- 1Department of Neurology, Stroke Center, The First Hospital of Jilin University, Changchun, China
- 2Department of Neurology, Clinical Trial and Research Center for Stroke, The First Hospital of Jilin University, Changchun, China
Objectives: Stroke burden is especially heavy in northeast China. Facilities with the capacity to perform acute reperfusion therapies for stroke are unevenly dispersed and are especially inadequate in rural areas. The aim of this study was to establish an effective measure to improve stroke emergency care, eventually increasing the capacity for reperfusion therapy in Jilin province, a less developed province in northeast China.
Methods: We created the Jilin province Stroke Emergency Maps (JSEM), a regional stroke emergency network. Qualified hospitals in Jilin province were integrated into JSEM according to strict inclusion criteria. With constant evaluation and screening, more qualified hospitals may be enrolled into the JSEM, which is updated and published once per year. Locations of hospitals with the capacity to perform intravenous thrombolysis and emergency mechanical thrombectomy were labeled on the map.
Results: After strict evaluation and screening, 19 designated hospitals were integrated into the JSEM in August 2017 (baseline). Following the implementation of the JSEM, 21 more designated hospitals (40 in all) were included in 2018, and 48 more designated hospitals were included in 2019. With the guidance of the JSEM, the rate of intravenous thrombolysis in Jilin province increased remarkably from 3.3% (2017, baseline) and 4.6% (2018) to 5.5% (2019). Mean door-to-needle time decreased from 62 min at baseline (2017) to 45 min 2 years later. The number of mechanical thrombectomy was increased from 457 at baseline (2017) to 749 (2018) and 1,137 (2019) per year, respectively, and mean door-to-puncture time was shortened from 136 to 120 min.
Conclusion: The JSEM, a regional stroke emergency network, serves to improve patient care for stroke. The map's publication increased rates of intravenous thrombolysis and mechanical thrombectomy. JSEM effectively connected more qualified designated hospitals, stroke patients and emergency medical service systems in Jilin province.
Introduction
Effective treatments for acute ischemic stroke rely on timely restoration of blood flow for brain tissue. Currently, <3% of patients with ischemic stroke in China receive intravenous thrombolysis (1). The availability of hospitals with the capacity to perform acute reperfusion therapies for stroke patients is unevenly dispersed and is especially inadequate in rural areas (2). There is a population of nearly 27 million in the Jilin province, Northeast China, and a large portion of the populations is dispersed in rural areas that lack high-quality medical resources. It is assumed that the rate of stroke patients in Jilin province who receive emergency treatment within time window is much lower than average (3).
The Chinese government has instituted substantial strategies to reduce the burden of stroke. With the support of the Stroke Prevention Project Committee of the Chinese National Health Commission, The China Acute Stroke Care Mapping Steering Committee was established and Acute Stroke Care Maps have been implemented in more than 40 Chinese cities. Those maps integrate prehospital emergency medical service (EMS) systems and in-hospital strategies to provide improved pathways for Chinese acute ischemic stroke patients. In an effort to provide guidance to hospitals, EMS systems and residents in Jilin province, we established an effective measure, the Jilin province Stroke Emergency Maps (JSEM), the first province-wide stroke emergency map in China, to improve stroke emergency care. The purposes of this article are to present the designation, implementation, refinement, and improvement process of JSEM. We aim to eventually increase the capacity of reperfusion therapy after stroke, meet the needs of stroke patients, hospitals, and the EMS system in Jilin province.
Materials and Methods
Study Design
This is a retrospective observational study comparing the rates of intravenous thrombolysis and mechanical thrombectomy as well as EMS system response time in Jilin province using data 1 year before (Aug 2016–July 2017), 1 year after (Aug 2017–July 2018) and 2 years after (Aug 2018–July 2019) JSEM project initiation. The study was approved by the ethics committee of the First Hospital of Jilin University.
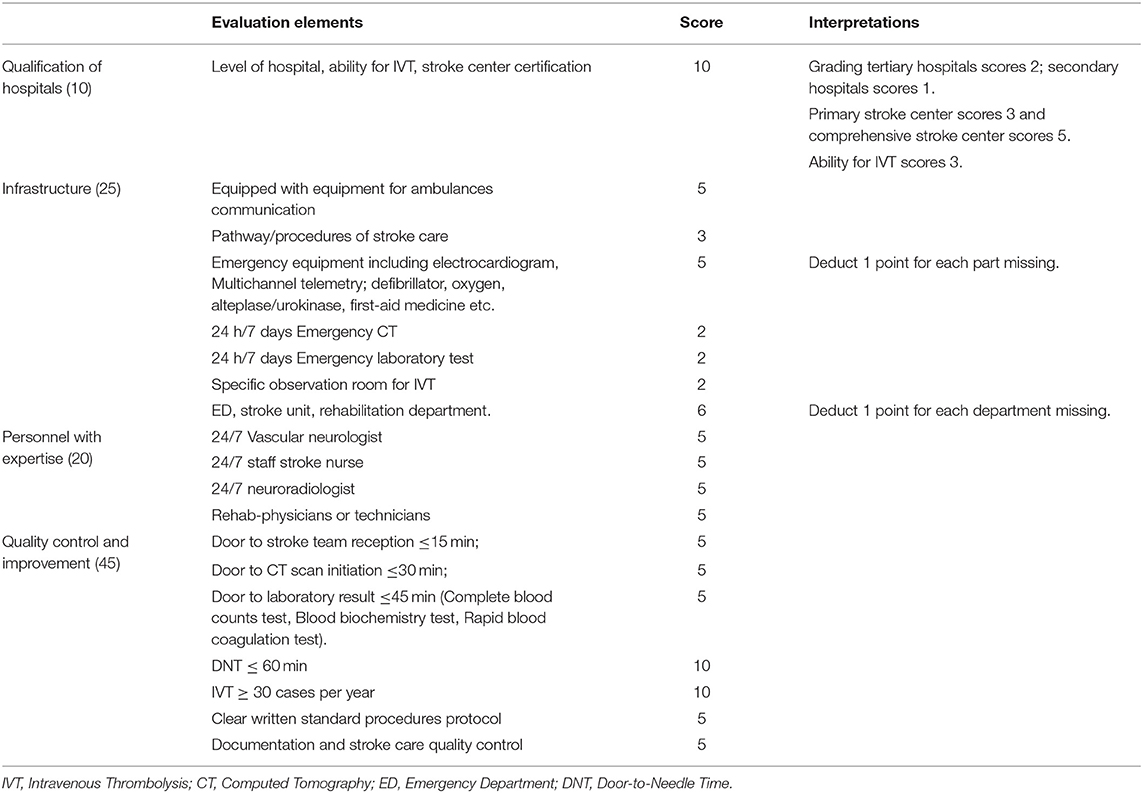
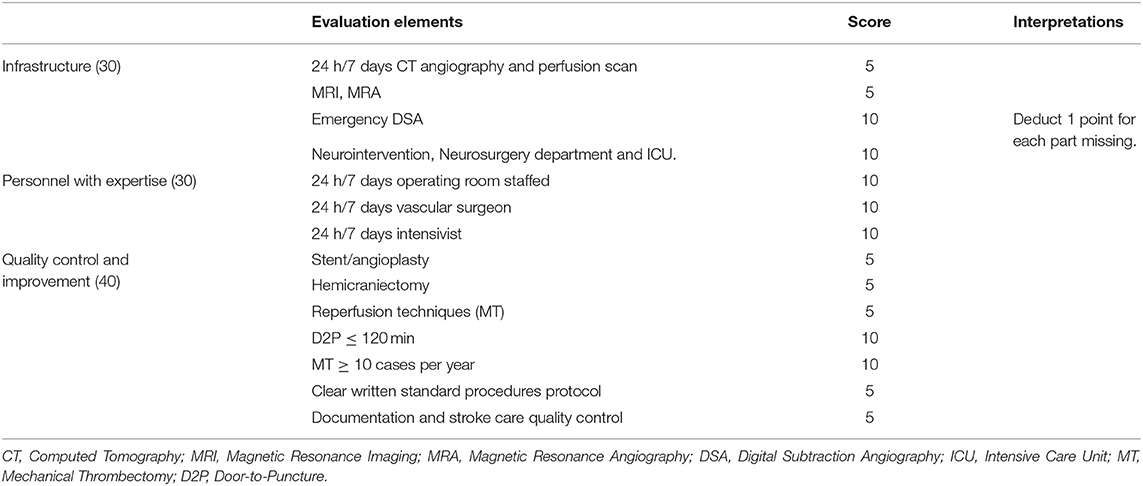
Certification for JSEM
JSEM is a regional stroke emergency network. This project has been sponsored by the Jilin Province Health Ministry and implemented by the Jilin Stroke association and Jilin Stroke Care Quality Management Center since 2017. Jilin Stroke Committee of Experts was established to develop certification criteria of JSEM. The key components of qualified hospital for JSEM can be defined in 4 major areas revised and refined from recommendations for Primary Stroke Center (4) and Comprehensive Stroke Center (5, 6): (1) Qualification of hospitals; (2) Infrastructure; (3) Personnel with expertise; and (4) Quality control and improvement (Tables 1, 2). In addition, JSEM creatively developed two settings of certification criteria especially for screening hospitals qualified for intravenous thrombolysis and emergency mechanical thrombectomy according to 2018 AHA/ASA Guidelines (7). Qualified local hospitals that successfully met the certification criteria were awarded certification and integrated into JSEM. This strategy provided precise guidance for EMS systems to rapidly transfer patients with acute ischemic stroke to a properly qualified hospital.
Stroke Identification
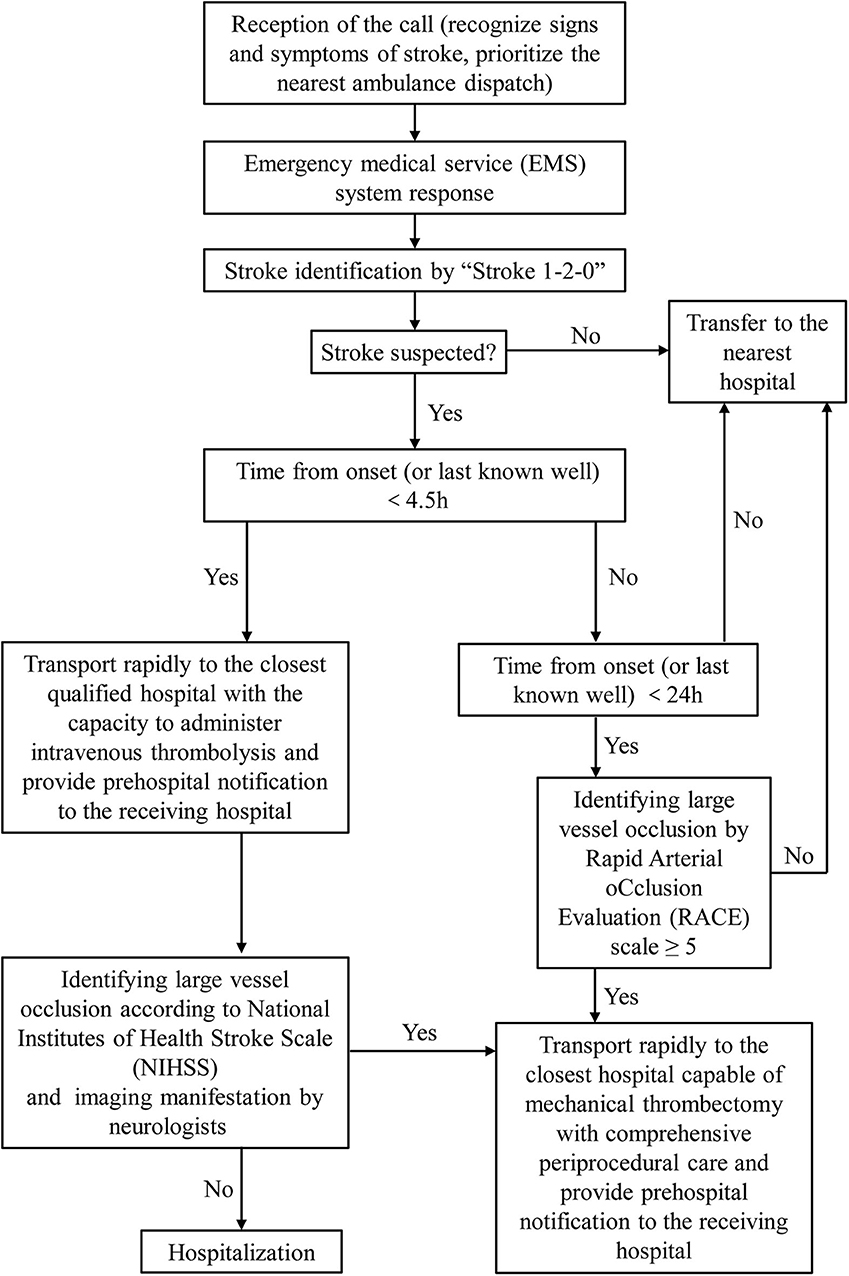
EMS system staff identifies patients with suspected stroke according to “Stroke 1-2-0” (8) and recognizes patients for whom a suspicion of large vessel occlusion is strong by Rapid Arterial oCclusion Evaluation (RACE) scale ≥ 5 (9). Jilin Stroke Committee of Experts provided the training of these two prediction instruments and prehospital management of patients with acute ischemic stroke for EMS staff to ensure rapid and effective transport.
Triage Paradigms of JSEM
Once the patient was suspected of stroke, EMS staff initiates operating procedures in accordance to JSEM transfer protocol (Figure 1). They should transport patients rapidly to the closest qualified hospital with the capacity to administer intravenous thrombolysis and provide prehospital notification to the receiving hospital to ensure earliest emergency department arrival. Quicker emergency department evaluation and rapid intravenous thrombolysis treatment to increase positive patient outcomes are needed. If the time from onset (or last known well) ≥ 4.5 h and the patient was under suspicion of large vessel occlusion, the patient should be transported rapidly to the closest hospital capable of endovascular stroke treatment with comprehensive periprocedural care. Meanwhile, EMS staff must consider the decision of patient and patient family members about which hospital they want to be transported to, avoiding unethical driving behaviors. Finally, neurologists in qualified hospitals decided the treatments according to the latest guidelines after communication with patient and patient family members.
Training and Update for JSEM
Constant JSEM quality improvement initiatives are required. Regular trainings are provided by the committee of expertise of JSEM. These trainings ensure that the EMS staff recognizes stroke symptoms more precisely, the ambulances are dispatched more rapidly, emergency department staff react more efficiently, and stroke teams determine the appropriate therapeutic schedule more safely. Training programs are conducted every 3 months.
Jilin Stroke Care Quality Management Center is in charge of JSEM quality control. Multiple elements of stroke care quality benchmarks include the number of stroke patients who received intravenous thrombolysis or mechanical thrombectomy, mean door-to-needle time, mean door-to-puncture time, etc. All qualified hospitals are required to collect and submit their corresponding data quarterly. JSEM were updated and published once per year based on the quality control data.
Results
Implementation and Update of the JSEM
Jilin province covers an area of 73,000 square miles and contains eight prefecture-level cities (Changchun, Baicheng, Baishan; Jilin City; Liaoyuan; Siping; Songyuan and Tonghua) and one autonomous prefecture (Yanbian). With strict evaluation and screening, the 1st version of JSEM was released in August 2017 (baseline). Nineteen designated hospitals capable for intravenous thrombolysis were integrated into the 1st map, among which only 10 hospitals are qualified for mechanical thrombectomy (Figures 2A,D,E). There were no qualified hospitals in two cities (Baishan, Baicheng) and Yanbian Korean autonomous prefecture on the 1st version of JSEM. Following 1 year of development, 21 more hospitals (40 in all) were designated as qualified to perform intravenous thrombolysis on July 2018. The number of hospitals capable of mechanical thrombectomy increased to 17 (Figures 2B,D,E). All the cities and prefectures were covered. In August 2019, 8 more hospitals were incorporated, and 22 hospitals were capable of performing mechanical thrombectomy (Figures 2C–E).
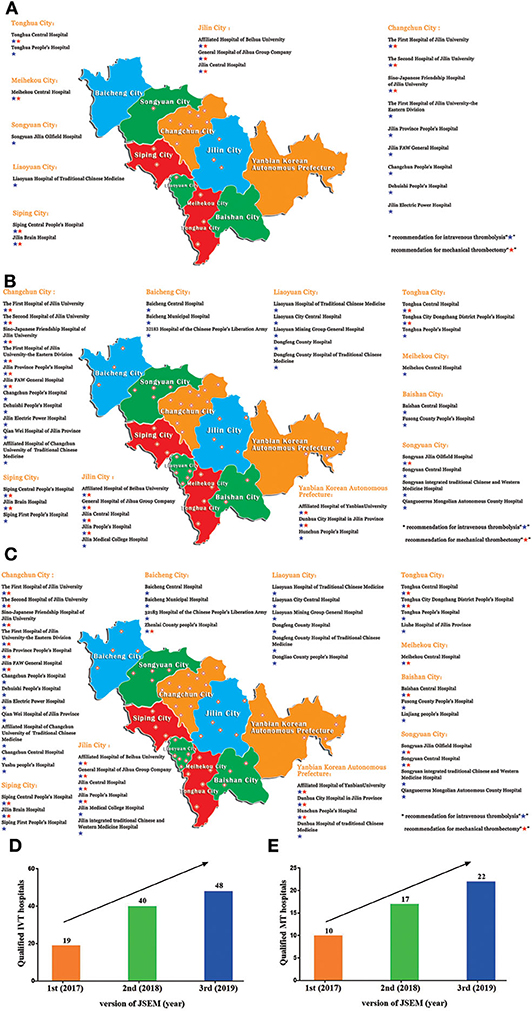
Figure 2. The (A) 1st, (B) 2nd, and (C) 3rd version of JSEM. The number of qualified (D) intravenous thrombolysis (IVT) and (E) mechanical thrombectomy (MT) hospitals was increased after the publication of JSEM.
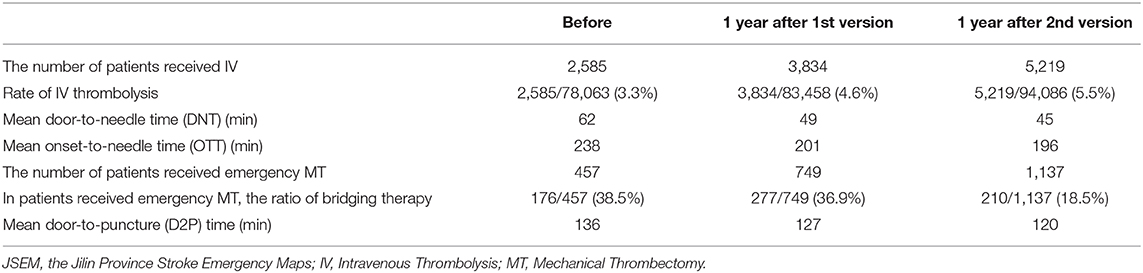
Increasing Capacity of Intravenous Thrombolysis After JSEM Implementation
With the increasing number of designated hospitals in the JSEM capable of performing intravenous thrombolysis, the number of patients who received intravenous thrombolysis increased remarkably from 2,585 1 year (Aug 2016–July 2017) prior to JSEM project initiation, 3,834 per year (Aug 2017–July 2018), to 5,219 (Aug 2018–July 2019). The rate of intravenous thrombolysis increased correspondingly from 3.31% (2,585/78,063) at baseline JSEM, 4.59% (3,834/83,458) 1 year later to 5.5% (5,219/94,086) 2 years later. Mean door-to-needle time and mean onset-to-needle time was shortened from 62 and 238 min at baseline JSEM, 49 and 201 min after 1 year, to 45 and 196 min after 2 years, respectively (Table 3).
Increasing Capacity of Mechanical Thrombectomy After JSEM Implementation
Due to the regular trainings provided by the JSEM committee, the hospitals met the mechanical thrombectomy qualification increased. Concomitantly, the number of patients who received emergency mechanical thrombectomy in Jilin province increased from 457 per year at baseline JSEM to 749 1 year later, 1,137 2 years later, and mean door-to-puncture time was reduced from 136 to 120 min. Among patients who received emergency mechanical thrombectomy, the ratio of bridging therapy was decreased year after year, from 38.5% (176/457) at baseline JSEM, 36.9% (277/749) 1 year later to 18.5% (210/1137) 2 years later (Table 3).
Discussion
The JSEM was successful in increasing the number of qualified hospitals and patients who received intravenous thrombolysis and mechanical thrombectomy, and decreasing mean onset-to-needle, door-to-needle, and door-to-puncture times. More importantly, JSEM improved the overall acute stroke care level of Jilin province and strengthened the connection between hospitals, stroke patients, and EMS systems, which should be implemented in other provinces, especially less developed provinces in China, to aid in reducing stroke morbidity and mortality.
Stroke is one of the leading causes of death and disability at the national level in China. The National Epidemiological Survey of Stroke in China reported that the age-standardized stroke prevalence was 1,115 cases per 100,000 people, and mortality was 115 cases per 100,000. The highest incidence and mortality of stroke was in the Northeast region (365.2/100,000 person-years and 158.5/100,000 person-years, respectively) (10). Jilin province is located in Northeast China, which has borders with Russia and North Korea. It encompasses an area of 190,000 square km and the population is around 27 million. It is a less developed province in China; its age-standardized years of life lost (2,100 vs. 2,000 per 100,000 population) and disability-adjusted life-years (1.52 vs. 1.33 per 100,000 population) of stroke were significantly higher than the national averages (11).
The Role and Benefit of JSEM
To the best of our knowledge, JSEM is the first province-wide stroke emergency map in China. Prior to establishment of the JSEM, several city-wide stroke emergency maps have been published in Shenzhen city (12), Shenyang city, and Qingdao city. These cities are densely populated and evenly distributed and located in developed areas with adequate medical resources. However, Jilin is a less developed province and most of the population is dispersed in rural areas that lack high-quality medical resources. If the map covered only Changchun city, the capital of Jilin province, most residents of our province would not benefit. JSEM demonstrated all the locations of qualified hospitals certified by the Jilin Province Health Ministry. We creatively labeled the recommendation for intravenous thrombolysis and emergency mechanical thrombectomy for each hospital on this map, which can assist hospitals and EMS system so that stroke patients in Jilin Province receive timely care that is most appropriate for their clinical condition. Moreover, after multifaceted quality improvement intervention organized by the JSEM committee, for example, sending doctors in rural areas to qualified hospitals for further study and providing regular guidance to unqualified hospitals, more and more hospitals met the intravenous thrombolysis and mechanical thrombectomy qualification and was integrated into JSEM. The baseline JSEM did not cover all the cities and prefecture, and regional distribution of qualified hospitals was extremely uneven, for instance, most are located in urban areas; however, more than two-thirds are located in the central part of Jilin province (Changchun, Jilin city, Liaoyuan, and Siping). On the contrary, there was no qualified hospital in Yanbian Korean autonomous prefecture, a mountainous country. Although sparsely populated (2.1 million), it makes up around one fourth of Jilin's land area. There may not be a stroke center located nearby for local patients in this region, which is inadequate for emergency stroke care. With the development of JSEM, there are now four identified qualified hospitals are capable of providing intravenous thrombolysis and three of them meet all of the requirements for emergency mechanical thrombectomy in Yanbian Korean autonomous prefecture 2 years later.
The implementation of JSEM was also successful according to the increased rate of intravenous thrombolysis and decreased onset-to-needle time, reflecting the transportation of patients is more effective. Traditional Chinese thought considers large scale comprehensive hospitals to be more reliable, thus, a large portion of acute ischemic stroke patients may choose a comprehensive hospital despite the long distance rather than the nearest one. As a result, they may miss the critical time window for optimal stroke treatment. Under the guidance of JSEM, traditional stereotypes are broken and more eligible patients with acute ischemic stroke can be transported to the nearest qualified hospitals within the appropriate time window. Door-to-needle time decreased, likely due to prehospital hospital notification and unobstructed in-hospital work-flow as a result of the regular trainings provided by the JSEM committee.
The total number of patients who received emergency mechanical thrombectomy increased rapidly, partly due to our JSEM with the recommendation of mechanical thrombectomy. Alternatively, this may also be due to the extension of the endovascular thrombectomy time window (13, 14). Specifically, among patients who received emergency mechanical thrombectomy, the ratio of bridging therapy was decreased each year, which indicates that the number of patients who received direct thrombectomy increased actually. Interestingly, number of patients receiving bridging therapy decreased 2 years later comparing with 1 year after JESM publication. In recent years, it is controversial whether acute ischemic stroke patients with large vessel occlusion who are eligible for both intravenous thrombolysis and mechanical thrombectomy benefit from pretreatment with alteplase or not. Interventional neurologists in hospitals with both intravenous thrombolysis and mechanical thrombectomy qualifications may choose direct mechanical thrombectomy other than bridging therapy in some conditions (for example, patients with atrial fibrillation or older patients) considering that thrombolysis prior to intra-arterial trombectomy might increase the incidence of symptomatic intracerebral hemorrhage, limit additional procedures during mechanical thrombectomy, such as administration of antiplatelet, cause thrombus fragility and thrombus migration and so on (15). This phenomenon is becoming increasingly common in China and may lead to the decrease in the number of bridge therapy. With the enhancement of acute ischemic stroke therapy education for the public and the increased number of recommended hospitals for emergency mechanical thrombectomy, the patients who receive direct thrombectomy is expected to further increase.
Overall, the success of the JSEM indicates that similar emergency maps should be implemented by other provinces, especially less developed provinces in China to further reduce stroke morbidity and mortality. The implementation of this emergency map not only helped to establish the prehospital emergency network to shorten transportation time and prompt the formation of stroke centers in some rural areas but also can improve awareness of stroke among the public to strengthen compliance with primary and secondary prevention methods.
Limitation
There are also some limitations in this study. First, the increasing incidence of stroke in China year by year would also have an impact on the results, however, the rates of intravenous thrombolysis may partly overcome the influence of stroke incidence comparing with the number of intravenous thrombolysis. Mean door-to-needle time, mean onset-to-needle time and mean door-to-puncture may not be impacted by stroke incidence. Second, we did not carry out quality control assessments of the staff of EMS at present, so we do not have data for EMS and the accuracy of stroke identifications by EMS staff of JSEM could not be analyzed.
Perspective
To further improve JSEM quality control, several initiatives are needed as follows: First, the number of patients transported by EMS did not increased thus far, possibly because public awareness of stroke symptoms and treatment remains poor in Jilin province. A study from three cities in China indicated that only 18.8% of the patients used the EMS (16). Therefore, public stroke education should emphasize the importance of the therapeutic time window. Second, in terms of EMS staff, one study demonstrated that nearly one-third of stroke cases were not identified by ambulance doctors (16). Previous studies demonstrate that the use of prehospital tools, such as the Face Arm Speech Time (FAST) test and Cincinnati Prehospital Stroke Scale (CPSS) to screen for stroke can improve stroke identification (17, 18). Furthermore, “stroke 1-2-0” are used widely in China (8). Alternatively, the newest guidelines call for large vessel occlusion identification ability (19). However, currently, no scale predicts large vessel occlusion with both high sensitivity and high specificity (19, 20). As a frequently validated large vessel occlusion prediction instrument, the sensitivities and specificities of the Cincinnati Prehospital Stroke Severity Scale (CPSSS) ≥ 2 for suspected stroke patients ranged from 56 to 58% and 77 to 85%, respectively (20, 21). Furthermore, CPSSS was user-friendlier than RACE scale. EMS staff, the most important part of prehospital procedures, could be provided with exhaustive “stroke 1-2-0,” FAST test, CPSS, and CPSSS training to improve stroke identification. Third, recently, telestroke has been proven to be one of the most successful applications of telemedicine (22). A systematic review and meta-analysis indicates that intravenous alteplase eligibility decision through telestroke networks is safe and effective within the 3-h time window (23). It seems that telestroke is suitable for Jilin province. Stroke centers in cities, such as Changchun can provide remote guidance to urban centers to ensure the best interests of stroke patients in remote areas are met. Further, telemedicine may help identify patients who are suspected with large vessel occlusion, while primarily admitted to only thrombolysis-capable hospitals (12). These will be the next direction in the informatization.
Conclusion
In summary, this study described the key components of JSEM, the first province-wide stroke emergency map in China, including its certification, triage paradigms, and training and update. The publication of JSEM not only integrated more intravenous thrombolysis and mechanical thrombectomy qualified hospitals, but also significantly increased the rates of intravenous thrombolysis and mechanical thrombectomy and decreased onset-to-needle, door-to-needle, and door-to-puncture times in a less developed province of China.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Human and Research Ethics committees of the First Hospital of Jilin University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
YY and Z-NG devised the study design and supervised study procedures. HJ, YQ, and X-LY analyzed the data and wrote the manuscript. XS collected the data. All authors provided critical review, edits, and approval of the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (81971109) to HJ.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Jin H, Zhu S, Wei JW, Wang J, Liu M, Wu Y, et al. Factors associated with prehospital delays in the presentation of acute stroke in urban China. Stroke. (2012) 43:362–70. doi: 10.1161/STROKEAHA.111.623512
2. Wu S, Wu B, Liu M, Chen Z, Wang W, Anderson CS, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. (2019) 18:394–405.
3. Wand LD, Liu JM, Yang Y, Peng B, Wang YL. The prevention and treatment of stroke still face huge challenges—brief report on stroke prevention and treatment in China, 2018. Chin Circ J. (2019) 34:105–19.
4. Alberts MJ, Hademenos G, Latchaw RE, Jagoda A, Marler JR, Mayberg MR, et al. Recommendations for the establishment of primary stroke centers. Brain attack coalition. JAMA. (2000) 283:3102–9. doi: 10.1001/jama.283.23.3102
5. Alberts MJ, Latchaw RE, Jagoda A, Wechsler LR, Crocco T, George MG, et al. Revised and updated recommendations for the establishment of primary stroke centers: a summary statement from the brain attack coalition. Stroke. (2011) 42:2651–65. doi: 10.1161/STROKEAHA.111.615336
6. Alberts MJ, Latchaw RE, Selman WR, Shephard T, Hadley MN, Brass LM, et al. Recommendations for comprehensive stroke centers: a consensus statement from the Brain Attack Coalition. Stroke. (2005) 36:1597–616. doi: 10.1161/01.STR.0000170622.07210.b4
7. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2018) 49:e46–110. doi: 10.1016/j.jvs.2018.04.007
8. Zhao J, Liu R. Stroke 1-2-0: a rapid response programme for stroke in China. Lancet Neurol. (2017) 16:27–8. doi: 10.1016/S1474-4422(16)30283-6
9. Carrera D, Campbell BC, Cortes J, Gorchs M, Querol M, Jimenez X, et al. Predictive value of modifications of the prehospital rapid arterial occlusion evaluation scale for large vessel occlusion in patients with acute stroke. J Stroke Cerebrovasc Dis. (2017) 26:74–7. doi: 10.1016/j.jstrokecerebrovasdis.2016.08.032
10. Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480,687 adults. Circulation. (2017) 135:759–71. doi: 10.1161/CIRCULATIONAHA.116.025250
11. Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
12. Ye S, Hu S, Lei Z, Li Z, Li W, Sui Y, et al. Shenzhen stroke emergency map improves access to rt-PA for patients with acute ischaemic stroke. Stroke Vasc Neurol. (2019) 4:115–22. doi: 10.1136/svn-2018-000212
13. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. (2018) 378:708–18. doi: 10.1056/NEJMoa1713973
14. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. (2018) 378:11–21.
15. Fischer U, Kaesmacher J, Mendes Pereira V, Chapot R, Siddiqui AH, Froehler MT, et al. Direct mechanical thrombectomy versus combined intravenous and mechanical thrombectomy in large-artery anterior circulation stroke: a topical review. Stroke. (2017) 48:2912–8. doi: 10.1161/STROKEAHA.117.017208
16. Jiang B, Ru X, Sun H, Liu H, Sun D, Liu Y, et al. Pre-hospital delay and its associated factors in first-ever stroke registered in communities from three cities in China. Sci Rep. (2016) 6:29795. doi: 10.1038/srep29795
17. De Luca A, Giorgi Rossi P, Villa GF, Stroke group Italian Society pre hospital emergency S. The use of Cincinnati prehospital stroke scale during telephone dispatch interview increases the accuracy in identifying stroke and transient ischemic attack symptoms. BMC Health Serv Res. (2013) 13:513. doi: 10.1186/1472-6963-13-513
18. Berglund A, Svensson L, Wahlgren N, von Euler M, collaborators H. Face arm speech time test use in the prehospital setting, better in the ambulance than in the emergency medical communication center. Cerebrovasc Dis. (2014) 37:212–6. doi: 10.1159/000358116
19. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019. Update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2019) 50:211. doi: 10.1161/STR.0000000000000211
20. Smith EE, Kent DM, Bulsara KR, Leung LY, Lichtman JH, Reeves MJ, et al. Accuracy of prediction instruments for diagnosing large vessel occlusion in individuals with suspected stroke: a systematic review for the 2018 guidelines for the early management of patients with acute ischemic stroke. Stroke. (2018) 49:e111–22. doi: 10.1161/STR.0000000000000160
21. Lima FO, Silva GS, Furie KL, Frankel MR, Lev MH, Camargo EC, et al. Field assessment stroke triage for emergency destination: a simple and accurate prehospital scale to detect large vessel occlusion strokes. Stroke. (2016) 47:1997–2002. doi: 10.1161/STROKEAHA.116.013301
22. Wechsler LR, Demaerschalk BM, Schwamm LH, Adeoye OM, Audebert HJ, Fanale CV, et al. Telemedicine quality and outcomes in stroke: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2017) 48:e3–25. doi: 10.1161/STR.0000000000000114
Keywords: acute stroke, thrombolysis, prehospital delay, ischemic stroke, stroke care
Citation: Jin H, Qu Y, Guo Z-N, Yan X-L, Sun X and Yang Y (2020) Impact of Jilin Province Stroke Emergency Maps on Acute Stroke Care Improvement in Northeast China. Front. Neurol. 11:734. doi: 10.3389/fneur.2020.00734
Received: 27 March 2020; Accepted: 15 June 2020;
Published: 22 July 2020.
Edited by:
Jean-Marc Olivot, Centre Hospitalier Universitaire de Toulouse, FranceReviewed by:
Mohammad Anadani, Washington University School of Medicine in St. Louis, United StatesLijie Ren, Shenzhen Second People's Hospital, China
Copyright © 2020 Jin, Qu, Guo, Yan, Sun and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi Yang, ZG9jdG9yeWFuZ3lpQDE2My5jb20=
†These authors have contributed equally to this work
 Hang Jin
Hang Jin Yang Qu
Yang Qu Zhen-Ni Guo
Zhen-Ni Guo Xiu-Li Yan1
Xiu-Li Yan1 Yi Yang
Yi Yang