
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 02 July 2019
Sec. Stroke
Volume 10 - 2019 | https://doi.org/10.3389/fneur.2019.00708
This article is part of the Research Topic Geospatial and Transport Modeling in Stroke Service Planning View all 13 articles
Background and Purpose: Endovascular clot retrieval (ECR) has revolutionized acute stroke therapy but is expensive to run and staff with accredited interventional neuroradiologists 24/7; consequently, it is only feasible for each metropolitan city to have a minimum number of hubs that is adequate to service the population. This method is applied to search the minimum number of hospitals to be designated as ECR hubs in Sydney as well as the population at risk of stroke reachable within 30 min.
Methods: Traveling time from the centroids of each suburbs to five ECR capable hubs [Royal Prince Alfred/RPA, Prince of Wales/POW, Royal North Shore/RNS, Liverpool/LH and Westmead/WH]. This step was performed using ggmap package in R to interface with Google Map application program interface (API). Next, we calculate the percentage of suburbs within each catchment in which traveling time to the ECR hub is <30 min. This step was performed for all possible combination of ECR hubs. The maps are available at https://gntem3.shinyapps.io/ambsydney/. The population at risk of stroke was estimated using stroke incident studies in Melbourne and Adelaide.
Results: The best 3-hospital combinations are LPH/WH/RNS (82.3, 45.7, and 79.7% of suburbs reachable within 30 min or 187 of 226 suburbs) follow by RPA/LPH/RNS (100.0, 80.9, and 73.1% of suburbs) and LPH/POW/RNS (83.3, 90.7, and 76.6% of suburbs). The best 4-hospital model is LPH/WH/POW/RNS (84.2%, 91.1%, 90.7%, 77.8%). In the 5-hospital model, ECR is available for 191 suburbs within 30 min: LPH (83%), RPA (100%), WH (90.2%), RNS (72.7%), POW (88.9%). Based on 3-hospital model and 15% of patient eligible for ECR, the expected number of cases to be handled by each hospital is 465. This number drops down to 374 if a 4-hospital model is preferred.
Conclusions: The simulation studies supported a minimum of 4 ECR hubs servicing Sydney. This model provides data on number of suburbs and population at risk of stroke that can reach these hubs within 30 min.
Recent advances in stroke therapy has generated debate on translating clinical trial findings to service the entire population (1–6). This is an issue which come to the attention of mainstream media from time to time when the ability of the team to provide 24/7 did not meet public expectation (7). This case in 2016 illustrated that even 1 year after publications the ECR trials, the ability to translate findings into clinical practice can remain elusive. It is possible that the enormous logistic required to bring together a highly skilled teams comprising of interventional neuroradiologists (INR), stroke (vascular) neurologists, support staff (anesthetists, neurosurgeons, trainee doctors, radiographers, and nurses), and dedicated angiography suites and bed availability financially supported by the government (8).
In Australia, the state of Victoria and South Australia have set up a statewide service protocol (9) for ECR immediately after the publication of the ECR trials (1–6). This idea is similar to the concept of comprehensive stroke center (CSC) but with a difference that the CSC provide care for the catchment and also outlying rural areas (10). In this framework, two hospitals were designated as ECR hubs from a pool of 4 ECR capable hospitals. These ECR hubs are required to provide a 24 h service not just for patients in their immediate local catchment but also for all residents of the states. Using a data driven approach, we showed that it was possible to service most of Melbourne within 30 min with 2 ECR hubs (11). In this paper, an idealized time of 30 min is used based on the modeling in the redesign of stroke service in London (12). A similar process has been developed in South Australia, with one hospital providing ECR service from a pool of 3 ECR capable hospitals. Such a service is in development in Sydney, New South Wales but as yet an official policy statement has not been released (13). Using method for mapping catchment areas in Melbourne and Adelaide (11), we apply similar approach to search the minimum number of hospitals to be designated as ECR hubs in Sydney. Further, we estimate the ECR case load for each combination of hospital to help determine the minimum number of hospitals required as ECR hubs.
Sydney is the capital city of the state of New South Wales, Australia with a population density of approximately 407 person per km2 in greater Sydney (https://www.abs.gov.au/). Excluding the surrounding parks, the population density is 1237 person per km2. The postcodes for metropolitan Sydney are in the range 2000–2234, 2555–2567, 2761–2768. The 2016 census data from each postal area in New South Wales can be obtained from https://datapacks.censusdata.abs.gov.au/datapacks/. The number of strokes was estimated using the census data for each age band and the stroke incidence study in Melbourne and Adelaide (14, 15). This study involves simulations (no patient data are used) and as such received a waiver from the Monash Health Human Research Ethics Committee.
At present there is no official statewide protocol for ECR in Sydney (https://www.aci.health.nsw.gov.au/networks/stroke). There are five hospitals (Royal Prince Alfred/RPA, Prince of Wales/POW, Royal North Shore/RNS, Liverpool/LH and Westmead/WH) capable of acting as ECR hubs. The John Hunter Hospital provides ECR service in Newcastle, 162 km to the North of Sydney. This hospital (postcode 2305) is not considered as part of Sydney catchment. Each of the ECR capable hospitals were considered as a potential ECR hub for the simulation. Membership of a hub was determined using logical comparison of traveling time from each address to the different ECR hospitals. Within each catchment, we calculate the percentage of suburbs in which traveling time to the ECR hub is <30 min. This step was performed for all possible combinations of ECR hubs. The locations of the ECR capable hospitals relative to these arterial roads can be seen in Figures 1, 2. The best combination of ECR hubs were defined according to travel time.
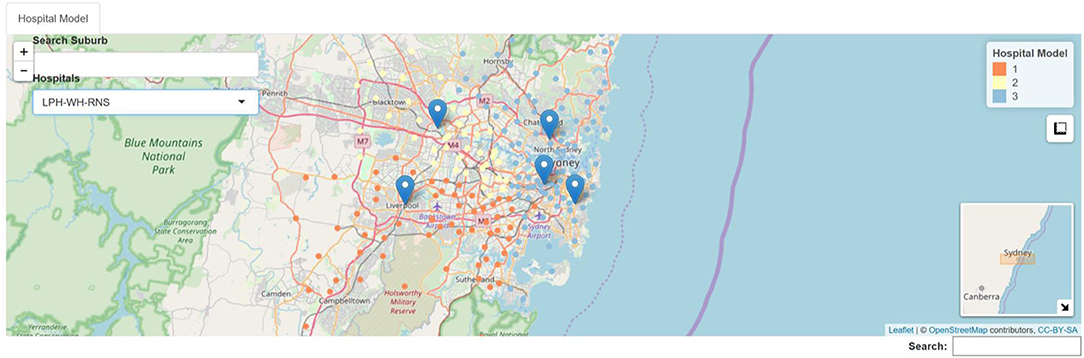
Figure 1. Example of 3 hospital model. RNS, Royal North Shore Hospital, light blue; LPH, Liverpool Hospital, orange; WH, Westmead Hospital, light yellow.
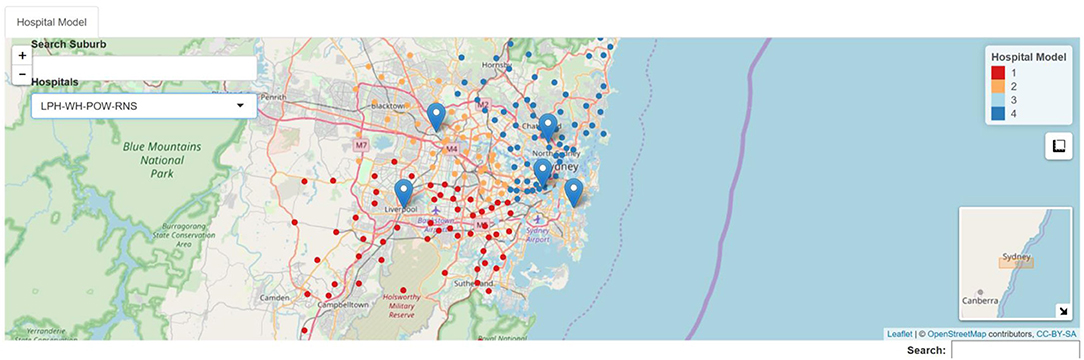
Figure 2. Example of 4 hospital model. RNS, Royal North Shore Hospital, blue; LPH, Liverpool Hospital, red; WH, Westmead Hospital, orange, POW, Prince of Wales Hospital, light blue.
We used ggmap package R (R Project for Statistical Computing, version 3.4.4) to query Google Map application program interface (API) (https://developers.google.com/maps/) (16). The transport times to each hospital from each suburb centroid were computed for morning peak hour traffic.
Results of analyses were displayed as interactive web-based maps using R package leaflet and tiles from OpenStreetMap (©OpenStreetMap contributors. For copyright see www.openstreetmap.org/copyright) (17). These maps were uploaded using Shiny onto the web (RStudio Inc) available at https://gntem3.shinyapps.io/ambsydney/.
The results are available in Table 1 and on the web. The best 3-hospital combinations are LPH/WH/RNS (82.3, 45.7, and 79.7% of suburbs reachable within 30 min or 187 of 226 suburbs) follow by RPA/LPH/RNS (100.0, 80.9, and 73.1% of suburbs reachable within 30 min, 184 of 226 suburbs) and LPH/POW/RNS (83.3, 90.7, and 76.6% of suburbs reachable within 30 min, 184 of 226 suburbs).
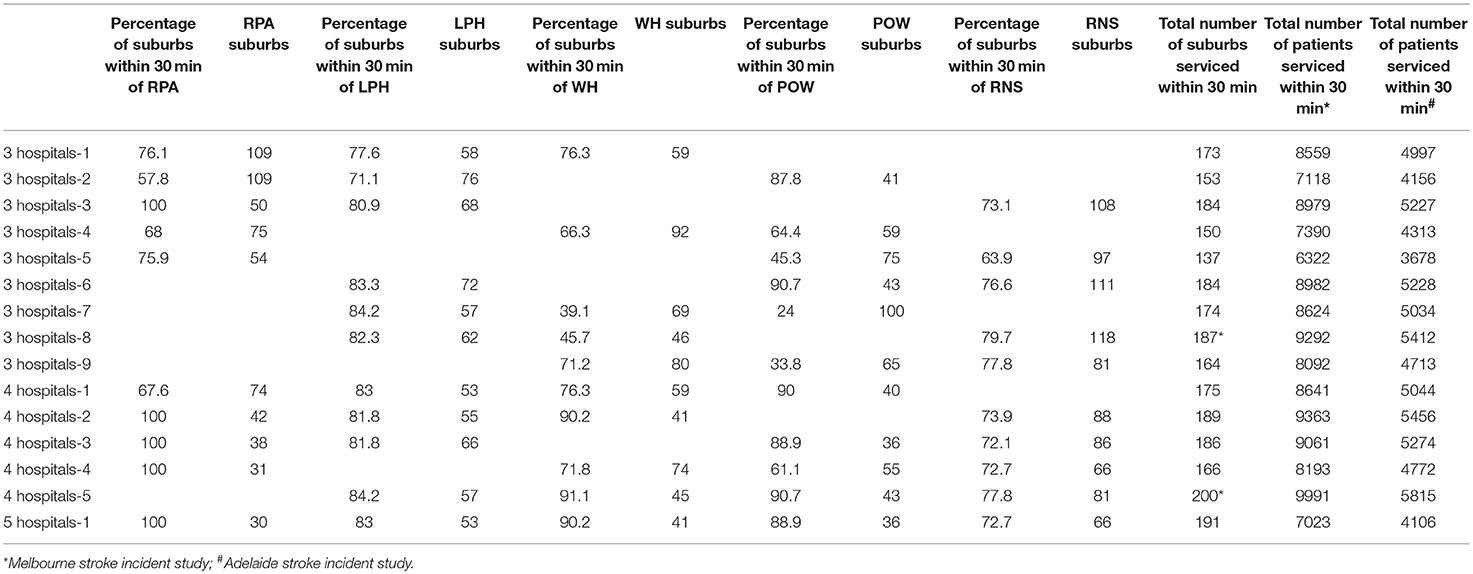
Table 1. Traveling time and coverage area for different combinations of ECR hub models in metropolitan Sydney.
The best 4-hospital model is LPH/WH/POW/RNS (84.2%, 91.1%, 90.7%, 77.8% reachable within 30 min or 200 of 226 suburbs). This model provides better coverage than the next best 4-hospital model (RPA/LPH/WH/RNS) by 11 suburbs and the next best 3-hospital model (LPH/WH/RNS) by 13 suburbs.
In the 5-hospital model, ECR is available for 191 suburbs within 30 min: LPH (83%), RPA (100%), WH (90.2%), RNS (72.7%), POW (88.9%). The 5-hospital model is not superior to the 4-hospital model because RPA is situated in the center of LPH/WH/POW/RNS.
The estimated number of patients that can be treated with each model for each hospital are provided in Table 2. The maximum estimated population reachable within 30 min is observed in 3-hospital model 8 (LPH/WH/POW−9292 cases), follow by model 6 (LPH/POW/RNS−8982 cases) and by model 1 (RPA/LPH/WH−8559 cases). The maximum estimated population reachable within 30 min is observed in 4-hospital model 5 (LPH/WH/POW/RNS−9991 cases), follow by model 2 (RPA/LPH/WH/RNS−9363 cases).
The number are lower if based on the Adelaide stroke incident study (15) and higher if based on Melbourne stroke incident study (see Table 1) (14). These hospitals serviced the largest population at risk of stroke. Based on 3-hospital model and 15% of patient eligible for ECR, the expected number of cases to be handled by each hospital is 465. This number drops down to 374 if a 4-hospital model is preferred.
In this study, we have used data driven method to map service boundaries for ECR hubs based on Google Map API estimate of travel time to the hub in Sydney. We estimated that the minimum number of hubs to service Sydney is 4 based on the number of suburbs and population at risk. Further below we will discuss if it is possible to have 4 ECR hubs given availability of INR in Sydney, Australia. Our extension of the methodology to estimation of population at risk will be useful for planning capacity of health services.
In our initial publication on the map of ECR hub catchment for Melbourne, we were challenged by the reviewers to demonstrate that the method could be applied elsewhere (11). We subsequently added the catchment area of ECR hubs for Adelaide, Australia, and now Sydney, Australia (11). Other investigators have described the use of Google Map API for modeling stroke services in North America (18). As such, we postulate that the method can be applied to any international locations serviced by Google Map API and for any time-dependent conditions such as acute coronary syndrome (19). There are several countries, such as Republic of Korea (South Korea) and People's Republic of China, where Google Map API may not be the optimal tool; Google Map API is available for use in Republic of China (Taiwan).
The use of geographical information systems for health service design is evolving since 2017 with several publications in the journal Stroke and Jama Neurology (11, 18, 20–22). In this study, we have accessed Google Map API for traffic data due to our familiarity with this platform (11). There are other platforms such as Bing Map API (tarifX and tarifX.geo packages in R), Yahoo (https://github.com/trestletech/rydn) and Baidu Map (https://github.com/badbye/baidumap). Outside of the R environment, there is package in Python for performing geospatial analysis (23) and investigators have also used Matlab (MathWorks@) for accessing Google Map API (18). Google Map API has a constraint in that it allows only 2500 queries per day; it charges for additional queries.
The data driven method described here show that selection of ECR hubs for other cities cannot be empirically inferred directly from the Melbourne or Adelaide models. This is likely the case since each city has their individual geography, arterial roads, and locations of ECR capable hospitals. Using the idealistic notion of a maximum 30 min traveling time to the ECR hospital, we can assess the ECR hub location which best suits this requirement. In Sydney, it would appear that the optimal models for 3-hospital and 4-hospital models are combinations of LPH/WH/RNS and LPH/WH/POW/RNS. The suburbs serviced by these hospitals have the largest population at risk of stroke. It is likely that the geography of Sydney makes it difficult to service the population with a small number of ECR hubs such as the case in Melbourne. By comparison, >85% of patients can arrive within 30 min with just 2 ECR hub model in Melbourne (11).
The issue of transport to the most appropriate hospital has been the focus of recent research regarding “drip and ship vs. direct to comprehensive stroke center” (20, 24). These strategies were not evaluated here as that is not the intention of this study. A question arises as to the compatibility of the approach based on 30 min trip to ECR hub and “drip and ship” model of care. Our model provides a mean to address this question directly by showing that a large part of Sydney can be reached within 30 min and thus a direct trip to “mothership” ECR hub is possible. These estimates of the population at risk should not be seen as an endorsement of the strategies of sending all patients to ECR hubs. Rather the estimates are provided as a mean to evaluate the capacity of the system to handle the ECR case load. The ability to handle all caseload is part of the equation in the approach to “drip and ship” vs. direct to “mothership” hub conundrum. There has been an increase number of ECR cases since 2015 (25). However, it has been estimated that approximately 84 to 90% cases do not go on to ECR. In this situation the medical stroke code team can be overwhelmed unless some strategies are put in place to limit the transfer of cases to ECR hub (26). A similar strategy that takes into account the population serviced is used in the evaluation of stroke service in England (27). Even with 4-hospital model the average annual ECR case load is 374. This number is a significant challenge to individual ECR hub and a centralized flexible model is required to return patients to a non-ECR hospital nearest to their residential addresses after acute clot retrieval (12). At present such a flexible model had been described with the London reconfiguration but the durability of the repatriation model is not known. A model for repatriation does not yet exist for ECR in Australia. The Victorian statewide protocol emphasizes repatriation of patients back to referring hospital after ECR. However, it does not provide a mean to enforce the referring hospital to accept the patient once repatriation at present (28). Stroke experts will need to actively engage with local government, chief executives of all hospitals, including ambulance services to design these aspects of statewide ECR services.
In discussion on ambulance transport, one often hypothesizes that ambulances arrive faster at destination when using lights and sirens compares to estimations of travel time by Google Map API. We had compared the travel time between observed (ambulance) and simulated travel time by Google Map API and found minimal difference (approximately 3.5 ± 2.5 min) (11). In Australia, ambulance officers are required to obey traffic light and signs, and required to stop at traffic light, check road condition before crossing road intersections. Google Map API provides direction in accordance with traffic regulations (no traveling in the opposite lane). In some cases, estimation of travel time was much faster by Google Map API. It is possible that when Google Map API provides estimate of best-case scenario, it simulates traffic condition in which all traffic lights are green. This effect may be akin to the emergency vehicle prioritization (EVP) protocol. To our knowledge the EVP system is being trial in Queensland but has not been implemented in Adelaide, Melbourne nor Sydney (29).
Our study has several limitations. The simulations were made under certain assumptions about the interventional neuroradiologists (INR) workforce. In the development of the Victorian ECR model, each site was required to have at least 3 accredited INR (28). The register of accredited INR in the State of New South Wales is available at this web address (http://www.ccinr.org.au/register accessed 23/3/19). With 13 available INR, the number of ECR hubs that can be served would be 4. Taking into account the ECR hub in John Hunter Hospital, there would be just sufficient INR to staff 3 ECR hubs in Sydney. Our proposed model requires that the interventional neuroradiologists are not simultaneously on-call at two ECR hub and that each hub has two angiograph suites. The issue of INR rostering is not a just a theoretical concern with a recent coronial inquest over availability of INR in Adelaide, Australia (30). In the event of such staffing shortage or angiographic suite being used for another reason, the model does not hold true as there is a time cost of transporting the patient and additional cost of transporting the interventional neuroradiologist. In an earlier study of cardiac revascularization service, we had shown the impact staff residential location on providing timely service (19). In that study only 45% of inner Melbourne and 56% of outer Melbourne staff could reach hospital within 30 min. Such considerations were not performed here as it would require access to personal data. Our emphasis on 30 min to hospital can be interpreted as too stringent for other countries or a need for centralization of service. Investigators reported that access to access to intravenous-capable hospitals within 60 min was available to 81% of US population and 56% had access to endovascular-capable hospitals (31). In this analysis, we have not considered ECR experiences, interventional neuroradiologists or infrastructure at a potential hub. Of the 5 potential hubs in Sydney, only RNS and WH had participated in the recent ECR trial (5, 32). While services within each hub can be re-organized with increased funding, it is possible that a bottle neck in the consideration of a site for ECR hub is the availability of interventional neuroradiologists.
Our use of ggmap package and which relies on Google Map API has several drawbacks. Principally, Google Map cannot be used to predict future traveling time. Future scenarios can be performed using purpose built strategic model for each state of Australia (33). Further, the ggmap package requires modification to perform trip estimation at different time of day. Some of the newer packages in R such as googleway permits specification of time of travel (34). In this study we were reassured in that the results from ggmap had differed from real ambulance trips by 3 to 5 min in an earlier study (11).
Another limitation of our approach is the reliance on population based studies in other cities within Australia to estimate the number of stroke patients (14, 15). These studies showed a decline in the number of stroke cases over time and it is not certain if our projections do not overestimate the number of stroke cases and which can impact on configuration of ECR hubs. One approach would be to use a current estimate of the number of stroke cases in Sydney. This data is not available at the time of this analysis.
In summary, we estimated the minimum number of ECR hubs to service Sydney and the optimal combination of sites. The choice of sites and their combinations depends on the government agencies and policy makers.
TP is on the Advisory Board of Genzyme on Fabry Disease and has received payment for lectures including service on speakers' bureaus for Bayer, Boehringer Ingelheim, Pfizer and Genzyme.
The datasets generated for this study are available on request to the corresponding author.
TP: design, analysis, and writing manuscript. RB, VS, and HM: writing manuscript.
VS is the recipient of a National Health and Medical Research Foundation of Australia/National Heart Foundation Career Development Fellowship.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Figures provided in the web link (https://gntem3.shinyapps.io/ambsydney/) were created using data© OpenStreetMap contributors and tiles from osm.org. The data is available under the Open Database License while the tiles are available under Creative Commons Attribution-ShareAlike 2.0 license. Details are available at www.openstreetmap.org/copyright. The maps were created using the OpenStreetMap tiles but does not suggests the licensor endorses the use of this map.
1. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. (2015) 372:11–20. doi: 10.1056/NEJMoa1411587
2. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet. (2016) 387:1723–31. doi: 10.1016/S0140-6736(16)00163-X
3. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. (2015) 372:1019–30. doi: 10.1056/Nejmoa1414905
4. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. (2015) 372:2296–2306. doi: 10.1056/NEJMoa1503780
5. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. (2015) 372:1009–18. doi: 10.1056/NEJMoa1414792
6. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-pa vs. T-pa alone in stroke. N Engl J Med. (2015) 372:2285–95. doi: 10.1056/NEJMoa1415061
7. Alexander H. Sydney Morning Herald. (2016). Available online at: https://www.Smh.Com.Au/healthcare/stroke-patients-missing-out-on-lifesaving-treatment-after-hours-20161006-grw1qh.Html (accessed March 23, 2019).
8. Smith EE, Schwamm LH. Endovascular clot retrieval therapy: implications for the organization of stroke systems of care in north america. Stroke. (2015) 46:1462–7. doi: 10.1161/STROKEAHA.115.008385
9. Hand P. Statewide Frameworks for Acute Stroke Services. Available online at: https://www2.health.vic.gov.au/hospitals-and-health-services/quality-safety-service/clinical-networks/clinical-network-stroke/stroke-statewide-frameworks (accessed January 24, 2017).
10. Alberts MJ, Latchaw RE, Jagoda A, Wechsler LR, Crocco T, George MG, et al. Revised and updated recommendations for the establishment of primary stroke centers: a summary statement from the brain attack coalition. Stroke. (2011) 42:2651–65. doi: 10.1161/STROKEAHA.111.615336
11. Phan TG, Beare R, Chen J, Clissold B, Ly J, Singhal S, et al. Googling service boundaries for endovascular clot retrieval hub hospitals in a metropolitan setting: Proof-of-concept study. Stroke. (2017) 48:1353–61. doi: 10.1161/STROKEAHA.116.015323
12. Fulop N, Boaden R, Hunter R, McKevitt C, Morris S, Pursani N, et al. Innovations in major system reconfiguration in england: a study of the effectiveness, acceptability and processes of implementation of two models of stroke care. Implement Sci. (2013) 8:e5. doi: 10.1186/1748-5908-8-5
13. Hwang YT, Gawarikar Y. Clot retrieval and acute stroke care. Med J Aust. (2017) 207:361. doi: 10.5694/mja17.00526
14. Thrift AG, Dewey HM, Macdonell RA, McNeil JJ, Donnan GA. Stroke incidence on the east coast of australia: the north east melbourne stroke incidence study (nemesis). Stroke. (2000) 31:2087–92. doi: 10.1161/01.STR.31.9.2087
15. Leyden JM, Kleinig TJ, Newbury J, Castle S, Cranefield J, Anderson CS, et al. Adelaide stroke incidence study: declining stroke rates but many preventable cardioembolic strokes. Stroke. (2013) 44:1226–31. doi: 10.1161/STROKEAHA.113.675140
16. Kahle D, Wickham H. Ggmap: Spatial visualization with ggplot2. R J. (2013) 5:144–61. doi: 10.32614/RJ-2013-014
17. Cheng J, Xie Y, Wickham H, Agafonkin V. Leaflet: Create Interactive web Maps With the Javascript ‘leaflet’ Library. Available online at: https://cran.r-project.org/web/packages/leaflet/leaflet.pdf (accessed January 24, 2017).
18. Milne MS, Holodinsky JK, Hill MD, Nygren A, Qiu C, Goyal M, et al. Drip 'n ship versus mothership for endovascular treatment: Modeling the best transportation options for optimal outcomes. Stroke. (2017) 48:791–4. doi: 10.1161/STROKEAHA.116.015321
19. Cole J, Beare R, Phan TG, Srikanth V, MacIsaac A, Tan C, et al. Staff recall travel time for st elevation myocardial infarction impacted by traffic congestion and distance: a digitally integrated map software study. Front Cardiovasc Med. (2017) 4:89. doi: 10.3389/fcvm.2017.00089
20. Holodinsky JK, Williamson TS, Kamal N, Mayank D, Hill MD, Goyal M. Drip and ship versus direct to comprehensive stroke center: conditional probability modeling. Stroke. (2017) 48:233–8. doi: 10.1161/STROKEAHA.116.014306
21. Nogueira RG, Silva GS, Lima FO, Yeh YC, Fleming C, Branco D, et al. The fast-ed app: A smartphone platform for the field triage of patients with stroke. Stroke. (2017) 48:1278–84. doi: 10.1161/STROKEAHA.116.016026
22. Holodinsky JK, Williamson TS, Demchuk AM, Zhao H, Zhu L, Francis MJ, et al. Modeling stroke patient transport for all patients with suspected large-vessel occlusion. JAMA Neurol. (2018) 75:1477–86. doi: 10.1001/jamaneurol.2018.2424
23. Boeing G. Osmnx: new methods for acquiring, constructing, analyzing, and visualizing complex street networks. Comput Environ Urban Syst. (2017) 65:126–39. doi: 10.31235/osf.io/q86sd
24. Froehler MT, Saver JL, Zaidat OO, Jahan R, Aziz-Sultan MA, Klucznik RP, et al. Interhospital transfer before thrombectomy is associated with delayed treatment and worse outcome in the stratis registry (systematic evaluation of patients treated with neurothrombectomy devices for acute ischemic stroke). Circulation. (2017) 136:2311–21. doi: 10.1161/CIRCULATIONAHA.117.028920
25. Smith EE, Saver JL, Cox M, Liang L, Matsouaka R, Xian Y, et al. Increase in endovascular therapy in get with the guidelines-stroke after the publication of pivotal trials. Circulation. (2017) 136:2303–10. doi: 10.1161/CIRCULATIONAHA.117.031097
26. Man S, Zhao X, Uchino K, Hussain MS, Smith EE, Bhatt DL, et al. Comparison of acute ischemic stroke care and outcomes between comprehensive stroke centers and primary stroke centers in the united states. Circ Cardiovasc Qual Outcomes. (2018) 11:e004512. doi: 10.1161/CIRCOUTCOMES.117.004512
27. Allen M, Pearn K, Villeneuve E, James M, Stein K. Planning and providing acute stroke care in england: The effect of planning footprint size. Front Neurol. (2019) 10:150. doi: 10.3389/fneur.2019.00150
28. Hand P. Statewide Frameworks for Acute Stroke Services (2016). Available online at: https://www2.health.vic.gov.au/hospitals-and-health-services/quality-safety-service/clinical-networks/clinical-network-stroke/stroke-statewide-frameworks (accessed January 24, 2017).
29. Williams P. Available online at: https://www.Abc.Net.Au/news/2015-11-22/queensland-ambulance-fire-service-new-traffic-light-technology/6961982. 2015
30. Opie R. Available online at: https://www.Abc.Net.Au/news/2017-08-03/rah-radiologist-criticised-for-rostering-before-stroke-deaths/8770932. 2017
31. Adeoye O, Albright KC, Carr BG, Wolff C, Mullen MT, Abruzzo T, et al. Geographic access to acute stroke care in the united states. Stroke. (2014) 45:3019–24. doi: 10.1161/STROKEAHA.114.006293
32. Campbell BCV, Mitchell PJ, Churilov L, Yassi N, Kleinig TJ, Dowling RJ, et al. Tenecteplase versus alteplase before thrombectomy for ischemic stroke. N Engl J Med. (2018) 378:1573–82. doi: 10.1056/NEJMoa1716405
33. Rashidi TH, Kanaroglou P. The next generation of transportation demand models, toward an interdisciplinary science. In: Miller EJ, Roorda MJ, editors. International Association for Travel Behaviour Research Book. Bingley: Emerald Group Publishing (2013). p. 201–229.
34. Cooley D. Accesses Google Maps APIs to Retrieve Data and Plot Maps [Googleway Vignette] (2017). Available online at: https://cran.r-project.org/web/packages/googleway/index.html
Keywords: clot retrieval, stroke, geospatial, Google Map API, optimization, simulation
Citation: Phan TG, Beare R, Srikanth V and Ma H (2019) Googling Service Boundaries for Endovascular Clot Retrieval (ECR) Hub Hospitals in Metropolitan Sydney. Front. Neurol. 10:708. doi: 10.3389/fneur.2019.00708
Received: 23 March 2019; Accepted: 17 June 2019;
Published: 02 July 2019.
Edited by:
Guillaume Turc, Centre Hospitalier Sainte-Anne, FranceReviewed by:
Alexander Tsiskaridze, Tbilisi State University, GeorgiaCopyright © 2019 Phan, Beare, Srikanth and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thanh G. Phan, dGhhbmgucGhhbkBtb25hc2guZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.