Response: Commentary: The Impact of the Time Interval Between Radiation and Hyperthermia on Clinical Outcome in Patients With Locally Advanced Cervical Cancer
- 1Department of Radiation Oncology, Erasmus MC, University Medical Center Rotterdam, Rotterdam, Netherlands
- 2Holland Proton Therapy Center, Delft, Netherlands
A Commentary on
The Impact of the Time Interval Between Radiation and Hyperthermia on Clinical Outcome in Patients With Locally Advanced Cervical Cancer
by Crezee, H., Kok, H. P., Oei, A. L., Franken, N. A. P., and Stalpers, L. J. A. (2019). Front. Oncol. 9:412. doi: 10.3389/fonc.2019.00412
We thank Crezee et al. for their opinion article concerning the impact of the time interval between radiotherapy (RT) and hyperthermia (HT), elicited by our recent publication showing no effect of the time interval on clinical outcome (1). We welcome the discussion, as time interval between RT and HT is one of the important issues to solve for the hyperthermia community in the near future. As stated in our conclusion, several hyperthermia centers are centralized and receive many patients from radiotherapy departments elsewhere. Also, from a patient perspective, receiving a daily radiotherapy fraction nearby and only traveling to a more distant located hyperthermia facility once a week is preferable and could increase acceptance and tolerance of the thermoradiotherapy treatment.
We regret the feeling of insufficient caution in our conclusions. In fact, we and our referring radiation oncologists took the results of the study of van Leeuwen very seriously. It initiated an intense discussion as to whether the treatment procedure for RT+HT should be offered only if both treatments could be delivered in the same institution to maintain a short treatment interval between the therapies. After all, the international standard for locally advanced cervix cancer consists of combined radiotherapy and platinum-based chemotherapy (2). However, there is a gray zone for elderly patients or patients with larger tumors depending on the confidence in the alternative of combined RT + HT and the regional availability of hyperthermia (3–5). In addition, the adjuvant effect of chemotherapy seems to be less in locally advanced cases and toxicity of thermoradiotherapy is mild (2, 5). We share the common opinion of Crezee et al. that the important clinical consequence of hyperthermia and radiotherapy in the same center should not be based on a single institutions' experience. Hence, our decision to investigate the issue of the time interval in our patient population (6). It was to our honest surprise that we found an absolute null effect of the time interval with Hazard Ratio's of a perfect 1.0 in 400 patients. In our discussion we thought of potential explanations for the different findings between the two studies, including the potential difference in temperatures achieved, as also pointed out by Crezee et al. (7).
A limitation of both our studies, besides the retrospective nature, is the long inclusion period; 1999–2014 for van Leeuwen et al. and 1996–2016 for our cohort. This makes both our analyses subject to confounding factors, because of changes in interval times in different time periods. For example, in our cohort we observed longer waiting times between RT and HT in earlier years vs. more recent years. Given the larger number of patients in our cohort, we were able to analyze the effect of the time interval per time period of 4–5 years, showing no effect of the time interval for all time periods (1).
We agree with Crezee et al. that there is sufficient data showing the effect of hyperthermia on DNA repair inhibition at temperatures higher than 41°C in preclinical models (8–10), but not yet in patients (8). The median temperature increase in our cohort was 40.5°C, which seemed lower than the cohort of van Leeuwen et al. Of note, the difference in temperatures reported in both our cohorts, does not automatically reflect a dose difference to the tumor, as there are distinct differences in the treatment strategies regarding guidance of SAR steering and temperature measurements (11, 12). Looking at our data, however, we observed a wide range in the distribution of TRISE in our cohort, ranging from 0.54 to 5.16°C. We hypothesized that in patients with a high thermal dose, which are also present in our cohort, the effect of the time interval on clinical outcome could be present and could provide an independent confirmation of the finding of van Leeuwen et al. Therefore, we performed an additional analysis for the effect of the time interval on clinical outcome in patients with a high thermal dose. For this, we divided the cohort over the quartiles of TRISE and using univariate Cox proportional hazard analysis, analyzed the effect of the time interval on clinical outcome per TRISE group. As stated by Crezee et al. the medium temperature of their patient group is close to 41°C, which is highly comparable to the temperatures measured in patients of our highest thermal dose group (40.87–42.16°C). Strikingly, also in the group of patients with the highest thermal dose, the Hazard Ratio for Local Control remained 1.0 (95% CI 0.99–1.01; p = 0.624) (Table 1). These results strongly indicate that—at least in our cohort—the time interval also has not an effect on outcome in patients with an average target temperature above 40.8°C. Due to the retrospective design of both our studies, without direct comparison with radiotherapy alone, nor with chemoradiotherapy, the effectiveness of hyperthermia cannot be directly proven. However, the strong correlation of thermal dose with clinical outcome in our study is a strong indication of the adjuvant effect of hyperthermia (13).
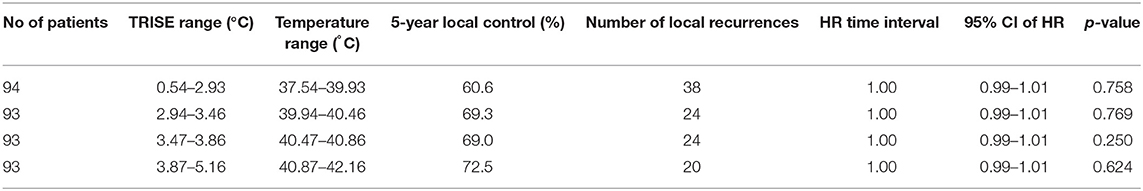
Table 1. Analysis of the effect of the time interval using univariate Cox analysis in patients groups divided over the quartiles of TRISE.
Clearly, the result of our additional analysis for the high thermal dose group will not close the discussion on the relevance of proper selection of the time interval between RT and HT. The results of both cohort studies published on the time interval question, strongly call for further future research in a cooperative manner. We believe, that for the benefit of future patients, further research should be performed at two different levels. First at the clinical level, prospective and uniform measurements and registration on all aspects of hyperthermia treatments, including standardized thermal dose and time interval measurements, should be performed across multiple hyperthermia centers. Second, in vivo studies regarding the exact working mechanisms of hyperthermia in patients, not in models, are highly needed. We feel that the Overgaard paper is an important paper, but it represents only a single experimental setup in one tumor model, and can thus not be generalized to the clinic (14).
Finally, fueled by similar level evidence showing conflicting results, the controversy about the effect of the time interval between RT and HT on clinical outcome will be ongoing. We conclude that, during this period, patients with a contraindication or refusing concurrent chemoradiotherapy, can undergo thermoradiotherapy even with long time intervals with the suggestion of no detriment in efficacy compared to short intervals.
Ethics Statement
The research protocol for this investigation was approved by the medical ethics committee of Erasmus MC Cancer Institute, Rotterdam, the Netherlands (MEC-2018-1081).
Author Contributions
MK: drafting of the manuscript. HM and MF: critical review of the manuscript. GR: drafting of the manuscript and critical review of the manuscript.
Funding
This study was supported by the Dutch Cancer Society (grant DDHK 2013-6072).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Kroesen M, Mulder HT, van Holthe JML, Aangeenbrug AA, Mens JWM, van Doorn HC, et al. The effect of the time interval between radiation and hyperthermia on clinical outcome in 400 locally advanced cervical carcinoma patients. Front Oncol. (2019) 9:134. doi: 10.3389/fonc.2019.00134
2. Chemoradiotherapy for Cervical Cancer Meta-Analysis Collaboration. Reducing uncertainties about the effects of chemoradiotherapy for cervical cancer: a systematic review and meta-analysis of individual patient data from 18 randomized trials. J Clin Oncol. (2008) 26:5802–12. doi: 10.1200/JCO.2008.16.4368
3. Franckena M, Stalpers LJ, Koper PC, Wiggenraad RG, Hoogenraad WJ, van Dijk JD, et al. Long-term improvement in treatment outcome after radiotherapy and hyperthermia in locoregionally advanced cervix cancer: an update of the Dutch Deep Hyperthermia Trial. Int J Radiat Oncol Biol Phys. (2008) 70:1176–82. doi: 10.1016/j.ijrobp.2007.07.2348
4. Franckena M, Lutgens LC, Koper PC, Kleynen CE, van der Steen-Banasik EM, Jobsen JJ, et al. Radiotherapy and hyperthermia for treatment of primary locally advanced cervix cancer: results in 378 patients. Int J Radiat Oncol Biol Phys. (2009) 73:242–50. doi: 10.1016/j.ijrobp.2008.03.072
5. van der Zee J, Koper PC, Lutgens LC, Burger CW. Point-counterpoint: what is the optimal trial design to test hyperthermia for carcinoma of the cervix? Point: addition of hyperthermia or cisplatin to radiotherapy for patients with cervical cancer; two promising combinations–no definite conclusions. Int J Hyperthermia. (2002) 18:19–24. doi: 10.1080/02656730110083738
6. van Leeuwen CM, Oei AL, Chin KWTK, Crezee J, Bel A, Westermann AM, et al. A short time interval between radiotherapy and hyperthermia reduces in-field recurrence and mortality in women with advanced cervical cancer. Radiat Oncol. (2017) 12:75. doi: 10.1186/s13014-017-0813-0
7. Crezee H, Kok HP, Oei AL, Franken NAP, Stalpers LJA. The impact of the time interval between radiation and hyperthermia on clinical outcome in patients with locally advanced cervical cancer. Front Oncol. (2019) 9:412. doi: 10.3389/fonc.2019.00412
8. van den Tempel N, Odijk H, van Holthe N, Naipal K, Raams A, Eppink B, et al. Heat-induced BRCA2 degradation in human tumours provides rationale for hyperthermia-PARP-inhibitor combination therapies. Int J Hyperthermia. (2017) 34:407–14. doi: 10.1080/02656736.2017.1355487
9. van den Tempel N, Laffeber C, Odijk H, van Cappellen WA, van Rhoon GC, Franckena M, et al. The effect of thermal dose on hyperthermia-mediated inhibition of DNA repair through homologous recombination. Oncotarget. (2017) 8:44593–604. doi: 10.18632/oncotarget.17861
10. Krawczyk PM, Eppink B, Essers J, Stap J, Rodermond H, Odijk H, et al. Mild hyperthermia inhibits homologous recombination, induces BRCA2 degradation, and sensitizes cancer cells to poly (ADP-ribose) polymerase-1 inhibition. Proc Natl Acad Sci USA. (2011) 108:9851–6. doi: 10.1073/pnas.1101053108
11. Kok HP, Korshuize-van Straten L, Bakker A, de Kroon-Oldenhof R, Geijsen ED, Stalpers LJA, et al., Online adaptive hyperthermia treatment planning during locoregional heating to suppress treatment-limiting hot spots. Int J Radiat Oncol Biol Phys. (2017) 99:1039–47. doi: 10.1016/j.ijrobp.2017.07.011
12. Franckena M, Canters R, Termorshuizen F, Van Der Zee J, Van Rhoon G. Clinical implementation of hyperthermia treatment planning guided steering: a cross over trial to assess its current contribution to treatment quality. Int J Hyperthermia. (2010) 26:145–57. doi: 10.3109/02656730903453538
13. Kroesen M, Mulder HT, van Holthe JML, Aangeenbrug AA, Mens JWM, van Doorn HC, et al. Confirmation of thermal dose as a predictor of local control in cervical carcinoma patients treated with state-of-the-art radiation therapy and hyperthermia. Radiother Oncol. (2019) 140:150–8.
Keywords: hyperthermia, cervical cancer, thermal dose, clinical outcome, time interval
Citation: Kroesen M, Mulder HT, van Rhoon GC and Franckena M (2019) Commentary: The Impact of the Time Interval Between Radiation and Hyperthermia on Clinical Outcome in Patients With Locally Advanced Cervical Cancer. Front. Oncol. 9:1387. doi: 10.3389/fonc.2019.01387
Received: 13 August 2019; Accepted: 25 November 2019;
Published: 17 December 2019.
Edited by:
Daniel Grant Petereit, Rapid City Regional Hospital, United StatesReviewed by:
Pranshu Mohindra, University of Maryland, Baltimore, United StatesCopyright © 2019 Kroesen, Mulder, van Rhoon and Franckena. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Martine Franckena, m.franckena@erasmusmc.nl
 Michiel Kroesen
Michiel Kroesen H. Tim Mulder
H. Tim Mulder Gerard C. van Rhoon
Gerard C. van Rhoon Martine Franckena1*
Martine Franckena1*