- 1Institute for Health and Society, Newcastle University, Newcastle upon Tyne, United Kingdom
- 2Speech and Language Therapy Department, City Hospitals Sunderland Foundation Trust, Sunderland, United Kingdom
The prevalence of head and neck cancer (HNC) survivors is on the rise. Treatments for HNC can have a major deleterious impact on functions such as swallowing and voice. Poor functional outcomes are strongly correlated with distress, low quality of life, difficulties returning to work and socializing. Furthermore, dysphagia can have serious medical consequences such as malnutrition, dehydration, and pneumonia. A conservative estimate of the percentage of survivors living with dysphagia in the long-term is between 50 and 60%. Evidence is emerging that functions can worsen over time, sometimes several years following treatment due to radiation-associated fibrosis, neuropathy, intractable edema, and atrophy. Muscles lose their strength, pliability, stamina, and range, speed, precision, and initiation of movements necessary for swallowing and voice functions. Late treatment effects can go unrecognized, and may only be identified when there is a medical complication such as hospitalization for aspiration pneumonia. In the routine healthcare setting methods of evaluation include a detailed case history, a thorough clinical examination and instrumental assessments. Interventions for late treatment effects are limited and it is imperative that patients at risk are identified as early as possible. This paper considers the role of screening tests in monitoring swallowing and detecting aspiration in the long-term. Further work is indicated for addressing this pressing and increasingly common clinical problem.
Introduction
The prevalence of head and neck cancer (HNC) survivors is on the increase, likely due to improvements in diagnostic technologies, treatment techniques, and a rising number of HPV-related oropharyngeal cancers, with patients presenting at a younger age with good survival outcome (1). HNC treatments can result in a multitude of side effects resulting in poor function. Post-treatment swallowing and voice difficulties are strongly related to psychosocial problems, poorer quality of life, anxiety, and low mood (2, 3). In addition, dysphagia can pose a serious medical threat, being associated with malnutrition, dehydration, and possibly pneumonia. Survivors may therefore live for a long time with significant symptom burden, which can increase in severity over time. This paper reports on the presentation, assessment, and potential screening tests for late treatment effects on swallowing and voice.
The Complexity of Swallowing and Voice
Swallowing and voice are highly coordinated, specialized functions involving over 25 pairs of muscles under both voluntary and involuntary control. Swallowing is a finely tuned process, primarily because the oropharynx is a shared passageway for swallowing and respiration. It needs to be executed safely, avoiding spillage into the airway, and efficiently, to ensure adequate nourishment and hydration. Voice is produced by air passing through the vocal folds, causing the edges to vibrate rapidly. This sound is amplified by resonating cavities in the vocal tract, giving it a distinctive quality. The active articulators (tongue, lips and soft palate) modify the voiced sound into speech via quick and precise movements.
Late Treatment Effects on Function
Surgical treatment for HNC may result in functional impairment, dependent on factors such as tumor site, volume resected, reconstruction, and the subsequent level of edema, scarring, and atrophy (4). Radiotherapy can create significant dysfunction both acutely and progressively also termed “late effects.” Acute radiotherapy side effects usually include pain, mucosititis, edema, and xerostomia. For some, this results in mild or short-term dysphagia and dysphonia, resolving by 3 months. This group are likely to return to their normal diet with minor limitations. This is a typical pattern for those treated by low dose radiotherapy (2, 5), but may be achieved by a small percentage of patients with advanced disease treated by intensity-modulated radiotherapy (IMRT) (6).
Dysphagia
Evidence relating to the long-term impact of treatment on swallowing is emerging, with a number of potential patterns described by Christianen (5). Some patients experience progressive deterioration in the months and years following treatment, whereas others may have a sudden onset of severe dysphagia. Causes of these differing trajectories are not well-understood. Chronic edema and increased fibroblast formation are responsible for the overproduction of collagen, leading to scarring, and fibrosis (7). Consequently, tissues lose their elasticity and movements for adequate functioning are restricted. Atrophy can alter oropharyngeal anatomical relationships and reduce muscle strength. Furthermore, sensory impairment can blunt the cough response, should food, or drink enter the airway. Lower cranial nerve palsies (CN IX, X, and XII) have been noted, probably due to compression or direct nerve damage (8). Mandible osteoradionecrosis is a further late complication, resulting in exposed, non-healing bone (9). This is strongly associated with severe, chronic dysphagia (OR: 4.6, 95% CI: 2.1–10.3), making chewing painful and swallowing less efficient (10). Dysphagia is strongly associated with psychological distress, poorer quality of life, and is a top priority concern for HNC survivors (2, 11, 12)
Prevalence of Late Effects Dysphagia
Little information is published on swallowing outcomes beyond 2 years. In our longitudinal study (n = 146 recruited pre-treatment), aspiration rates remained stable between one and 6 years following chemoradiotherapy (22–25%), with one half of these patients having silent aspiration (13). At 1 year, two patients had a laryngectomy for a dysfunctional larynx and four had a tracheostomy due to airway compromise. By 6 years, five further patients had a laryngectomy for a dysfunctional larynx (13). An Australian study reported a decline in swallowing efficiency over the same time frame (14). The RTOG 91–11 5 year follow up identified severe dysphagia in a third of the retained sample (15). SEER data reported a 49% rate of persistent dysphagia (16, 17), with older patients following non-surgical treatment being most at risk (18, 19).
Dysphagia Associated Risk
Aspiration is a medical concern as it can lead to repeated chest infections, poor pulmonary function, and life-threatening aspiration pneumonia (20). In our 6 year follow up cohort, 28% reported at least one chest infection, with an increased risk ratio of 6.25 [p = 0.03 CI 1.1–35.7] for aspirators (13). Seven percent of those initially diagnosed with oropharyngeal cancer had a non-functioning larynx, requiring complex, and major reconstructive surgery (13). SEER data suggests the incidence of aspiration pneumonia in HNC is 8.7% (95% CI: 8.2–9.1) (17) and it is estimated that over 80% require hospital admission, half of whom transfer to intensive care (20). Case series and cross-sectional data report alarmingly high rates of aspiration-related deaths (21–23). For example, the 30-day mortality rate in a series of nasopharyngeal cancer patients was 51% (24). It is crucial that we identify those at risk of developing aspiration pneumonia as early as possible.
Dysphonia
The prevalence of late voice problems are not well-documented. Small studies suggest deterioration in patient reports and clinical tests of voice up to 7 years post-treatment (25, 26). However, patients treated with IMRT appear to have better outcomes than those treated with conventional radiotherapy, in the long-term (3). A small percentage of patients may require a tracheostomy or laryngectomy, significantly altering voice quality (13).
Assessment
Clinical Swallowing and Voice Assessment
In the first instance, patients presenting with new symptoms, or deterioration in function should have recurrent or primary disease excluded as a possible cause. A comprehensive clinical history of late effects will include details on patients' perceptions of the onset, trajectory, and symptoms. Clinical information such as co-morbidities, reflux, chest status, oral intake, oral hygiene, and weight should be gathered. For older survivors, expected, age-related functional decline i.e., loss of muscle mass and elasticity, reduced saliva production should be taken into account. An examination will typically include and oral and oromotor assessment, palpation of laryngeal structures, voice, and speech quality assessment and an observation of eating and drinking.
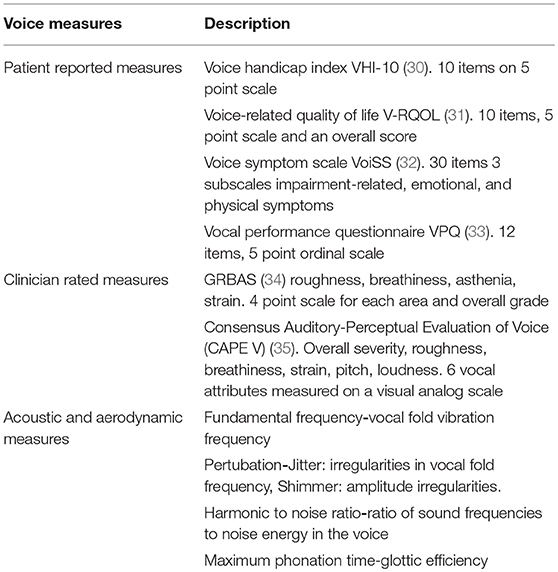
There are no agreed standards for long-term voice assessment, although review papers call for structured, standardized protocols, with measurements taken at baseline and long-term (27, 28). These typically include clinician rated scales, intelligibility rating, and acoustic measures (29). Examples of scales and measures used in HNC are given in Table 1.
Patient Reported Outcome Measures
Measures of function in HNC should include patient-reported outcomes both pre- and post-treatment. Swallowing questionnaires and symptom report tools capture patients' perspectives of dysphagia, but they are only weakly correlated with swallowing impairment and aspiration, the relationship being particularly poor beyond 12 months post-treatment. They are therefore not interchangeable with clinical assessment (36, 37). The most commonly reported swallowing questionnaires used in HNC care include M.D. Anderson Dysphagia Inventory (38), SWAL-QOL (39), Sydney Swallow Questionnaire (40), and the EAT-10 (41). Examples of patient reported voice questionnaires include Voice Handicap Index (30), Voice Symptom Scale (32), and the Vocal Performance Questionnaire (42).
Instrumental Assessment
Instrumental examination(s) is indicated for a thorough investigation of pathophysiology. Videofluoroscopy (VF) and Fiberoptic Endoscopic Evaluation of Swallowing (FEES®) are the most commonly used instrumental swallow assessments (43). VF is a recorded radiographic study of the swallowing structures, their movement and co-ordination. It is usually conducted in the lateral and anterior-posterior plane. Test boluses are mixed with radio-opaque material to enable visualization. FEES® allows a direct view of nasolaryngopharyngeal anatomy and physiology followed by an assessment of swallowing function (44, 45). A range of fluid and food can be given, without requiring radio opaque contrast. This may be combined with a voice assessment, which also requires a stroboscopic light source to fully assess vocal fold function and mucosal wave pattern.
The presentation of late treatment effects on instrumental assessment constitutes a number of features such as;
• Excessive external lymphedema, with underlying tissue hardening.
• Internal edema in critical structures and spaces for functioning e.g., true vocal folds, epiglottis, pyriform sinuses.
• Thickening of structures e.g., pharyngo-epiglottic folds creating a shelf-like barrier to bolus flow.
• Muscle thinning e.g., atrophied tongue base and pharyngeal wall.
• Palsies of the tongue, vocal fold, soft palate.
• Excessively dry laryngopharyngeal muscosa.
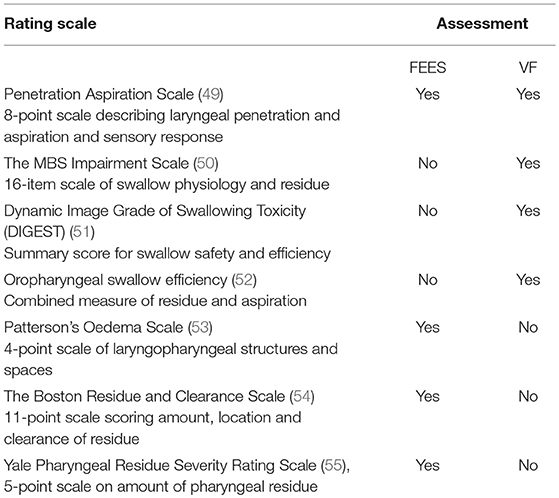
The pathophysiology, safety, and efficiency of swallowing can be analyzed and measured using rating scales, a selection of which are presented in Table 2.
Monitoring
Cancer surveillance reviews are usually offered up to 5 years following treatment (1). Swallowing and voice function may not be routinely tested, unless patients report a problem. One preliminary study proposes four questions that could be used as part of a clinical assessment to detect dysphagia i.e., Do you have difficulties: (1) drinking? (2) eating? (3) swallowing? (4) Do you cough when eating/drinking? When three or more of these questions were answered affirmatory, the likelihood of aspiration observed on VF increased (46). Given afore described mortality risks, and the preponderance of sub-clinical aspiration, the immediate clinical challenge is identifying those at risk of developing pneumonia, using reliable, repeatable, and cost-effective tests.
Identifying Patients at Risk of Aspiration Pneumonia
Healthy adults can experience trace aspiration without adverse consequences, and not every HNC survivor with aspiration appears to develop pneumonia. In a series of partial laryngectomy patients, 65% were identified with aspiration, but without x-ray evidence of pneumonia or infection (47). There may be additional factors to be taken into account, when weighing up pneumonia risk. For example, older adults in a care facility developed pneumonia only when aspiration co-occurred with poor oral hygiene, dependence on others for eating, poor dentition and co-morbidities (48). Most HNC studies have explored patient and disease characteristics and treatment type as predictors of pneumonia, with no clear pattern emerging (see Table 3). Further work on identifying predictor variables for aspiration pneumonia to be used as part of an algorithm for monitoring purposes is required.
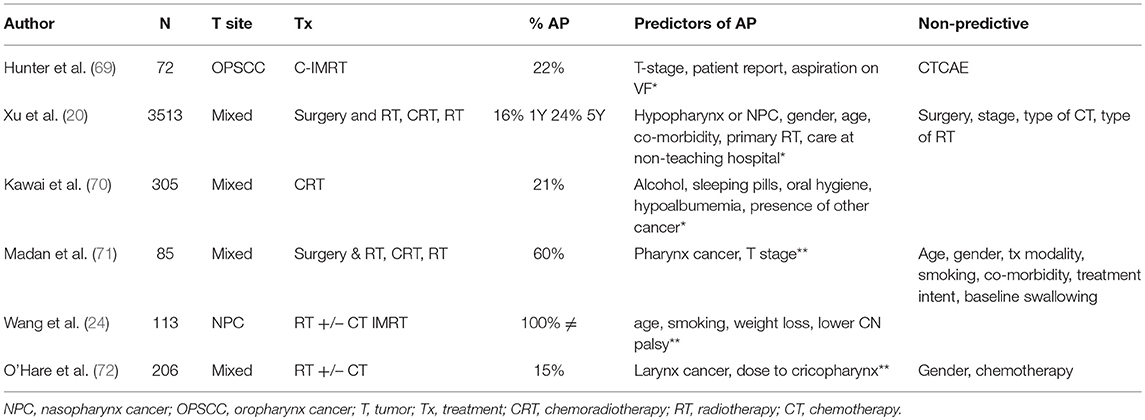
Table 3. HNC studies reporting predictors of (1) aspiration pneumonia* (2) aspiration pneumonia-related death** ≠ Wang et al. (24) only included patients with a diagnosis of aspiration pneumonia.
Screening Assessments
Instrumental assessments provide a more objective way of measuring swallowing, but have limited access and high cost, due to the need for specialist equipment and personnel (56). In Stroke care, early detection of dysphagia by screening reduces pulmonary complications, length of hospital stay, and overall health care costs (57). No such programme exists for HNC survivors, but the following section reviews candidate screening tests for this group.
Water Swallow Test
A water swallow test (WST) is the most commonly reported aspiration screening tool (58). Two systematic reviews report a range of protocols, predominantly for testing neurological dysphagia (56, 58–61). Using prescribed amounts of water and recording coughing or a wet voice gave the most accurate results for identifying aspiration (56, 62). Consecutive sips with large volumes had the best sensitivity (91% CI 89, 93%) while, single sips of water were better at ruling out aspiration (90% CI 86, 93%) (58). We have reported on the timed 100 mLs WST in HNC, recording swallowing performance overtime, as well as a screening test for aspiration (63). This test was acceptable for identifying aspiration in early post-operative or chemoradiotherapy patient groups (63, 64), but its reliability for late effects patients has not been investigated.
Cough Reflex Test
This test assesses the cough reflex by introducing a tussive agent such as citric acid via a facemask and nebulizer and observing for a responsive cough (65). The outcome is judged on reflexive cough strength and has been used as screening test in Stroke (65), Parkinson's Disease (66), and post-extubation (67). The absence of a cough reflex in neurological patients has a sensitivity of 69% (95% CI 55, 81%) and specificity of 71% (95% CI 63, 77%) to detect aspiration (65). No studies have reported on its use in HNC, but given that late effects can result in silent aspiration, further investigation is warranted.
Pulmonary Function
Many patients elect to eat and drink despite experiencing aspiration. Assessments to monitor pulmonary function such as spirometry and flow-volume loops may be indicated together with close collaboration with Respiratory Physicians to develop mechanisms to detect deterioration in chest status.
Future Directions
There are a number of current trials investigating treatment modulation to prevent or reduce toxicities without compromising survival (68). In the meantime, further work on late functional effects is indicated in the following areas.
• Information on the long-term outcomes for voice and speech.
• Identification of predictors of significant fibrosis and exploration of preventative interventions.
• Identification of predictor variables for pneumonia in patients who aspirate.
• Reliable screening tests for identifying aspiration and dysphagia for long-term follow up.
• Accurate patient information regarding late treatment effects.
• Clinical care pathways for identifying and monitoring late functional effects.
Conclusion
The number of HNC survivors is rising and this trend is set to continue. Late functional effects of treatment is a common, distressing, and potentially life-threatening problem. Assessment and monitoring of HNC survivors in the long-term is an important step for identifying those at risk, as early as possible. Reliable, acceptable, and repeatable screening assessments are needed to address this growing problem.
Author Contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of Interest Statement
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Nguyen NTA, Ringash J. Head and neck cancer survivorship care: a review of the current guidelines and remaining unmet needs. Curr Treat Options Oncol. (2018) 19:44. doi: 10.1007/s11864-018-0554-9
2. Wilson JA, Carding PN, Patterson JM. Dysphagia after nonsurgical head and neck cancer treatment: patients' perspectives. Otolaryngol Head Neck Surg. (2011) 145:767–71. doi: 10.1177/0194599811414506
3. Kraaijenga SAC, Oskam IM, van Son RJ, Hamming-Vrieze O, Hilgers FJ, van den Brekel MW, van der Molen L. Assessment of voice, speech, and related quality of life in advanced head and neck cancer patients 10-years+ after chemoradiotherapy. Oral Oncol. (2016) 55:24–30. doi: 10.1016/j.oraloncology.2016.02.001
4. Mittal BB, Pauloski BR, Haraf DJ, Pelzer HJ, Argiris A, Vokes EE, et al. Swallowing dysfunction–preventative and rehabilitation strategies in patients with head-and-neck cancers treated with surgery, radiotherapy, and chemotherapy: a critical review. Int J Radiation Oncol Biol Phys. (2003) 57:1219–30. doi: 10.1016/S0360-3016(03)01454-8
5. Christianen MEMC, Verdonck-de Leeuw IM, Doornaert P, Chouvalova O, Steenbakkers RJ, Koken PW, et al. Patterns of long-term swallowing dysfunction after definitive radiotherapy or chemoradiation. Radiother Oncol. (2015) 117:139–44. doi: 10.1016/j.radonc.2015.07.042
6. Roe JWG, Carding PN, Drinnan MJ, Harrington KJ, Nutting CM, et al. Swallowing performance and tube feeding status in patients treated with parotid-sparing intensity-modulated radiotherapy for head and neck cancer. Head Neck. (2016) 38:E1436–44. doi: 10.1002/hed.24255
7. Straub JM, New J, Hamilton CD, Lominska C, Shnayder Y, Thomas SM. Radiation-induced fibrosis: mechanisms and implications for therapy. J Cancer Res Clin Oncol. (2015) 141:1985–94. doi: 10.1007/s00432-015-1974-6
8. Rison RA, Beydoun SR. Delayed cervicobulbar neuronopathy and myokymia after head and neck radiotherapy for nasopharyngeal carcinoma: a case report. J Clin Neuromuscul Dis. (2011) 12:147–52. doi: 10.1097/CND.0b013e31820d4f20
9. Strojan P, Hutcheson KA, Eisbruch A, Beitler JJ, Langendijk JA, Lee AWM, et al. Treatment of late sequelae after radiotherapy for head and neck cancer. Cancer Treat Rev. (2017) 59:79–92. doi: 10.1016/j.ctrv.2017.07.003
10. Wong ATT, et al. Symptom burden and dysphagia associated with osteoradionecrosis in long-term oropharynx cancer survivors: a cohort analysis. Oral Oncol. (2017) 66:75–80. doi: 10.1016/j.oraloncology.2017.01.006
11. Rhoten BA, et al. Depressive symptoms, social anxiety, and perceived neck function in patients with head and neck cancer. Head and Neck. (2018) 40:1443–1452. doi: 10.1002/hed.25129
12. Patterson JM, McColl E, Carding PN, Hildreth AJ, Kelly C, Wilson JA. Swallowing in the first year after chemoradiotherapy for head and neck cancer: clinician-and patient-reported outcomes. Head Neck. (2014) 36, 352–8. doi: 10.1002/hed.23306
13. Patterson JM, McColl E, Carding PN, Wilson JA. Swallowing beyond six years post (chemo)radiotherapy for head and neck cancer; a cohort study. Oral Oncol. (2018) 83:53–8. doi: 10.1016/j.oraloncology.2018.06.003
14. Frowen J, Drosdowsky A, Perry A, Corry J. Long-term swallowing after chemoradiotherapy: prospective study of functional and patient-reported changes over time. Head Neck. (2016) 38:E307–15. doi: 10.1002/hed.23991
15. Ward MC, Adelstein DJ, Bhateja P, Nwizu TI, Scharpf J, Houston N, et al. Severe late dysphagia and cause of death after concurrent chemoradiation for larynx cancer in patients eligible for RTOG 91-11. Oral Oncol. (2016) 57:21–6. doi: 10.1016/j.oraloncology.2016.03.014
16. Shune SE, Karnell LH, Karnell MP, Van Daele DJ, Funk GF. Association between severity of dysphagia and survival in patients with head and neck cancer. Head Neck-J Sci Special Head Neck. (2012) 34:776–84. doi: 10.1002/hed.21819
17. Hutcheson KA, Nurgalieva Z, Zhao H, Gunn GB, Giordano SH, Bhayani MK, et al. Two-year prevalence of dysphagia and related outcomes in head and neck cancer survivors: an updated SEER-Medicare analysis. Head Neck. (2019) 41:479–87. doi: 10.1002/hed.25412
18. Gourin CG, Starmer HM, Herbert RJ, Frick KD, Forastiere AA, Quon H, et al. Quality of care and short- and long-term outcomes of laryngeal cancer care in the elderly. Laryngoscope. (2015) 125:2323–9. doi: 10.1002/lary.25378
19. Motz K, Herbert RJ, Fakhry C, Quon H, Kang H, Kiess AP, Eisele DW, et al. Short- and long-term outcomes of oropharyngeal cancer care in the elderly. Laryngoscope. (2018) 128:2084–93. doi: 10.1002/lary.27153
20. Xu B, Boero IJ, Hwang L, Le QT, Moiseenko V, Sanghvi PR, et al. Aspiration pneumonia after concurrent chemoradiotherapy for head and neck cancer. Cancer. (2015) 121:1303–11. doi: 10.1002/cncr.29207
21. Hutcheson KA, Lewin JS, Barringer DA, Lisec A, Gunn GB, Moore MW, et al. Late dysphagia after radiotherapy-based treatment of head and neck cancer. Cancer. (2012) 118:5793–9. doi: 10.1002/cncr.27631
22. Szczesniak MM, Maclean J, Zhang T, Graham PH, Cook IJ. Persistent dysphagia after head and neck radiotherapy: a common and under-reported complication with significant effect on non-cancer-related mortality. Clin Oncol. (2014) 26:697–703. doi: 10.1016/j.clon.2014.08.009
23. Dong Y, Ridge JA, Li T, Lango MN, Churilla TM, Bauman JR, et al. Long-term toxicities in 10-year survivors of radiation treatment for head and neck cancer. Oral Oncol. (2017) 71(Suppl C):122–8. doi: 10.1016/j.oraloncology.2017.05.009
24. Wang JJ, Jiang RS, Yen TT, Liang KL. Risk factors for recurrent pneumonia in post-irradiated patients with nasopharyngeal carcinoma. J Chin Med Assoc. (2017) 80:558–62. doi: 10.1016/j.jcma.2017.01.006
25. Davies-Husband C, Murphy J, Kelly C, Drinnan M, Paleri V. Extreme long-term voice outcomes after concurrent chemoradiotherapy for advanced non-laryngeal head and neck cancer: eight-year post-treatment analysis. Clin Otolaryngol. (2018) 43:1494–9. doi: 10.1111/coa.13204
26. Dwivedi RC, St Rose S, Chisholm EJ, Clarke PM, Kerawala CJ, Nutting CM, et al. Acoustic parameters of speech: lack of correlation with perceptual and questionnaire-based speech evaluation in patients with oral and oropharyngeal cancer treated with primary surgery. Head Neck. (2016) 38:670–6. doi: 10.1002/hed.23956
27. Jacobi I, van der Molen L, Huiskens H, van Rossum MA, Hilgers FJ. Voice and speech outcomes of chemoradiation for advanced head and neck cancer: a systematic review. Eur Arch Oto-Rhino-Laryngol. (2010) 267:1495–505. doi: 10.1007/s00405-010-1316-x
28. Schuster M, Stelzle F. Outcome measurements after oral cancer treatment: speech and speech-related aspects-an overview. Oral Maxillofacial Surg. (2012) 16:291–8. doi: 10.1007/s10006-012-0340-y
29. Dwivedi RC, Kazi RA, Agrawal N, Nutting CM, Clarke PM, Kerawala CJ, et al. Evaluation of speech outcomes following treatment of oral and oropharyngeal cancers. Cancer Treat Rev. (2009) 35:417–24. doi: 10.1016/j.ctrv.2009.04.013
30. Rosen CA, Lee AS, Osborne J, Zullo T, Murry T. Development and validation of the voice handicap index-10. Laryngoscope. (2004) 114:1549–56. doi: 10.1097/00005537-200409000-00009
31. Hogikyan ND, Sethuraman G Validation of an instrument to measure voice-related quality of life (V-RQOL). J Voice. (1999) 13:557–69. doi: 10.1016/S0892-1997(99)80010-1
32. Deary IJ, Wilson JA, Carding PN, MacKenzie K. VoiSS: a patient-derived voice symptom scale. J Psychosomat Res. (2003) 54:483–489. doi: 10.1016/S0022-3999(02)00469-5
33. Carding PN, Horsley IA. An evaluation study of voice therapy in non-organic dysphonia. Int J Lang Commun Disord. (1992) 27:137–58. doi: 10.3109/13682829209012036
35. Association A.S.a.H. Consensus Auditory-Perceptual Evaluation of Voice (CAPE-V). (2002) Available online at: https://www.asha.org/uploadedFiles/members/divs/D3CAPEVprocedures.pdf.
36. Pedersen A, Wilson J, McColl E, Carding P, Patterson J. Swallowing outcome measures in head and neck cancer - How do they compare? Oral Oncol. (2016) 52:104–8. doi: 10.1016/j.oraloncology.2015.10.015
37. Arrese LC, Carrau R, Plowman EK. Relationship between the eating assessment Tool-10 and objective clinical ratings of swallowing function in individuals with head and neck cancer. Dysphagia. (2017) 32:83–9. doi: 10.1007/s00455-016-9741-7
38. Chen AY, Frankowski R, Bishop-Leone J, Hebert T, Leyk S, Lewin J, et al. The development and validation of a dysphagia-specific quality-of-life questionnaire for patients with head and neck cancer: the M. D. Anderson Dysphagia Inventory. Arch Otolaryngol Head Neck Surg. (2001) 127:870–6. doi: 10.1001/pubs.ArchOtolaryngol.HeadNeckSurg.-ISSN-0886-4470-127-7-ooa00162
39. McHorney CA, Robbins J, Lomax K, Rosenbek JC, Chignell K, Kramer AE, et al. The SWAL-QOL and SWAL-CARE outcomes tool for oropharyngeal dysphagia in adults: III. Documentation of reliability and validity. Dysphagia. (2002) 17:97–114. doi: 10.1007/s00455-001-0109-1
40. Wallace KL, Middleton S, Cook IJ. Development and validation of a self-report symptom inventory to assess the severity of oral-pharyngeal dysphagia. Gastroenterology. (2000) 118:678–87. doi: 10.1016/S0016-5085(00)70137-5
41. Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, et al. Validity and reliability of the eating assessment tool (EAT-10). Ann Otol Rhinol Laryngol. (2008) 117:919–24. doi: 10.1177/000348940811701210
42. Carding PN, Horsley IA, Docherty GJ. A study of the effectiveness of voice therapy in the treatment of 45 patients with nonorganic dysphonia. J Voice. (1999) 13:72–104. doi: 10.1016/S0892-1997(99)80063-0
43. Goldsmith T, Jacobson MC. Managing the late effects of chemoradiation on swallowing: bolstering the beginning, minding the middle, and cocreating the end. Curr Opin Otolaryngol Head Neck Surg. (2018) 26:180–7. doi: 10.1097/MOO.0000000000000455
44. RCSLT. Fibreoptic Endoscopic Evaluation of Swallowing (FEES): The Role of Speech and Language Therapy Royal College of Speech and Language Therapists Position Paper. London: RCSLT (2015). Available online at: https://www.rcslt.org/-/media/Project/RCSLT/fees-position-paper-march-2015.pdf.
45. Langmore SE. Endoscopic Evaluation and Treatment of Swallowing Disorders. New York, NY: Thieme. (2001).
46. Hedström J, Tuomi L, Finizia C, Olsson C. Correlations between patient-reported dysphagia screening and penetration-aspiration scores in head and neck cancer patients post-oncological treatment. Dysphagia. (2018) 33:206–15. doi: 10.1007/s00455-017-9847-6
47. Simonelli M, Ruoppolo G, de Vincentiis M, Di Mario M, Calcagno P, Vitiello C, et al. Swallowing ability and chronic aspiration after supracricoid partial laryngectomy. Otolaryngol Head Neck Surg. (2010) 142:873–8. doi: 10.1016/j.otohns.2010.01.035
48. Langmore SE, Terpenning MS, Schork A, Chen Y, Murray JT, Lopatin D, et al. Predictors of aspiration pneumonia: how important is dysphagia? Dysphagia. (1998) 13:69–81. doi: 10.1007/PL00009559
49. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. (1996) 11:93–8. doi: 10.1007/BF00417897
50. Martin-Harris B, Brodsky MB, Michel Y, Castell DO, Schleicher M, Sandidge J, et al. MBS measurement tool for swallow impairment-MBSimp: establishing a standard. Dysphagia. (2008) 23:392–405. doi: 10.1007/s00455-008-9185-9
51. Hutcheson KA, Barrow MP, Barringer DA, Knott JK, Lin HY, Weber RS, et al. Dynamic imaging grade of swallowing toxicity (DIGEST): scale development and validation. Cancer. (2017) 123:62–70. doi: 10.1002/cncr.30283
52. Rademaker AW, Pauloski BR, Logemann JA, Shanahan TK. Oropharyngeal swallow efficiency as a representative measure of swallowing function. J Speech Hear Res. (1994) 37:314–25. doi: 10.1044/jshr.3702.314
53. Patterson JM, Hildreth A, Wilson JA. Measuring edema in irradiated head and neck cancer patients. Ann Otol Rhinol Laryngol. (2007) 116:559–64. doi: 10.1177/000348940711600801
54. Kaneoka AS, Langmore SE, Krisciunas GP, Field K, Scheel R, McNally E, et al. The Boston residue and clearance scale: preliminary reliability and validity testing. Folia Phoniatr et Logopaed. (2014) 65:312–7. doi: 10.1159/000365006
55. Neubauer PD, Rademaker AW, Leder S B. The yale pharyngeal residue severity rating scale: an anatomically defined and image-based tool. Dysphagia. (2015) 30:521–8. doi: 10.1007/s00455-015-9631-4
56. Bours GJ, Speyer R, Lemmens J, Limburg M, de Wit R. Bedside screening tests vs. videofluoroscopy or fibreoptic endoscopic evaluation of swallowing to detect dysphagia in patients with neurological disorders: systematic review. J Adv Nurs. (2009) 65:477–93. doi: 10.1111/j.1365-2648.2008.04915.x
57. Marsh K, Bertranou E, Suominen H, Venkatachalam M. The Economic Case for Speech And Language Therapy. Report Matrix Evidence (2010). Available online at: https://optimityadvisors.com/sites/default/files/research-papers/45-Speech-and-Language.pdf
58. Brodsky MB, Suiter DM, González-Fernández M, Michtalik HJ, Frymark TB, Venediktov R, et al. Screening accuracy for aspiration using bedside water swallow tests: a systematic review and meta-analysis. Chest. (2016) 150:148–63. doi: 10.1016/j.chest.2016.03.059
59. Jiang JL, Fu SY, Wang WH, Ma YC. Validity and reliability of swallowing screening tools used by nurses for dysphagia: a systematic review. Tzu Chi Med J. (2016) 28:41–8. doi: 10.1016/j.tcmj.2016.04.006
60. Chen PC, Chuang CH, Leong CP, Guo SE, Hsin YJ. Systematic review and meta-analysis of the diagnostic accuracy of the water swallow test for screening aspiration in stroke patients. J Adv Nurs. (2016) 72:2575–86. doi: 10.1111/jan.13013
61. Virvidaki IE, Nasios G, Kosmidou M, Giannopoulos S, Milionis H. Swallowing and aspiration risk: a critical review of non instrumental bedside screening tests. J Clin Neurol. (2018) 14:265–74. doi: 10.3988/jcn.2018.14.3.265
62. McCullough GH, Rosenbek JC, Wertz RT, McCoy S, Mann G, McCullough K. Utility of clinical swallowing examination measures for detecting aspiration post-stroke. J Speech Language Hear Res. (2005) 48:1280–93. doi: 10.1044/1092-4388(2005/089)
63. Patterson JM, McColl E, Carding PN, Kelly C, Wilson JA. Swallowing performance in patients with head and neck cancer: a simple clinical test. Oral Oncol. (2009) 45:904–7. doi: 10.1016/j.oraloncology.2009.03.012
64. Hey C, Lange BP, Eberle S, Zaretsky Y, Sader R, Stöver T, et al. Water swallow screening test for patients after surgery for head and neck cancer: early identification of dysphagia, aspiration and limitations of oral intake. Anticancer Res. (2013) 33:4017–22. doi: 10.1007/s00455-014-9536-7
65. Miles A, Moore S, McFarlane M, Lee F, Allen J, Huckabee ML. Comparison of cough reflex test against instrumental assessment of aspiration. Physiol Behav. (2013) 118:25–31. doi: 10.1016/j.physbeh.2013.05.004
66. Troche MS, Schumann B, Brandimore AE, Okun MS, Hegland KW. Reflex cough and disease duration as predictors of swallowing dysfunction in parkinson's disease. Dysphagia. (2016) 31:757–64. doi: 10.1007/s00455-016-9734-6
67. Kallesen M, Psirides A, Huckabee ML. Comparison of cough reflex testing with videoendoscopy in recently extubated intensive care unit patients. J Crit Care. (2016) 33:90–4. doi: 10.1016/j.jcrc.2016.02.004
68. Patterson JM, Brady GC, JRoe WG. Research into the prevention and rehabilitation of dysphagia in head and neck cancer: a UK perspective. Curr Opin Otolaryngol Head Neck Surg. (2016) 24:208–14. doi: 10.1097/MOO.0000000000000260
69. Hunter KU, Lee OE, Lyden TH, Haxer MJ, Feng FY, Schipper M, et al. Aspiration pneumonia after chemo-intensity-modulated radiation therapy of oropharyngeal carcinoma and its clinical and dysphagia-related predictors. Head Neck. (2014) 36:120–5. doi: 10.1002/hed.23275
70. Kawai S, Yokota T, Onozawa Y, Hamauchi S, Fukutomi A, Ogawa H, et al. Risk factors for aspiration pneumonia after definitive chemoradiotherapy or bio-radiotherapy for locally advanced head and neck cancer: a monocentric case control study. BMC Cancer. (2017) 17:59. doi: 10.1186/s12885-017-3052-8
71. Madan R, Kairo AK, Sharma A, Roy S, Singh S, Singh L, et al. Aspiration pneumonia related deaths in head and neck cancer patients: a retrospective analysis of risk factors from a tertiary care centre in North India. J Laryngol Otol. (2015) 129:710–4. doi: 10.1017/S0022215115001450
Keywords: head and neck cancer, late radiation, function, dysphagia, aspiration, voice, assessment, screening
Citation: Patterson JM (2019) Late Effects of Organ Preservation Treatment on Swallowing and Voice; Presentation, Assessment, and Screening. Front. Oncol. 9:401. doi: 10.3389/fonc.2019.00401
Received: 30 January 2019; Accepted: 29 April 2019;
Published: 21 May 2019.
Edited by:
Andreas Dietz, Leipzig University, GermanyReviewed by:
Susanne Wiegand, Leipzig University, GermanyChristiane Hey, Goethe-Universität Frankfurt, Germany
Copyright © 2019 Patterson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: J. M. Patterson, am9hbm5lLnBhdHRlcnNvbkBuY2wuYWMudWs=
 J. M. Patterson
J. M. Patterson