- 1Stroke Unit, Monash Health, Melbourne, VIC, Australia
- 2Stroke and Aging Research Group, Medicine, School of Clinical Sciences, Monash University, Melbourne, VIC, Australia
- 3Department of Medicine, Frankston Hospital, Peninsula Health, Melbourne, VIC, Australia
- 4Central Clinical School, Monash University, Melbourne, VIC, Australia
- 5Developmental Imaging, Murdoch Children Research Institute, Melbourne, VIC, Australia
Background and purpose: The recent advances in stroke therapy have placed focus on delivering care within the first hour after stroke onset (golden hour), principally through the use of Mobile Stroke Unit (MSU) to bring the hospital to the patient. The aim of this project is to search the location of MSU hub in Sydney, Australia, optimizing for catchment, transport to nearest thrombolysis and endovascular clot retrieval (ECR)/thrombectomy capable hospital and population at risk.
Methods: Traveling time was performed using ggmap package in R to interface with Google Maps application program interface (API). This analysis estimates the travel time from the centroids of each suburbs to five potential MSU hubs (Royal Prince Alfred, Prince of Wales, Royal North Shore, Liverpool, and Westmead hospitals) and eight thrombolysis capable hospitals. It is proposed that the MSU should be deployed at ECR hub to cover the suburbs, not well-covered by thrombolysis and ECR capable hospitals. This step was performed by assigning membership to hospitals within 30 min traveling time to the ECR hub. The base hub of the MSU was proposed as the closest hub (providing ECR) to the least well-served suburbs. The population serviceable by MSU was estimated using stroke incidence studies in Melbourne and Adelaide.
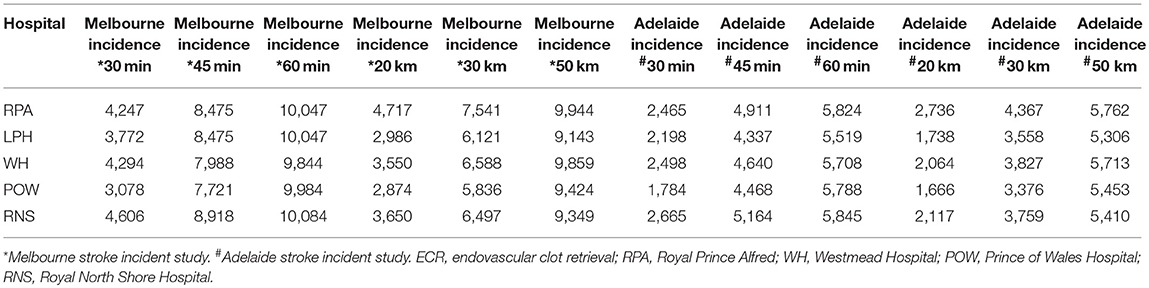
Results: The largest population, serviceable by MSU within 30 min (4,606 cases), 45 min radius (8,918 cases), and 60 min (10,084 cases), was Royal North Shore followed by Royal Prince Alfred, Liverpool, Westmead, and Prince of Wales hospitals. Prince of Wales hospital has the smallest catchment within 30 min (3,078 cases), 45 min (7,721 cases), and 60 min (9,984 cases). Suburbs at the edge of metropolitan Sydney such as the Northern Suburbs are less well-served by thrombolysis and ECR capable hospitals. There are 10 suburbs within 30 min travel of one hospital. The remainders are within 30 min of two or more hospitals.
Conclusions: Any of the five endovascular clot retrieval capable hospitals are capable of serving as a hub for MSU. We provide a method to identify the hub based on location of suburbs less well-served by other hospital.
Introduction
The recent advances in stroke therapy have placed focus on delivering care within the first hour after stroke onset (golden hour) (1). A potential solution is the use of Mobile Stroke Unit (MSU) to bring the hospital to the patient for providing thrombolysis. Since the publications of the endovascular clot retrieval hospital (ECR)/thrombectomy trials in 2015 (2–7), a new indication for MSU is to triage transportation of patients to the appropriate hospital for ECR. The first randomized trial in 2012 showed an absolute difference of 16 min (8); this had occurred in the context of the MSU operating only a short range from base (8). Subsequent publications showed a difference of 39 min in time to thrombolysis (9). The MSU is a modified ambulance, which sometimes approaches the size of a truck. It is equipped with CT scanner and a mobile pathology laboratory and staffed by ambulance officer, nurse, radiographer, and in some places, doctor. There is strong interest in developing this platform and a model currently exist in Melbourne, Australia's second largest city.
There are several models for operating MSU around the world (1). In one model, MSU is located in a central location in a fire station and travel up to 16 min from base (10). A health economic analysis in Germany suggested MSU can provide service up to 30 km radius from base (11). The model in Edmonton, Canada provides service in rural Alberta up to a radius of 250 km2 (12). The varying operating radii of MSU suggest that its deployment has not been formally evaluated. In the Australian context, the Melbourne model operates MSU from a centrally located major hospital, Royal Melbourne Hospital, and travel a 20 km radius from 8 a.m. to 6 p.m. (13). This model had occurred at Royal Melbourne Hospital and was nominated as the first designated ECR hub in Melbourne (14). Subsequently, a geospatial optimization analysis suggested that such a model can operate up to 76 min from base (15). In another paper, in this special issue of Frontiers in Neurology, the role of MSU in performing triaging of patients for therapy in the rural setting was explored (16). In this study, we propose the use of ggmap interface to Google Maps API to assign the base for operating MSU in Sydney based on proximity of the hub to the suburbs less well-resourced in terms of closeness to hospitals providing ECR and thrombolysis (14). The optimization will be performed for catchment, transport to nearest thrombolysis-capable hospital, and population at risk of stroke. Sydney is the ideal site for this study, as the locations of the ECR hubs have not been finalized and all potential ECR hubs are eligible as the base (17).
Methods
Setting
Sydney is the capital city of the state of New South Wales, Australia with a population of ~5.1 million. The number of strokes has been estimated using the 2016 census data (1) for each age band and the stroke incidence study in Melbourne and Adelaide (18, 19). This study involves simulations (no patient data are used) and as such received a waiver from the Monash Health Human Research Ethics Committee.
ECR Capable Hospitals in Sydney
At present there is no official statewide protocol for ECR in Sydney (20). There are five hospitals (Royal Prince Alfred, Prince of Wales, Royal North Shore, Liverpool, and Westmead) capable of acting as ECR hubs. There is one ECR hub, located 159 km north of Sydney. Similar to the Melbourne model of basing the hub in a major teaching hospital, these hubs may serve as the base for MSU. In addition, there are eight hospitals providing thrombolysis service in metropolitan Sydney and eight outside of metropolitan Sydney (20).
Google Maps API
Estimation of ambulance travel times and potential hospital catchment were performed using the ggmap (21) (R Project for Statistical Computing, version 3.4.4) interface to the Google Maps Distance Matrix API. The transport time, from each hospital to each suburb centroid, was computed during peak morning traffic. Interactive web-based maps of the models were generated using leaflet (R package) with tiles from OpenStreetMap (OpenStreetMap contributors; for copyright, see www.openstreetmap.org/copyright) (22).
Optimization
We formulated the problem as a variant of the maximum coverage (23). In a traditional maximum coverage problem, the hospital sites are not yet determined and the optimization is performed to allocate the sites, which provide best coverage for the area. In this case, the hospitals have been built and each have their own capabilities such as thrombolysis capable or ECR capable. We propose that the MSU should be deployed to cover the suburbs, not well-covered by thrombolysis and ECR capable hospitals. This step was performed by assigning membership to hospitals within 30 min (24). From an equitable point, the suburbs, which have least memberships, were considered to be more likely to benefit from MSU compared to suburbs with multiple memberships (25). The base hub of the MSU was proposed as the closest hub to the least well-served suburbs.
In addition, we provide a sensitivity analysis by estimating the population at risk of stroke serviced by MSU. This analysis was done by extending the base from 30 to 60 min (24).
Results
The map (Figure 1) illustrates the suburbs, well-served by overlapping catchment of other hospitals. These are suburbs, located between the following Royal Prince Alfred, Westmead, Sydney Adventist, Bankstown, and St. George. Concord hospital is located at the center of these suburbs with overlapping catchment. By contrast, the suburbs at the edge of metropolitan Sydney such as the Northern Suburbs are less well-served by thrombolysis and ECR capable hospitals. On the map these Northern suburbs have values of one only, indicating that they are serviced by only 1 hospital. Figure 2 is a histogram of the suburbs and their 30 min proximity to a thrombolysis and ECR capable hospitals. Ten suburbs are within reach of one hospital within 30 min and 200 suburbs are within reach of two or more hospitals within 30 min. Thirty suburbs are within 30 min of one ECR capable hospital. One hundred and thirty-five suburbs are within 30 min of more than three ECR capable hospitals (Figure 3).
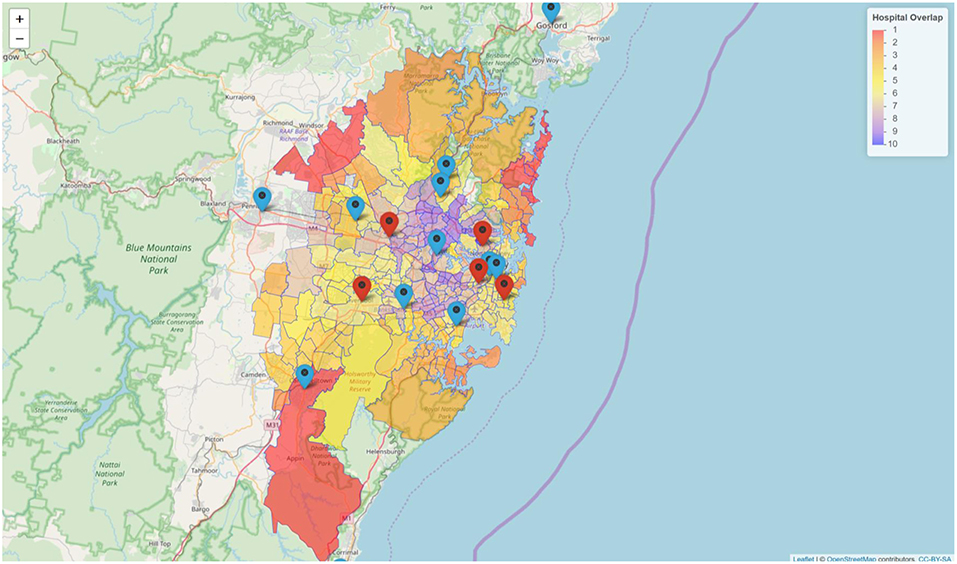
Figure 1. Coverage of suburbs by thrombolysis and clot retrieval hospitals. There are five ECR capable hospitals (red icons) and eight thrombolysis capable hospitals (blue icon) in metropolitan Sydney. The red color polygon indicates less overlap and the purple color indicates high number of overlap.
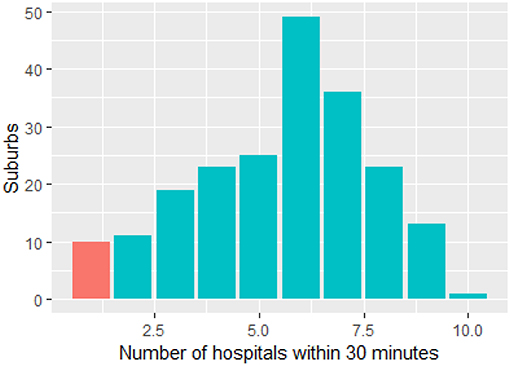
Figure 2. Relationship between suburbs and hospital coverage in Sydney. There are 10 suburbs within 30 min travel of one hospital (red). The remainders are within 30 min of two or more hospitals.
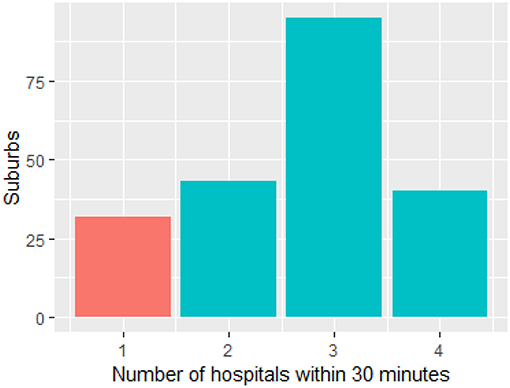
Figure 3. Relationship between number of suburbs and coverage by ECR capable hospitals. Thirty-two suburbs are within 30 min of one ECR capable hospital (red). ECR, endovascular clot retrieval.
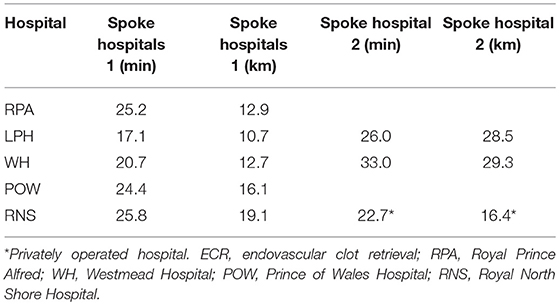
The largest population, serviceable by MSU within 30 min (4,606 cases), 45 min radius (8,918 cases), and 60 min (10,084 cases), was by Royal North Shore hospital followed by Royal Prince Alfred, Liverpool, Westmead, and Prince of Wales hospitals (Table 1). Prince of Wales hospital has the smallest catchment within 30 min (3,078 cases), 45 min (7,721 cases), and 60 min (9,984 cases). Within 60 min from hub, five sites differ by 140 cases. Three of the sites have two associated spokes hospitals (Table 2; Figure 1).
Discussion
In this study, we have used data driven method to map location of MSU base in Sydney using Google Maps API estimate of travel time from the ECR and thrombolysis capable hospitals. This issue arises as there are five ECR capable hospitals in Sydney; each has their merits of operating as a base for MSU. Using the idea of equity, an ECR hub was identified as the one that was closest to the suburbs, least served by ECR and thrombolysis capable hospitals. Our methodological approach is of use when planning to invest in MSU.
The use of geographical information systems for health service design is evolving since 2017 (14, 15, 26–30). In this study, we have accessed Google Maps API for traffic data due to our familiarity with this platform (14, 15, 26–30). Use of Google Maps API for this purpose has been done in Australia and North America (14, 15). Those planning similar studies in other part of world such as Republic of Korea (South Korea) would need to access to Daum, Naver, or VWorld Map API. In People's Republic of China, Baidu Map API is preferred to Google Maps API. These tools can be combined with ggmap or other tools discussed in this special issue of Frontiers in Neurology (Stroke). In the Republic of China (Taiwan), Google Maps API is available for travel time estimation.
The approach we have taken for evaluating MSU base in Sydney is different from that in Melbourne (15). The MSU base in Melbourne has already been chosen and stroke neurologists and nurses from Royal Melbourne Hospital form part of the crew for the MSU (30). The objective of the paper is to ascertain the range of the MSU in Melbourne as the original intention was to restrict its operation to just 20 km from base. Our approach shows that in Melbourne, MSU can operate as far as 76 min from base and would provide superior time with respect to administration of TPA (31). With the range of operation in mind, it is proposed that provision of MSU service to an area, well-served by multiple adjacent hospitals, would not be equitable. The alternative argument is that MSU provides a mean to reduce door-in to door-out time, even within these well-covered suburbs. The argument would be that even among suburbs, well-served by other hospitals, there is still the issue of door-in to door-out time, which can vary from 85 min in Rhode Island (32) to 106 min in Melbourne (31).
It is possible that the issue of deciding between thrombolysis and ECR capable hospitals and MSU in a well-service catchment has not been explored in detail, as some of the centers operating MSU have only one ECR hub and have a small catchment population. Sites such as Lucas County serves a population of 433,689 (33); New Jersey model serves a modest population of 460,000 (34); and the Cleveland model serves a population of 390,000 (35). In Germany, there is exploration on the deployment of MSU in rural areas (16). In Edmonton, Canada, there is extension of the operating radius as far as 250 km from base (12).
Similar to the Houston and Melbourne model of basing the MSU hub in a major public teaching hospital (36), the rationale for the use of major hospital is that a stroke neurologist or neurology trainee from that hospital participates in the team. This has been the case for the first 2 years in Houston (36). This approach is different from the original model in Berlin in which the base is in a centrally located fire station in Berlin. If the desire is to locate the base in a central location, then the choice would be Royal Prince Alfred hospital, which is closest to the center of Sydney. However, such a model would be less equitable, given the number of suburbs, serviced by other hospitals. A counter argument would be that the suburbs with service by multiple hospitals is that where people live with risk of stroke.
Projection of patients at risk of stroke is based on stroke incidence studies from Melbourne (on the East coast of Australia) and Adelaide (on the South Coast of Australia) (18, 19). The studies were performed 13 years apart with the latter study from Adelaide documenting a much lower stroke incidence. The improved stroke incidence can be due to different methodology or improved stroke prevention strategy. As such we have provided data on the estimated number of stroke cases using stroke incidence both studies.
A limitation of this study is that it is based on simulations and not observed cases of stroke. We had circumvented this by simulating stroke cases in the centroid of each suburb. This approach provides an average of the trip time. Another limitation in the proposal for MSU is the issue of cost effectiveness, which has not yet been done. Current studies are underway on cost effectiveness of analyses of MSU (37, 38). A critical issue for cost effectiveness is the requirement to demonstrate difference in primary outcome on disability; so far the trial confirmed reduction in time to give thrombolysis only (9). The findings with reduction in time to thrombolysis are consistent whether in Europe or North America (35). However, this study has not focused on clinical outcome. The flow chart from this study shows another issue while constructing the cost effectiveness analysis (35). Twenty eight of 100 patients, treated by MSU, did not have stroke and 30 were classified as possible acute ischemic stroke. A further 217 trips (out of total 317 trips) were canceled prior to MSU arrival in this Cleveland Clinic study (35).
Depending on the configuration of MSU, the cost has been estimated to be around US$750,000 to US$1,400,000. The running cost of operating MSU during office hour is estimated to be around US$1,000,000 (34). Recently, a group in Lucas County Ohio reported on their initial experience with operating MSU 24 h a day (33). Data on 24-h operation and cost effectiveness study such as these will help inform the need for MSU.
This study was not designed to address the issue of cost effectiveness or propose the purchase of MSU but rather to evaluate the location for deployment of MSU. In the process of performing these analyses, there were issues on clustering or proximity of hospitals with thrombolysis and ECR capability. There may be a need to allocate resources equitably from inner Sydney to outer Sydney while planning the location of MSU hub. This is an issue that is not unique to Australia but is also relevant in Europe (16) and Canada (12). In London, this had been addressed by reducing the number of hospitals providing thrombolysis service (24, 39). The model was designed in such a way that no Londoner should be more than 30 min away from a hyperacute stroke service (24). A recent analysis on the effect of centralizing and rationalizing of stroke service in two metropolitan cities in England shows that the changes result in improved outcome (length of stay and mortality) and are sustainable (40). These centralized stroke services are configured for thrombolytic therapy and works are underway to examine implementation of ECR (41). It is not clear if this process would result in further reduction in hospitals providing thrombolysis and ECR. Decisions on the number of ECR and thrombolysis capable hospitals serving Sydney would need to be made before deciding on base for MSU.
In summary, any of the ECR-capable hospital can serve as a hub for MSU. We provide a method to identify the hub based on location of suburbs less well-served by other hospital.
Data Availability
The datasets generated for this study are available on request to the corresponding author.
Author Contributions
TP: design, analysis, and writing the manuscript. RB, VS, and HM: writing the manuscript.
Funding
VS was the recipient of a National Health and Medical Research Foundation of Australia/National Heart Foundation Career Development Fellowship.
Conflict of Interest Statement
TP is on the Advisory Board of Genzyme on Fabry Disease and has received payment for lectures including service on speakers' bureaus for Bayer, Boehringer Ingelheim, Pfizer, and Genzyme.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Figures provided are created using data OpenStreetMap contributors and tiles from osm.org. The data are available under the Open Database License while the tiles are available under Creative Commons Attribution-ShareAlike 2.0 license. Details are available at: www.openstreetmap.org/copyright. The maps are created using the OpenStreetMap tiles but do not suggest the licensor endorsing the use of this map.
References
1. Audebert H, Fassbender K, Hussain MS, Ebinger M, Turc G, Uchino K, et al. The pre-hospital stroke treatment organization. Int J Stroke. (2017) 12:932–40. doi: 10.1177/1747493017729268
2. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. (2015) 372:11–20. doi: 10.1056/NEJMoa1411587
3. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet. (2016) 387:1723–31. doi: 10.1016/S0140-6736(16)00163-X
4. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. (2015) 372:1019–30. doi: 10.1056/NEJMoa1414905
5. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. (2015) 372:2296–06. doi: 10.1056/NEJMoa1503780
6. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. (2015) 372:1009–18. doi: 10.1056/NEJMoa1414792
7. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-pa vs. T-pa alone in stroke. N Engl J Med. (2015) 372:2285–95. doi: 10.1056/NEJMoa1415061
8. Walter S, Kostopoulos P, Haass A, Keller I, Lesmeister M, Schlechtriemen T, et al. Diagnosis and treatment of patients with stroke in a mobile stroke unit versus in hospital: a randomised controlled trial. Lancet Neurol. (2012) 11:397–404. doi: 10.1016/S1474-4422(12)70057-1
9. Kunz A, Ebinger M, Geisler F, Rozanski M, Waldschmidt C, Weber JE, et al. Functional outcomes of pre-hospital thrombolysis in a mobile stroke treatment unit compared with conventional care: an observational registry study. Lancet Neurol. (2016) 15:1035–43. doi: 10.1016/S1474-4422(16)30129-6
10. Koch PM, Kunz A, Ebinger M, Geisler F, Rozanski M, Waldschmidt C, et al. Influence of distance to scene on time to thrombolysis in a specialized stroke ambulance. Stroke. (2016) 47:2136–40. doi: 10.1161/STROKEAHA.116.013057
11. Dietrich M, Walter S, Ragoschke-Schumm A, Helwig S, Levine S, Balucani C, et al. Is pre-hospital treatment of acute stroke too expensive? An economic evaluation based on the first trial. Cerebrovasc Dis. (2014) 38:457–63. doi: 10.1159/000371427
12. Shuaib A, Jeerakathil T. Alberta mobile stroke unit I. The mobile stroke unit and management of acute stroke in rural settings. CMAJ. (2018) 190:E855–8. doi: 10.1503/cmaj.170999
13. The Royal Melbourne Hospital is Proud to be a Major Partner and Host to the Melbourne Mobile Stroke Unit, the First of Its Kind in Australia (2018). Available online at: https://www.thermh.org.au/health-professionals/clinical-services/neurology/mobile-stroke-unit (accessed March 23, 2019).
14. Phan TG, Beare R, Chen J, Clissold B, Ly J, Singhal S, et al. Googling service boundaries for endovascular clot retrieval hub hospitals in a metropolitan setting: proof-of-concept study. Stroke. (2017) 48:1353–61. doi: 10.1161/STROKEAHA.116.015323
15. Phan TG, Beare R, Parsons M, Zhao H, Davis S, Donnan GA, et al. Googling boundaries for operating mobile stroke unit for stroke codes. Front Neurol. (2019) 10:331. doi: 10.3389/fneur.2019.00331
16. Mathur S, Walter S, Grunwald IQ, Helwig SA, Lesmeister M, Fassbender K. Improving pre-hospital stroke services in rural and underserved settings with mobile stroke units. Front Neurol. (2019) 10:159. doi: 10.3389/fneur.2019.00159
17. Hwang YT, Gawarikar Y. Clot retrieval and acute stroke care. Med J Aust. (2017) 207:361. doi: 10.5694/mja17.00526
18. Thrift AG, Dewey HM, Macdonell RA, McNeil JJ, Donnan GA. Stroke incidence on the east coast of Australia: The north east Melbourne stroke incidence study (nemesis). Stroke. (2000) 31:2087–92. doi: 10.1161/01.STR.31.9.2087
19. Leyden JM, Kleinig TJ, Newbury J, Castle S, Cranefield J, Anderson CS, et al. Adelaide stroke incidence study: declining stroke rates but many preventable cardioembolic strokes. Stroke. (2013) 44:1226–31. doi: 10.1161/STROKEAHA.113.675140
20. Innovation AfC. Stroke Network. (2019). Available online at: https://www.aci.health.nsw.gov.au/networks/stroke (accessed March 23, 2019).
21. Kahle D, Wickham H. Ggmap: spatial visualization with ggplot2. R J. (2013) 5:144–61. doi: 10.32614/RJ-2013-014
22. Cheng J, Xie Y, Wickham H, Agafonkin V. Leaflet: Create Interactive Web Maps With the Javascript ‘Leaflet’ Library. (2018). Available online at: https://cran.r-project.org/web/packages/leaflet/leaflet.pdf (accessed January 24, 2017).
23. Tierney NJ, Reinhold HJ, Mira A, Weiser M, Burkart R, Benvenuti C, et al. Novel relocation methods for automatic external defibrillator improve out-of-hospital cardiac arrest coverage under limited resources. Resuscitation. (2018) 125:83–9. doi: 10.1016/j.resuscitation.2018.01.055
24. Fulop N, Boaden R, Hunter R, McKevitt C, Morris S, Pursani N, et al. Innovations in major system reconfiguration in England: a study of the effectiveness, acceptability and processes of implementation of two models of stroke care. Implement Sci. (2013) 8:e5. doi: 10.1186/1748-5908-8-5
25. Smith EE, Schwamm LH. Endovascular clot retrieval therapy: implications for the organization of stroke systems of care in North America. Stroke. (2015) 46:1462–7. doi: 10.1161/STROKEAHA.115.008385
26. Milne MS, Holodinsky JK, Hill MD, Nygren A, Qiu C, Goyal M, et al. Drip ‘n ship versus mothership for endovascular treatment: Modeling the best transportation options for optimal outcomes. Stroke. (2017) 48:791–4. doi: 10.1161/STROKEAHA.116.015321
27. Holodinsky JK, Williamson TS, Kamal N, Mayank D, Hill MD, Goyal M. Drip and ship versus direct to comprehensive stroke center: Conditional probability modeling. Stroke. (2017) 48:233–8. doi: 10.1161/STROKEAHA.116.014306
28. Nogueira RG, Silva GS, Lima FO, Yeh YC, Fleming C, Branco D, et al. The fast-ed app: a smartphone platform for the field triage of patients with stroke. Stroke. (2017) 48:1278–84. doi: 10.1161/STROKEAHA.116.016026
29. Rhudy JP Jr, Alexandrov AW, Rike J, Bryndziar T, Hossein Zadeh Maleki A, Swatzell V, et al. Geospatial visualization of mobile stroke unit dispatches: a method to optimize service performance. Interv Neurol. (2018) 7:464–70. doi: 10.1159/000490581
30. Mullen MT, Pajerowski W, Messe SR, Mechem CC, Jia J, Abboud M, et al. Geographic modeling to quantify the impact of primary and comprehensive stroke center destination policies. Stroke. (2018) 49:1021–3. doi: 10.1161/STROKEAHA.118.020691
31. Ng FC, Low E, Andrew E, Smith K, Campbell BCV, Hand PJ, et al. Deconstruction of interhospital transfer workflow in large vessel occlusion: Real-world data in the thrombectomy era. Stroke. (2017) 48:1976–9. doi: 10.1161/STROKEAHA.117.017235
32. McTaggart RA, Moldovan K, Oliver LA, Dibiasio EL, Baird GL, Hemendinger ML, et al. Door-in-door-out time at primary stroke centers may predict outcome for emergent large vessel occlusion patients. Stroke. (2018) 49:2969–74. doi: 10.1161/STROKEAHA.118.021936
33. Lin E, Calderon V, Goins-Whitmore J, Bansal V, Zaidat O World's first 24/7 mobile stroke unit: Initial 6-month experience at mercy health in Toledo, Ohio. Front Neurol. (2018) 9:283. doi: 10.3389/fneur.2018.00283
34. Belt GH, Felberg RA, Rubin J, Halperin JJ. In-transit telemedicine speeds ischemic stroke treatment: preliminary results. Stroke. (2016) 47:2413–5. doi: 10.1161/STROKEAHA.116.014270
35. Taqui A, Cerejo R, Itrat A, Briggs FB, Reimer AP, Winners S, et al. Reduction in time to treatment in prehospital telemedicine evaluation and thrombolysis. Neurology. (2017) 88:1305–12. doi: 10.1212/WNL.0000000000003786
36. Wu TC, Parker SA, Jagolino A, Yamal JM, Bowry R, Thomas A, et al. Telemedicine can replace the neurologist on a mobile stroke unit. Stroke. (2017) 48:493–6. doi: 10.1161/STROKEAHA.116.015363
37. Walter S, Grunwald IQ, Helwig SA, Ragoschke-Schumm A, Kettner M, Fousse M, et al. Mobile stroke units - cost-effective or just an expensive hype? Curr Atheroscler Rep. (2018) 20:49. doi: 10.1007/s11883-018-0751-9
38. Yamal JM, Rajan SS, Parker SA, Jacob AP, Gonzalez MO, Gonzales NR, et al. Benefits of stroke treatment delivered using a mobile stroke unit trial. Int J Stroke. (2018) 13:321–7. doi: 10.1177/1747493017711950
39. Monks T, Pitt M, Stein K, James MA. Hyperacute stroke care and NHS England's business plan. BMJ. (2014) 348:e3049. doi: 10.1136/bmj.g3049
40. Morris S, Ramsay AIG, Boaden RJ, Hunter RM, McKevitt C, Paley L, et al. Impact and sustainability of centralising acute stroke services in English metropolitan areas: retrospective analysis of hospital episode statistics and stroke national audit data. BMJ. (2019) 364:l1. doi: 10.1136/bmj.l1
41. Stroke patients in England set to receive revolutionary new treatment. NHS England (2017). Available online at: https://www.england.nhs.uk/2017/04/stroke-patients-in-england-set-to-receive-revolutionary-new-treatment (accessed March 23, 2019).
Keywords: stroke, mobile stroke unit, optimization, google maps, endovascular clot retrieval
Citation: Phan TG, Beare R, Srikanth V and Ma H (2019) Googling Location for Operating Base of Mobile Stroke Unit in Metropolitan Sydney. Front. Neurol. 10:810. doi: 10.3389/fneur.2019.00810
Received: 29 March 2019; Accepted: 15 July 2019;
Published: 06 August 2019.
Edited by:
Ayrton R. Massaro, Hospital Sírio-Libanês, BrazilReviewed by:
Silvia Schönenberger, Heidelberg University Hospital, GermanySimone Beretta, Azienda Ospedaliera San Gerardo, Italy
Copyright © 2019 Phan, Beare, Srikanth and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thanh G. Phan, dGhhbmgucGhhbiYjeDAwMDQwO21vbmFzaC5lZHU=
 Thanh G. Phan
Thanh G. Phan Richard Beare
Richard Beare Velandai Srikanth
Velandai Srikanth Henry Ma
Henry Ma