time before and after first drug injection (denoted as “0”) in min. Graphs are presented in red for the atropine-propofol group and in blue for the atropine-atracurium-sufentanil group. CI, confidence interval; rScO2, regional cerebral oxygen saturation; FTOE, fractional cerebral tissue oxygen extraction; SpO2, oxygen saturation; MABP, mean arterial blood pressure; TcPCO2, transcutaneous partial carbon dioxide pressure; HR, heart rate.
Correlations between FTOE and MABP are shown in Figure 3. No correlation higher than 0.5 was found between FTOE and MABP 1 min before (Figure 3A), 6 min (Figure 3B), or 15 min (Figure 3C) after the first injection in both groups. Correlation coefficients varied between 0.08 and 0.19 in the whole population, between 0.17 and 0.33 in the SufTrac group, and between 0.13 and 0.42 in the Prop group (Figure 3).
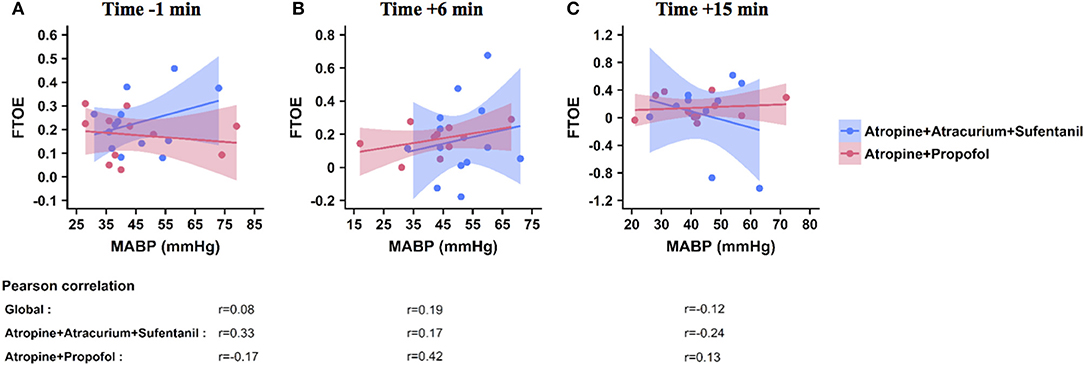
Figure 3. Correlation between FTOE and MABP at predefined time points. These graphs illustrate the correlation between FTOE (Y axis) and MABP (X axis) 1 min before (A), and 6 min (B), and 15 min (C) after the first drug injection. Each point represents a patient, the solid line represents the regression line and the colored area represents the 95% CI interval within each group (atropine-propofol in red, atropine-atracurium-sufentanil in blue). Pearson correlation coefficients calculated for the whole population (global) and for each group are included below the graph for each time point. FTOE, fractional cerebral tissue oxygen extraction; MABP, mean arterial blood pressure.
To our knowledge, this is the first study reporting cerebral NIRS profiles with two premedication regimens during neonatal intubation. This study demonstrated the feasibility of cerebral oxygenation monitoring during this procedure. rSCO2 decreased over time and FTOE frequently decreased from baseline but remained relatively stable over time. FTOE curves were graphically superimposable in the two treatment groups. FTOE was not strongly correlated with MABP.
Strengths of this study include the quality of evidence due to the design of the main study and its originality since cerebral oxygenation profiles were described with 2 premedication regimens acceptable for neonatal intubation. The findings provide limited but valuable information on the studied drugs' safety and should discourage physicians from performing awake neonatal intubation outside life-threatening situations.
To date, three studies have analyzed cerebral NIRS profiles during neonatal intubation. van den Berg et al. compared infants receiving an InSurE (Intubation-Surfactant-Extubation) procedure preceded by morphine or pethidin to matched controls with nCPAP (20). Bertini et al. compared cerebral NIRS profiles during surfactant administration either by an InSurE or a LISA (Less Invasive Surfactant Administration) technique, both requiring a laryngoscopy, without premedication (21). Smits et al. conducted a dose-finding study on propofol used as premedication before a (semi)-elective intubation (22) and specifically assessed CAR in a subset of this population in another publication by Thewissen et al. (23). Although Van den Berg et al. found no statistically significant effect of the InSurE procedure on rScO2 or FTOE (20), the other studies found a short-lasting decrease in rScO2 just after the procedure (21–23), which is consistent with our results. Whereas, mean FTOE values seemed more stable over time in our study, Bertini et al. found an increase in FTOE after the LISA procedure but not after the InSurE procedure. This finding was interpreted as a “compensatory mechanism” but no speculation was made on CAR (21). Conversely, Smits et al. found a decrease in FTOE after intubation with propofol, that they attributed to a decrease in cerebral consumption (22).
In our study, cerebral desaturation was concomitant with systemic desaturation, especially in the SufTrac group. Systemic desaturation leads physiologically to cerebral desaturation. Oxygen transport to the living tissues depends on the arterial oxygen content, which is determined among others by arterial oxygen saturation and hemoglobin. Thus, a decrease in rScO2 can occur in case of an isolated hypoxemia without hemodynamic disturbance. In stable preterm babies, multiple episodes of hypoxemia alone can lead to a decrease in rScO2 without any trouble in cerebral FTOE (31). Smits et al. also described this phenomenon and defined it as a “hypoxic hypoxia” rather than an “ischemic hypoxia,” because of a brief and short-lasting decrease in rScO2 despite a prolonged decrease in MABP (22). Our results are consistent with this hypothesis since the decrease in SpO2 was concomitant with the decrease in rScO2. Moreover, FTOE values were preserved in the two groups despite a low rScO2. As FTOE reflects the balance between oxygen demand and supply, this suggests a trouble affecting the cerebral oxygen delivery without any trouble in oxygen consumption by the brain tissue. This might be attributable to a physiological process called “neurometabolism coupling,” which links cerebral blood flow and vasoreactivity to cerebral metabolic demand. Cerebral oxygen consumption reflects cerebral metabolism, which depends on cerebral oxygen extraction and cerebral blood flow. We can assume that in our study, patients had low cerebral oxygen consumption induced by sedative drugs; this could have led to a lower cerebral blood flow that maintained a stable FTOE despite a low rScO2. This hypothesis is supported by the results from the ancillary study of the NEOPROP study that found mostly intact CAR with suppressed cerebral activity measured by aEEG in preterm infants premedicated with propofol for an INSURE procedure (23).
Some physiological parameters, such as SpO2 or MABP seemed to have different patterns over time in the 2 treatment groups. These seemingly different observed patterns could be attributed to many factors such as the treatment group, the imbalance between groups in patients' weight, gestational age, and indications for intubation, or chance. Thus, the interpretation of these results should be careful.
Deeper systemic desaturation observed in the SufTrac group might also be due to the decrease in lung residual capacity due to the use of a muscle-blocker (atracurium) (6), while propofol is known to preserve spontaneous ventilation. The higher TcPCO2 in this group is consistent with this hypothesis and was previously reported in other studies using muscular-blockers prior to neonatal intubation (6, 32).
MABP seemed to be more preserved in the SufTrac group than in the Prop group. Despite decreased MABP in the Prop group, FTOE values from both groups were superimposable and no strong correlation was found between FTOE and MABP. Results in the Prop group support the existing hypothesis that a drop in tissue oxygenation is uncertain during propofol-induced hypotension (22, 23, 33, 34). A correlation coefficient < 0.5 has been considered to rule out impaired CAR (35). In our study, we observed low correlation coefficient, suggesting that most of our population had a preserved CAR. Consistently, Thewissen et al. observed one case among 22 patients of impaired CAR associated with systemic hypotension, although 5 other cases of impaired CAR were observed with normal or elevated MABP (23). Based on these results isolated hypotension with signs of good perfusion might be respected (16). However, our findings might not be applicable to critically ill neonates such as extremely low birth weight neonates (13) or infants who had non-inclusion criteria for our study, such as needing emergency intubation or having signs of hemodynamic compromise.
Our study had two major limitations. First, patients were recruited only between March and August 2016, while the larger trial started in 2011, resulting in a limited number of recruited patients. Second, there were important imbalances in gestational age and weight at inclusion, and in indication for intubation between groups, leading to different populations despite randomization. This might have biased results, although baseline characteristics concerning physiological parameters including rScO2 were comparable at inclusion. However, the patterns of physiological parameters' changes over time in the recruited patients were very similar to those observed in the main trial (24), suggesting a representative sample. The third limitation of our study is its exploratory nature, without any pre-specified hypothesis concerning a specific NIRS-related outcome, nor sample size calculation. Our study may therefore lack power and potentially expose to selection bias. These first three limitations did not allow us to perform a formal comparison between the 2 studied regimens so we cannot conclude about any differences between them. Fourth, for MABP measures we used non-invasive measures that might not be correlated with invasive measures in premature neonates (36). Fifth, we analyzed correlations between FTOE and MABP at predefined time points and did not collect data continuously as others (23). Thus, we could not assess coherence, which is a better estimation of CAR (23, 37).
Cerebral NIRS appeared as a feasible and informative monitoring device to investigate the hemodynamic tolerance of neonatal intubation with premedication. For both premedication regimens a decrease in rSCO2 that paralleled a decrease in SpO2 was observed during neonatal intubation, but the study's design did not allow for comparison between the premedication regimens. However, no strong indicator of impaired CAR was observed. Adequately powered trials using cerebral NIRS are required to further assess the safety of premedication drugs for neonatal intubation.
The study was approved by an ethics committee (Paris Ile de France 3, approval n° 2895) and by the French Medicinal Products Agency (n° A110281-16). Written informed consent was obtained from the parents of all infants.
MV-C and XD conceived the study. XD and CJ were in charge of overall direction and planning, and supervised the project. MV-C, SB, and XD contributed to the investigation and collection of the data. MV-C, LM-M, XD, and AD contributed to the interpretation of the results. LM-M performed the statistical analysis. MV-C took the lead in the initial manuscript, supervised by XD. SB, AD, CJ, and SR provided critical feedback and helped shape the research, analysis, and manuscript. All authors approved the final version of the manuscript.
This study was supported by 2 grants from the French Health Ministry (Programme Hospitalier de Recherche Clinique, PHRC): grant AOM 09 096 in 2009 and grant Prettineo 00-96 in 2014. Masimo Inc. provided some equipment for monitoring pulse oximetry.
XD reports grants from Ministry of health, non-financial support from Masimo Inc., during the conduct of the study; personal fees, and non-financial support from Chiesi Pharmaceuticals, outside the submitted work. CJ reports grants from the Ministry of Health during the conduct of the study.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2019.00040/full#supplementary-material
1. Kumar P, Denson SE, Mancuso TJ. Premedication for non-emergency endotracheal intubation in the neonate. Pediatrics (2010) 125:608–15. doi: 10.1542/peds.2009-2863
2. Friesen RH, Honda AT, Thieme RE. Changes in anterior fontanel pressure in preterm neonates during tracheal intubation. Anesth Analg. (1987) 66:874–8.
3. Durrmeyer X, Daoud P, Decobert F, Boileau P, Renolleau S, Zana-Taieb E, et al. Premedication for neonatal endotracheal intubation: results from the epidemiology of procedural pain in neonates study. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc. (2013) 14:e169–75. doi: 10.1097/PCC.0b013e3182720616
4. Muniraman HK, Yaari J, Hand I. Premedication use before non-emergent intubation in the newborn infant. Am J Perinatol. (2015) 32:821–4. doi: 10.1055/s-0034-1543987
5. Barrington K. Premedication for endotracheal intubation in the newborn infant. Paediatr Child Health (2011) 16:159–71.
6. Durrmeyer X, Dahan S, Delorme P, Blary S, Dassieu G, Caeymaex L, et al. Assessment of atropine-sufentanil-atracurium anaesthesia for endotracheal intubation: an observational study in very premature infants. BMC Pediatr. (2014) 14:120. doi: 10.1186/1471-2431-14-120
7. Ghanta S, Abdel-Latif Me, Lui K, Ravindranathan H, Awad J, Oei J. Propofol compared with the morphine, atropine, and suxamethonium regimen as induction agents for neonatal endotracheal intubation: a randomized, controlled trial. Pediatrics (2007) 119:e1248–55. doi: 10.1542/peds.2006-2708
8. Welzing L, Kribs A, Eifinger F, Huenseler C, Oberthuer A, Roth B. Propofol as an induction agent for endotracheal intubation can cause significant arterial hypotension in preterm neonates. Paediatr Anaesth. (2010) 20:605–11. doi: 10.1111/j.1460-9592.2010.03330.x
9. Simons SH, Van Der Lee R, Reiss IK, Van Weissenbruch MM. Clinical evaluation of propofol as sedative for endotracheal intubation in neonates. Acta Paediatr Oslo Nor. (2013) 102:e487–92. doi: 10.1111/apa.12367
10. Hunt RW, Evans N, Rieger I, Kluckow M. Low superior vena cava flow and neurodevelopment at 3 years in very preterm infants. J Pediatr. (2004) 145:588–92. doi: 10.1016/j.jpeds.2004.06.056
11. Kluckow M, Evans N. Low superior vena cava flow and intraventricular haemorrhage in preterm infants. Arch Dis Child Fetal Neonatal Ed. (2000) 82:F188–94. doi: 10.1136/fn.82.3.F188
12. Lou HC, Lassen NA, Friis-Hansen B. Impaired autoregulation of cerebral blood flow in the distressed newborn infant. J Pediatr. (1979) 94:118–21.
13. Tsuji M, Saul JP, du Plessis A, Eichenwald E, Sobh J, Crocker R, et al. Cerebral intravascular oxygenation correlates with mean arterial pressure in critically ill premature infants. Pediatrics (2000) 106:625–32.
14. Dempsey EM, Barrington KJ. Diagnostic criteria and therapeutic interventions for the hypotensive very low birth weight infant. J Perinatol Off J Calif Perinat Assoc. (2006) 26:677–81. doi: 10.1038/sj.jp.7211579
15. Groves AM, Kuschel CA, Knight DB, Skinner JR. Relationship between blood pressure and blood flow in newborn preterm infants. Arch Dis Child Fetal Neonatal Ed. (2008) 93:F29–32. doi: 10.1136/adc.2006.109520
16. Dempsey EM, Hazzani FAL, Barrington KJ. Permissive hypotension in the extremely low birthweight infant with signs of good perfusion. Arch Dis Child Fetal Neonatal Ed. (2009) 94:F241–4. doi: 10.1136/adc.2007.124263
17. Thewissen L, Caicedo A, Lemmers P, Van Bel F, Van Huffel S, Naulaers G. Measuring near-infrared spectroscopy derived cerebral autoregulation in neonates: from research tool toward bedside multimodal monitoring. Front Pediatr. (2018) 6:117. doi: 10.3389/fped.2018.00117
18. Myers DE, Anderson LD, Seifert RP, Ortner JP, Cooper CE, Beilman GJ, et al. Non-invasive method for measuring local hemoglobin oxygen saturation in tissue using wide gap second derivative near-infrared spectroscopy. J Biomed Opt. (2005) 10:034017. doi: 10.1117/1.1925250
19. Hyttel-Sorensen S, Pellicer A, Alderliesten T, Austin T, Van Bel F, Benders M, et al. Cerebral near infrared spectroscopy oximetry in extremely preterm infants: phase ii randomised clinical trial. BMJ (2015) 350:g7635. doi: 10.1136/bmj.g7635
20. van den Berg E, Lemmers PM, Toet MC, Klaessens JH, van Bel F. Effect of the “InSurE” procedure on cerebral oxygenation and electrical brain activity of the preterm infant. Arch Dis Child Fetal Neonatal Ed. (2010) 95:F53–8. doi: 10.1136/adc.2008.156414
21. Bertini G, Coviello C, Gozzini E, Bianconi T, Bresci C, Leonardi V, et al. Change of Cerebral oxygenation during surfactant treatment in preterm infants: “LISA” versus “InSurE” procedures. Neuropediatrics (2017) 48:98–103. doi: 10.1055/s-0037-1598647
22. Smits A, Thewissen L, Caicedo A, Naulaers G, Allegaert K. Propofol dose-finding to reach optimal effect for (Semi-)elective intubation in neonates. J Pediatr. (2016) 179:54–60.e9. doi: 10.1016/j.jpeds.2016.07.049
23. Thewissen L, Caicedo A, Dereymaeker A, Van Huffel S, Naulaers G, Allegaert K, et al. Cerebral autoregulation and activity after propofol for endotracheal intubation in preterm neonates. Pediatr Res. (2018) 8:719–25. doi: 10.1038/s41390-018-0160-3
24. Durrmeyer X, Breinig S, Claris O, Tourneux P, Alexandre C, Saliba E, et al. Effect of atropine with propofol vs. atropine with atracurium and sufentanil on oxygen desaturation in neonates requiring non-emergency intubation: a randomized clinical trial. JAMA (2018) 319:1790–801. doi: 10.1001/jama.2018.3708
25. Naulaers G, Meyns B, Miserez M, Leunens V, Van Huffel S, Casaer P, et al. Use of tissue oxygenation index and fractional tissue oxygen extraction as non-invasive parameters for cerebral oxygenation. A validation study in piglets. Neonatology (2007) 92:120–6. doi: 10.1159/000101063
26. Dix LML, van Bel F, Lemmers PMA. Monitoring cerebral oxygenation in neonates: an update. Front Pediatr. (2017) 5:46. doi: 10.3389/fped.2017.00046
27. Michelet D, Arslan O, Hilly J, Mangalsuren N, Brasher C, Grace R, et al. Intraoperative changes in blood pressure associated with cerebral desaturation in infants. Paediatr Anaesth. (2015) 25:681–8. doi: 10.1111/pan.12671
28. Koch HW, Hansen TG. Perioperative use of cerebral and renal near-infrared spectroscopy in neonates: a 24-h observational study. Paediatr Anaesth. (2016) 26:190–8. doi: 10.1111/pan.12831
29. Kooi EMW, van der Laan ME, Verhagen EA, Van Braeckel KN, Bos AF. Volume expansion does not alter cerebral tissue oxygen extraction in preterm infants with clinical signs of poor perfusion. Neonatology (2013) 103:308–14. doi: 10.1159/000346383
30. Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ (2010) 340:c869. doi: 10.1136/bmj.c869
31. Petrova A, Mehta R. Regional tissue oxygenation in association with duration of hypoxaemia and haemodynamic variability in preterm neonates. Arch Dis Child Fetal Neonatal Ed. (2010) 95:F213–9. doi: 10.1136/adc.2009.161604
32. Chandrasekharan P, Nrusimha A, Rawat M, Lakshminrusimha S. Using paralytic as part of premedication for elective intubation of premature neonates may result in transient impairment of ventilation. Am J Perinatol. (2018) 35:1127–30. doi: 10.1055/s-0038-1635092
33. Fleck T, Schubert S, Ewert P, Stiller B, Nagdyman N, Berger F. Propofol effect on cerebral oxygenation in children with congenital heart disease. Pediatr Cardiol. (2015) 36:543–9. doi: 10.1007/s00246-014-1047-7
34. Vanderhaegen J, Naulaers G, Van Huffel S, Vanhole C, Allegaert K. Cerebral and systemic hemodynamic effects of intravenous bolus administration of propofol in neonates. Neonatology (2010) 98:57–63. doi: 10.1159/000271224
35. Alderliesten T, Lemmers PM, Smarius JJ, Van De Vosse Re, Baerts W, Van Bel F. Cerebral oxygenation, extraction, and autoregulation in very preterm infants who develop peri-intraventricular hemorrhage. J Pediatr. (2013) 162:698–704.e2. doi: 10.1016/j.jpeds.2012.09.038
36. König K, Casalaz DM, Burke EJ, Watkins A. Accuracy of non-invasive blood pressure monitoring in very preterm infants. Intensive Care Med. (2012) 38:670–6. doi: 10.1007/s00134-012-2499-y
Keywords: neonatal intubation, premedication, cerebral oxygenation, near infrared spectroscopy, hypotension, propofol
Citation: Vedrenne-Cloquet M, Breinig S, Dechartres A, Jung C, Renolleau S, Marchand-Martin L and Durrmeyer X (2019) Cerebral Oxygenation During Neonatal Intubation–Ancillary Study of the Prettineo–Study. Front. Pediatr. 7:40. doi: 10.3389/fped.2019.00040
Received: 14 November 2018; Accepted: 30 January 2019;
Published: 01 March 2019.
Edited by:
Maximo Vento, Hospital Universitari i Politècnic La Fe, SpainReviewed by:
Anup C. Katheria, Sharp Mary Birch Hospital for Women & Newborns, United StatesCopyright © 2019 Vedrenne-Cloquet, Breinig, Dechartres, Jung, Renolleau, Marchand-Martin and Durrmeyer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Meryl Vedrenne-Cloquet, bWVyeWwudmVkcmVubmVAYXBocC5mcg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.