- 1Weill Cornell Medicine- Qatar, Ar-Rayyan, Qatar
- 2Pediatric Surgery, Hamad Medical Corporation, Doha, Qatar
- 3College of Medicine, Qatar University, Doha, Qatar
Perinatal testicular torsion is a relatively rare event that remains unidentified in many situations and managed only after an avoidable delay of time. Its current management approaches include watchful observation, delayed contralateral orchiopexy, and emergent contralateral orchiopexy. On the other hand, bilateral torsion is now being more frequently reported. However, the assessment of the contralateral testis through physical examination and imaging can be inaccurate in cases of perinatal torsion. We report a case of prenatal testicular torsion with incidentally discovered metachronous contralateral extravaginal testicular torsion. Therefore, immediate surgical intervention is recommended both when uni- or bilateral testicular torsion is suspected. Whenever possible, affected testes should be preserved as some endocrine function may be retained.
Introduction
Neonatal testicular torsion (NTT) was first described by Taylor et al. in 1897 (1). It can be either unilateral or, less frequently, bilateral. In addition, bilateral NTT can be synchronous or metachronous. However, the exact time of the beginning of the torsion is difficult to determine. A high index of suspicion is mandatory for timely diagnosis of perinatal torsion even in the presence of “normal” other side. However, management plan and mode of intervention is highly controversial. We present here a case of bilateral NTT and challenge the importance of earlier surgical exploration whenever doubt exist. Moreover, recent insights into this condition were reviewed.
Case Report
A 2-day old, male baby, product of a normal vaginal delivery, had a right hemi-scrotal swelling since birth, with bluish scrotal pigmentation (Figure 1). General examination was normal. Color Doppler Ultrasound of the scrotum, showed absence of vascularity in the right testis and maintained blood flow to the other one (Figure 2). Right scrotal exploration was done through midline raphe incision and revealed right extra-vaginal testicular torsion with a necrotic testis (Figure 3A). Contralateral exploration showed extra-vaginal testicular torsion with normal vascularity (Figure 3B).
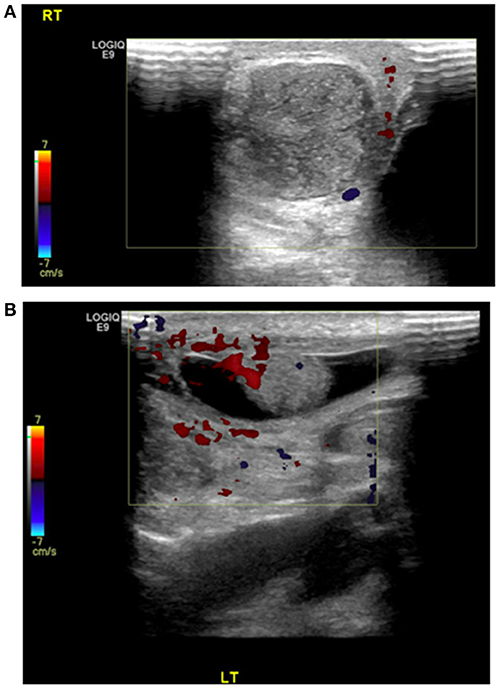
Figure 2. Doppler US showed (A) no blood flow to the right testis with (B) preservation of the vascularity of the left testis.
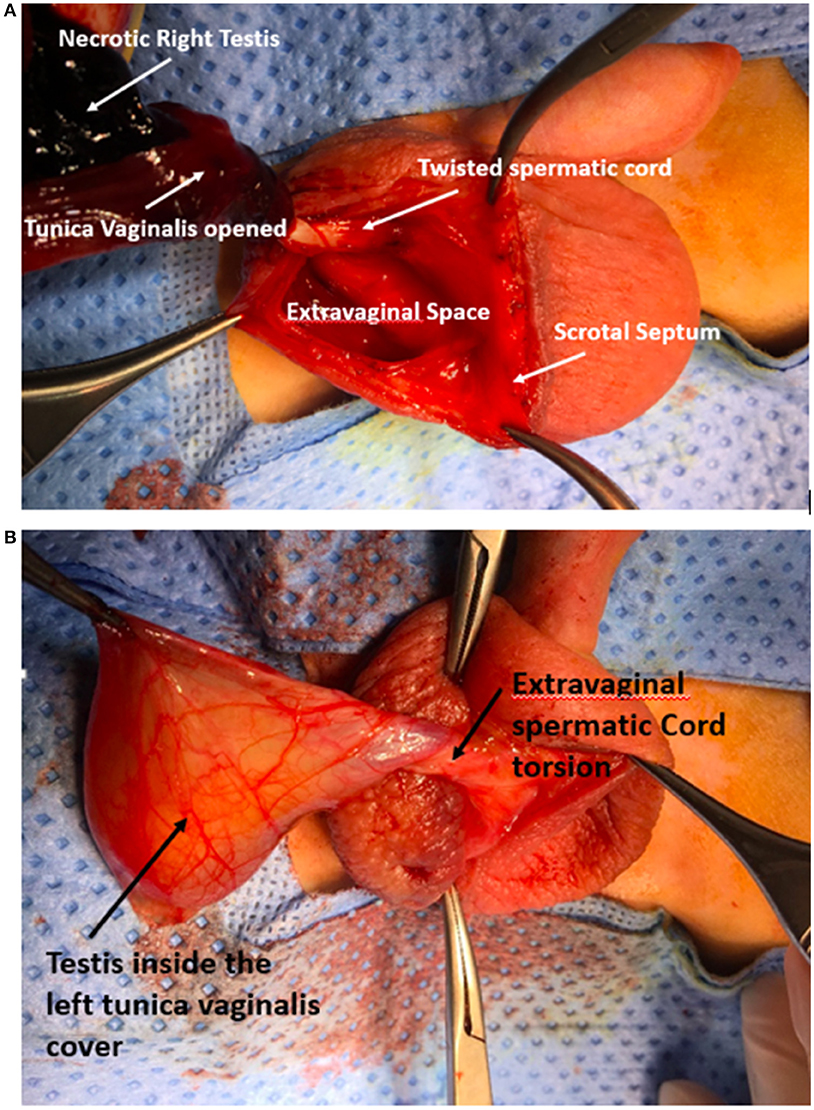
Figure 3. Intraoperative photo showing (A) extra-vaginal torsion of the right side with necrotic testis after opening the tunica vaginalis, (B) left side early onset of extra-vaginal TT and tunica vaginalis freely moving within the hemiscrotal sac with viable testis within it.
Right orchiectomy with 3-point fixation of the left testis was performed. Histological examination confirmed right testicular coagulative necrosis. Follow-up at 3 months showed that the left testis was normal in size with good blood flow by Doppler signal.
Discussion
Neonatal scrotal swelling has several causes, including: birth trauma, epididymitis, appendicitis, hydrocele, and Testicular Torsion. Although neonatal testicular torsion is considered a rare clinical entity, several reports indicate that it is recently more frequently encountered. Most of the cases happen before birth and only about 20% occur following delivery (2, 3) About 150 perinatal TT have been reported since 2010, with a significant percentage of bilateral cases (4). However, bilateral NTT is much rarer and was not described until 1967 (5). It is synchronous in 50–80% of the cases (6–9).
Neonatal testicular torsion is of the extravaginal type where all scrotal contents twist around the spermatic cord (10). Genetic predisposition might play a rule in the etiology of NTT as several familial cases has been reported (11, 12). Furthermore, Insl3 knockout mice was shown to have both intraabdominal undescended tests and spontaneous TT. As a result, the INSL3 hormone and its receptor, RXLF2, have been pointed to be candidate genes for testicular torsion (13, 14). This explains the occurrence of prenatal TT and vanished testes events in humans. However, human post-natal TT takes place in the scrotal sac and not inside the abdomin, as in the mice. However, Wang et al. studied DNA samples of 39 males (11 neonatal: 21 peri-pubertal; 7 post-pubertal) with testicular torsion. Bilateral testicular torsion was present in 2/11 (18%) neonatal and 2/28 (7%) older cases. A positive family history of TT was present in about one third of both groups. He did not detect any functionally significant mutations in INSL3 or RXFP2, questioning that mutations in these genes are not a common de novo or inherited cause for testicular torsion (15).
Clinical diagnosis of perinatal TT can be a challenging task as most of the cases are asymptomatic, with no tenderness but slight scrotal induration and discoloration. Although Doppler US is frequently utilized as an adjunct to ease that diagnosis of borderline cases, it has its own limitations (16–18). On the other hand parenchymal heterogeneity of the testes was shown to correlate significantly with testicular unsalvagability (19). Therefore, some people suggest that in the presence of parenchymal heterogeneity, orchidectomy, and contralateral fixation can be performed in a less urgent manner (20). However, we do not recommend this approach as there is still good chance of salvagability of testes (21); moreover, there is a real danger of contralateral synchronous TT as we had in this case. On the other hand, Martin et al. has suggested that routine contralateral orchiopexy is not needful in cases of NTT as the presence of bell-clapper anomaly in the other “normal” testis is very rare (22). However, this is arguable by the fact that contralateral testicular torsion in cases of perinetal TT is from the extra-vaginal variety, therefore we still propose contralateral fixation.
Lastly, prompt intervention could save the patients the pain and potential complications that they might have. Recently, near-infrared spectroscopy (NIRS) was shown to provide noninvasive transcutaneous monitoring of deep tissue oxygen saturation (%StO2). It was demonstrated that %StO2 values in the affected testis were significantly lower than unaffected testis (23). Nevertheless, no single investigation is flawless and, when it comes to TT, it is always advised to rely on the detailed history and a thorough physical exam to reach the diagnosis and surgical intervention should take place whenever the diagnosis is in doubt.
Perinatal torsion has been subdivided into prenatal and postnatal (event occurring from birth to 1 month of life) torsion. Management of prenatal neonatal testicular torsion has a lack of consensus in terms of surgical timing and need for contralateral fixation (24). Likewise, there is a scarcity of reports on testicular salvagability in this group of patients secondary to the established infarction (25–27). Moreover, relieving the “testicular compartment” (28) might not be beneficial, but worth trying in selective cases. Metachronous contralateral PTT has been reported and emergent exploration with contralateral orchiopexy was raised as the best method of intervention (29). It has recently been shown that 25 orchiopexies are needed to potentially prevent the loss of a contralateral TT (30). On the other hand, management of synchronous bilateral PTT appears has more consensus, and immediate exploration and orchiopexy rather than orchiectomy is most frequently advocated as Leydig cells tolerate severe ischemia more than other cell types of the testes maintaining the capacity to endogenously produce testosterone. Therefore, the capacity of endogenous testosterone production may continue (4, 31). However, leaving nechrotic testes behind carries the risk of abscess formation and wound infection. On the other hand, postnatal TT should be managed with immediate surgical exploration similar to that an older patients with TT as there is a real potential for testicular conservation (32, 33).
In conclusion, immediate surgical intervention is recommended in suspected bilateral NTT as well as in cases of unilateral torsions with “normal” contralateral one. Whenever possible, affected testes should be retained as endocrine function has the potential to persist.
Ethics Statement
The project has been approved by the Medical Research Centre (MRC) of Hamad Medical Corporation (HMC). Study Number (MRC-4-18-230).
Author Contributions
TA prepared and wrote the article. MA has reviewed and critically analyzed the manuscript.
Photography Consent
Written informed consent was obtained from the parent of the patient for the publication of this case report.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The publication of the article was funded by the Qatar National Library.
References
1. Atallah MW, Ippolito JJ, Rubin BW. Intrauterine bilateral torsion of the spermatic cord. J Urol. (1976) 116:128–9. 10.1016/S0022-5347(17)58712-1
2. Abraham MB, Charles A, Gera P, Srinivasjois R. Surgically managed perinatal testicular torsion: a single centre experience. J Matern Neonatal Med. (2016) 29:1265–8. 10.3109/14767058.2015.1044430
3. Mano R, Livne PM, Nevo A, Sivan B, Ben-Meir D. Testicular torsion in the first year of life – characteristics and treatment outcome. Urology (2013) 82:1132–7. 10.1016/j.urology.2013.07.018
4. Callewaert PRH, Van Kerrebroeck P. New insights into perinatal testicular torsion. Eur J Pediatr. (2010) 169:705–12. 10.1007/s00431-009-1096-8
5. Frederick PL, Dushku N, Eraklis AJ. Simultaneous bilateral torsion of the testes in a newborn infant. Arch Surg. (1967) 94:299. 10.1001/archsurg.1967.01330080137034
6. Barca PR, Dargallo T, Jardon JA, Estevez E, Bautista A, Varela Cives R. Bilateral testicular torsion in the neonatal period. J Urol. (1997) 158:1957–9. 10.1016/S0022-5347(01)64193-4
7. Burge DM. Neonatal testicular torsion and infarction: aetiology and management. Br J Urol. (1987) 59:70–3. 10.1111/j.1464-410X.1987.tb04583.x
8. LaQuaglia MP, Bauer SB, Eraklis A, Feins N, Mandell J. Bilateral neonatal torsion. J Urol. (1987) 138:1051–4. 10.1016/S0022-5347(17)43499-9
9. Baglaj M, Carachi R. Neonatal bilateral testicular torsion: a plea for emergency exploration. J Urol. (2007) 177:2296–9. 10.1016/j.juro.2007.02.005
10. Baud C, Veyrac C, Couture A, Ferran JL. Spiral twist of the spermatic cord: a reliable sign of testicular torsion. Pediatr Radiol. (1998) 28:950–4. 10.1007/s002470050507
11. Cubillos J, Palmer JS, Friedman SC, Freyle J, Lowe FC, Palmer LS. Familial testicular torsion. J Urol. (2011) 185:2469–73. 10.1016/j.juro.2011.01.022
12. Gorbonos A, Cheng EY. Perinatal testicular torsion in siblings. J Pediatr Urol. (2007) 3:514–5. 10.1016/j.jpurol.2007.04.009
13. Parada LF, Nef S. Cryptorchidism in mice mutant for Insl3. Nat Genet. (1999) 22:295–9. 10.1038/10364
14. Sozubir S, Barber T, Wang Y, Ahn C, Zhang S, Verma S, et al. Loss of Insl3: a potential predisposing factor for testicular torsion. J Urol. (2010) 183:2373–9. 10.1016/j.juro.2010.02.2390
15. Wang Y, Fina M, Zhang S, Taussig R, Baker LA. Screening for a genetic basis for testicular torsion: the insulin-3 (INSL3) and LGR8 genes. J Urol. (2008) 179:147. 10.1016/S0022-5347(08)60421-8
16. Kalfa N, Veyrac C, Baud C, Couture A, Averous M, Galifer RB. Ultrasonography of the spermatic cord in children with testicular torsion: impact on the surgical strategy. J Urol. (2004) 172:1692–5; discussion: 1695. 10.1097/01.ju.0000138477.85710.69
17. Frauscher F, Klauser A, Radmayr C. Ultrasonographic assessment of the scrotum. Lancet (2001) 357:721–2. 10.1016/S0140-6736(05)71481-1
18. Kalfa N, Veyrac C, Lopez M, Lopez C, Maurel A, Kaselas C, et al. Multicenter assessment of ultrasound of the spermatic cord in children with acute scrotum. J Urol. (2007) 177:297–301. 10.1016/j.juro.2006.08.128
19. Kaye JD, Shapiro EY, Levitt SB, Friedman SC, Gitlin J, Freyle J, et al. Parenchymal echo texture predicts testicular salvage after torsion: potential impact on the need for emergent exploration. J Urol. (2008) 180:1733–6. 10.1016/j.juro.2008.03.104
20. DaJusta DG, Granberg CF, Villanueva C, Baker LA. Contemporary review of testicular torsion: new concepts, emerging technologies and potential therapeutics. J Pediatr Urol. (2013) 9:723–30. 10.1016/j.jpurol.2012.08.012
21. Sorensen MD, Galansky SH, Striegl AM, Mevorach R, Koyle MA. Perinatal extravaginal torsion of the testis in the first month of life is a salvageable event. Urology (2003) 62:132–4. 10.1016/S0090-4295(03)00402-3
22. Martin AD, Rushton HG. The prevalence of bell clapper anomaly in the solitary testis in cases of prior perinatal torsion. J Urol. (2014) 191:1573–7. 10.1016/j.juro.2013.09.013
23. Burgu B, Aydogdu O, Huang R, Soygur T, Baker LA. Feasibility of transscrotal Near-Infrared Spectroscopy (NIRS) in the evaluation of acute scrotum: a pilot human study. J Urol. (2011) 185:e228. 10.1016/j.juro.2011.02.1376
24. Guerra LA, Wiesenthal J, Pike J, Leonard MP. Management of neonatal testicular torsion: which way to turn? Can Urol Assoc J. (2008) 2:376–9. 10.5489/cuaj.792
25. Pepe P, Panella P, Pennisi M, Aragona F. Does color Doppler sonography improve the clinical assessment of patients with acute scrotum? Eur J Radiol. (2006) 60:120–4. 10.1016/j.ejrad.2006.04.016
26. Paltiel HJ, Connolly LP, Atala A, Paltiel AD, Zurakowski D, Treves ST. Acute scrotal symptoms in boys with an indeterminate clinical presentation: comparison of color Doppler sonography and scintigraphy. Radiology (1998) 207:223–31. 10.1148/radiology.207.1.9530319
27. Brandt MT, Sheldon CA, Wacksman J, Matthews P. Prenatal testicular torsion: principles of management. J Urol. (1992) 147:670–2. 10.1016/S0022-5347(17)37342-1
28. Kutikov A, Casale P, White MA, Meyer WA, Chang A, Gosalbez R, et al. Testicular compartment syndrome: a new approach to conceptualizing and managing testicular torsion. Urology (2008) 72:786–9. 10.1016/j.urology.2008.03.031
29. Roth CC, Mingin GC, Ortenberg J. Salvage of bilateral asynchronous perinatal testicular torsion. J Urol. (2011) 185:2464–8. 10.1016/j.juro.2011.01.013
30. Monteilh C, Calixte R, Burjonrappa S. Controversies in the management of neonatal testicular torsion: A meta-analysis. J Pediatr Surg. (2018). [Epub ahead of print]. 10.1016/j.jpedsurg.2018.07.006
31. Baker LA, Turner TT. Leydig cell function after experimental testicular torsion despite loss of spermatogenesis. J Androl. (1995) 16:12–7.
32. Yerkes EB, Robertson FM, Gitlin J, Kaefer M, Cain MP, Rink RC. Management of perinatal torsion: today, tomorrow or never? J Urol. (2005) 174:1579–82; discussion: 1582–3. 10.1097/01.ju.0000179542.05953.11
Keywords: neonatal, testicular torsion, perinatal, exploration, extravaginal
Citation: Abbas TO and Ali M (2018) Bilateral Neonatal Testicular Torsion; Hidden Surgical Nightmare. Front. Pediatr. 6:318. doi: 10.3389/fped.2018.00318
Received: 08 May 2018; Accepted: 05 October 2018;
Published: 20 November 2018.
Edited by:
Lisandro Ariel Piaggio, Universidad Nacional del Sur, ArgentinaReviewed by:
Juan Ignacio Bortagaray, Monash Children's Hospital, AustraliaCésar Benmaor, Independent Researcher, Argentina
Copyright © 2018 Abbas and Ali. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tariq O. Abbas, dGFyaXEyY0Bob3RtYWlsLmNvbQ==
 Tariq O. Abbas
Tariq O. Abbas Mansour Ali2
Mansour Ali2